Transcatheter device closures of atrial septal defects (ASD) and ventricular septal defects (VSD) have many advantages over surgical repair. Percutaneous intervention avoids the morbidity and mortality associated with open heart surgery, and is associated with a shorter hospital stay, lower risk of complications, and lower procedural costs.[1] Appropriate matching of the device to the defect is crucial to successfully close the defect and to prevent complications such as device embolization, erosion, and obstruction of structures near the device. Two-dimensional (2D) echocardiographic and three-dimensional (3D) echocardiographic (3DE) data are used to inform this process, but typically require multiple measurements in different imaging planes. The complexity of cardiac anatomy can make 2D and even 3D derived linear measurements difficult to translate into improved contextualization of relevant patient anatomy and appropriate device selection.
In order to inform patient selection and appropriate device selection for ASD and VSD closure, we created a modeling and visualization system to insert virtual device models into both segmented and volume rendered 3DE images of patients with ASD and VSD using custom code in 3D Slicer.[2, 3] First, we generated parametric models mimicking the size and shape of commonly used commercial occlusion devices including 30 ASD occlusion devices, 8 muscular VSD occlusion devices, and 13 devices designed for patent ductus arteriosus occlusion (Video 1). In addition to these pre-configured devices, we constructed a simple user interface enabling users to create new “prototype” devices (Video 2). We then created static 3D segmentations of hearts with septal defects from 3D transesophogeal images using segmentation tools in 3D Slicer as we have previously described (Figure S1). [3, 4] Segmentation takes time and manual effort, and although necessary for modalities such as 3D printing, is not practical for visualization in multiple frames of data. To address this, we also created custom echo-focused volume rendering functionality(Figure 1, Figure S2, Video 1, Video 3, Video 4).
Figure 1.
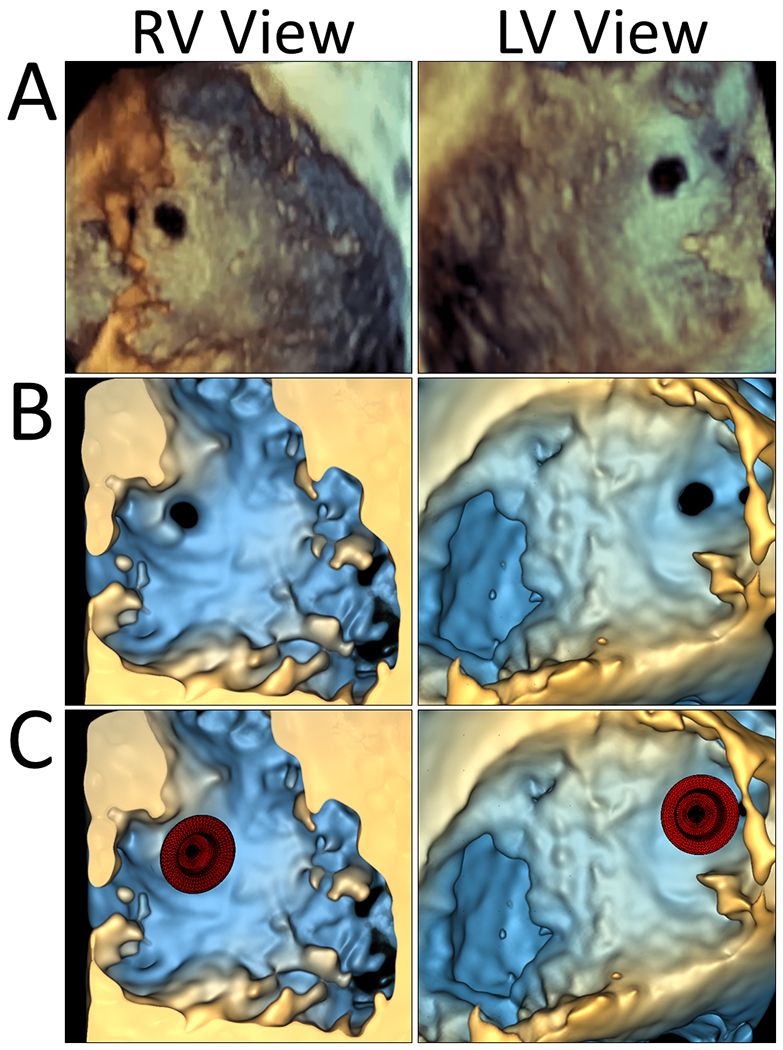
Volume Rendered Images of VSD and Virtual Implantation of a Muscular VSD Occlusion Device. A. Philips Qlab volume rendering of VSD; B. 3D Slicer volume rendering of VSD; C. Virtual implantation of muscular VSD occlusion device in volume rendered image in 3D Slicer.
We then inserted these virtual devices into the segmented and volume rendered images to better understand 3D spatial relationships of the device with surrounding cardiac structures(Videos 3 and 4). Devices were moved within the 3D models and volume rendered images using linear and rotational transforms. While feasible, we found it relatively challenging to place devices in 3D onscreen views due to the inability to appreciate the “depth” of the object relative to the heart models. As such, we explored visualization of models and rendered images in virtual reality (VR) on an HTC Vive system (HTC, Taoyuan City, Taiwan) using the SlicerVR extension.[2] VR provides the depth cues of stereo disparity and motion parallax, and an immersive experience not available via traditional viewing. Subjectively, it is much more intuitive to place devices in VR than to move devices through orthogonal 2D planes or in “3D” views on flat screens.
