Abstract
Introduction
This is an overall review on mindfulness-based interventions (MBIs).
Sources of data
We identified studies in PubMed, EMBASE, CINAHL, PsycINFO, AMED, Web of Science and Google Scholar using keywords including ‘mindfulness’, ‘meditation’, and ‘review’, ‘meta-analysis’ or their variations.
Areas of agreement
MBIs are effective for improving many biopsychosocial conditions, including depression, anxiety, stress, insomnia, addiction, psychosis, pain, hypertension, weight control, cancer-related symptoms and prosocial behaviours. It is found to be beneficial in the healthcare settings, in schools and workplace but further research is warranted to look into its efficacy on different problems. MBIs are relatively safe, but ethical aspects should be considered. Mechanisms are suggested in both empirical and neurophysiological findings. Cost-effectiveness is found in treating some health conditions.
Areas of controversy
Inconclusive or only preliminary evidence on the effects of MBIs on PTSD, ADHD, ASD, eating disorders, loneliness and physical symptoms of cardiovascular diseases, diabetes, and respiratory conditions. Furthermore, some beneficial effects are not confirmed in subgroup populations. Cost-effectiveness is yet to confirm for many health conditions and populations.
Growing points
Many mindfulness systematic reviews and meta-analyses indicate low quality of included studies, hence high-quality studies with adequate sample size and longer follow-up period are needed.
Areas timely for developing research
More research is needed on online mindfulness trainings and interventions to improve biopsychosocial health during the COVID-19 pandemic; Deeper understanding of the mechanisms of MBIs integrating both empirical and neurophysiological findings; Long-term compliance and effects of MBIs; and development of mindfulness plus (mindfulness+) or personalized mindfulness programs to elevate the effectiveness for different purposes.
Keywords: mindfulness-based interventions, biopsychosocial health, safety, ethics, compliance, mechanisms
Mindfulness and mindfulness-based interventions
Mindfulness is a moment-by-moment awareness of thoughts, feelings, bodily sensations and surrounding environment. Being mindful is related to be open, nonjudgmental, friendly, curious, accepting, compassionate and kind.1 Mindfulness practices aim to cultivate mindfulness state. These practices can be formal (e.g. breathing, sitting, walking, body scan) or informal (e.g. mindfulness in everyday life). Many mindfulness-based intervention (MBI) programmes have been established. Among all the MBIs, mindfulness-based stress reduction (MBSR), which was launched by Jon Kabat-Zinn in 1979,2 and mindfulness-based cognitive therapy (MBCT) by Segal, Teasdale and Williams based on MBSR,3,4 are the two most widely adopted MBIs. These two programmes include eight weekly mindfulness sessions with one-day retreat.
Mindfulness is rooted in Buddhist traditions. However, it has become popular in recent years among various secular populations in healthcare, educational and workplace settings: from pre-school children to older adults across the world. Publications on mindfulness have increased dramatically in the recent decade. The publications on mindfulness is starting to be more comparable to publications on cognitive behavioural therapy (CBT), which is one of the most widely used psychotherapies (Fig. 1).
Fig. 1.
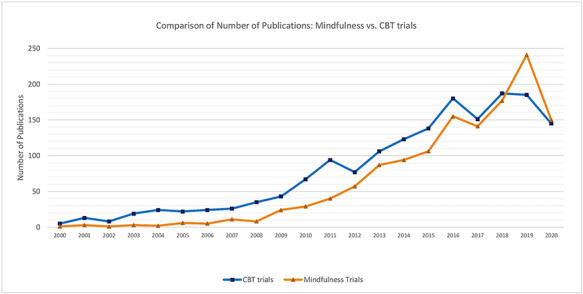
Comparison on number of publications: mindfulness vs. CBT trials (by August 2020) [Note: Search terms included (‘mindful* or meditate*’ AND ‘trial or random or random* control* trial*’); (‘cognitive behavioural therapy or cognitive behavioural therapy or CBT’ AND ‘trial or random or random* control* trial*’) in Title; Databases included MEDLINE, EMBASE and PsycINFO.]
Methods used for identifying relevant evidence
Literature in English was searched in MEDLINE, EMBASE, CINAHL, PsycInfo, AMED, Web of Science and Google Scholar using keywords including ‘mindfulness’, ‘meditation’ and ‘review’, ‘meta-analysis’ or their variations, with no restrictions on the year of publication. The search was conducted in July 2020. In choosing evidence, these general principals were applied: (i) published in more recent years if similar reviews were identified; (ii) included randomized controlled trials or meta-analysis in the review; (iii) presented with more conclusive conclusions. Literature with other types of study design (e.g. randomized controlled trials, cohorts, cross-sectional studies) were also manually searched and included when no systematic review was found or when considered as appropriate. However, while it was intent to include all important literature in a certain area, the review might not exhaust all relevant literature but had only selected key references of interest that we thought to be most pertinent and insightful for a specific topic.
Effects on mental health
MBIs have been shown to be efficacious in improving some of the common mental health problems.5
Depression and anxiety
For depression and anxiety, the efficacy of MBIs is sufficiently confirmed with meta-analyses demonstrating moderate to strong effect sizes for the reduction of the two conditions.6–8 The effects were also applicable during pregnancy, where a systematic review showed that MBIs helped reducing perinatal anxiety of moderate to large magnitude; however, the effects were less consistent in terms of reducing perinatal depression.9 The trending web-based interventions on mindfulness have also shown effectiveness in reducing depression and anxiety among people diagnosed with anxiety disorders as well.10 It was unclear, however, whether the benefits of mindfulness practices as a stand-alone intervention still exist, as it is difficult to dismantle the effects from social interaction and psychoeducation, which are the other components integrated in many MBIs (e.g. group MBCT), from standalone mindfulness practices. Therefore, a recent meta-analyses11 of 18 eligible studies investigated the gap, and has demonstrated that even mindfulness practice itself (e.g. breathing space, body scan, sitting meditation, soundscan) had small to medium effects on both anxiety (SMD = 0.39; CI: 0.22, 0.56; PI: 0.07, 0.70; P < .001, I2 = 18.90%) and depression (SMD = 0.41; CI: 0.19, 0.64; PI: −0.05, 0.88; P < .001; I2 = 33.43%).
