Abstract
Background:
Bilateral cardiac sympathetic denervation (BCSD) is a surgical treatment for refractory ventricular arrhythmias. Although the procedure has shown efficacy at reducing cardiac arrhythmias, its impact on mental health is unknown. In the current study we examined associations between the BCSD procedure and mental health.
Methods:
10 ventricular arrhythmia patients undergoing BCSD completed assessments of anxiety, depression, and posttraumatic stress symptoms at pre- and post-BCSD time points. Wilcoxon signed rank and Mann-Whitney U tests were used to examine differences mental health symptoms in the pre- and post-BSCD states. Point biserial correlations were used to explore associations between BCSD response and mental health symptoms.
Results:
A significant reduction of anxiety symptoms was observed from pre- to post-BCSD. At the post-BCSD assessment, participants who successfully responded to the BCSD procedure exhibited lower anxiety symptoms compared to non-responders. However, no significant relationships were identified for depressive or PTSD symptoms.
Conclusion:
The BCSD procedure is associated with reduced anxiety shortly after successful treatment for refractory ventricular arrhythmias in a small sample. Longitudinal surveillance of mental health symptoms after BCSD may be warranted to monitor the impact of this procedure on mental health.
Keywords: cardiac arrhythmia, autonomic nervous system, mental health, sympathectomy, anxiety, depression, PTSD
1. Introduction
Implantable cardioverter-defibrillator (ICD) placement, to treat ventricular arrhythmias (Mirowski et al., 1980), is now a common procedure with survival benefits (Moss et al., 1996, Maron, 2000, Corrado et al., 2003, Arya et al., 2005). ICD placement is even associated with reduced mortality risk across a variety of heart failure conditions (Vakil et al., 2016), leading to increased implementation over time. However, placement is associated with the occurrence of repeated and unpredictable defibrillator shocks with and without presence of detected arrhythmias (Sears and Conti, 2003, Germano et al., 2006). ICD placement has also been associated with poorer mental health including increased levels of anxiety, depression, and posttraumatic stress disorder (PTSD), particularly in the setting of repeated shock episodes to resynchronize the heart rhythm (Sears et al., 1999, Sears and Conti, 2002, Sears and Conti, 2003, Germano et al., 2006, Serber et al., 2007, Matchett et al., 2009, Pedersen et al., 2009, Sears et al., 2009, Sears et al., 2011, Lang et al., 2014). Anxiety, depression and PTSD have been consistently linked with increased risk for cardiovascular and cardiometabolic disease, and importantly, increased rates of mortality (Cohen et al., 2009, Phillips et al., 2009, Cohen et al., 2015, Seldenrijk et al., 2015, Emdin et al., 2016, Wolf and Schnurr, 2016, Dyball et al., 2019), underscoring the critical need for treatments that effectively target cardiovascular diseases without negatively impacting mental health symptoms.
Cardiac sympathetic denervation is a surgical treatment for refractory ventricular arrhythmias that has been increasingly utilized in recent years (Collura et al., 2009, Ajijola et al., 2012a, Ajijola et al., 2012b). Bilateral cardiac sympathetic denervation (BCSD) in particular has shown preliminary efficacy reducing arrhythmia expression (Shah et al., 2019), with one year survival rates of approximately 50% in one study (Vaseghi et al., 2017). The BCSD procedure involves removal of the bilateral segment of the sympathetic chain from T1-T4 that includes the proximal portion of the stellate ganglion, which provides excitatory input to the heart. Resection of this portion of the sympathetic chain is thought to reduce excitatory drive from higher centers of the central nervous system including the brainstem, subcortical and cortical regions, via engagement of central and intrathoracic sympathetic reflexes (Ardell et al., 2019).
Although the BCSD procedure shows promise in ameliorating recurrent ventricular arrhythmias, the impact of this procedure on mental health is unknown. Given the link between sympathetic nervous system activity and mental health symptoms (Pohjavaara et al., 2003, Barton et al., 2007, Morris and Rao, 2013, Khalsa et al., 2018), it seems conceivable that treatments manipulating the sympathetic chain might be capable of modulating mental health symptoms (Pohjavaara et al., 2003, Lipov and Kelzenberg, 2012, Streeter et al., 2012). The BCSD procedure represents a prime target for investigation as it plays a direct role in dampening sympathetic responses. We previously described a case study in which the combination of BCSD, cognitive behavioral psychotherapy and initiation of serotonergic medication was effective in attenuating severe anxiety ensuing from recurring ICD shocks (Khalsa et al., 2014). However, we observed relatively less improvement in depression symptoms, and no improvement in PTSD symptoms at one year. The lack of a substantial group, given the rarity of this procedure, precluded the ability to conduct any statistical analyses and generation of inferences regarding the impact of the procedure on mental health. Furthermore, while employing a combined therapeutic approach allowed targeted treatments for both physical and mental health symptoms, we were unable to examine the potentially unique effects that BCSD may have on mental health symptoms.
In the current study, we assessed associations between the BCSD procedure and mental health in a somewhat larger cohort of individuals. Our primary aims were to 1) examine the effects of BCSD procedure on mental health including anxiety, depression, and PTSD symptoms, and 2) to examine clinical profiles of patients from whom the BCSD procedure was successful (i.e., treatment responders). We hypothesized that the BCSD procedure might be sufficient to attenuate symptoms of anxiety, depression, and PTSD. Additionally, we hypothesized that symptomatic improvement of mental health symptoms would be greater in individuals for whom the BSCD procedure was successful.