Finally, we created handles on the devices which allowed the devices to be deformed, or curved around the visualized anatomy. The difference in shape between the deformed device and the original device was calculated across the device, and then displayed as a color map showing regions of the device which were displaced(Figure S2).
We believe that having this ability to build both novel and existing devices, and to interact with them in routine, clinically acquired 3D images has the potential to inform both patient candidacy for device closure and appropriate device selection. Modeling such as this could eventually be incorporated into commercial echo platforms, allowing virtual “testing” of device placements in multiple cardiac phases, rather than inferring adequate fit from multiple 2D measurements. The combination of the deformation measurements and spring constants from commercial devices could, in the future, allow calculation of force of the device on the tissue which may be relevant for predicting embolization and erosion.[3] We postulate that application of these methods could inform device selection for multiple procedures, as recently demonstrated using 3D printing.[5]
We have made this device insertion functionality part of the SlicerHeart module within the 3D Slicer Extension manager. The 3D Slicer platform is available at http://www.slicer.org. Open-source code and documentation are available at https://github.com/SlicerHeart.
Supplementary Material
Supplemental Figure S1. Virtual Implantation of a Muscular VSD Occlusion Device in a 3D Segmented Model. A. Philips Qlab volume rendering of VSD viewed from the right ventricle (left) and left ventricle (right); B. 3D Slicer segmented heart model of VSD viewed from the right ventricle (left) and left ventricle (right); C. Virtual implantation of VSD occlusion device (red) in a segmented heart model in 3D Slicer (left) and visualization of the spatial relationships between the segmented tricuspid valve, mitral valve, and aortic valve in relation to the VSD occlusion device (right).
Supplemental Figure S2. Visualization of ASD in Volume Rendered Images and 3D Segmented Models. A. Philips Qlab volume rendering of ASD (left) and with implantation of septal occlusion device (right); B. 3D Slicer volume rendering of ASD (left) and with virtual implantation of septal occlusion device with color map showing device deformation (right); C. 3D Slicer segmented model of ASD (left) and with virtual implantation of septal occlusion device with color map showing device deformation (right).
Video 1: Overview of Device Selection and Placement
Video 2: Example of Customization of Device Using Parametric Modeling
Video 3: Insertion of Virtual Devices in Segmented and Volume Rendered Images of ASD
Video 4: Insertion of Virtual Devices in Segmented and Volume Rendered Images of VSD
Acknowledgments
Funding: This work was supported by the Department of Anesthesia and Critical Care at the Children’s Hospital of Philadelphia, A Children’s Hospital of Philadelphia Cardiac Center Innovation Grant, National Institute of Health NIBIB R01EB021391, and CANARIE’s Research Software Program.
Footnotes
Disclosures: Beatriz Paniagua is an employee of Kitware, Inc., an open-source software company.
References
- [1].Holzer R, Balzer D, Cao QL, Lock K, Hijazi ZM, Amplatzer Muscular Ventricular Septal Defect I. Device closure of muscular ventricular septal defects using the Amplatzer muscular ventricular septal defect occluder: immediate and mid-term results of a U.S. registry. J Am Coll Cardiol. 2004;43:1257–63. [DOI] [PubMed] [Google Scholar]
- [2].Lasso A, Nam HH, Dinh PV, Pinter C, Fillion-Robin JC, Pieper S, et al. Interaction with Volume-Rendered Three-Dimensional Echocardiographic Images in Virtual Reality. J Am Soc Echocardiogr. 2018;31:1158–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jolley MA, Lasso A, Nam HH, Dinh PV, Scanlan AB, Nguyen AV, et al. Toward predictive modeling of catheter-based pulmonary valve replacement into native right ventricular outflow tracts. Catheter Cardiovasc Interv. 2019;93:E143–E52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Scanlan AB, Nguyen AV, Ilina A, Lasso A, Cripe L, Jegatheeswaran A, et al. Comparison of 3D Echocardiogram-Derived 3D Printed Valve Models to Molded Models for Simulated Repair of Pediatric Atrioventricular Valves. Pediatr Cardiol. 2018;39:538–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fan Y, Yang F, Cheung GS, Chan AK, Wang DD, Lam YY, et al. Device Sizing Guided by Echocardiography-Based Three-Dimensional Printing Is Associated with Superior Outcome after Percutaneous Left Atrial Appendage Occlusion. J Am Soc Echocardiogr. 2019;32:708–19 e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1. Virtual Implantation of a Muscular VSD Occlusion Device in a 3D Segmented Model. A. Philips Qlab volume rendering of VSD viewed from the right ventricle (left) and left ventricle (right); B. 3D Slicer segmented heart model of VSD viewed from the right ventricle (left) and left ventricle (right); C. Virtual implantation of VSD occlusion device (red) in a segmented heart model in 3D Slicer (left) and visualization of the spatial relationships between the segmented tricuspid valve, mitral valve, and aortic valve in relation to the VSD occlusion device (right).
Supplemental Figure S2. Visualization of ASD in Volume Rendered Images and 3D Segmented Models. A. Philips Qlab volume rendering of ASD (left) and with implantation of septal occlusion device (right); B. 3D Slicer volume rendering of ASD (left) and with virtual implantation of septal occlusion device with color map showing device deformation (right); C. 3D Slicer segmented model of ASD (left) and with virtual implantation of septal occlusion device with color map showing device deformation (right).
Video 1: Overview of Device Selection and Placement
Video 2: Example of Customization of Device Using Parametric Modeling
Video 3: Insertion of Virtual Devices in Segmented and Volume Rendered Images of ASD
Video 4: Insertion of Virtual Devices in Segmented and Volume Rendered Images of VSD


