Abstract
Atrial fibrillation (Afib) is the most common abnormal heart rhythm in adults and has become a significant public health concern affecting 2% to 3% of the population in Europe and North America. Left atrial appendage (LAA) thrombi is the source of 90% of left-sided cardiac thrombi in patients with Afib, which can cause stroke and other systemic vascular events. Right atrial appendage (RAA) thrombi formation in Afib is much less common but complications include pulmonary embolism or paradoxical migration across patent foramen ovale with risk of systemic embolization. The prevalence and subsequent clinical complications of RAA thrombi formation in Afib patients is not well understood. Management of RAA thrombi should be similar to that of LAA thrombi which includes delaying cardioversion and anticoagulating with warfarin therapy to achieve international normalized ratio of 2 to 3.
Keywords: cardiology, atrial fibrillation, right atrial appendage thrombus
Introduction
Atrial fibrillation (Afib) is the most common abnormal heart rhythm in adults.1 It affects 2% to 3% of the population in Europe and North America with 14% of the population over the age of 80 years old diagnosed.2 Although hemodynamic impairment from Afib can result in debilitating symptoms, the most dreaded complication of Afib is thromboembolic events. At least 1 in every 5 strokes are a result of atrial thrombi due to Afib.1,3 The left atrial appendage (LAA) is the source of 90% of left-sided cardiac thrombi.4,5 Right atrial appendage (RAA) thrombi formation in Afib is much less common. Potential complications of RAA thrombi include pulmonary embolism (PE) or paradoxical migration across patent foramen ovale (PFO) with risk of systemic embolization. No case reports have identified PE or paradoxical stroke that occurred as a result of dislodged RAA thrombus after cardioversion.6 However, the clinical significance and prevalence of RAA thrombi is not well established.1 We present the case of a patient, diagnosed with Afib, who was found to have a RAA thrombus, discuss the implications of this finding, and management.
Case Presentation
A 47-year-old male presented with worsening shortness of breath for the prior 2 months. The past medical history was significant for hypertension, non-ischemic cardiomyopathy with a left ventricular ejection fraction of 15% to 20%, and paroxysmal Afib. Notably, he reported noncompliance with outpatient guideline-directed medical therapy for heart failure and anticoagulation with apixaban due to financial constraints.
On presentation, he was noted to be in Afib with a ventricular rate of 160 beats per minute, blood pressure of 121/80 mm Hg, and oxygen saturation of 97% on room air. There was bipedal edema and mild pulmonary edema without respiratory distress suggestive of decompensated acute on chronic heart failure with reduced ejection fraction. He was admitted for diuresis and pharmacologic rate control strategies. Initial transthoracic echocardiography showed a left ventricular ejection fraction of 15% to 20% with an enlarged left ventricle and a mild to moderately impaired right ventricle function. There was moderate to severe mitral regurgitation with a severely dilated left atrium.
Over the ensuing few days, euvolemia was achieved but the ventricular rate persisted at around 140 beats per minute despite optimal AV nodal blocking therapies. Thus, a rhythm control strategy was planned with transesophageal echocardiogram (TEE) and subsequent electrical cardioversion. The TEE revealed an estimated ejection fraction of 10% to 15%, severe mitral regurgitation, no evidence of PFO, and no LAA clot despite very low velocities in the LAA. However, on examination of the RAA, a 2.7 × 1.7 cm clot was noted (Figures 1 and 2). Given these findings, cardioversion was delayed and he was placed on subcutaneous low-molecular-weight heparin injections until a therapeutic international normalized ratio (INR) of 2 to 3 could be achieved with oral warfarin. He was eventually discharged to follow-up as an outpatient for planned cardioversion.
Figure 1.
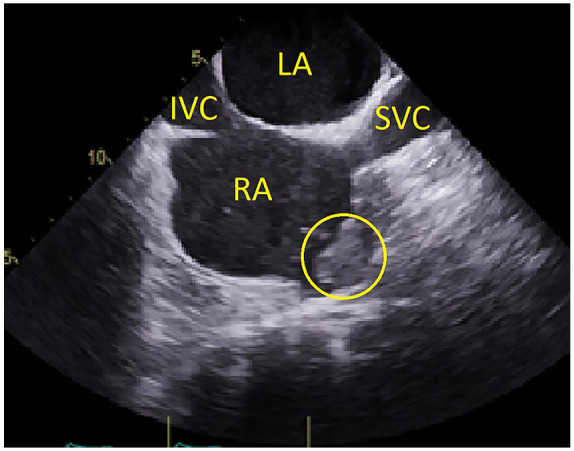
Bicaval transesophageal echocardiogram view. Right atrial appendage thrombus is noted by the yellow circle. LA, left atrium; RA, right atrium; IVC, inferior vena cava; SVC, superior vena cava.
