Abstract
Introduction:
The mental health of the health care professionals is more likely to be affected by the coronavirus disease-19 compared to the general population. Accordingly, the current study aimed to summarize the magnitudes and determinants of the psychological impact of coronavirus among health care professionals.
Methods:
The studies from Medline via PubMed, Science Direct, and Google Scholar were searched from 5 September to 19 October 2020. The review was conducted as per PRISMA-2009 (Preferred Reporting Items for Systematic Reviews and Meta-analyses).
Result:
Initially, 6316 articles were searched from three databases (PubMed, Science Direct, and Google Scholar). Finally, 20 articles were filtered to be included in our review. Among different types of psychological impact, stress was reported that lies within the range from 5.2% to 100%, anxiety was reported from 11.1% to 100%, depression was from 10.6% to 58%, and insomnia was from 28.75% to 34%. Several factors were related to the negative psychological state of health care workers due to coronavirus disease-19 like educational level, occupation, gender, age, working environment, work experience, legal status, ethnicity, psychological comorbidity, social support, personal/family exposure, and feeling of health care providers.
Conclusion:
The most common psychological impacts among health care workers were anxiety and stress. Besides different sociodemographic factors that determine the psychological impacts, front-line health care workers and participants having psychological comorbidity have a high risk of negative psychological state impacts as compared to their counterparts. Therefore, special attention should tend to health care workers directly involved in the prevention and management of coronavirus disease-19 and having a different risk of mental health condition.
Keywords: COVID-19, determinants, magnitude, psychological impacts, health care workers
Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory infectious disease that is caused by a novel coronavirus1 and is characterized, especially, by fever, cough, fatigue, dyspnea, and sputum production.2
COVID-19 became an epidemic affecting all countries of the planet.3 It has been reported that prime rates of symptoms are related to somatic, emotional, and behavioral disturbances. Such as dissociative disorders, conversion disorder, depression, post-traumatic stress (PTS) disorder, and psychological distress are occurred as consequences of the psychological impact of COVID-19.4 The study conducted on the previous strain of virus named Severe Acute Respiratory Syndrome (SARS) showed that the onset of a sudden and immediate life-threatening illness had led to extraordinary amounts of pressure on health care workers (HCWs) and might have caused adverse psychological disorders, like anxiety, fear, and stigmatization.5,6 In spite of its importance, the quarantine period for the reduction of COVID-19 transmission has a significant impact on the development of various negative psychological outcomes both short and long term.7 This psychological impact encompasses depression, conversion, dissociative disorders, anxiety, and stress.8
HCWs had a direct and continuous contact with patients having COVID-19 and their professions were risk factors for various psychological symptoms. Therefore, the burden of psychological impact was high compared to the general population.9,10
HCWs who are directly involved within the prevention, diagnosis, treatment and care of patients with COVID-19 could be at high risk of developing anxiety and stress.11
Front-line health care professionals presented a wide variety of psychological impacts like stress, mania, fear, and insomnia.12,13 This psychological pressure can reduce the health care services of the patients.14 If anxiety is left untreated, it is likely to have long-term health effects on health care workers and prevent them from fulfilling their duties, including the operations aimed at optimal control of the COVID-19 pandemic.11
The psychological status of health care professionals is impacted by a variety of factors like unknown isolation period, shortage of medical instruments, concerns about the disease, the rapid increase of the COVID-19 cases, overwhelming workload, plenty of information on the burden of the disease released on different social media, lack of treatment, and lack of social support, discrimination and stigma.9,12,14
Similarly, presence of comorbidities, rural residence, female gender, marital status, the title and level of professionalism, having children, and having close contact with the coronavirus disease (COVID-19) infected patients were the most common predictors of the negative psychological impacts among health care professional.14
Despite the psychological state effects of the coronavirus disease (COVID-19) should be recognized, it has been given less consideration across the world and ignored by simple intervention strategies like social distancing, hand washing, using masks, and quarantine.1
To make early interventions, comprehensive knowledge of the psychological effects of COVID-19 on health care professionals is indispensable. Besides this, it is paramount to identify different determinants of the psychological impacts of COVID-19 among health care providers.13 There was scanty of findings on the mental health impacts of COVID-19 in developing countries. As the result, this review examines the determinants of psychological effects in both developed and low resource setting (developing) countries.
