Abstract
This systematic review provides a comprehensive, up-to-date summary of traumatic brain injury (TBI) epidemiology in Europe, describing incidence, mortality, age, and sex distribution, plus severity, mechanism of injury, and time trends. PubMed, CINAHL, EMBASE, and Web of Science were searched in January 2015 for observational, descriptive, English language studies reporting incidence, mortality, or case fatality of TBI in Europe. There were no limitations according to date, age, or TBI severity. Methodological quality was assessed using the Methodological Evaluation of Observational Research checklist. Data were presented narratively. Sixty-six studies were included in the review. Country-level data were provided in 22 studies, regional population or treatment center catchment area data were reported by 44 studies. Crude incidence rates varied widely. For all ages and TBI severities, crude incidence rates ranged from 47.3 per 100,000, to 694 per 100,000 population per year (country-level studies) and 83.3 per 100,000, to 849 per 100,000 population per year (regional-level studies). Crude mortality rates ranged from 9 to 28.10 per 100,000 population per year (country-level studies), and 3.3 to 24.4 per 100,000 population per year (regional-level studies.) The most common mechanisms of injury were traffic accidents and falls. Over time, the contribution of traffic accidents to total TBI events may be reducing. Case ascertainment and definitions of TBI are variable. Improved standardization would enable more accurate comparisons.
Keywords: epidemiology, living systematic review, traumatic brain injury
Editor's Note: This article is published as a Living Systematic Review. All Living Systematic Reviews will be updated at approximately three-six month intervals, with these updates published as supplementary material in the online version of the Journal of Neurotrauma (see Update 5).
Introduction
Traumatic brain injury (TBI) is among the most severe types of injury in terms of both case fatality1 and long-term implications for survivors.2 Treatment of TBI can be complex and expensive.3 Upon clinical examination, TBI is most commonly sub-divided into mild, moderate, and severe, according to the Glasgow Coma Scale (GCS).4,5 Such categories have been found to be predictive of a patient's long-term outcome,6 although other measures and models also have been tested.7,8
A previous review of the epidemiology of TBI in Europe concluded that the leading causes of TBI were road traffic collisions, and falls.3 Consequently, in a densely populated and economically advanced area such as the European Union (EU), the potential for prevention of morbidity and mortality is great. The variability in incidence and mechanism of TBI, which may be observed on this mainly contiguous land-mass with a well-developed road network, is also of scientific interest, as it may lead to better prevention of TBI. Countries within the EU adhere to certain multi-national laws and agreements, but nonetheless retain their own law-making and enforcement responsibilities.9 This may add further complexity to the understanding of TBI epidemiology, for example, in the contributions of varying road speed limits or the legal restrictions on the availability of firearms. More generally, the issues relating to the contemporary demographic and lifestyle characteristics of the similar countries or regions suggest that epidemiological trends from EU countries also may be applicable to other high income countries.
Considerable variability has been observed between national rates, largely attributable to significant variability in data collection, case ascertainment, and case definition. This has led to calls for standardized definitions and data collection in population-based studies, and an associated paradigm shift in studying TBI and its impact.10–12
In order to improve the understanding of causes of TBI and the scale of the problem, it is important to analyze the current situation and time trends, using good quality comparable observational studies. One comprehensive systematic review of the epidemiology of TBI in Europe was published nearly ten years ago.3 A recent systematic review,13 published as a follow-up to Tagliaferri (2006),3 addresses similar issues but was more restrictive in dates of publication (1990–2014) and has not been set up as a “living” systematic review (i.e., it is not expected that it will be kept up-to-date as new research is published).13
The overall objective of this systematic review was to provide a comprehensive, up-to-date summary of TBI epidemiology in Europe by reviewing all relevant observational studies. Specific aims were to determine the incidence, mortality, age, and sex distribution of TBI in Europe, along with the severity and mechanism of injury and time trends.
Methods
This review was conducted and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.14 Details of the protocol for this systematic review were registered on PROSPERO (registration number 2014: CRD42014015517) and can be accessed at www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014015517.
This review was prepared as a “living systematic review” as part of the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) project. CENTER-TBI is a European project aiming to improve outcomes for people with TBI through better classification, characterization, and management of this injury.15 A living systematic review is a high quality, up-to-date online summary of health research that is updated as data from new relevant research that meets study inclusion criteria becomes available.16 In practice, this means that the searches will be re-run frequently, any new studies incorporated into the review, and updates will be regularly published.17
Information sources
The following databases were searched: PubMed, Web of Science, CINAHL, and EMBASE from 1960 up to January 15, 2015. For each of these, searches were performed in March and April 2014 with a combination of key words and subject headings (Appendix 1). The same searches were re-run in January 2015. To reduce the risk of publication bias, searches also were undertaken in gray literature and references of included studies.
Study selection/inclusion criteria
Retrospective and prospective descriptive studies that reported on the epidemiology of TBI in Europe were included. To be eligible for the review, studies must have been an original study (i.e., not a review or duplicate of previously published data) that measured and reported incidence, mortality, or case fatality of TBI in Europe, and was published in English. Study size was not restricted and data collected from hospitals or official statistics were eligible. There were no limitations regarding the dates of data collection, study performance or publication, participant age, or TBI severity.
For some of these terms, such as TBI, incidence, mortality, and case fatality, the definition used by authors can vary. For the purposes of this review, these terms were defined in the following ways:
TBI: Defined as an injury to the head, by either blunt force or penetrative means, which causes sufficient damage that the patient suffers a change in brain function; or more recently, as an alteration in brain function, or other evidence of brain pathology, caused by an external force.11 Ascertainment of a TBI case could be by any of the following: International Classification of Diseases (ICD) in its 8th, 9th and 10th revision codes, Abbreviated Injury Score for head injuries (AISHead or HAIS), the Glasgow Coma Scale (GCS), or clinical signs (such as loss of consciousness, post-traumatic amnesia, or pathologies found in computed tomography/magnetic resonance imaging scan).
Incidence: Rate of TBIs recorded per 100,000 population per year. These were usually first-time events.
Mortality: Total number of fatal TBIs in a given population per 100,000 population per year.
Case fatality: Proportion of people with TBI who subsequently died due to a cause related to the TBI at certain time-points.
TBI severity: Categories of severity (severe, moderate, mild), as defined by the GCS (e.g., 3–8 [mild], 9–12 [moderate], and 13–15 [severe],5 or other classification system used by the authors.
Two authors (WP, VB) independently screened citations on titles and abstracts, excluding any obviously irrelevant or duplicate citations. Results were compared and disagreements discussed with a third author and/or with members of an expert panel. Agreed citations were retrieved in full text and screened independently by two authors (AB, VB, MM, VR, MT) using the same process. Screening was undertaken using Covidence, a not-for-profit web-based tool designed to assist in conducting systematic reviews.18
Data collection and assessment of methodological quality
Two authors (AB, VB, MM, VR, or MT) independently extracted data and assessed methodological quality of selected studies. Any discrepancies were resolved by discussion.
The following items were extracted from each study: study authors, year of publication, study time period, type of data source, method and completeness of case ascertainment, criteria for identifying TBI, source population, number of TBI cases reported, reported data on TBI incidence, mortality, and case fatality, broken down by sex, age, severity, and mechanism of injury.
Methodological quality was assessed using the Methodological Evaluation of Observational Research (MORE) checklist, as previously used in reviews of non-therapeutic studies.19,20 The following domains of bias or quality are assessed with the MORE checklist: funding of study, conflict of interest, study design, sampling, definition of cases, source of data, and reliability of estimates. Each domain was judged according to specific criteria and scored as “OK, Minor Flaw, Major Flaw, and Poor reporting” (Appendix 2) No studies were excluded from the review based on methodological quality.
Data synthesis
To facilitate appropriate comparisons, studies were first grouped according to whether they reported country-level data (derived from national hospital or mortality registries) or regional-level data, denoting smaller populations within studies (derived from regional/country or hospital catchment areas). Other stratifications–for example, by study design and retrospective/prospective data collection–were considered, but the strata generated by this means were too small to make meaningful comparisons.
Findings are described overall, and also broken down according to age, sex, severity of TBI, and mechanism of injury. Time trends of incidence and mortality of TBI also are described.
Statistical analysis
Data are presented in tables and figures. Meta-analysis of incidence and mortality rates was not possible, as too few studies reported age-adjusted data and it was not possible to obtain the raw data from study authors to perform standardization. A funnel plot was generated to consider small study effects in regional-level studies; the country-level studies were not plotted as there were too few studies (fewer than 10).
Results
Description of studies
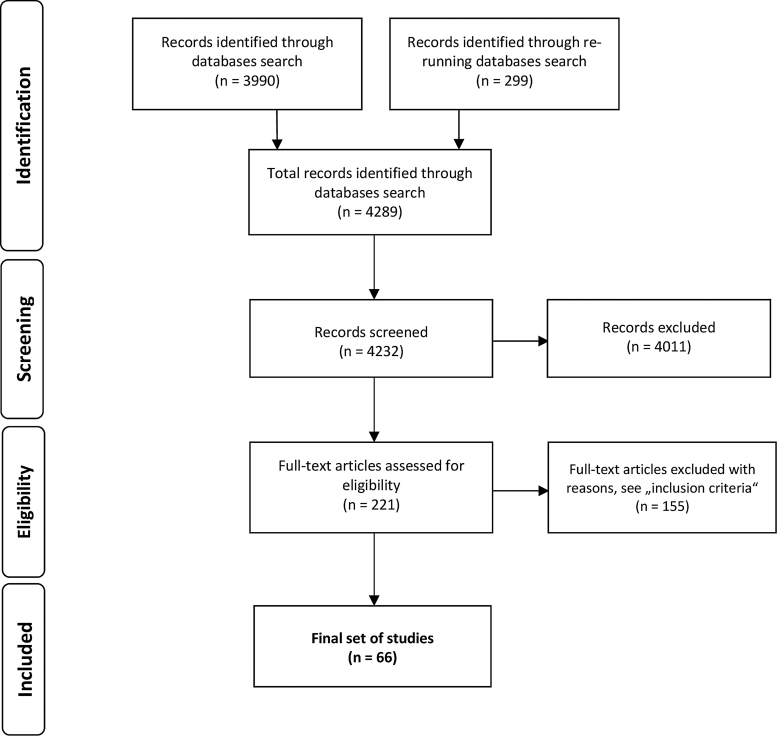
A total of 4289 citations were identified. After removing duplicates, 4232 were screened on citation and abstract and 4011 were excluded. As such, 221 papers were screened for eligibility, with 66 included as full-text (Fig. 1).
FIG. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart of the study selection process.
Characteristics of included studies
Of the 66 included studies, 22 provided country-level data from Finland (n = 4); Austria (n = 4); Denmark (n = 3); the Netherlands (n = 2); Norway (n = 2); Sweden (n = 2); and Scotland, Germany, Great Britain, Spain, Portugal, Switzerland, and the Republic of San Marino, (n = 1, each). A further 44 reported on either a regional population (one or more country regions, counties or provinces) or the catchment area of one or more treatment centers. All studies together represented 23 European countries–those mentioned above and Italy, France, Iceland, Ireland, United Kingdom, Bosnia, Croatia, Macedonia, Slovak Republic, Estonia, and Greece.
The majority of studies (n = 25) had study periods of 1 or 2 years, with a further 17 reporting data over 10 years or more. The remaining studies reported a time period of 3 – 10 years. The number of included cases ranged from 10121 (included severe TBI only) to 208,195.22 Tables 1 and 2 present the characteristics of included studies.
Table 1.
Characteristics of Studies With Country-Level Population
| Study author(s) (year) reference number | Source population | Study period | Data source | Case ascertainment | Type of severity | Number of cases | Average age | % of males/M:F ratio | Mechanism of TBI injury (up to 3 most frequent in % *) | |
|---|---|---|---|---|---|---|---|---|---|---|
|
1 |
Kannus and colleagues (1999)48 |
Finland (≥ 60 years; fall-induced only) |
1970–1995 |
National hospital discharge registry |
ICD 8, ICD 9 |
Severe |
554 in 1970 1393 in 1995 |
69.6 in 1970 75 in 1995 |
NR |
F only |
|
2 |
Steudel and colleagues (2005)31 |
Germany |
1972–1998 |
Hospital admissions registry; mortality registry |
ICD 9, ICD 10 |
All |
279,029 (in 1996) |
NR |
NR |
NR |
|
3 |
Jennett and MacMillan (1981)49 |
Scotland, England, Wales |
1974–1975 |
Hospital admissions report; Registrar's general report |
Clinical definition |
All |
Unclear |
NR |
NR |
Unclear |
|
4 |
Engberg, and Teasdale (1998)23 |
Denmark (0–14 years) |
1979–1993 |
Danish hospital registry |
ICD 8 |
All |
47,794 |
NR |
58 |
NR |
|
5 |
Engberg and colleagues (2001)50 |
Denmark |
1979–1996 |
Danish hospital registry |
ICD 8, ICD 10 |
All |
166,443 |
NR |
2.12:1 |
NR |
|
6 |
Mauritz and colleagues (2014)51 |
Austria |
1980–2012 |
Statistik Austria (national statistical office) |
ICD 9, ICD 10 |
Fatal |
47,827 |
NR |
2.2:1 |
T F Su |
|
7 |
Brazinova and colleagues (2014)52 |
Austria (≥ 65 years) |
1980–2012 |
Statistik Austria (national statistical office) |
ICD 9, ICD 10 |
Fatal |
16,204 |
NR |
61 |
F 48 T 22 Su 17 |
|
8 |
Majdan and colleagues (2014)53 |
Austria (0–19 years) |
1980–2012 |
Statistik Austria (national statistical office) |
ICD 9, ICD 10 |
Fatal |
5319 |
NR |
75 |
T 78 F 8 |
|
9 |
Servadei and colleagues (1985)28 |
Republic of San Marino |
1981 and 1982 |
Hospital records |
Clinical definition |
All |
207 |
26.7 |
67.2 |
NR |
|
10 |
Williamson and colleagues (2002)54 |
Scotland (0–14 years) |
1986–1995 |
Registrar General's report |
Clinical definition; ICD 9 |
Fatal |
290 |
NR |
64/1.7:1 |
T 72 F 11 |
|
11 |
Hartholt and colleagues (2011)46 |
Netherlands (≥ 65 years; fall-induced only) |
1986–2008 |
National medical registration |
ICD 9 |
Severe |
32,133 |
NR |
40 |
F only |
|
12 |
Sundstrøm and colleagues (2007)55 |
Denmark, Finland Norway, Sweden |
1987–2001 |
National statistical offices |
ICD 8; ICD 9; ICD 10 |
Fatal |
NR |
1987: Denmark M 41.8, F 50.1 Finland M 44.2, F 56.3 Norway M 44.5, F 54.8 Sweden M 48.1, F 53.6 2001: Denmark M 49.8, F 60.1 Finland M 52.1, F 62.3 Norway M 52.3, F 66.3 Sweden M 56.8, F 69.3 |
NR |
NR |
|
13 |
Kleiven and colleagues (2003)56 |
Sweden |
1987–2000 |
Swedish Hospital Discharge Registry |
ICD 9; ICD 10 |
All |
≈22,000/year |
NR |
2:1 |
F T |
|
14 |
Alaranta and colleagues (2000)57 |
Finland |
1991–1995 |
National hospital discharge registry |
ICD 9 |
All |
24,497 |
NR |
58.7 |
F 61 T 26 |
|
15 |
Koskinen and Alaranta (2008)58 |
Finland |
1991–2005 |
National hospital discharge registry; cause of death registry |
ICD 9; ICD 10 |
All |
77,959 |
NR |
59.2 |
F 51.8 T 16.6 V 2.9 |
|
16 |
Shivaji and colleagues (2014)22 |
Scotland |
1998–2009 |
Scottish Morbidity Record |
ICD 10 |
All |
208,195 |
NR |
70 |
F 47 V 18 |
|
17 |
Pérez and colleagues (2012)27 |
Spain |
2000–2009 |
National hospital discharge registry |
ICD 9; ISS; Barell matrix |
All |
206,503 |
NR |
2.7:1 |
T |
|
18 |
Dias and colleagues (2014)59 |
Portugal (≥ 18 years) |
2000–2010 |
National diagnosis-related groups database |
ICD 9 |
All |
72,865 |
57.9 ± 21.8 |
64.1/1.8:1 |
F 57 T 29 |
|
19 |
Walder and colleagues (2013)24 |
Switzerland (≥ 16 years) |
2007–2010 |
Hospital records (all hospitals) |
HAIS |
Severe |
921 |
Median, 55 |
74.2 |
F 52.6 T 31.6 |
|
20 |
Mauritz and colleagues (2014)32 |
Austria |
2009–2011 |
Statistik Austria (national statistical office); AUVA hospital discharges database |
ICD 10 |
All |
73,622 |
44.5 ± 29.2 |
58.3 |
T 6.8 (81% unknown) |
|
21 |
Andelic and colleagues (2012)60 |
Norway (≥ 16 years) |
2009–2010 |
Norwegian trauma referral centers |
ICD 10, GCS |
Severe |
359 |
46.7 ± 21.6 |
77 |
F 50 T 40 |
| 22 | Scholten and colleagues (2014)61 | Netherlands | 2010–2012 | Dutch Injury Surveillance System; national hospital discharge registry | ICD 9 | All | 3762/year (DIS), 34,681/year (natlional estimate) | NR | NR | H 48 T 33.4 S 8.2 |
% if clearly stated.