Stress
Current evidence overall supports a moderate effect of MBIs on reducing stress; however, more robust studies are needed to make clear conclusions among different populations. A meta-analysis of five randomized control trials tested the effects of MBIs on cortisol levels, a stress-mediated hormone, and found that there may be a beneficial effect in healthy adult populations.12 Yet, the overall effect size was moderately low (g = 0.41; P = 0.025).12 On the other hand, another meta-analysis indicated that there was a significant, medium effect of meditation interventions on cortisol levels, but the effect was only present for at-risk samples such as those living in stressful life situations.13 There are also studies done among specific populations such as tertiary education students14 and older adults,15 showing inconclusive results. Among tertiary education students, the effect sizes of interventions for stress were moderate (g = 0.42, 95% CI: 0.27–0.57), but most studies were of poor quality.14 Among older adults, no clear evidence was found that MBIs can reduce the perception of stress.15
Insomnia
The current evidence on the effects of MBIs on insomnia and sleep disturbance is promising. A meta-analysis concluded that MBIs are effective in improving symptoms of insomnia and sleep quality when compared to attention/education and waitlist control with medium to large effects (g = 0.67, 95% confidence interval [CI] = 0.30–1.05) and that the effects seem to endured at 3 months postintervention (g = 1.06, 95% CI = 0.48–1.64).16 Several other meta-analyses also found similar results, which all showed significant improvement in insomnia or sleep quality as measured by the Pittsburgh Sleep Quality Index.17–19
Eating disorders
Current studies provided preliminary evidence on the potential effects of MBIs on eating disorders (EDs). One systematic review and meta-analysis showed a within-condition effect of MBIs on ED symptoms, emotional eating, negative affect and body dissatisfaction, and on the body mass index (BMI) in anorectic and bulimic participants relative to pre-assessment.20 Another systematic review and meta-analysis also found that MBIs may help reducing body image concern and negative affect, while promoting body appreciation.21 Both authors concluded that more rigorous studies are needed before the efficacy of MBIs on EDs can be confirmed.20,21
Addiction
Literature supports the efficacy of MBIs in both substance and behavioural addictions. A systematic review of 54 randomised controlled trials found that MBIs were successful in the reduction of dependence, craving and other symptoms related to addiction, and the improvement of mood state and emotion dysregulation.22 Two other meta-analytic results also revealed significant small-to-large effects of MBIs in reducing levels of perceived craving,23,24 severity of stress,23,24 frequency and severity of substance misuse,23 anxiety and depressive symptoms,24 negative affectivity,24 and post-traumatic symptoms24 for the treatment of substance misuse. Although the effectiveness is promising, more research is needed especially on longer follow-up assessments and among diverse populations.
Psychosis
It seems that MBIs have potential benefits for people with psychosis, but further research is warranted.25 A systematic review and meta-analysis on 434 patients found short-term moderate evidence of MBIs on total psychotic symptoms, positive symptoms, hospitalization rates, duration of hospitalization, and mindfulness as short-term effects and total psychotic symptoms and duration of hospitalization as long-term effects in patients with psychosis.26 Another systematic review also confirmed that MBIs are feasible for individuals with psychosis and it could provide a number of significant benefits over routine care such as improving negative symptoms and measures of functioning.27 Future large trials adopting randomization procedure are suggested to gain greater insight into the mechanisms and long-term effectiveness of MBIs among people with psychosis.
Post-traumatic stress disorder
MBIs among post-traumatic stress disorder (PTSD)-diagnosed participants were less conclusive. A systematic review and meta-analysis of 10 trials on meditation interventions have shown that the effects for PTSD were positive but not statistically significant.28 The variety of meditation intervention types, the short follow-up times and the quality of studies limited the analyses.28 Other systematic reviews reported similar findings, where they reported MBIs such as mindfulness, yoga and relaxation studies maybe useful for the mind–body treatments for PTSD but many of the trials suffered from methodologic weaknesses or were of low to moderate methodological rigor.29,30 Further high-quality studies are needed on MBIs among PTSD-diagnosed participants in order to increase confidence in its effectiveness.
Attention-deficit hyperactivity disorder
There is a need for further research before determining the effectiveness of MBIs on attention-deficit hyperactivity disorder (ADHD) despite current studies showed that it can be a promising intervention. A systematic review and meta-analysis has found statistically significant effect of MBIs in decreasing the severity of ADHD core symptoms such as inattention, hyperactivity or impulsivity (children/adolescents: Hedge’s g = −0.44, 95% CI −0.69 to −0.19, I2 0%; adults: Hedge’s g = −0.66, 95% CI –1.21 to −0.11, I2 81.81%).31 However, the authors concluded that there is insufficient methodologically sound evidence to support the effectiveness due to limited number of studies, heterogeneity across studies and high risk of bias.31 Similar results and conclusions were also noted in several other systematic reviews.32–34
Autism spectrum disorders
Current literature on MBIs for people with autism spectrum disorders (ASD) or their carers is very limited. A systematic review done in 2017 analysed 16 eligible studies but definitive recommendations could not be made on the effects of MBIs for people with ASD or their carers.35 This was because those studies included very diverse age groups and outcome measures, including behavioural, social and psychological symptoms, as well as the subjective well-being of children and adults with ASD and their parents.35 Overall, there may be some potential benefits of MBIs among people with ASD, these include: reducing anxiety,35,36 thought problems,35,36 rumination,35 aggression,36 parental stress37, and increasing subjective well-being38 as well as parental psychological wellbeing.37
Cognition
The current available evidence to support MBIs on cognition is weak. A systematic review conducted in older adults with mild cognitive impairment found that MBIs improved participant’s cognitive function and everyday activities functioning.39 However, the available studies had small sample sizes, lack of control comparison and lack of follow-up to understand the effects on preventing progression of dementia.39 Further high-quality trials and on different populations are required to confirm the effectiveness of the benefits of MBIs on cognitive function.
Effects on physical health
MBIs can provide positive effects on physical health and evidence is strong regarding benefits of MBIs on the psychological symptoms among people with chronic diseases.
Pain
The evidence of benefits of MBIs on pain is abundant among different populations.40,41 A systematic review and meta-analysis of 30 RCTs on chronic pain conducted in 2017 showed improvement on chronic pain management after mindfulness meditation intervention.40 The percent change of the mean in pain for intervention subjects was −0.19% (SD, 0.91; min, −0.48; max, 0.10), which was significantly higher than the control groups (−0.08% (SD, 0.74; min, −0.35; max, 0.11)).40 A network meta-analysis found MBSR is effective for chronic pain, and the effects are not significantly different between MBSR and CBT; though more studies are needed to confirm this.41 Furthermore, for the effects of brief MBIs with a total contact time of less than 1.5 hours, current evidence is inadequate to confirm the effectiveness on acute and chronic pain.42
Hypertension and cardiovascular diseases
A few systematic reviews and meta-analyses suggested that MBIs can reduce blood pressure (BP).43–45 A systematic review and meta-analysis of five studies on MBSR showed reduction on systolic and diastolic blood pressure in people with hypertension or elevated blood pressure. However, most of the studies were related to clinical blood pressure only and evidence on ambulatory blood pressure is needed.43 A systematic review among people with non-communicable diseases found systolic BP was reduced after the eight-week MBSR (−6.90 mmHg [95% CI: −10.82, −2.97]), followed by the 12-week breathing awareness meditation (−4.10 mmHg [95% CI: −7.54, −0.66]), and eight-week mindfulness-based intervention (−2.69 mmHg [95% CI: −3.90, −1.49]) and diastolic BP was reduced after eight-week MBSR (−2.45 mmHg [95% CI: −3.74, −1.17]) and the eight-week MBI (−2.24 mmHg [95% CI: −3.22, −1.26]).44 Another systematic review among patients with CVD in 2020 showed benefits on systolic BP (d+ = 0.89, 95% CI = 0.26, 1.51) and psychological symptoms (d+s = 0.49–0.64), but not diastolic BP.45 Another systematic review by Zou evaluated the effect of mindful exercises for patients after stroke showed significantly improvement on the sensorimotor function on lower limb (SDM = 0.79; 95% CI, 0.43–1.15; I2 = 62.67%) and upper limb (SDM = 0.7; 95% CI, 0.39–1.01; I2 = 32.36%).46 Further studies can assess gait speed, leg strength, aerobic endurance, motor function, cognitive function and gait parameters.
