Supplemental digital content is available in the text.
Key Words: maternal, confidence, infant, utilization
Abstract
Objectives
To determine if maternal confidence affects emergency department (ED) utilization in the first year of life.
Methods
This retrospective cohort study examined the Maternal Confidence Questionnaire responses from a longitudinal birth cohort study and ED visits for these subjects across all Inova hospitals from January 2012 to July 2017 for full-term children 12 months or younger at the time of visit. Using logistic regression, maternal confidence, maternal race/ethnicity, age, education, parity, and insurance were evaluated against Emergency Severity Index acuity levels and ED visit frequency.
Results
Of 2429 participants in the longitudinal study, 316 subjects visited the ED and met inclusion criteria. Medicaid status was the main factor associated with any ED visit. Low maternal confidence did not correlate with more frequent or nonurgent ED visits. Higher maternal confidence scores were seen in Hispanic or Latino mothers and mothers with parity greater than 1. Hispanic or Latino mothers were more likely to have Medicaid and more likely to bring their child to the ED. Mothers with college education had lower maternal confidence scores, were less likely to visit the ED, but had higher acuity level visits.
Conclusions
Low maternal confidence did not correlate with frequent ED visits or nonurgent visits. Medicaid status was the main factor associated with any ED visit. Hispanic or Latino mothers had higher maternal confidence scores, were more likely to have Medicaid and more likely to bring their child to the ED.
Emergency department (ED) visits continue to increase at a rapid rate across the country. The 2017 National Hospital Ambulatory Medical Care Survey found that the annual number of visits in children younger than 15 years increased by 27% since 2007 with approximately 28.4 million ED visits.1,2 Infants younger than 12 months accounted for the group with the highest annual ED visit rate of 95.8 visits per 100 persons per year.2 Fever, cough, and abdominal pain were the main reasons for children visiting the ED.2
There are multiple factors that influence a caregiver's decision to bring their child to the ED. Studies have shown that factors can be related to the child or the parent. Sharma et al3 found several factors associated with increased total and nonurgent ED visits in infants younger than 1 year. These factors include Medicaid insurance, self-pay, Black race, rural region, presence of birth defects, and a nursery stay of longer than 2 days. Maternal factors that have been shown to play a role in increased nonurgent ED visits include younger maternal age, primiparous mothers, non-White race, and Medicaid insurance.4
The association between maternal confidence and ED visits has not been previously studied. Maternal confidence has been defined as the perception mothers have of their ability to care for and understand their children.5,6 Studies have shown that high maternal confidence and maternal competence are associated with low maternal parenting stress in newborn care.7 Factors, such as higher maternal education, greater family income, increased social support, and prior caretaking experience, correlated with higher confidence in mothers parenting premature infants at 4 and 8 months.6 The Maternal Confidence Questionnaire (MCQ) is a tool that was created over 30 years ago to understand the efficacy of an intervention in the Neonatal Intensive Care Unit (NICU) in mothers and infants at 8 months after they were discharged from the hospital.8 A higher score on the MCQ correlates with a mother feeling more competent. This tool has subsequently been validated in multiple studies and has been used to help further understand maternal confidence in correlation with different factors such as breastfeeding, social support, and maternal depression.8
The aim of this study was to determine if maternal confidence, as demonstrated by the MCQ, is associated with ED utilization in infants 12 months and younger. We hypothesized that lower maternal confidence is associated with increased ED utilization in children younger than 12 months. If maternal confidence does play a role, this could help us further understand the factors that influence a parent's decision to bring their children to the ED and potentially help us develop interventions at the level of the primary care physician to decrease ED utilization in this age group.
METHODS
Study Design/Setting
This study was a retrospective, cohort study that took place at 3 general and 2 pediatric Inova EDs within the Inova health system from January 2012 to July 2017. This health system serves approximately 1.74 million residents in a 3-county suburban area of Northern Virginia. Most participants were seen at the primary study institution, a Level I trauma center with approximately 45,000 annual pediatric ED visits and over 10,000 annual births.
