Abstract
Context:
Chronic tendinopathy is a challenging problem that can lead to significant disability and limitation in not only athletics but also activities of daily living. While there are many treatment techniques described for this overuse injury, no single modality has been proven superior to all others. With recent advances in medical technology, percutaneous ultrasonic tenotomy (PUT) for tendinosis has gained traction with promising results.
Objective:
To examine the data published on PUT for treatment of tendinopathy, analyze the outcomes of the procedure, including duration of pain relief and patient-reported outcomes, and assess the rate of complications associated with the procedure.
Data Sources:
PubMed, MEDLINE, EMBASE, and Google Scholar.
Study Selection:
The following combination of keywords was entered into the electronic search engines: ultrasonic tenotomy, ultrasound tenotomy, Tenex, and ultrasonic percutaneous tenotomy. The search results were screened for studies relevant to the topic. Only English-language studies were considered for inclusion. Studies consisting of level 4 evidence or higher and those involving human participants were included for more detailed evaluation.
Level of Evidence:
Level 4.
Data Extraction:
Articles meeting the inclusion criteria were sorted and reviewed. Type of tendinopathy studied, outcome measures, and complications were recorded. Both quantitative and qualitative analyses were performed on the data collected.
Results:
There were a total of 7 studies that met the inclusion criteria and quality measures—5 studies involving the treatment of elbow tendinopathy and 1 study each involving the management of Achilles tendinopathy and plantar fasciitis. PUT resulted in decreased pain/disability scores and improved functional outcome scores for chronic elbow tendinopathy and plantar fasciitis. Results for Achilles tendinopathy showed modest improvement in the short term, but long-term data are lacking.
Conclusion:
PUT is a minimally invasive treatment technique that can be considered in patients with tendinopathy refractory to conservative treatment measures. Further higher quality studies are necessary to accurately assess the comparative effectiveness of this treatment modality.
Keywords: ultrasonic tenotomy, tenex, tendinopathy, tendinosis, tendonitis, systematic review
Tendinopathy is a common clinical condition resulting in pain and disability. Achilles, patellar, rotator cuff, and elbow extensor tendons are the most commonly affected, although involvement of the tendons of the wrist and ankle is not uncommon.28,55 The burden of this disease is often underestimated because it results in not only direct health care costs but also indirect costs in the form of lost productivity, decreased quality of life, and increased worker’s compensation cases.23
Tendinopathy is a chronic disease of the tendons resulting in disorganization of collagen fibrils, neovascularization, and degeneration of tenocytes.53 Recent research has led to awareness of a distinction between tendonitis and tendinosis. While tendonitis is an inflammatory condition resulting from microtears of the musculotendinous unit, tendinosis refers to degeneration of collagen resulting from chronic overuse.5 While inflammatory cells can be found on histopathology of tendinosis as well, recent evidence suggests that a failed healing response in the face of repetitive stresses placed on the tendon leads to decreased mechanical integrity.15,31 It is important to distinguish between these 2 entities because patients may experience pain relief once inflammation is reduced in tendonitis, but this is not guaranteed in tendinosis.
Treatment for tendinosis starts with nonoperative measures such as nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy (PT), although the long-term efficacy of NSAIDs is debatable in chronic cases.40 Eccentric loading exercises produce beneficial results in Achilles tendinopathy.33,35,43 Other nonoperative measures provide pain relief include bracing and shockwave therapy, although randomized controlled trials and systematic reviews have failed to demonstrate superiority of these treatment modalities over others.29,32,42,46 Injectable biologic substances such as platelet-rich plasma (PRP) are also gaining traction based on results from recent animal and clinical studies.16,20,44 These biologic agents usually consist of 2 kinds of mediators: (1) naturally occurring growth factors that act by stimulating angiogenesis, matrix synthesis, or remodeling or (2) anti-inflammatory molecules that inhibit tissue degradation.11 While basic science studies suggest that the potential of these agents to reduce pain, encourage tissue healing, and stimulate tendon regeneration is great, robust clinical data supporting their regular use are sparse.11
Invasive treatment options can be broadly classified into 3 categories—minimally invasive percutaneous techniques, arthroscopic techniques, and open surgical debridement. Historically, open surgical debridement of extensor tendons with or without suture anchor repair provides high rates (95%-97%) of patient satisfaction with minimal complications in refractory cases of lateral epicondylitis.17,18,48 However, a recent randomized controlled trial showed no additional benefit of excision of diseased extensor carpi radialis brevis tendon compared with sham surgery.27 Conflicting results have been observed in surgical treatment of other tendinopathies as well, with patient satisfaction ranging from 69% to 100% and complication rates varying from 0% to 85%.2,21 With the advent of endoscopic techniques, arthroscopic debridement of diseased tendons has touted similar satisfaction rates but lower complication rates in some studies, while others have shown that open treatment groups have better functional outcomes.2,30,56 One of the latest advancements for treatment of recalcitrant tendinopathy is percutaneous ultrasonic tenotomy (PUT) (Tenex).3,34,47 It involves phacoemulsification to debride and aspirate diseased tendon tissue through a small incision. The device consists of a suction and irrigation system connected to a handheld tool with an ultrasonic vibrating double-lumen needle that is the size of an 18-guage needle.9,41 The handheld instrument produces small-amplitude, high-frequency oscillations that target angiofibroblastic tissue in the tendon and emulsify necrotic areas. This debris is then aspirated through an irrigation system.54 This evolving technique has been cleared through the 510 (k) pathway by the US Food and Drug Administration for use in general surgery, orthopaedic surgery, laparoscopic surgery, and plastic and reconstructive surgery.41
The purpose of this study is to provide a comprehensive review of the evidence published on the effectiveness of PUT in the treatment of tendinopathy.
