Abstract
Context:
Older adults are remaining active longer and continuing during later stages of life to participate in sports and activities that involve pivoting on 1 foot. The rate of anterior cruciate ligament (ACL) tears is increasing in people older than 40 years of age, which has caused a concomitant increase in the rate of surgical reconstruction.
Evidence Acquisition:
We searched the PubMed database for articles published in English between January 1980 and January 2018 using the terms anterior cruciate ligament injury, ACL injury, ACL tear, anterior cruciate ligament reconstruction, ACLR, older, older athlete, and elderly.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
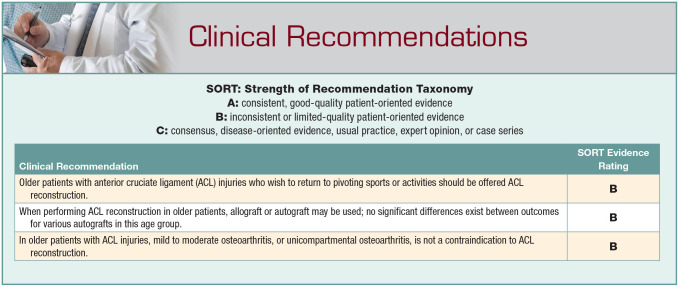
Nonoperative treatment with activity modification and physical therapy may be an appropriate option for nonathletes older than 40 years of age with physically low-demand lifestyles. For patients with injuries that are unresponsive to nonoperative treatment or athletes participating in physically demanding activities, ACL reconstruction can improve function and facilitate return to sports. When evaluating whether a patient is a candidate for surgery, numerous variables should be considered, such as timing, graft choice, and postoperative rehabilitation.
Conclusion:
Outcomes of ACL reconstruction in older athletes are similar to those of younger patients. To date, published evidence is inadequate to determine the long-term effects of nonoperative and operative treatment as well as the role of ACL reconstruction in the development of osteoarthritis in the older athlete.
Keywords: anterior cruciate ligament, injury, osteoarthritis, reconstruction
As the US population continues to age, an increasing number of older patients are sustaining sports-related injuries. Patients older than 40 years of age are remaining active and performing high-level athletic activities.3,28 With this increased participation in physical fitness and sports, there has been a concomitant increase in sports-related injuries. From 1990 to 2006, the rate of anterior cruciate ligament (ACL) reconstructions in patients older than 40 years of age increased by more than 200%.17 Many patients in this age group opt for surgical reconstruction to treat ACL injuries so they can return to their previous athletic activities.
In patients aged 18 to 35 years with ACL tears, reconstruction is recommended to reduce risks of chondral and meniscal injury and facilitate return to sports and activities.1 However, less is known about the treatment of ACL injuries in older patients. Salzler et al20 reviewed ACL tear treatment in patients older than 40 years of age and concluded that reconstruction is appropriate for active patients who wish to return to sports but conceded that more research is needed to determine the long-term effects of operative and nonoperative treatments. Toanen et al25 analyzed ACL reconstruction with hamstring autograft in patients older than 60 years of age and found that reconstruction restored anterior tibial stability and was associated with good functional recovery, with most patients returning to their preinjury activity level.