Study Participants
All subjects were recruited into the longitudinal birth cohort study,“Inova's First 1000 Days of Life and Beyond Study,” examining the role of genetic and clinical factors in predicting childhood health outcomes (n = 2429, response rate 67%). Institutional review board approval (protocol ID 15-1804) was obtained, and recruitment began in 2012 with women at least 18 years of age recruited during their second trimester of pregnancy. All women provided written informed consent for herself and her child and were followed up longitudinally from childbirth through their child's first 2 years of life by means of longitudinal surveys every 6 months. Children 12 months or younger with 1 or more ED visits and had 6 month surveys completed by mothers were included. Exclusion criteria included children with prematurity (<37 weeks gestation) and chronic medical conditions, including syndromic conditions, metabolic or cardiac issues, epilepsy, cancer, and those requiring medical devices, such as gastrostomy or tracheostomy tubes because these conditions are likely to increase ED usage.
Data Collection
Information from longitudinal surveys completed at 6 months of life by the mother was collected and included self-reported maternal confidence scores measured by the MCQ and other demographic, socioeconomic and mental health data elements (maternal age, education, parity, race, ethnicity). The survey had to be completed within 2 months of the child being 6 months to be counted for timeline accuracy. Information regarding those children who also had an ED visit at 12 months or younger was retrospectively obtained from the Electronic Health Record (EHR). Data collected included maternal age at completion of 6 month survey, sex, ethnicity, race, mother's education, insurance status, number of ED visits, acuity of each visit and disposition. Ethnicity was categorized as: Hispanic or Latino, Not Hispanic or Latino. Race was categorized as: Asian, Black or African American, White or Caucasian, more than 1 race, all other races, missing/declined. Insurance status was categorized as: Medicaid/Family Access to Medical Insurance Security, Private (private, Kaiser, military, Exchange), data not available/not insured. Mother's education was categorized as: lower than 11th Grade, High School graduated/General Educational Development/Associates Degree, some college or higher level of education. Acuity was measured by the Emergency Severity Index (ESI) in which level 1 indicates immediate attention, 2 emergent, 3 urgent, 4 less urgent and 5 not urgent. In this study, visits were categorized as either “urgent visit” (ESI levels 1, 2 or 3) or “nonurgent visit” (ESI levels 4 or 5). High frequency ED visit was defined as more than 1 visit during the first year of life. If a child had more than 1 visit to the ED, the visit with the most severe acuity was used to categorize that child. Characteristics of those who went to the ED during the first year of life were analyzed.
The MCQ is a series of 14 questions relating to a mother's confidence in her role as a mother and her ability to understand and care for her child (see Text, Supplemental Digital Content 1, which describes MCQ score, http://links.lww.com/PEC/A741).8 A previous study examining maternal confidence found a mean MCQ score = 61 and was the score used in our study to determine low(er) versus high)er maternal confidence.9 Thus, mothers were categorized to either have low(er) maternal confidence if the total score was less than or equal to 61 or high(er) maternal confidence if the total score was greater than 61 with a total possible score of 70.
Data Analysis
SAS V.9.4 was used for all analyses. Logistic regression analysis was used to determine the general demographic and sociodemographic predictive variables of ED visit as well as maternal confidence. Statistical significance was defined by a P value less than 0.05. All outliers were identified using boxplot graphs using interquartile method and were removed before the detailed analysis.
Pearson's correlation coefficient was used to analyze the relationship between maternal confidence among ED mothers and the frequency and urgency of their ED visit(s). Pearson correlation coefficient greater than 0.7 was considered a strong correlation.
Among those who went to the ED, Wilcoxon rank-sum test was used to assess whether there is a difference in the MCQ score for mothers whose children get admitted to the hospital following an ED visit as compared with those whose children do not.
RESULTS
Of the 2429 study participants in the longitudinal, cohort study, there were 1413 who visited the ED. Subjects were excluded based on exclusion criteria and availability of data elements of interest (ie, demographics, insurance information, MCQ scores) leaving a total of 316 (Fig. 1).
FIGURE 1.
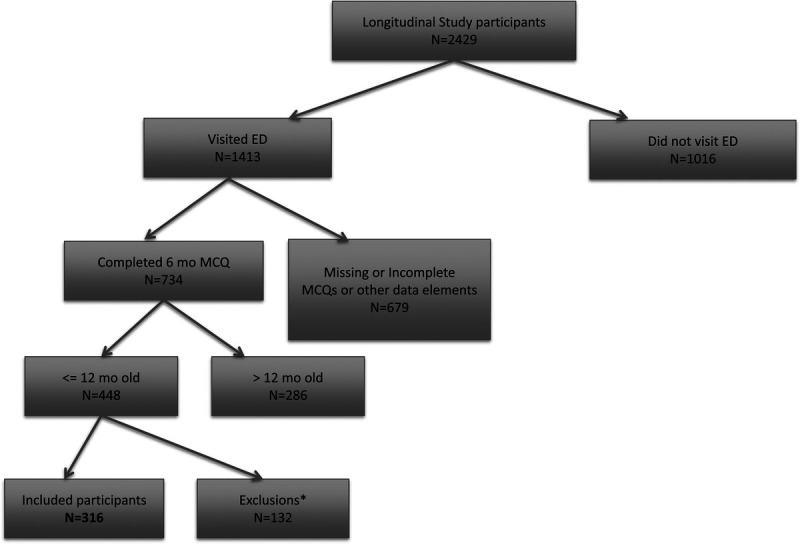
Patient selection criteria.
