Abstract
Background
Early hemorrhage control is important in trauma-related death prevention. Tranexamic acid (TXA) has shown to be beneficial in patients in hemorrhagic shock, although widespread adoption might result in incorrect TXA administration leading to increased morbidity and mortality.
Methods
A 7-year prospective cohort study with consecutive trauma patients admitted to a Level-1 Trauma Center ICU was performed to investigate administration of both pre- and in-hospital TXA and its relation to morbidity and mortality. Indication for prehospital and in-hospital TXA administration was (suspicion of) hemorrhagic shock, and/or systolic blood pressure (SBP) ≤ 90 mmHg. Demographics, data on physiology, resuscitation and outcomes were prospectively collected.
Results
Four hundred and twenty-two patients (71% males, median ISS 29, 95% blunt injuries) were included. Even though TXA patients were more severely injured with more deranged physiology, no differences in outcome were noted. Overall, thrombo-embolic complication rate was 8%. In half the patients, hemorrhagic shock was the indication for prehospital TXA, whereas 79% of in-hospital TXA was given based on suspicion of hemorrhagic shock. Thirteen percent of patients with SBP ≤ 90 mmHg in ED received no TXA at all. Based on SBP alone, 22% of prehospital TXA and 25% of in-hospital TXA were justified.
Conclusions
Despite being more severely injured, TXA patients had similar outcome compared to patients without TXA. Thrombo-embolic complication rate was low despite liberal use of both prehospital and in-hospital TXA. Caution should be exercised in selecting patients for TXA, although this might be challenging based on SBP alone in patients who do not yet show signs of deranged physiology on arrival in ED.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00268-021-06143-y.
Background
Early hemorrhage control and adequate blood product transfusion are important in trauma-related death prevention [1, 2]. Hemostatic resuscitation prevents ongoing blood loss, restores volume status and corrects coagulopathy development [3]. Tranexamic acid (TXA) is an anti-fibrinolytic agent that acts by inhibiting plasminogen activation and fibrinolysis and promotes the ability to sustain formed clots [4]. The Clinical Randomization of an Anti-fibrinolytic in Significant Hemorrhage 2 (CRASH-2) trial showed statistically significant improvement in the rates of both overall mortality and in hemorrhage-caused mortality as a result of early administration of TXA in adults who sustained an injury within 8 h and had either significant hemorrhage, hypotension or who were considered to be at risk of significant hemorrhage [5]. These results have led to widespread incorporation of TXA in damage control resuscitation with low thresholds to administer TXA, including in prehospital settings. However, concerns have been raised that indiscriminate widespread adoption might result in TXA administration in the wrong patients, leading to increased morbidity and mortality [6–9]. Data in the literature have been contradicting, however, with others reporting no significant differences or even decreased adverse effects [10–14]. At present, it remains unclear what the exact mechanism behind TXA is and how it has reduced mortality in CRASH-2 trial, since there was no reduction in packed red blood cells (PRBC) transfusion between patients who received TXA and the ones who did not [5]. Data are still lacking regarding which trauma patients might benefit most, optimal dosing and timing and potential complications in both prehospital and in-hospital setting [4, 15].
Since most studies only focused on either prehospital or in-hospital TXA administration, we conducted a prospective population-based cohort study in polytrauma patients to investigate the indication of both pre- and in-hospital TXA administration and its relation to morbidity and mortality. We hypothesized that neither prehospital nor in-hospital TXA administration was related to increased morbidity or mortality.
Materials and methods
A 7-year prospective population-based cohort study (starting November 2013) was undertaken to investigate outcomes in severely injured patients admitted to the Intensive Care Unit (ICU) of a major (Level-1) trauma center (University Medical Center Utrecht, The Netherlands). Details of the hospital and catchment area were previously described [16]. All consecutive polytrauma patients who were admitted to the adult ICU were included. ICU admission could be either directly from the emergency department (ED) or postoperatively after urgent surgery. Patients with isolated traumatic brain injury (TBI), asphyxiation, drowning and burns were excluded, because of potential different physiologic response to severe trauma and a significantly different mortality and morbidity profile [17, 18]. Isolated injury to the brain was defined as Abbreviated Injury Score (AIS) head ≥ 3 and AIS ≤ 2 in other regions.
All data were prospectively collected by both authors and included demographics, shock and resuscitation parameters. Administration of both crystalloid and blood products including packed red blood cells (PRBC), fresh frozen plasma (FFP) and platelets (PLT) was documented in the first 24 h after admission. Additionally, prehospital and in-hospital administration (in ED, OR, ≤ 8 h and ≤ 24 h) of tranexamic acid (TXA) was recorded. Our trauma system’s protocols, including prehospital protocols, recommend administering TXA within 3 h of injury for signs of the presence of impending hemorrhagic shock, hypotension (systolic blood pressure ≤ 90 mmHg) and/or clinical suspicion of major hemorrhage. Prehospital TXA dosage was 1 g bolus, in-hospital TXA dosage was also 1 g bolus, and 1 g infusion was repeated over 8 h at discretion of the treating surgeon and/or intensivist.
Denver MOF scores [19] and ARDS Berlin criteria [20] were registered daily up until 28 days or discharge from ICU. Primary outcome was the relation between TXA administration and potentially adverse outcomes such as mortality, thrombo-embolic complications (TEC), MODS, ARDS and infections.
Secondary outcome was potential difference between pre- and in-hospital TXA administration on outcome parameters.
