Abstract
Background.
Strategies to reduce anxiety prior to injection procedures are not well understood. The purpose is to determine the effect of a meditation monologue intervention delivered via phone/mobile application on pre-injection anxiety levels among patients undergoing a clinical injection. The following hypothesis was tested: patients who listened to a meditation monologue via phone/mobile application prior to clinical injection would experience less anxiety compared to those who did not.
Methods.
A prospective, randomized controlled trial was performed at an orthopedics and sports medicine clinic of a tertiary level medical center in the New England region, USA. Thirty patients scheduled for intra- or peri-articular injections were randomly allocated to intervention (meditation monologue) or placebo (nature sounds) group. Main outcome variables were state and trait anxiety inventory (STAI) scores and blood pressure (BP), heart rate, and respiratory rate.
Results.
There were 16 participants who were allocated to intervention (meditation monologue) while 14 participants were assigned to placebo (nature sounds). There was no interaction effect. However, a main time effect was found. Both state anxiety (STAI-S) and trait anxiety (STAI-T) scores were significantly reduced post-intervention compared to pre-intervention (STAI-S: p = 0.04, STAI-T: p = 0.04). Also, a statistically significant main group effect was detected. The pre- and post- STAI-S score reduction was greater in the intervention group (p = 0.028). Also, a significant diastolic BP increase between pre- and post-intervention was recorded in the intervention group (p = 0.028), but not in the placebo group (p = 0.999).
Conclusion.
Listening to a meditation monologue via phone/mobile application prior to clinical injection can reduce anxiety in adult patients receiving intra- and peri-articular injections. Registration: ClinicalTrials.gov NCT02690194
Keywords: relaxation, mental status, clinical injection
What Is Known About the Issue
Δ Music is helpful to reduce anxiety for pre-surgical patients.
What This Study Adds to Existing Knowledge
Δ Listening to a meditation monologue through phone/mobile application prior to clinical injection can reduce anxiety level in adult patients receiving intra- and peri-articular injection.
Introduction
Injections, both intra-1–5 and extra-articular,6–8 are commonly administered in orthopedic and sports medicine clinics mainly for diagnostic evaluation9–11 and pain relief12–14 purposes. Corticosteroids and platelet rich plasma injections have been shown to decrease pain related to certain orthopedic conditions.15–17 Although injections may be useful for alleviating pain,15,16,18,19 they are often accompanied by anxiety.20–22 In an effort to reduce anxiety, a variety of relaxation techniques have been described, including visualization of positive images,23,24 distraction from clinical procedures,25–27 and alteration of breathing patterns.28,29 Recent studies also suggest that breathing techniques based on yoga practices substantially reduce anxiety levels.30–32 Additionally, listening to music prior to various medical procedures has been found to be effective in anxiety reduction.33,34
In the last 5-years, clinical interventions administered through a phone/mobile applications have increased substantially.35 According to a recent PubMed search, there were fewer than 100 publications related to phone/mobile applications prior to 2013, and over 300 investigations related to phone/mobile applications published between 2018 and 2019.35 One of the phone/mobile applications designed to reduce anxiety that we found was Buddhify (Mindfulness Everywhere Ltd, Glasgow, UK). According to the website,36 Buddhify was designed based on an urban meditation monologue to facilitate mindfulness in daily life and to help manage stress. We hypothesized that this application could be utilized in the clinical setting to reduce anxiety. Despite an extensive literature search, we were unable to find published studies on the use of this type of application-based meditation program in the orthopedic or sports medicine setting. The purpose of this study was to determine the effect of a meditation monologue delivered via phone/mobile application on pre-injection anxiety levels in patients receiving injections in an orthopaedics and sports medicine clinic. Our hypothesis was that patients who listened to the meditation monologue prior to the procedure would experience less anxiety, compared to those who did not.
Methods
Study Design
We conducted a prospective randomized controlled trial at an orthopaedics and sports medicine clinic of a regional tertiary level academic medical center located in the New England region of the United States. The study duration was from June 2015 to January 2017. A study ethical approval form was developed based on the Declaration of Helsinki and ethical standards in sport and exercise science research.37 The study was approved by our institutional review board (IRB-P-00016464) and was registered under the ClinicalTrials.gov (NCT02690194).
