Abstract
Background:
Baseball is one of the most popular boy’s youth sports, and there has been a rise in the rates of certain overuse injuries among players. Specialization has been identified as a risk factor for overuse injury in high school athlete populations, but there is little understanding of the prevalence or consequences of sport specialization in Little League baseball players.
Hypothesis:
Sport specialization will be highly prevalent among Little League baseball players and specialization will be associated with worse throwing arm health.
Study Design:
Cross-sectional study.
Level of Evidence:
Level 3.
Methods:
A total of 246 Little League baseball players (male; N = 241; age, 9.5 ± 1.6 years) between 7 and 12 years old completed an anonymous, online questionnaire with their parent’s assistance. The questionnaire consisted of participant demographics and baseball participation information, including sport specialization status and the Youth Throwing Score (YTS), a valid and reliable patient-reported outcome measure for youth baseball players.
Results:
Only 29 (11.8%) players met the criteria for high specialization. Approximately one-third of all players (n = 77; 31.3%) reported participating in baseball year-round or receiving private coaching outside of their league (n = 81; 32.9%). Highly specialized athletes demonstrated worse scores on the YTS on average compared with low-specialization athletes (mean [SE]: 56.9 [1.6] vs 61.1 [1.2]; P = 0.01). Similarly, pitching in the previous year (P < 0.01) or traveling overnight regularly for showcases (P = 0.01) were associated with a worse score on the YTS.
Conclusion:
While the prevalence of high sport specialization was low among Little League baseball players, other behaviors associated with specialization such as year-round play and the receiving of private coaching were more common. Highly specialized Little League players demonstrated worse throwing arm health compared with low-specialization players.
Clinical Relevance:
Little League players and their parents may represent a potential target audience for dissemination campaigns regarding sport specialization.
Keywords: overuse injury, overhead athlete, training volume, pitching
Youth baseball is the second most popular boy’s youth team sport in the United States, with nearly 4 million participants in 2017.32 Despite the popularity of youth baseball and the known benefits of youth sport participation, there has been a concerning rise in the rates of certain overuse injuries among youth baseball players.16,22,33 For example, the infamous “Tommy John” surgery, also known as elbow ulnar collateral ligament (UCL) reconstruction, was once reserved for veteran pitchers nearing the end of their careers. However, 60% of current UCL reconstructions are performed on pitchers between 10 and 19 years old.9 Coupled with this alarming rise in youth athlete surgery rates is an increasing trend toward sport specialization.4
Sport specialization has been officially defined by the American Medical Association for Sports Medicine as “year-round intensive training in a single sport at the exclusion of other sports.”8 Using this definition, a 3-question sport specialization scale was developed by Jayanthi et al14 that classifies youth athletes as low, moderate, or highly specialized in a single sport. Recent reports utilizing this scale indicate that sport specialization is highly prevalent, with up to 37% of youth athletes from various sports classified as highly specialized.30 Specialization has also been widely identified as a risk factor for lower extremity overuse injury in high school–aged athlete populations.4 Among professional baseball players, specialization during childhood was associated with greater prevalence of injuries during their professional career.7,34 Participation in baseball for more than 8 months in a year was identified as a risk factor for shoulder or elbow injury among adolescent baseball pitchers.21 In a magnetic resonance imaging study of 23 asymptomatic Little League players, year-round participation in baseball and single-sport participation were associated with abnormal shoulder magnetic resonance imaging findings.13,24 However, there have been no reports on the prevalence or consequences of sport specialization in large samples of Little League baseball players.
The purpose of this study was to (1) quantify the prevalence of sport specialization in a large sample of Little League baseball players and (2) determine the association between sport specialization and throwing arm health in Little League baseball players. We hypothesized that sport specialization would be highly prevalent among Little League baseball players and that highly specialized players would have worse throwing arm health compared with low or moderately specialized players, independent of potential covariates.
Methods
Participants
This study was approved by the institutional review board at San Diego State University. Potential participants were recruited via emails to parents in 12 Southern California Little League organizations and asked to complete an anonymous, online questionnaire. Email recruitment took place between June and December 2019. To participate in the current study, the participant had to have competed on an organized youth baseball team in the previous 12 months and must have been between 7 and 12 years old at the time of survey completion. Parental consent and participant assent were obtained prior to participation. Parents were encouraged to help their child complete the child’s survey in case their child had any questions.