2. Materials and Methods
2.1. Participants
Participants were recruited from the UCLA Cardiac Arrhythmia Center between July 2012 and January 2018. Eligible participants included male and female adult patients between the ages of 18–71 years. All participants were diagnosed with cardiovascular disease, had received ICD placement for the treatment of ventricular arrythmias, and were undergoing evaluation for BCSD to manage recurrent ICD shocks. Participants were screened for inclusion during an inpatient evaluation for treatment of acute VT storm. Those deemed appropriate for the BCSD procedure provided informed consent and were included in the present study. Individuals under the age of 18, those known to have prior removal, damage, destruction of nerve tissue, or infiltration of thoracic sympathetic nerve tissue by cancer were excluded from undergoing the BCSD procedure, and thus were excluded from the present study.
Participants completed one baseline visit prior to undergoing the BCSD procedure (Pre-BCSD assessment; described below), one visit shortly after the procedures (Post-BCSD assessment), and when able, one follow-up visit which occurred at least one month after the Post-BCSD visit. Visit 1 included baseline assessment of demographics, baseline cardiovascular assessment and psychological assessment. Visit 2 included a Post-BCSD psychological assessment Post-BCSD and evaluation of response to the procedure. Visit 3 included a follow-up assessment of BCSD response and psychological assessment. Figure 1 provides an overview of study measurements at each visit. Several data points were missing for each measure across each visit, and several subjects did not complete Pre- and Post-BCSD assessments; a detailed listing and a secondary analysis including these parameters can be found in the Supplement.
Figure 1.
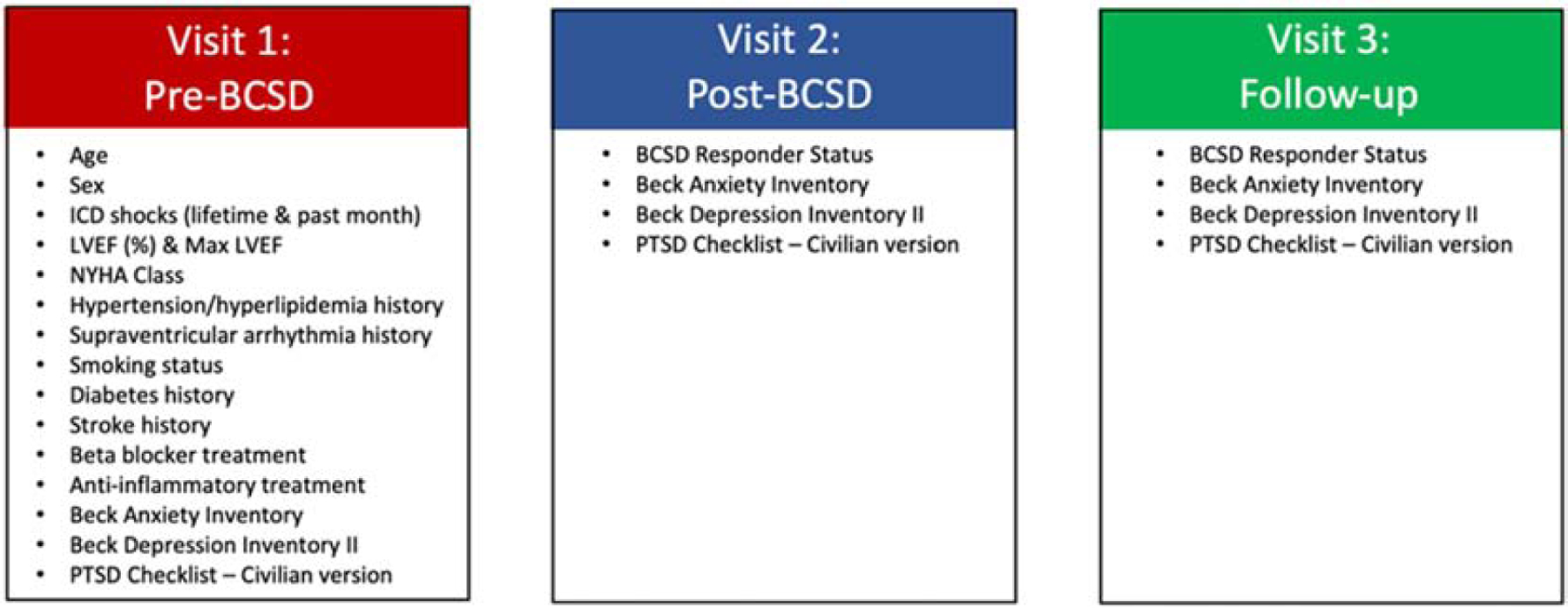
Overview of study measurements at each visit. Participants completed assessments during a pre BCSD visit (visit 1), a post-BCSD visit (visit 2) and at a follow-up visit (visit 3). The mean time between visits 1 and 2 was 1.6 months, and the mean time between visits 2 and 3 was 12.8 months.
The present study was approved by the University of California Los Angeles Institutional Review Board, and the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. All participants provided written informed consent prior to study enrollment.