Participants
We recruited adult patients who visited our clinic to receive injections. The inclusion criteria were i) patients aged 21 years or older and ii) seeking intra- or extra-articular injections. The exclusion criteria were i) patients under 21 years of age, ii) taking medications to manage mental/psychiatric conditions, and iii) using the Buddhify phone/mobile application intervention regularly. These exclusion criteria were selected to avoid teh potential confounding effect on the study purpose and hypothesis.
Interventions
This study utilized a true intervention (Buddhify meditation monologue) and a placebo intervention (recorded nature sounds). The Buddhify phone/mobile application offers multiple modules and recordings. For the purpose of this study, the “feeling stressed” module was selected from the “stress and difficult emotion 1” section. This specific module involves a 5-minute guided meditation monologue, which encourages relaxation and offers instruction on breathing techniques. Sounds of birds chirping, moving water, and breezes are also included. The true intervention (Buddhify meditation monologue) was chosen to examine how a meditation monologue would affect anxiety levels before and after clinical injection (within comparison) in the setting of an orthopedic and sports medicine clinic. For comparison, a placebo intervention (nature sounds) was incorporated, in order to helps minimize potential bias such as the Hawthorne effect.38
Procedures
After obtaining consent, demographic data, and physiological measures including blood pressure (BP), heart rate, and respiratory rate were collected. Additional questions were asked related to history of prior injection aas well as recent (within the last hour) oral intake and physical activity. Following this initial data collection, anxiety levels were measured through the state and trait anxiety inventory (STAI) questionnaire. The STAI was developed by Spielberger et al.39 and consists of state anxiety (STAI-S) and trait anxiety (STAI-T).39 The STAI-S was designed to assess how one feels right now, at this moment while the STAI-T was developed to evaluate how one generally feels.39 The STAI-S and STAI-T consist of 20 questions each.39
Once both STAI-S- and STAI-T scores were obtained, randomization was performed. Randomization to either the true intervention (Buddhify meditation monologue) or the placebo intervention (nature sounds recording), was determined by a random number generator, and the allocation was concealed. Participants were blinded from status of randomization, and an intention to treat protocol40 was employed. Based on the result of the randomization, each participant received a 5 minute intervention, either the Buddhify (true intervention) or the nature sounds recording (placebo), via headphones. Following the allocated intervention, physiological measurements and the STAI-S and STAI-T were collected, using the same method as pre-intervention. Once the steps above were completed, participants received their clinical injections.
Main Outcome Measures
The primary outcome variable in the current study was STAI-S scores. The STAI-S was selected because it measures how one feels at that moment, and our aim was to test the hypothesis that the meditation monologue intervention would reduce anxiety immediately. The STAI-T was treated as a secondary outcome variable because it is a measure of how one generally feels. Tertiary outcome variables were physiological measures including systolic BP, diastolic BP, heart rate, and respiratory rate. All analyses were performed by an investigator who was blinded from the group randomization assignment.
Statistical Analysis
First, patients’ demographic data were compared by a descriptive statistics including mean and standard deviation values. An independent t-test was used when the values were normally distributed. Mann Whitney U test was used for non-normal data. All variables that appeared different between the 2 groups with a significant level of p < 0.20 were considered as covariates. The covariates were entered in the repeated analysis of covariance (ANCOVA) model. Interaction between time (pre, post) and groups (Buddhify, placebo), main effect of time (pre, post) and group (Buddhify, placebo) were examined. When a main group effect was found, a pairwise comparison was performed between Buddhify and placebo. Statistical significance of p < 0.05 was used for interaction, main time effect, main group effect, and pairwise comparison. All analyses were performed by SPSS software (IBM, Version 23.0, Chicago, IL, USA).
Results
We enrolled 30 patients including 21 females and 9 males. Sixteen participants were allocated to the intervention group (Buddhify meditation monologue) and 14 participants were assigned to the placebo group (nature sounds). There were no drop-outs in the current study. Participants’ characteristics including demographics, physiological parameters (BP, heart rate, and respiratory rate), oral intake in last hour, exercise status in last hour, and previous injection history were listed in Table 1. Baseline values of heart rate, respiratory rate, and exercises in the last hour were significantly different between the 2 groups (Table 1) and met our a priori criteria for covariates (Table 1); therefore, they were treated as covariates and were included in the repeated ANCOVA model.
Table 1.