All statistical analyses were performed using IBM SPSS Statistics, version 25.0 (Armonk, NY, USA). Results are presented as median and interquartile range (IQR). Kruskal–Wallis was used to test continuous variables for equality between TXA and patients without TXA, whereas Chi-square or Fisher’s exact test was used to test categorical data. Variables with univariate statistical significance of less than 0.10 were included in a multivariate logistic regression analysis to identify independent risk factors for TXA administration and mortality and presented as odds ratios and 95% confidence intervals. Statistical significance was set at p < 0.05.
Results
In this study, 422 patients (71% male) with a median age of 46 (28–62) years admitted to ICU were included. Ninety-five percent of injuries were caused by a blunt mechanism, 50% was prehospitally intubated, and median ISS was 29 (22–36) with most severe injuries located in the brain (AIS head 3 (1–4)) and chest (AIS chest 3 (2–4)). One hundred and three patients (24%) underwent an urgent laparotomy. Physiology, resuscitation and outcome data are presented in Table 1. In this cohort, 79 (19%) patients died; 57 (72%) of them died of traumatic brain injury (TBI), 7 (9%) died of respiratory insufficiency, 4 (5%) due to exsanguination, 3 (4%) due to cardiac origin, 2 (3%) due to MODS, 2 (3%) due to sepsis, 1 (1%) due to ARDS and 3 (4%) due to miscellaneous causes.
Table 1.
Demographics, physiology and outcome
| Total population (n = 422) | TXA (n = 280) | No TXA (n = 142) | p-Value | |
|---|---|---|---|---|
| Age (years) | 46 (28–62) | 41 (26–59) | 51 (32–67) | 0.005* |
| Male gender | 298 (71) | 202 (72) | 96 (68) | 0.37 |
| Blunt MOI | 402 (95) | 263 (94) | 139 (98) | 0.09 |
| Prehospital intubation | 211 (50) | 151(54) | 60 (42) | 0.002* |
| Urgent laparotomy | 103 (24) | 88 (32) | 15 (11) | < 0.001* |
| ISS | 29 (22–36) | 29 (23–38) | 29 (21–34) | 0.003* |
| AIS head | 3 (1–4) | 3 (0–4) | 3 (2–4) | 0.22 |
| AIS face | 0 (0–2) | 0 (0–1) | 0 (0–2) | 0.28 |
| AIS chest | 3 (2–4) | 3 (2–4) | 3 (2–3) | 0.27 |
| AIS abdomen | 2 (0–3) | 2(0–3) | 0 (0–2) | 0.004* |
| AIS pelvis/extremities | 2 (0–3) | 2 (1–3) | 2 (0–3) | 0.005* |
| AIS external | 0 (0–1) | 0 (0–1) | 0 (0–1) | 0.31 |
| SBP_ED (mmHg) | 120 (98–140) | 117 (91–135) | 130 (105–144) | < 0.001* |
| SBP ≤ 90 mmHg_ED | 86 (20) | 68 (24) | 18 (13) | 0.005* |
| Hb_ED (mmol/L) | 8.0 (7.2–8.9) | 7.8 (7.0–8.9) | 8.4 (7.8–9.1) | < 0.001* |
| pH_ED | 7.31 (7.25–7.36) | 7.30 (7.23–7.36) | 7.33 (7.28–7.39) | < 0.001* |
| PaC02_ED (mmHg) | 46 (41–53) | 47 (42–54) | 45 (41–51) | 0.06 |
| BD _ED (mmol/L) | 3.0 (0.0–6.0) | 4.0 (1.0–8.0) | 2.0 (0.5–5.0) | < 0.001* |
| PT_ED (sec) | 14.6 (13.1–16.9) | 14.8 (13.4–17.4) | 14.4 (12.7–16.1) | 0.04* |
| Resuscitation parameters | ||||
| Crystalloids ≤ 8 h (L) | 4.5 (2.3–6.2) | 5.1 (3.0–7.0) | 2.9 (1.4–5.0) | < 0.001* |
| PRBC ≤ 8 h (U) | 1 (0–4) | 2 (0–6) | 0 (0–0) | < 0.001* |
| FFP ≤ 8 h (U) | 0 (0–4) | 2 (0–6) | 0 (0–0) | < 0.001* |
| PLT ≤ 8 h (U)# | 0 (0–1) | 0 (0–1) | 0 (0–0) | < 0.001* |
| Crystalloids ≤ 24 h (L) | 7.3 (4.8–10.1) | 8.2 (6.0–11.0) | 5.5 (3.7–7.9) | < 0.001* |