2.2. BCSD Procedure
During the BCSD procedure, the bilateral sympathetic chain from T1-T4 that included the proximal portion of the stellate ganglion was removed. The surgery was discussed in detail with each patient by a cardiothoracic surgeon who conducted the BCSD procedure. Individuals who underwent the procedure were evaluated during the follow-up visit (at least one-month post-BCSD) to determine if denervation was achieved, and were subsequently classified as BCSD responders or non-responders during routine clinical follow-up at Visit 2 and/or Visit 3 (see below for cardiovascular assessment). If a subject was classified as a non-responder at either Visit 2 or 3, they were included in the BCSD non-responder category; whereas those who were classified as a responder at either Visit 2 or 3 were included in the BCSD responder category. Additional assessments were conducted evaluating the impact of the BCSD procedure on measures of sympathetic or vagal tone including finger pulse volumetry, skin impedance, and continuous cardiac functional parameters; the results of this testing are reported elsewhere (Dusi et al., 2020).
2.3. Psychological Assessment
Self-report questionnaires were used to examine current mental health symptoms pre- and post-BCSD. Specifically, depression, anxiety and posttraumatic stress disorder (PTSD) symptoms were measured using the Beck Depression Inventory (BDI-II) (Beck et al., 1996), Beck Anxiety Inventory (BAI)(Beck et al., 1988), and the PTSD Symptom Checklist (PCL-Civilian Version) (Weathers et al., 1994) during visits 1 and 2. Of note, the BDI-II and BAI assess symptoms of depression and anxiety over the past two weeks, whereas the PCL assesses PTSD symptoms over the past week. Total severity scores were calculated for each measure, with higher scores indicating more severe symptoms.
2.4. Cardiovascular Assessment
Clinical cardiovascular assessments were conducted by trained cardiology personnel, with routine follow-up visits conducted as clinically indicated. At baseline, the following measures were collected for each patient: 1) height and weight to calculate body mass index (BMI), 2) number of lifetime shocks, left ventricular ejection (LVE), 3) history of previous cardiovascular treatments, 4) history of previous heart surgeries, 5) current diagnosis of hypertension, diabetes mellites and/or hyperlipidemia, 6) current smoking status, 7) history of transischemic attacks and supraventricular arrythmias, 8) New York Heart Association (NYHA) assessment to classify degree of heart failure, and 9) current medications including prescriptions for beta-blockers and anti-inflammatories. BCSD responders were defined as a reduction in arrhythmias detected by the patient’s defibrillator, defibrillator shocks or therapies in the 3–6 months following BCSD compared to the same interval prior to BCSD.
2.5. Statistical Analysis
Statistical analyses were conducted using the R Statistical Package. A robust analytic approach was employed to accommodate the small sample size and unequal variances between groups, and to limit the influence of outliers. Pairwise changes in psychological symptoms from pre- to post-BCSD were conducted using Wilcoxon Signed Rank tests (two-sided) (wilcox.test, paired command)). Mann-Whitney U tests (wilcox.test command), were used to explore differences between mean pre- and post-BCSD anxiety, depression, and PTSD symptoms. Point biserial correlations were used to examine associations between BCSD response and mental health symptoms (pbcor command; beta constant = 0.1). Visual inspection of baseline demographic information and medical history was used to qualitatively consider the profile of individuals who were clinically classified as BCSD responders. Given the exploratory nature of the analysis, a critical p-value of 0.05 was used to determine significance.
3. Results
A total of 30 ventricular arrhythmia patients (77% male; mean age = 49.7, SD = 15.6 years) undergoing BCSD completed assessments of depression, anxiety, and PTSD symptoms pre-BCSD. 16 patients completed assessments post-BCSD. We obtained pre- and post-BCSD assessments from 10 patients, and we focus our analysis on these individuals. Demographic characteristics for the paired sample are presented in Table 1 (demographics for the entire sample are listed in the Supplement). During the baseline (i.e., pre-BCSD) assessment, participants endorsed mild levels of depression symptoms and moderate levels of anxiety and PTSD symptoms on average. During the post-BCSD assessment, participants endorsed mild levels of depression, mild anxiety, and moderate levels of PTSD symptoms on average. The time between pre- and post-BCSD assessments ranged from one week to 63 months (median = 1.0, median absolute deviation = 7.4). The time between the post-BCSD and follow-up visits ranged from one to 27 months (median = 15, median absolute deviation = 0.0).
Table 1.
Baseline demographic information and medical history prior to BCSD procedure for the paired sample.
| Mean (SD) | Median (MAD) | Percent (n) | N | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 49.3 (12.9) | 51 (12.6) | -- | 10 |
| Sex (% male) | -- | -- | 80% (8) | 10 |
| BMI | 31.4 (4.3) | 30.6 (5.3) | -- | 9 |
| Medical | ||||
| Shocks (lifetime) | 9.3 (12.5) | 6.5 (5.9) | -- | 10 |
| Pre-BCSD LVE (max %) | 35.2 20.0) | 42.5 (18.5) | -- | 9 |
| Previous Cardiac Treatment | -- | -- | 100% (10) | 10 |
| Previous Heart Surgery | -- | -- | 30% (3) | 10 |
| Hypertension | -- | -- | 20% (2) | 10 |
| Diabetes Mellites | -- | -- | 0% (0) | 10 |
| Hyperlipidemia | -- | -- | 20% (2) | 10 |
| Smoking status (% current or past) | -- | -- | 87.5% (6) | 7 |
| Transischemic Attacks | -- | -- | 0% (0) | 8 |
| History of SV arrhythmia | -- | -- | 40% (4) | 10 |
| Beta-blocker (% prescribed) | -- | -- | 100% (10) | 10 |
| Anti-inflammatory (% prescribed) | -- | -- | 12.5% (1) | 8 |
| BCSD Responder (% yes) | -- | -- | 66.7% (6) | 9 |
Note: BCSD = bilateral cardiac sympathetic denervation; SD = standard deviation; MAD = median absolute deviation; BMI = body mass index; LVE = left ventricular ejection; SV = supraventricular. The numerical column indicates the number of individuals for whom the relevant assessment was obtained.