Questionnaire
The questionnaire consisted of 3 sections: (1) participant demographics (including age, sex, and year in school), (2) baseball participation information (including position, sport specialization status, and baseball participation volume), and (3) the Youth Throwing Score (YTS). Throwing arm health was assessed using the YTS, a 14-item patient-reported outcome measure that is validated and reliable for use in youth baseball players.2 Responses on the YTS generate a score between 14 and 70, with higher scores indicating better arm health.2 The questionnaire was designed to be completed in less than 10 minutes and was written at a Flesch-Kincaid grade level35 of 2.9.
Participants were classified as either low, moderate, or highly specialized based on their responses to the validated Jayanthi 3-point specialization scale, which was recently modified to improve its accuracy.19 The questions that comprise this scale are based on the definition of sport specialization as “year-round intensive training in a single sport at the exclusion of other sports” and include the following: “Have you only ever played one sport?,” “Have you quit other sports to focus on baseball?,” “Do you participate for more than 8 months out of the year in baseball?,” and “Do you consider baseball to be more important than your other sports?”14,19 A categorical classification system was used to assess the athletes’ responses to these sport specialization questions (yes = 1, no = 0), with a total score of 3 considered high specialization, a score of 2 considered moderate specialization, and a score of 0 or 1 considered low specialization.19
Statistical Analysis
Data were summarized by means and standard deviations, medians and interquartile ranges, and frequencies and proportions (%). Continuous variables were assessed for normality by calculating skewness/kurtosis values and via visual inspection of histograms. Univariate parametric analyses (independent t tests, 1-way analyses of variance) and bivariate correlations (Pearson r) were used to examine mean differences and associations of YTS based on variables of interest. Cohen d effect sizes (ESs) were calculated with 95% CIs for differences in YTS between categorical variables, with ES < 0.20 considered a small effect, ES = 0.50 considered a medium effect, and ES > 0.80 considered a large effect.15
Multivariable linear regression was used to examine the association between variables of interest and YTS. Least-squares mean estimates with standard errors were calculated for the variables of interest from the linear regression model, adjusting for covariates. Selecting the factors to include in the model consisted of determining any variable that was significant in the univariate analysis and was collected from all participants (ie, not pitcher specific). The final model consisted of specialization status, age, hours per week of baseball participation, pitching in the previous year, and regular overnight travel for showcases. Although significant in the univariate analysis, months per year of baseball participation was not included in the final model because it is one of the components of the 3-point specialization scale, thus already accounted for in the model.
The multivariable linear regression model was assessed to determine whether it met the assumptions of linear regression using the Global Validation of Linear Model Assumptions package23 in R and via visual inspection of quantile-quantile and residual plots. Comparisons of least-squares means estimates of YTS between levels of the variables of interest were conducted using post hoc pairwise Tukey honestly significance difference tests. Statistical significance was set at 2-sided a priori P < 0.05, and all analyses were performed in R statistical software (R Foundation for Statistical Computing).
Results
Overall, 246 Little League athletes (boys; N = 241; age, 9.5 ± 1.6 years old) fully completed the questionnaire and were included in the analysis. Participant demographics and sport participation characteristics are presented in Table 1. The age distribution of athletes by specialization level is presented in Figure 1. While highly specialized athletes (10.1 ± 1.4 years old) were significantly older than low-specialization athletes (9.3 ± 1.6 years old; P = 0.02), no differences were found in age between moderately specialized athletes (9.7 ± 1.7 years old) and high (P = 0.26) or low-specialization athletes (P = 0.09). Only 29 (11.8%) athletes were categorized as highly specialized using the modified Jayanthi 3-point specialization scale. Approximately one-third of all athletes (n = 77; 31.3%) reported participating in baseball year-round or receiving private coaching outside of their league (n = 81; 32.9%). Three-fourths (n = 184; 75.1%) of all athletes reported pitching at least once for their team in the previous year.
Table 1.