Methods
Data sources and searching procedure
This study aims to integrate the previously conducted studies on the prevalence ad determinants of the psychological effects of COVID-19 among health care workers. The review was conducted in line with PRISMA-2009.15 The two reviewers named F.B. and M.H. were blinded and continuously searched the published studies. The two reviewers have discussed together for disagreement of the relevance of the studies to be included in the review. The articles that were found from PubMed, Science Direct, and Google Scholar and fulfilling the eligibility criteria were included. The review was conducted from 5 September to 19 October 2020. Authors manually checked for a further article to be included within the study. Endnote X5 was used to get rid of any duplicates. The Mesh terms for the entire database were: Determinants OR magnitude AND psychological impact AND health care provide AND COVID-19.
Eligibility criteria
Published findings on coronavirus disease in the English language, which contain the outcomes of interest, and full texts available, were included. The article with the unclear outcome of interest, meta-analysis studies, inaccessible full texts, preprints, and letters (short communication) to editors were excluded.
Data abstraction
Articles fulfilling the inclusion criteria were extracted on a data abstraction sheet. The following data were extracted, that is, first name of the investigator and year of study, study setting and design, sample size, age of the participants, sex, occupation, primary outcomes, and their determinants.
Methodology quality assessment
National Institute of Health quality assessment tool for observational cohort and cross-sectional studies was used to determine the quality of methodology. As per the tool, all queries were filled with “yes,” “no” or “cannot determine” and “not applicable” and “not reported.”16 Accordingly, 10 articles were good,12,14,17–24 7 were fair,1,9,25–29 and 3 article was poor.10,30,31
Results
Search results
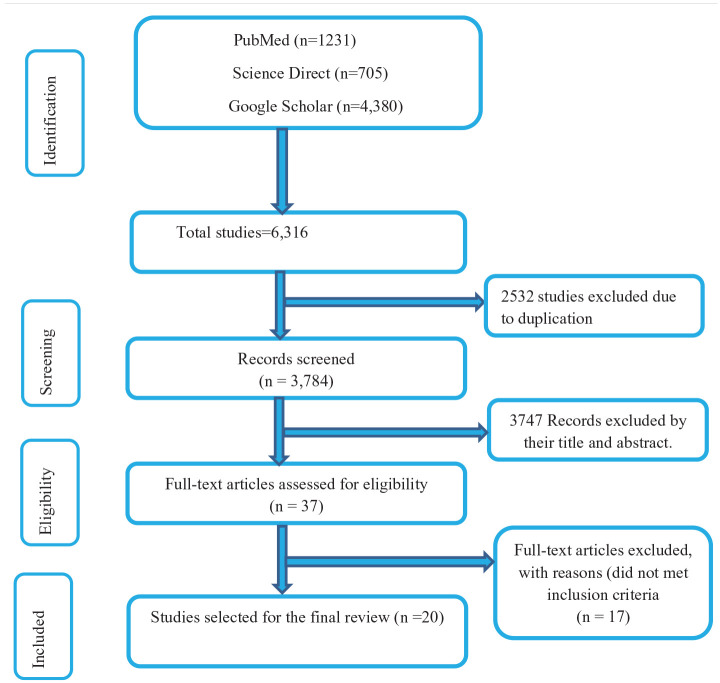
The articles were searched from PubMed, Science Direct, and Google Scholar. From three databases, 6316 articles were found initially. A total of 2532 articles were removed due to duplication which later 3784 articles were left. After seeing their titles and abstracts, 3747 articles were removed. Therefore, only 37 articles were undergone a full-text review. Finally, we included 20 articles that fulfilled the inclusion criteria to conduct the systematic review (Figure 1).
Figure 1.
Flow chart of the systematic research and study selection process.