Epidemiology
The rates of ACL injuries have increased in older patients since the 1990s. Sanders et al21 showed that the incidence of ACL injury (per 100,000 person-years) increased in men aged 36 to 45 years from 77 in 1990-1994 to 100 in 2000-2005. Likewise, in men aged 46 years or older, the incidence increased from 10 in 1990-1994 to 24 in 2000-2005. A more dramatic change occurred in the incidence among women aged 36 to 45 years, who experienced an increase from 40 to 72 from 1990 to 2005, whereas the incidence for women aged 46 years or older increased from 6.1 to 23.21
In addition to increasing rates of ACL injury, there has been a concomitant increase in ACL reconstruction in older patients. More than 120,000 ACL reconstructions are performed annually in the United States,7,17 and this number continues to rise. Mall et al17 studied trends in ACL reconstruction in the United States and found that ACL reconstruction performed in patients aged 40 years or older increased from 1.7 per 100,000 person-years in 1994 to 7.6 per 100,000 person-years in 2006. Sanders et al21 conducted a population-based study from 1990 to 2010 and reported increasing incidence of ACL reconstruction for all age groups studied. They also showed an increase in the percentage of patients undergoing ACL reconstruction within 1 year of sustaining an ACL injury. In patients aged 36 to 45 years, the percentage of patients undergoing ACL reconstruction within 1 year of injury increased from 26% in 1990-1994 to 65% in 2000-2005. Similarly, the percentage of patients aged 46 years or older who underwent ACL reconstruction within 1 year of injury was 17% in 1990-1994 compared with 40% in 2000-2005.21
Evaluation
History
Any history of injury or surgery should be ascertained because patients may present with previous meniscal or chondral injury, as well as acute or chronic injuries. A thorough history of activity-induced knee pain, stiffness, swelling, mechanical symptoms (eg, locking or catching), exacerbating or alleviating factors, and the use of supportive walking aids should also be investigated and may provide insight into other conditions, such as degenerative osteoarthritis. It is also important to screen for other joint arthralgias to help elucidate any history of systemic inflammatory conditions. Additionally, it is critical to evaluate any patellofemoral symptoms, such as pain with patellar compression or anterior knee pain with ascending stairs, because these symptoms may influence graft choice and subsequent rehabilitation. Finally, the severity of “giving way” symptoms should be assessed and graded. It is important to note whether the “giving way” symptoms occur with walking, with light activity or moderate work, or with strenuous sports or heavy work. The impact of “giving way” episodes on activities of daily living can help determine whether to reconstruct the ACL. Older patients presenting with ACL injuries are not necessarily low-functioning patients. Many patients older than 40 years of age are continuing to participate in sports and high-functioning athletic activities13,28; therefore, recreational activities and the patient’s goals for physical activity should be discussed at the time of initial evaluation because these factors can influence treatment. Additionally, any symptoms of instability or “giving way” should be noted and factored into treatment decisions.14
Imaging
In patients older than 40 years of age, standing anteroposterior, lateral, and posteroanterior flexion radiographs should be obtained during the initial evaluation of ACL injuries. In younger patients, conventional radiographs may be used to assess overall alignment and evaluate for any bony abnormalities, fractures, or loose bodies; however, in the older population, radiographs are also important to evaluate for signs of degenerative osteoarthritis.20 In addition to conventional radiographs, magnetic resonance images are essential not only for confirming an ACL tear, but also for identifying concomitant ligamentous, meniscal, or cartilage injuries.1
Treatment Options
Nonoperative
Nonoperative treatment should be provided as an option for older patients with ACL tears, especially those with physically low-demand lifestyles and those who do not intend to return to pivoting sports. In addition to physical therapy, patients should avoid high-risk activities or sports that predispose them to instability episodes. Salzler et al20 reviewed ACL tear treatment in older patients and proposed an algorithm based on activity level, presence of degenerative osteoarthritis, and tear morphology (partial vs complete). They concluded that patients with partial tears, low-demand activity level, or moderate to severe osteoarthritis are candidates for nonoperative treatment with bracing, physical therapy, and activity modification.20
Several studies provide insight into outcomes of nonoperative treatment. Ciccotti et al8 studied 30 patients aged 40 to 60 years who underwent nonoperative treatment for ACL tears. These patients were all middle-aged, and approximately 50% of them sustained an ACL tear while skiing.8 Importantly, the authors noted that all patients were compliant with the rehabilitation protocol, had comprehensive health insurance, and were employed and able to financially afford continuing physical therapy.8 They reported satisfactory outcomes in 25 patients at a mean 7-year follow-up. In a study of 29 alpine skiers who underwent nonoperative treatment of magnetic resonance imaging–confirmed ACL tears at a mean age of 42 years, Hetsroni et al11 reported good functional outcomes and normal knee laxity at 2 years postinjury in patients who, within 6 to 12 weeks after the initial injury, demonstrated a negative Lachman test and a negative pivot-shift test. Exercises that improve or restore the kinetic chain and core strength may lead to improved function and better overall health in older patients.
Drawbacks of nonoperative treatment include difficulty or dissatisfaction with activity modification, which may not be tolerated by very active patients. In young athletes, nonoperative treatment is associated with increased risk of meniscal and cartilage injuries.2,4 Although more studies are needed to determine whether these effects also occur in older adults, it is reasonable to assume that older patients with instability episodes are at high risk of additional injuries.