M, males; F, females; TBI, traumatic brain injury; ICD, International Classification of Diseases; NR, not reported; T, traffic related; F, falls; Su, suicide; ISS, Injury Severity Score; HAIS, Head Abbreviated Injury Scale; GCS, Glasgow Coma Scale.
Table 2.
Characteristics of Studies With Regional-Level Population
| Study author(s) (year) reference number | Source population | Study period | Data source | Case ascertainment | Type of severity | Number of cases | Average age | % of males/M:F ratio | Mechanism of TBI injury (up to 3 most frequent in % *) | |
|---|---|---|---|---|---|---|---|---|---|---|
| 23 |
Winqvist and colleagues (2007)62 |
Finland (≤34 years; birth cohort) |
1966–2000 |
Finnish Hospital Discharge Registry; Causes and Death Register |
ICD 8; ICD 9; ICD 10 |
All |
457 |
NR |
66.5 |
T 41.7 F 25.8 |
| 24 |
Berney and colleagues (1995)63 |
Switzerland (0–15 years) |
1969–1991 |
Children's Hospital of Geneva records |
Clinical definition |
All |
4003 |
NR |
NR |
1969: T 56.5 F 26.5 1990: T 46 F 32 |
| 25 |
Berney and colleagues (1994)64 |
Switzerland (0–15 years) |
1975–1983 |
Children's Hospital of Geneva records |
Clinical definition |
All |
1835 |
NR |
63 |
F 46 T 43 |
| 26 |
Nestvold and colleagues (1988)65 |
Norway |
1975 |
Hospital. records of four hospital of Akershus county |
Clinical definition |
All |
488 |
29.75 |
1.9:1 |
T 57.6 H 7.8 |
| 27 |
Edna and Cappelen (1984)66 |
Norway |
1979–1980 |
Hospital records of four hospital of Trøndelag county |
Clinical definition |
All |
1124 |
NR |
69.7 |
T 44.8 S 13.9 H 12.5 |
| 28 |
Edna and Cappelen (1985)67 |
Norway (traffic-induced only) |
1979–1980 |
Hospital records of four hospitals of Trøndelag county |
Clinical definition |
All |
503 |
NR |
2.0:1 |
T only |
| 29 |
Alvarez and colleagues (2011)68 |
Spain (1 m.–14 years) |
1983–2009 |
Pediatric ICU of The Canary Islands provincial hospital |
Clinical definition; GCS |
Severe |
389 |
67.9 ± 41.6 m. |
67 |
T 56 F 24 |
| 30 |
Johansson and colleagues (1991)69 |
Sweden (16–60 years) |
1984–1985 |
Hospital records of regional hospitals of Umeå district |
ICD 9 |
All |
242 |
NR |
64.5 |
NR |
| 31 |
Servadei and colleagues (1988)30 |
Italy |
1984–1985 |
Ravenna City hospital records |
Clinical definition |
All |
1468 |
NR |
NR |
T 66.4 F 27.7 |
| 32 |
Tiret and colleagues (1990)70 |
France |
1986 |
Hospital records of referral teaching hospitals in Aquitaine registry |
Clinical definition |
All |
8940 |
NR |
2.1:1 |
T 59.6 F 32.5 |
| 33 |
Emanuelson and Wendt (1997)71 |
Sweden (0–17 years) |
1987–1991 |
Hospital records of hospital of southwestern Sweden |
Clinical definition; ICD 9 |
All |
210 |
9.44 ± 4.96 |
64.3 |
T 60 F 22 S 7 |
| 34 |
Arnarson and colleagues (1995)72 |
Iceland (0–14 years) |
1987–1991 |
Reykjavík City hospital records |
Clinical definition; ICD 9 |
All |
359 |
NR |
62.4 |
F 62 T 19 |
| 35 |
Boto and colleagues (2009)25 |
Spain (>14 years) |
1987–1999 |
Department of Neurosurgery of the Hospital “12 de Octubre,” Madrid |
GCS |
Severe |
895 |
35.2 ± 17.8 |
78.2 |
T 64.6 F 30.9 |
| 36 |
Vazquez-Barquero and colleagues (1992)26 |
Spain |
1988 |
Hospital records of University Hospital “Marqués de Valdecilla” |
Clinical definition |
All |
477 |
NR |
73.4 |
T 60 F 24 W 8 |
| 37 |
Bouillon and colleagues (1999)73 |
Germany |
1990–1996 |
Prehospital and hospital records of Cologne region |
GCS or AISHead |
Severe |
650 |
39 |
71 |
T 56 F 31 |
| 38 |
Maegele and colleagues (2007)74 |
Germany |
1990–1999 |
Pre-hospital and hospital records of Cologne region |
GCS or AISHead |
Severe |
731 |
40.3 |
73 |
T 55.3 F 35 |
| 39 |
Andersson and colleagues (2003)75 |
Sweden |
1992–1993 |
Central Hospital Borås records |
ICD 9; ACRM categories |
All |
753 |
27 |
59 |
F 58 T 16 |
| 40 |
Hawley and colleagues (2003)37 |
United Kingdom (0–15 years) |
1992–1998 |
North Staffordshire health district hospitals records |
GCS; British Society of Rehabilitation Medicine Classification |
All |
1,553 |
6.76 ± 4.6 |
64.3 |
F 45.1 T 21.1 |
| 41 |
Ingebrigtsen and colleagues (1998)76 |
Norway |
1993 |
University Hospital of Tromsø records |
Clinical definition; HISS |
All |
247 |
NR |
63.6/1.7:1 |
F 62 T 21 V 7 |
| 42 |
Javouhey and colleagues (2006)77 |
France (traffic-induced only) |
1996–2001 |
Road Trauma Registry in Rhône region |
Clinical definition; AIS |
All |
64,298 |
NR |
severe 74.7 |
T only |
| 43 |
Baldo and colleagues (2003)78 |
Italy |
1996–2000 |
Hospital records of Veneto Region; Regional Statistics Office |
ICD 9; AIS |
All |
55,368 |
M 37.7 ± 24.7 F 45.6 ± 29.7 |
61.1 |
T 48.5 H 12.2 W 8.8 |
| 44 |
Masson and colleagues (2001)79 |
France |
1996 |
Hospital records in Aquitaine region |
HAIS; GCS |
Severe |
497 |
HAIS4 median, 44 HAIS5 median, 45 |
71.4/2.5:1 |
T 48.3 F 41.8 |
| 45 |
Puljula and colleagues (2013)47 |
Finland |
1999 and 2007 |
Oulu University Hospital records, Northern Ostrobothnia region |
GCS |
Moderate; severe |
126 in 1999 135 in 2007 |
44 in 1999 48 in 2007 |
72.2 in 1999 76.3 in 2007 |
1999: F 33 V 30 T 29 2007: F 50 T 22 V 20 |
| 46 |
Servadei and colleagues (2002)80 |
Italy |
1998 |
Ospedale Maurizio Bufalini records, Romagna region |
ICD 9 |
All |
2,430 |
NR |
61.5 |
T 47.9 F 32.6 W 7.8 |
| 47 |
Di Bartolomeo and colleagues (2001)81 |
Italy |
1998–1999 |
regional trauma data bank of Friuli Venezia Giulia Region |
ISS; AIS; TRISS; GCS |
Severe |
184 |
44.5 |
77.2 |
NR |
| 48 |
Servadei and colleagues (2002)82 |
Italy |
1998 |
hosp. records of Romagna and Trention regions |
ICD 9 |
All |
4,442 |
NR |
61.5 Romagna 63.7 Trentino |
Romagna: T 48.2 Trentino: T 23, H 19.6 |
| 49 |
Dahl and colleagues (2006)83 |
Sweden (0–17 years) |
1999 and 2000 |
Central Hosp.of Borås records, south-western Sweden |
Clinical definition; GCS |
Mild |
192 |
7.5 ± 4.8 |
57.3 |
F 61 S 16 T 13 |
| 50 |
Rusnak and colleagues (2007)45 |
Austria |
1999–2004 |
Hospital records of five participating hospitals |
GCS |
Severe |
492 |
47.5 (95% CI, 45.7 – 49.3) |
71.9 |
NR |
| 51 |
Rickels and colleagues (2010)33 |
Germany |
2000–2001 |
Hospital records, Hannover region, Münster county |
ICD 10 |
All |
6783 |
NR |
58.4 |
F 52,5 T 26,3 V 14,2 |
| 52 |
Ventsel and colleagues (2008)84 |
Estonia (0–14 years) |
2001–2005 |
Tartu University Hospital records, Tartu county |
ICD 10 |
All |
478 |
6.2 (95% CI, 5.80 – 6.64) |
57 |
F 63.6 T 16.9 |
| 53 |
Styrke and colleagues (2007)34 |
Sweden |
2001 |
Hospital records of regional hospital of Umeå district |
ICD 10 |
All |
449 |
median, M 23 median, F 22 |
55 |
F 55 T 30 |
| 54 |
Rosso and colleagues (2007)85 |
Austria |
1999–2004 |
hosp. records of 5 participating hosp. |
GCS |
Severe |
492 |
48.2 ± 21.1 |
72 |
T 44 F 41 S 5 |
| 55 |
Mauritz and colleagues (2008)86 |
Austria, Bosnia, Croatia, Macedonia and Slovak Republic |
2001–2005 |
Hospital records of 13 participating hospital |
GCS |
Severe |
1172 |
41 |
77.3 |
T 44.3 F 36 |
| 56 |
Numminen (2011)87 |
Finland (>14 years) |
2002–2004 |
Hospital records from three municipalities in South East Finland |
ICD 10, GCS |
All |
370 |
M 50.6 F 55.7 |
54 |
F 58.4 T 17.8 |
| 57 |
Falk (2007)88 |
Sweden (<16 years) |
2002–2003 |
Astrid Lindgren Children's Hospital records, Stockholm region |
Clinical definition |
All |
3168 |
5.5 |
NR |
F 68 T 8 |
| 58 |
Heskestad and colleagues (2009)89 |
Norway |
2003 |
University Hospital of Stavanger records, Stavanger region |
Clinical definition; GCS; Scandinavian guidelines |
All |
585 |
NR |
1.7:1 |
F 51 T 21 V 14 |
| 59 |
Andelic and colleagues (2008)29 |
Norway |
2005–2006 |
Ulleval University hospital records, Oslo City |
Clinical definition; ICD 10; GSC |
All |
445 |
median, 29 |
63.8 |
F 51 T 29.7 V 12.8 |
| 60 |
Von Elm and colleagues (2008)21 |
Switzerland |
2005 (6 months) |
Hospital records of three trauma centers |
GCS and AISHead |
Severe |
101 |
median, 41 |
74.2 |
T 40 F 31 |
| 61 |
Frohlich and colleagues (2011)35 |
Ireland |
2005–2007 |
One university teaching hospital ICU records |
Clinical definition |
All |
46 |
NR |
80 |
V 37 T 33 F 24 |
| 62 |
Van Pelt and colleagues (2011)38 |
Netherlands (1m.-24 years) |
2007–2008 |
Sophia Children's Hospital records |
Clinical definition |
All |
472 |
12 ± 7.5 |
67.2 |
T 40.7 H 18.9 S 7.4 |
| 63 |
Andriessen and colleagues (2011)90 |
Netherlands (≥ 16 years) |
2008–2009 |
Hospital records of five trauma centers |
GCS |
Moderate; severe |
508 |
47.3 |
70.1 |
T 50.6 F 38 |
| 64 |
Roe and colleagues (2013)91 |
Norway (≥16 years) |
2009–2011 |
Hospital records of five university hospitals |
ICD 10; GCS |
Severe |
271 |
NR |
77.5 |
F 57.2 T 32.5 |
| 65 |
Hawley and colleagues (2013)36 |
United Kingdom (0–14 years) |
2011 (6 months) |
Children's ED at University Hospital Coventry and Warwickshire records |
Clinical definition; GCS |
Mild |
1,747 |
5.5 ± 4.8 |
63.9 |
F 62.2 V 6.3 T 3.2 |
| 66 | Katsaragakis and colleagues (2010)92 | Greece | 12 months, year unclear | Hospital records of 30 participating hospitals | Clinical definition | All | 3,383 | NR | 72.5 | T 54.1 F 27.7 |
% if clearly stated.
M, males; F, females; TBI, traumatic brain injury; ICD, International Classification of Diseases; NR, not reported; T, traffic related; F, falls; H, accidents at home; ICU, intensive care unit; GCS, Glasgow Coma Scale; S, sport; W, accidents at work/industrial accidents; AISHead, Abbreviated Injury Score for head injuries; ACRM, American Congress of Rehabilitation Medicine; HISS, Head Injury Severity Scale; V, violence; HAIS, Head Abbreviated Injury Scale; TRISS, Trauma and Injury Severity Score.
Inclusion criteria, case ascertainment, and case definition varied markedly across studies. Most had data from hospital registries, either directly from participating centers or from regional/national registries to which the hospitals reported. Some studies also used mortality registries, either hospital-based or regional/national mortality databases. Our review found a wide variety of definitions of the injury itself. A summary of the inclusion criteria, case ascertainment, and classification of TBI in individual studies is presented in Tables 3 and 4.