Weight control and obesity
Overweight and obesity are a significant health risk factor leading to tremendous disease burden due to the associated comorbidities.47 Mindful eating is an effective intervention for weight control, especially among people with binge eating or emotional eating tendency. Mindful eating might have longer-term effects when comparing to conventional diet programmes, which involves limiting energy intake and restricting food choices, because mindful eating tends to be more sustainable and also deal with emotional problems that may influence unhealthy diet.48–52 A systematic review and meta-analysis in 2019 evaluated ten mindful eating and weight control studies, and found significant weight reduction after mindful eating program when compared with control groups (−0.348 kg, 95% CI: −0.591 to −0.105).53 Furthermore, effects of MBIs were equal to conventional diet programmes.53 However, limitations were found in the studies, such as short duration and biased samples (unbalanced sex ratio, source and place of living). Hence, further studies with longer duration and modifications of subject selection could be beneficial to evaluate long-term improvement among different populations.
Diabetes
The current evidence to support the effect of MBIs on the physiological outcomes of diabetes is inconclusive. One systematic review found mixed results on the effectiveness of MBIs for physiological outcomes (glycaemic control and blood pressure) on both types 1 and 2 diabetes patients.54 Another systematic review and meta-analysis found that meditative movements significantly improved the glycaemic control including fasting blood glucose, glycated haemoglobin (HbA1c) and postprandial blood glucose in type 2 diabetes mellitus (T2DM) patients.55 Nonetheless, the authors noted it is difficult to conclude the extent to which MBIs are effective because of the small sample size, short duration and diverse delivery methods within the published studies.55 Apart from glycaemic control, systematic reviews also found improvement in psychological symptoms such as anxiety,54 distress symptoms,54,56 depression54,57 and quality of life.57 Further research addressing the limitations is necessary to gauge the efficacy of MBIs for diabetes.
Cancer
There may be some benefits of MBIs on the physical health outcomes in cancer patients especially on cancer-related fatigue and pain, besides psychological benefits.58,59 A systematic review and meta-analysis found that MBIs led to a statistically significant reduction in cancer-related fatigue (CRF) score among cancer patients (SMD = -0.51, 95%CI [−0.81–0.20]),59 especially among lung cancer patients.60 Apart from CRF, a range of other outcomes such as improvements in sleep disturbances, pain and other psychological symptoms including anxiety, depression, fear of cancer recurrence were also found in another systematic review and meta-analysis.61 Overall, although MBIs appeared effective in reducing CRF and other symptoms, further high-quality studies are still required to provide additional insights and to confirm the existing evidence.
Respiratory health (COPD, asthma, etc.)
The effectiveness of MBIs on respiratory health remained unclear. A systematic review and meta-analysis of 16 studies found that meditative movement may have the potential to enhance lung function and physical activity in Chronic obstructive pulmonary disease (COPD) patients.62 When compared to nonexercised group, the intervention enhanced the 6-minute walking distance (3 months: mean difference [MD] = 25.40 m, 95% CI: 16.25–34.54; 6 months: MD = 35.75 m, 95% CI: 22.23–49.27), as well as functions on forced expiratory volume in 1 s (FEV1) (3 months: MD = 0.1 L, 95% CI: 0.02–0.18; 6 months: MD = 0.18 L, 95% CI: 0.1–0.26).62 However, taking into considerations of the limitations of the studies such as small sample sizes, inconsistency in study quality and the diverse style of meditative movement in studies, the authors noted that further trials are needed to substantiate the findings.62 Other systematic reviews and meta-analyses on COPD65 and asthma63 also concluded that further high-quality trials are needed to confirm the effectiveness of MBIs on respiratory health.63,64
Effects on social health and prosocial behaviours
There is evidence supporting effects of MBIs on social health and prosocial behaviours (i.e. voluntary behaviour intended to benefit another).65,66 A systematic review found medium effects on prosocial behaviours for both correlational and intervention studies, and the effects are similar to known and unknown others.65 The results suggest that mindfulness fosters ethical and cooperative behaviour across a range of interpersonal contexts and may reduce intergroup biases.65 Another recent review with 29 studies also find similar results with small to medium effect sizes, suggesting MBIs reliably improve compassionate helping and reduces prejudice and retaliation.66 Furthermore, MBIs can effectively reduce anger,67 violence68 and aggression.69 It also may help improve social and ecological sustainability, by improving individuals’ subjective well-being and benign connection with others, the society and the nature.70
Loneliness and social isolation are an increasing public health concern, especially during COVID-19 and for older adults. Some preliminary studies indicated that mindfulness training might have positive effect in mitigating loneliness.71–74 A preliminary study showed MBSR effectively reduced loneliness in older adults.71 Another study found positive effect on mitigating the loneliness of women with HIV.72 A study among Chinese college students found a positive relationship between mindfulness and loneliness reduction.73 Lindsay et al. raised that mindfulness both reduced loneliness and increased social interactions in daily life compared with an active control program, in the experiment of smartphone-based mindfulness training.74
Mindfulness in different settings
Mindfulness among professionals in healthcare settings
Mindfulness has been adopted as a stress management tool for healthcare professionals, with a medium effect size was found (r = 0.342, CI = 0.202–0.468).75 Systematic reviews and meta-analyses have shown the promising effects on the other psychological indicators among healthcare professionals and students, e.g. reducing depression and burnout and improving emotional resilience.76,77 However, both benefits and challenges (time limitations and feasibility) were perceived at the same time,78 and there are insufficient studies on indirect outcomes of MBIs among healthcare professionals, e.g. how it may influence professional-patient communication, relationship and patient outcomes.