The demographic information for ED participants is shown in Table 1. Among the 316 children who visited the ED during the first year of life, 53.8% were male, mean age of mother was 30 years, 52.2% had mothers who were of Hispanic or Latino ethnicity, 75.6% of mothers had a high school degree or higher and 53.8% were covered by Medicaid. Of participants with urgent v. nonurgent ED visits, 156 had an urgent visit (ESI levels 2 or 3) and 160 had nonurgent visits (ESI levels 4 or 5). There were no participants with an ESI level 1 visit.
TABLE 1.
Demographic Characteristics of ED Subjects within Inova Health System, 2012–2017
| Characteristics | ED, n = 316 |
|---|---|
| Male | 170 (53.8%) |
| Mother's ethnicity | |
| Hispanic or Latino | 165 (52.2%) |
| Not Hispanic or Latino | 151 (47.8%) |
| Mother's race | |
| Asian | 5 (1.6%) |
| Black or African-American | 5 (1.6%) |
| More than 1 race | 14 (4.4%) |
| All other races* | 155 (49.1%) |
| White or Caucasian | 81 (25.6%) |
| Unknown, declined | 56 (17.7%) |
| Mother's age: | |
| Mean | 30 ± 5 |
| Mother's education: | |
| <11th Grade | 77 (24.4%) |
| High school graduated/GED/Associates degree | 64 (20.3%) |
| Some college or higher level of education | 175 (55.4%) |
| Insurance status: | |
| Medicaid/FAMIS | 170 (53.8%) |
| Private† | 146 (46.2%) |
| Data not available/not insured | 0 (0%) |
| ESI level: | |
| Level 1–3—urgent‡ | 156 (49.4%) |
| Level 4–5—nonurgent | 160 (50.6%) |
*All other races include “do not know/not sure,” “Native Hawaiian or Other Pacific Islander,” “American Indian or Alaska Native.”
†Includes Private, Kaiser, Military, Exchange.
‡There were no ESI level 1 visits.
GED, general educational development; FAMIS, Family Access to Medical Insurance Security.
In this study, we did not find a significant relationship between maternal confidence and ED visits. The mean MCQ score for ED patients was 63.2 and range of scores was 45 to 70. Low(er) maternal confidence did not correlate with frequent ED visits (r = −0.15) or nonurgent visits (r = −0.0147) (Table 2). Hispanic or Latino mothers (P = 0.0092) and mothers with higher parity (P = 0.0488) were more likely to have higher maternal confidence. Mothers with any college education were less likely to have high maternal confidence (P = 0.0026) (Fig. 2). Maternal confidence was not associated with ED visits (P = 0.2804), having a pediatrician (P = 0.0788), hospital admission (P = 0.0768), or Medicaid insurance (P = 0.2537) (Table 3). Additional factors associated with ED visits and urgent visits are shown.
TABLE 2.
Correlations between Maternal Confidence and Nonurgent and High-frequency ED Visits
| Variables | Relationship | Pearson’s r |
|---|---|---|
| Maternal confidence and nonurgent visit | No correlation | −0.0147 |
| Maternal confidence and high-frequency visits (>1) | No correlation | −0.1524 |
Pearson’s r indicates Pearson correlation coefficient.
FIGURE 2.