Methods
Search Strategy
A thorough search of the electronic databases PubMed, MEDLINE, EMBASE, and Google Scholar was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement with the following date ranges for filters: December 1, 1990, to February 1, 2019. The following combination of keywords was entered into the electronic search engines: ultrasonic tenotomy, ultrasound tenotomy, Tenex, and ultrasonic percutaneous tenotomy. The search results were screened for studies relevant to the topic. Only English-language studies were considered for inclusion. Studies consisting of level 4 evidence or higher and those involving human participants were included for more detailed evaluation.
Study Selection
The following inclusion criteria were used for study selection: The study design had to (1) be level of evidence 1, 2, 3, or 4 as defined by the Centre for Evidence-Based Medicine,10 (2) include treatment of the condition of interest (tendinopathy), and (3) include treatment with PUT. There was no minimum duration of follow-up, as the authors wanted to include as many studies for evaluation as possible given the limited data published so far on this particular topic.
The following exclusion criteria were applied: (1) case reports, expert opinions, or other studies with level 5 evidence; (2) reviews; (3) non-English studies; (4) studies on nonhuman subjects; (5) basic science or biomechanical studies; and (6) studies on other percutaneous treatment options not involving PUT. The study selection algorithm and the search results that were obtained as a result of this algorithm are illustrated in a stepwise fashion in Figure 1.
Figure 1.
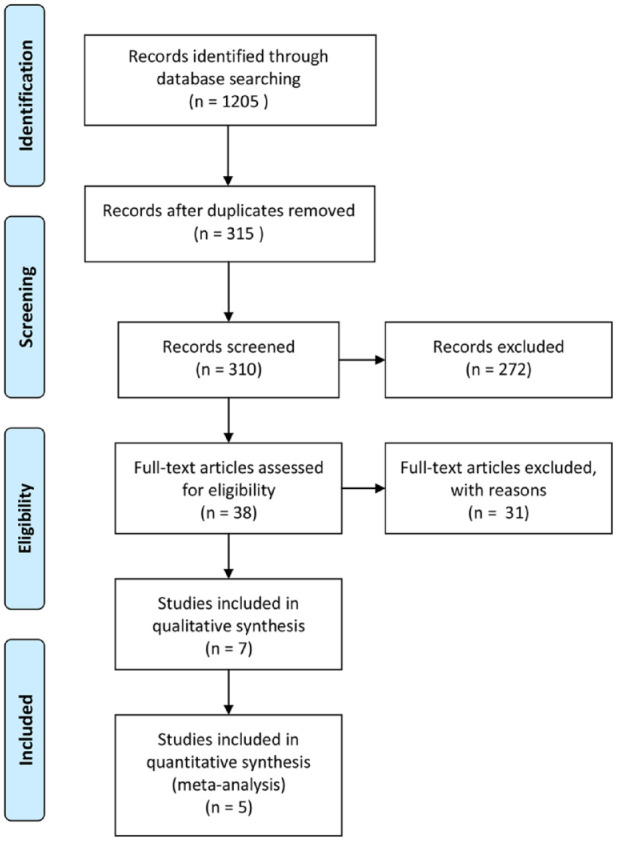
Search algorithm used to select studies for inclusion using the PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines.