Patient Characteristics.
| Group | Buddhify (N = 16) | Placebo (N = 14) | P-value |
|---|---|---|---|
| Demographics | |||
| Age | 50.9 ± 18.0 | 53.9 ± 15.8 | .625 |
| Sex | |||
| Female | 10 (62.5%) | 11 (78.6%) | |
| Male | 6 (37.5%) | 3 (21.4%) | |
| (x2) test | .338 | ||
| Physiological measures | |||
| Blood Pressure | |||
| BP—Systolic | 121.9 ± 17.5 | 121.9 ± 9.5 | .992 |
| BP—Diastolic | 77.2 ± 10.8 | 78.9 ± 8.1 | .639 |
| Cardiovascular: | |||
| Heart Rate | 75.6 ± 14.3 | 66.4 ± 14.4 | .093* |
| Respiration Rate | 16.1 ± 3.0 | 14.0 ± 2.1 | .030* |
| Oral intake | |||
| Drink in last hr: | |||
| No | 8 (50.0%) | 4 (28.6%) | |
| Yes | 8 (50.0%) | 10 (71.4%) | |
| (x2) test | .232 | ||
| Food in last hr: | |||
| No | 13 (81.3%) | 11 (78.6%) | |
| Yes | 3 (18.7%) | 3 (21.4%) | |
| (x2) test | .855 | ||
| Physical activity | |||
| Exercise in last hr: | |||
| No | 16 (100%) | 9 (64.3%) | |
| Yes | 0 (0%) | 5 (35.7%) | |
| (x2) test | .009* | ||
| Previous injection history | |||
| Previous injection | |||
| No | 5 (33.3%) | 5 (35.7%) | |
| Yes | 10 (66.7%) | 9 (64.3%) | |
| (x2) test | .893 | ||
| Number of previous injections | 5.8 ± 8.9 | 5.2 ± 3.4 | .857 |
There were no interactions between the 2 groups (intervention and placebo groups) in the 2 time points (pre- and post-interventions) in STAI-S (p = 0.555), STAI-T (p = 0.077), and physiological measures, including systolic BP (p = 0.402), diastolic BP (p = 0.070), heart rate (p = 0.471), and respiratory rate (p = 0.450). However, a statistically significant main effect of time was found in STAI-S and STAI-T. Both STAI-S and STAI-T scores were significantly reduced post-intervention compared to pre-intervention (STAI-S: p = 0.04, Figure 1; STAI-T: p = 0.04, Figure 2). There were no time effects on the rest of the variables (systolic BP: p = 0.495, Figure 3; diastolic BP: p = 0.074, Figure 4; heart rate: p = 0.569, Figure 5; respiratory rate: p = 0.083, Figure 6). A statistically significant main effect of groups was detected in STAI-S (p = 0.041), but not in the rest of the outcome variables (STAI-T: p = 0.404, systolic BP: p = 0.402, diastolic BP: p = 0.070, heart rate: p = 0.573, and respiratory rate: p = 0.280). Pairwise comparison indicated significant STAI-S score reduction between pre- and post-intervention in the intervention group (p = 0.028, Figure 1), but not in the placebo group (p = 0.070, Figure 1). Also, although a main group effect was not noted in diastolic BP (p = 0.070), a statistically significant diastolic BP increase between pre- and post-intervention was recorded in the intervention group (p = 0.028, Figure 4); however, this was not noted in the placebo group (p = 0.999).
Figure 1.
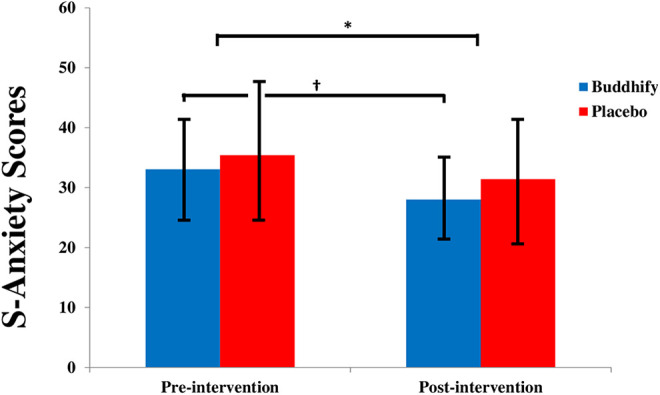
Pre- and post-S-Anxiety scores between intervention (meditation monologue) and placebo (nature sounds).
Figure 2.