Mindfulness in schools
Mindfulness programmes in schools are increasingly popular. Many different school mindfulness programmes (e.g. ‘.b’, mindful schools, well and resilience program) have been implemented across the world.79,80 These programmes can target at students, teachers, and even parents or caregivers.81 Recent systematic reviews found MBIs hold promises in particular in improving resilience to stress, cognitive performance such as attention, and emotional problems in children and youths.82,83 The reviews showed a significant effect for resilience in regards to well-being, positive and constructive emotions or affect, social skills and positive relationships, self-concept and self-esteem. The effects (effect size = 0.36–0.80) are comparable or better than the effects (overall effect size = 0.30) of school-based social and emotional learning programs as revealed in the meta-analysis.84 It is promising in applying MBIs as a life skill within pre-, elementary, middle or high schools. Students might be benefited from 90-min mindfulness practice per week (i.e. 18 minutes on average per day).85 In building up mindful schools, a whole school approach is valuable to integrate mindfulness through the curriculum, professional development of teachers, leadership practice and across the learning environment.86
Mindfulness in workplace
A systematic review on 58 592 adults from nonclinical samples showed that trait mindfulness was positively associated with confidence, job satisfaction, performance and interpersonal relations, and negatively associated with burnout and work withdrawal.87 A recent systematic review on 56 randomized controlled trials shows that MBIs are beneficial to employees in reducing stress, burnout, mental distress and somatic complaints, while improving mindfulness, well-being, compassion and job satisfaction—all with small to large effect sizes ranging from Hedge’s g = 0.32–0.77, but effects on work engagement and productivity were limited by low number of studies.88
Cost-effectiveness of MBIs
MBIs are likely to be cost-effective and value for money as it can be provided in group format or as self-help interventions,89 and it can also be integrated into educational programmes for clinicians, educationalists and other professionals to directly and indirectly benefit themselves, students, their clients and people around them.90 While the benefits are almost equal to cognitive behavioural interventions, mindfulness may require less professional training and take less time for both workers and clients to master, and they are probably less expensive to provide.91 For example, studies showed that the training cost for teachers in a mindfulness training program ranged from US$515 to US$1850 per teacher depending on the number of teachers being trained and the ancillary and opportunity costs.92 However, more studies are needed to confirm their cost-effectiveness. Preliminary evidence support its cost-effectiveness,93 including but not limited to pain in breast cancer,94 fibromyalgia,95 low back pain96 and caregiver training.97 It is also a cost-saving treatment for improving quality of life for distressed cancer patients using both online or face-to-face MBCT.98 However, uncertainties existed in workplace,99 and yet it needs cost-effectiveness studies on many other health problems aswell.
Compliance of MBIs
Non-compliance is a barrier to learning mindfulness100 and research shows that the drop-out rate can reach 25% or higher.101,102 Inconsistent findings were shown in previous studies regarding who might or might not comply with MBIs. Although in general, women, those with higher openness to experience, higher resistance to change and severer symptoms showed higher levels of compliance.103,104 The relationship between participants’ compliance and intervention outcomes is inconsistent, ranging from no correlation to a positive correlation,105 although one recent systematic review based on 28 studies found a small but significant association between participants’ self-reported home practice and intervention outcomes (r = 0.26, 95% CI: 0.19–0.34).106 In terms of factors associated with better compliance, a good natural setting is found to be important, especially for beginners.100 And some researchers suggested to identify meditation exercises that can balance optimizing effectiveness and enhancing adherence to strengthen the compliance to MBIs.107 It still needs more research to understand who might comply with and benefit from which type of MBIs the most, and to look into factors and strategies enhancing compliance.
Mechanisms of MBIs
Studies suggested that the mechanisms of MBIs include changes in mindfulness, rumination, worry, self-regulation, compassion or meta-awareness, which predicted or mediated the treatment effects, which are theoretically predicted mechanisms of MBIs.108–111 Preliminary results also suggested alterations in attention, memory specificity, self-discrepancy, emotional reactivity and momentary positive and negative affect, can be part of the mechanisms.108 Recently, the mindfulness-to-meaning (MMT) approach has also been recognized as providing a theoretical framework to investigate specific mindfulness components and their contributions to the positive health outcomes.112,113 In this approach, the iterative cycle of appraisal, decentering and metacognition would lead to positive reappraisals of broader contexts that extinguish negative affect and promote positive effects and eudaimonic meaning in life.112,113 Yet, there are still many unknowns regarding the mechanisms ofMBIs.
Neurophysiological findings
The changes on brain and biomarkers of immune function and stress might have provided neurophysiological basis for explaining the positive effects of MBIs. Systematic reviews have consistently found effects of MBIs on brain activity that involves in processing self-relevant information, self-regulation, focused problem-solving, adaptive behaviour and interoception, among both healthy populations and patient groups.114–119 Eight brain regions key to meta-awareness (frontopolar cortex), body awareness (sensory cortices and insular), memory consolidation and reconsolidation (hippocampus), self and emotion regulation (anterior and mid cingulate; orbitofrontal cortex), and intra- and interhemispheric communication (superior longitudinal fasciculus; corpus callosum) consistently altered with a medium effect size after mindfulness practices.118 In expert meditators, both functional and structural brain modifications have been induced, especially in areas involved in self-referential processes such as self-awareness and self-regulation, though not enough evidence suggests structural brain modifications in short-term meditators.114 Among people with major depressive disorders, MBIs have also modulatory effects on several brain regions (e.g. the prefrontal cortex, the basal ganglia, the anterior and posterior cingulate cortices and the parietal cortex).115 Another systematic review on 78 functional neuroimaging (fMRI and PET) studies of meditation found patterns of brain activation and deactivation for common styles of meditation (focused attention, mantra recitation, open monitoring and compassion/loving-kindness), with medium effects for both activations (d = 0.59) and deactivations (d = −0.74), suggesting potential practical significance.116 The systematic review on EEG results suggested that mindfulness is associated with increased alpha and theta power in both healthy populations and patient groups, which may signify a relaxed alertness state contributing to mental health.117
