Abstract
Back ground
Complex gap nonunion of tibia following open fractures and osteomyelitis with pathological fractures in children is a treatment challenge with unpredictable outcome. Treatment options available are bone transport, bone grafting, induced membrane technique, allograft reconstruction and Huntington procedure (ipsilateral transposition of vascularized fibula). There is no consensus in the literature about which technique is optimal in the given situation. The purpose of the present study is to evaluate the role of Huntington procedure in the management of complex gap nonunion of tibia in paediatric patients.
Material and method
Eighteen patients (11 males and 7 females) with a mean age of 8.4 years (range 3–12 years) having complex gap nonunion of tibia with an average bone defect of 6.6 cm (range 5–17 cm) were treated with Huntington procedure between June 2008 to December 2016. The mean follow-up was 4.3years (range 3.5–6 years).
Result
Union was seen in all except one, with an average time to union being 11.5 weeks and13.8 weeks at proximal and distal tibio-fibular synostosis respectively. Revision plating was done in one patient with nonunion. Hypertrophy of fibula was seen in all patients. One patient developed 15° ankle varus and required corrective osteotomy. Ankle was fixed in equinus in three patients with a mean value of 13.3° (range 5°–25°). Lambrinaudi procedure was done to correct 25° fixed ankle equinus in one patient. Fixed flexion deformity of knee was seen in nine patients with a mean value of 9.7° (range 5°–20°). Two patients had iatrogenic foot drop; one recovered completely and one had only partial recovery. Shortening was seen in eight patients with a mean value of 3.5 cm (range 1–5 cm). At final evaluation 9 patients were very satisfied, 8 satisfied and 1 was dissatisfied.
Conclusion
Huntington procedure is a useful limb salvage surgery for complex gap nonunion of tibia in children. However; further improvements in the surgical technique are needed to increase the patient satisfaction by reducing the risk of complications.
Keywords: Trauma, Osteomyelitis, Gap nonunion, Tibia, Children, Huntington surgery
1. Introduction
Complex gap nonunion of long bones is associated with bone loss, infection and compromised soft tissue envelop.1,2 Complex gap nonunion of tibia in children may follow haematogenous osteomyelitis as well as open fractures, despite multiple attempts to achieve fracture union and control of infection. The problem is of special concern in developing countries due to ignorance, prevalent quackery and lack of adequate health facilities in the remote areas.
Various surgical techniques available to manage complex gap nonunion of tibia include, bone transport using the Ilizarove frame,3 non-vascular4,5 and free vascularized bone grafting techniques,6,7 induced membrane (Masquelet) technique8,9 and allograft reconstruction.10,11 Each of these surgical techniques has its own merits and demerits and cannot be practiced universally owing to issues inherent to each of these techniques.12, 13, 14, 15, 16, 17 Final outcome may be unpredictable and survival of the limb may be threatened even in best hands.
Huntington procedure involves ipsilateral transposition of vascularized fibula and has been used both in children as well as adults, to manage complex segmental bone defects of tibia for diverse indications including trauma and infection.18, 19, 20, 21, 22 Although Huntington procedure is claimed to be an easy and cost effective treatment option for limb salvage in complex gap nonunion of tibia; there are reports of complications like delayed and nonunion, shortening, deformity, joint stiffness and stress fracture of the fibula.23,24 Therefore, the aim of present study was to evaluate the role of Huntington procedure in the management of complex gap nonunion of tibia in paediatric patients.
2. Methods
This was a retrospective study done between June 2008 to December 2016 after approval from institutional ethical committee. The inclusion criteria were patients having complex gap nonunion of tibia with, intact or united fibula, preserved sensation in the sole, adequate vascularity and soft tissue cover in the involved limb. Patients with impaired sensations at sole and those with signs of limb ischemia and inadequate soft tissue cover that precluded the closure of the wound at the time of Huntington procedure were excluded from the study. After application of inclusion and exclusion criteria 18 out of 24 patients were found eligible for the study. Medical records of all 18 eligible patients (male = 11, female = 7) with mean age of 8.4 (range 3–12 years) who underwent Huntington procedure for complex gap nonunion of tibia were studied.