Table 3.
Case Ascertainment in Studies With Country-Level Population
| Study author(s) (year) reference number | Study period | Case ascertainment |
|||
|---|---|---|---|---|---|
| Inclusion criteria* | TBI classification** | Clinical definition** | |||
| 1 |
Kannus and colleagues (1999)48 |
1970–1995 |
People ≥60 years old in Finland with a fall-induced severe TBI as a consequence of a fall from standing height (1 m) or less and that results in hospitalization of the victim |
ICD 8: 80000 - 80410, 85000 - 85100, 85200 - 85411 ICD 9: 8000A - 8033A, 8500A - 8519X, and 8520A - 8541X |
- |
| 2 |
Steudel and colleagues (2005)31 |
1972–1998 |
People in Germany who were hospitalized with and those who died due to TBI |
ICD 9: 800 - 804, 850 - 854 ICD 10: S02.0 - S02.9, S06.0 - S06.9 |
- |
| 3 |
Jennett and MacMillan (1981)49 |
1974–1975 |
People of Scotland, England, and Wales who were hospitalized with head injury |
- |
Patients with a history of a blow to the head or with altered consciousness after a relevant injury, or with a scalp or forehead laceration, or who had had a skull x-ray examination |
| 4 |
Engberg, and Teasdale (1998)23 |
1979–1993 |
People of Denmark 0–14 years old who were hospitalized with TBI |
ICD 8: 800,801, 803, 850 - 854 |
- |
| 5 |
Engberg and colleagues (2001)50 |
1979–1996 |
People of Denmark who were hospitalized with and those who died due to TBI |
ICD 8: 800,801, 803, 851 - 854 ICD 10: S01.0 - S09.9 |
- |
| 6 |
Mauritz and colleagues (2014)51 |
1980–2012 |
People of Austria who died due to TBI |
ICD 9: 800, 801, 803, 804, 850 - 854, 873, 905, 907 ICD10: S01.0 - S01.9, S02.0 - S02.3, S02.7 - S02.9, S04.0, S06.0 - S06.9, S07.0 -S07.9, S09.7 - S09.9, T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, T90.4, T90.5, T90.8, T90.9 |
- |
| 7 |
Brazinova and colleagues (2014)52 |
1980–2012 |
People of Austria ≥65 years old who died due to TBI |
ICD 9: 800, 801, 803, 804, 850 - 854, 873, 905, 907 ICD10: S01.0-S01.9, S02.0-S02.3, S02.7-S02.9, S04.0, S06.0-S06.9, S07.0-S07.9, S09.7-S09.9, T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, T90.4, T90.5, T90.8, T90.9 |
- |
| 8 |
Majdan and colleagues (2014)53 |
1980–2012 |
People of Austria 0–19 years old who died due to TBI |
ICD 9: 800, 801, 803, 804, 850 - 854, 873, 905, 907 ICD10: S01.0 - S01.9, S02.0 - S02.3, S02.7 - S02.9, S04.0, S06.0 - S06.9, S07.0 -S07.9, S09.7 - S09.9, T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, T90.4, T90.5, T90.8, T90.9 |
- |
| 9 |
Servadei and colleagues (1985)28 |
1981 and 1982 |
People of the Republic of San Marino who were hospitalized with TBI |
- |
All patients with a head injury (scalp lacerations were considered separately), those having a skull fracture and/or loss of consciousness (no matter how brief) |
| 10 |
Williamson and colleagues (2002)54 |
1986–1995 |
People of Scotland 0–14 years old who died due to TBI |
ICD 9 |
ICD 9 injury code of either skull fracture or intracranial injury |
| 11 |
Hartholt and colleagues (2011)46 |
1986–2008 |
People of Netherlands ≥65 years who were hospitalized with a fall-induced severe TBI |
ICD 9: 800, 801, 803, 804, 850 - 854 |
- |
| 12 |
Sundstrøm and colleagues (2007)55 |
1987–2001 |
People of Denmark, Finland, Norway, Sweden who died due to head injury |
ICD 8: 800, 801, 803, 851 - 854 ICD 9: 800 - 804, 850 - 854 ICD 10: S00, S02 - S04, S06 - S09 |
- |
| 13 |
Kleiven and colleagues (2003)56 |
1987–2000 |
People of Sweden who were hospitalized due to head injury |
ICD 9: 800 - 804; 850 - 854 ICD 10: S2.0 - S2.9; S6.0 - S6.9 |
- |
| 14 |
Alaranta and colleagues (2000)57 |
1991–1995 |
People of Finland who were hospitalized with TBI |
ICD 9: 800, 801, 803, 850-854 |
- |
| 15 |
Koskinen and Alaranta (2008)58 |
1991–2005 |
People of Finland who were hospitalized with TBI |
ICD 9: 800, 801, 803, 850, 851 - 854 ICD 10: S02.0, S02.00, S02.01, S02.1, S02.10, S02.11, S02.7, S02.70, S02.71, S02.8, S02.80, S02.81, S02.9, S02.90, S02.91, T020, S06.0, S06.1 - 9 |
- |
| 16 |
Shivaji and colleagues (2014)22 |
1998–2009 |
People of Scotland who were hospitalized with TBI |
ICD 10: S01.0, S01.9, S02.0,S02.1, S02.3, S02.7, S02.9, S04.0, S06.0, S06.9, S07.0, S07.1, S07.8, S07.9, S09.7, S09.9, T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, T90.4, T90.5, T90.8, T90.9 |
An occurrence of an injury to the head with one or more of the following attributable to the head injury: decreased level of consciousness, amnesia, skull fracture, a neurological, neurophysiological or intracranial lesion, or an occurrence of death from trauma with head injury listed in the sequence of conditions leading to death |
| 17 |
Pérez and colleagues (2012)27 |
2000–2009 |
People of Spain who were hospitalized with TBI |
ICD 9: 800,801; 803,804, 850, 851, 852, 853, 854 |
- |
| 18 |
Dias and colleagues (2014)59 |
2000–2010 |
People of Portugal ≥18 years who were hospitalized with TBI |
ICD 9: 800-804, 850 - 854 |
- |
| 19 |
Walder and colleagues (2013)24 |
2007–2010 |
People of Switzerland ≥16 years who were hospitalized with severe TBI |
all admissions with head trauma and HAIS >3 |
- |
| 20 |
Mauritz and colleagues (2014)32 |
2009–2011 |
People of Austria who were hospitalized with and those who died due to TBI |
ICD 10: S01.0 - S01.9, S02.0, S02.1, S02.7, S06.0 - S06.9,T01.0, T02.0, T04.0, T06.0, T90.1, T90.2, or T90.4 - T90.9 |
- |
| 21 |
Andelic and colleagues (2012)60 |
2009–2010 |
People of Norway ≥16 years who were hospitalized with severe TBI |
ICD 10:S06.0 - S06.9 |
- |
| 22 | Scholten and colleagues (2014)61 | 2010–2012 | People of Netherlands who were hospitalized with TBI | ICD 9: 850, 800 - 801, 803, 804, 851 - 854, 905, 907, 950, 959 | - |
all ages and all severity if not specified otherwise; **presented terminology is the same as in the original study.
TBI, traumatic brain injury; ICD, International Classification of Diseases.
Table 4.
Case Ascertainment in Studies With Regional-Level Population
| Study author(s) (year) (reference number | Study period | Case ascertainment |
|||
|---|---|---|---|---|---|
| Inclusion criteria* | TBI classification** | Clinical definition** | |||
| 23 |
Winqvist and colleagues (2007)62 |
1966–2000 |
Members of Northern Finland Birth Cohort ≤34 years who were hospitalized with TBI and those who died due to TBI |
ICD 8 and ICD 9: 800, 801, 803, 850, 851 - 854 ICD 10: S02.0 - S02.11, S06.0 - S06.9, S07.1 |
- |
| 24 |
Berney and colleagues (1995)63 |
1969–1991 |
People of Geneva region, Switzerland 0–15 years who were hospitalized with TBI |
- |
Alteration of consciousness (primary or secondary), neurological deficit, or early epileptic seizures, with or without confirmation by CT scan or operation |
| 25 |
Berney and colleagues (1994)64 |
1975–1983 |
People of Geneva region, Switzerland 0–15 years who were hospitalized with TBI |
- |
Severe trauma contained the categories extradural haematoma, subdural haematoma, open brain laceration and brain contusion. Contusion was defined on clinical grounds, with or without CT, angiography, operation or EEG. |
| 26 |
Nestvold and colleagues (1988)65 |
1975 |
People of Akershus county, Norway who were hospitalized with and those who died due to head injury |
- |
Trauma to face, head or neck with one or more of the following symptoms: unconsciousness, retrograde amnesia, posttraumatic amnesia, scull or neck fracture, or trauma combined with headache, nausea or vomiting during the first day after the accident |
| 27 |
Edna and Cappelen (1984)66 |
1979–1980 |
People of Trøndelag county, Norway who were hospitalized with head injury |
- |
Loss of consciousness following the head trauma, a skull fracture, and development of intracranial hematoma |
| 28 |
Edna and Cappelen (1985)67 |
1979–1980 |
People of Trøndelag county, Norway who were hospitalized with traffic-induced head injury |
- |
Loss of consciousness following the head trauma, a skull fracture, and development of intracranial hematoma |
| 29 |
Alvarez and colleagues (2011)68 |
1983–2009 |
People of the Canary Islands, Spain 1 m.-14 years who were hospitalized with severe head injury |
Classification of the Trauma Coma Data Bank93 |
- |
| 30 |
Johansson and colleagues (1991)69 |
1984–1985 |
People of Umeå district, Sweden 16–60 years who were hospitalized with TBI |
ICD 9: 850.00 - 854.00 |
- |
| 31 |
Servadei and colleagues (1988)30 |
1984–1985 |
People of Ravenna region, Italy who were hospitalized with and those who died due to TBI |
- |
Loss of consciousness, clinical, radiological or EEG findings |
| 32 |
Tiret and colleagues (1990)70 |
1986 |
People of Aquitaine region, France who were hospitalized with and those who died due to head trauma |
- |
Contusions, lacerations, skull fractures or brain injuries, and/or loss of consciousness after a relevant injury |
| 33 |
Emanuelson and Wendt (1997)71 |
1987–1991 |
People of south-western Sweden 0–17 years who were hospitalized with and those who died due to TBI |
ICD 9: 800 - 801, 803 - 804, 851 - 854 |
TBI was defined as the presence of unconsciousness lasting ≥60 min and/or clinical signs of brain contusion and/or radiological and/or neurophysiological signs of brain contusion |
| 34 |
Arnarson and colleagues (1995)72 |
1987–1991 |
People of Reykjavík area, Iceland 0–14 years who were hospitalized with head trauma |
ICD 9: 850, 851 - 854 |
Head trauma requiring at least 1 night in hospital |
| 35 |
Boto and colleagues (2009)25 |
1987–1999 |
People of Madrid area, Spain >14 years who were hospitalized with severe head injury |
Head injury with GCS score ≤8 |
- |
| 36 |
Vazquez-Barquero and colleagues (1992)26 |
1988 |
People of Autonomous Region of Cantabria, Spain who were hospitalized with head injury |
- |
Head injury with loss of consciousness, skull fracture, objective neurologic findings which could be reasonably attributed to the head injury |
| 37 |
Bouillon and colleagues (1999)73 |
1990–1996 |
People of Cologne region, Germany who were hospitalized with and those who died due to severe brain trauma |
Brain trauma with GCS ≤8 or AISHead ≥3 |
- |
| 38 |
Maegele and colleagues (2007)74 |
1990–1999 |
People of Cologne region, Germany who were hospitalized with and those who died due to severe TBI |
TBI with GCS ≤8 or AISHead ≥2 |
- |
| 39 |
Andersson and colleagues (2003)75 |
1992–1993 |
People of Borås region, Sweden who were hospitalized with TBI |
ICD 9: 800 - 804 and 850 - 854 |
- |
| 40 |
Hawley and colleagues (2003)37 |
1992–1998 |
People of North Staffordshire region, United Kingdom 0–15 years who were hospitalized with TBI |
TBI with period of unconsciousness, GCS |
- |
| 41 |
Ingebrigtsen and colleagues (1998)76 |
1993 |
People of Tromsø region, Norway who were hospitalized with head injury |
- |
Head injury was defined as physical damage to the brain or skull caused by external force |
| 42 |
Javouhey and colleagues (2006)77 |
1996–2001 |
People of Rhône region, France who were hospitalized with and those who died due to traffic-induced TBI |
- |
Injury to the brain or the skull |
| 43 |
Baldo and colleagues (2003)78 |
1996–2000 |
People of Veneto region, Italy who were hospitalized with or died due to TBI |
ICD9:800.0 - 801.9, 803.0 - 804.9, 850.0 - 854.1 |
- |
| 44 |
Masson and colleagues (2001)79 |
1996 |
People of Aquitaine region, France who were hospitalized with severe TBI |
Severe TBI with HAIS ≥4, GCS ≤8 |
- |
| 45 |
Puljula and colleagues (2013)47 |
1999 and 2007 |
People of Northern Ostrobothnia region, Finland who were hospitalized with or died due to moderate to severe TBI |
Moderate-to-severe TBI GCS ≤12 on admission to ED |
- |
| 46 |
Servadei and colleagues (2002)80 |
1998 |
People of Romagna region, Italy who were hospitalized with and those who died due to TBI |
ICD 9: 800.0 - 800.3, 801.0 - 801.3, 803.0 - 804.3, 850, 851, 851.1, 852.0, 852.1, 853.0, 853.1, 854.0, 854.1 |
- |
| 47 |
Di Bartolomeo and colleagues (2001)81 |
1998–1999 |
People of Friuli Venezia Giulia region, Italy who were hospitalized with or died due to severe head injury |
Severe head injury with ISS >16, AIS of the head ≥4 |
- |
| 48 |
Servadei and colleagues (2002)82 |
1998 |
People of Romagna and Trentino regions, Italy who were hospitalized with head injury |
ICD 9: 800.0 - 854.1 |
- |
| 49 |
Dahl and colleagues (2006)83 |
1999 and 2000 |
People of Borås region, south-western Sweden 0–17 years hospitalized with mild TBI |
- |
Loss of consciousness, loss of memory of events immediately before or after the accident, any alteration in mental state at the time of the accident, focal neurological deficit |
| 50 |
Rusnak and colleagues (2007)45 |
1999–2004 |
Patients of 5 treatment centers in Austria who were hospitalized with severe TBI |
Severe TBI with GCS ≤8 |
- |
| 51 |
Rickels and colleagues (2010)33 |
2000–2001 |
People of Hannover and Münster regions, Germany who were hospitalized with TBI |
ICD 10: S02, S04, S06, S07, S09 |
Nausea or vomiting, headache, loss of consciousness with anterograde/retrograde amnesia, impaired consciousness or impaired vigilance, fracture of face and/or scull, focal neurological symptom |
| 52 |
Ventsel and colleagues (2008)84 |
2001–2005 |
People of Tartu county, Estonia 0–14 years who were hospitalized with and those who died due to TBI |
ICD 10: S02.0, S02.1, S02.7, S06, S07, S09.7 |
- |
| 53 |
Styrke and colleagues (2007)34 |
2001 |
People of Umeå district, Sweden who were hospitalized with TBI |
ICD 10: S06 |
- |
| 54 |
Rosso and colleagues (2007)85 |
1999–2004 |
Patients of 5 treatment centers in Austria who were hospitalized with severe TBI |
Severe TBI with GCS ≤8 |
- |
| 55 |
Mauritz and colleagues (2008)86 |
2001–2005 |
Patients of thirteen participating hospitals in Austria, Bosnia, Croatia, Macedonia and Slovak Republic who were hospitalized with severe TBI |
Severe TBI with GCS ≤8 |
- |
| 56 |
Numminen (2011)87 |
2002–2004 |
People of 3 municipalities in South East Finland >14 years who were hospitalized with and died due to TBI |
ICD 10: S06, S07 |
Patients who had experienced loss of consciousness or had a headache, nausea or dizziness after head trauma |
| 57 |
Falk (2007)88 |
2002–2003 |
People of Stockholm region, Sweden <16 years who were hospitalized with TBI |
- |
Head injury was defined as any physical damage to the brain or scull caused by external force |
| 58 |
Heskestad and colleagues (2009)89 |
2003 |
People of Stavanger region, Norway who were hospitalized with head injury |
- |
Head injury was defined as physical damage to the brain or skull caused by external force |
| 59 |
Andelic and colleagues (2008)29 |
2005–2006 |
People of Oslo City, Norway who were hospitalized with TBI |
ICD 10: S02.0 - S02.9, S06.0 - S06.9, S07.0, S07.1, S07.8, S07.9, S09.7 - S09.9, T04, T06 |
TBI was defined as damage to brain tissue caused by external mechanical force as evidenced by: loss of consciousness due to brain trauma, or posttraumatic amnesia, or skull fracture |
| 60 |
Von Elm and colleagues (2008)21 |
2005 (6 m.) |
Patients of three trauma centers, Switzerland hospitalized with and those who died due to severe TBI |
Severe TBI with GCS <9 and AISHead >3 |
- |
| 61 |
Frohlich and colleagues (2011)35 |
2005–2007 |
Patients of one university teaching hospital, Ireland hospitalized with TBI |
- |
Patients who were admitted to ICU due to TBI |
| 62 |
Van Pelt and colleagues (2011)38 |
2007–2008 |
Patients of one children's hospital in Netherlands 1 month.-24 years hospitalized with TBI |
- |
History or observed loss of consciousness after head trauma, and/or posttraumatic amnesia, and/or abnormalities at neurological examination, and/or acute traumatic abnormalities on scan images of brain |
| 63 |
Andriessen and colleagues (2011)90 |
2008–2009 |
Patients of five trauma centres in Netherlands ≥16 years hospitalized with moderate and severe TBI |
TBI with GCS ≤13 |
- |
| 64 |
Roe and colleagues (2013)91 |
2009–2011 |
Patients of five university hospitals, Norway ≥16 years hospitalized with severe TBI |
ICD 10: S06.1- S06.9 and TBI with GCS ≤8 within first 24 hours after injury |
- |
| 65 |
Hawley and colleagues (2013)36 |
2011 (6 m.) |
People of Coventry and Warwickshire, United Kingdom 0–14 years hospitalized with minor head injury |
Minor child head injury with GCS of 13–15 |
Head injury defined as any trauma to the head, other than superficial injuries to the face |
| 66 | Katsaragakis and colleagues (2010)92 | 12 m., year unclear | Patients of 30 hospitals in Greece hospitalized with TBI | - | All patients that had at least one brain injury as assessed in the receiving hospital |
all ages and all severity if not specified otherwise; **presented terminology is the same as in the original study.