Participant demographics and sport participation characteristics (N = 246)
| Variable | N (%), Mean ± SD, or Median [IQR] |
|---|---|
| Sex | |
| Male | 241 (98.0) |
| Female | 5 (2.0) |
| Age, y | 9.5 ± 1.6 |
| Baseball start age, y | 5.3 ± 1.6 |
| Years of baseball participation | 4.2 ± 2.0 |
| Months/year of organized baseball | 7.2 ± 2.7 |
| Hours/week of organized baseball | 9 (6-15) |
| Primary position | |
| Pitcher | 38 (15.7) |
| Catcher | 44 (18.1) |
| First base | 36 (14.8) |
| Second base | 29 (11.9) |
| Shortstop | 34 (14.0) |
| Third base | 25 (10.3) |
| Outfield | 37 (15.2) |
| Specialization scale | |
| Low | 134 (54.5) |
| Moderate | 83 (33.7) |
| High | 29 (11.8) |
| Youth Throwing Score | 61.8 ± 7.7 |
| Travel overnight regularly for showcases | |
| Yes | 13 (5.3) |
| No | 233 (94.7) |
| Receive private coaching outside of league | |
| Yes | 81 (32.9) |
| No | 165 (67.1) |
| Participate in baseball >8 months per year | |
| Yes | 77 (31.3) |
| No | 169 (68.7) |
| Hours/week of organized baseball > Age | |
| Yes | 106 (44.5) |
| No | 132 (55.5) |
| Pitched in previous year | |
| Yes | 184 (75.1) |
| No | 61 (24.9) |
Figure 1.
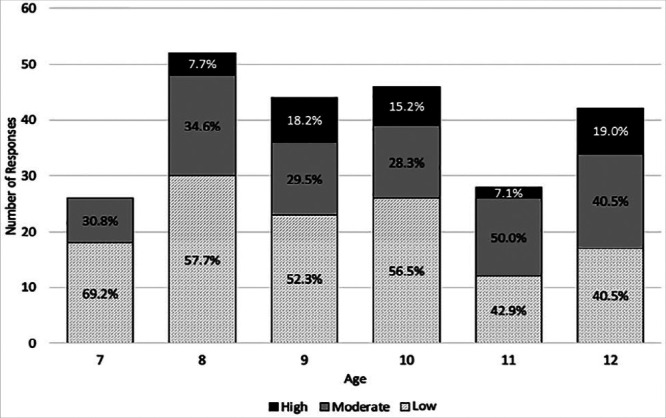
Age distribution of participants by specialization level.
Univariate differences in YTS and bivariate correlations with YTS are presented in Tables 2 and 3, respectively. Highly specialized athletes, on average, reported worse scores on the YTS (57.0 ± 9.2) compared with low-specialization athletes (63.1 ± 7.4; P < 0.001), with a medium ES (95%CI, 0.59 [0.2-1.0]). Athletes who reported pitching in the previous year also had lower (worse) mean YTS scores compared with nonpitchers (60.4 ± 8.0 vs 66.0 ± 4.8; P < 0.001) with a large ES (95%CI, 0.97 [0.7-1.3]). Worse scores on the YTS with a large ES were also observed among individuals who reported traveling overnight regularly for showcases (53.6 ± 10.4 vs 62.2 ± 7.6; ES [95%CI]: 0.84 [0.3-1.4]; P = 0.01). Increased age, months per year of baseball participation, and hours per week of organized baseball participation were all negatively correlated with worse scores on the YTS (Table 2).
Table 2.