For each patient the duration of disease, number and nature of surgeries done prior to Huntington procedure were recorded. A routine orthogonal radiographic analysis was done for each patient. No pre-operative arteriography was done. A gap nonunion was defined as when there was no radiographic contact between proximal and distal fragments of tibia seen in two orthogonal views and it was measured at a point at which 50% of the diameter of the proximal fragment to the corresponding point on distal fragment on a radiograph.
Debridement and sequestrectomy was done to successfully control infection in all patients except one before doing Huntington procedure. All patients underwent Huntington procedure in two stages except one. All surgeries were done under regional or general anesthesia on a plane operation table. During stage 1 surgery proximal fibula and corresponding tibia was exposed through a single anterolateral skin incision. The neurovascular bundle in the anterior compartment was preserved. We tried to osteotomise the fibula sufficiently proximal to lower end of proximal tibial fragment to facilitate the fixation of resulting tibio-fibular synostosis using 4.5 mm cortical screws with or without supplemental k wire. When a very short bone fragment precluded screw placement only k wire were used to secure tibio-fibular synostosis. After surgery limb was kept in an above knee plaster of Paris (pop) splint for an average 11.1 weeks (range 8wks–18wks) till there was clinico-radiological evidence of union. This was followed by stage 2 surgery, done in a similar fashion in which distal fibular osteotomy was done and, resulting distal tibiofibular synostosis was fixed with an appropriate implant. After surgery limb was kept in an above knee pop splint for an average duration of 13.8weeks (range 8wks–21wks) till there was clinico-radiological evidence of union. At this time above knee cast was converted to PTB (patella Tendon bearing) cast or caliper, partially weight bearing walk allowed initially followed by full weight bearing walk for next 12–18 months to allow hypertrophy of fibula so as to minimize the chances of stress fracture.
Except in difficult cases, we preferred to centralize the fibula by inserting the osteotomised end of the fibula into the medullary canal of tibia for better alignment.
Two patients underwent distal tibio-fibular synostosis as stages 1 surgery both having gap nonunion of tibia due to osteomyelitis. One patient underwent only proximal tibio-fibular synostosis as patient was reluctant for stage 2 surgery till his last follow-up.
Initially all patients were followed up clinico-radiologically at 6 weeks interval for first six months, followed by 3 monthly visit for next six months and thereafter every six months or whenever required till final follow-up. The average duration of clinico-radiological follow up was 4.3years (range 3.5–6 years). All patients were assessed for various clinico-radiological parameters like bone healing, implant failure, fibular hypertrophy among others. Final outcome evaluation was done based on functional, clinical and radiological parameters. The parameters assessed in each category include , school attendance, outdoor playing activities, pain score (on a scale of 1–10, where 1 is no pain and 10 is unbearable pain), movements and deformities at knee and ankle. Limb length discrepancy was also taken into consideration. Based on these parameters final outcome was categorized as very satisfied, satisfied and dissatisfied. Som P Gupta et al. used Huntington procedure to manage large bone defects in children and evaluated final outcome using identical parameters.25
3. Results
The most common underlying cause of complex gap nonunion of tibia in the present study was trauma (n = 12) followed by infection (n = 6). Average size of the bone defect was 6.6 cm (range 5 cm–17cm). The most common location of bone defect in tibia was in the middle 1/3rd in post-traumatic cases and proximal 1/3rd in post osteomyelitic cases. Average time between stage 1 and 2 surgery was 11.1 weeks (range 8–18 weeks). Bone union occurred in 17 (94.4%) out of 18 patients. Nonunion was seen in one (5.6%) patient. The average time to radiological union was 11.5weeks (range 8–37 weeks) and 13.8 weeks (range 8–18 weeks) at proximal and distal tibio-fibular synostosis respectively. Hypertrophy of fibula was evident radiologically at one year follow-up in majority of patients. One patient with 17 cm segmental defect developed stress fracture of fibula.