Data Extraction
The included studies were reviewed independently by 2 authors, and data were extracted for analysis in a spreadsheet. The data collected included study design, number of patients treated, level of evidence of the study, average duration of follow up, type of tendinopathy treated, patient demographics, outcomes and complications of treatment, and any subgroup analysis performed in the study and conclusions resulting from those analyses. The spreadsheets were analyzed independently by 3 authors, and any discrepancies in the data were resolved by consensus. Furthermore, independent risk of bias assessment was performed for each study by all 3 authors and discrepancies were again resolved through discussion.
Quality Appraisal
The methodological quality of each included study was evaluated independently by 3 authors using the following criteria: scope and depth of the topic, study design, level of evidence included, sample size studied, average time of follow-up, use of independent examiners, attrition rate, and use of objective outcome measures. The internal and external validity of each study was also assessed using specific criteria set forth by National Institute for Health Research and National Health Service Centre for Reviews and Dissemination.22,49,50 In particular, the internal validity of each study was assessed using the criteria found in Appendix 1 (available in the online version of this article). The external validity of each study was assessed using the criteria found in Appendix 2 (available online).
Based on these quality analyses, 1 more study was excluded from analysis due to poor quality of the reported results.
Data Analysis
Data related to the variables of interest such as patient-reported outcome measures from all studies were pooled and reported as weighted mean and standard deviation. Student t test was used where appropriate to determine if the change in outcome score of interest was statistically significant after the PUT procedure. Level of significance was set at 0.05.
Results
Study Characteristics
There were 7 studies that met the inclusion criteria and quality measures. Three of these 7 were retrospective studies and 4 were prospective studies. Only studies meeting at least 5 or more of the quality criteria set forth for assessing internal and external validity were included for analysis (Table 1).
Table 1.
Study description and quality
| Author(s) (Year) | Journal | Study Design | Level of Evidence | Average Follow-up, mo | Quality Criteria Met (Out of 10) |
|---|---|---|---|---|---|
| Barnes et al (2015)4 | Journal of Shoulder and Elbow Surgery | Prospective case series | 4 | 12 | 9 |
| Battista et al (2018)6 | Techniques in Hand & Upper Extremity Surgery | Retrospective case series | 4 | 24 | 6 |
| Boden et al (2019)8 | Journal of Shoulder and Elbow Surgery | Retrospective case series | 4 | 10 | 8 |
| Chimenti et al (2018)12 | Journal of Ultrasound Medicine | Retrospective case series | 4 | 20 | 9 |
| Koh et al (2013)25 | American Journal of Sports Medicine | Prospective case series | 4 | 12 | 7 |
| Patel (2015)39 | American Journal of Orthopaedics | Prospective case series | 4 | 12 | 7 |
| Seng et al (2016)45 | American Journal of Sports Medicine | Prospective case series | 4 | 36 | 7 |
Study Surgical Details
Different tendinopathies treated with PUT include lateral and medial elbow tendinopathy, plantar fasciitis, and Achilles tendinopathy. The visual analogue scale (VAS) score, the American Shoulder and Elbow Surgeons score, Disabilities of the Arm, Shoulder and Hand (DASH) score, Mayo Elbow Performance Score, 12-Item Short Form Health Survey (SF-12), and the American Orthopaedic Foot & Ankle Score (AOFAS) were the most commonly used (Table 2).
Table 2.