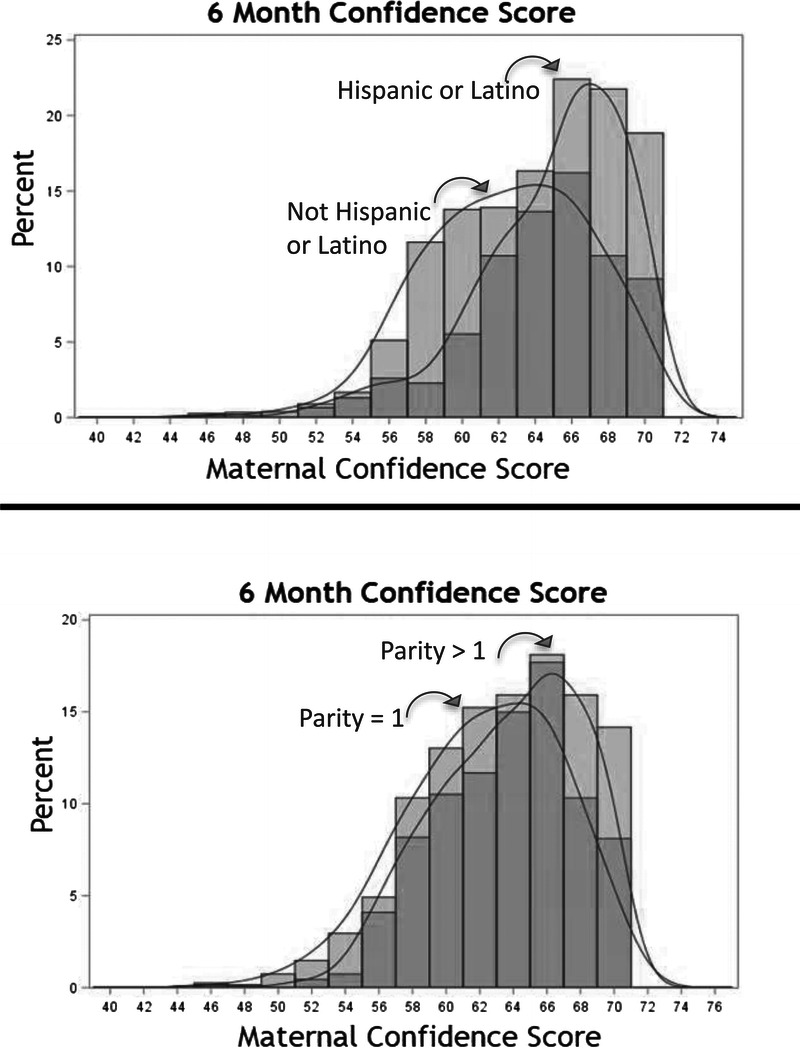
6 month maternal confidence scores according to ethnicity and parity.
TABLE 3.
Factors Associated with Maternal Confidence, Medicaid and ED/urgent visits
| Maternal confidence | ||
|---|---|---|
| Variable | Relationship | P |
| Hispanic or Latino mother | Positive | 0.0092 |
| Mother has any college education | Negative | 0.0026 |
| Mother's parity > 1 | Positive | 0.0488 |
| ED visit | None | 0.2804 |
| Has a pediatrician | None | 0.0788 |
| Hospital admission | None | 0.0768 |
| Medicaid | None | 0.2537 |
| Medicaid | ||
| Variable | Relationship | P |
| ED visit | Positive | <0.0001 |
| Hispanic or Latino mother | Positive | <0.0001 |
| Mother has any college education | Negative | <0.0001 |
| Mother's parity > 1 | Positive | 0.0096 |
| Older mother | Negative | 0.0013 |
| ED visit | ||
| Variable | Relationship | P |
| Hispanic or Latino mother | Positive | <0.0001 |
| Mother has any college education | Negative | 0.0008 |
| Mother's parity > 1 | None | 0.3395 |
| Older mother | None | 0.0518 |
| Urgent ED visit | ||
| Variable | Relationship | P |
| Mother has any college education | Positive | 0.0008 |
| Mother's parity > 1 | Positive | 0.0035 |
| Older mother | None | 0.3305 |
Factors associated with Medicaid insurance were also analyzed (Table 3). Medicaid status was the most significant factor associated with an ED visit (P < 0.0001, adjusted odds ratio, 7.290; confidence interval, 3.755–14.153) and high frequency ED visits (P = 0.0164, adjusted odds ratio, 2.545; confidence interval, 1.187–5.457). Although ED visit could be predicted by a few variables (Hispanic or Latino mother, no college) that were significantly associated, these variables were not significant in the binary logistic regression analyses when Medicaid was included.