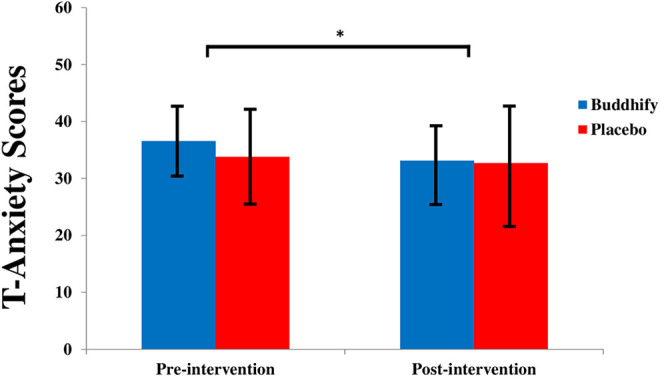
Pre- and post-T-Anxiety scores between intervention (meditation monologue) and placebo (nature sounds).
Figure 3.
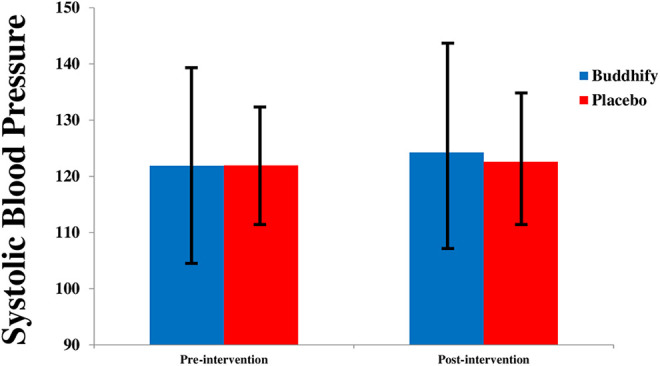
Pre- and post-systolic BP between intervention (meditation monologue) and placebo (nature sounds).
Figure 4.
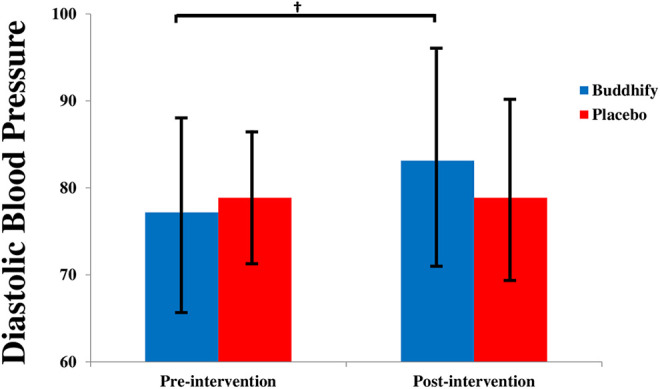
Pre- and post-diastolic BP between intervention (meditation monologue) and placebo (nature sounds).
Figure 5.
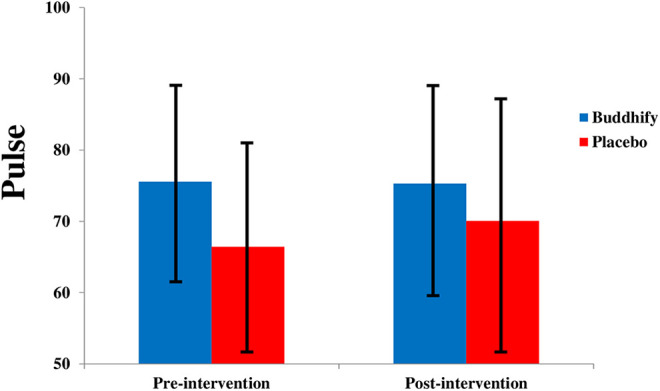
Pre- and post-heart rate between intervention (meditation monologue) and placebo (nature sounds).
Figure 6.
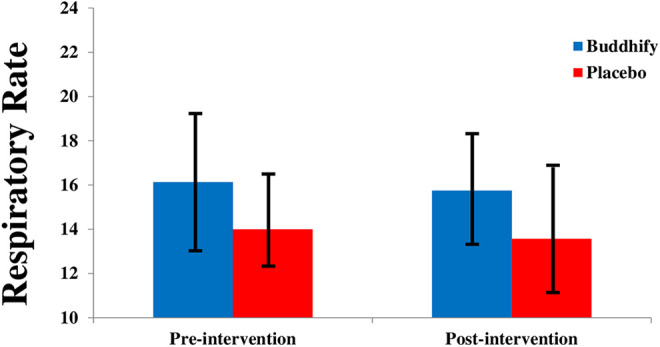
Pre- and post-respiratory rate between intervention (meditation monologue) and placebo (nature sounds).