Operative
Older patients with injuries that are unresponsive to nonoperative treatment or those who wish to participate in high-functioning athletic activities or pivoting sports may be candidates for surgery. ACL reconstruction is not indicated in the presence of advanced tricompartmental osteoarthritis because ACL reconstruction has been associated with progression of disease and increased pain.9 However, in patients with less severe osteoarthritis or unicompartmental disease, ACL reconstruction may provide knee stability and good functional outcomes.23 Shelbourne and Benner23 analyzed 53 patients with medial compartment osteoarthritis and found that ACL reconstruction provided good subjective results and stability at 10-year follow-up. Mild osteoarthritis is not a contraindication to ACL reconstruction; however, more research is needed to determine the benefit of ACL reconstruction in patients with moderate osteoarthritis. If moderate radiographic or arthroscopic evidence of arthritis is present, then patients should be advised to modify their activity level to avoid contact, pivoting, and repetitive high-loading sports.6 Several groups have studied operative versus nonoperative treatment of ACL injuries in older patients. Zysk and Refior29 evaluated 133 patients aged 40 to 59 years and found worse functional scores; worse Lachman, pivot-shift, and KT-1000 test results; and lower activity levels in the 31 patients treated nonoperatively. They also showed that increasing age was not associated with worse treatment outcomes, suggesting improvement with surgery regardless of age.29 In a value decision analysis, Seng et al22 evaluated 69 patients with a mean age of 53 years and found an expected value of operative treatment of 8.0 value units compared with 1.9 value units for nonoperative treatment. They concluded that surgery is the optimal treatment for ACL rupture in patients older than 40 years.22
Treatment Considerations
Timing
Timing of ACL reconstruction depends on multiple factors. Restoration of knee range of motion and quadriceps control are important goals before ACL reconstruction, regardless of age. Among older adults, variables such as work-related schedule limitations and family circumstances may be more important factors than among young athletes. These factors should be considered, along with the duration and likelihood of compliance with postoperative rehabilitation.
No studies have compared early versus delayed reconstruction in older patients with ACL tears. Although early reconstruction lowers risk of chondral and meniscal injury in young patients,1 this same association has not been adequately studied in athletes older than 35 years of age. Research is needed to determine the optimal timing of reconstruction in older athletes.
Graft Choice
Graft choice should involve a shared decision-making process with the patient because allograft and autograft have different risks and benefits. In older patients and nonathletes, allograft has been the traditional choice for ACL reconstruction; however, autograft may also be a good option. Kaeding et al12 analyzed differences in failure between allograft and autograft ACL reconstruction in 645 patients. They found that allograft had a failure rate 4 times higher than autograft, but when analyzing age groups, this failure rate was only 2% higher in patients older than 40 years of age.12 Although differences in failure rate based on graft selection exist in younger patients, several other studies have shown no difference in failure rates between autograft and allograft in patients older than 40 years of age.6,16 Importantly, these findings may be different in older athletes participating in higher-intensity, pivoting sports, such as basketball or soccer, and more research in this area may verify these differences.
Similarly, no significant differences for stability assessment and functional outcome scores have been reported between autograft types in older patients. Brown et al6 analyzed 627 patients older than 40 years (mean age, 49 years), of whom 71% underwent autograft ACL reconstruction (41% bone–patellar tendon–bone, 29% hamstring, 1% quadriceps). They found an overall graft failure rate of 1.9% at mean follow-up of 40 months and no differences between graft types and functional outcome scores or stability assessment.6
Graft Fixation
In the older athlete, bone quality may be a factor in determining optimal graft fixation technique. In a biomechanical study, Brand et al5 analyzed hamstring autograft fixation in cadaveric knees (mean age, 66 years) and found that soft tissue fixation strength using an interference screw was correlated with bone mineral density. They also showed that insertion torque was a useful predictor of graft fixation strength.5 If bone mineral density was less than 0.6 g/cm2, then fixation of a soft tissue graft with an interference screw would not provide enough strength to withstand activities of daily living.5
Conversely, extracortical fixation may reduce the risk of soft tissue graft fixation failure in osteopenic bone5,18 compared with interference screw fixation. In a cadaveric study, Domnick et al10 tested ACL soft tissue graft fixation and compared interference screw, extracortical button, and hybrid interference screw with extracortical button techniques in osteopenic bone. Hybrid fixation of ACL soft tissue grafts provided less vertical graft movement and higher load-to-failure than either technique (interference screw or extracortical button) alone.10 The aforementioned studies were performed in cadavers and should be interpreted accordingly. Further research is needed to determine whether these findings hold true in vivo.