The mean range of motion (ROM) at knee joint was 117.7° (range 100°–130°) excluding patients with fixed flexion deformity of knee. Nine patients had fixed flexion deformity of knee joint with a mean value of 9.7° (range 5°–20°). The average value of planter flexion was 13.3° (range 10°–20°) and dorsiflexion was 7.4° (range 5°–15°). Calculation of mean planter and dorsiflexion excluded three patients with a mean fixed equinus deformity of 6.6° (5°-10°) at ankle and another three (n = 3) patients with their ankle fixed in equinus with a mean value of 13.3° (5°-25°). Two patients had foot drop due to iatrogenic Common Peroneal nerve injury. One had complete recovery at one year follow-up, second case had partial recovery. Ankle varus of 15 seen in one patient was corrected by osteotomy. Shortening was seen in eight patients with mean value of 3.5 cm (range1–5 cm). Postoperative infection was seen in four patients. At final follow up based on functional, clinical and radiological outcomes 9 Patients were very satisfied, 8 patients were satisfied, and 1 patient was dissatisfied [Table 1].
Table 1.
Final outcome in individual patients.
| Case No | Range of motion |
Time of Radiological Union (weeks) |
Time b/w stage I & stage II procedure (wks) | Major remarks | Final outcome | ||
|---|---|---|---|---|---|---|---|
| Knee | Ankle | Proximal site | Distal site | ||||
| 1 | 0°–120° | PF∗ 0°–15° DF∗ 0°–5° |
9 | 14 | 10 | V·S. | |
| 2 | 8°–110° FFD# 8° |
PF 5°–10° Eq∗∗ 5° |
8 | 12 | 9 | S | |
| 3 | 12°–100° FFD 12° |
PF 0°–16° DF 0°–10° |
12 | 15 | 12 | S | |
| 4 | 0°–130° | PF 0°–10° DF 0°–5° |
10 | Not done | Not done | V·S. | |
| 5 | 5°–125° FFD 5° |
Ankle fixed in 25° equinus | 14 | 18 | 15 | Foot equinus corrected | S |
| 6 | 0°–130° | PF 0°–10° DF 0°–8° |
17 | 21 | 18 | V·S. | |
| 7 | 0°–125° | PF 0°–15° DF 0°–5° |
10 | 13 | 10 | V·S. | |
| 8 | 0°–110° | PF 0°–12° DF 0°–8° |
8 | 12 | 9 | S | |
| 9 | 0°–130° | Ankle fixed in 10° equinus | 9 | 12 | 9 | Ankle varus corrected | S |
| 10 | 20°–105° FFD 20° |
PF 0°–10° DF 0°–5° |
12 | 14 | 13 | S | |
| 11 | 10°–130° FFD 10° |
PF 0°–12° DF 0°–6° |
37 | 8 | 8 | Nonunion treated with revision plating | V·S. |
| 12 | 5°–110° FFD 5° |
PF 0°–10° DF 0°–6° |
8 | 10 | 9 | Stress fracture of fibula | V·S. |
| 13 | 0°–100° | PF 0°–15° DF 0°–8° |
10 | 15 | 13 | S | |
| 14 | 10°–90° FFD - 10° |
Ankle fixed in 5° equinus | 12 | 14 | 13 | D.S. | |
| 15 | 7°–105° FFD 7° |
PF 0°–15° DF 0°–10° |
9 | 15 | 10 | V·S. | |
| 16 | 10°–120° FFD 10° |
PF 5°–20° Eq (5)° |
10 | 16 | 11 | V S. | |
| 17 | 0°–110° | PF 0°–20° DF 0°–15° |
8 | 12 | 8 | V S | |
| 18 | 0°–105° | PF 10°–22° Eq (10)° |
12 | 14 | 12 | S | |
FFD# Fixed flexion deformity PF∗ -planter flexion DF∗∗-dorsiflexion Eq∗∗ Equinus at ankle. V.S-very satisfied, S-satisfied, D.S.- dissatisfied
4. Discussion
A complex gap nonunion of long bones should be managed based on the principles of stable fixation and adequate control of infection to provide a favorable environment for bone and soft tissue healing.26 Treatment of such cases is challenging, as even careful execution of a meticulous treatment plan may end up with an unpredictable final outcome in the form of amputation or disarticulation. It is difficult to have a single ideal solution for such complex gap nonunion of tibia in any age group. Autologous cancellous bone grafting is a viable option to manage complex gap nonunion in adults, but its major limitation for its paediatric use is difficulty