3.1. Pairwise changes in Mental Health Symptoms from Pre- to Post-BCSD
A significant pairwise reduction in anxiety symptoms was observed from pre- to post-BCSD (V = 52, p = 0.010) with a median difference between assessments of 12 points. Depression symptoms also decreased from pre- to post-BCSD with a median difference of 4 points. However, this symptom reduction did not meet the threshold for statistical significance (V = 25, p = 0.078). No significant reductions were identified in PTSD symptoms from pre- to post-BCSD (V = 27, p = 0.635; median difference = 6). Individual changes in symptoms are presented in Figure 2 and Table 3.
Figure 2.
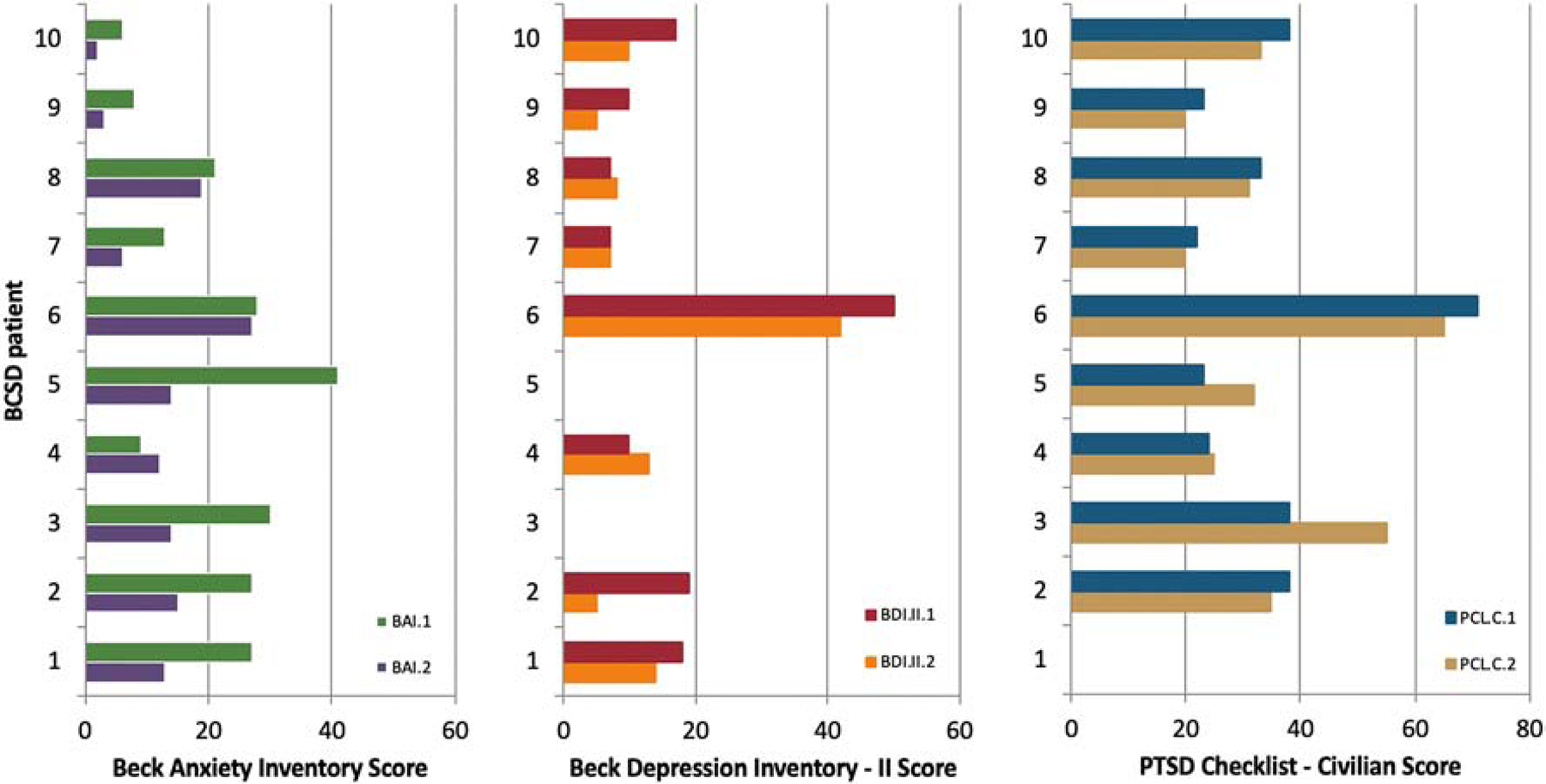
Pairwise illustration of mental health symptoms in 10 individuals pre- and post-bilateral cardiac sympathetic denervation (BCSD). Subject 3 was missing pre-data for depression, and subject 5 was missing post-data for depression. Subject 1 was missing pre-data for PTSD.
Table 3.
