Abstract
Purpose
Infantile hemangiomas (IH) are the most common benign vascular tumors of infancy. Ocular complications due to orbital IH include strabismal, deprivational, or anisometropic astigmatism, and visual loss secondary to amblyopia.
Observations
We report a case of a two-month-old female infant with a severe deep orbital IH. The diagnosis was established by clinical examination and magnetic resonance imaging (MRI). The patient was treated with oral propranolol for six months. Complete tumor regression was observed clinically and by MRI following the treatment. The patient showed no adverse effects or tumor recurrence at the 14-month follow-up.
Conclusions and Importance
Despite its benign nature, periorbital IH requires a rapid diagnosis and prompt treatment to prevent vision loss, particularly in infants. Our case confirms that oral propranolol may be regarded as a safe drug for periorbital IH with an excellent outcome.
Keywords: Hemangioma, Benign tumors, Infants, Treatment, Propranolol
List of abbreviations
- CE-MRI
Contrast-enhanced magnetic resonance imaging
- IH
Infantile hemangioma
- MRI
Magnetic resonance imaging
- PHACE
Posterior fossa brain malformations, hemangiomas (face), arterial, cardiac, and eye abnormalities
1. Introduction
Infantile hemangiomas (IHs) are the most common benign solid tumors of the ocular adnexa in children. IHs can cause significant functional and cosmetic deformities. Although IHs tend to regress spontaneously, those located periorbitally may cause unique complications including ptosis, strabismus, and anisometropia, each of which may, in turn, result in astigmatism, amblyopia, or blindness.1 Therefore, early treatment of these high-risk periocular tumors is necessary to prevent permanent vision loss.1 Both medical and surgical modalities are suggested to manage periocular IHs, but none have been uniformly safe and effective. Until the recent introduction of beta-blockers,2 systemic corticosteroids (prednisolone) were considered the mainstay therapy for complicated IHs, but long-term steroid use was associated with numerous side effects.3
Herein, we report a case of deep orbital proliferating phase IH in a female infant that was successfully treated with a nonselective β-blocker propranolol. We also review the literature and discuss the pathophysiology, diagnostic, and treatment considerations for this rare condition.
2. Case report
An otherwise healthy 2-month-old female infant was referred to our department for evaluation and treatment of painless unilateral left proptosis, which had been slowly progressing over the past 15 days. She was born at 37 weeks' gestation by a cesarean section. The 'patient's history and family history were not contributory. Laboratory investigations, including the complete blood count and routine blood chemistry, did not reveal any abnormality. Clinical examination revealed mild left eye axial proptosis with the fullness of the eyelids (Fig. 1A). There was no associated pupillary abnormality, and the rest of the neurologic examination was otherwise normal. The infant had no evidence of other head and neck cutaneous IHs. A contrast-enhanced magnetic resonance imaging (CE-MRI) of the brain and orbits, at the age of 66 days, revealed the presence of large, multilobulated lesion involving extra- and intraconal space extending in the mediolateral direction, measuring 37 × 19 × 27mm (AP x LL x CC). The lesion was slightly T1w hypointense, T2w isointense with multiple serpiginous flow voids, and with somewhat homogeneous contrast enhancement and marked enhancement of intratumoral vessels (Fig. 2A). We opted for oral propranolol therapy. Before administering propranolol, comprehensive history taking, vital signs, physical examinations, electrocardiogram test, routine blood tests, and blood glucose test were performed and interpreted by a pediatrician. The treatment regimens and potential adverse effects of propranolol were explained to the family of the patient. Parental education related to identifying potential complications of propranolol therapy has been performed. Propranolol was initially administered on the first day at a dosage of 1 mg/kg/day and then at a dose of 2 mg/kg/day divided into three doses under careful monitoring of heart rate and blood glucose levels in the hospital, and weekly follow-up at the outpatient clinic was arranged. At follow-up clinic visits, the dosage of propranolol was doubled to a maximum of 3 mg/kg/day. A follow-up MRI of the orbits performed at the 3-month visit revealed a significant regression of the lesion that measured 17 × 15 × 14 mm (APxLLxCC). At that point, her propranolol was tapered by 0.5 mg/kg per month. A follow-up MRI of the orbits scheduled and performed at the 6-month visit revealed complete regression of the left orbital mass with no detectable left intraorbital lesion present (Fig. 2B). Propranolol therapy was terminated when the child reached eight months of age (treatment for six months). At the end of therapy, the child showed complete lesion regression (Fig. 1B). The patient showed no adverse effects or tumor recurrence at the 14-month follow-up.