Figure 2.
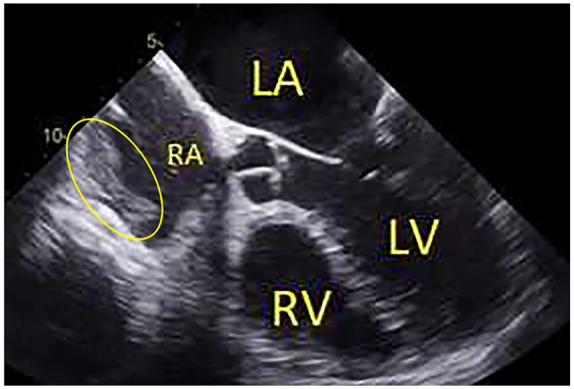
Five-chamber transesophageal echocardiogram view. Right atrial appendage thrombus is noted by the yellow circle. LA, left atrium; RA, right atrium; RV, right ventricle; LV, left ventricle.
Discussion
Atrial fibrillation has become a significant public health concern in the Western world affecting an increasing number of the population. Afib places a person at a much higher risk for formation of thrombi in the left-sided cardiac chambers most commonly the LAA.2 Patients with Afib are at an increased risk of stroke, hemorrhagic complications (as a result of stroke and oral anticoagulation), and death. Heart failure, cognitive impairment, systemic vascular events, and socioeconomic consequences are other complications of Afib. Patients diagnosed with Afib have a 5-fold increased risk of stroke and an estimated 25% of all strokes in patients over age 80 years of age are a result of thrombi attributed to Afib.7 Less understood are the prevalence and consequences of RAA thrombi in the setting Afib. Potential complications from RAA thrombi include PE or paradoxical clot through PFO although it is unclear how often these occur in Afib patients.6
There are a limited amount of data available in regard to the anatomy, function, and prevalence of thrombi in the RAA. Five separate shapes of the RAA have been identified.8 Multilobed RAA (2 lobes or greater) is identified in 84.3% of adults.8 Studies have shown that RAA dysfunction and spontaneous echocardiographic contrast predispose patients to RAA thrombi. Increased lobe complexity has been shown to be another risk factor for right atrial thrombi. Furthermore, right atrial enlargement and appendage dysfunction is correlated with increased right ventricular size and decreased right ventricular systolic function.9
The prevalence of LAA thrombi is as high as 11% to 18% based on data from TEEs. RAA thrombi are much less common based on data from TEEs, reported to be as low as 0.6% to 0.75% in Afib patients.1,3,10,11 However, a study that included a total of 23 796 autopsies suggested that the prevalence of right atrial thrombi was the same as left atrial thrombi; however, it was not clear how many of these were located in the appendages. The percentage of right and left atrial thrombi were reported to be ~3.1% in these autopsies. Of the autopsies in this study, 7% of the patients who died as a result of PE had evidence of right-sided intracardiac thrombus.7 The lower reported number of RAA thrombi on TEE may be secondary to visualization issues.12 The inability to visualize the RAA on a TEE has been reported to be as high as 16%.1 While RAA anatomy may be more difficult to visualize, the RAA should be assessed for any thrombotic burden before cardioversion.12
There is a pathophysiological connection between Afib and PE given coexistence of activated coagulation and platelet cascades. Blood stasis within the atria along with rough pectinate muscles provide a substrate for thrombus formation in Afib. Despite this pathophysiological association, there are insufficient clinical data on the association of these 2 conditions. One such reason is development of PE if small in Afib can be silent without any clinical evidence unlike LAA embolization within the systemic circulation that usually manifest with symptoms. Another reason for lack of information on their association is that guidelines do not recommend routine TEE for evaluation of RAA in patients who have suffered a PE. Transthoracic echocardiograms, which are routinely obtained after PE diagnosis, are incapable of visualization of the RAA. More research is needed to better understand the relation among Afib, RAA thrombi, and PE.11
Previous authors have suggested that the management of RAA thrombi should be the same as LAA thrombus. Patients who are found to have RAA thrombus should have cardioversion delayed. Anticoagulation with warfarin should be initiated with goal INR of 2 to 3. For all patients undergoing TEE for evaluation of LAA thrombus prior to cardioversion, the RAA appendage thrombus should be examined.1,3,10