Pre- and post-BCSD mental health symptom severity scores.
| Pre-BCSD | Post-BCSD | |||||
|---|---|---|---|---|---|---|
| N | Mean (SD) | Median (MAD) | N | Mean (SD) | Median (MAD) | |
| Anxiety | 10 | 21.0 (11.6) | 24.0 (12.6) | 10 | 12.5 (7.5) | 13.5 (5.2) |
| Depression | 9 | 17.0 (13.2) | 15.0 (7.3) | 9 | 13.9 (11.7) | 10.0 (5.9) |
| PTSD | 9 | 34.4 (15.4) | 33.0 (13.3) | 10 | 34.9 (14.5) | 32.5 (7.4) |
Note: Anxiety reflects total scores on the Beck Anxiety Inventory; Depression reflects total scores on the Beck Depression Inventory-II; PTSD reflects total scores on the PTSD Checklist-Civilian Version; BCSD = bilateral cardiac sympathetic denervation; MAD = median absolute deviation; PTSD = posttraumatic stress disorder; SD = standard deviation. There was missing pre-data for depression in one subject, missing post-data for depression in one subject, and pre-data for PTSD in one subject.
3.3. Demographic profiles of BCSD responders
To further understand the clinical characteristics of patients who respond to BCSD treatment, we examined the profiles of individuals who were classified as BCSD responders (n = 6) and non-responders (n = 3). BCSD response was missing for one subject. With respect to mental health symptoms at baseline (Visit 1), anxiety (p = 0.171), depression (p = 0.800) and PTSD (p = 0.653) were not related to BCSD response. At visit 2 (post procedure), BCSD response was significantly associated with anxiety symptoms (rpb = −0.68, p = 0.043), with responders exhibiting lower levels of anxious symptoms compared to non-responders (median difference = 9.5 points). However, neither depressive (rpb = −0.29, p = 0.480) nor PTSD (rpb = −0.32, p = 0.397) symptoms were significantly associated with BCSD response.
4. Discussion
The current study represents the largest investigation of associations between BCSD and mental health symptoms to date. In a paired sample of 10 individuals receiving treatment for refractory ventricular arrhythmias, we found that the BCSD procedure was associated with reduced anxiety but not depression or PTSD symptoms shortly after treatment. Consistent with the clinical observation in our earlier case study (Khalsa et al., 2014), we identified a statistically significant reduction in anxiety symptoms following the BCSD procedure at the group level. While reductions did not reach statistical significance for depression, a small effect in the predicted direction was observed. We did not see any appreciable reduction in PTSD symptoms following the procedure. In addition, BCSD response was associated with significantly lower levels of anxiety but not depression or PTSD symptoms post-treatment.
Previous studies have suggested that BCSD is an important adjunctive treatment for individuals with refractory ventricular arrythmias (Vaseghi et al., 2017, Shah et al., 2019). However, despite the association of increased mental health symptoms in this patient population (Sears et al., 1999, Sears and Conti, 2002, Sears and Conti, 2003, Germano et al., 2006, Serber et al., 2007, Matchett et al., 2009, Pedersen et al., 2009, Sears et al., 2009, Sears et al., 2011, Lang et al., 2014), this is the first study to date to examine the potential impact of BCSD on anxiety, depression and PTSD symptomatology. Similar to previous studies, we observed clinically significant levels of anxiety, depression, and PTSD in such patients prior to undergoing the BCSD procedure, underscoring the need for routine standardized approaches to mental health screening, evaluation and treatment in patients with ventricular arrythmias.
We observed significant reductions in self-reported anxiety symptoms following the BCSD procedure. It seems theoretically plausible the interruption of sympathetic chain fibers during the BCSD procedure (Ardell et al., 2019) might beneficially impact patients’ perceptions of anxious symptoms through a general reduction of afferent neurovisceral signals (see (Smith et al., 2017) for a review). However, without a sham treatment group, this associational study cannot conclusively identify the source of the anxiety reductions. Other potential contributors might relate to post-procedural relief that an intervention was delivered, early signs of resolution of ventricular tachyarrhythmias, and/or subsequent access to mental health treatment. These explanations are speculative as we did not control for or measure each of these events in enough detail.
While our results provide initial evidence that the BCSD procedure is associated with reduced anxiety symptoms, the sustained elevation in PTSD symptoms, and to a lesser extent, depression is concerning particularly given the link between increased mortality with depression and PTSD in cardiovascular disease (Cohen et al., 2009, Phillips et al., 2009, Cohen et al., 2015, Seldenrijk et al., 2015, Emdin et al., 2016, Wolf and Schnurr, 2016, Dyball et al., 2019); for review, see (Edmondson and von Kanel, 2017)). The availability of effective pharmacologic and non-pharmacologic interventions for depression and PTSD in cardiac patients (Pedersen et al., 2007, Hirsh et al., 2009, Dunbar et al., 2012, Qintar et al., 2015) suggests that BCSD patients experiencing depression and PTSD may derive significant improvements in mental health upon receiving the appropriate treatment referral. Our results underscore the importance of longitudinal surveillance of mental health symptoms, beyond standard pre-surgical screenings, before and after BCSD both for responders. Such monitoring could occur remotely, but should be paired with the appropriate clinical services in the event that treatment referral is indicated (e.g., to help them cope with the psychological trauma associated with repeated near-death experiences, or to address underlying anxiety or depression), as well as to provide supportive care for non-responders (Kamphuis et al., 2003, Carroll, 2008, Kramer et al., 2017). We have argued previously for the application of a synergistic therapeutic approach employing treatments targeting both physical and mental health symptoms (Khalsa et al., 2014). Interdisciplinary or integrated care programs involving cardiologists, psychiatrists, psychologists and nurses are well-suited to accomplish this objective, as are web-based interventions (Schulz et al., 2019). Interestingly, several studies have suggested the potential efficacy of unilateral stellate ganglion blockade injection in reducing treatment resistant PTSD, particularly for symptoms of avoidance and hyperarousal (Mulvaney et al., 2010, Lipov and Kelzenberg, 2012, Olmsted et al., 2019). However, the long-term efficacy of stellate blockade is unknown, the employed methodology varies considerably from that of BCSD (unilateral vs bilateral), and the application of a local anesthetic to induce stellate blockade would only be expected to provide a temporary reprieve (if effective) for cardiac arrhythmias.