DISCUSSION
This is the first study to look at the relationship between maternal confidence and ED visit rates. We hypothesized that having lower maternal confidence would be associated with increased ED utilization in children younger than 12 months. Our hypothesis, however, was not supported. Lower maternal confidence did not correlate with frequent ED use or with nonurgent ED visits. We did find that Medicaid status was the main factor associated with ED visits as well as high frequency ED visits.
In this study, maternal confidence was measured using a previously validated tool called the Maternal Confidence Questionnaire. Although this tool has not been used before in the ED setting, it has been used to further understand the relationships between maternal confidence and maternal behaviors and skills in other clinical settings, including the NICU and the newborn period.6–8 A higher MCQ score correlates with a mother feeling more competent in caring for her child. This survey tool was 1 component of a larger, longitudinal birth cohort study examining mothers and their children for the first 2 years of life, and its use was novel in examining the relationship between maternal confidence and ED utilization in infants.
Interestingly, we found that mothers with a college or higher level of education compared with those with only a high school education or less had lower MCQ scores. It is not clear why more educated mothers who bring their child to the ED would have lower scores as previous studies have shown higher maternal education correlating with higher MCQ scores.6 The severity of illness may have been a factor in the decision for these mothers to bring their child to the ED because they were less likely to visit the ED but more likely to have a higher acuity visit. Not surprisingly, higher parity as previously shown was associated with higher MCQ scores.6
When examining ethnicity we found that Hispanic or Latino mothers had higher MCQ scores compared to not Hispanic or Latino mothers. One factor that may contribute to higher MCQ scores among Hispanic or Latino mothers is increased social support within the household. Increased social support, as measured by NET-HELP which is a scale that estimates the percent of time family members and friends assist the mother with housework and infant care, has been found to have a positive correlation with increased maternal confidence.6 Other studies have described the importance of social support for Latino mothers for low-birth-weight infants as well as for children with illness and needing medical care.10,11 Specific examples of social support within Hispanic or Latino families was demonstrated in a study which looked at factors associated with nonurgent use of the pediatric ED among Hispanic or Latino families.12 Focus groups were held, and all of the parents described efforts to treat the child's symptoms at home before seeking care from a healthcare professional as well as asking neighbors for advice and use of natural medicine and seeking advice from family and friends who were still living in their country of origin.12
Healthcare access and cultural differences in understanding common symptoms could explain why we found that Hispanic or Latino mothers were more likely to bring their child to the ED. Barriers or perceived barriers to accessing health care including lack of health insurance, cost of care, long wait times in clinic or for an appointment, and perception that they would receive better care in ED have been described among Hispanic or Latino immigrants.13–15 Healthcare disparities in Hispanic or Latino families and racial/ethnic differences reporting no usual source of care continue to exist.16,17 Additionally, Taveras et al18 found that Latino parents were more likely to use the ED to manage febrile children, and Rupe et al19 found that Hispanic ethnicity was the strongest predictor for fever worry.
In our study, we found that Hispanic or Latino mothers were more likely to have Medicaid, the main factor associated with ED visits. Although ethnicity was not significantly associated with ED use after adjusting for insurance status in our study, a recent pediatric study found that independent risk factors for recurrent ED use included younger age of child, Black or Hispanic race or ethnicity, and public health insurance.20
As mentioned previously, maternal factors, such as younger maternal age, primiparous mothers, non-White race, and Medicaid insurance have all been found to be associated with nonurgent ED visits.4 In addition, many studies have demonstrated the association between maternal depression and ED visits. Grupp-Phelan et al21 found that almost 1 in 5 mothers who brought their children to a pediatric ED for nonurgent visits had a positive screen for depression. Additional studies have found that having at least 1 depressed parent is associated with a greater rate of ED visits across all age groups.22 Interestingly, a recent study showed an association between current postpartum anxiety and depressive disorders and maternal self-confidence. Although a different maternal self-confidence scale was used, they found that women with a previous history of depression or anxiety scored lower in maternal self-confidence.23 This was not examined in our study but would be worthy of exploring further.
There are several limitations with our study. The first limitation is generalizability. The study health system serves 3 different counties with approximately 2 million residents. Approximately 496,000 children in Virginia are enrolled in Medicaid, and rates of uninsured residents in the region are near or above Virginia's average.24,25 The Hispanic or Latino population makes up approximately 18.1% of the population in this region which is similar to the United States as a whole.26 Only the pediatric and general emergency departments within the health system were included in the study. The majority of study participants were seen in the pediatric emergency department at the study institution which is the largest tertiary care hospital in the region.27 We excluded urgent care visits as ESI levels are not assigned to patients. In addition, not all mothers who gave birth at the study institution consented to the original longitudinal, cohort study. It is possible that families that choose to take part in such a study may not be representative of the entire population of mothers giving birth at Inova.