Characteristics of studies included in this review
In our review 19 articles were cross-sectional and one article was prospective. The majority of the study was done by the online administration of the questionnaire and all of the studies were published in 2020. The study was conducted in 16 countries like China, Indonesia, Italy, Ethiopia, Nepal, Spain, USA, Oman, Israel, Peru, UK, and Saudi Arabia, India, Singapore, Malaysia, Vietnam. The review was undertaken from 5 September to 19 October 2020. The majority of the respondents were female in 17 of the articles, whereas male was predominant in the study of Ethiopia and the United States.1,17,22 In relation to their age, the majority of the participants fall in the adulthood age category. In terms of their occupations, the study conducted in Italy17 and Spain30 showed that most of the participants were physicians. However, Nurses were dominant in Indonesia,10 Oman,31 Nepal,20 Ethiopia, India, Singapore, Malaysia, and Vietnam Indonesia.1,14,23,24 In the United Kingdom and the United States, all of the participants were physicians.19,28 Variable reports were obtained in China9,18,12,25,29 (Table 1).
Table 1.
Summary of baseline characteristics of the articles that were previously published and included studies in the systematic review 2020.
| Primary author | Year of publication | Study design | Country (study setting) | Average age in years (mean or median) | Sample size | Gender (Male %) | Occupation |
|---|---|---|---|---|---|---|---|
| Si et al.9 | 2020 | Cross-sectional | China | • ⩽29 = 32.1% • 30–39 = 45.2% • 40–49 = 16.8% • ⩾50 = 5.9% |
863 | 29.3% | • Doctor = 43.7% • Nurse = 24.4% • Other health worker = 31.9% |
| Margaretha et al.10 | 2020 | Cross-sectional | Indonesia | • Late teens = 16.4% • Adulthood = 71.7% • Elderly = 11.9% |
682 | 28.2 % | • Nurse = 71.7% • Doctor = 3.7% • Radiographer = 0.7% • Midwife = 13.9% • Other health worker = 10.6% |
| Lai et al.12 | 2020 | Cross-sectional | China | • 18–25 = 15.8% • 26%–40% = 64.7% • >40 = 19.5% |
1257 | 23.3% | • Doctor = 39.2% • Nurses = 60.8% |
| Giusti et al.17 | 2020 | prospective cohort | Italy | • 44.6 ± 13.5 | 330 | 37.4% | • Doctor = 42.2% • Nurse = 26.0% • Nurse assistant = 11.5% • Physiotherapist = 10.6% • Other = 9.7% |
| Que et al.18 | 2020 | Cross-sectional | China | • 31.06 ± 6.99 | 2285 | 30.94% | • medical residents = 39.96% • Doctor = 37.64% • nurses = 9.10% • technicians = 7.83 % • public health practitioners = 5.47% |
| Romero et al.30 | 2020 | Cross-sectional | Spain | • 45.14 ± 6.48 | 3109 | – | • Medical staff = 56.6% • Nursing staff = 26.5% • Nurse assistants = 7.7% • Laboratory technicians = 0.8% • Hospital pharmacists = 2.9% • Other = 5.5% |
| Kannampallil et al.19 | 2020 | Cross-sectional | USA | __ | 393 | 55.5% | • Physicians = 100% |
| Badahdah et al.31 | 2020 | Cross-sectional | Oman | • 37.67 ± 7.68 | 509 | 19.7% | • Nurses = 61.9% • Doctor = 38.1% |
| Cai et al.25 | 2020 | Cross-sectional | China | • 36.4 ± 16.18 | 534 | 31.3% | • Doctors = 43.6% • Nurse = 46.4% • Medical technician = 9.0% • Hospital staff = 1.0% |
| Shacham et al.26 | 2020 | Cross-sectional | Israel | • 46.39 ± 11.18 | 338 | 41.4% | • Dentists = 58.6% • Dental Hygienists = 41.4% |
| Liu et al.27 | 2020 | Cross-sectional | China | • 18–39 = 75.39% • 40–59 = 24.41% • 40–49 = 23.95% • ⩾60 = 0.20% |