Type of tendinopathy treated and study outcomes
| Author(s) (Year) | No. of Cases Included | Demographics | Tendinopathy Treated | Outcomes |
|---|---|---|---|---|
| Barnes et al (2015)4 | 19 | • Average age, 55.3 y • 10 male, 9 female • Median duration of symptoms, >6 mo |
Lateral and medial epicondylitis of the elbow | Baseline VAS improved from 6.4 to 0.7 at 1 y, majority of improvement occurring in the first 3 months. Q-DASH score improved from 44.1 to 8.6 at 1 year. MEPS improved from 59.1 to 90.5 at 1 year. |
| Battista et al (2018)6 | 7 | • Mean duration of symptoms, 21.4 mo | Lateral epicondylitis of the elbow | Preoperative VAS score was 7.9 and decreased to 1.1 postoperatively at 2 y. Preoperative ASES score was 55.6 and at 1 y it was 93.4. One of 7 patients underwent open tendon debridement after failure of symptom relief. |
| Boden et al (2019)8 | 30 | • Mean age, 51 y • 40% female • On average experience, 25 mo of pain prior to intervention |
Medial and lateral epicondylitis of the elbow | 80% of Tenex patients were satisfied vs 79% of PRP patients; 16% of PRP patients and 20% of Tenex patients had refractory pain requiring further procedures. No statistical difference in outcomes between PRP and Tenex. |
| Chimenti et al (2019)12 | 34 | • Median duration of symptoms, 1.5 y • Mean age, 52.2 y • Mean BMI, 32.9 kg/m2 • 21 female, 13 male |
Insertional Achilles tendinopathy | At long-term follow-up, 4 of 34 had no pain, 13 had mild pain, 2 had moderate pain, 1 had worse pain, and rest were lost to follow-up. Physical component of SF-12 improved but no change in mental component at short-term (6- or 12-week) follow-up. Complications: 1 superficial skin infection that resolved with oral antibiotics. |
| Koh et al (2013)25 | 20 | • Average age, 45.5 y • 7 male, 13 female • Median duration of symptoms, 12.5 mo • 17/20 had repetitive strain injury, 4 had sporting injury, 3 had history of trauma |
Lateral epicondylitis of the elbow | Median VAS score decreased from 5.5 at baseline to 0.5 at 1 year. Median DASH-Compulsory score dropped from 21.7 to 2.5 at 1 y and DASH-Work went from 25.0 to 0. 19 of 20 were satisfied and 1 neutral. 19 of 20 had reduction in extensor tendon thickness at 6 mo, 1 had increased thickness. |
| Patel (2015)39 | 12 | • Median duration of symptoms, >6 mo • 4/12 had endoscopic or open partial releases at other institutions |
Plantar fasciitis | Mean preoperative AOFAS score improved from 30.1 to 88.1 by 3 mo and sustained at 12 mo. No treatment complications noted. |
| Seng et al (2016)45 | 20 | • 7 male, 13 female • Average age, 45.5 y |
Lateral epicondylitis of the elbow | DASH-Compulsory score decreased to a median of 0. Tendon hypervascularity decreased in 94% and tendon thickness reduction in 100%. |
AOFAS, American Orthopaedic Foot & Ankle Society; ASES, American Shoulder and Elbow Surgeons; BMI, body mass index; DASH, Disabilities of the Arm, Shoulder and Hand; MEPS, Mayo Elbow Performance Score; PRP, platelet-rich plasma; Q-DASH, Quick-DASH (11-item version of the DASH); SF-12; 12-Item Short Form Health Survey; VAS, visual analogue scale.
Chronic Epicondylosis of the Elbow
Five of the 7 studies (76 patients) included involved treatment of elbow tendinopathies with PUT.4,6,25,45 The pain/disability scores for these 5 studies were evaluated in aggregate and the results are provided in Figure 2. Overall, the VAS and DASH scores improved 1 year status post–PUT procedure as compared with baseline. These improvements were not only statistically significant for each outcome measure but may also be clinically important. Recent research has shown that the minimal clinically important difference in VAS pain score for shoulder arthroplasty was 1.4 and 13.0 for DASH score.26 Patients undergoing PUT for elbow tendinopathy observed a difference of more than 4 points in the VAS score and more than 20 points for each of the DASH subscores (Figure 2).
Figure 2.
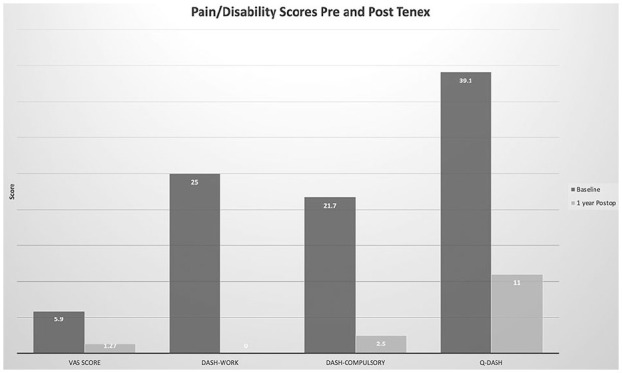
Improved pain and disability scores after Tenex procedure. DASH, Disabilities of the Arm, Shoulder and Hand; Postop, postoperative; Q-DASH, Quick-DASH (11-item version of the DASH); VAS, visual analogue scale.
Furthermore, patients undergoing PUT for refractory elbow tendinopathies also experienced an overall improvement in functional scores 1 year status post-Tenex as compared with baseline (Figure 3).52
Figure 3.