TBI, traumatic brain injury; ICD, International Classification of Diseases; CT, computed tomography; EEG, electroencephalogram; GCS, Glasgow Coma Scale; AISHead, Abbreviated Injury Score for head injuries; HAIS, Head Abbreviated Injury Scale; ED, emergency department; ISS, Injury Severity Score; ICU, intensive care unit.
More recent studies commonly, although not exclusively, use the ICD 9 and ICD 10 coding systems. Some early studies used ICD 8 (e.g., Engberg and Teasdale [1998]).23 Other standardized coding schemes, such as the Abbreviated Injury Score for head injuries (AISHead or HAIS) as in Walder and colleagues (2013),24 and the Glasgow Coma Scale (GCS) as in Boto and colleagues (2009),25 also were used occasionally. In summary, 31 studies used ICD (8th, 9th, or 10th revision), and 20 studies used GCS or GCS and/or other criteria (usually AIS).
Older studies (from the 1980s and 1990s) tended to use definitions of TBI based on clinical signs, such as “[Head/brain injury with] a) loss of consciousness; b) skull fracture; c) objective neurologic findings which could be reasonably attributed to the head injury,” as in Vazquez-Barquero and colleagues (1992).26
Severity of TBI was measured mainly by GCS, although other scales such as AISHead also were seen, along with non-standardized clinical definitions, for example, based on duration of lost consciousness.
Of the 66 included studies, 15 presented information on severe TBI only, two on moderate and severe, and two on mild TBI only. The rest of the studies presented information on all TBI severities.
Methodological quality
General markers of study rigor, such as a clearly specified research design and the reporting of ethical clearance, funding sources, or potential conflicts of interest were more complete in more recent papers, but rarely found in older papers (see Table 5 for summary assessment).
Table 5.
Quality Assessment of Included Studies Using MORE Checklist–Summary Results
| |
OK |
Minor flaws |
Major flaws |
Poor reporting |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| General descriptive elements | ||||
| Aim of study |
46 (67.6) |
7 (10.3) |
8 (11.8) |
5 (7.4) |
| Funding of study |
38 (55.9) |
0 |
0 |
29 (42.6) |
| Conflict of interest |
31 (45.6) |
0 |
0 |
36 (52.9) |
| Ethical approval |
24 (35.3) |
0 |
0 |
38 (55.9) |
| Study design |
42 (61.8) |
0 |
0 |
24 (35.3) |
| External validity | ||||
| Sampling |
25 (36.8) |
40 (58.8) |
0 |
2 (2.9) |
| Definition of cases | ||||
| • Validation |
42 (61.8) |
20 (29.4) |
3 (4.4) |
2 (2.9) |
| • Severity of TBI |
37 (54.4) |
12 (17.6) |
8 (11.8) |
1 (1.5) |
| Address bias |
5 (7.4) |
36 (52.9) |
19 (27.9) |
6 (8.8) |
| Subject flow |
58 (85.3) |
7 (10.3) |
2 (2.9) |
0 |
| Internal validity | ||||
| Reporting of methods | ||||
| • Source of data |
32 (47.1) |
35 (51.5) |
0 |
0 |
| • Reliability of estimates |
50 (73.5) |
13 (19.1) |
4 (5.9) |
0 |
| Reporting of estimates | ||||
| • Incidence |
38 (55.9) |
11 (16.2) |
11 (16.2) |
1 (1.5) |
| • Mortality | 22 (32.4) | 3 (4.4) | 24 (35.3) | 0 |
MORE, Methodological Evaluation of Observational Research checklist; TBI, traumatic brain injury.
The quality of reporting in the final set of studies was found to be mixed. Some items were generally well reported, for example, the criteria used to define TBI and the data source use of either hospital records or national statistics to calculate incidence.
Incidence
Fifty-one studies reported a measure of TBI incidence, albeit with significant variation around the definition of case ascertainment and case definition (Tables 3, 4, 6, 7). Only eight studies reported the use of age-standardization of incidence rates or confidence intervals around these figures.
Table 6.
Outcomes in Studies With Country-Level Population
| Study author(s) (year) reference number | Source population* | Incidence** per 100,000 | Mortality** per 100,000 | Case fatality rate*** % | |
|---|---|---|---|---|---|
| 1 |
Kannus and colleagues (1999)48 |
Finland (≥60 years, fall-induced only) |
Severe: 85 in 1970 Severe:144 in 1995 |
NR |
NR |
| 2 |
Steudel and colleagues (2005)31 |
Germany |
337 Severe: 33.50 |
27.20 in 1972 9 in 2000 |
NR |
| 3 |
Jennett and MacMillan (1981)49 |
Scotland, England, Wales |
270 (En and W) 313 (Scot) |
10.50 in 1972 (En and W), 9.20 in 1976 (En and W), 10.90 in 1972 (Scot), 9.30 1976 (Scot) |
NR |
| 4 |
Engberg, and Teasdale (1998)23 |
Denmark (0–14 years) |
430 in 1979 240 in 1993 |
M 7.40 and F 4.20 in 1979–1981 M 4.40 and F 3.10 in 1991–1993 |
1.40 |
| 5 |
Engberg and colleagues (2001)50 |
Denmark |
265st. in 1979–1981 157st. in 1991–1993 |
14.68 in 1979–1981 10.67 1991–1993 |
30 |
| 6 |
Mauritz and colleagues (2014)51 |
Austria |
NR |
28.10 in 1980–1984 11.80 in 2010 – 2012 |
NR |
| 7 |
Brazinova and colleagues (2014)52 |
Austria (≥65 years) |
NR |
40 |
NR |
| 8 |
Majdan and colleagues (2014)53 |
Austria (0–19 years) |
NR |
76 in 1980 5 in 2012 |
NR |
| 9 |
Servadei and colleagues (1985)28 |
Republic of San Marino |
694 |
NR |
NR |
| 10 |
Williamson and colleagues (2002)53 |
Scotland (0–14years) |
NR |
4.10 - 1.80 |
NR |
| 11 |
Hartholt and colleagues (2011)46 |
Netherlands (≥65 years, fall-induced only) |
Severe: 53.10st. in 1986 Severe: 119.30st. in 2008 |
NR |
NR |
| 12 |
Sundstrøm and colleagues (2007)55 |
Denmark, Finland Norway, Sweden |
NR |
12.6a 11.50 DE, 21.20 FI, 10.40 NO, 9.50 SE |
NR |
| 13 |
Kleiven and colleagues (2003)56 |
Sweden |
259 |
NR |
NR |
| 14 |
Alaranta and colleagues (2000)57 |
Finland |
99.50 in 1991 99 in 1995 |
NR |
NR |
| 15 |
Koskinen and Alaranta (2008)58 |
Finland |
101b |
18.30b |
5.10 in 2001 – 2005 |
| 16 |
Shivaji and colleagues (2014)22 |
Scotland |
M 446.4 in 2009 F 194,80 in 2009 |
NR |
NR |
| 17 |
Pérez and colleagues (2012)27 |
Spain |
47.26 |
NR |
NR |
| 18 |
Dias and colleagues (2014)59 |
Portugal (≥18 years) |
NR |
NR |
8.70 Mild: 1.10 Moderate - severe: 12.90 |
| 19 |
Walder and colleagues (2013)24 |
Switzerland (≥16 years) |
Severe: 10.58 |
NR |
30.20 (at 14 days) |
| 20 |
Mauritz and colleagues (2014)32 |
Austria |
303 |
11 |
3.60 |
| 21 |
Andelic and colleagues (2012)60 |
Norway (≥16 years) |
Severe: 5.20st. in 2009 Severe: 4.10st. in 2010 |
NR |
29.00 |
| 22 | Scholten and colleagues (2014)61 | Netherlands | 213.60 | NR | NR |
All ages, if not specified otherwise; **crude rates, if not specified otherwise; ***hospital, if not specified otherwise; st.standardized; amedian for all countries; baverage during 15 years.
NR, not reported; En, England; W, Wales; Scot, Scotland; M, males; F, females; DE, Denmark; FI, Finland; NO, Norway; SE, Sweden.
Table 7.
Outcomes in Studies With Regional-Level Population
| Study author(s) (year) reference number | Source population* | Incidence** per 100,000 | Mortality** per 100,000 | Case fatality rate*** % | |
|---|---|---|---|---|---|
| 23 |
Winqvist and colleagues (2007)62 |
Finland (≤ 34 years; birth cohort) |
118 (95% CI,108 – 130) |
14 (95% CI, 11 – 18) |
12 |
| 24 |
Berney and colleagues (1995)63 |
Switzerland (0–15 years) |
291 in 1969–1973 368 in 1986–1990 |
10.40 in 1969–1973 3.50 in 1986–1990 |
29.4 in 1975–1978 15.2 in 1986–1990 |
| 25 |
Berney and colleagues (1994)64 |
Switzerland (0–15 years) |
334 |
NR |
NR |
| 26 |
Nestvold and colleagues (1988)65 |
Norway |
236 |
NR |
4.50 |
| 27 |
Edna and Cappelen (1984)66 |
Norway |
200 |
NR |
2.76 |
| 28 |
Edna and Cappelen (1985)67 |
Norway (traffic-induced only) |
89 |
NR |
3.60 |
| 29 |
Alvarez and colleagues (2011)68 |
Spain (1 months–14 years) |
11 Severe: 5 |
NR |
24.70 |
| 30 |
Johansson and colleagues (1991)69 |
Sweden (16–60 years) |
249 |
NR |
NR |
| 31 |
Servadei and colleagues (1988)30 |
Italy |
849 |
24.40 |
NR |
| 32 |
Tiret and colleagues (1990)70 |
France |
281 |
22 |
6.4 |
| 33 |
Emanuelson and Wendt (1997)71 |
Sweden (0–17 years) |
12 |
2.60 |
NR |
| 34 |
Arnarson and colleagues (1995)72 |
Iceland (0–14 years) |
170 |
3 |
NR |
| 35 |
Boto and colleagues (2009)25 |
Spain (>14 years) |
NR |
NR |
Severe: 46.80 |
| 36 |
Vazquez-Barquero and colleagues (1992)26 |
Spain |
91 |
19.70 |
1.70 |
| 37 |
Bouillon and colleagues (1999)73 |
Germany |
Severe: 10 |
NR |
46.60 |
| 38 |
Maegele and colleagues (2007)74 |
Germany |
Severe: 7.30 |
NR |
Severe: 45.80 |
| 39 |
Andersson and colleagues (2003)75 |
Sweden |
546 |
NR |
NR |
| 40 |
Hawley and colleagues (2003)37 |
United Kingdom (0–15 years) |
280 Mild: 232 Moderate: 25 Severe: 17 |
2 |
NR |
| 41 |
Ingebrigtsen and colleagues (1998)76 |
Norway |
229 |
NR |
NR |
| 42 |
Javouhey and colleagues (2006)77 |
France (traffic-induced only) |
Mild: 74.7 Moderate: 47.5 Severe: 13.7 |
5.30 |
38.10 |
| 43 |
Baldo and colleagues (2003)78 |
Italy |
301 in 1996 212.40 in 2000 |
7.40 in 1996 6.10 in 2000 |
NR |
| 44 |
Masson and colleagues (2001)79 |
France |
Severe:17.30 (95% CI, 15.80 – 18.80) |
Severe: 5.20 (95% CI, 4.29 – 6) |
Severe: 30 |
| 45 |
Puljula and colleagues (2013)47 |
Finland |
Moderate-severe:34 in 1999 Moderate-severe:35 in 2007 |
NR |
60 |
| 46 |
Servadei and colleagues (2002)80 |
Italy |
250 |
18.3 |
2.8 |
| 47 |
Di Bartolomeo and colleagues (2001)81 |
Italy |
NR |
NR |
Severe: 27 |
| 48 |
Servadei and colleagues (2002)82 |
Italy |
314 |
NR |
NR |
| 49 |
Dahl and colleagues (2006)83 |
Sweden (0–17 years) |
Mild: 468 |
0 |
0 |
| 50 |
Rusnak and colleagues (2007)45 |
Austria |
NR |
NR |
38 |
| 51 |
Rickels and colleagues (2010)33 |
Germany |
332 Mild: 302, moderate: 13, s: 17 |
3.3 |
NR |
| 52 |
Ventsel and colleagues (2008)84 |
Estonia (0–14 years) |
369 (95% CI, 337 – 403) Mild: 303 (95% CI, 274 – 334) Moderate: 30 (95% CI, 21 – 40) Severe: 36 (95% CI, 27 – 47) |
3.10 |
NR |
| 53 |
Styrke and colleagues (2007)34 |
Sweden |
354 |
NR |
NR |
| 54 |
Rosso and colleagues (2007)85 |
Austria |
NR |
NR |
Severe: 34 (at 3 months) |
| 55 |
Mauritz and colleagues (2008)86 |
Austria, Bosnia, Croatia, Macedonia and Slovak Republic |
NR |
NR |
42 in HI 48 in UMI 55 in LMI (at 3 months) |
| 56 |
Numminen (2011)87 |
Finland (>14 years) |
221 (95% CI, 176–265) |
NR |
7.60 (at 1 month) |
| 57 |
Falk (2007)88 |
Sweden (<16 years) |
865 (95% CI, 835–895) |
NR |
NR |
| 58 |
Heskestad and colleagues (2009)89 |
Norway |
207 |
NR |
NR |
| 59 |
Andelic and colleagues (2008)29 |
Norway |
83.30 |
5.00 |
2 Severe: 18.5 Moderate: 5.7 Mild: 0.5 |
| 60 |
Von Elm and colleagues (2008)21 |
Switzerland |
Severe: 8.20 |
NR |
70 |
| 61 |
Frohlich and colleagues (2011)35 |
Ireland |
NR |
NR |
37 |
| 62 |
Van Pelt and colleagues (2011)38 |
Netherlands (1m.–24 years) |
113.90 |
1.50 |
NR |
| 63 |
Andriessen and colleagues (2011)90 |
Netherlands (≥16 years) |
NR |
NR |
Severe: 46 Moderate: 21 (at 6 months) |
| 64 |
Roe and colleagues (2013)91 |
Norway (≥16 years) |
NR |
NR |
Severe: 34.00 (at 3 months) |
| 65 |
Hawley and colleagues (2013)36 |
United Kingdom (0–14 years) |
Mild: 3419 |
NR |
NR |
| 66 | Katsaragakis and colleagues (2010)92 | Greece | NR | NR | 11.50 |
All ages, if not specified otherwise; **crude rates, if not specified otherwise; ***hospital, if not specified otherwise; st.standardized; amedian for all countries; baverage during 15 years.