512 | 15.43% | • Doctors, nurses, and administrative workers = 100% |
| Khanal et al.20 | 2020 | Cross-sectional | Nepal | • 28.20 ± 5.80 | 475 | 47.4% | • Nurses = 35.2% • Doctors = 33.9% • others = 30.9% |
| Yañez et al.21 | 2020 | Cross-sectional | Peru | • 18–24 = 3.0% • 25–34 = 31% • 35–44 = 45% • 45–54 = 17% • >55 = 4% |
303 | 36.0% | • Physician = 17.0% • Nurses = 21.0% • Pharmacists = 21.0% • Technician = 26,0% • Others = 15.0% |
| Temsah et al.22 | 2020 | Cross-sectional | Saudi Arabia | • ⩽30 = 30.6% • 31–39 = 38.3% • 40–49 = 22.9% • ⩾50 = 8.2% |
582 | 25.0% | • Doctor = 26.80% • Interns = 5.8% • Nurse and midwife = 62.4% Other = 5.0% |
| Shah et al.28 | 2020 | Cross-sectional | UK | • 20–34 = 44.9% • 35–49 = 44.9% • 50–69 = 10.1% |
207 | 18.9 % | • Doctor = 100% |
| Xiao et al.29 | 2020 | Cross-sectional | China | ___ | 958 | 32.8% | • Doctor = 39.5% • Nurse = 37.5% • Laboratory = 9.1% • Others = 15.9% |
| Chekole et al.1 | 2020 | Cross-sectional | Ethiopia | • 18–24 = 19.7% • 25–31 = 66.4% • >31 = 13.9% |
244 | 66% | • Doctor = 11.1% • Nurse = 41.0% • Health officer = 6.1% • Midwifery = 9.8% • Laboratory technology = 9.8% • Pharmacist = 9.4% • Others = 12.7 |
| Teshome et al.14 | 2020 | Cross-sectional | Ethiopia | • 29.29 ± 5.69 | 798 | 60.4% | • Nurse = 44.6% • Doctor = 8.1% • Medical laboratory = 10.5% • Midwifery = 15.0% • Pharmacist = 9.6% • Public health officer = 12.0% |
| Chew et al.23 | 2020 | Cross-sectional | India, Singapore Malaysia, Vietnam Indonesia |
• 31.7 ± 7.8 | 1146 | 34.9% | • Physicians = 27.1% • Nurse = 38.7% • Other technical team = 34.2% |
| Chew et al.24 | 2020 | Cross-sectional | Singapore India |
• 29 (25–35) | 906 | 35.7% | • Physician = 29.6% • Nurse = 39.2% • Others = 10.6% • Technicians = 20.6% |
Risk of bias
The randomization and hiding of study participants were unknown in 10 articles and sufficient in the remaining 10.1,12,14,18,23,25,26,29,30 Blinding of health care workers was unknown in 12 of the articles and sufficient in 8.1,9,12,14,23–25,29 In 18 studies, there was sufficient blinding of outcome measures, but unknown in 2 articles.10,22 Incomplete outcome data were obtained in Saudi Arabia.22 There were systematic differences in the loss of participants from the study and how they are accounted in the results and methods of outcomes assessment affects group comparison. Other types of bias like Selective outcome reporting were not found in the study.
Magnitude of the psychological impact of COVID-19
Among various types of mental health impact, stress was most common in four articles conducted in China ranges from 40.2% to 71.5%,9,12 Italy 36.7%,17 and Oman 56.4%.31 The study of Spain,30 China,25 and Israel26 reports only on stress. However, anxiety was predominant in five articles conducted in Indonesia 33.4%,10 China 46.04%,18 Nepal 41.9%,20 Saudi Arabia 68.2%,22 Singapore, and India.24 Anxiety was solely studied in China27 and Ethiopia.14 The magnitude of the depression was high in the two countries: the United States, 27.2%,19 and China 58%.29 PTS was highly reported in the study of China, Italy, India, Singapore, Malaysia, Vietnam, and Indonesia which ranges from 7.4% to 47.3%,9,17,23 and insomnia has occurred in the study of China and Nepal12,18,20 (Table 2).
Table 2.