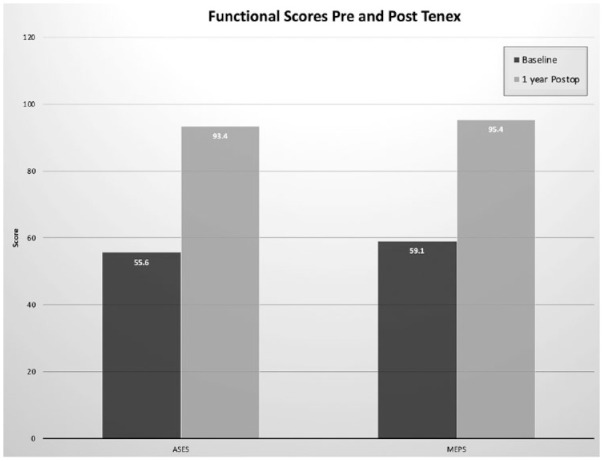
Improved functional scores pre- and post-Tenex. ASES, American Shoulder and Elbow Surgeons; MEPS, Mayo Elbow Performance Score; postop, postoperative.
Plantar Fasciitis
Of the 12 patients evaluated prospectively, 11 experienced complete pain relief 3 months after Tenex and this improvement was sustained at 12 months postoperatively. There were no complications noted and the mean AOFAS score improved from 30.1 at baseline to 88.1 at 3 months postoperatively. However, 4 out of the 12 patients treated in this study underwent prior open or partial plantar fascial release.
Achilles Tendinopathy
Chimenti et al12 studied 34 patients who underwent Tenex for insertional Achilles tendinopathy. There was 1 complication reported: superficial surgical site infection treated with oral antibiotics alone. Of the 34 patients, 4 had no pain at long-term follow-up (11-36 months), 13 had mild pain, 2 had moderate pain, 1 had severe pain, and the rest were lost to follow-up. There was some improvement in the physical component of SF-12 but no improvement in the mental component of SF-12 survey at short-term follow-up (6-12 weeks).
Discussion
This systematic review focused on assessment of effectiveness of PUT for the treatment of tendinopathy and demonstrated that PUT has the potential to be an effective treatment alternative in patients with epicondylitis of the elbow.4,6,8,25,45 Patients with plantar fasciitis may also experience improvement in pain with this procedure, but evidence is limited.39 Results for Achilles tendinopathy revealed that while PUT may provide short-term pain relief in the majority of the patients, it may not reliably improve quality of life as perceived by patients in the long term.12
Tendinopathy has been historically difficult to treat perhaps because our understanding of its histopathology has evolved over the years and continues to evolve. Even though initially it was thought of as an overuse condition, more recently underuse has also been implicated in this disease process.24 While the diagnosis can be made relatively easily through clinical history and examination, prescribing the right treatment for the right patient can be more challenging. Recommendation of rest, activity modification, PT and anti-inflammatories may be appropriate initial treatment for tendinopathy pain and dysfunction and can result in remission in most cases after 52 weeks of treatment.1 Corticosteroid injections have not resulted in any significantly different outcomes from rest.1 However, PT with a focus on range of motion and eccentric strengthening exercises is superior to conservative treatment with rest alone in the management of lateral epicondylitis at 6 weeks.7 Similarly, PT with the addition of other modalities such as cryotherapy, ultrasound, and laser therapy results in significant pain relief and return to sport in patellar tendinopathy as well.37 Extracorporeal shockwave therapy is also another treatment option that results in superior results compared with conservative treatment alone in a recent study of 27 patients with patellar tendinopathy.51
In recent years, biologic treatments such as autologous blood injections and PRP injections have gained some acceptance. A randomized control trial by Mishra et al36 compared outcomes in 2 groups of patients with lateral epicondylitis: those who underwent needling with PRP and those who underwent needling without PRP. Even though there were no significant differences in pain relief at 12 weeks, only 29.1% of the PRP group still reported pain at 24 weeks compared with 54.0% in the control group.36 While preliminary results for biologic injections are promising in cadaveric and small sample prospective human studies, further investigation is needed to determine their long-term efficacy.13,14
Surgery is an alternative treatment option: arthroscopic or open debridement. Pascarella et al38 studied the outcomes of arthroscopic debridement of Hoffa fat pad, abnormal patellar tendon, and excision of the lower pole of the patella in patients with chronic patellar tendinopathy refractory to corticosteroid injections and PT. They showed that of the 27 professional athletes included in the study, 19 patients returned to their sports at the same preoperative level and the average Lysholm score improved from 52.3 preoperatively to 95.5 at 3 years postoperatively. However, 7 patients had recurrence of pain when they returned to sports within 3 years of operation. Furthermore, there are limited data available on whether these improvements in pain and function are sustainable over longer periods. Similarly, Gill et al19 studied the outcomes after open debridement of the patellar tendon for tendinopathy and showed an overall improvement in pain and patient satisfaction in up to 82% of the 34 patients they studied. However, 7 patients said they would not have the surgery again. These results and those from prior studies show that despite exhaustive conservative management, use of minimally invasive treatment options, and appropriate surgical intervention in the form of either arthroscopic or open debridement, there can be a small contingent of patients with tendinopathy who have refractory symptoms.