| PRBC ≤ 24 h (U) | 1 (0–5) | 3 (0–7) | 0 (0–1) | < 0.001* |
| PRBC ≥ 10 units ≤ 24 h | 44 (10) | 42 (15) | 2 (1) | < 0.001* |
| FFP ≤ 24 h (U) | 0 (0–5) | 2 (0–7) | 0 (0–0) | < 0.001* |
| PLT ≤ 24 h (U)# | 0 (0–1) | 0 (0–1) | 0 (0–0) | < 0.001* |
| Outcome parameters | ||||
| Ventilator days | 6 (2–11) | 5 (2–11) | 6 (2–11) | 0.68 |
| ICU LOS (days) | 7 (3–13) | 7 (3–13) | 7 (3–13) | 0.86 |
| H-LOS (days) | 20 (11–31) | 21 (10–33) | 18 (11–29) | 0.40 |
| MODS | 66 (16) | 42 (15) | 24 (17) | 0.67 |
| ARDS | 16 (4) | 7 (3) | 9 (6) | 0.06 |
| Infectious complications | 179 (42) | 119 (43) | 60 (42) | 1.0 |
| Thrombo-embolic complications | 32 (8) | 25 (9) | 7 (5) | 0.18 |
| Mortality | 79 (19) | 56 (20) | 23 (16) | 0.36 |
Data are expressed in median (IQR) or absolute numbers (%)
MOI Mechanism of Injury, ISS injury severity score, AIS abbreviated injury scale, ED emergency department, SBP systolic blood pressure, Hb hemoglobin, PaC02 partial pressure of carbon dioxide in arterial blood, BD base deficit, PT prothrombin time, PRBC packed red blood cells, ICU intensive care unit, LOS length of stay, H-LOS hospital length of stay, MODS multiple organ dysfunction syndrome, ARDS adult respiratory distress syndrome
* Statistically significant
#1 unit of platelets contains five donors
Sixty-six percent of patients received TXA at any point in time. During the 7-year study period, prehospital TXA administration increased (p = 0.005, Figure S1A), whereas in-hospital TXA administration did not change over time (p = 0.14, Figure S1B). Patients who received TXA were younger, more severely injured, with lower SBP and hemoglobin (Hb) in ED. Further, they were more acidotic and coagulopathic, underwent more often an urgent laparotomy and received more crystalloids and blood products both ≤ 8 and ≤ 24 h than patients who did not receive TXA. There was, however, no difference in outcome between TXA and no-TXA patients (Table 1). There was also no difference in outcome between patients with SBP ≤ 90 mmHg who received TXA and those who did not.
Subanalysis of patients who received prehospital TXA compared to patients who did not
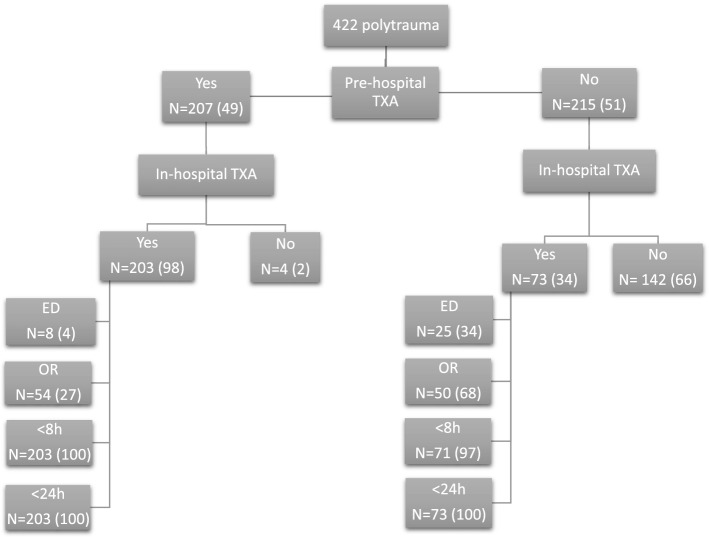
Forty-nine percent (n = 207) of patients received prehospital TXA, whereas 51% (n = 215) did not (Fig. 1). Median time from call to dispatch to ED (prehospital time) was 1:00 h (0:55–1:08), so all prehospital TXA was administered within 1 h after injury. Patients who received prehospital TXA were younger, slightly more severely injured and more often prehospitally intubated. Further, prehospital TXA patients had lower Hb and were more acidotic in ED with higher PaCO2. They received more crystalloids and PRBC ≤ 8 and ≤ 24 h. There was no difference in outcome (Table 2). All four patients (50% had SBP ≤ 90 mmHg) who later died of hemorrhage did not receive prehospital TXA. However, they all did receive TXA in OR.
Fig. 1.
Diagram of polytrauma patients and location of administered tranexamic acid. Data are expressed as absolute numbers (%). ED emergency department, OR operating room, TXA tranexamic acid
Table 2.