Summary of included studies on magnitude and determinants of psychological impact of COVID-19 among health care workers, 2020.
| Author | Psychological impact | Determinants |
|---|---|---|
| Si et al.9 | • Post-traumatic stress (PTS) = 40.2% • Depression = 13.6% • Perceived threat Anxiety = 13.9% • Stress = 8.6% |
• Perceived threat • Perceived social support • Active coping (AC) • Passive coping (PC) • Being Nurse |
| Margaretha et al.10 | • Anxiety = 33.4% • Depression = 17.2% • Stress = 31.7% |
• Gender • Age • Health Care Provider • Work Place • Marital status |
| Lai et al.12 | • Depression = 50.4% • Anxiety = 44.6% • Insomnia = 34.0% • Distress = 71.5% |
• Being a nurse • Women • Front-line health care workers, • Working in Wuhan, China |
| Giusti et al.17 | • Depression = 26.8% • Anxiety = 31.3% • Stress = 34.3% • Post-traumatic stress = 36.7% |
• Work hours, • Psychological comorbidities, • Fear of infection and • Perceived support by friends • Gender, • Being a nurse • working in the hospital, • Being in contact with COVID-19 patients. • Age. |
| Que et al.18 | • Anxiety = 46.04% • Depression = 44.37%, • Insomnia = 28.75% |
• Front-line health care • Attention to neutral information • Receiving negative feedback from families or friends |
| Romero et al.30 | • Stress = 100% | • Work environment • Psychotherapy use • Personal exposure • Family exposure |
| Kannampallil et al.19 | • Depression = 27.2% • Stress = 24.7% • Anxiety = 18.6% |
• Gender • Marital status • Trainees exposed to COVID-19 testing |
| Badahdah et al.31 | • High anxiety = 25.9% • High stress = 56.4% |
• Gender(being female) • Age • Working environments (HCWs who worked closely with COVID-19 patients) • Work experience |
| Cai H et al25 | • Stress = 100% | • Age • Concerns for personal safety/family/their own • Lack of treatment for COVID‑19 • Their attitude |
| Shacham et al.26 | • Stress = 100% | • Background illness • Fear of contracting COVID-19 from a patient • Higher subjective overload • Being in a committed relationship • Having higher self-efficacy |
| Liu et al.27 | • Anxiety = 100% | • Direct contact treating with COVID-19 infected patients • Medical staff from Hubei province • Suspect cases with high anxiety |
| Khanal et al.20 | • Anxiety = 41.9% • Depression = 37.5% • Insomnia = 33.9% |
• Precautionary measures in the workplace • Faced stigma • History of medication • Profession • Ethnicity • Age • Aware about government incentive • Work experience |
| Yañez et al.21 | • Severe anxiety = 21.7% • Severe mental distress = 26.1% |
• Education level • Age • Working in the private sector • Distance from the center |
| Temsah et al.22 | • Mild anxiety = 68.2% • Moderate anxiety = 20.8% • High moderate anxiety = 8.1% • Very high anxiety = 2.9% • Stress = 17.5% • worried about COVID-19 = 41.1% |
___ |
| Shah et al.28 | • Anxiety = 51 (24.64 %) • Depression = 51(40.04%) |
• Sex |
| Xiao et al.29 | • Anxiety = 54.2% • Depression = 58% |
• Gender, • Title • Protective measures • Contact history |
| Chekole et al.1 | • Stress = 100% | • Being at the age range of 25–31 years • Level of education • Being nurse • Being pharmacist |
| Teshome et al.14 | • Anxiety = 100% | • Contact with confirmed or suspected cases • No COVID-19 update • No confidence on coping with stresses • COVID-19-related worry • Their feelings |
| Chew et al.23 | • Depression = 28.9% • PTSD = 47.3% • Anxiety = 11.1% • Stress = 15.8% |
• Non-medically trained personnel • Presence of physical symptoms • Presence of prior medical conditions |
| Chew et al.24 | • Depression = 10.6% • Stress = 5.2% • PTSD = 7.4% • Anxiety = 15.7% |
• Pre-existing comorbidities • Pre-existing psychological symptoms • Being female • Older age |
PTS: post-traumatic stress; COVID: coronavirus disease; PTSD: post-traumatic stress disorder.