NR, not reported; CI, confidence interval; HI, high income; UMI, upper middle income; LMI, lower middle income.
Of the 22 country-level studies (Table 6), 12 reported on the incidence of TBI across all severities and of these, 11 included subjects of all ages. Two studies reported on fall-related TBIs only, while the majority of studies reported two or more types of mechanism of injury.
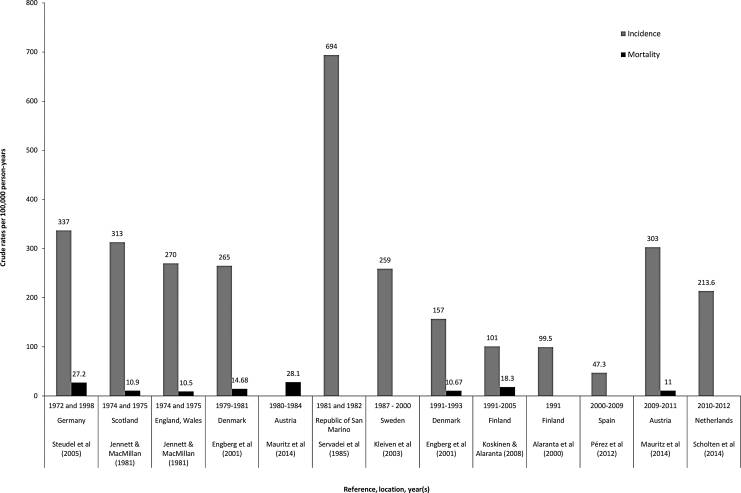
In the group of country-level studies, the range of reported crude incidence rates is as follows: the lowest reported incidence rate is by Pérez and colleagues (2012) in Spain (study period 2000–2009; 47.3 per 100,000 population per year)27; the highest is reported by Servadei and colleagues (1985) for the Republic of San Marino (study period 1981–1982; 694 per 100,000 population per year).28 Crude incidence and mortality rates of all country-level studies that include all ages and all severities of injury are presented in Figure 2 in chronological order by study period.
FIG. 2.
Traumatic brain injury incidence and mortality rates (crude) per 100,000 population per year in country-level studies.
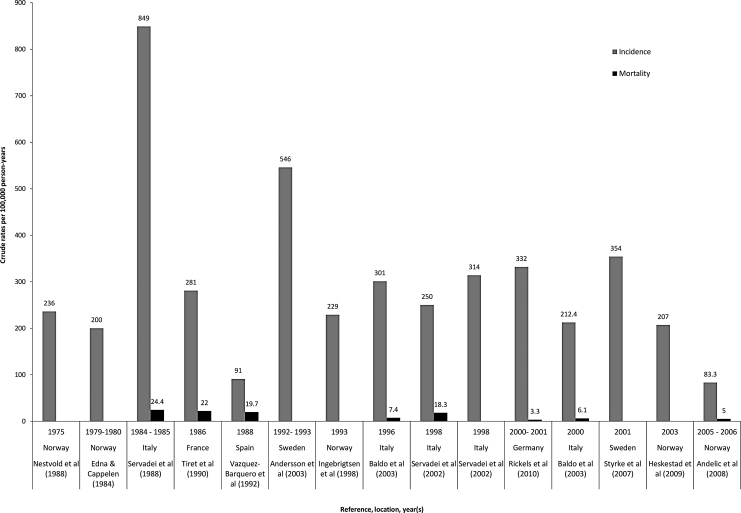
Of 44 regional-level area studies (Table 7), 14 reported incidence rates for all ages and all severities. Two studies reported on only one mechanism of injury–traffic accidents. Figure 3 shows the crude incidence and mortality rates of these studies that include all ages and all TBI severity in chronological order by study period. The range is even larger here than in the group of country-level studies (Fig. 2): the lowest is reported by Andelic and colleagues (2008) for Norway (83.3 per 100,000 population per year)29; and the largest is reported by Servadei and colleagues (1988) for Italy (849 per 100,000 population per year).30
FIG. 3.
Traumatic brain injury incidence and mortality (crude) rates per 100,000 population per year in regional-level studies.
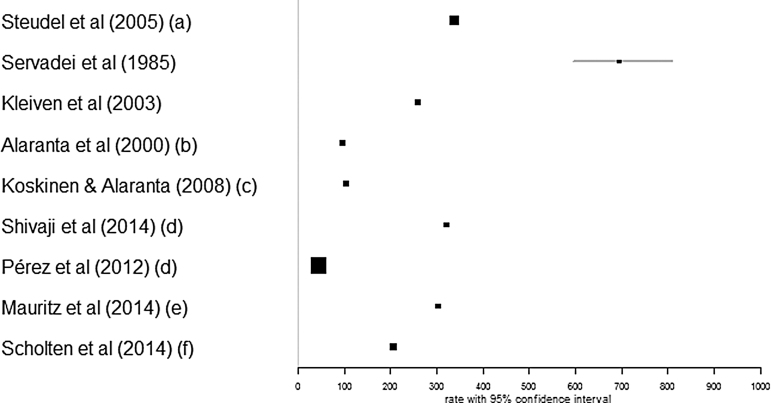
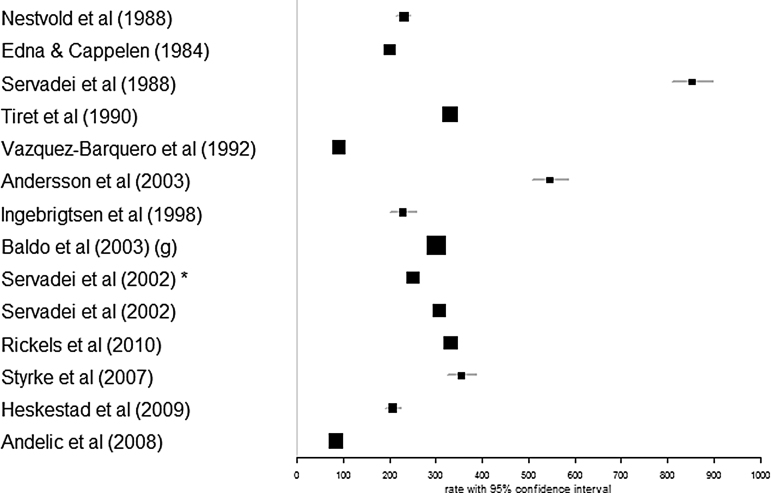
The range of crude incidence rates with confidence intervals in two sets of studies – nine country-level studies and 14 regional-level studies is shown in Figure 4 and 5, respectively. In order to make the fairest assessment, the figures include only studies reporting on all ages and all TBI severities.
FIG. 4.
Traumatic brain injury (TBI) incidence rates (crude) per 100,000 population per year in country-level studies. Studies reporting on all ages and all TBI severity were used. The size of the boxes depicts the weight (relative to other studies in the analysis) that the study has in relation to the summary measure of the meta-analysis; larger boxes depict higher weight. (a), 1998 data; (b), average for 5-year period (1991–1995); (c), 2001–2005 data; (d), 2009 data; (e), average for 2009–2011; (f), average for 2010–2012.
FIG. 5.
Traumatic brain injury (TBI) incidence rates (crude) per 100,000 population per year in regional-level studies. Studies reporting on all ages and all TBI severity were used. The size of the boxes depicts the weight (relative to other studies in the analysis) that the study has in relation to the summary measure of the meta-analysis; larger boxes depict higher weight. *ref. no. 80; (g), 1996 data.
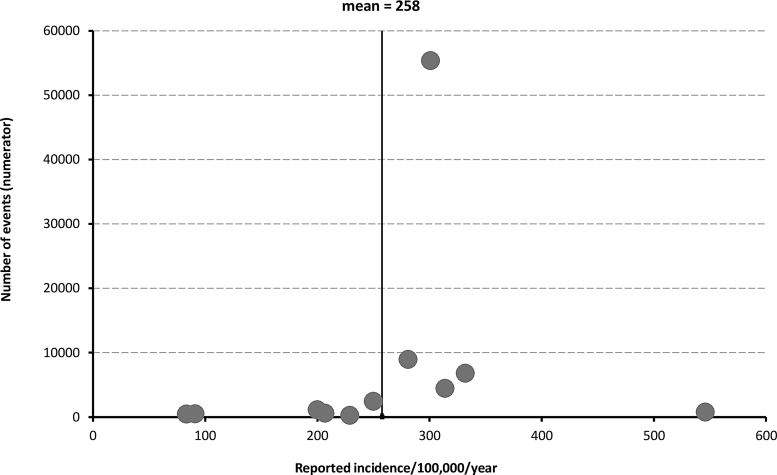
The funnel plot of incidence rates of regional-level studies, shown in Figure 6, suggests there is little indication of missing or selectively unpublished data. The plot shows a wider variability in incidence estimates in smaller studies, with a more stable incidence rate in larger studies, close to the mean value of 258 per 100,000 population per year. There were insufficient studies at national level reporting enough detail to produce a funnel plot for country-level studies.
FIG. 6.
Funnel plot of traumatic brain injury incidence in regional-level studies.
Mortality and case fatality rates
Of the 27 studies reporting mortality rates, 14 reported mortality across ages and severities (Tables 6 and 7). Mortality rates of studies including all ages and all severities are presented together, with incidence rates in Figure 2 for country-level studies, and Figure 3 for regional-level area studies. As with incidence, range of reported crude mortality rates is quite large–from 9 per 100,000 population per year (Steudel and colleagues [2005])37 to 28.10 per 100,000 population per year (Mauritz and colleagues [2014])38 in country-level studies, and from 3.3 per 100,000 population per year (Rickels and colleagues [2010])39 to 24.4 per 100,000 population per year (Servadei and colleagues [1988])36 in regional-level studies.
Age and sex
Age and sex breakdown was reported in the majority of studies. It is difficult to compare distribution of TBI across populations, as many studies report only on part of the population (children or older adults, or adults only, etc.). Mean (or median) age was stated in 32 studies. In studies of all ages, all TBI severities, and all mechanisms, the lowest reported mean age was 26.7 in the Republic of San Marino (Servadei and colleagues [1985]),28 the highest was 44.5 in Austria in 2009–2011.32 The reported proportion of males was always greater than that of females (irrespective of age, severity and mechanism of injury), ranging from 55% in Sweden in 200134 to 80% in Ireland in 2005–2007.35
Mechanism of injury
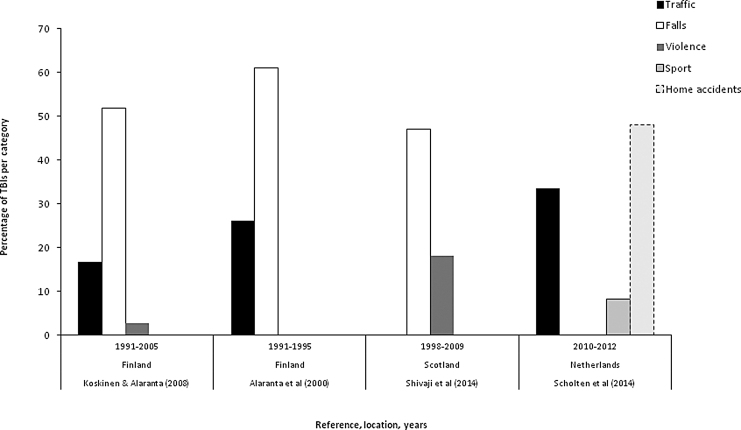
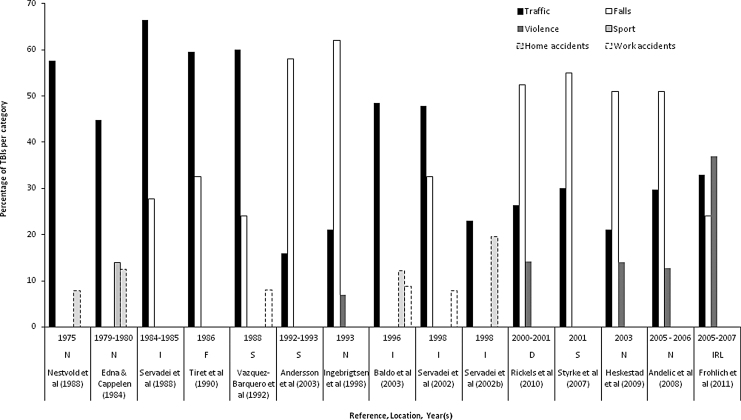
A total of 57 studies recorded the mechanisms of injury; of these, 16 were studies that reported on TBI across country-level populations and a further 41 studies reported on specific mechanisms of injury from regional-level populations. Across ages and severities, the three most common mechanisms (or two if only two mechanisms were reported) of injury for each sample are presented in the Figures 7 and 8.