4.1. Limitations
The present study provides an initial framework for examining the effects of BCSD treatment on mental health outcomes, but it is not without limitations. First, BCSD is a fairly rare intervention for treatment-refractory ventricular arrythmias, with a limited number of patients who are eligible for treatment. Thus, the sampling pool for recruitment was small. Additionally, only a small number (n =10) of participants completed both pre- and post-BCSD assessments. As a result we were unable to conduct more sophisticated analyses including inferential statistics and inclusion of relevant covariates, which rely on greater statistical power. There was also variability in the number of individuals completing the different visits, the timing of follow-up visits and also in the number of available measurements, which was influenced by pragmatic constraints involved in conducting research assessments in an acute inpatient environment. Nevertheless, the present results underscore the prevalence of mental health symptoms in ventricular arrhythmia patients undergoing BCSD treatment, and provides further evidence of an association between modulation of the autonomic nervous system and anxiety.
4.2. Conclusion
The BCSD procedure is associated with reduced anxiety but not depression or PTSD symptoms shortly after successful treatment for refractory ventricular arrhythmias. Larger prospective longitudinal studies may be warranted to monitor the impact of this procedure on mental health.
Supplementary Material
Highlights.
Stellate ganglia removal was associated with lower anxiety in cardiac arrhythmias
Successful arrhythmia response to denervation was associated with lower anxiety
Stellate ganglia removal was not associated with lower depression or PTSD symptoms
Acknowledgments
Funding
Dr. Khalsa received funding from the National Institute of Mental Health (K23MH112949) and from the National Institute of General Medical Sciences (P20GM121312). Dr. Clausen was supported by the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the Durham VA Health Care System, and the Department of Veterans Affairs Mid-Atlantic MIRECC. Drs. Shahabi and Naliboff were supported in part by the Gail and Gerald Oppenheimer Family Foundation. Dr. Ajijola was supported by National Institutes of Health grants HL125730 and DP2HL142045. Dr. Shivkumar was supported by National Institutes of Health grants HL084261 and OT2OD023848. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institutes of Health, the Department of Veterans Affairs, or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
Declarations of interest
The authors have no competing interests or conflicts of interest to disclose.
References
- Ajijola OA, Lellouche N, Bourke T, Tung R, Ahn S, Mahajan A, Shivkumar K (2012a) Bilateral cardiac sympathetic denervation for the management of electrical storm. J Am Coll Cardiol 59:91–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajijola OA, Vaseghi M, Mahajan A, Shivkumar K (2012b) Bilateral cardiac sympathetic denervation: why, who and when? Expert review of cardiovascular therapy 10:947–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardell JL, Foreman RD, Armour JA, Shivkumar K (2019) Cardiac sympathectomy and spinal cord stimulation attenuate reflex-mediated norepinephrine release during ischemia preventing ventricular fibrillation. JCI Insight [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arya A, Haghjoo M, Dehghani MR, Alasti M, Alizadeh H, Kazemi B, Sadr-Ameli MA (2005) Effect of cardiac resynchronization therapy on the incidence of ventricular arrhythmias in patients with an implantable cardioverter-defibrillator. Heart Rhythm 2:1094–1098. [DOI] [PubMed] [Google Scholar]
- Barton DA, Dawood T, Lambert EA, Esler MD, Haikerwal D, Brenchley C, Socratous F, Kaye DM, Schlaich MP, Hickie I, Lambert GW (2007) Sympathetic activity in major depressive disorder: identifying those at increased cardiac risk? J Hypertens 25:2117–2124. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56:893–897. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK (1996) Beck depression inventory-II San Antonio. [Google Scholar]
- Carroll SL (2008) A potential barrier to discussing deactivation of implantable cardioverter defibrillators was patients’ lack of knowledge. Evid Based Nurs 11:95. [DOI] [PubMed] [Google Scholar]
- Cohen BE, Edmondson D, Kronish IM (2015) State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. Am J Hypertens 28:1295–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH (2009) Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA 302:489–492. [DOI] [PubMed] [Google Scholar]
- Collura CA, Johnson JN, Moir C, Ackerman MJ (2009) Left cardiac sympathetic denervation for the treatment of long QT syndrome and catecholaminergic polymorphic ventricular tachycardia using video-assisted thoracic surgery. Heart Rhythm 6:752–759. [DOI] [PubMed] [Google Scholar]
- Corrado D, Leoni L, Link MS, Della Bella P, Gaita F, Curnis A, Salerno JU, Igidbashian D, Raviele A, Disertori M, Zanotto G, Verlato R, Vergara G, Delise P, Turrini P, Basso C, Naccarella F, Maddalena F, Estes NA 3rd, Buja G, Thiene G (2003) Implantable cardioverter-defibrillator therapy for prevention of sudden death in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation 108:3084–3091. [DOI] [PubMed] [Google Scholar]