Determinants of the psychological impact of COVID-19
In the current study, multiple predictors of the psychological impact of COVID-19 were obtained. The study done in China,9,10 Italy,17 and Ethiopia1 revealed that being a nurse was the common factor that leads to high negative mental health outcomes. However, the study done in Ethiopia revealed that being a pharmacist was a predisposing factor for the psychological impacts of COVID-19.1 Lack of treatment for COVID‑19 was a risk factor for negative mental impacts of COVID-19 among health care professionals in China.25 The attitudes of the health care providers were the determinants of the psychological impacts of COVID-19 in China and Ethiopia.14,25
Among sociodemographic factors, gender was a determinant of the psychological impacts, consistent with the study of China, Italy, the United States, Oman, Singapore, and India.10,17,19,24,29,31 In our study being a female was predictor of the various types of psychological features. Age is a determinants in 7 articles conducted in China, Italy, Oman, Nepal, Peru, Singapore and India.10,17,20,21,24,25,31 The majority of the studies found that the mental health impacts were higher in older populations. Marital status was predictors in the study of Indonesia and the United States.10,19 Front-line health care workers had a high risk of psychological impacts as compared to others in two studies of China.12,18
Participants having psychological comorbidity have a high risk of negative mental health impacts, according to the study of Italy, China, India, Singapore, Malaysia, Vietnam, and Indonesia17,23,24,27 (Table2).
Discussion
Globally, the mental health impact and discriminations due to coronavirus disease-19 infections are increasing.32 These discriminations have resulted in different psychological effects such as anxiety and stress.3,7 This psychological impact was exacerbated by different situations like separation of partners, unknown disease characteristics, lack of supplies for preventive measures, lack of money, a low attitude of the peoples, and false information from media.8
Health care professionals directly involved in coronavirus disease-19 management were more likely affected by different psychological symptoms of depression, stress, anxiety, anger, fear, and lack of sleep.33
In the current study, the three commonly occurred psychological features were common mental disorder which includes anxiety, stress, and depression. However, three articles studied in China, and Nepal found insomnia among health care workers,12,18,20 which is consistent with the finding of Philip and Cherian13 Similar results were observed in Italy and, China.17,18 However, insomnia was the most commonly reported problem, and depression and PTSD were the least commonly occurred psychiatric features according to the study of de Pablo et al.34
The introduction of online-based psychotherapy intervention like cognitive behavioral therapy (CBT) and mindfulness-based cognitive therapy (MBCT) can enhance the mental wellbeing of the HCWs.35 There was strong support for the effectiveness of Internet cognitive behavioral therapy in treating insomnia.36
Anxiety was only reported in the finding of a study from China27 and Ethiopia.14 This is in line with the systematic review conducted previously by Bekele et al.37 The variable reports of psychological impacts are because of different sociodemographic factors and psychological comorbidities of included HCW across the different countries.
In the current review, different types of risk factors have been identified which might be correlated with the psychological impacts of COVID-19 among health care workers have been identified which includes sociodemographic factors (age, gender, ethnicity, marital status, occupation).9,10,12,17,19–21,25,28,29,31 This is similar to the study of Germany,3 Mexico,38 the United Kingdom,28 and a finding of China,12 Luo et al.39 and different from the study of China.27
In the elderly populations, the magnitudes of anxiety, depression, and stress were found to be high as compared to younger ages,10,17,20,21,25,31 which is consistent with the study of Asia and Europe40 and inconsistent with the study of Mexico in which the psychological distress was prevalent in younger ages.38 This might be due to the impact of the comorbidities, immune system capacity, and poor coping strategies elders experience with aging. Gender was another factor shown to have an association with common psychological conditions among HCW. Accordingly, female health care workers have more risks of anxiety, insomnia, and stress than men,10,12,17,19,28,29,31 and this is similar to the study done in Addis Ababa41 and the reports of Salari et al.40
The working environment was another determinant of psychological impacts.10,12,17,21,27,30,31 Similar reports were obtained in Saudi Arabia and Indonesia.10,42 Two of the studies conducted in China revealed that health care professionals working in the front-line were more likely to be affected by different psychological effects like stress, anxiety, depression, and insomnia.12,18 This is consistent with the study of Saudi Arabia and China.42,43 This might be related to increased risk of contracting the infection and care demands leading to reduced psychological stability and will increase the risks of developing emotional disturbance.