Discussion
Our hypothesis was that patients who used phone/mobile application of the meditation monologue before clinical injection would demonstrate less anxiety compared to those who did not use meditation monologue phone/mobile application. Our results indicate that the post-STAI-S scores were significantly reduced compared to pre-STAI-S scores after the meditation monologue intervention (Figure 1). These findings support our hypothesis that the meditation monologue may reduce anxiety prior to orthopedic injections. It is interesting to note that our secondary outcome variable, STAI-T, also showed reductions between pre-and post-intervention regardless of the intervention (Buddhify meditation monologue) or placebo (nature sounds). In fact, there were no intervention specific differences on STAI-T reduction between the intervention and placebo groups. We used a nature sound recording as a placebo in this study, and the results suggest that nature sounds alone may be as effective as a meditation monologue in reducing general anxiety (STAI-T). In short, the current study findings suggest that anxiety at that moment (STAI-S) can be reduced by listening to a meditation monologue, and general anxiety (STAI-T) can be reduced by listening to either a meditation monologue or natural sounds prior to clinical injection. The clinical relevance of this study is that a brief (5-minute) intervention involving a cost-effective, easily administered meditation monologue, can effectively reduce pre-injection anxiety in patients.
The current study results were largely supported by past findings. Previous studies have investigated the effects of music interventions. For example, Lieber et al. reviewed 12 studies and evaluated the effect of music interventions on anxiety levels among angiography patients.33 They concluded that there was a significant STAI reduction (2.81 points, p = 0.004) among angiography patients who listened to music compared to those who did not.33 Furthermore, Jayakar and Alter performed a meta-analysis of 15 studies that used music interventions in patients who received cardiac catheterization.34 The results found significant STAI-S reduction (3.95 points, p < 0.005) following a music intervention compared to patients who did not listen to music.34 In the current study, the STAI-S reduction in patients who received the Buddhify meditation monologue was 5.06 points compared to a 4.00 point reduction in those patients who received the nature sounds. The greater STAI-S reduction observed among patients who listened to either the meditation monologue or the nature sound recording might be due to differences in thepatient populations. In this study, patients were awaiting intra- or peri-articular injection, rather than the angiography and cardiac catheterization procedures described in the other studies. 33,34 The nature of the procedure likely impacts the level of effect of the intervention, therefore, the differences in severity and risk involved in these various procedures may help explain the magnitude of the intervention effect; lower levels of distress among our patients might result in a greater STAI-S reduction than observed in the Lieber and Jayakar studies.33,34
One unexpected finding was a diastolic BP increase between the pre- and post-intervention measurements in the Buddhify group (Figure 4). Physiological outcomes were added as tertiary variables to understand potential reactive responses of our intervention in addition to anxiety levels. We hypothesized that BP would be reduced following the meditation monologue intervention. This notion was developed because a study conducted by Ifeagwazi et al. found that BP increases were linearly correlated with anxiety.41 Therefore, we conceptualized that BP would decrease following the intervention, especially if the meditation monologue was shown to reduce anxiety. Additionally, a randomized controlled trial performed by Wiwatwongwana et al. compared 2 different types of music interventions (plain music and binaural beat music) with a control group on anxiety levels in patients who underwent phacoemulsification under local anesthesia.42 In this study, significant STAI-S reductions between pre- and post-interventions (plain music, 7.0 points, p < 0.001; binaural beat music, 9.0 points, p < 0.001) were recorded.42 Along with the STAI-S reductions, systolic BP decreases were also noted (plain music, −3.3 mmHG; binaural beat music, −3.2 mmHG).42 However, diastolic BP increases were actually documented (plain music, 2.5 mmHG; binaural beat music, 0.7 mmHG).42 The diastolic BP increase observed in the current study was 5.94 mmHG, which is much greater than the study conducted by Wiwatwongwana et al.42 Future studies are warranted to investigate the physiological mechanisms related to anxiety, particularly BP change mechanisms.