There were several major limitations to our review. First, there are very limited data on this narrow research topic. There is sparse information available on patient-reported outcomes, and follow-up duration was short in the available data. As such, the quality of evidence in the available literature did not allow a robust statistical analysis due to small sample sizes and high variety of conditions treated with PUT. Second, only a limited number of tendons have been studied. Third, all the articles included in this review were uncontrolled case series consisting of level 4 evidence. Hence, there is a risk that conclusions drawn from these data may be prone to selection bias, among other types of biases.
Conclusion
PUT is a minimally invasive treatment technique that can be considered in patients with tendinopathy refractory to conservative treatment measures. Further, higher quality studies are necessary to accurately assess the comparative effectiveness of this treatment modality.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_1941738120951764 for Utility of Percutaneous Ultrasonic Tenotomy for Tendinopathies: A Systematic Review by Sravya Vajapey, Sennay Ghenbot, Michael R. Baria, Robert A. Magnussen and W. Kelton Vasileff in Sports Health: A Multidisciplinary Approach
Footnotes
The following authors declared potential conflicts of interest: W.K.V. is a paid consultant for Zimmer Biomet. M.B., R.M., and W.K.V. received payments for development of educational presentations from CDC Medical, and R.M. also received payments from Zimmer Biomet.
References
- 1. Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: a review of pathology and management. Bone Joint J. 2013;95-B:1158-1164. [DOI] [PubMed] [Google Scholar]
- 2. Baltes TPA, Zwiers R, Wiegerinck JI, van Dijk CN. Surgical treatment for midportion Achilles tendinopathy: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25:1817-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barnes DE. Ultrasonic energy in tendon treatment. Oper Tech Orthop. 2013;23:78-83. [Google Scholar]
- 4. Barnes DE, Beckley JM, Smith J. Percutaneous ultrasonic tenotomy for chronic elbow tendinosis: a prospective study. J Shoulder Elbow Surg. 2015;24:67-73. [DOI] [PubMed] [Google Scholar]
- 5. Bass E. Tendinopathy: why the difference between tendinitis and tendinosis matters. Int J Ther Massage Bodywork. 2012;5:14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Battista CT, Dorweiler MA, Fisher ML, Morrey BF, Noyes MP. Ultrasonic percutaneous tenotomy of common extensor tendons for recalcitrant lateral epicondylitis. Tech Hand Up Extrem Surg. 2018;22:15-18. [DOI] [PubMed] [Google Scholar]
- 7. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Boden AL, Scott MT, Dalwadi PP, Mautner K, Mason RA, Gottschalk MB. Platelet-rich plasma versus Tenex in the treatment of medial and lateral epicondylitis.J Shoulder Elbow Surg. 2019;28:112-119. [DOI] [PubMed] [Google Scholar]
- 9. Burke CJ, Adler RS. Ultrasound-guided percutaneous tendon treatments. AJR Am J Roentgenol. 2016;207:495-506. [DOI] [PubMed] [Google Scholar]
- 10. Centre for Evidence-Based Medicine. Accessed August 7, 2019.http://www.cebm.net
- 11. Carr JB, 2nd, Rodeo SA. The role of biologic agents in the management of common shoulder pathologies: current state and future directions. J Shoulder Elbow Surg. 2019;28:2041-2052. [DOI] [PubMed] [Google Scholar]
- 12. Chimenti RL, Stover DW, Fick BS, Hall MM. Percutaneous ultrasonic tenotomy reduces insertional Achilles tendinopathy pain with high patient satisfaction and a low complication rate. J Ultrasound Med. 2019;38:1629-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chong AK, Ang AD, Goh JC, et al. Bone marrow-derived mesenchymal stem cells influence early tendon-healing in a rabbit Achilles tendon model. J Bone Joint Surg Am. 2007;89:74-81. [DOI] [PubMed] [Google Scholar]
- 14. Connell D, Datir A, Alyas F, Curtis M. Treatment of lateral epicondylitis using skin-derived tenocyte-like cells. Br J Sports Med. 2009;43:293-298. [DOI] [PubMed] [Google Scholar]
- 15. Del Buono A, Battery L, Denaro V, Maccauro G, Maffulli N. Tendinopathy and inflammation: some truths. Int J Immunopathol Pharmacol. 2011;24 (suppl 2):45-50. [DOI] [PubMed] [Google Scholar]