Comparison of patients who received prehospital tranexamic acid (TXA) and patients who did not
| Demographics N = 422 | Prehospital TXA (n = 207) | No prehospital TXA (n = 215) | p-Value |
|---|---|---|---|
| Age (years) | 40 (26–57) | 49 (31–66) | 0.004* |
| Male gender | 152 (73) | 146 (68) | 0.24 |
| Blunt MOI | 195 (94) | 207 (96) | 0.36 |
| Prehospital intubation | 134 (65) | 77 (36) | < 0.001 |
| Urgent laparotomy | 52 (25) | 51 (24) | 0.82 |
| ISS | 29 (22–38) | 29 (22–35) | 0.01* |
| AIS head | 3 (1–4) | 3 (1–4) | 0.68 |
| AIS face | 0 (0–2) | 0 (0–1) | 0.43 |
| AIS chest | 3 (2–4) | 3 (2–4) | 0.26 |
| AIS abdomen | 2(0–3) | 0 (0–3) | 0.76 |
| AIS pelvis/extremities | 2 (1–3) | 2 (0–3) | 0.17 |
| AIS external | 0 (0–1) | 0 (0–1) | 0.84 |
| SBP_ED (mmHg) | 120 (95–136) | 120 (100–140) | 0.22 |
| SBP ≤ 90 mmHg_ED | 45(22) | 41 (19) | 0.55 |
| Hb_ED (mmol/L) | 7.8 (7.0–8.9) | 8.2 (7.4–9.1) | 0.008* |
| pH_ED | 7.29 (7.23–7.35) | 7.32 (7.27–7.38) | 0.001* |
| PaCO2_ED (mmHg) | 48 (42–54) | 45 (34–51) | < 0.001* |
| BD _ED (mmol/L) | 3.0 (1.0–7.5) | 3.0 (0.0–6.0) | 0.22 |
| PT_ED (sec) | 14.7 (13.1–17.3) | 14.5 (13.2–16.8) | 0.76 |
| Resuscitation parameters | |||
| Crystalloids ≤ 8 h (L) | 4.9 (2.7–6.8) | 3.8 (1.9–5.9) | 0.001* |
| PRBC ≤ 8 h (U) | 2 (0–5) | 0 (0–4) | 0.003* |
| FFP ≤ 8 h (U) | 2 (0–5) | 0 (0–0) | 0.14 |
| PLT ≤ 8 h (U)# | 0 (0–4) | 0 (0–4) | 0.28 |
| Crystalloids ≤ 24 h (L) | 7.8 (5.6–10.5) | 6.7 (4.4–9.5) | 0.002* |
| PRBC ≤ 24 h (U) | 2 (0–6) | 0 (0–4) | 0.002* |
| PRBC ≥ 10 units ≤ 24 h | 28 (14) | 16 (8) | 0.06 |
| FFP ≤ 24 h (U) | 2 (0–6) | 0 (0–4) | 0.17 |
| PLT ≤ 24 h (U)# | 0 (0–1) | 0 (0–1) | 0.21 |
| Outcome parameters | |||
| Ventilator days | 5 (2–10) | 6 (2–11) | 0.40 |
| ICU LOS (days) | 7 (3–12) | 7 (3–14) | 0.29 |
| H-LOS (days) | 20 (10–31) | 20 (11–32) | 0.87 |
| MODS | 28 (14) | 38 (18) | 0.28 |
| ARDS | 4 (2) | 12 (6) | 0.07 |
| Infectious complications | 85 (41) | 94 (44) | 0.56 |
| Thrombo-embolic complications | 12 (6) | 20 (9) | 0.20 |
| Mortality | 39 (19) | 40 (19) | 1.0 |
Data are expressed in median (IQR) or absolute numbers (%)
MOI Mechanism of injury, ISS injury severity score, AIS abbreviated injury scale, ED emergency department, SBP systolic blood pressure, Hb hemoglobin, PaC02 partial pressure of carbon dioxide in arterial blood, BD base deficit, PT prothrombin time, PRBC packed red blood cells, ICU intensive care unit, LOS length of stay, H-LOS hospital length of stay, MODS multiple organ dysfunction syndrome, ARDS adult respiratory distress syndrome
*Statistically significant
#1 unit of platelets contains five donors
Subanalysis of patients who received in-hospital TXA compared to patients who did not
Two hundred and seventy-six (65%) patients received in-hospital TXA, whereas 146 did not (Fig. 1). Seventy-four percent had already received prehospital TXA. Patients who received in-hospital TXA were younger, more severely injured with lower SBP and Hb, more acidotic and coagulopathic in ED than patients who did not receive in-hospital TXA. Further, they underwent more often urgent laparotomies and received more crystalloids and blood products ≤ 8 and ≤ 24 h. Again, there was no difference in outcome (Table 3).
Table 3.
Comparison of patients who received in-hospital TXA and patients who did not
| Demographics N = 422 | In-hospital TXA (n = 276) | No in-hospital TXA (n = 146) | p-Value |
|---|---|---|---|
| Age (years) | 42 (26–59) | 51 (32–67) | 0.01* |
| Male gender | 200 (72) | 98 (67) | 0.26 |
| Blunt MOI | 259 (94) | 143 (98) | 0.09 |
| Prehospital intubation | 149 (54) | 62 (43) | 0.001* |
| Urgent laparotomy | 88 (32) | 15 (10) | < 0.001* |
| ISS | 29 (22–38) | 29 (22–34) | 0.005* |
| AIS head | 3 (0–4) | 3 (2–4) | 0.02* |
| AIS face | 0 (0–1) | 0 (0–2) | 0.58 |
| AIS chest | 3 (2–4) | 3 (2–3) | 0.82 |
| AIS abdomen | 2 (0–3) | 0 (0–2) | < 0.001* |
| AIS pelvis/extremities | 2 (1–3) | 2 (0–3) | < 0.001* |
| AIS external | 0 (0–1) | 0 (0–1) | 0.96 |