FIG. 7.
The most common mechanisms of injury in country-level studies.
FIG. 8.
The most common mechanisms of injury in regional-level studies.
These seven distinct injury mechanisms include traffic-related, falls, violence, sports-related, accidents in the home or at work, and suicides or suicide attempts. Some studies also reported “struck by object” as a separate mechanism36,37; however, this is not reported in the graphs as it was felt that it may overlap with other more specific causes, such as violence, sports, or domestic accident. One study noted that the mechanism of “accidents in the home” may include instances of domestic violence.38
Time trends
Although no formal test or meta-analysis has been carried out, it is possible to observe an apparent slight downwards trend in incidence of TBI over time, in both country-level (Fig. 2) and regional-level graphs (Fig. 3). However, if the highest outliers on each graph are ignored (Servadei and colleagues [1985]28 and Servadei and colleagues [1988],30 respectively), the reduction over time is much less apparent. There is little or no indication of a change over time in the mortality rates at either country- or regional-level.
When examining mechanisms, the proportion of TBIs caused by traffic collisions has been lower in recent years, and correspondingly there is an increase in the proportion of cases attributed to falls. This pattern appears in the studies of mechanisms of injury at a regional level. Country-level studies–which included all severities of injury and all age groups, and reported on mechanism of injury–number only four, and three of these describe overlapping time periods; it is not possible to make any inferences regarding time trends among this small sub-group.
Discussion
The aim of this work was to produce a comprehensive and up-to-date review of incidence, mortality, and mechanisms of TBI across Europe. In accordance with the geographical scope of the over-arching CENTER-TBI project, the aim of this study was to review TBI patterns in Europe. A wide range of rates of incidence and mortality were reported. For all ages, all TBI severity studies, the lowest reported crude incidence rate was 47.3 per 100,000 population per year; the highest was 849 per 100,000 population per year. The reported crude mortality rates ranged from 3.3 to 28.10 per 100,000 population per year. These rates are broadly similar to those seen in the 2006 review.3 The most common mechanism of injury in studies within our review appears to be shifting in Europe from road traffic incidents to falls in more recent studies (Fig. 7 and Fig. 8).
Distribution of TBI in European populations is widely researched and presented in numerous published studies. However, it is difficult to produce informative comparisons of these presented data, as the studies vary greatly in TBI definition and case ascertainment methods. Comparison is also difficult due to the fact the reviewed data were not standardized. This should be improved in the future by standardized data collection and coding.10 For the time being, it is important to make the best use the existing data, and we believe the systematic review presented here provides the most useful opportunity to compare results with those of Tagliaferri and colleagues published a decade ago53 and Peeters and colleagues published recently.13 The incidence is changing only slightly over time and it may be contributed by the reporting variations during the period under investigation..
The recently-published systematic review of traumatic brain injury in Europe–set up as an update to Tagliaferri and colleagues' 2006 review,3 presenting data for the period 1990-2014–had broadly similar findings and conclusions to our review, (i.e., no decreasing trend of TBI incidence in Europe). This review, like ours, found large variations in inclusion criteria, case ascertainment and case definitions. The incidence of TBI is thus difficult to compare between included studies, as well as between this and other reviews. In Peeters and colleagues' report, the incidence of TBI ranged between 47.3 and 546 per 100,000 population per year.13 Given our broader time scale (no time limit), we found an even larger range–the incidence range in combined country- and regional-level studies was 47.3 to 849 per 100,000 population per year.
While some countries may be seeing a reduction in TBI (or a subgroup of TBI) incidence,39–41 our review suggests that across the continent of Europe, mean incidence rates remain broadly the same as in the 2006 review.3 These findings from Europe are similar to the incidence rates in the United States (180 to 250 per 100,000 population per year),42 but considerably lower than in a recent study in New Zealand, which found an incidence in excess of 700 per 100,000 person-years.43
Worldwide, TBI incidence may be increasing still due to the wider use of motor vehicles in low-middle income countries and an increase in falls among older people in high-income countries.41,44
The main methodological weaknesses observed in studies included in our review concerned poor reporting of funding, ethical approval, and study design. Very few studies were performed well according to the MORE assessment criteria. This may be in part because of the differing objectives of the included studies (some set out to study incidence and/or mortality, but others focused on mechanisms). However, it might have been expected that more of the studies focusing on incidence would perform well on this checklist. This again highlights the need for standardization of definitions and reporting if published studies are to be more comparable and informative.
It is also important to note that in this systematic review, which set out to review the available studies from all of Europe, suitable nationally-representative data were only found for 13 countries. These countries were principally members of the EU, plus Switzerland and Norway. Given that the EU currently comprises 28 countries and Europe as a whole includes almost 50 countries, it is apparent that there is a lack of good quality data collection and publication in many states. This limits the completeness of any attempt to describe European TBI incidence and mortality.
The reported crude incidence rates in regional populations or hospital catchment areas were found to be slightly higher than national surveys. It may be that studies of smaller regions or in a few nominated hospitals were conducted there because that region or hospital contains a specialist center, to which TBI cases are more frequently referred. International transfers of patients are assumed to be rarer, so national incidence data may be more complete.
When regional data were examined in a funnel plot, publication bias appeared unlikely.
There was some variability in the way relevant scientific terms have been used in different studies. In this review, incidence is defined as the rate of TBIs recorded in the original studies per 100,000 population per year. Using this measure, the majority of included studies reported actual hospital admission rate of participating treatment centers (or all hospitals in case of country-level studies). This is a slightly different measure to population incidence, in which all cases would have been traced, rather than just those arriving in a hospital. Again this limits the completeness of this review and implies that true population incidences are likely to be higher than the rates reported here.
Although the lack of age-adjusted figures make it difficult to draw direct comparisons, certain trends can be observed. Mortality rates in studies, including TBIs of all severities, vary many-fold; however, there was little indication of a trend towards increase or decrease over time. Some studies stated that they excluded patients who were dead on arrival at hospital (e.g., Rusnak and colleagues [2007], Vazquez-Barquero and colleagues [1992]).26,45 As such, mortality rates shown in national data, rather than hospital records, may present a more complete picture.
In every study reporting sex ratios, there are more male patients recorded as having TBI than female patients. This may reflect the fact that some of the major causes of TBI, such as traffic incidents, violence, and sporting injuries, are related to more male-dominated activities. But the proportion of men in TBI studies decreased with age. In studies of older patients, with more women, the prevailing mechanism of TBI in older cases is falls.46 However, a lack of age-adjusted results makes it impossible to draw firm conclusions about any difference in sex distributions of TBI.
There appears to be a changing pattern of mechanisms of injury over time, as the number of TBIs occurring in traffic incidents reduces, and conversely the contribution of falls becomes relatively greater in recent studies. This trend already has been described in studies in high-income countries.44 This may relate to improved road infrastructure and traffic discipline and therefore declining traffic-related TBI incidence, as well as demographic trend of population aging. Few studies have attempted to look at epidemiological causes “upstream” of the immediate injury event; however, alcohol is considered a possible risk factor contributing to traffic or personal violence incidents.47 This topic warrants further investigation.
Strengths and limitations
This review follows contemporary best practice in systematic review methods, with a comprehensive search strategy specified a priori, and a clear indication of why studies were included or excluded. It is likely that this search strategy, which was re-run as close as possible to the time of publication, has captured the vast majority of relevant published results.
It is likely that the figures shown here represent a relatively complete picture of the existing research on the burden of TBI in Europe. It is possible that mild TBIs may be under-diagnosed when a patient is admitted with multiple trauma or other injuries in addition to TBI. However, it seems unlikely that many TBI sufferers would be treated at home without the attention of medical professionals. The legal requirements for recording of fatal traumatic injuries vary across Europe but are usually strict. The gradual acceptance of systematic classification of injuries, such as ICD 10, means that, especially in more recent studies, data can be easily sorted to analyze events such as TBI.
Many studies stated that their incidence rates excluded non-residents who suffered TBI in the area. Hence, it is possible that some cases may not have been normally resident in the population used as the denominator in incidence calculations, leading to a small bias toward increased rates in places such as holiday destinations.
In summarizing the studies of TBI here, all papers that include an incidence, mortality or case-fatality rate for TBI are presented, regardless of how the authors defined the actual injury. In recent studies the ICD 9 or 10 coding systems were widely used and specifically described; however, in older papers, there were several different non-standard descriptions used based on external signs of injury and/or assessment of brain function. Thus, it is possible that there will be some variability in those deemed eligible, which may reduce the relevance of comparisons between different papers. The same can be said for classifications according to severity, where GCS is now a widely-accepted standard but alternative classifications, such as duration of lost consciousness, have been used at times.
No attempts were made to identify or translate non-English language publications. This is a weakness and it is possible that some relevant studies have been omitted due to this.
No attempt was made to verify the methods used by different research groups to ascertain mechanism of injury. Whereas some events may be unlikely to be misclassified (e.g., a traffic accident will often be associated with police reports of the event), others may possibly be confused, such falls and (attempted) suicides. One paper mentioned the likelihood that some acts of inter-personal violence (i.e., domestic abuse) are sometimes recorded as home accidents.38 Further, the different countries included at different time-points may also exhibit other characteristics that would affect the likelihood of a particular mechanism of injury (e.g., variation in the laws or conventions of driving certain classes of vehicle). Hence, no causal conclusions are drawn about changing mechanisms, but the general trend of reduction in the proportion of traffic-related injury is consistent with the findings of other recent research.
Conclusions and Recommendations
This review found that large variations of TBI incidence and mortality rates exist between different countries and populations. There is some evidence of a changing pattern of mechanisms over time, which may indicate success of previous public health initiatives to reduce traffic-related injuries, but also highlight the contemporary need to understand fall-related injuries, especially among the elderly. The higher rates observed in these studies present opportunities for public health policy and evidence-based clinical guidelines to reduce the suffering caused by this serious injury.
We have highlighted above the variable nature of the definitions of TBI, and the thresholds applied to classify such injuries as mild, moderate, or severe. We concur with other research groups (Maas and colleagues; Feigin and colleagues)10,43 who have argued that the comparability of research outputs and the opportunities to exploit collaborative research can only benefit from improved levels of standardization of case ascertainment and definitions of grades of injury.
Acknowledgments
This study was funded by the European Union FP 7th Framework program (grant 602150).
Appendix 1. Database Search Algorithms and Key Words
PubMed search algorithm
(((((((((epidemiology[Title/Abstract]) OR case fatality[Title/Abstract]) OR incidence[Title/Abstract]) OR prevalence[Title/Abstract]) OR mortality[Title/Abstract])) AND ((europe[MeSH Terms]) OR europ*)) AND ((((((craniocerebral injuries[MeSH Terms]) OR brain injuries[MeSH Terms]) OR head injur*[Title/Abstract]) OR brain injur*[Title/Abstract]) OR head trauma[Title/Abstract]) OR brain trauma[Title/Abstract]))))
Web of Science search algorithm
((TS = (“brain injur*”)) OR (TS = (“head injur*”)) OR (TS = (“brain trauma”)) OR (TS = (“head trauma”))) AND ((TS = (epidemiology)) OR (TS = (incidence)) OR (TI = (prevalence)) OR (TI = (mortality))) Refined by: *[excluding]:* *DOCUMENT TYPES:* (REVIEW) AND *COUNTRIES/TERRITORIES:* (CROATIA OR ENGLAND OR WALES OR GERMANY OR CZECH REPUBLIC OR ITALY OR SLOVAKIA OR MACEDONIA OR FRANCE OR SPAIN OR NORTH IRELAND OR SWEDEN OR NETHERLANDS OR SCOTLAND OR SWITZERLAND OR ALBANIA OR HUNGARY OR AZERBAIJAN OR NORWAY OR AUSTRIA OR SERBIA OR SLOVENIA OR BYELARUS OR ESTONIA OR DENMARK OR FINLAND OR IRELAND OR ICELAND OR LITHUANIA OR BELGIUM OR ROMANIA OR GREECE OR YUGOSLAVIA OR POLAND)
CINAHL search
S1 TI epidemiology OR AB epidemiology
S2 TI case fatality OR AB case fatality
S3 TI incidence OR AB incidence
S4 TI prevalence OR AB prevalence
S5 TI mortality OR AB mortality
S6 S1 OR S2 OR S3 OR S4 OR S5
S7 (MH “Europe”)
S8 TI europe*
S9 S7 OR S8
S10 (MH “Brain Injuries”)
S11 (MH “Head Injuries”)
S12 TI head injur* OR AB head injur*
S13 TI brain injur* OR AB brain injur*
S14 TI head trauma OR AB head trauma
S15 TI brain trauma OR AB brain trauma
S16 S10 OR S11 OR S12 OR S13 OR S14 OR S15
S17 S6 AND S9 AND S16
EMBASE Search
-
1.
epidemiology.mp.
-
2.
case fatality.mp.
-
3.
incidence.mp.
-
4.
prevalence.mp.
-
5.
mortality.mp.
-
6.
exp head injury/
-
7.
head*.mp.
-
8.
brain*.mp.
-
9.
7 or 8
-
10.
(injur* or trauma*).mp
-
11.
((head* or brain*) adj2 (injur* or trauma*)).mp.
-
12.
exp Europe/
-
13.
europ*.mp.
-
14.
12 or 13
-
15.
6 or 11
-
16.
or/1–5
-
17.
14 and 15 and 16
Appendix 2.