Systematic reviews on RCTs revealed that mindfulness meditation have effects on stress and immune-related physiological markers of inflammation, cell-mediated immunity and biological aging: reductions in the activity of the cellular transcription factor NF-kB, reductions in circulating levels of C-reactive protein, increases in CD4+ T cell count (in HIV-diagnosed individuals), and increases in telomerase activity.120 Another systematic review on RCTs found that, compared to an active control (relaxation, exercise or education), mindfulness meditation reduced physiological markers of stress, such as cortisol, C-reactive protein, systolic blood pressure, heart rate, triglycerides and tumour necrosis factor-alpha, in various populations.121 And a greater number of hours of meditation are associated with a greater impact on telomere biology.122 However, these tentative findings need further replication and the review authors call for studies to include physiological markers as primary outcome of RCTs.120–123
Ethics of MBIs
Ethical questions are fundamental and essential in guiding the future directions of MBIs to use the right mindfulness rightly, and also the application of MBIs should not overstate the organizational and social determinants of ill health. In the books of ‘Practitioner’s Guide to Ethics and Mindfulness-Based Interventions’ (edited by Lynette Monteiro, Jane Compson and Frank Musten) and ‘Handbook of Ethical Foundations of Mindfulness’ (edited by Stanley Steven, Ronald Purser and Nirbhay Singh), ethical questions of mindfulness are discussed extensively. Many questions on ethics are yet to be addressed for MBIs. For example, paradox in teaching mindfulness in business and military settings, depriving superiors to make use of subordinates through mindfulness regardless of other organizational factors causing work-related stress or depression. On the other hand, there are many virtues and strengths in MBIs in providing personally meaningful and prosocial values,124 and MBIs can improve ethical standards, that mindfulness promotes greater ethical intentions and lesser ethical infractions, with more mindful people revealed a greater emphasis on moral principles than those who are less mindful.125
Safety of MBIs
MBIs are regarded as relatively safe interventions.126 Like many other psychological intervention trials, adverse events and adverse effects of MBIs are largely underreported. A previous systematic review on safety of MBSR and MBCT indicated that fewer than one in five trials had mentioned the monitoring of adverse effects.126 Program-related factors, participant-related factors, and clinician- or teacher-related factors are potential sources of adverse effects.1,126–132 A safety checklist is yet needed to be built based on previous studies and empirical experiences. Practitioners and researchers in future MBI programmes are advised to report the potential adverse events using such a checklist, and also continue to take safety precautions such as screening and caring for vulnerable individuals. These individuals could be those with PTSD, seizure disorder/epilepsy, acute psychosis, mania, suicidality or other health problems of concern.133
Future directions
Despite the increasing trend of mindfulness studies and applications, there are still many areas need exploration. First, higher quality of research studies is needed. The most frequent limitations mentioned in the systematic reviews on effectiveness and cost-effectiveness of MBIs are low quality of study design, small sample size, short follow-up period, and inconsistent terminology and measurement tools. Future more robust studies are needed to address these caveats. Second, more studies on online MBIs intervention and training are needed to understand if online alternatives have equal or better effects and cost-effectiveness, though preliminary benefits are seen.10,134,135 Online alternatives might be important, especially given the pandemic of COVID-19. Third, more understanding of the mechanisms by integrating both empirical findings and neurophysiological findings. Fourth, more research is needed to explore the acceptance and compliance of MBIs to understand who might benefit more from MBIs, and barriers and respective strategies (e.g. better meditation environment) for improving the acceptance and compliance, taken into considerations of safety issues and ethical concerns. And a closer look at the long-term compliance is needed. This may call for large-scale cohort studies on MBIs. Fifth, develop more mindfulness related research and services guidelines and regulations, e.g. on adverse events monitoring and safety guarantee, and qualifications of mindfulness teachers. These might be important when MBIs are provided as a collective action in schools, companies or organizations. Sixth, exploration of Mindfulness Plus (Mindfulness+), i.e. combination of MBIs with other effective interventions (for example, mindfulness plus medications, mindfulness plus behavioural activation,136 mindfulness plus reflection training137 and mindfulness plus Qigong movement therapy138), or exploration of personalized/individualized mindfulness-based interventions for individuals with different characteristics and needs, selecting from many different mindfulness programs. This would provide more potential to improve the effects of MBIs for different goals.
Conclusion
MBIs are effective for many common mental, physical and social health conditions among different populations. Beneficial effects of MBIs have been found on depression, anxiety, stress, insomnia, addiction, psychosis, pain, hypertension, weight control, cancer-related symptoms and prosocial behaviours. Current evidence suggested MBIs can be beneficial for healthcare professionals and within schools and workplaces although more studies are still needed to look into its efficacy on many different biopsychosocial health conditions. MBIs are relatively safe. Ethical aspects should always be taken into account during mindfulness-based trainings and interventions. Mechanisms of MBIs have been suggested in both empirical and neurophysiological findings. Cost-effectiveness is found for some health problems (e.g. breast cancer, fibromyalgia, low back pain or caregiver training). More high-quality studies with adequate sample size and longer follow-up duration are needed to confirm its effectiveness and cost-effectiveness in many other problems and among sub-groups. Some other areas needing additional research are suggested in this review.
Contributor Information
Dexing Zhang, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Eric K P Lee, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Eva C W Mak, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
C Y Ho, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Samuel Y S Wong, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Conflict of interest statement
None.
Data availability statement
There are no new data associated with this article.
References
- 1. Baer R, Crane C, Miller E et al. Doing no harm in mindfulness-based programs: conceptual issues and empirical findings. Clin Psychol Rev 2019;71:101–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kabat-Zinn J. Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences 2003;8:73. [Google Scholar]
- 3. Segal ZV, Teasdale JD, Williams JMG. Mindfulness-Based Cognitive Therapy: Theoretical Rationale and Empirical Status. New York: Guilford Press, 2004.
- 4. Teasdale JD, Segal ZV, Williams JMG et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 2000;68:615. [DOI] [PubMed] [Google Scholar]