Psychological comorbidity was one of the risk factors for negative impacts of mental health in Italy,17 which is similar to the study of Luo et al.39 It is noteworthy that this population especially has a higher chance of severe mental disorder due to the fear of new pandemic disease. As limitations, the study included in this systematic review mainly used self-reported questionnaires to measure psychiatric symptoms and did not make a clinical diagnosis. Furthermore, all of the articles were cross-sectional, making it difficult to determine temporal relationships other than a single study. The limited number of studies published, heterogeneity of the articles, and incomplete outcomes of the psychological impacts were other limitations. Besides this, only published articles in reputable international journals were included and most articles failed to report proper randomization techniques.
Conclusion
In our review, different psychological disorders like depression, PTSD, anxiety, insomnia, and stress were reported. Several demographic factors were associated with the psychological impacts of coronavirus disease-19, such as educational level, occupation, marital status, ethnicity, gender, and age. Besides, front-line health care workers and participants having psychological comorbidity have a high risk of negative mental health impacts as compared to their counterparts.
Therefore, the current review will update the health care workers with the different psychological impacts of COVID-19 during their clinical practice. Besides this, special attention should be given to health care workers directly involved in the prevention and management of coronavirus disease-19 and having the different risks of mental illness.
Footnotes
Author contributions: F.B. involved in the searching of the literature and extraction of results and editing the manuscript. M.H. involved in the interpretation and revision of this systematic literature review.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was not sought for the present study because this was a review article and did not involve any patients.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was not sought for the present study because this was a review article and did not involve any subjects
ORCID iD: Firomsa Bekele  https://orcid.org/0000-0002-7855-9838
https://orcid.org/0000-0002-7855-9838
Availability of data and materials: The datasets used are available from the corresponding author on a reasonable request.
References
- 1. Chekole YA, Yimer Minaye S, Mekonnen Abate S, et al. Perceived stress and its associated factors during COVID-19 among healthcare providers in Ethiopia: A cross-sectional study. Adv Publ Healt 2020; 2020: 5036861. [Google Scholar]
- 2. Sheleme T, Bekele F, Ayela T. Clinical presentation of patients infected with coronavirus disease 19: a systematic review. Infect Dis 2020; 13: 952076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schäfer S, Sopp R, Schanz C, et al. Impact of COVID-19 on public mental health and the buffering effect of sense of coherence. Psychother Psychosom 2020; 89: 386–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord 2020; 277: 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Liu X, Kakade M, Fuller CJ, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry 2012; 53(1): 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koh D, Lim MK, Chia SE, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore what can we learn. Med Care 2005; 43(7): 676–682. [DOI] [PubMed] [Google Scholar]
- 7. Serafini G, Parmigiani B, Amerio A, et al. The psychological impact of COVID-19 on the mental health in the general population. QJM: Int J Med 2020; 113(8): 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dubey S, Biswas P, Ghosh R, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr 2020; 14: 779–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Si M, Su X, Jiang Y, et al. The psychological impact of COVID-19 on medical care workers in China. SSRN 3592, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3592642 [DOI] [PMC free article] [PubMed]
- 10. Margaretha SE, Effendy C, Kusnanto H, et al. determinants psychological distress of Indonesian health care providers during a COVID-19 pandemic. Syst Rev Pharm 2020; 11(6): 1052–1059. [Google Scholar]
- 11. Kibret S, Teshome D, Fenta E, et al. Prevalence of anxiety towards COVID-19 and its associated factors among healthcare workers in a Hospital of Ethiopia. PLoS ONE 2020; 15(12): e0243022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3(3): e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Philip J, Cherian V. Factors affecting the psychological well-being of health care workers during an epidemic: a thematic review. Indian J Psychol Med 2020; 42(4): 323–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Teshome A, Glagn M, Shegaze M, et al. Generalized anxiety disorder and its associated factors among health care workers fighting COVID-19 in southern Ethiopia. Psychol Res Behav Manag 2020; 13: 907–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med 2010; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Institutes of Health. Quality assessment tool for observational cohort and cross-sectional studies, 2004, https://www.nhlbi.nih.gov/health-pro/guidelines