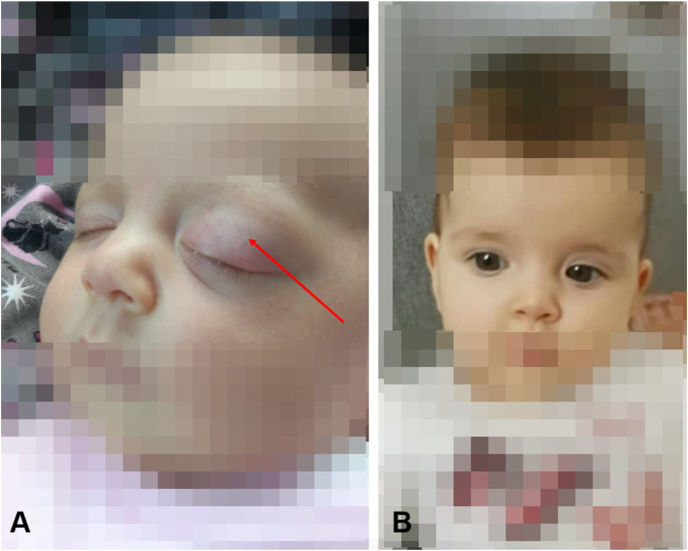
Fig. 1.
A-B. A: A photograph of the patient at the age of two months showing left eye proptosis and periorbital swelling (red arrow) (before treatment). B: A complete disappearance of the deep orbital hemangioma following the treatment with propranolol. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
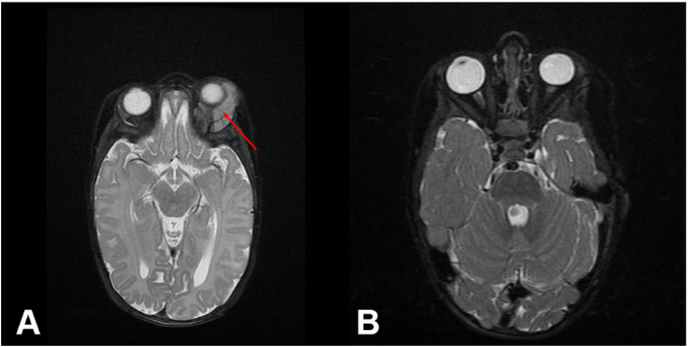
Fig. 2.
A-B. Transverse T2 WI scans of the orbits: A: Initial finding with a large left intraorbital, extra- and intraconal T2 hyperintense mass (red arrow) in the lateral aspect of the orbit with consequent proptosis; B: Post-treatment complete disappearance of the deep orbital hemangioma with entirely resolved left proptosis. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
We present an illustrative and rare case of an infant with deep orbital IH, discovered during the evaluation of unilateral left proptosis and treated successfully with oral propranolol. We also reviewed the recent literature that reported deep IH treatment with propranolol in infants <6 months (the results are summarized in Table 1).
Table 1.
A summary of the previous studies that reported treatment with propranolol in infants <6 months with isolated deep orbital hemangiomas. Our literature survey covered recent publications (since 2010) in the English language from the PubMed/MEDLINE and Google Scholar databases. The studies that included other treatment modalities (e.g., Corticosteroids or surgery) are not included in the table.
| References (year) | Number of patients and age at presentation (weeks/months) | Tumor size (mm) | Location |
|---|---|---|---|
| Albanese et al. (2019)4 | Six patients (median age of 2.7 weeks) | Not available | Deep ocular |
| Ginguerra et al. (2018)15 | Four patients (median age 15 weeks) | 19 (median size) | Deep ocular |
| Lewitt et al. (2014)16 | Five patients (median age of 5.8 weeks) | Not available | Deep ocular |
| Thoumazet al. (2012)17 | One patient (2 weeks) | Not available | Deep ocular |
| Burne et al. (2011)18 | Nine patients (6 patients with deep ocular localization) (8–50 weeks) | Not available | Deep ocular |
| Li et al. (2010)19 | One patient (4 weeks) | 30 × 15 × 25 | Deep ocular |
| Fay et al. (2010)20 | One patient (4 weeks) | Not available | Deep ocular |
| Cheng et al. (2010)21 | Ten patients (3 days–6 months) | 756.7 (median size) | Deep ocular |
The diagnosis of IH is based on history and clinical presentation. In the present case, our patient was without overlying skin surface changes that were suggestive of IH. Due to uncertain diagnosis, the patient required prompt imaging to confirm the presence of orbital IHs and to exclude other diagnoses, including rhabdomyosarcoma and lymphatic malformations. Recent studies have shown that magnetic imaging resonance (MRI) is the preferred imaging modality in deep orbital IH investigations, showing vascular features, detailed orbital extension, and possibly associated malformations such as PHACE syndrome (posterior fossa anomalies, hemangiomas, arterial, cardiac, and eye anomalies). PHACE (OMIM# 606519) represents a rare condition in which a patient has a segmental-type hemangioma along with structural and developmental anomalies.4 In our patient's case, MRI imaging confirmed the presence of an orbital mass suggestive of IH. However, MRI imaging showed that our patient had no other symptoms typically seen in patients with PHACE syndrome. Since capillary hemangiomas are the most common tumors of the eyelids and orbits in childhood, the Kasabach-Merritt syndrome (OMIM#141000) should be considered in the differential diagnosis. This rare syndrome (also called hemangioma with thrombocytopenia) is associated with vascular tumors such as giant capillary hemangiomas, and these tumors should always be ruled out.5 However, Kasebach-Merritt syndrome is rarely associated with isolated hemangiomas, as in our case. Our patient also had a normal platelet count and showed no signs of thrombocytopenic purpura or ecchymoses.