Methodological Evaluation of Observational Research (MORE) Checklist for Quality Assessment of Included Studies
| Type | Criteria | Conditions | Assessment | |
|---|---|---|---|---|
| General descriptive |
Aim of study |
a) Included incidence/prevalence estimation with clear target population |
OK |
|
| b) Included incidence/prevalence estimation without clear target population |
Minor flaw |
|||
| c) Aim of study was not stated |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| Funding of study |
Reported |
OK |
||
| Not reported |
Poor reporting |
|||
| Conflict of interest |
Reported |
OK |
||
| Not reported |
Poor reporting |
|||
| Ethical approval |
Reported |
OK |
||
| Not reported |
Poor reporting |
|||
| Study design |
Reported |
OK |
||
| Not reported |
Poor reporting |
|||
| External validity |
Sampling |
Sampling frame |
a) Not applicable for study design |
NA |
| b) Sampling within nationally representative registries or databases |
OK |
|||
| c) Medical records |
Minor flaw |
|||
| d) Insurance claims |
Minor flaw |
|||
| e) Outpatients contacts |
Major flaw |
|||
| f) Unclear due to poor reporting |
Poor reporting |
|||
| Definition of cases |
Validation |
a) Criteria of TBI were stated according to the guidelines |
OK |
|
| b) TBI were defined by ICD codes |
OK |
|||
| c) Criteria of TBI were not stated according to the guidelines |
Minor flaw |
|||
| d) Criteria of TBI were not stated |
Major flaw |
|||
| e) Unclear due to poor reporting |
Poor reporting |
|||
| Severity of TBI |
a) Stated in the study with scales |
OK |
||
| b) Stated in the study without scales |
Minor flaw |
|||
| c) Not stated in the study |
Major flaw |
|||
| d) Unclear due to poor reporting |
poor reporting |
|||
| Address bias |
Sampling bias is addressed in the analysis (can by mentioned in recommendations) |
a) Not applicable for study design |
NA |
|
| b) Weighting of the estimates by probability of selection |
OK |
|||
| c) Weighting of the estimates by non-response adjustment within sampling subgroups |
OK |
|||
| d) Post-stratification by age |
OK |
|||
| e) Post-stratification by sex |
OK |
|||
| f) Mentioned, but not addressed in analysis |
Minor flaw |
|||
| g) Not mentioned and not addressed in analysis |
Major flaw |
|||
| h) Unclear due to poor reporting |
Poor reporting |
|||
| Subject flow |
a) Not applicable for study design |
NA |
||
| b) Number of enrolled stated clearly |
OK |
|||
| c) Number of enrolled not stated clearly |
Minor flaw |
|||
| d) Number of enrolled not stated |
Major flaw |
|||
| e) Unclear due to poor reporting |
Poor reporting |
|||
| Internal validity | Reporting of methods |
Source of data |
a) Objectively measured with diagnostic methods for the purpose of the study (independent on health care) |
OK |
| b) Measured by interviewers for the study |
OK |
|||
| c) Obtained during clinical examination for the purpose of the study |
OK |
|||
| d) Obtained from registries or administrative databases (collected for epidemiologic evaluation independent of health care) |
OK |
|||
| e) Obtained from medical records (mining of the data collected for health care purposes) |
Minor flaw |
|||
| f) Obtained from administrative database (mining of the data collected for health care purposes) |
Minor flaw |
|||
| g) Source of data is not stated in the study |
Major flaw |
|||
| h) Unclear due to poor reporting |
Poor reporting |
|||
| Reliability of the estimates |
a) Methods of data analysis (nominators/denominators) are stated clearly |
OK |
||
| b) Methods of data analysis (nominators/denominators) are stated, but not clearly |
Minor flaw |
|||
| c) Methods of data analysis (nominators/denominators) are not stated |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| Reporting of estimates | Incidence |
a) Incidence type (cumulative incidence, incidence rate) stated and counted clearly |
OK |
|
| b) Incidence type (cumulative incidence, incidence rate) stated and counted not clearly |
Minor flaw |
|||
| c) Incidence type (cumulative incidence, incidence rate) not stated and not counted |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Precision of estimation (error, 95% CI) reported in all |
OK |
|||
| b) Precision of estimation (error, 95% CI) reported not in all |
Minor flaw |
|||
| c) Precision of estimation (error, 95% CI) omitted |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Age adjusted incidence in total sample |
OK |
|||
| b) Crude incidence in total sample |
Minor flaw |
|||
| c) The incidence is not stated as age adjusted or crude |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Age adjusted incidences in all population subgroups |
OK |
|||
| b) Age adjusted incidences not in all population subgroups |
Minor flaw |
|||
| c) Crude incidences in subgroups |
Minor flaw |
|||
| d) Incidences are not stated as age adjusted or crude |
Major flaw |
|||
| e) Unclear due to poor reporting |
Poor reporting |
|||
| Mortality | a) Mortality in all population is counted from all population |
OK |
||
| b) Mortality in all population is counted not clearly |
Minor flaw |
|||
| c) Mortality in all population is counted as case fatality rate (only from the cases not from all population) |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Precision of estimation (error, 95% CI) reported in all |
OK |
|||
| b) Precision of estimation (error, 95% CI) reported not in all |
Minor flaw |
|||
| c) Precision of estimation (error, 95% CI) omitted |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Age adjusted mortality in total sample |
OK |
|||
| b) Crude mortality in total sample |
Minor flaw |
|||
| c) The mortality is not stated as age adjusted or crude |
Major flaw |
|||
| d) Unclear due to poor reporting |
Poor reporting |
|||
| a) Age adjusted mortalities in all population subgroups |
OK |
|||
| b) Age adjusted mortalities not in all population subgroups |
Minor flaw |
|||
| c) Crude mortalities in subgroups |
Minor flaw |
|||
| d) Mortalities are not stated as age adjusted or crude |
Major flaw |
|||
| e) Unclear due to poor reporting | Poor reporting | |||
TBI, traumatic brain injury; ICD, International Classification of Diseases; NA, not applicable.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Rodriguez, S.R., Mallonee, S., Archer, P., and Gofton, J. (2006). Evaluation of death certificate-based surveillance for traumatic brain injury: Oklahoma 2002. Public Health Rep. 121, 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Faul, M.D., Wald, M.M., Xu, L., and Coronado, V.G. (2010). Traumatic brain injury in the United States; Emergency Department Visits, Hospitalizations, and Deaths, 2002–2006. Centers for Disease Control and Prevention. Atlanta, GA [Google Scholar]
- 3. Tagliaferri, F., Compagnone, C., Korsic, M., Servadei, F., and Kraus, J. (2006). A systematic review of brain injury epidemiology in Europe. Acta Neurochir. (Wien) 148, 255–268 [DOI] [PubMed] [Google Scholar]
- 4. Hellawell, D.J., Taylor, R.T., and Pentland, B. (1999). Cognitive and psychosocial outcome following moderate or severe traumatic brain injury. Brain Inj. 13, 489–504 [DOI] [PubMed] [Google Scholar]
- 5. Teasdale, G. and Jennett, B. (1976). Assessment and prognosis of coma after head injury. Acta Neurochir. 34, 45–55 [DOI] [PubMed] [Google Scholar]
- 6. Ono, J.I., Yamaura, A., Kubota, M., Okimura, Y., and Isobe, K. (2001). Outcome prediction in severe head injury: analyses of clinical prognostic factors. J. Clin. Neurosci. 8, 120–123 [DOI] [PubMed] [Google Scholar]
- 7. Dikmen, S.S., Machamer, J.E., Powell, J.M., and Temkin, N.R. (2003). Outcome 3 to 5 years after moderate to severe traumatic brain injury. Arch. Phys. Med. Rehabil. 84, 1449–1457 [DOI] [PubMed] [Google Scholar]
- 8. Maas, A.I., Lingsma, H.F., and Roozenbeek, B. (2015). Predicting outcome after traumatic brain injury. Handb. Clin. Neurol. 128, 455–474 [DOI] [PubMed] [Google Scholar]
- 9. European Parliament. Available at: www.europarl.europa.eu/aboutparliament/en/20150201PVL00004/Legislative-powers. Accessed January15, 2015
- 10. Maas, A.I., Harrison-Felix, C.L., Menon, D., Adelson, P.D., Balkin, T., Bullock, R., Engel, D.C., Gordon, W., Langlois-Orman, J., Lew, H.L., Robertson, C., Temkin, N., Valadka, A., Verfaellie, M., Wainwright, M., Wright, D.W., and Schwab, K. (2011). Standardizing data collection in traumatic brain injury. J. Neurotrauma 28, 177–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Menon, D.K., Schwab, K., Wright, D.W., and Maas, A.I. (2010). Position statement: definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 91, 1637–1640 [DOI] [PubMed] [Google Scholar]
- 12. Menon, D.K. and Maas, A.I. (2015). Traumatic brain injury in 2014. Progress, failures and new approaches for TBI research. Nat. Rev. Neurol. 11, 71–72 [DOI] [PubMed] [Google Scholar]
- 13. Peeters, W., van den Brande, R., Polinder, S., Brazinova, A., Steyerberg, E.W., Lingsma, H.F., and Maas, A.I. (2015). Epidemiology of traumatic brain injury in Europe. Acta Neurochir. 157, 1683–1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moher, D., Liberati, A., Tetzlaff, J., and Altman, D.G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 62, 1006–1012 [DOI] [PubMed] [Google Scholar]
- 15. Maas, A.I., Menon, D.K., Steyerberg, E.W., Citerio, G., Lecky, F., Manley, G.T., Hill, S., Legrand, V., and Sorgner, A. (2015). Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): a prospective longitudinal observational study. Neurosurgery 76, 67–80 [DOI] [PubMed] [Google Scholar]
- 16. Elliott, J.H., Turner, T., Clavisi, O., Thomas, J., Higgins, J.P., Mavergames, C., and Gruen, R.L. (2014). Living systematic reviews: an emerging opportunity to narrow the evidence-practice gap. PLoS Med. 11, e1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Synnot, A., Gruen, R.L., Menon, D., Steyerberg, E.W., Buki, A., Peul, W., Elliott, J.H., and Maas, A. (2015). A new approach to evidence synthesis in traumatic brain injury: living systematic reviews. J. Neurotrauma 2015 Sep 28; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Covidence. Available at: www.covidence.org. Accessed December20, 2015
- 19. Shamliyan, T.A., Kane, R.L., Ansari, M.T., Raman, G., Berkman, N.D., Grant, M., Janes, G., Maglione, M., Moher, D., Nasser, M., Robinson, K.A., Segal, J.B., and Tsouros, S. (2011). Development quality criteria to evaluate nontherapeutic studies of incidence, prevalence, or risk factors of chronic diseases: pilot study of new checklists. J. Clin. Epidemiol. 64, 637–657 [DOI] [PubMed] [Google Scholar]
- 20. Stolwijk, C., van Tubergen, A., Castillo-Ortiz, J.D., and Boonen, A. (2015). Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann. Rheum. Dis. 74, 65–73 [DOI] [PubMed] [Google Scholar]
- 21. von Elm, E., Osterwalder, J.J., Graber, C., Schoettker, P., Stocker, R., Zangger, P., Vuadens, P., Egger, M., and Walder, B. (2008). Severe traumatic brain injury in Switzerland - feasibility and first results of a cohort study. Swiss Med. Wkly. 138, 327–334 [DOI] [PubMed] [Google Scholar]
- 22. Shivaji, T., Lee, A., Dougall, N., McMillan, T., and Stark, C. (2014). The epidemiology of hospital treated traumatic brain injury in Scotland. BMC Neurol. 14, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Engberg, A. and Teasdale, T.W. (1998). Traumatic brain injury in children in Denmark: a national 15-year study. Eur. J. Epidemiol. 14, 165–173 [DOI] [PubMed] [Google Scholar]
- 24. Walder, B., Haller, G., Rebetez, M.M., Delhumeau, C., Bottequin, E., Schoettker, P., Ravussin, P., Brodmann Maeder, M., Stover, J.F., Zurcher, M., Haller, A., Wackelin, A., Haberthur, C., Fandino, J., Haller, C.S., and Osterwalder, J. (2013). Severe traumatic brain injury in a high-income country: an epidemiological study. J. Neurotrauma 30, 1934–1942 [DOI] [PubMed] [Google Scholar]
- 25. Boto, G.R., Gomez, P.A., De la Cruz, J., and Lobato, R.D. (2009). A historical analysis of severe head injury. Neurosurg. Rev. 32, 343–353 [DOI] [PubMed] [Google Scholar]
- 26. Vazquez-Barquero, A., Vazquez-Barquero, J.L., Austin, O., Pascual, J., Gaite, L., and Herrera, S. (1992). The epidemiology of head injury in Cantabria. Eur. J. Epidemiol. 8, 832–837 [DOI] [PubMed] [Google Scholar]
- 27. Perez, K., Novoa, A.M., Santamarina-Rubio, E., Narvaez, Y., Arrufat, V., Borrell, C., Cabeza, E., Cirera, E., Ferrando, J., Garcia-Altes, A., Gonzalez-Luque, J.C., Lizarbe, V., Martin-Cantera, C., Segui-Gomez, M., and Suelves, J.M. (2012). Incidence trends of traumatic spinal cord injury and traumatic brain injury in Spain, 2000–2009. Accid. Anal. Prev. 46, 37–44 [DOI] [PubMed] [Google Scholar]
- 28. Servadei, F., Bastianelli, S., Naccarato, G., Staffa, G., Morganti, G., and Gaist, G. (1985). Epidemiology and sequelae of head injury in San Marino Republic. J. Neurosurg. Sci. 29, 297–303 [PubMed] [Google Scholar]
- 29. Andelic, N., Sigurdardottir, S., Brunborg, C., and Roe, C. (2008). Incidence of hospital-treated traumatic brain injury in the Oslo population. Neuroepidemiology 30, 120–128 [DOI] [PubMed] [Google Scholar]
- 30. Servadei, F., Ciucci, G., Piazza, G., Bianchedi, G., Rebucci, G., Gaist, G., and Taggi, F. (1988). A prospective clinical and epidemiological study of head injuries in northern Italy: the Comune of Ravenna. Ital. J. Neurol. Sci. 9, 449–457 [DOI] [PubMed] [Google Scholar]
- 31. Steudel, W.I., Cortbus, F., and Schwerdtfeger, K. (2005). Epidemiology and prevention of fatal head injuries in Germany–trends and the impact of the reunification. Acta Neurochir. 147, 231–242 [DOI] [PubMed] [Google Scholar]
- 32. Mauritz, W., Brazinova, A., Majdan, M., and Leitgeb, J. (2014). Epidemiology of traumatic brain injury in Austria. Wien. Klin. Wochenschr. 126, 42–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rickels, E., von Wild, K., and Wenzlaff, P. (2010). Head injury in Germany: A population-based prospective study on epidemiology, causes, treatment and outcome of all degrees of head-injury severity in two distinct areas. Brain Inj. 24, 1491–1504 [DOI] [PubMed] [Google Scholar]
- 34. Styrke, J., Stalnacke, B.M., Sojka, P., and Bjornstig, U. (2007). Traumatic brain injuries in a well-defined population: epidemiological aspects and severity. J. Neurotrauma 24, 1425–1436 [DOI] [PubMed] [Google Scholar]