in procuring sufficient graft to fill large bone defects besides, the construct is mechanically weak. Free non-vascularized fibula has a long healing time, significant risk of stress fracture (26%), donor site morbidity and the graft may not undergo hypertrophy, when used to manage bone defects, ultimately having poor outcome.23,27 Use of free vascularized fibula requires micro-surgical skills, sophisticated instruments and the procedure is time consuming.28 Isolation and anastomosis of the peroneal vessels in presence of scarred soft tissue is a challenging task.29 The outcome of tibial allograft reconstruction in gap nonunion is inconsistent with a high failure rate with notable complications of nonunion, infection, fracture, graft rejection and fear of disease transmission.10,11
Ilizarov method of treating complex gap nonunion is technically demanding, needs special instruments with frequent follow-ups to identify and manage various obstacles and complications, which may not be feasible in children belonging to remote areas.30 Induced membrane (Masquelet) technique when used for complex gap nonunion has 18% risk of infection and nonunion. Two recent systematic reviews on Masquelet technique to manage large bone defects in children report bone healing in 91% cases with a complication rate as high as 54%.8,9
Huntington procedure was first described by Hahn, later on the procedure was popularized by Huntington to manage complex tibial nonunion.31, 32 Huntington procedure has several advantages over the above mentioned methods as a limb salvage surgery for complex gap nonunion of tibia in children. The procedure is easy to perform and can be performed in an average set-up without needing prolonged hospitalization and frequent follow-ups. It provides a large graft of the ipsilateral fibula raised on a pedicle of the peroneal artery, aligned and fixed to the tibia; providing a sound mechanical and biological environment favorable for bone healing. When the procedure is done in two stages it is quicker, involves less soft tissue dissection and the retained vascularity at opposite end of fibula further helps in bone healing. The rate of union in our study was 94.4% [Fig. 1]. Although, few authors have shown 100% union rate in their studies for similar indications.25 Nonunion seen in one of our patient, due to screw cut out at proximal tibio-fibular synostosis, healed after revision plating. Compared to children the rate of union in adults treated by Huntington procedure may be up to 72.7% for similar indications. In adults the procedure is associated with increased risk of delayed and nonunion requiring multiple surgeries to achieve union.23 A better union rate in our study compared to above mentioned study, may be because all our patients were children. It emphasizes that Huntington procedure is effective in achieving bone healing even in complex paediatric gap nonunion of tibia.
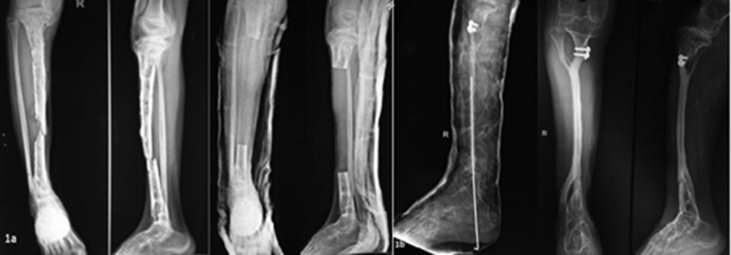
Fig. 1.
a. Radiographs of a 12 years female with chronic osteomyelitis complicated by pathological fracture. Following serial debridement and sequestrectomy the resultant bone gap was 17 cm This patient was managed by two stage Huntington Procedure.
b. Follow up radiographs of same patient at 3.5 years showing consolidation at proximal and distal radioulnar synostosis. Hypertrophy of fibula is also evident. The cross union at proximal and distal ends is helpful to prevent coronal plane mal alignment to some extent.