- 5. Aghaie E, Roshan R, Mohamadkhani P et al. Well-being, mental health, general health and quality of life improvement through mindfulness-based interventions: a systematic review and meta-analysis. Iran Red Crescent Med J 2018;20:7. doi: 10.5812/ircmj.16231 [DOI] [Google Scholar]
- 6. Khoury B, Sharma M, Rush SE et al. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res 2015;78:519–28. doi: 10.1016/j.jpsychores.2015.03.009 [DOI] [PubMed] [Google Scholar]
- 7. Hofmann SG, Sawyer AT, Witt AA et al. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010;78:169–83. doi: 10.1037/a0018555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khoury B, Lecomte T, Fortin G et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev 2013;33:763–71. doi: 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 9. Shi ZR, MacBeth A. The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: a systematic review. Mind 2017;8:823–47. doi: 10.1007/s12671-016-0673-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sevilla-Llewellyn-Jones J, Santesteban-Echarri O, Pryor I et al. Web-based mindfulness interventions for mental health treatment: systematic review and meta-analysis. JMIR Ment Health 2018;5:16. doi: 10.2196/10278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blanck P, Perleth S, Heidenreich T et al. Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: systematic review and meta-analysis. Behav Res Ther 2018;102:25–35. doi: 10.1016/j.brat.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 12. Sanada K, Montero-Marin J, Diez MA et al. Effects of mindfulness-based interventions on salivary cortisol in healthy adults: a meta-analytical review. Front Physiol 2016;7:12. doi: 10.3359/fphys.2016.00/171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koncz A, Demetrovics Z, Takacs ZK. Meditation interventions efficiently reduce cortisol levels of at-risk samples: a meta-analysis. Health Psychol Rev 2020:1–29. doi: 10.1080/17437199.2020.1760727. [DOI] [PubMed]
- 14. Breedvelt JJF, Amanvermez Y, Harrer M et al. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: a meta-analysis. Front Psych 2019;10:15. doi: 10.3389/fpsyt.2019.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li SYH, Bressington D. The effects of mindfulness-based stress reduction on depression, anxiety, and stress in older adults: a systematic review and meta-analysis. Int J Ment Health Nurs 2019;28:635–56. doi: 10.1111/inm.12568. [DOI] [PubMed] [Google Scholar]
- 16. Rash JA, Kavanagh VAJ, Garland SN. A meta-analysis of mindfulness-based therapies for insomnia and sleep disturbance moving towards processes of change. Sleep Med Clin 2019;14:209-+. doi: 10.1016/j.jsmc.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 17. Wang YY, Wang F, Zheng W et al. Mindfulness-based interventions for insomnia: a meta-analysis of randomized controlled trials. Behav Sleep Med 2020;18:1–9. doi: 10.1080/15402002.2018.1518228. [DOI] [PubMed] [Google Scholar]
- 18. Gong H, Ni CX, Liu YZ et al. Mindfulness meditation for insomnia: a meta-analysis of randomized controlled trials. J Psychosom Res 2016;89:1–6. doi: 10.1016/j.jpsychores.2016.07.016 [published online first: September 25, 2016]. [DOI] [PubMed] [Google Scholar]
- 19. Chen T-L, Chang S-C, Hsieh H-F et al. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J Psychosom Res 2020;135:110144. doi: 10.1016/j.jpsychores.2020.110144. [DOI] [PubMed] [Google Scholar]
- 20. Turgon R, Ruffault A, Juneau C et al. Eating disorder treatment: a systematic review and meta-analysis of the efficacy of mindfulness-based programs. Mind 2019;10:2225–44. doi: 10.1007/s12671-019-01216-5. [DOI] [Google Scholar]
- 21. Beccia AL, Dunlap C, Hanes DA, et al. Mindfulness-based eating disorder prevention programs: a systematic review and meta-analysis. Mental Health & Prevention 2018;9:1–12 doi: 10.1016/j.mhp.2017.11.001. [DOI] [Google Scholar]
- 22. Sancho M, De Gracia M, Rodriguez RC et al. Mindfulness-based interventions for the treatment of substance and Behavioral addictions: a systematic review. Front Psych 2018;9:9. doi: 10.3389/fpsyt.2018.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li W, Howard MO, Garland EL et al. Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J Subst Abus Treat 2017;75:62–96. doi: 10.1016/j.jsat.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 24. Cavicchioli M, Movalli M, Maffei C. The clinical efficacy of mindfulness-based treatments for alcohol and drugs use disorders: a meta-analytic review of randomized and nonrandomized controlled trials. Eur Addict Res 2018;24:137–62. doi: 10.1159/000490762. [DOI] [PubMed] [Google Scholar]
- 25. Louise S, Fitzpatrick M, Strauss C et al. Mindfulness-and acceptance-based interventions for psychosis: our current understanding and a meta-analysis. Schizophr Res 2018;192:57–63. [DOI] [PubMed] [Google Scholar]
- 26. Cramer H, Lauche R, Haller H et al. Mindfulness- and acceptance-based interventions for psychosis: a systematic review and meta-analysis. Glob Adv Health Med 2016;5:30–43. doi: 10.7453/gahmj.2015.083 [published online first: March 5, 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Aust J, Bradshaw T. Mindfulness interventions for psychosis: a systematic review of the literature. J Psychiatr Ment Health Nurs 2017;24:69–83. doi: 10.1111/jpm.12357. [DOI] [PubMed] [Google Scholar]
- 28. Hilton L, Maher AR, Colaiaco B et al. Meditation for posttraumatic stress: systematic review and meta-analysis. Psychol Trauma 2017;9:453–60. doi: 10.1037/tra0000180. [DOI] [PubMed] [Google Scholar]
- 29. Niles BL, Mori DL, Polizzi C et al. A systematic review of randomized trials of mind-body interventions for PTSD. J Clin Psychol 2018;74:1485–508. doi: 10.1002/jclp.22634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Banks K, Newman E, Saleem J. An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J Clin Psychol 2015;71:935–63. doi: 10.1002/jclp.22200. [DOI] [PubMed] [Google Scholar]
- 31. Zhang JH, Diaz-Roman A, Cortese S. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: a systematic review and meta-analysis. Evid-Based Ment Health 2018;21:87–94. doi: 10.1136/ebmental-2018-300015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mak C, Whittingham K, Cunnington R et al. Efficacy of mindfulness-based interventions for attention and executive function in children and adolescents-a systematic review. Mind 2018;9:59–78. doi: 10.1007/s12671-017-0770-6. [DOI] [Google Scholar]
- 33. Lee CSC, Ma M-T, Ho H-Y et al. The effectiveness of mindfulness-based intervention in attention on individuals with ADHD: a systematic review. Hong Kong J Occup Ther 2017;30:33–41. doi: 10.1016/j.hkjot.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Poissant H, Mendrek A, Talbot N et al. Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: a systematic review. Behav Neurol 2019;2019:16. doi: 10.1155/2019/5682050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hourston S, Atchley R. Autism and mind-body therapies: a systematic review. J Altern Complement Med 2017;23:331–9. doi: 10.1089/acm.2016.0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cachia RL, Anderson A, Moore DW. Mindfulness in individuals with autism Spectrum disorder: a systematic review and narrative analysis. Rev J Autism Dev Disord 2016;3:165–78. doi: 10.1007/s40489-016-0074-0. [DOI] [Google Scholar]
- 37. Cachia RL, Anderson A, Moore DW. Mindfulness, stress and well-being in parents of children with autism Spectrum disorder: a systematic review. Journal of Child and Family Studies 2016;25(1):1–14 doi: 10.1007/s10826-015-0193-8. [DOI] [Google Scholar]