Limitation
This study has several limitations. Sample size was relatively small. However, the a priori power analysis demonstrated a minimum number of 15 per group when the pre-and post-differences of the primary outcome variable (STAI-S) was greater than 6 with α = 0.05 and β = 0.80. Additionally, our patients were older than what we initially expected. Mean ages of each group, the intervention and placebo, were 50.9 and 53.9 years. Hence, the current findings may not be applicable to children, adolescents, and young adults. Moreover, the current study did not incorporate biological data which might have been used to better understand the underlying mechanisms of injection-related anxiety reduction. Finally, while we asked mental/psychiatric conditions, the responses were self-reported, and not confirmed by medical records or independent professional evaluation.
Conclusion
Despite the limitations, our study suggests that use of a brief meditation monologue prior to injection can reduce anxiety in the moment prior to intra- and peri-articular injection in adult patients. Also, both meditation monologues and nature sounds can decrease general anxiety before the clinical injection. Diastolic BP, however, showed an increase with use of the meditation monologue. At this point, specific physiological mechanisms that led to the diastolic BP increase are not well understood. Future studies are warranted to examine potential physiological mechanisms related to changes in anxiety levels.
Acknowledgments
The authors genuinely appreciate to a research team of division of Sports Medicine, Boston Children’s Hospital.
Authors’ Note: IRB-P00016464 Boston Children’s Hospital—institutional review board. Dai Sugimoto: study design development, data analysis and interpretation, manuscript writing; Nathalie R. Slick: data collection, data organization, and manuscript draft; David L. Mendel: data collection, data organization, and manuscript draft; Cynthia J. Stein: data collection, manuscript draft; Emily Pluhar: data collection, data interpretation, manuscript draft; Joana L. Fraser: data interpretation, manuscript draft; William P. Meehan III: study (trial) consultant, data analysis, and manuscript draft; Gianmichel D. Corrado: original concept dissemination, data interpretation, manuscript draft and final approval.
Declaration of Conflicting Interests: All authors have no conflicting of interests in this study. However, one of the authors, Dr. William P. Meehan III, discloses the following information to keep himself transparent: ABC-Cliopublishing for the sale of the books Kids, Sports and Concussion a Guide for Coaches and Parents, and Concussions; Springer International for the book Head and Neck Injuries in Young Athletes; Wolters Kluwer for working as an author for UpToDate; My research is funded, in part, by philanthropic support from the National Hockey League Alumni Association through the Corey C Griffin Pro-Am tournament and a grant from the National Football League. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. Peer reviewers on this manuscript have no relevant financial relationships to disclose.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Dai Sugimoto, PhD, ATC  https://orcid.org/0000-0001-6858-4434
https://orcid.org/0000-0001-6858-4434
References
- 1. Anderson CN. Iliopsoas: pathology, diagnosis, and treatment. Clin Sports Med. 2016;35(3):419–433. [DOI] [PubMed] [Google Scholar]
- 2. Agten CA, Rosskopf AB, Zingg PO, Peterson CK, Pfirrmann CW. Outcomes after fluoroscopy-guided iliopsoas bursa injection for suspected iliopsoas tendinopathy. Eur Radiol. 2015;25(3):865–871. [DOI] [PubMed] [Google Scholar]
- 3. Contreras ME, Dani WS, Endges WK, De Araujo LC, Berral FJ. Arthroscopic treatment of the snapping iliopsoas tendon through the central compartment of the hip: a pilot study. J Bon Joint Surg Br. 2010;92(6):777–780. [DOI] [PubMed] [Google Scholar]
- 4. Flanum ME, Keene JS, Blankenbaker DG, Desmet AA. Arthroscopic treatment of the painful “internal” snapping hip: results of a new endoscopic technique and imaging protocol. Am J Sports Med. 2007;35(5):770–779. [DOI] [PubMed] [Google Scholar]
- 5. Kroger EW, Griesser MJ, Kolovich GP, Ellis TJ. Efficacy of surgery for internal snapping hip. Int J Sports Med. 2013;34(10):851–855. [DOI] [PubMed] [Google Scholar]