Although IHs follow a predictable clinical course with a proliferative phase (first year of life), followed by an involuting phase (from 2 to 7 years), and an involuted phase (complete regression by 8–12 years of age),6 10% of children, particularly those with IHs in the periorbital and orbital region, may require treatment.7 Since visual development begins in early infancy, the stimulus deprivation during the first year of life has been proven to be detrimental to visual development.8 It has been demonstrated that a total eye closure for one week in infants in the first year of life can cause a permanent visual impairment.8 Due to the potential disruption of visual pathways through stimulus deprivation, a prompt intervention against IHs is necessary for visually significant lesions to improve visual outcomes.1 Schwartz et al. found that hemangioma-specific treatment initiated before 6 months of age substantially improved anisometropic astigmatism with shrinkage of the hemangioma.9
Treatment options for complicated hemangiomas include oral steroids, laser surgery, and cryosurgery, while chemotherapy (vincristine, interferon or cyclophosphamide) may be used in life-threatening cases. However, each of these options has its limitations and ⁄or side effects. Leaute-Labreze et al. first described in 2008 the successful and relatively safe use of oral propranolol, a nonselective blocker of β-adrenergic receptors, in the management of IH.2 Since that time, propranolol has been increasingly used for the treatment of IHs, including life-threatening, function-threatening, and severely ulcerated forms.10,11 A meta-analysis conducted by Lou et al. provided concrete evidence for propranolol as first-line therapy for the management of IHs.12 Although the exact mechanism of action is unknown, propranolol probably inhibits angiogenesis, recruitment of endothelial progenitor cells to the IH site, and induces vasoconstriction, all of which lead to the shrinkage and reduction of IHs.13 The complications of propranolol treatment include hypoglycemia, wheezing, transient hypotension, asymptomatic and transient bradycardia, and hyperkalemia. Therefore careful monitoring of all infants before and during beta-blocker therapy is mandatory. In our case, oral propranolol therapy resulted in a rapid complete regression of the IH without any systemic side effects. Some studies have reported rebound growth after propranolol therapy requiring modification of systemic therapy in 15% of the patients.14 In our case, no relapse occurred within a 1-year follow-up period.
Despite its benign nature, periorbital IH requires a rapid diagnosis and prompt treatment to prevent vision loss, particularly in infants. Our case confirms that oral propranolol may be regarded as a safe drug for deep orbital IH with an excellent outcome.
Patient consent
The current study has been performed in accordance with the ethical standards from the Declaration of Helsinki (1964). The study was also shared with the local institutional review board, which has the policy not to review case reports. Written informed consent was obtained from the patient's mother for anonymized patient information and images to be published in this article.
Funding
The publication of this article was funded by the Qatar National Library.
Author contributions
Conceptualization: Denisa Zvizdic, Zlatan Zvizdic, Semir Vranic.
Data curation: Denisa Zvizdic, Zlatan Zvizdic, Denis Bulja, Amila Sidran, Faruk Skenderi, Semir Vranic.
Formal analysis: Denisa Zvizdic, Zlatan Zvizdic, Semir Vranic.
Investigation: Denisa Zvizdic, Denis Bulja, Amila Sidran.
Resources: Semir Vranic.