| SBP_ED (mmHg) | 117 (91–135) | 130 (105–144) | < 0.001* |
| SBP ≤ 90 mmHg_ED | 68(25) | 18 (12) | 0.002* |
| Hb_ED (mmol/L) | 7.8 (7.0–8.9) | 8.4 (7.8–9.1) | < 0.001* |
| pH_ED | 7.30 (7.23–7.36) | 7.33 (7.28–7.39) | < 0.001* |
| PaCO2 (mmHg) | 47 (41–54) | 45 (41–51) | 0.12 |
| BD _ED (mmol/L) | 4.0 (1.0–8.0) | 2.0 (1.0–5.0) | < 0.001* |
| PT_ED (sec) | 14.9 (13.3–17.5) | 14.3 (12.7–16.0) | 0.02* |
| Resuscitation parameters | |||
| Crystalloids ≤ 8 h (L) | 5.2 (3.1–7.1) | 2.9 (1.4–5.0) | < 0.001* |
| PRBC ≤ 8 h (U) | 2 (0–7) | 0 (0–0) | < 0.001* |
| FFP ≤ 8 h (U) | 2 (0–6) | 0 (0–0) | < 0.001* |
| PLT ≤ 8 h (U)# | 0 (0–1) | 0 (0–0) | < 0.001* |
| Crystalloids ≤ 24 h (L) | 8.2 (6.1–11.0) | 5.5 (3.7–7.9) | < 0.001* |
| PRBC ≤ 24 h (U) | 3 (0–7) | 0 (0–1) | < 0.001* |
| PRBC≥ 10units ≤ 24 h | 42 (15) | 2 (1) | < 0.001* |
| FFP ≤ 24 h (U) | 2 (0–7) | 0 (0–0) | < 0.001* |
| PLT ≤ 24 h (U)# | 0 (0–1) | 0 (0–0) | < 0.001* |
| Outcome parameters | |||
| Ventilator days | 5 (2–11) | 6 (2–10) | 0.79 |
| ICU LOS (days) | 7 (3–13) | 7 (3–13) | 0.81 |
| H-LOS (days) | 21 (10–33) | 18 (11–29) | 0.54 |
| MODS | 42 (15) | 24 (16) | 0.78 |
| ARDS | 7 (3) | 9 (6) | 0.10 |
| Infectious complications | 117 (42) | 62 (42) | 1.0 |
| Thrombo-embolic complications | 25 (9) | 7 (5) | 0.13 |
| Mortality | 55 (20) | 24 (16) | 0.43 |
Data are expressed in median (IQR) or absolute numbers (%)
MOI Mechanism of injury, ISS injury severity score, AIS abbreviated injury scale, ED emergency department, SBP systolic blood pressure, Hb hemoglobin, PaC02 partial pressure of carbon dioxide in arterial blood, BD base deficit, PT prothrombin time, PRBC packed red blood cells, ICU intensive care unit, LOS length of stay, H-LOS hospital length of stay, MODS multiple organ dysfunction syndrome, ARDS adult respiratory distress syndrome
*Statistically significant
#1 unit of platelets contains five donors
Median time to TXA was 1:02 h (0:58–1:20). The time frame within TXA was administered is shown in Fig. 2. Ninety-three percent of patients who had TXA received it early (< 3 h) after injury. There was no difference in outcome in patients who had early TXA compared to late TXA (≥ 3 h) (Table S1).
Fig. 2.
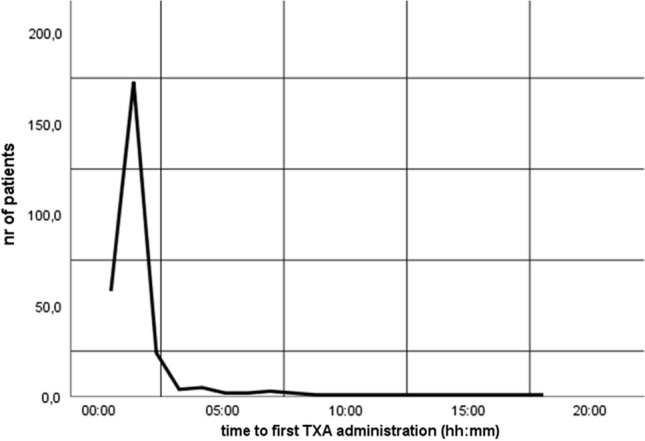
Time to first tranexamic acid (TXA) administration
There was no significant difference in TXA dosage in TXA patients who received early TXA compared to late TXA (1 g (1–2) vs. 1 g (1–1), p = 0.16). There was also no difference in TXA dosage between patients who developed TEC and those who did not (1 g (1–2) vs. 1 g (1–1), respectively, p = 0.20).
Fifty-two percent (45/86) of patients who received prehospital TXA had SBP ≤ 90 mmHg compared to 79% (68/86) of patients who received in-hospital TXA (Table 4). Seventy-eight percent (162/207) of patients received prehospital TXA despite SBP > 90 mmHg in ED, and 75% (208/276) of patients received in-hospital TXA despite SBP > 90 mmHg in ED. Further, 32% (23/73) of patients who had in-hospital TXA had unjustified not received prehospital TXA, and 13% (18/142) of patients who had SBP ≤ 90 mmHg in ED received no TXA at all. Based on systolic blood pressure alone, 22% (45/207) of prehospital TXA and 25% (68/276) of in-hospital TXA were justified (Table 4).
Table 4.
Relation between systolic blood pressure (SBP) ≤ 90 mmHg in ED and TXA administration
| Prehospital TXA | No prehospital TXA | In-hospital TXA | No in-hospital TXA | Total no. of patients | |
|---|---|---|---|---|---|
| SBP_ED ≤ 90 mmHg | 45 | 41 | 68 | 18 | 86 |
| SBP_ED > 90 mmHg | 162 | 174 | 208 | 128 | 336 |
| Total no. of patients | 207 | 215 | 276 | 146 | 422 |
SBP systolic blood pressure, ED emergency department, TXA tranexamic acid
In multivariate analysis, age, hemoglobin, PaCO2 and pH in ED were independent predictors for TXA administration. Age, ISS and base deficit in ED were independent predictors for mortality. TXA, however, was not related to death (Tables 5, 6).