- Dunbar SB, Dougherty CM, Sears SF, Carroll DL, Goldstein NE, Mark DB, McDaniel G, Pressler SJ, Schron E, Wang P, Zeigler VL, American Heart Association Council on Cardiovascular Nursing CoCC, Council on Cardiovascular Disease in the Y (2012) Educational and psychological interventions to improve outcomes for recipients of implantable cardioverter defibrillators and their families: a scientific statement from the American Heart Association. Circulation 126:2146–2172. [DOI] [PubMed] [Google Scholar]
- Dusi V, Shahabi L, Lapidus RC, Sorg JM, Naliboff BD, Shivkumar K, Khalsa SS, Ajijola OA. Cardiovascular autonomic reflex function following bilateral cardiac sympathetic denervation for ventricular arrhythmias. Heart Rhythm (2020). S1547–5271(20)30354–4. doi: 10.1016/j.hrthm.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyball D, Evans S, Boos CJ, Stevelink SAM, Fear NT (2019) The association between PTSD and cardiovascular disease and its risk factors in male veterans of the Iraq/Afghanistan conflicts: a systematic review. Int Rev Psychiatry 31:34–48. [DOI] [PubMed] [Google Scholar]
- Edmondson D, von Kanel R (2017) Post-traumatic stress disorder and cardiovascular disease. The lancet Psychiatry 4:320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BH (2016) Meta-Analysis of Anxiety as a Risk Factor for Cardiovascular Disease. Am J Cardiol 118:511–519. [DOI] [PubMed] [Google Scholar]
- Germano JJ, Reynolds M, Essebag V, Josephson ME (2006) Frequency and causes of implantable cardioverter-defibrillator therapies: is device therapy proarrhythmic? Am J Cardiol 97:1255–1261. [DOI] [PubMed] [Google Scholar]
- Hirsh AT, Sears SF Jr., Conti JB (2009) Cognitive and behavioral treatments for anxiety and depression in a patient with an implantable cardioverter defibrillator (ICD): a case report and clinical discussion. J Clin Psychol Med Settings 16:270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamphuis HC, de Leeuw JR, Derksen R, Hauer RN, Winnubst JA (2003) Implantable cardioverter defibrillator recipients: quality of life in recipients with and without ICD shock delivery: a prospective study. Europace 5:381–389. [DOI] [PubMed] [Google Scholar]
- Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, Feusner JD, Garfinkel SN, Lane RD, Mehling WE, Meuret AE, Nemeroff CB, Oppenheimer S, Petzschner FH, Pollatos O, Rhudy JL, Schramm LP, Simmons WK, Stein MB, Stephan KE, Van den Bergh O, Van Diest I, von Leupoldt A, Paulus MP, Interoception Summit p (2018) Interoception and Mental Health: A Roadmap. Biological psychiatry : cognitive neuroscience and neuroimaging 3:501–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, Shahabi L, Ajijola OA, Bystritsky A, Naliboff BD, Shivkumar K (2014) Synergistic application of cardiac sympathetic decentralization and comprehensive psychiatric treatment in the management of anxiety and electrical storm. Front Integr Neurosci 7:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer DB, Habtemariam D, Adjei-Poku Y, Samuel M, Engorn D, Reynolds MR, Mitchell SL (2017) The Decisions, Interventions, and Goals in Implantable Cardioverter-DefIbrillator TherapY (DIGNITY) Pilot Study. J Am Heart Assoc 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang S, Becker R, Wilke S, Hartmann M, Herzog W, Lowe B (2014) Anxiety disorders in patients with implantable cardioverter defibrillators: frequency, course, predictors, and patients’ requests for treatment. Pacing Clin Electrophysiol 37:35–47. [DOI] [PubMed] [Google Scholar]
- Lipov E, Kelzenberg B (2012) Sympathetic system modulation to treat post-traumatic stress disorder (PTSD): a review of clinical evidence and neurobiology. J Affect Disord 142:1–5. [DOI] [PubMed] [Google Scholar]
- Maron BJ (2000) Hypertrophic cardiomyopathy and sudden death: new perspectives on risk stratification and prevention with the implantable cardioverter-defibrillator. Eur Heart J 21:1979–1983. [DOI] [PubMed] [Google Scholar]
- Matchett M, Sears SF, Hazelton G, Kirian K, Wilson E, Nekkanti R (2009) The implantable cardioverter defibrillator: its history, current psychological impact and future. Expert Rev Med Devices 6:43–50. [DOI] [PubMed] [Google Scholar]
- Mirowski M, Reid PR, Mower MM, Watkins L, Gott VL, Schauble JF, Langer A, Heilman MS, Kolenik SA, Fischell RE, Weisfeldt ML (1980) Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings. N Engl J Med 303:322–324. [DOI] [PubMed] [Google Scholar]
- Morris MC, Rao U (2013) Psychobiology of PTSD in the acute aftermath of trauma: Integrating research on coping, HPA function and sympathetic nervous system activity. Asian J Psychiatr 6:3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M (1996) Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med 335:1933–1940. [DOI] [PubMed] [Google Scholar]
- Mulvaney SW, McLean B, de Leeuw J (2010) The use of stellate ganglion block in the treatment of panic/anxiety symptoms with combat-related post-traumatic stress disorder; preliminary results of long-term follow-up: a case series. Pain practice : the official journal of World Institute of Pain 10:359–365. [DOI] [PubMed] [Google Scholar]