An additional limitation with our study is the use of MCQ scores in this study population and our definition of low versus high maternal confidence. The MCQ scores have only been used in the NICU/newborn setting and not in an ED setting in which patients are being evaluated for acute illness and injury. However, it was felt that using this tool could add novel and valuable information when looking at predictors for ED utilization among infants. The MCQ is described as being “unidimensional with a higher score indicating a higher perceived competence.”8 We chose to analyze scores as dichotomous rather than continuous variables, which may have affected our results, but felt this would help streamline its impact on ED usage and provide a new perspective on using the tool. One study assessing the maternal confidence of first-time mothers found a total mean MCQ of 61 and another study assessing the maternal confidence of Latina mothers in the care of full term low birth weight (LBW) infants found the total mean MCQ of 55.4.9,10 Our total mean MCQ was higher at 63.2 and thus, our lower MCQ scores may still represent relatively high maternal confidence.
Lastly, we did not examine the father's role in the original longitudinal, cohort study or current study. We also did not determine if it was the father or another guardian who brought the child to the ED. It is possible that a father's confidence in caring for a child could influence the decision to bring a child to the ED.
This is the first study to examine the relationship between maternal confidence and ED visit rates. Although we did not find an association between maternal confidence and both frequent and nonurgent ED utilization, we would recommend further studies using the MCQ. Further directions include studying the relationship between health literacy and maternal confidence as well as depression and maternal confidence as both affect ED utilization. In addition, further use of MCQ scores could potentially help identify mothers who may need additional support to assist with making appropriate health care decisions and examine the father's role with these decisions, and determine how maternal confidence plays a role in other clinical settings, including primary care offices, urgent care centers and care of premature, medically complex children.
Supplementary Material
Footnotes
Disclosure: The authors declare no conflict of interest.
This work was supported by the Inova Research Seed Grant.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.pec-online.com).
Contributor Information
Jina Giusto, Email: jinahyun@gmail.com.
Megan Anton, Email: khandanbarani.meg@gmail.com.
Sabrina Gaiazov, Email: SabrinaAli65@gmail.com.
Kathi Huddleston, Email: kathihuddleston@cox.net.
Shira Levy, Email: Shira.Levy@inova.org.
Alma Fuller, Email: afuller9@gmu.edu.
Suchitra Hourigan, Email: suchihourigan@googlemail.com.
John Niederhuber, Email: jniederhuber@msn.com.
REFERENCES
- 1.Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. Natl Health Stat Report. 2010:1–31. [PubMed] [Google Scholar]
- 2.National Hospital Ambulatory Medical Care Survey: 2017 Emergency Department Summary Tables. Available at: https://www.cdc.gov/nchs/data/nhamcs/web_tables/2017_ed_web_tables-508.pdf. CDC Web site. Accessed November 6, 2020.
- 3.Sharma V Simon SD Bakewell JM, et al. Factors influencing infant visits to emergency departments. Pediatrics. 2000;106:1031–1039. [DOI] [PubMed] [Google Scholar]
- 4.Pomerantz WJ Schubert CJ Atherton HD, et al. Characteristics of nonurgent emergency department use in the first 3 months of life. Pediatr Emerg Care. 2002;18:403–408. [DOI] [PubMed] [Google Scholar]
- 5.Gross D, Rocissano L, Roncoli M. Maternal confidence during toddlerhood: comparing preterm and fullterm groups. Res Nurs Health. 1989;12:1–9. [DOI] [PubMed] [Google Scholar]
- 6.Zahr LK. The relationship between maternal confidence and mother-infant behaviors in premature infants. Res Nurs Health. 1991;14:279–286. [DOI] [PubMed] [Google Scholar]
- 7.Liu CC Chen YC Yeh YP, et al. Effects of maternal confidence and competence on maternal parenting stress in newborn care. J Adv Nurs. 2012;68:908–918. [DOI] [PubMed] [Google Scholar]
- 8.Badr LK. Further psychometric testing and use of the Maternal Confidence Questionnaire. Issues Compr Pediatr Nurs. 2005;28:163–174. [DOI] [PubMed] [Google Scholar]
- 9.Russell K. Maternal Confidence of First-time Mothers during their Child's Infancy. Dissertation, Georgia State University, 2006. Available at: https://pdfs.semanticscholar.org/4222/ca99ea44c7e669c5d571aebdd4612b45a508.pdf. Accessed November 20, 2020.