The transposed fibula has muscles attached to it, along with its nutrient artery supply, this helps in hypertrophy of fibula that may substitute the tibia for normal activities particularly in children.25 One of our patients with large bone gap (17 cm) had stress fracture, that healed conservatively. Stress fracture of fibula has also been reported and treated both conservatively as well by revision surgery in other studies as well.24,33 We encountered difficulty in securing the tibio-fibular synostosis due to very small bone fragment in two patients, similar problems has also been highlighted in other studies as well.24,25
Although fibula is a strong cortical bone; it increases the strength as well as length of the limb however; limb length discrepancy due to growth plate damage may not be effectively addressed by Huntington procedure. In one study where Huntington procedure was done in adults, shortening was seen in all patients; this signifies that apart from growth plate deficiency certain other factors are also responsible for limb length discrepancy in these patients.24 Shortening in eight of our patients was managed with appropriate shoe raise. The residual shortening in these patients can be managed both conservatively as well as by surgical methods.24,25
One of the limitations of Huntington procedure is that it may not provide an acceptable limb alignment in all patients. This was source of initial dissatisfaction in two of our patients. We did corrective osteotomy for 15° symptomatic ankle varus and Lambrinaudi procedure for 25° foot equinus in one patient each. These deformities should be addressed tailored to requirement of individual patients to increase patient satisfaction.24,25
Huntington procedure avoids exposure of the site that is vulnerable to infection and there is also debulking of the leg that facilitates wounds closure and subsequent soft tissue healing.22 Both these factors are helpful in reducing the post-operative infection. Despite this fact, four of our patients developed infection that responded to conservative treatment. However; at times the post-operative infection may be severe enough leading to popliteal artery hemorrhage and ultimately the patient may end up with an above knee amputation.23
The cause of iatrogenic common peroneal nerve injury in two of our patients was traction injury to nerve while attempting to centralize the fibula into medullary canal of tibia in patients with extensive soft tissue fibrosis. Therefore; the authors would suggest not being overzealous to centralize the fibula in such cases. Iatrogenic nerve damage has not been mentioned by other authors; this may be due to difficulty in recognizing the resulting foot drop in such patients due to tendency of foot to be in equinus and concurrent stiffness of ankle and toes.
At final follow-up, 9 Patients were very satisfied, 8 patients were satisfied, and 1 patient was dissatisfied. One of the limitations of Huntington procedure in adults is their inability to participate in strenuous activities due to risk of fibular graft fracture.24 We did not encounter such limitation in paediatric patient population in our study except in one case with large bone defects as mentioned above. This is due to the fact that in children there is good fibular hypertrophy with lesser risk of fibula fracture.34 The cause of dissatisfaction in one patient was persistent foot drop, stiff ankle joint, shortening and fixed flexion deformity of knee. The outcome following Huntington procedure is reliable and consistent with satisfactory outcome in majority of patients. This makes Huntington procedure as a useful limb salvage surgery for complex gap nonunion of tibia in chidren. The limitations of the procedure include its inability to effectively address the limb length discrepancy, and occasional deformity and joint stiffness. These complications may require additional surgeries to improve the final outcome and patient satisfaction.
5. Conclusion
Huntington procedure is an easy and cost-effective treatment option to achieve a cosmetically acceptable limb with satisfactory functional outcome in majority of paediatric patients with complex gap-nounion of tibia, even in resource limited set-up. However; complications like limb length discrepancy, joint stiffness, and deformities; that may warrant an additional surgery are an obstacle in achieving an ideal outcome in certain selected patients. This emphasizes the need of further refining the existing surgical technique to overcome these obstacles and increase the patient satisfaction by minimizing complications.
Author contribution
Abdul Qayyum Khan- Conceptualization
Yasir Salam Siddiqui- Methodology
Julfiqar- original draft; Writing, review & editing.