Univariate differences in Youth Throwing Score based on categorical baseball participation characteristics
| Variable | Youth Throwing Score, Mean ± SD | Effect Size (95% CI) | P |
|---|---|---|---|
| Specialization | 0.59 (0.2 to 1.0) | <0.001 | |
| Low | 63.1 ± 7.4 | ||
| Moderate | 61.2 ± 7.1 | ||
| High | 57.0 ± 9.2 | ||
| Baseball >8 months | 0.36 (0.1 to 0.6) | 0.01 | |
| Yes | 59.8 ± 7.9 | ||
| No | 62.6 ± 7.5 | ||
| Pitched in previous year | 0.97 (0.7 to 1.3) | <0.001 | |
| Yes | 60.4 ± 8.0 | ||
| No | 66.0 ± 4.8 | ||
| Hours/week of baseball > Age | 0.13 (−0.1 to 0.4) | 0.33 | |
| Yes | 61.2 ± 7.7 | ||
| No | 62.2 ± 7.6 | ||
| Regular travel for showcases | 0.84 (0.3 to 1.4) | 0.01 | |
| Yes | 53.6 ± 10.4 | ||
| No | 62.2 ± 7.3 | ||
| Private baseball coaching | 0.19 (−0.1 to 0.5) | 0.17 | |
| Yes | 60.8 ± 7.8 | ||
| No | 62.2 ± 7.7 |
Table 3.
Correlations of continuous baseball participation characteristics with Youth Training Score
| Variable | Pearson r (95% CI) | P |
|---|---|---|
| Age, y | −0.23 (−0.35 to −0.10) | <0.001 |
| Baseball start age, y | −0.10 (−0.22 to 0.03) | 0.13 |
| Years of baseball participation | −0.12 (−0.24 to 0.01) | 0.07 |
| Months/year of organized baseball | −0.19 (−0.31 to −0.06) | 0.003 |
| Hours/week of organized baseball | −0.17 (−0.28 to −0.04) | 0.01 |
The results of the final multivariate model are presented in Table 4. After adjusting for all other factors in the model, highly specialized athletes, on average, demonstrated worse scores on the YTS compared with low-specialization athletes (Means [SE]: 56.9 [1.6] vs 61.1 [1.2]; P = 0.01). Similarly, pitching in the previous year (P < 0.01) or traveling overnight regularly for showcases (P = 0.01) were associated with a worse score on the YTS, even after adjusting for specialization, age, hours per week of baseball, pitching in previous year, and regular travel for showcases.
Table 4.
Least-squares mean estimates for Youth Throwing Score (YTS) based on multivariate linear regression
| YTS Least-Squares Mean Estimate (SE) | P a | |
|---|---|---|
| Sport specialization scale | ||
| Low | 61.1 (1.2) | 0.59b |
| Moderate | 60.1 (1.3) | 0.09c |
| High | 56.9 (1.6) | 0.01d |
| Pitcher as one of the positions | ||
| Yes | 57.5 (1.1) | <0.01 |
| No | 61.3 (1.4) | |
| Regular travel for showcases | ||
| Yes | 56.5 (2.0) | 0.01 |
| No | 62.2 (0.7) | |
Model includes specialization, age, hours per week of baseball, pitching in previous year, and regular travel for showcases. Adjusted R2 for model: 0.17.
Comparison between low and moderate specialization categories.
Comparison between moderate and high specialization categories.
Comparison between low and high specialization categories.
Discussion
Contrary to our hypothesis, the first key finding of this study indicated that specialization, as measured by the Jayanthi 3-point specialization scale, was not prevalent among this sample of Little League players. This finding is surprising, as the location where this study took place (Southern California) allows for year-round participation in outdoor sports, such as baseball. Additionally, previous surveys of youth athletes from a variety of sports have typically reported rates of specialization between 30% and 40%, which is considerably higher than the 11.8% of players who were classified as highly specialized in this study.5,14,28,30 One potential reason for this difference may be the fact that we surveyed a younger athlete population between the ages of 7 and 12 years, while prior research has focused on adolescent athletes.5,28,30 While approximately one-third (31.3%) of our population reported playing baseball year-round, which is one criterion of the Jayanthi 3-point specialization scale, our results indicate that they likely had not reached a level where they needed to make a decision to quit other sports and focus on baseball. Therefore, athletes in this age group and their parents may represent an ideal audience for dissemination campaigns regarding sport specialization in order to help provide them information as they decide whether to pursue a single sport at the exclusion of others. Noteworthy is that while very few athletes were classified as highly specialized, approximately one-third (32.9%) of athletes reported receiving private coaching outside of their league and nearly half (44.5%) reported participating in more hours per week of organized baseball than their age. Both findings are behaviors commonly reported by highly specialized athletes that have been linked with injury.3,11,36 This relationship with injury, however, was not found in the present study.14,25,30