- 6. Jacobson JA, Bedi A, Sekiya JK, Blankenbaker DG. Evaluation of the painful athletic hip: imaging options and imaging-guided injections. AJR Am J Roentgenol. 2012;199(3):516–524. [DOI] [PubMed] [Google Scholar]
- 7. Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36(12):2363–2371. [DOI] [PubMed] [Google Scholar]
- 8. Kivlan BR, Martin RL, Sekiya JK. Response to diagnostic injection in patients with femoroacetabular impingement, labral tears, chondral lesions, and extra-articular pathology. Arthroscopy. 2011;27(5):619–627. [DOI] [PubMed] [Google Scholar]
- 9. Adler RS, Buly R, Ambrose R, Sculco T. Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am J Roentgenol. 2005;185(4):940–943. [DOI] [PubMed] [Google Scholar]
- 10. Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35(8):565–571. [DOI] [PubMed] [Google Scholar]
- 11. Wilson MD, Keene JS. Treatment of ischiofemoral impingement: results of diagnostic injections and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg. 2016;3(2):146–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Araujo JP, Silva L, Andrade R, et al. Pain reduction and improvement of function following ultrasound-guided intra-articular injections of triamcinolone hexacetonide and hyaluronic acid in hip osteoarthritis. J Biol Regul Homeost Agent. 2016;30(4 Suppl 1):51–62. [PubMed] [Google Scholar]
- 13. Petterson SC, Plancher KD. Single intra-articular injection of lightly cross-linked hyaluronic acid reduces knee pain in symptomatic knee osteoarthritis: a multicenter, double-blind, randomized, placebo-controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1992–2002. [DOI] [PubMed] [Google Scholar]
- 14. van Middelkoop M, Arden NK, Atchia I, et al. The OA Trial Bank: meta-analysis of individual patient data from knee and hip osteoarthritis trials show that patients with severe pain exhibit greater benefit from intra-articular glucocorticoids. Osteoarthritis Cartilage. 2016;24(7):1143–1152. [DOI] [PubMed] [Google Scholar]
- 15. Hechtman KS, Uribe JW, Botto-vanDemden A, Kiebzak GM. Platelet-rich plasma injection reduces pain in patients with recalcitrant epicondylitis. Orthopedics. 2011;34(2):92. [DOI] [PubMed] [Google Scholar]
- 16. Han JS, Sugimoto D, McKee-Proctor MH, Stracciolini A, d’Hemecourt PA. Short-term effect of ultrasound-guided iliopsoas peritendinous corticosteroid injection. J Ultrasound Med. 2019;38(6):1527–1536. [DOI] [PubMed] [Google Scholar]
- 17. Ranalletta M, Rossi LA, Bongiovanni SL, Tanoira I, Elizondo CM, Maignon GD. Corticosteroid injections accelerate pain relief and recovery of function compared with oral NSAIDs in patients with adhesive capsulitis: a randomized controlled trial. Am J Sports Med. 2016;44(2):474–481. [DOI] [PubMed] [Google Scholar]
- 18. Conaghan PG, Hunter DJ, Cohen SB, et al. Effects of a single intra-articular injection of a microsphere formulation of triamcinolone acetonide on knee osteoarthritis pain: a double-blinded, randomized, placebo-controlled, multinational study. J Bone Joint Surg Am. 2018;100(8):666–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cushman D, Teramoto M, Curtis B, Lee DT, Marcolina A, McCormick Z. Does trainee involvement in fluoroscopic injections affect fluoroscopic time, immediate pain reduction, and Complication rate? PM R. 2017;9(10):1013–1019. [DOI] [PubMed] [Google Scholar]
- 20. Noble LM, Farquharson L, O’Dwyer NA, Behrens RH. The impact of injection anxiety on education of travelers about common travel risks. J Travel Med. 2014;21(2):86–91. [DOI] [PubMed] [Google Scholar]
- 21. Nelson CJ, Hsiao W, Balk E, et al. Injection anxiety and pain in men using intracavernosal injection therapy after radical pelvic surgery. J Sex Med. 2013;10(10):2559–2565. [DOI] [PubMed] [Google Scholar]
- 22. Celik N, Khorshid L. The use of shotblocker for reducing the pain and anxiety associated with intramuscular injection: a randomized, Placebo controlled study. Holist Nurs Pract. 2015;29(5):261–271. [DOI] [PubMed] [Google Scholar]
- 23. Norgaard MW, Pedersen PU, Bjerrum M. Understanding how patients use visualization during ablation of atrial fibrillation in reducing their experience of pain, anxiety, consumption of pain medication and procedure length: integrating quantitative and qualitative results. Appl Nurs Res. 2018;39:229–240. [DOI] [PubMed] [Google Scholar]