- 17. Giusti EM, Pedroli E, D’Aniello GE, et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol 2020; 11: 1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Que J, Shi L, Deng J, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020; 33(3): e100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kannampallil TG, Goss CW, Evanoff BA, et al. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE 2020; 15(8): e0237301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Khanal P, Devkota N, Dahal M, et al. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Healt 2020; 16(1): 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yáñez JA, Afshar Jahanshahi A, Alvarez-Risco A, et al. Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. Am J Trop Med Hyg 2020; 103(4): 1614–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Temsah MH, Al-Sohime F, Alamro N, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health 2020; 13(6): 877–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chew NWS, Ngiam JN, Tan BY, et al. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. Bjpsych Open 2020; 6(6): e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chew NWS, Lee GKH, Tan BYQ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020; 88: 559–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of Coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit: Int Med J Exp Clin Res 2020; 26: e924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shacham M, Hamama-Raz Y, Kolerman R, et al. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. Int J Environ Res Publ Healt 2020; 17(8): 2900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu CY, Yang YZ, Zhang XM, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiology & Infection 2020; 148: e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shah N, Raheem A, Sideris M, et al. Mental health amongst obstetrics and gynaecology doctors during the COVID-19 pandemic: results of a UK-wide study. Eur J Obstet Gynecol Reprod Biol 2020; 253: 90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Xiao X, Zhu X, Fu S, et al. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Dis 2020; 274: 405–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Romero CS, Catalá J, Delgado C, et al. COVID-19 psychological impact in 3109 healthcare workers in Spain: the PSIMCOV group. Psychol Med. Epub ahead of print 14 May 2020. DOI: 10.1017/S0033291720001671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Badahdah A, Khamis F, Al Mahyijari N, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psych. Epub ahead of print 8 July 2020. DOI: 10.1177/0020764020939596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nursalam N, Sukartini T, Priyantini D, et al. Risk factors for psychological impact and social stigma among people facing COVID-19: a systematic review. Syst Rev Pharm 2020; 11: 1022–1028. [Google Scholar]
- 33. Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 2020; 13(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. de Pablo GS, Serrano JV, Catalan A, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J Affect Dis 2020; 275: 48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ho CS, Chee CY, Ho RC, et al. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med 2020; 49(3): 155–160. [PubMed] [Google Scholar]
- 36. Soh HL, Ho RC, Ho CS, et al. Efficacy of digital cognitive behavioral therapy for insomnia: a meta-analysis of randomized controlled trials. Sleep Med 2020; 75: 315–325. [DOI] [PubMed] [Google Scholar]
- 37. Bekele F, Sheleme T, Fekadu G, et al. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: a systematic review. SAGE Open Med 2020; 8: 970721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ramírez LP, Arriaga RJ, Hernández-Gonzalez MA, et al. Psychological distress and signs of post-traumatic stress in response to the COVID-19 health emergency in a Mexican sample. Psychol Res Behav Manag 2020; 13: 589–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Luo M, Guo L, Yu M, et al. The psychological and mental impact of Coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res 2020; 291: 113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Healt 2020; 16(1): 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kassaw C. The magnitude of psychological problem and associated factor in response to COVID-19 pandemic among communities living in Addis Ababa, Ethiopia, March 2020: a cross-sectional study design. Psychol Res Behav Manag 2020; 13: 631–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Al-Hanawi MK, Mwale ML, Alshareef N, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy 2020; 13: 733–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cai Q, Feng H, Huang J, et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: a case-control study. J Affect Dis 2020; 275: 210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]