- 35. Frohlich, S., Johnson, P., and Moriarty, J. (2011). Prevalence, management and outcomes of traumatic brain injury patients admitted to an Irish intensive care unit. Ir. J. Med. Sci. 180, 423–427 [DOI] [PubMed] [Google Scholar]
- 36. Hawley, C., Wilson, J., Hickson, C., Mills, S., Ekeocha, S., and Sakr, M. (2013). Epidemiology of paediatric minor head injury: Comparison of injury characteristics with Indices of Multiple Deprivation. Injury 44, 1855–1861 [DOI] [PubMed] [Google Scholar]
- 37. Hawley, C.A., Ward, A.B., Long, J., Owen, D.W., and Magnay, A.R. (2003). Prevalence of traumatic brain injury amongst children admitted to hospital in one health district: a population-based study. Injury 34, 256–260 [DOI] [PubMed] [Google Scholar]
- 38. Danielle van Pelt, E., de Kloet, A., Hilberink, S.R., Lambregts, S.A., Peeters, E., Roebroeck, M.E., and Catsman-Berrevoets, C.E. (2011). The incidence of traumatic brain injury in young people in the catchment area of the University Hospital Rotterdam, The Netherlands. Eur. J. Paediatr. Neurol. 15, 519–526 [DOI] [PubMed] [Google Scholar]
- 39. Fabbri, A., Servadei, F., Marchesini, G., Negro, A., and Vandelli, A. (2010). The changing face of mild head injury: temporal trends and patterns in adolescents and adults from 1997 to 2008. Injury 41, 913–917 [DOI] [PubMed] [Google Scholar]
- 40. Summers, C.R., Ivins, B., and Schwab, K.A. (2009). Traumatic brain injury in the United States: an epidemiologic overview. Mt. Sinai J. Med. 76, 105–110 [DOI] [PubMed] [Google Scholar]
- 41. Coronado, V.G., Xu, L., Basavaraju, S.V., McGuire, L.C., Wald, M.M., Faul, M.D., Guzman, B.R., and Hemphill, J.D. (2011). Surveillance for traumatic brain injury-related deaths–United States, 1997–2007. MMWR Surveill. Summ. 60, 1–32 [PubMed] [Google Scholar]
- 42. Bruns, J. Jr. and Hauser, W.A. (2003). The epidemiology of traumatic brain injury: a review. Epilepsia 44 Suppl 10, 2–10 [DOI] [PubMed] [Google Scholar]
- 43. Feigin, V.L., Theadom, A., Barker-Collo, S., Starkey, N.J., McPherson, K., Kahan, M., Dowell, A., Brown, P., Parag, V., Kydd, R., Jones, K., Jones, A., and Ameratunga, S. (2013). Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 12, 53–64 [DOI] [PubMed] [Google Scholar]
- 44. Roozenbeek, B., Maas, A.I., and Menon, D.K. (2013). Changing patterns in the epidemiology of traumatic brain injury. Nat. Rev. Neurol. 9, 231–236 [DOI] [PubMed] [Google Scholar]
- 45. Rusnak, M., Janciak, I., Majdan, M., Wilbacher, I., and Mauritz, W. (2007). Severe traumatic brain injury in Austria VI: effects of guideline-based management. Wien. Klin. Wochenschr. 119, 64–71 [DOI] [PubMed] [Google Scholar]
- 46. Hartholt, K.A., Van Lieshout, E.M., Polinder, S., Panneman, M.J., Van der Cammen, T.J., and Patka, P. (2011). Rapid increase in hospitalizations resulting from fall-related traumatic head injury in older adults in The Netherlands 1986–2008. J. Neurotrauma 28, 739–744 [DOI] [PubMed] [Google Scholar]
- 47. Puljula, J., Makinen, E., Cygnel, H., Kortelainen, M.L., and Hillbom, M. (2013). Incidence of moderate-to-severe traumatic brain injuries after reduction in alcohol prices. Acta Neurol. Scand. 127, 192–197 [DOI] [PubMed] [Google Scholar]
- 48. Kannus, P., Palvanen, M., Niemi, S., Parkkari, J., Natri, A., Vuori, I., and Jarvinen, M. (1999). Increasing number and incidence of fall-induced severe head injuries in older adults: nationwide statistics in Finland in 1970–1995 and prediction for the future. Am. J. Epidemiol. 149, 143–150 [DOI] [PubMed] [Google Scholar]
- 49. Jennett, B. and MacMillan, R. (1981). Epidemiology of head injury. Br. Med. J. (Clin. Res. Ed.) 282, 101–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Engberg Aa, W. and Teasdale, T.W. (2001). Traumatic brain injury in Denmark 1979–1996. A national study of incidence and mortality. Eur. J. Epidemiol. 17, 437–442 [DOI] [PubMed] [Google Scholar]
- 51. Mauritz, W., Brazinova, A., Majdan, M., Rehorcikova, V., and Leitgeb, J. (2014). Deaths due to traumatic brain injury in Austria between 1980 and 2012. Brain Inj. 28, 1096–1101 [DOI] [PubMed] [Google Scholar]
- 52. Brazinova, A., Mauritz, W., Majdan, M., Rehorcikova, V., and Leitgeb, J. (2014). Fatal traumatic brain injury in older adults in Austria 1980–2012: an analysis of 33 years. Age Ageing 44, 502–506 [DOI] [PubMed] [Google Scholar]
- 53. Majdan, M., Mauritz, W., Rusnak, M., Brazinova, A., Rehorcikova, V., and Leitgeb, J. (2014). Long-term trends and patterns of fatal traumatic brain injuries in the pediatric and adolescent population of austria in 1980–2012: analysis of 33 years. J. Neurotrauma 31, 1046–1055 [DOI] [PubMed] [Google Scholar]
- 54. Williamson, L.M., Morrison, A., and Stone, D.H. (2002). Trends in head injury mortality among 0–14 year olds in Scotland (1986–95). J. Epidemiol. Community Health 56, 285–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sundstrom, T., Sollid, S., Wentzel-Larsen, T., and Wester, K. (2007). Head injury mortality in the Nordic countries. J. Neurotrauma 24, 147–153 [DOI] [PubMed] [Google Scholar]
- 56. Kleiven, S., Peloso, P.M., and von Holst, H. (2003). The epidemiology of head injuries in Sweden from 1987 to 2000. Inj. Control Saf. Promot. 10, 173–180 [DOI] [PubMed] [Google Scholar]
- 57. Alaranta, H., Koskinen, S., Leppanen, L., and Palomaki, H. (2000). Nationwide epidemiology of hospitalized patients with first-time traumatic brain injury with special reference to prevention. Wien. Med. Wochenschr. 150, 444–448 [PubMed] [Google Scholar]
- 58. Koskinen, S. and Alaranta, H. (2008). Traumatic brain injury in Finland 1991–2005: a nationwide register study of hospitalized and fatal TBI. Brain Inj. 22, 205–214 [DOI] [PubMed] [Google Scholar]
- 59. Dias, C., Rocha, J., Pereira, E., and Cerejo, A. (2014). Traumatic brain injury in Portugal: trends in hospital admissions from 2000 to 2010. Acta Med. Port. 27, 349–356 [DOI] [PubMed] [Google Scholar]
- 60. Andelic, N., Anke, A., Skandsen, T., Sigurdardottir, S., Sandhaug, M., Ader, T., and Roe, C. (2012). Incidence of hospital-admitted severe traumatic brain injury and in-hospital fatality in Norway: a national cohort study. Neuroepidemiology 38, 259–267 [DOI] [PubMed] [Google Scholar]
- 61. Scholten, A.C., Haagsma, J.A., Panneman, M.J., van Beeck, E.F., and Polinder, S. (2014). Traumatic brain injury in the Netherlands: incidence, costs and disability-adjusted life years. PLoS One 9, e110905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Winqvist, S., Lehtilahti, M., Jokelainen, J., Luukinen, H., and Hillbom, M. (2007). Traumatic brain injuries in children and young adults: a birth cohort study from northern Finland. Neuroepidemiology 29, 136–142 [DOI] [PubMed] [Google Scholar]
- 63. Berney, J., Favier, J., and Rilliet, B. (1995). Head injuries in children: a chronicle of a quarter of a century. Childs. Nerv. Syst. 11, 256–264 [DOI] [PubMed] [Google Scholar]
- 64. Berney, J., Favier, J., and Froidevaux, A.C. (1994). Paediatric head trauma: influence of age and sex. I. Epidemiology. Childs. Nerv. Syst. 10, 509–516 [DOI] [PubMed] [Google Scholar]
- 65. Nestvold, K., Lundar, T., Blikra, G., and Lonnum, A. (1988). Head injuries during one year in a central hospital in Norway: a prospective study. Epidemiologic features. Neuroepidemiology 7, 134–144 [DOI] [PubMed] [Google Scholar]
- 66. Edna, T.H. and Cappelen, J. (1984). Hospital admitted head injury. A prospective study in Trondelag, Norway, 1979–80. Scand. J. Soc. Med. 12, 7–14 [DOI] [PubMed] [Google Scholar]
- 67. Edna, T.H. and Cappelen, J. (1985). Head injury in road traffic accidents. A prospective Study in Trondelag, Norway, 1979–80. Scand. J. Soc. Med. 13, 23–27 [DOI] [PubMed] [Google Scholar]
- 68. Lopez Alvarez, J.M., Valeron Lemaur, M.E., Perez Quevedo, O., Liminana Canal, J.M., Jimenez Bravo de Laguna, A., Consuegra Llapurt, E., Moron Saen de Casas, A., and Gonzalez Jorge, R. (2011). [Severe pediatric head injuries (I). Epidemiology, clinical manifestations and course]. Med. Intensiva 35, 331–336 [DOI] [PubMed] [Google Scholar]
- 69. Johansson, E., Ronnkvist, M., and Fugl-Meyer, A.R. (1991). Traumatic brain injury in northern Sweden. Incidence and prevalence of long-standing impairments and disabilities. Scand. J. Rehabil. Med. 23, 179–185 [PubMed] [Google Scholar]
- 70. Tiret, L., Hausherr, E., Thicoipe, M., Garros, B., Maurette, P., Castel, J.P., and Hatton, F. (1990). The epidemiology of head trauma in Aquitaine (France), 1986: a community-based study of hospital admissions and deaths. Int. J. Epidemiol. 19, 133–140 [DOI] [PubMed] [Google Scholar]
- 71. Emanuelson, I. and v Wendt, L. (1997). Epidemiology of traumatic brain injury in children and adolescents in south-western Sweden. Acta Paediatr. 86, 730–735 [DOI] [PubMed] [Google Scholar]
- 72. Arnarson, E.O. and Halldorsson, J.G. (1995). Head trauma among children in Reykjavik. Acta Paediatr. 84, 96–99 [DOI] [PubMed] [Google Scholar]
- 73. Bouillon, B., Raum, M., Fach, H., Buchheister, B., Lefering, R., Menzel, J., and Klug, N. (1999). The incidence and outcome of severe brain trauma - Design and first results of an epidemiological study in an urban area. Restor. Neurol. Neurosci. 14, 85–92 [PubMed] [Google Scholar]
- 74. Maegele, M., Engel, D., Bouillon, B., Lefering, R., Fach, H., Raum, M., Buchheister, B., Schaefer, U., Klug, N., and Neugebauer, E. (2007). Incidence and outcome of traumatic brain injury in an urban area in Western Europe over 10 years. Eur. Surg. Res. 39, 372–379 [DOI] [PubMed] [Google Scholar]
- 75. Andersson, E.H., Bjorklund, R., Emanuelson, I., and Stalhammar, D. (2003). Epidemiology of traumatic brain injury: a population based study in western Sweden. Acta Neurol. Scand. 107, 256–259 [DOI] [PubMed] [Google Scholar]
- 76. Ingebrigtsen, T., Mortensen, K., and Romner, B. (1998). The epidemiology of hospital-referred head injury in northern Norway. Neuroepidemiology 17, 139–146 [DOI] [PubMed] [Google Scholar]
- 77. Javouhey, E., Guerin, A.C., and Chiron, M. (2006). Incidence and risk factors of severe traumatic brain injury resulting from road accidents: a population-based study. Accid. Anal. Prev. 38, 225–233 [DOI] [PubMed] [Google Scholar]
- 78. Baldo, V., Marcolongo, A., Floreani, A., Majori, S., Cristofolettil, M., Dal Zotto, A., Vazzoler, G., and Trivello, R. (2003). Epidemiological aspect of traumatic brain injury in Northeast Italy. Eur. J. Epidemiol. 18, 1059–1063 [DOI] [PubMed] [Google Scholar]
- 79. Masson, F., Thicoipe, M., Aye, P., Mokni, T., Senjean, P., Schmitt, V., Dessalles, P.H., Cazaugade, M., and Labadens, P. (2001). Epidemiology of severe brain injuries: a prospective population-based study. J. Trauma 51, 481–489 [DOI] [PubMed] [Google Scholar]
- 80. Servadei, F., Antonelli, V., Betti, L., Chieregato, A., Fainardi, E., Gardini, E., Giuliani, G., Salizzato, L., and Kraus, J.F. (2002). Regional brain injury epidemiology as the basis for planning brain injury treatment. The Romagna (Italy) experience. J. Neurosurg. Sci. 46, 111–119 [PubMed] [Google Scholar]
- 81. Di Bartolomeo, S., Sanson, G., Nardi, G., Scian, F., Michelutto, V., and Lattuada, L. (2001). Effects of 2 patterns of prehospital care on the outcome of patients with severe head injury. Arch. Surg. 136, 1293–1300 [DOI] [PubMed] [Google Scholar]
- 82. Servadei, F., Verlicchi, A., Soldano, F., Zanotti, B., and Piffer, S. (2002). Descriptive epidemiology of head injury in Romagna and Trentino. Comparison between two geographically different Italian regions. Neuroepidemiology 21, 297–304 [DOI] [PubMed] [Google Scholar]
- 83. Dahl, E., von Wendt, L., and Emanuelson, I. (2006). A prospective, population-based, follow-up study of mild traumatic brain injury in children. Injury 37, 402–409 [DOI] [PubMed] [Google Scholar]
- 84. Ventsel, G., Kolk, A., Talvik, I., Vali, M., Vaikmaa, M., and Talvik, T. (2008). The incidence of childhood traumatic brain injury in Tartu and Tartu County in Estonia. Neuroepidemiology 30, 20–24 [DOI] [PubMed] [Google Scholar]
- 85. Rosso, A., Brazinova, A., Janciak, I., Wilbacher, I., Rusnak, M., and Mauritz, W. (2007). Severe traumatic brain injury in Austria II: epidemiology of hospital admissions. Wien. Klin. Wochenschr. 119, 29–34 [DOI] [PubMed] [Google Scholar]
- 86. Mauritz, W., Wilbacher, I., Majdan, M., Leitgeb, J., Janciak, I., Brazinova, A., and Rusnak, M. (2008). Epidemiology, treatment and outcome of patients after severe traumatic brain injury in European regions with different economic status. Eur. J. Public Health 18, 575–580 [DOI] [PubMed] [Google Scholar]
- 87. Numminen, H.J. (2011). The incidence of traumatic brain injury in an adult population–how to classify mild cases? Eur. J. Neurol. 18, 460–464 [DOI] [PubMed] [Google Scholar]
- 88. Falk, A.C., Klang, B., Paavonen, E.J., and von Wendt, L. (2007). Current incidence and management of children with traumatic head injuries: the Stockholm experience. Dev. Neurorehabil. 10, 49–55 [DOI] [PubMed] [Google Scholar]
- 89. Heskestad, B., Baardsen, R., Helseth, E., Romner, B., Waterloo, K., and Ingebrigtsen, T. (2009). Incidence of hospital referred head injuries in Norway: a population based survey from the Stavanger region. Scand. J. Trauma Resusc. Emerg. Med. 17, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Andriessen, T.M., Horn, J., Franschman, G., van der Naalt, J., Haitsma, I., Jacobs, B., Steyerberg, E.W., and Vos, P.E. (2011). Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: a prospective multicenter study. J. Neurotrauma 28, 2019–2031 [DOI] [PubMed] [Google Scholar]
- 91. Roe, C., Skandsen, T., Anke, A., Ader, T., Vik, A., Lund, S.B., Mannskow, U., Sollid, S., Sundstrom, T., Hestnes, M., and Andelic, N. (2013). Severe traumatic brain injury in Norway: impact of age on outcome. J. Rehabil. Med. 45, 734–740 [DOI] [PubMed] [Google Scholar]
- 92. Katsaragakis, S., Drimousis, P.G., Toutouzas, K., Stefanatou, M., Larentzakis, A., Theodoraki, M.E., Stergiopoulos, S., and Theodorou, D. (2010). Traumatic brain injury in Greece: report of a countrywide registry. Brain Inj. 24, 871–876 [DOI] [PubMed] [Google Scholar]
- 93. Foulkes, M.A., Eisenberg, H.M., Jane, J.A., Marmarou, A., and Marshall, L.F. (1991). The Traumatic Coma Data Bank: Design, methods, and baseline characteristics. J. Neurosurg. 75 Suppl 1, 8–13 [Google Scholar]