Mazhar Abbas- Formal analysis
Aamir Bin Sabir- Supervision
Declaration of competing interest
None
Acknowledgement
None
References
- 1.Kumar Seenappa Hiranya, Shukla Manoj Kumar, Narasimhaiah Muralidhar. Management of complex long bone nonunions using limb reconstruction system. Indian J Orthop. 2013 Nov-Dec;47(6):602–607. doi: 10.4103/0019-5413.121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Rosasy M.A. Acute shortening and re-lengthening in the management of bone and soft-tissue in complicated fractures of the tibia. J Bone Joint Surg [Br] 2007;89-B:80–88. doi: 10.1302/0301-620X.89B1.17595. [DOI] [PubMed] [Google Scholar]
- 3.Catagni M.A., Camagni M., Combi A., Ottaviani G. Medial fibula transport with the Ilizarov frame to treat massive tibial bone loss. Clin Orthop Relat Res. 2006;448:208–216. doi: 10.1097/01.blo.0000205878.43211.44. [DOI] [PubMed] [Google Scholar]
- 4.Simon J.P., Hoogmartens M. The value of postero lateral bone grafting for nonunion of the tibia. Acta Orthop Belg. 1984;50:557–564. [PubMed] [Google Scholar]
- 5.Ryzewicz M., Morgan S.J., Linford E., Thwing J.I., de Resende G.V., Smith W.R. Central bone grafting for nonunion of fractures of the tibia: a retrospective series. J Bone Joint Surg Br. 2009;91:522–529. doi: 10.1302/0301-620X.91B4.21399. [DOI] [PubMed] [Google Scholar]
- 6.Wood M.B. Free vascularized fibular grafting-25 years’ experience: tips, techniques, and pearls. Orthop Clin N Am. 2007;38(1):1–12. doi: 10.1016/j.ocl.2006.10.007. (v) [DOI] [PubMed] [Google Scholar]
- 7.Patzakis M.J., Zalavras C.G. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005;13:417–427. doi: 10.5435/00124635-200510000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Morelli I., Drago L., George D.A., Gallazzi E., Scarponi S., Romanò C.L. Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. 2016;47(Suppl 6):S68-S76. doi: 10.1016/S0020-1383(16)30842-7. [DOI] [PubMed] [Google Scholar]
- 9.Morelli I., Drago L., George D.A., Romanò D., Romanò C.L. Managing large bone defects in children: a systematic review of the ’induced membrane technique. J Pediatr Orthop B. 2018;27(5):443–455. doi: 10.1097/BPB.0000000000000456. doi:10.1097. [DOI] [PubMed] [Google Scholar]
- 10.Puri A., Subin B.S., Agarwal M.G. Fibular centralisation for the reconstruction of defects of the tibial diaphysis and distal metaphysis after excision of bone tumours. J Bone Joint Surg Br. 2009;91:234–239. doi: 10.1302/0301-620X.91B2.21272. [PubMed: 19190060] [DOI] [PubMed] [Google Scholar]
- 11.Ramseier L.E., Malinin T.I., Temple H.T., Mnaymneh W.A., Exner G.U. Allograft reconstruction for bone sarcoma of the tibia in the growing child. J Bone Joint Surg Br. 2006;88:95–99. doi: 10.1302/0301-620X.88B1.16253. [PubMed: 16365128] [DOI] [PubMed] [Google Scholar]
- 12.Phieffer L.S., Goulet J.A. Delayed unions of the tibia. J Bone Joint Surg [Am] 2006;88-A:206–216. doi: 10.2106/00004623-200601000-00026. [DOI] [PubMed] [Google Scholar]
- 13.Sen C., Eralp L., Gunes T. An alternative method for the treatment of nonunion of the tibia with bone loss. J Bone Joint Surg [Br] 2006;88-B:783–789. doi: 10.1302/0301-620X.88B6.17515. [DOI] [PubMed] [Google Scholar]
- 14.Jain A.K., Sinha S. Infected nonunion of the long bones. Clin Orthop. 2005;431:57–65. doi: 10.1097/01.blo.0000152868.29134.92. [DOI] [PubMed] [Google Scholar]
- 15.Vail T.P., Urbaniak J.R. Donor-site morbidity with use of vascularized autogenous fibular grafts. J Bone Joint Surg [Am] 1996;78-A:204–211. doi: 10.2106/00004623-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Weiland A.J., Moore J.M., Daniel R.K. The efficacy of free tissue transfer in the treatment of osteomyelitis. J Bone Joint Surg [Am] 1984;66-A:181–193. [PubMed] [Google Scholar]
- 17.Green S.A., Jackson J.M., Wall D.M. Management of segmental defects by Ilizarov intercalary bone transport method. Clin Orthop. 1992;280:136–141. [PubMed] [Google Scholar]