Table 5.
Independent predictors for TXA administration
| Variables in the equation | Β Coefficient | p-Value | Odds ratio | 95% C.I | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | − 0.019 | 0.001 | 0.981 | 0.969 | 0.992 |
| ISS | 0.011 | 0.306 | 1.011 | 0.990 | 1.033 |
| SBP_ED | − 0.001 | 0.893 | 0.999 | 0.991 | 1.008 |
| Hb_ED | − 0.041 | 0.000 | 0.960 | 0.939 | 0.982 |
| BD_ED | 0.017 | 0.099 | 1.017 | 0.997 | 1.037 |
| PT_ED | − 0.001 | 0.573 | 0.999 | 0.995 | 1.003 |
| PaCO2_ED | − 0.096 | 0.034 | 0.908 | 0.831 | 0.993 |
| pH_ED | − 0.159 | 0.023 | 0.853 | 0.744 | 0.978 |
| Constant | 125.723 | 0.019 | 3.989E+54 | ||
Table 6.
Independent predictors for mortality
| Variables in the Equation | Β Coefficient | P-Value | Odds Ratio | 95% C.I | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Age | 0.046 | 0.000 | 1.047 | 1.030 | 1.065 |
| Laparotomy | − 0.156 | 0.695 | 0.856 | 0.393 | 1.865 |
| ISS | 0.050 | 0.000 | 1.052 | 1.025 | 1.079 |
| SBP_ED | 0.008 | 0.095 | 1.008 | 0.999 | 1.018 |
| Hb_ED | − 0.006 | 0.609 | 0.994 | 0.971 | 1.017 |
| BD_ED | − 0.016 | 0.000 | 0.984 | 0.978 | 0.990 |
| Thrombo-embolic complications | − 0.453 | 0.560 | 0.636 | 0.139 | 2.914 |
| TXA | −0.096 | 0.773 | 0.908 | 0.472 | 1.749 |
| Constant | − 6.625 | 0.000 | 0.001 | ||
ISS Injury severity score, SBP systolic blood pressure, BD base deficit, ED emergency department, Hb hemoglobin, PT prothrombin time, PaCO2 partial pressure of carbon dioxide, TXA tranexamic acid
Discussion
In this cohort of polytrauma patients, there was no difference in outcome between patients who received TXA and those who did not, even though TXA patients were more severely injured with more deranged physiology. Subanalysis of prehospital and in-hospital TXA administration also revealed no difference in outcome. Based on systolic blood pressure alone (SBP ≤ 90 mmHg), large numbers of unjustified prehospital and in-hospital TXA administration were found. However, these large numbers could be slightly overestimated since no data on prehospital SBP were collected and the first collected SBP for this study was in ED. It is possible that prehospital SBP could have been higher and decreased during transport. Moreover, since the original inclusion to administer TXA was a rather vague and subjective description of “signs of the presence of impending hemorrhagic shock and/or clinical suspicion of major hemorrhage,” in this study SBP ≤ 90 mmHg was used as most objective measurement of hemorrhagic shock to be able to calculate whether TXA administration was justified. This strict inclusion of SBP ≤ 90 mmHg might label TXA as “unjustified” in some patients with normal SBP even though they were in imminent shock. Especially in prehospital settings, it could be difficult to diagnose early signs of hemorrhagic shock, and a “better safe than sorry” attitude is often adopted. Another reason for TXA administration in patients without hypotension might be explained by a previously described phenomenon in which severely injured patients in smaller service areas with short transport times do not have deranged physiologic parameters on arrival in ED. These patients did not have the time to deteriorate, because they were in the hospital before blood pressure, BD and hemoglobin will change distinctly [21, 22].
This liberal approach of prehospital TXA administration even increased over time during the 7-year study and has recently also been described by Kheirbek et al. Despite large numbers of unjustified TXA use, they also did not demonstrate difference in TEC [23].
In addition to the rationale of unjustified TXA administration, it is also intriguing why patients with signs of shock did not receive TXA. A few of these patients had shock based on other causes than hemorrhage such as neurogenic shock based on high spinal cord lesion. Four patients (5%) who died due to hemorrhagic shock did not receive prehospital TXA, nor in ED. They all did receive TXA in OR. It could be debated that time was so critical in these exsanguinating patients that there was simply no time to administer TXA prehospitally nor in ED. This was contradicted by reviewing both prehospital transport times and time from ED to OR in these patients, and there was no difference compared to other patients who needed urgent surgery. It remains unclear whether these patients would have survived if they had received TXA earlier.
Almost all patients who received TXA for the first time had it within the recommended 3 h after injury. There was no difference in dosage between patients who had early TXA and those who had late TXA nor was there any difference in outcome suggesting that both dosage and timing of TXA did not influence outcome.
Our data are in line with several other reports in the literature suggesting that TXA in a polytrauma population was not associated with increased TEC and mortality even if it was administered liberally [10–13]. However, current data are in contrast to other studies that demonstrated increased mortality after TXA [6–9]. A possible explanation for these seemingly contradicting data was proposed by Moore et al. suggesting that outcome after TXA might be related to fibrinolytic state of the patient with least expected benefit from TXA in patients with physiological fibrinolysis [9, 24]. In our hospital, viscoelastic tests are not routinely used in trauma. However, in a previous study thromboelastography in severely injured patients (who were part of the same cohort used in this study) showed no abnormalities [25]; therefore, it could be assumed that the patients in this study had physiological levels of fibrinolysis. Nevertheless, there was no difference in mortality between patients who received TXA and patients who did not in this study.