Postoperative Rehabilitation
Accelerated rehabilitation programs may be more desirable in older athletes to facilitate return to work and family life; however, rehabilitation after ACL reconstruction may be prolonged, and the healing response may be less robust in older patients because of reduced ability to regain muscle strength and increased time needed to regain coordination.20 In addition, the less robust healing response in older patients may delay return to sport.13 When considering an accelerated rehabilitation program, graft selection and fixation must be carefully considered, because interference fixation of allograft and soft tissue grafts may require prolonged healing time. Rehabilitation protocols should focus on range of motion and regaining full extension because the risk of osteoarthritis is higher in patients who do not regain normal range of motion postoperatively.24 Initial exercises should consist of closed-chain movements and should focus on balance, core strength, and sport-specific biomechanics.19,26,27
Complications
In patients older than 40 years of age, complication rates after ACL reconstruction are similar to those of younger patients.6 In a systematic review, Brown et al6 analyzed complication rates in 17 studies and found similar rates between patients older than 40 years of age and younger patients. However, rates of hospital readmission may be higher in the older population, which may be attributable to a greater number of medical comorbidities. The most common surgical complications in the study included symptomatic hardware (5.1%), loss of knee range of motion (3.5%), and graft failure (1.9%).6 The most common medical complications included deep vein thrombosis (0.3%) and pulmonary embolism (0.2%).6 Lyman et al15 analyzed more than 70,000 patients who underwent ACL reconstruction between 1997 and 2006 and found a higher risk of 90-day readmission in patients older than 40 years of age compared with younger patients. Although overall complication rates may be similar in the older population, medical comorbidities should be thoroughly evaluated and preoperative risk stratification should be performed before ACL reconstruction.
Conclusion
Patients aged older than 40 years are remaining active and participating in high-level sports at later stages in life,3,28 which has led to an increase in ACL injuries in this age group.17 ACL reconstruction can improve function and enable return to sport in the older athlete, whereas activity modification and nonoperative treatment may be the preferred treatment in lower-functioning patients or nonathletes. Numerous treatment variables should be considered and discussed with the patient before surgery, such as timing, graft choice, and postoperative rehabilitation. Appropriately selected older patients may benefit from ACL reconstruction and have similar complications and outcomes as younger athletes.
Footnotes
The following authors declared potential conflicts of interest: B.A.Z. is a paid consultant for Vericel and J.H.W. has received royalties from Wolters Kluwer Health and Lippincott Williams & Wilkins.
References
- 1. American Academy of Orthopaedic Surgeons. Management of anterior cruciate ligament injuries. Accessed February 6, 2020. https://www.aaos.org/globalassets/quality-and-practice-resources/anterior-cruciate-ligament-injuries/anterior-cruciate-ligament-injuries-clinical-practice-guideline-4-24-19.pdf
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:275-281. [DOI] [PubMed] [Google Scholar]
- 3. Barrett G, Stokes D, White M. Anterior cruciate ligament reconstruction in patients older than 40 years: allograft versus autograft patellar tendon. Am J Sports Med. 2005;33:1505-1512. [DOI] [PubMed] [Google Scholar]
- 4. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med 2015;43:2966-2973. [DOI] [PubMed] [Google Scholar]
- 5. Brand JC, Jr, Pienkowski D, Steenlage E, Hamilton D, Johnson DL, Caborn DN. Interference screw fixation strength of a quadrupled hamstring tendon graft is directly related to bone mineral density and insertion torque. Am J Sports Med. 2000;28:705-710. [DOI] [PubMed] [Google Scholar]