- 24. Padrino-Barrios C, McCombs G, Diawara N, De Leo G. The use of immersive visualization for the control of dental anxiety during oral debridement. J Dent Hyg. 2015;89(6):372–377. [PubMed] [Google Scholar]
- 25. Gezginci E, Iyigun E, Kibar Y, Bedir S. Three distraction methods for pain reduction during cystoscopy: a randomized controlled trial evaluating the effects on pain, anxiety, and satisfaction. J Endourol. 2018;32(11):1078–1084. [DOI] [PubMed] [Google Scholar]
- 26. Millett CR, Gooding LF. Comparing active and passive distraction-based music therapy interventions on preoperative anxiety in pediatric patients and their caregivers. J Music Ther. 2018;54(4):460–478. [DOI] [PubMed] [Google Scholar]
- 27. Debs NN, Aboujaoude S. Effectiveness of intellectual distraction on gagging and anxiety management in children: a prospective clinical study. J Int Soc Prev Community Dent. 2017;7(6):315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen YF, Huang XY, Chien CH, Cheng JF. The effectiveness of diaphragmatic breathing relaxation training for reducing anxiety. Perspect Psychiatr Care. 2017;53(4):329–336. [DOI] [PubMed] [Google Scholar]
- 29. Nunna M, Dasaraju RK, Kamatham R, Mallineni SK, Nuvvula S. Comparative evaluation of virtual reality distraction and counter-stimulation on dental anxiety and pain perception in children. J Dent Anesth Pain Med. 2019;19(5):277–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tiwari N, Sutton M, Garner M, Baldwin DS. Yogic breathing instruction in patients with treatment-resistant generalized anxiety disorder: pilot study. Int J Yoga. 2019;12(1):78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kuloor A, Kumari S, Metri K. Impact of yoga on psychopathologies and quality of life in persons with HIV: a randomized controlled study. J Bodyw Move Ther. 2019;23(2):278–283. [DOI] [PubMed] [Google Scholar]
- 32. Doria S, de Vuono A, Sanlorenzo R, Irtelli F, Mencacci C. Anti-anxiety efficacy of Sudarshan Kriya yoga in general anxiety disorder: a multicomponent, yoga based, breath intervention program for patients suffering from generalized anxiety disorder with or without comorbidities. J Affect Disord. 2015;184:310–317. [DOI] [PubMed] [Google Scholar]
- 33. Lieber AC, Bose J, Zhang X, et al. Effects of music therapy on anxiety and physiologic parameters in angiography: a systematic review and meta-analysis. J Neurointerv Surg. 2019;11(4):416–423. [DOI] [PubMed] [Google Scholar]
- 34. Jayakar JP, Alter DA. Music for anxiety reduction in patients undergoing cardiac catheterization: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2017;28:122–130. [DOI] [PubMed] [Google Scholar]
- 35. Proffen BL, Perrone GS, Fleming BC, et al. Electron beam sterilization does not have a detrimental effect on the ability of extracellular matrix scaffolds to support in vivo ligament healing. J Orthop Res. 2015;33(7):1015–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Buckley PS, Bishop M, Kane P, et al. Early single-sport specialization: a survey of 3090 high school, collegiate, and professional athletes. Orthop J Sports Med. 2017;5(7):2325967117703944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Harriss DJ, Atkinson G. Ethical standards in sport and exercise science research: 2016 Update. Int J Sports Med. 2015;36(14):1121–1124. [DOI] [PubMed] [Google Scholar]
- 38. Nguyen VN, Miller C, Sunderland J, McGuiness W. Understanding the Hawthorne effect in wound research—a scoping review. Int Wound J. 2018;15(6):1010–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Spielberger CD, Gorssuch RL, Lushene PR, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press: Mind Garden Inc; 1983. [Google Scholar]
- 40. Montori VM, Guyatt GH. Intention-to-treat principle. CMAJ. 2001;165(10):1339–1341. [PMC free article] [PubMed] [Google Scholar]
- 41. Ifeagwazi CM, Egberi HE, Chukwuorji JC. Emotional reactivity and blood pressure elevations: anxiety as a mediator. Psychol Health Med. 2018;23(5):585–592. [DOI] [PubMed] [Google Scholar]
- 42. Wiwatwongwana D, Vichitvejpaisal P, Thaikruea L, Klaphajone J, Tantong A, Wiwatwongwana A. The effect of music with and without binaural beat audio on operative anxiety in patients undergoing cataract surgery: a randomized controlled trial. Eye (Lond, Eng). 2016;30(11):1407–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]