Despite being more severely injured TXA patients had no difference in outcome suggesting that TXA has ameliorated outcome. This should be concluded with caution; First of all, even if only patients with SBP ≤ 90 mmHg in ED were analyzed, there was no difference in morbidity and mortality between patients with and without TXA. Further, the numbers of exsanguinating patients were very low since only four patients died of hemorrhage. Additionally, it remains to be seen whether TXA is truly advantageous in settings with small service areas with short transport times and with the immediate availability of blood products and operating room to control hemorrhagic shock.
In this cohort of polytrauma patients, many patients also sustained TBI (AIShead 3 (1–4)). TBI was also the main cause of death in this population (72%). Data even suggest that prehospital TXA was often given in patients with TBI since patients who received prehospital TXA had higher AIShead, were more often prehospitally intubated and had higher PaCO2 with similar pH in ED (suggestive for prehospital hypoventilation) than patients who did not receive prehospital TXA. Several studies have reported various effects of TXA on outcome in TBI from depending on brain injury severity and timing of TXA administration [26] to no difference in outcome after prehospital TXA [27], or even a potential harmful effect of prehospital TXA on mortality in severe TBI patients [28]. The effect of TXA on TBI in this polytrauma population was beyond the scope of this paper. Future research will focus on the effect of TXA on TBI.
A few limitations need to be acknowledged: First of all, this was a single-institution study. Further, clinicians who were treating these patients were also the researchers. Another limitation is that no details on comorbidities nor any data on prehospital and in-hospital Glasgow Coma Scale were collected.
In conclusion, TXA patients had similar outcome compared to patients without TXA despite being more severely injured. There was a liberal use of both prehospital and in-hospital TXA with large numbers of patients receiving TXA without hypotension. Hemorrhagic shock was indication for prehospital TXA in only half the patients, whereas in-hospital TXA was given based on suspicion of hemorrhagic shock in the vast majority of patients. Caution should be exercised since it can be difficult to select the right patient for TXA especially in severely injured patients who do not show grossly signs of deranged physiology prehospitally or on arrival in ED yet.
Supplementary Information
Below is the link to the electronic supplementary material.
Authors’ contributions
KW and LL have contributed to the conception and design of the study, performed acquisition of data and given final approval of the version to be submitted. KW has done the analysis and interpretation of data and drafted the article. LL has revised it critically for important intellectual content.
Funding
No funds were received in connection with the presented study.
Availability of data and materials
The datasets supporting the conclusions of this article are available upon reasonable request from the corresponding author.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The local ethics committee approved this prospective observational study and waived consent (reference number WAG/mb/16/026664).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Karlijn J. P. van Wessem, Email: kwessem@umcutrecht.nl
Luke P. H. Leenen, Email: l.p.h.Leenen@umcutrecht.nl
References
- 1.Gruen RL, Jurkovich GJ, McIntyre LK, et al. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006;244:371–380. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evans JA, van Wessem KJ, McDougall D, et al. Epidemiology of traumatic deaths: comprehensive population-based assessment. World J Surg. 2010;34(1):158–163. doi: 10.1007/s00268-009-0266-1. [DOI] [PubMed] [Google Scholar]
- 3.Spahn DR, Bouillon B, Cerny V, et al. The European guideline on management of major bleeding and coagulopathy following trauma. Crit Care. 2019;23(1):98. doi: 10.1186/s13054-019-2347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramirez RJ, Spinella PC, Bochicchio GV. Tranexamic acid update in trauma. Crit Care Clin. 2017;33(1):85–99. doi: 10.1016/j.ccc.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 5.CRASH-2 Trial Collaborators. Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23–32. doi: 10.1016/S0140-6736(10)60835-5. [DOI] [PubMed] [Google Scholar]
- 6.Valle EJ, Allen CJ, Van Haren RM, et al. Do all trauma patients benefit from tranexamic acid? J Trauma Acute Care Surg. 2014;76(6):1373–1378. doi: 10.1097/TA.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 7.Myers SP, Kutcher ME, Rosengart MR, et al. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J Trauma Acute Care Surg. 2019;86(1):20–27. doi: 10.1097/TA.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 8.Richards JE, Fedeles BT, Chow JH, et al. Is Tranexamic acid associated with mortality or multiple organ failure following severe injury? Shock. 2021;55(1):55–60. doi: 10.1097/SHK.0000000000001608. [DOI] [PubMed] [Google Scholar]