Writing – original draft: Denisa Zvizdic, Zlatan Zvizdic, Semir Vranic.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Frank R.C., Cowan B.J., Harrop A.R., Astle W.F., McPhalen D.F. Visual development in infants: visual complications of periocular haemangiomas. J Plast Reconstr Aesthetic Surg. 2010;63:1–8. doi: 10.1016/j.bjps.2008.08.045. [DOI] [PubMed] [Google Scholar]
- 2.Leaute-Labreze C., Dumas de la Roque E., Hubiche T., Boralevi F., Thambo J.B., Taieb A. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008;358:2649–2651. doi: 10.1056/NEJMc0708819. [DOI] [PubMed] [Google Scholar]
- 3.Boon L.M., MacDonald D.M., Mulliken J.B. Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg. 1999;104:1616–1623. doi: 10.1097/00006534-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Albanese G., Mohandas P., Wells L. Orbital infantile haemangioma: radiological features and treatment - case series and literature review. Orbit. 2019;38:67–71. doi: 10.1080/01676830.2018.1501397. [DOI] [PubMed] [Google Scholar]
- 5.Bang G.M., Setabutr P. Periocular capillary hemangiomas: indications and options for treatment. Middle East Afr J Ophthalmol. 2010;17:121–128. doi: 10.4103/0974-9233.63071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berenguer B., Mulliken J.B., Enjolras O. Rapidly involuting congenital hemangioma: clinical and histopathologic features. Pediatr Dev Pathol. 2003;6:495–510. doi: 10.1007/s10024-003-2134-6. [DOI] [PubMed] [Google Scholar]
- 7.Leaute-Labreze C., Harper J.I., Hoeger P.H. Infantile haemangioma. Lancet. 2017;390:85–94. doi: 10.1016/S0140-6736(16)00645-0. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg N.S., Rosanova M.A. Periorbital hemangiomas. Dermatol Clin. 1992;10:653–661. [PubMed] [Google Scholar]
- 9.Schwartz S.R., Kodsi S.R., Blei F., Ceisler E., Steele M., Furlan L. Treatment of capillary hemangiomas causing refractive and occlusional amblyopia. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus. 2007;11:577–583. doi: 10.1016/j.jaapos.2007.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Starkey E., Shahidullah H. Propranolol for infantile haemangiomas: a review. Arch Dis Child. 2011;96:890–893. doi: 10.1136/adc.2010.208884. [DOI] [PubMed] [Google Scholar]
- 11.Drolet B.A., Frommelt P.C., Chamlin S.L. Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics. 2013;131:128–140. doi: 10.1542/peds.2012-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lou Y., Peng W.J., Cao Y., Cao D.S., Xie J., Li H.H. The effectiveness of propranolol in treating infantile haemangiomas: a meta-analysis including 35 studies. Br J Clin Pharmacol. 2014;78:44–57. doi: 10.1111/bcp.12235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Storch C.H., Hoeger P.H. Propranolol for infantile haemangiomas: insights into the molecular mechanisms of action. Br J Dermatol. 2010;163:269–274. doi: 10.1111/j.1365-2133.2010.09848.x. [DOI] [PubMed] [Google Scholar]
- 14.Shah S.D., Baselga E., McCuaig C. Rebound growth of infantile hemangiomas after propranolol therapy. Pediatrics. 2016;137 doi: 10.1542/peds.2015-1754. [DOI] [PubMed] [Google Scholar]
- 15.Ginguerra M.A., Saito O., Fernandes J., Castro D.S., Matayoshi S. Clinical and radiological evaluation of periocular infantile hemangioma treated with oral propranolol: a case series. Am J Ophthalmol. 2018;185:48–55. doi: 10.1016/j.ajo.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Levitt M., Coumou A.D., Groeneveld L., Freling N.J., van der Horst C.M., Saeed P. Propranolol as first-line treatment in orbital infantile haemangiomas: a case series. Orbit. 2014;33:178–183. doi: 10.3109/01676830.2014.884148. [DOI] [PubMed] [Google Scholar]
- 17.Thoumazet F., Leaute-Labreze C., Colin J., Mortemousque B. Efficacy of systemic propranolol for severe infantile haemangioma of the orbit and eyelid: a case study of eight patients. Br J Ophthalmol. 2012;96:370–374. doi: 10.1136/bjophthalmol-2011-300047. [DOI] [PubMed] [Google Scholar]
- 18.Burne R., Taylor R., Medscape Monitoring propranolol treatment in periocular infantile haemangioma. Eye (Lond) 2014;28:1281–1284. doi: 10.1038/eye.2014.237. quiz 1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Y.C., McCahon E., Rowe N.A., Martin P.A., Wilcsek G.A., Martin F.J. Successful treatment of infantile haemangiomas of the orbit with propranolol. Clin Exp Ophthalmol. 2010;38:554–559. doi: 10.1111/j.1442-9071.2010.02327.x. [DOI] [PubMed] [Google Scholar]
- 20.Fay A., Nguyen J., Jakobiec F.A., Meyer-Junghaenel L., Waner M. Propranolol for isolated orbital infantile hemangioma. Arch Ophthalmol. 2010;128:256–258. doi: 10.1001/archophthalmol.2009.375. [DOI] [PubMed] [Google Scholar]
- 21.Cheng J.F., Gole G.A., Sullivan T.J. Propranolol in the management of periorbital infantile haemangioma. Clin Exp Ophthalmol. 2010;38:547–553. doi: 10.1111/j.1442-9071.2010.02344.x. [DOI] [PubMed] [Google Scholar]