- 16. Di Matteo B, Filardo G, Kon E, Marcacci M. Platelet-rich plasma: evidence for the treatment of patellar and Achilles tendinopathy—a systematic review. Musculoskelet Surg. 2015;99:1-9. [DOI] [PubMed] [Google Scholar]
- 17. Dunn JH, Kim JJ, Davis L, Nirschl RP. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36:261-266. [DOI] [PubMed] [Google Scholar]
- 18. Dwyer AJ, Govindaswamy R, Elbouni T, Chambler AF. Are “knife and fork” good enough for day case surgery of resistant tennis elbow? Int Orthop. 2010;34:57-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gill TJ, 4th, Carroll KM, Hariri S. Open patellar tendon debridement for treatment of recalcitrant patellar tendinopathy: indications, technique, and clinical outcomes after a 2-year minimum follow-up. Sports Health. 2013;5:276-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gonzalez JC, Lopez C, Alvarez ME, Perez JE, Carmona JU. Autologous leukocyte-reduced platelet-rich plasma therapy for Achilles tendinopathy induced by collagenase in a rabbit model. Sci Rep. 2016;6:19623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Griffiths GP, Selesnick FH. Operative treatment and arthroscopic findings in chronic patellar tendinitis. Arthroscopy. 1998;14:836-839. [DOI] [PubMed] [Google Scholar]
- 22. Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20 (suppl 1):21-35. [DOI] [PubMed] [Google Scholar]
- 23. Hopkins C, Fu SC, Chua E, et al. Critical review on the socio-economic impact of tendinopathy. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;4:9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kannus P. Etiology and pathophysiology of chronic tendon disorders in sports. Scand J Med Sci Sports. 1997;7:78-85. [DOI] [PubMed] [Google Scholar]
- 25. Koh JS, Mohan PC, Howe TS, et al. Fasciotomy and surgical tenotomy for recalcitrant lateral elbow tendinopathy: early clinical experience with a novel device for minimally invasive percutaneous microresection. Am J Sports Med. 2013;41:636-644. [DOI] [PubMed] [Google Scholar]
- 26. Koorevaar RCT, Kleinlugtenbelt YV, Landman EBM, van ‘t Riet E, Bulstra SK. Psychological symptoms and the MCID of the DASH score in shoulder surgery. J Orthop Surg Res. 2018;13:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kroslak M, Murrell GAC. Surgical treatment of lateral epicondylitis: a prospective, randomized, double blinded, placebo controlled clinical trial. Am J Sports Med. 2018;46:1106-1113. [DOI] [PubMed] [Google Scholar]
- 28. Lai WC, Erickson BJ, Mlynarek RA, Wang D. Chronic lateral epicondylitis: challenges and solutions. Open Access J Sports Med. 2018;9:243-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Langer PR. Two emerging technologies for Achilles tendinopathy and plantar fasciopathy. Clin Podiatr Med Surg. 2015;32:183-193. [DOI] [PubMed] [Google Scholar]
- 30. Lohrer H, David S, Nauck T. Surgical treatment for Achilles tendinopathy—a systematic review. BMC Musculoskelet Disord. 2016;17:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Loppini M, Maffulli N. Conservative management of tendinopathy: an evidence-based approach. Muscles Ligaments Tendons J. 2011;1:134-137. [PMC free article] [PubMed] [Google Scholar]
- 32. Luginbühl R, Brunner F, Schneeberger AG. No effect of forearm band and extensor strengthening exercises for the treatment of tennis elbow: a prospective randomised study. Chir Organi Mov. 2008;91:35-40. [DOI] [PubMed] [Google Scholar]
- 33. Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009;19:54-64. [DOI] [PubMed] [Google Scholar]
- 34. McMullen C, Liem B. Efficacy of percutaneous ultrasonic ablation of soft tissue (Tenex) in tendinopathy and fasciopathy. Curr Phys Med Rehab Rep. 2018;6:156-160. [Google Scholar]
- 35. Meyer A, Tumilty S, Baxter GD. Eccentric exercise protocols for chronic non-insertional Achilles tendinopathy: how much is enough? Scand J Med Sci Sports. 2009;19:609-615. [DOI] [PubMed] [Google Scholar]
- 36. Mishra AK, Skrepnik NV, Edwards SG, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter, randomized controlled trial of 230 patients. Am J Sports Med. 2014;42:463-471. [DOI] [PubMed] [Google Scholar]