- 9.Moore HB, Moore EE, Huebner BR, Stettler GR, Nunns GR, Einersen PM, Silliman CC, Sauaia A. Tranexamic acid is associated with increased mortality in patients with physiological fibrinolysis. J Surg Res. 2017;220:438–443. doi: 10.1016/j.jss.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guyette FX, Brown JB, Zenati MS, STAAMP Study Group et al. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: a double-blind, placebo-controlled, randomized clinical trial. JAMA Surg. 2020;156(1):11–20. doi: 10.1001/jamasurg.2020.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Menyar A, Sathian B, Wahlen BM, et al. Prehospital administration of tranexamic acid in trauma patients: A 1:1 matched comparative study from a level 1 trauma center. Am J Emerg Med. 2020;38(2):266–271. doi: 10.1016/j.ajem.2019.04.051. [DOI] [PubMed] [Google Scholar]
- 12.Rivas L, Estroff J, Sparks A, et al. The incidence of venous thromboembolic events in trauma patients after tranexamic acid administration: an EAST multicenter study. Blood Coagul Fibrinolysis. 2021;32(1):37–43. doi: 10.1097/MBC.0000000000000983. [DOI] [PubMed] [Google Scholar]
- 13.Cole E, Davenport R, Willett K, et al. Tranexamic acid use in severely injured civilian patients and the effects on outcomes: a prospective cohort study. Ann Surg. 2015;261(2):390–394. doi: 10.1097/SLA.0000000000000717. [DOI] [PubMed] [Google Scholar]
- 14.Mitra B, Mazur S, Cameron PA, PATCH-Trauma Study Investigators et al. Tranexamic acid for trauma: filling the 'GAP' in evidence. Emerg Med Australas. 2014;26(2):194–197. doi: 10.1111/1742-6723.12172. [DOI] [PubMed] [Google Scholar]
- 15.Napolitano LM. Prehospital tranexamic acid: what is the current evidence? Trauma Surg Acute Care Open. 2017;2(1):e000056. doi: 10.1136/tsaco-2016-000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunning AC, Lansink KWW, van Wessem KJP, et al. Demographic patterns and outcomes of patients in level-1 trauma centers in three international trauma systems. World J Surg. 2015;39(11):2677–2684. doi: 10.1007/s00268-015-3162-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dewar DC, Tarrant SM, King KL, et al. Changes in the epidemiology and prediction of multiple-organ failure after injury. J Trauma Acute Care Surg. 2013;74(3):774–779. doi: 10.1097/TA.0b013e31827a6e69. [DOI] [PubMed] [Google Scholar]
- 18.Dewar DC, White A, Attia J, et al. Comparison of postinjury multiple-organ failure scoring systems: Denver versus Sequential Organ Failure Assessment. J Trauma Acute Care Surg. 2014;77:624–629. doi: 10.1097/TA.0000000000000406. [DOI] [PubMed] [Google Scholar]
- 19.Sauaia A, Moore FA, Moore EE. Early predictors of postinjury multiple organ failure. Arch Surg. 1994;129:39–45. doi: 10.1001/archsurg.1994.01420250051006. [DOI] [PubMed] [Google Scholar]
- 20.Ranieri VM, Rubenfeld GD, Thompson BT, ARDS Definition Task Force et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 21.Gunning AC, Leenen LPH. Applicability of the predictors of the historical trauma score in the present Dutch trauma population: modelling the TRISS predictors. J Trauma Acute Care Surg. 2014;77:614–619. doi: 10.1097/TA.0000000000000415. [DOI] [PubMed] [Google Scholar]
- 22.Van Wessem KJP, Leenen LPH. Reduction in mortality rates of postinjury multiple organ dysfunction syndrome: a shifting paradigm? Prospect Popul-Based Cohort Study Shock. 2018;49(1):33–38. doi: 10.1097/SHK.0000000000000938. [DOI] [PubMed] [Google Scholar]
- 23.Heirbek T, Jikaria N, Murray B, et al. Unjustified administration in liberal use of tranexamic acid in trauma resuscitation. J Surg Res. 2021;258:125–131. doi: 10.1016/j.jss.2020.08.045. [DOI] [PubMed] [Google Scholar]
- 24.Napolitano LM, Cohen MJ, Cotton BA, et al. Tranexamic acid in trauma: how should we use it? J Trauma Acute Care Surg. 2013;74(6):1575–1586. doi: 10.1097/TA.0b013e318292cc54. [DOI] [PubMed] [Google Scholar]
- 25.van Wessem KJP, Leenen LPH. Thromboelastography does not provide additional information to guide resuscitation in the severely injured. ANZ J Surg. 2017 doi: 10.1111/ans.14357. [DOI] [PubMed] [Google Scholar]
- 26.CRASH-3 Trial Collaborators Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet. 2019;394:1713–1723. doi: 10.1016/S0140-6736(19)32233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rowell SE, Meier EN, McKnight B, Kannas D, May S, Sheehan K, Bulger EM, Idris AH, Christenson J, Morrison LJ, Frascone RJ, Bosarge PL, Colella MR, Johannigman J, Cotton BA, Callum J, McMullan J, Dries DJ, Tibbs B, Richmond NJ, Weisfeldt ML, Tallon JM, Garrett JS, Zielinski MD, Aufderheide TP, Gandhi RR, Schlamp R, Robinson BRH, Jui J, Klein L, Rizoli S, Gamber M, Fleming M, Hwang J, Vincent LE, Williams C, Hendrickson A, Simonson R, Klotz P, Sopko G, Witham W, Ferrara M, Schreiber MA. Effect of out-of-hospital tranexamic acid vs placebo on 6-month functional neurologic outcomes in patients with moderate or severe traumatic brain injury. JAMA. 2020;324(10):961–974. doi: 10.1001/jama.2020.8958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bossers SM, Loer SA, Bloemers FW, Den Hartog D, Van Lieshout EMM, Hoogerwerf N, van der Naalt J, Absalom AR, Peerdeman SM, Schwarte LA, Boer C, Schober P. Association between prehospital tranexamic acid administration and outcomes of severe traumatic brain injury. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets supporting the conclusions of this article are available upon reasonable request from the corresponding author.