- 38. Hartley M, Dorstyn D, Due C. Mindfulness for children and adults with autism Spectrum disorder and their caregivers: a meta-analysis. J Autism Dev Disord 2019;49:4306–19. doi: 10.1007/s10803-019-04145-3. [DOI] [PubMed] [Google Scholar]
- 39. Farhang MA-O, Miranda-Castillo C, Rubio M et al. Impact of mind-body interventions in older adults with mild cognitive impairment: a systematic review. Int Psychogeriatr 2019;31:643–66. doi: 10.1017/S1041610218002302. [DOI] [PubMed] [Google Scholar]
- 40. Hilton LA-O, Hempel S, Ewing BA et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med 2017;51:199–213. doi: 10.1007/s12160-016-9844-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Khoo E-L, Small R, Wei C et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network metaanalysis. Evid Based Ment Health 2019;22:26–35. doi: 10.1136/ebmental-2018-300062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McClintock AS, McCarrick SM, Garland EL et al. Brief mindfulness-based interventions for acute and chronic pain: a systematic review. J Altern Complement Med 2019;25:265–78. doi: 10.1089/acm.2018.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Solano Lopez AL. Effectiveness of the mindfulness-based stress reduction program on blood pressure: a systematic review of literature. Worldviews Evid-Based Nurs 2018;15:344–52. [DOI] [PubMed] [Google Scholar]
- 44. Intarakamhang U, Macaskill A, Prasittichok P. Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: a systematic review and meta-analysis. Heliyon 2020;6:9. doi: 10.1016/j.heliyon.2020.e03834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scott-Sheldon LA, Gathright EC, Donahue ML et al. Mindfulness-based interventions for adults with cardiovascular disease: a systematic review and meta-analysis. Ann Behav Med 2020;54:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zou LY, Sasaki JE, Zeng N et al. A systematic review with meta-analysis of mindful exercises on rehabilitative outcomes among poststroke patients. Arch Phys Med Rehabil 2018;99:2355–64. doi: 10.1016/j.apmr.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 47. Guh DP, Zhang W, Bansback N et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009;9:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lyzwinski LN, Caffery L, Bambling M et al. Relationship between mindfulness, weight, and weight-related behaviors in college students: a systematic review. Alternative & Complementary Therapies 2018;24:202–14. doi: 10.1089/act.2018.29182.lnl. [DOI] [Google Scholar]
- 49. Carriere K, Khoury B, Gunak MM et al. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev 2018;19:164–77. doi: 10.1111/obr.12623. [DOI] [PubMed] [Google Scholar]
- 50. Ruffault A, Czernichow S, Hagger MS et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract 2017;11:90–111. doi: 10.1016/j.orcp.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 51. Fulwiler C, Brewer JA, Sinnott S, et al. Mindfulness-based interventions for weight loss and CVD risk management. Curr Cardiovasc Risk Rep 2015;9(10):46. doi: 10.1007/s12170-015-0474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Katterman SN, Kleinman BM, Hood MM et al. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav 2014;15:197–204. doi: 10.1016/j.eatbeh.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 53. Artiles RF, Staub K, Aldakak L et al. Mindful eating and common diet programs lower body weight similarly: systematic review and meta-analysis. Obes Rev 2019;20(11):1619–27. doi: 10.1111/obr.12918. [DOI] [PubMed] [Google Scholar]
- 54. Noordali F, Cumming J, Thompson JL. Effectiveness of mindfulness-based interventions on physiological and psychological complications in adults with diabetes: a systematic review. J Health Psychol 2017;22:965–83. doi: 10.1177/1359105315620293. [DOI] [PubMed] [Google Scholar]
- 55. Xia TW, Yang Y, Li WH et al. Meditative movements for patients with type 2 diabetes: a systematic review and meta-analysis. Evid-based Complement Altern Med 2020;2020:12. doi: 10.1155/2020/5745013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bogusch LM, O'Brien WH. The effects of mindfulness-based interventions on diabetes-related distress, quality of life, and metabolic control among persons with diabetes: a meta-analytic review. Behav Med 2019;45:19–29. doi: 10.1080/08964289.2018.1432549. [DOI] [PubMed] [Google Scholar]
- 57. Xunlin NG, Lau Y, Klainin-Yobas P et al. The effectiveness of mindfulness-based interventions among cancer patients and survivors: a systematic review and meta-analysis. Support Care Cancer 2020;28:1563–78. doi: 10.1007/s00520-019-05219-9. [DOI] [PubMed] [Google Scholar]
- 58. Ngamkham S, Holden JE, Smith EL. A systematic review: mindfulness intervention for Cancer-related pain. Asia Pac J Oncol Nurs 2019;6:161–9. doi: 10.4103/apjon.apjon_67_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. He J, Hou JH, Qi J, et al. Mindfulness based stress reduction interventions for cancer related fatigue: a meta-analysis and systematic review. J Natl Med Assoc 2020;112(4):387–94. doi: 10.1016/j.jnma.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 60. Xie CY, Dong B, Wang LH et al. Mindfulness-based stress reduction can alleviate cancer-related fatigue: a meta-analysis. J Psychosom Res 2020;130:8. doi: 10.1016/j.jpsychores.2019.109916. [DOI] [PubMed] [Google Scholar]
- 61. Cillessen L, Johannsen M, Speckens AEM et al. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta-analysis of randomized controlled trials. Psychooncology 2019;28(12):2257–69. doi: 10.1002/pon.5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wu LL, Lin ZK, Weng HD et al. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018;13:1239–50. doi: 10.2147/COPD.S159042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Paudyal P, Jones C, Grindey C et al. Meditation for asthma: systematic review and meta-analysis. J Asthma 2018;55:771–8. doi: 10.1080/02770903.2017.1365887. [DOI] [PubMed] [Google Scholar]
- 64. Clari M, Conti A, Fontanella R et al. Mindfulness-based programs for people with chronic obstructive pulmonary disease: a mixed methods systematic review. Mind 2020;20. doi: 10.1007/s12671-020-01348-z. [DOI] [Google Scholar]
- 65. Donald JN, Sahdra BK, Van Zanden B et al. Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. Br J Psychol 2019;110:101–25. [DOI] [PubMed] [Google Scholar]
- 66. Berry DR, Hoerr JP, Cesko S et al. Does mindfulness training without explicit ethics-based instruction promote prosocial Behaviors? A meta-analysis. Personal Soc Psychol Bull 2020;46:1247–69. [DOI] [PubMed] [Google Scholar]
- 67. Wright S, Day A, Howells K. Mindfulness and the treatment of anger problems. Aggression and Violent Behavior 2009;14(5):396–401. doi: 10.1016/j.avb.2009.06.008. [DOI] [Google Scholar]
- 68. Gillions A, Cheang R, Duarte R. The effect of mindfulness practice on aggression and violence levels in adults: a systematic review. Aggress Violent Behav 2019;48:104–15. doi: 10.1016/j.avb.2019.08.012. [DOI] [Google Scholar]
- 69. Fix RL, Fix ST. The effects of mindfulness-based treatments for aggression: a critical review. Aggression and Violent Behavior 2013;18(2):219–27. doi: 10.1016/j.avb.2012.11.009. [DOI] [Google Scholar]
- 70. Friese M, Messner C, Schaffner Y. Mindfulness meditation counteracts self-control depletion. Conscious Cogn 2012;21:1016–22. doi: 10.1016/j.concog.2012.01.008 [published online first: February 09, 2012]. [DOI] [PubMed] [Google Scholar]
- 71. Creswell JD, Irwin MR, Burklund LJ et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun 2012;26(7):1095–101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Samhkaniyan E, Mahdavi A, Mohamadpour S, et al. The effectiveness of mindfulness-based cognitive therapy on quality of life and loneliness of women with HIV. J Med Life 2015;8(Spec Iss 4):107–113. [published online first: January 1, 2015] [PMC free article] [PubMed] [Google Scholar]