Treatment options for right-sided thrombi option include anticoagulation, thrombolysis, and surgery. However optimal management remains unclear for right-sided thrombi. Whether to pursue medical versus surgical management should be case by case. Some factors to consider are right heart function, hemodynamic instability, PFO, and cause for thrombus. Although most commonly right-sided thrombi are found in transit from a venous source, in some cases, they may be due to malignancy.13 Right heart thrombi with associated metastatic disease often require surgical intervention.14
Conclusion
Atrial fibrillation, the most common abnormal heart rhythm in the adult population, predisposes affected patients to a significantly higher risk of stroke due to formation of thrombi in left cardiac chambers.1,2,7 However, less understood is the prevalence and subsequent clinical complications of RAA thrombi formation in Afib patients. Potential complications of RAA thrombi include PE and paradoxical migration across PFO.6 Further work is required to better understand optimal management for RAA thrombi in patients who have Afib for PE. Management should be similar to that LAA thrombi that includes delaying cardioversion and anticoagulating with Warfarin therapy to achieve INR of 2 to 3.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Aaron C. Richardson  https://orcid.org/0000-0002-3786-4385
https://orcid.org/0000-0002-3786-4385
References
- 1. Ozer O, Sari I, Davutoglu V. Right atrial appendage: forgotten part of the heart in atrial fibrillation. Clin Appl Thromb Hemost. 2010;16:218-220. [DOI] [PubMed] [Google Scholar]
- 2. Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin Epidemiol. 2014;6:213-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cresti A, Garcia-Fernandez M, Miracapillo G, et al. Frequency and significance of right atrial appendage thrombi in patients with persistent atrial fibrillation or atrial flutter. J Am Soc Echocardiogr. 2014;27:1200-1207. [DOI] [PubMed] [Google Scholar]
- 4. Blackshear J, Odell J. Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg. 1996;61:755-759. [DOI] [PubMed] [Google Scholar]
- 5. Holmes D, Reddy V. Left atrial appendage and closure. Circ Cardiovasc Interv. 2016;9:1-10. [DOI] [PubMed] [Google Scholar]
- 6. Omran H, Werner J, Maccarter D, et al. Right atrial thrombi and depressed right atrial appendage function after cardioversion of atrial fibrillation. Echocardiography. 1999;16:245-251. [DOI] [PubMed] [Google Scholar]
- 7. Ögren M, Bergqvist D, Eriksson H, Lindblad B, Sternby NH. Prevalence and risk of pulmonary embolism in patients with intracardiac thrombosis: a population-based study of 23 796 consecutive autopsies. Eur Heart J. 2005;26:1108-1114. [DOI] [PubMed] [Google Scholar]
- 8. Rissi R, Julia M, Humberto M. Checking the shape and lobation of the right atrial appendage in view of their clinical relevance. Anat Sci Int. 2019;94:324-329. [DOI] [PubMed] [Google Scholar]
- 9. Divitiis M, Heyder O, Rabahieh R, et al. Right atrial appendage thrombosis in atrial fibrillation: its frequency and its clinical predictors. Am J Cardiol. 1999;84:1023-1028. [DOI] [PubMed] [Google Scholar]
- 10. Cresti A, Garcia-Fernandez M, De Sensi F, et al. Prevalence of auricular thrombosis before atrial flutter cardioversion: a 17-year transoesophageal echocardiographic study. Europace. 2016;18:450-456. [DOI] [PubMed] [Google Scholar]
- 11. Ptaszynska-Kopczynska K, Kiluk I, Sobkowicz B. Atrial fibrillation in patients with acute pulmonary embolism: clinical significance and impact on prognosis. Biomed Res Int. 2019;2019:7846291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bilge M, Eryonucu B, Güler N, Erkoç R. Right atrial appendage function in patients with chronic nonvalvular atrial fibrillation. Jpn Heart J. 2000;41:451-462. [DOI] [PubMed] [Google Scholar]
- 13. Lai E, Alishetti S, Wong J, Delic L, Egrie G, Rosenblatt A. Right ventricular thrombus in transit: raising the stakes in the management of pulmonary embolism. CASE (Phila). 2013; 6:272-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ishida N, Takemura H, Shimabukuro K, Matsuno Y. Complete resection of asymptomatic solitary right atrial metastasis from renal cell carcinoma without inferior vena cava involvement. J Thorac Cardiovasc Surg. 2011;142:e142-e144. [DOI] [PubMed] [Google Scholar]