- Olmsted KL, Bartoszek M, Mulvaney S, McLean B, Turabi A, Young R, Kim E, Vandermaas-Peeler R, Morgan JK, Constantinescu O, Kane S, Nguyen C, Hirsh S, Munoz B, Wallace D, Croxford J, Lynch JH, White R, Walters BB (2019) Effect of stellate ganglion block treatment on posttraumatic stress disorder symptoms: a randomized clinical trial. JAMA Psychiatry 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen SS, Sears SF, Burg MM, Van Den Broek KC (2009) Does ICD indication affect quality of life and levels of distress? Pacing Clin Electrophysiol 32:153–156. [DOI] [PubMed] [Google Scholar]
- Pedersen SS, van den Broek KC, Sears SF Jr. (2007) Psychological intervention following implantation of an implantable defibrillator: a review and future recommendations. Pacing Clin Electrophysiol 30:1546–1554. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Batty GD, Gale CR, Deary IJ, Osborn D, MacIntyre K, Carroll D (2009) Generalized anxiety disorder, major depressive disorder, and their comorbidity as predictors of all-cause and cardiovascular mortality: the Vietnam experience study. Psychosom Med 71:395–403. [DOI] [PubMed] [Google Scholar]
- Pohjavaara P, Telaranta T, Vaisanen E (2003) The role of the sympathetic nervous system in anxiety: Is it possible to relieve anxiety with endoscopic sympathetic block? Nord J Psychiatry 57:55–60. [DOI] [PubMed] [Google Scholar]
- Qintar M, George JJ, Panko M, Bea S, Broer KA, St John J, Blissett KA, Ching E, Sears SF, Pedersen SS, Pozuelo L, Chung MK (2015) A prospective study of anxiety in ICD patients with a pilot randomized controlled trial of cognitive behavioral therapy for patients with moderate to severe anxiety. J Interv Card Electrophysiol 43:65–75. [DOI] [PubMed] [Google Scholar]
- Schulz SM, Ritter O, Zniva R, Nordbeck P, Wacker C, Jack M, Groschup G, Deneke T, Puppe F, Ertl G, Angermann C, Stork S, Pauli P (2020). Efficacy of a web-based intervention for improving psychosocial well-being in patients with implantable cardioverter-defibrillators: the randomized controlled ICD-FORUM trial. Eur Heart J, 41: 1203–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears SE Jr., Conti JB (2003) Understanding implantable cardioverter defibrillator shocks and storms: medical and psychosocial considerations for research and clinical care. Clinical cardiology 26:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears SF, Hauf JD, Kirian K, Hazelton G, Conti JB (2011) Posttraumatic stress and the implantable cardioverter-defibrillator patient: what the electrophysiologist needs to know. Circ Arrhythm Electrophysiol 4:242–250. [DOI] [PubMed] [Google Scholar]
- Sears SF Jr., Conti JB (2002) Quality of life and psychological functioning of icd patients. Heart (British Cardiac Society) 87:488–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears SF Jr., Conti JB, Curtis AB, Saia TL, Foote R, Wen F (1999) Affective distress and implantable cardioverter defibrillators: cases for psychological and behavioral interventions. Pacing Clin Electrophysiol 22:1831–1834. [DOI] [PubMed] [Google Scholar]
- Sears SF, Matchett M, Conti JB (2009) Effective management of ICD patient psychosocial issues and patient critical events. Journal of cardiovascular electrophysiology 20:1297–1304. [DOI] [PubMed] [Google Scholar]
- Seldenrijk A, Vogelzangs N, Batelaan NM, Wieman I, van Schaik DJ, Penninx BJ (2015) Depression, anxiety and 6-year risk of cardiovascular disease. J Psychosom Res 78:123–129. [DOI] [PubMed] [Google Scholar]
- Serber ER, Sears SF, Nielsen CD, Spencer WH 3rd, Smith KM (2007) Depression, anxiety, and quality of life in patients with obstructive hypertrophic cardiomyopathy three months after alcohol septal ablation. Am J Cardiol 100:1592–1597. [DOI] [PubMed] [Google Scholar]
- Shah R, Assis F, Alugubelli N, Okada DR, Cardoso R, Shivkumar K, Tandri H (2019) Cardiac sympathetic denervation for refractory ventricular arrhythmias in patients with structural heart disease: A systematic review. Heart Rhythm 16:1499–1505. [DOI] [PubMed] [Google Scholar]
- Smith R, Thayer JF, Khalsa SS, Lane RD (2017) The hierarchical basis of neurovisceral integration. Neurosci Biobehav Rev 75:274–296. [DOI] [PubMed] [Google Scholar]
- Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP (2012) Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses 78:571–579. [DOI] [PubMed] [Google Scholar]
- Vakil K, Kazmirczak F, Sathnur N, Adabag S, Cantillon DJ, Kiehl EL, Koene R, Cogswell R, Anand I, Roukoz H (2016) Implantable Cardioverter-Defibrillator Use in Patients With Left Ventricular Assist Devices: A Systematic Review and Meta-Analysis. JACC Heart Fail 4:772–779. [DOI] [PubMed] [Google Scholar]
- Vaseghi M, Barwad P, Malavassi Corrales FJ, Tandri H, Mathuria N, Shah R, Sorg JM, Gima J, Mandal K, Saenz Morales LC, Lokhandwala Y, Shivkumar K (2017) Cardiac Sympathetic Denervation for Refractory Ventricular Arrhythmias. J Am Coll Cardiol 69:3070–3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman D, Huska J, Keane T (1994) The PTSD checklist-civilian version (PCL-C) Boston, MA: National Center for PTSD. [Google Scholar]
- Wolf EJ, Schnurr PP (2016) PTSD-Related Cardiovascular Disease and Accelerated Cellular Aging. Psychiatr Ann 46:527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