- 37. Panni AS, Tartarone M, Maffulli N. Patellar tendinopathy in athletes. Outcome of nonoperative and operative management. Am J Sports Med. 2000;28:392-397. [DOI] [PubMed] [Google Scholar]
- 38. Pascarella A, Alam M, Pascarella F, Latte C, Di Salvatore MG, Maffulli N. Arthroscopic management of chronic patellar tendinopathy. Am J Sports Med. 2011;39:1975-1983. [DOI] [PubMed] [Google Scholar]
- 39. Patel MM. A novel treatment for refractory plantar fasciitis. Am J Orthop (Belle Mead NJ). 2015;44:107-110. [PubMed] [Google Scholar]
- 40. Pattanittum P, Turner T, Green S, Buchbinder R. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst Rev. 2013;5:CD003686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Peck E, Jelsing E, Onishi K. Advanced ultrasound-guided interventions for tendinopathy. Phys Med Rehabil Clin N Am. 2016;27:733-748. [DOI] [PubMed] [Google Scholar]
- 42. Pettrone FA, McCall BR. Extracorporeal shock wave therapy without local anesthesia for chronic lateral epicondylitis. J Bone Joint Surg Am. 2005;87:1297-1304. [DOI] [PubMed] [Google Scholar]
- 43. Rowe V, Hemmings S, Barton C, Malliaras P, Maffulli N, Morrissey D. Conservative management of midportion Achilles tendinopathy: a mixed methods study, integrating systematic review and clinical reasoning. Sports Med. 2012;42:941-967. [DOI] [PubMed] [Google Scholar]
- 44. Seetharamaiah VB, Gantaguru A, Basavarajanna S. A comparative study to evaluate the efficacy of platelet-rich plasma and triamcinolone to treat tennis elbow. Indian J Orthop. 2017;51:304-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Seng C, Mohan PC, Koh SB, et al. Ultrasonic percutaneous tenotomy for recalcitrant lateral elbow tendinopathy: sustainability and sonographic progression at 3 years. Am J Sports Med. 2016;44:504-510. [DOI] [PubMed] [Google Scholar]
- 46. Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand (N Y). 2014;9:419-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tenex Health. Accessed August 7, 2019. https://tenexhealth.com
- 48. Thornton SJ, Rogers JR, Prickett WD, Dunn WR, Allen AA, Hannafin JA. Treatment of recalcitrant lateral epicondylitis with suture anchor repair. Am J Sports Med. 2005;33:1558-1564. [DOI] [PubMed] [Google Scholar]
- 49. University of York. Undertaking systematic reviews of research on effectiveness: CRD’s guidance for those carrying out or commissioning reviews. Accessed August 7, 2019. http://www.crd.york.ac.uk/CRDWeb/ShowRecord.asp?AccessionNumber=32001000984
- 50. Vajapey SP, Blackwell RE, Maki AJ, Miller TL. Treatment of extensor tendon disruption after total knee arthroplasty: a systematic review. J Arthroplasty. 2019;34:1279-1286. [DOI] [PubMed] [Google Scholar]
- 51. Wang CJ, Ko JY, Chan YS, Weng LH, Hsu SL. Extracorporeal shockwave for chronic patellar tendinopathy. Am J Sports Med. 2007;35:972-978. [DOI] [PubMed] [Google Scholar]
- 52. Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What change in American Shoulder and Elbow Surgeons Score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016;474:2672-2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Williams JG. Achilles tendon lesions in sport. Sports Med. 1993;16:216-220. [DOI] [PubMed] [Google Scholar]
- 54. Williams RC, Pourcho AM. Percutaneous ultrasonic tenotomy for refractory common extensor tendinopathy after failed open surgical release: a report of two cases. PM R. 2018;10:313-316. [DOI] [PubMed] [Google Scholar]
- 55. Wilson JJ, Best TM. Common overuse tendon problems: a review and recommendations for treatment. Am Fam Physician. 2005;72:811-818. [PubMed] [Google Scholar]
- 56. Yan H, Cui GQ, Liu YL, Xiao J, Yang YP, Ao YF. A randomized comparison of open and arthroscopic Nirschl debridement for refractory lateral epicondylitis [in Chinese]. Zhonghua Wai Ke Za Zhi. 2009;47:888-891. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_1941738120951764 for Utility of Percutaneous Ultrasonic Tenotomy for Tendinopathies: A Systematic Review by Sravya Vajapey, Sennay Ghenbot, Michael R. Baria, Robert A. Magnussen and W. Kelton Vasileff in Sports Health: A Multidisciplinary Approach