The second key finding of this study was that specialization was associated with worse throwing arm health. That is, on average, highly specialized Little League players scored lower (worse) on the YTS compared with low-specialization athletes, even after adjusting for age and weekly training volume. To our knowledge, this is the first study to report the association of sport specialization, as measured by the Jayanthi 3-point scale, with a validated patient-reported measure of arm health specifically in Little League–aged athletes. Our results are in agreement with the many studies that have identified sport specialization as a risk factor for overuse injury among large cohorts of athletes from multiple sports4,12,14,18,27,28,30 and also with the few studies that have specifically examined baseball players.3,11,35 Arnold et al3 prospectively followed youth baseball players, aged 9 to 12 years, who self-classified as specialized or nonspecialized and found that the frequency of arm injuries was greater among specialized players compared with nonspecialized players.3 Similarly, sport specialization was associated with previous upper extremity overuse injury history and lower YTS score in a sample of 551 high school baseball players.29 Several retrospective surveys of professional baseball players have similarly found that players who specialized early in baseball (ie, prior to high school) were more likely to sustain injuries during their professional careers.11,34
Athletes who reported pitching as one of their positions or who reported traveling at least once a month for showcases or tournaments also demonstrated significantly lower (worse) scores on the YTS, even after adjusting for covariates. Two recent systematic reviews identified playing pitcher as a risk factor for injury in youth baseball, in agreement with our findings.1,20 The unique nature of the pitcher position and the repetitive stresses placed on the arm during pitching have been widely described, along with the increased risks associated with several pitching-related variables, such as innings per year, pitches per game, pitching through fatigue or pain, and pitch velocity.1,20,37 However, at the Little League level, selection to pitch may be more indicative of overall baseball ability and therefore these players may also be selected to play other throwing-intensive positions such as shortstop, which may also increase their overall throwing volume and injury risk. The evidence regarding showcase participation as a risk factor for injury in youth baseball is more equivocal, with 2 studies finding no association between showcase participation and injury,6,21 and 1 study finding an association between showcase participation and elbow pain in Little League players.31 Our results indicate that among Little League players, regular travel (at least once a month) for showcases or tournaments is associated with worse throwing arm health. While very few players in this study reported traveling regularly for showcases or tournaments (5.3%), this aspect of sport specialization is becoming more common in younger age groups. For example, a cursory internet search revealed camps and travel team rankings by Perfect Game and Under Armor for 10U teams,26,36 and large tournaments and showcases held by other organizations for as young as 6U teams.10
Several limitations are noteworthy in this study. First, this study was cross-sectional, therefore we were not able to determine causality between sport specialization and the other variables of interest with throwing arm health. Second, the questionnaire in this study was not validated, but it included previously validated items such as the Jayanthi 3-point specialization scale and the YTS. Third, we relied on parents to help assist their children in completing the survey because of their young age. This may have resulted in the youth athlete feeling pressured to not answer honestly to certain parts of the survey that they thought might disappoint or upset their parents. However, we felt that this potential risk was acceptable when surveying a younger population than has typically been less represented in sport specialization research. Additionally, we were not able to calculate a response rate because of our survey distribution methodology. All surveys were distributed by the 12 Little League administrators to parents in their organization. We felt that having the administrators send out the survey would improve our credibility with members of that organization. However, this also meant that we did not have direct control over the exact number of individuals who had access to the survey. Finally, we surveyed athletes from a limited geographic area in Southern California and most athletes’ parents were White/Caucasian, had a bachelor’s degree or higher education, and reported household incomes of more than US$100,001 per year (parent demographics and socioeconomic information provided in Appendix 1, available in the online version of this article). Therefore, our results may not be representative of Little League athletes nationwide and from difference demographic or socioeconomic backgrounds.