- 18.Agarwal Pawan, Savant Rajiv, Sharma Dhnanjay. Huntington procedure revisited. J Clinical Orthop Trauma. 2019 Nov-Dec;10(6):1128–1131. doi: 10.1016/j.jcot.2019.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuli S.M. Tibialization of the fibula: a viable option to salvage limbs with extensive scarring and gap nonunions of the tibia. Clin Orthop Relat Res. 2005;431:80–84. [PubMed] [Google Scholar]
- 20.Tan J.S., Roach J.W., Wang A.A. Transfer of ipsilateral fibula on vascular pedicle for treatment of congenital pseudarthrosis of the tibia. J Pediatr Orthop. 2011 Jan-Feb;31(1):72–78. doi: 10.1097/BPO.0b013e318202c243. [DOI] [PubMed] [Google Scholar]
- 21.Mannion S., Chimangeni S., Lavy C. Ipsilateral vascularised fibular transfer for reconstruction of osteomyelitic tibial gap defects in Malawi. Orthopaedic Proceedings Volume. Mar 2008;90-B(suppl P_I01) [Google Scholar]
- 22.Puri A., Subin B.S., Agarwal M.G. Fibular centralisation for the reconstruction of defects of the tibial diaphysis and distal metaphysis after excision of bone tumours. J Bone Joint Surg. 2009;91-B(2):234–239. doi: 10.1302/0301-620X.91B2.21272. [DOI] [PubMed] [Google Scholar]
- 23.Kassab M., Samaha C., Saillant G. Ipsilateral fibular transposition in tibial nonunion using Huntington procedure: a 12-year follow-up study. Injury. 2003;34:770–775. doi: 10.1016/s0020-1383(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 24.Kundu Zile Singh, Gupta Vinay, Sukhbir S Sangwan, Kamboj Pradeep. Gap nonunion of tibia treated by Huntington procedure. Indian J Orthop. 2012;46(6):653–658. doi: 10.4103/0019-5413.104197. Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta Som P., Garg Gaurav. The Huntington procedure: still a reasonable option for large tibial defects in paediatric patients. Journal of children’s orthopaedics. 2014;8(5):413–421. doi: 10.1007/s11832-014-0618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Babhulkar S., Pande K., Babhulkar S. Nonunion of the diaphysis of long bones. Clin Orthop. 2005;431:50–56. doi: 10.1097/01.blo.0000152369.99312.c5. [DOI] [PubMed] [Google Scholar]
- 27.Al-Zahrani S., Harding M.G., Kremli M., Khan F.A., Ikram A., Takroni T. Free fibular graft still has a place in the treatment of bone defects. Injury. 1993;24(8):551–554. doi: 10.1016/0020-1383(93)90036-6. [DOI] [PubMed] [Google Scholar]
- 28.Weiland A.J., Daniel R.K. Microvascular anastomoses for bone grafts in the treatment of massive defects in bone. J Bone Joint Surg Am. 1979;61(1):98-104. [PubMed] [Google Scholar]
- 29.de Boer H.H., Wood M.B., Hermans J. Reconstruction of large skeletal defects by vascularized fibula transfer. Int Orthop. 1990;14:121–128. doi: 10.1007/BF00180115. [DOI] [PubMed] [Google Scholar]
- 30.Rajacich N., Bell D.F., Armstrong P.F. Pediatric applications of the Ilizarov method. Clin Orthop Relat Res. 1992 Jul;(280):72–80. PMID: 1611767. [PubMed] [Google Scholar]
- 31.Hahn E. Eine methode, Pseudarthrosen der tibia mit grossen knockendefekt zur heilung zu bringen. Zentralbl f Chir. 1884;11:337–341. [Google Scholar]
- 32.Huntington T.W. VI. Case of bone transference: use of a segment of fibula to supply a defect in the tibia. Ann Surg. 1905;41:249–251. doi: 10.1097/00000658-190502000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chacha P.B., Ahmed M., Daruwala J.S. Vascular pedicle graft of the ipsilateral fibula for non-union of the tibia with a large defect. An experimental and clinical study. J Bone Joint Surg Br. 1981;63:244–253. doi: 10.1302/0301-620X.63B2.7217150. [PubMed:7217150] [DOI] [PubMed] [Google Scholar]
- 34.Krieg A.H., Hefti F. Reconstruction with non-vascularized grafts after resection of bone tumours. J Bone Jt Surg Br. 2007;89-B:215–221. doi: 10.1302/0301-620X.89B2.17686. [DOI] [PubMed] [Google Scholar]