- 6. Brown CA, McAdams TR, Harris AH, Maffulli N, Safran MR. ACL reconstruction in patients aged 40 years and older: a systematic review and introduction of a new methodology score for ACL studies. Am J Sports Med. 2013;41:2181-2190. [DOI] [PubMed] [Google Scholar]
- 7. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3:2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients. Results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315-1321. [DOI] [PubMed] [Google Scholar]
- 9. Clatworthy M, Amendola A. The anterior cruciate ligament and arthritis. Clin Sports Med 1999;18:173-198. [DOI] [PubMed] [Google Scholar]
- 10. Domnick C, Herbort M, Raschke MJ, et al. Anterior cruciate ligament soft tissue graft fixation in the elderly: is there a reason to use interference screws? A human cadaver study. Arthroscopy. 2017;33:1694-1700. [DOI] [PubMed] [Google Scholar]
- 11. Hetsroni I, Delos D, Fives G, Boyle BW, Lillemoe K, Marx RG. Nonoperative treatment for anterior cruciate ligament injury in recreational alpine skiers. Knee Surg Sports Traumatol Arthrosc. 2013;21:1910-1914. [DOI] [PubMed] [Google Scholar]
- 12. Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kinugasa K, Mae T, Matsumoto N, Nakagawa S, Yoneda M, Shino K. Effect of patient age on morphology of anterior cruciate ligament grafts at second-look arthroscopy. Arthroscopy. 2011;27:38-45. [DOI] [PubMed] [Google Scholar]
- 14. Legnani C, Terzaghi C, Borgo E, Ventura A. Management of anterior cruciate ligament rupture in patients aged 40 years and older. J Orthop Traumatol. 2011;12:177-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321-2328. [DOI] [PubMed] [Google Scholar]
- 16. Maletis GB, Chen J, Inacio MC, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry.Am J Sports Med. 2016;44:331-336. [DOI] [PubMed] [Google Scholar]
- 17. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363-2370. [DOI] [PubMed] [Google Scholar]
- 18. Nurmi JT, Sievänen H, Kannus P, Järvinen M, Järvinen TL. Porcine tibia is a poor substitute for human cadaver tibia for evaluating interference screw fixation. Am J Sports Med. 2004;32:765-771. [DOI] [PubMed] [Google Scholar]
- 19. Risberg MA, Holm I, Myklebust G, Engebresten L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87:737-750. [DOI] [PubMed] [Google Scholar]
- 20. Salzler MJ, Chang J, Richmond J. Management of anterior cruciate ligament injuries in adults aged >40 years. J Am Acad Orthop Surg. 2018;26:553-561. [DOI] [PubMed] [Google Scholar]
- 21. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44:1502-1507. [DOI] [PubMed] [Google Scholar]
- 22. Seng K, Appleby D, Lubowitz JH. Operative versus nonoperative treatment of anterior cruciate ligament rupture in patients aged 40 years or older: an expected-value decision analysis. Arthroscopy. 2008;24:914-920. [DOI] [PubMed] [Google Scholar]
- 23. Shelbourne KD, Benner RW. Isolated anterior cruciate ligament reconstruction in the chronic ACL-deficient knee with degenerative medial arthrosis. J Knee Surg. 2007;20:216-222. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Urch SE, Gray T, Freeman H. Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. Am J Sports Med. 2012;40:108-113. [DOI] [PubMed] [Google Scholar]
- 25. Toanen C, Demey G, Ntagiopoulos PG, Ferrua P, Dejour D. Is there any benefit in anterior cruciate ligament reconstruction in patients older than 60 years? Am J Sports Med. 2017;45:832-837. [DOI] [PubMed] [Google Scholar]
- 26. van Grinsven S, van Cingel RE, Holla CJ, van Loon CJM. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2010;18:1128-1144. [DOI] [PubMed] [Google Scholar]
- 27. Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21:225-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wroblewski AP, Amati F, Smiley MA, Goodpaster B, Wright V. Chronic exercise preserves lean muscle mass in masters athletes. Phys Sportsmed. 2011;39:172-178. [DOI] [PubMed] [Google Scholar]
- 29. Zysk SP, Refior HJ. Operative or conservative treatment of the acutely torn anterior cruciate ligament in middle-aged patients. A follow-up study of 133 patients between the ages of 40 and 59 years. Arch Orthop Trauma Surg. 2000;120:59-64. [DOI] [PubMed] [Google Scholar]