Conclusion
Sport specialization was less common among Little League baseball players, but other behaviors associated with specialization such as year-round play and the receiving of private coaching were more common. Even at this young age, highly specialized Little League players reported worse throwing arm health compared with low-specialization players. Athletes in this younger age range and their parents may represent a potential target for dissemination campaigns regarding sport specialization, as many have not chosen to specialize in a single sport yet but are still vulnerable to the potential risks of specialization. The Pitch Smart campaign, which was developed by USA Baseball and Major League Baseball, focuses on monitoring and limiting pitch counts in youth baseball.17 A similar campaign organized by baseball governing bodies may be a potential model for raising awareness among youth athletes and their parents regarding sport specialization.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_1941738120970956 for Prevalence and Consequences of Sport Specialization Among Little League Baseball Players by Eric G. Post, Michael D. Rosenthal, Andrew T. Pennock and Mitchell J. Rauh in Sports Health: A Multidisciplinary Approach
Footnotes
The following author declared potential conflicts of interest: E.G.P. received grants from Far West Athletic Trainers Association.
References
- 1. Agresta CE, Krieg K, Freehill MT. Risk factors for baseball-related arm injuries: a systematic review. Orthop J Sports Med. 2019;7:2325967119825557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmad CS, Padaki AS, Noticewala MS, Makhni EC, Popkin CA. The Youth Throwing Score. Am J Sports Med. 2017;45:317-324. [DOI] [PubMed] [Google Scholar]
- 3. Arnold AJ, Thigpen CA, Beattie PF, Kissenberth MJ, Tokish JM, Shanley E. Sport specialization and increased injury frequency in youth baseball players: a prospective study. J Athl Train. 2019;54:1115-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bell DR, Post EG, Biese K, Bay C, Valovich McLeod T. Sport specialization and risk of overuse injuries: a systematic review with meta-analysis. Pediatrics. 2018;142:e20180657. [DOI] [PubMed] [Google Scholar]
- 5. Bell DR, Post EG, Trigsted SM, Hetzel S, McGuine TA, Brooks MA. Prevalence of sport specialization in high school athletics: a 1-year observational study. Am J Sports Med. 2016;44:1469-1474. [DOI] [PubMed] [Google Scholar]
- 6. Chalmers PN, Sgroi T, Riff AJ, et al. Correlates with history of injury in youth and adolescent pitchers. Arthroscopy. 2015;31:1349-1357. [DOI] [PubMed] [Google Scholar]
- 7. Confino J, Irvine JN, O’Connor M, Ahmad CS, Lynch TS. Early sports specialization is associated with upper extremity injuries in throwers and fewer games played in Major League Baseball. Orthop J Sports Med. 2019;7:2325967119861101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. DiFiori JP, Benjamin HJ, Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48:287-288. [DOI] [PubMed] [Google Scholar]
- 9. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43:1770-1774. [DOI] [PubMed] [Google Scholar]
- 10. Exposure Baseball Events. Upcoming events. Published 2020. Accessed March 10, 2020. https://baseball.exposureevents.com/youth-baseball-events
- 11. Ginsburg RD, Steven R, Danforth N, et al. Patterns of specialization in professional baseball players. J Clin Sport Psychol. 2014;8:261-275. [Google Scholar]
- 12. Hall R, Barber Foss K, Hewett TE, Myer GD. Sport specialization’s association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil. 2015;24:31-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holt JB, Stearns PH, Bastrom TP, Dennis MM, Dwek JR, Pennock AT. The curse of the all-star team: a single-season prospective shoulder MRI study of Little League Baseball players. J Pediatr Orthop. 2020;40:e19-e24. [DOI] [PubMed] [Google Scholar]
- 14. Jayanthi NA, LaBella CR, Fischer D, Pasulka J, Dugas LR. Sports-specialized intensive training and the risk of injury in young athletes: a clinical case-control study. Am J Sports Med. 2015;43:794-801. [DOI] [PubMed] [Google Scholar]
- 15. Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. LaPrade RF, Agel J, Baker J, et al. AOSSM Early Sport Specialization Consensus statement. Orthop J Sports Med. 2016;4:2325967116644241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Major League Baseball. Pitch Smart. Accessed August 6, 2019. https://www.mlb.com/pitch-smart/risk-factors