- 10.Zahr LK. The confidence of Latina mothers in the care of their low birth weight infants. Res Nurs Health. 1993;16:335–342. [DOI] [PubMed] [Google Scholar]
- 11.Fry-Bowers EK Maliski S Lewis MA, et al. The association of health literacy, social support, self-efficacy and interpersonal interactions with health care providers in low-income Latina mothers. J Pediatr Nurs. 2014;29:309–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grigg A Shetgiri R Michel E, et al. Factors associated with nonurgent use of pediatric emergency care among Latino families. J Natl Med Assoc. 2013;105:77–84. [DOI] [PubMed] [Google Scholar]
- 13.Zambrana RE Ell K Dorrington C, et al. The relationship between psychosocial status of immigrant Latino mothers and use of emergency pediatric services. Health Soc Work. 1994;19:93–102. [DOI] [PubMed] [Google Scholar]
- 14.Chan T Krishel S Bramwell K, et al. Survey of illegal immigrants seen in an emergency department. West J Med. 1996;164:212–216. [PMC free article] [PubMed] [Google Scholar]
- 15.Berdahl T Owens PL Dougherty D, et al. Annual report on health care for children and youth in the United States: racial/ethnic and socioeconomic disparities in children's health care quality. Acad Pediatr. 2010;10:95–118. [DOI] [PubMed] [Google Scholar]
- 16.Calvo R, Hawkins SS. Disparities in quality of healthcare of children from immigrant families in the US. Matern Child Health J. 2015;19:2223–2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zewde N, Berdahl T. Children's Usual Source of Care: Insurance, Income, and Racial/Ethnic Disparities, 2004–2014. In: Statistical Brief (Medical Expenditure Panel Survey (US)) [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2001–. STATISTICAL BRIEF #501; 2017. [PubMed] [Google Scholar]
- 18.Taveras EM, Durousseau S, Flores G. Parents' beliefs and practices regarding childhood fever: a study of a multiethnic and socioeconomically diverse sample of parents. Pediatr Emerg Care. 2004;20:579–587. [DOI] [PubMed] [Google Scholar]
- 19.Rupe A, Ahlers-Schmidt CR, Wittler R. A comparison of perceptions of fever and fever phobia by ethnicity. Clin Pediatr. 2010;49:172–176. [DOI] [PubMed] [Google Scholar]
- 20.Alpern ER Clark AE Alessandrini EA, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21:365–373. [DOI] [PubMed] [Google Scholar]
- 21.Grupp-Phelan J, Whitaker RC, Naish AB. Depression in mothers of children presenting for emergency and primary care: impact on mothers' perceptions of caring for their children. Ambul Pediatr. 2003;3:142–146. [DOI] [PubMed] [Google Scholar]
- 22.Sills MR Shetterly S Xu S, et al. Association between parental depression and children's health care use. Pediatrics. 2007;119:e829–e836. [DOI] [PubMed] [Google Scholar]
- 23.Reck C Noe D Gerstenlauer J, et al. Effects of postpartum anxiety disorders and depression on maternal self-confidence. Infant Behav Dev. 2012;35:264–272. [DOI] [PubMed] [Google Scholar]
- 24.Verité Healthcare Consulting . Community Health Needs Assessment Inova Fairfax Medical Campus. Available at: https://www.inova.org/sites/default/files/about-inova/Inova%20in%20the%20Community/2016-IFH-CHNA.pdf. Inova Web site. Accessed April 30, 2020.
- 25.American Academy of Pediatrics . MEDICAID FACTS Virginia. Available at: https://downloads.aap.org/AAP/PDF/federaladvocacy_medicaidfactsheet_virginia.pdf. AAP Web site. Accessed April 30, 2020. [Google Scholar]
- 26.US Census Bureau . QuickFacts: Fairfax County, Virginia; United States. Available at: https://www.census.gov/quickfacts/fact/table/fairfaxcountyvirginia,US/PST045219. US Census Bureau Web site. Accessed April 30, 2020.
- 27.Inova Health Systems . Inova Fairfax Medical Campus Quality Report. Available at: https://stg.inova.org/upload/docs/Quality/IFMC-quality-report.pdf. Inova Web site. Accessed April 30, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