- 18. McGuine TA, Post EG, Hetzel SJ, Brooks MA, Trigsted S, Bell DR. A prospective study on the effect of sport specialization on lower extremity injury rates in high school athletes. Am J Sports Med. 2017;45:2706-2712. [DOI] [PubMed] [Google Scholar]
- 19. Miller M, Malekian S, Burgess J, LaBella C. Evaluating a commonly used tool for measuring sport specialization in young athletes. J Athl Train. 2019;54:1083-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Norton R, Honstad C, Joshi R, Silvis M, Chinchilli V, Dhawan A. Risk factors for elbow and shoulder injuries in adolescent baseball players: a systematic review. Am J Sports Med. 2019;47:982-990. [DOI] [PubMed] [Google Scholar]
- 21. Olsen SJ, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912. [DOI] [PubMed] [Google Scholar]
- 22. Padaki AS, Ahmad CS. Can we reduce the epidemic of elbow injuries in youth throwers? J Orthop Sports Phys Ther. 2018;48:354-357. [DOI] [PubMed] [Google Scholar]
- 23. Peña EA, Slate EH. Global validation of linear model assumptions. J Am Stat Assoc. 2006;101:341-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pennock AT, Dwek J, Levy E, et al. Shoulder MRI abnormalities in asymptomatic Little League baseball players. Orthop J Sports Med. 2018;6:2325967118756825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pennock AT, Pytiak A, Stearns P, et al. Preseason assessment of radiographic abnormalities in elbows of Little League baseball players. J Bone Joint Surg Am. 2016;98:761-767. [DOI] [PubMed] [Google Scholar]
- 26. Perfect Game. 2020. Preseason 10U Rankings. Published 2020. Accessed March 10, 2020. https://www.perfectgame.org/Rankings/Team/Default.aspx?R=279
- 27. Post EG, Bell DR, Trigsted SM, et al. Association of competition volume, club sports, and sport specialization with sex and lower extremity injury history in high school athletes. Sports Health. 2017;9:518-523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Post EG, Biese KM, Schaefer DA, et al. Sport-specific associations of specialization and sex with overuse injury in youth athletes. Sports Health. 2020;12:36-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Post EG, Struminger AH, Hibberd EE. Sport specialization is associated with upper-extremity overuse injury in high school baseball players. J Shoulder Elbow Surg. 2020;29:1775-1782. [DOI] [PubMed] [Google Scholar]
- 30. Post EG, Trigsted SM, Riekena JW, et al. The association of sport specialization and training volume with injury history in youth athletes. Am J Sports Med. 2017;45:1405-1412. [DOI] [PubMed] [Google Scholar]
- 31. Register-Mihalik J, Oyama S, Marshall S, Mueller F. Pitching practices and self-reported injuries among youth baseball pitchers: a descriptive study. Athl Train Sports Health Care. 2012;4:11-20. [Google Scholar]
- 32. The Aspen Institute: Project Play. Sport participation and physical activity rates. Accessed August 27, 2019. https://www.aspenprojectplay.org/kids-sports-participation-rates
- 33. Trofa DP, Obana KK, Swindell HW, et al. Increasing burden of youth baseball elbow injuries in US emergency departments. Orthop J Sports Med. 2019;7:232596711984563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wilhelm A, Choi C, Deitch J. Early sport specialization: effectiveness and risk of injury in professional baseball players. Orthop J Sports Med. 2017;5:2325967117728922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Williamson JML, Martin AG. Analysis of patient information leaflets provided by a district general hospital by the Flesch and Flesch-Kincaid method. Int J Clin Pract. 2010;64:1824-1831. [DOI] [PubMed] [Google Scholar]
- 36. Under Armor Baseball Factory. Little League Events. Published 2020. Accessed March 10, 2020. https://www.baseballfactory.com/little-league-events/
- 37. Yang J, Mann BJ, Guettler JH, et al. Risk-prone pitching activities and injuries in youth baseball: Findings from a national sample. Am J Sports Med. 2014;42:1456-1463. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_1941738120970956 for Prevalence and Consequences of Sport Specialization Among Little League Baseball Players by Eric G. Post, Michael D. Rosenthal, Andrew T. Pennock and Mitchell J. Rauh in Sports Health: A Multidisciplinary Approach