- 73. Zhang N, FM F, Sy H et al. Mindfulness training for loneliness among Chinese college students: a pilot randomized controlled trial. Int J Psychol 2018;53:373–8. [DOI] [PubMed] [Google Scholar]
- 74. Lindsay EK, Young S, Brown KW et al. Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc Natl Acad Sci U S A 2019;116:3488–93. doi: 10.1073/pnas.1813588116 [published online first: February 28, 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Burton A, Burgess C, Dean S et al. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress & Health: J Int Soc for the Investigation of Stress 2017;33:3–13. doi: 10.1002/smi.2673. [DOI] [PubMed] [Google Scholar]
- 76. Lomas T, Medina JC, Ivtzan I et al. A systematic review and meta-analysis of the impact of mindfulness-based interventions on the well-being of healthcare professionals. Mind 2019;10:1193–216. doi: 10.1007/s12671-018-1062-5. [DOI] [Google Scholar]
- 77. Suleiman-Martos N, Gomez-Urquiza JL, Aguayo-Estremera R et al. The effect of mindfulness training on burnout syndrome in nursing: a systematic review and meta-analysis. J Adv Nursing (John Wiley & Sons, Inc) 2020;76:1124–40. doi: 10.1111/jan.14318. [DOI] [PubMed] [Google Scholar]
- 78. Scheepers RA, Emke H, Epstein RM et al. The impact of mindfulness-based interventions on doctors' well-being and performance: a systematic review. Med Educ 2020;54:138–49. doi: 10.1111/medu.14020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Bostic JQ, Nevarez MD, Potter MP et al. Being present at school: implementing mindfulness in schools. Child and Adolescent Psychiatric Clinics 2015;24:245–59. [DOI] [PubMed] [Google Scholar]
- 80. Sapthiang S, Van Gordon W, Shonin E. Health school-based mindfulness interventions for improving mental health: a systematic review and thematic synthesis of qualitative studies. Journal of Child and Family Studies 2019;28(10):2650–8. doi: 10.1007/s10826-019-01482-w. [DOI] [Google Scholar]
- 81. Burgdorf V, Szabo M, Abbott MJ. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: a systematic review and meta-analysis. Front Psychol 2019;10:1336. doi: 10.3389/fpsyg.2019.01336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Zenner C, Herrnleben-Kurz S, Walach H. Mindfulness-based interventions in schools—a systematic review and meta-analysis. Front Psychol 2014;5:603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Erbe R, Lohrmann D. Mindfulness meditation for adolescent stress and well-being: a systematic review of the literature with implications for school health programs. Health Educ 2015;47(2):12–9. [Google Scholar]
- 84. Durlak JA, Weissberg RP, Dymnicki AB et al. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev 2011;82:405–32. [DOI] [PubMed] [Google Scholar]
- 85. Klingbeil DA, Renshaw TL, Willenbrink JB et al. Mindfulness-based interventions with youth: a comprehensive meta-analysis of group-design studies. J Sch Psychol 2017;63:77–103. [DOI] [PubMed] [Google Scholar]
- 86. Bailey NW, Owen J, Hassed CS, et al. Evidence based guidelines for mindfulness in schools: a guide for teachers and principals. Smiling Mind, 2018. https://static1.squarespace.com/static/5a2f40a41f318d38ccf0c819/t/5b28988170a6ad07781beeb9/1529387171804/smiling-mind-mindfulness-guidelines-for-schools-whitepaper.pdf. (10 August 2020, date last accessed).
- 87. Mesmer-Magnus J, Manapragada A, Viswesvaran C et al. Trait mindfulness at work: a meta-analysis of the personal and professional correlates of trait mindfulness. Hum Perform 2017;30:79–98. doi: 10.1080/08959285.2017.1307842. [DOI] [Google Scholar]
- 88. Vonderlin R, Biermann M, Bohus M et al. Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mind 2020. doi: 10.1007/s12671-020-01328-3. [DOI] [Google Scholar]
- 89. Cavanagh K, Strauss C, Forder L et al. Can mindfulness and acceptance be learnt by self-help?: a systematic review and meta-analysis of mindfulness and acceptance-based self-help interventions. Clin Psychol Rev 2014;34:118–29. [DOI] [PubMed] [Google Scholar]
- 90. Ergas O. The deeper teachings of mindfulness-based "Interventions' as a reconstruction of "education'. J Philos Educ 2015;49:203–20. doi: 10.1111/1467-9752.12137. [DOI] [Google Scholar]
- 91. Singh SK, Gorey KM. Relative effectiveness of mindfulness and cognitive behavioral interventions for anxiety disorders: meta-analytic review. Soc Work Ment Health 2018;16:238–51. [Google Scholar]
- 92. Doyle SL, Brown JL, Rasheed D et al. Cost analysis of ingredients for successful implementation of a mindfulness-based professional development program for teachers. Mind 2019;10:122–30. [Google Scholar]
- 93. Duarte R, Lloyd A, Kotas E et al. Are acceptance and mindfulness-based interventions ‘value for money’? Evidence from a systematic literature review. Br J Clin Psychol 2019;58:187–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Johannsen M, Sørensen J, O'Connor M et al. Mindfulness-based cognitive therapy (MBCT) is cost-effective compared to a wait-list control for persistent pain in women treated for primary breast cancer—results from a randomized controlled trial. Psychooncology 2017;26:2208–14. [DOI] [PubMed] [Google Scholar]
- 95. Pérez-Aranda A, D’Amico F, Feliu-Soler A et al. Cost–utility of mindfulness-based stress reduction for fibromyalgia versus a multicomponent intervention and usual care: a 12-month randomized controlled trial (EUDAIMON study). J Clin Med 2019;8:1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Herman PM, Anderson ML, Sherman KJ et al. Cost-effectiveness of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care among adults with chronic low-back pain. Spine 2017;42:1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Singh NN, Lancioni GE, Karazsia BT et al. Effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) vs. training-as-usual (TAU): a randomized controlled trial. Front Psychol 2016;7:1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Compen F, Adang E, Bisseling E et al. Cost-utility of individual internet-based and face-to-face mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in cancer patients. Psychooncology 2020;29:294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. van Dongen JM, van Berkel J, Boot CR et al. Long-term cost-effectiveness and return-on-investment of a mindfulness-based worksite intervention: results of a randomized controlled trial. J Occup Environ Med 2016;58:550–60. [DOI] [PubMed] [Google Scholar]
- 100. Lymeus F, Lindberg P, Hartig T. A natural meditation setting improves compliance with mindfulness training. J Environ Psychol 2019;64:98–106. doi: 10.1016/j.jenvp.2019.05.008. [DOI] [Google Scholar]
- 101. Abbott RA, Whear R, Rodgers LR et al. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J Psychosom Res 2014;76:341–51. doi: 10.1016/j.jpsychores.2014.02.012 [published online first: April 22, 2014]. [DOI] [PubMed] [Google Scholar]
- 102. Lamothe M, Rondeau E, Malboeuf-Hurtubise C et al. Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complement Ther Med 2016;24:19–28. doi: 10.1016/j.ctim.2015.11.001 [published online first: February 11, 2016]. [DOI] [PubMed] [Google Scholar]
- 103. Hill CL, Updegraff JA. Mindfulness and its relationship to emotional regulation. Emotion 2012;12:81–90. doi: 10.1037/a0026355 [published online first: December 14, 2011]. [DOI] [PubMed] [Google Scholar]
- 104. Mikolasek M, Witt CM, Barth J. Adherence to a mindfulness and relaxation self-care app for Cancer patients: mixed-methods feasibility study. JMIR Mhealth Uhealth 2018;6:06. doi: 10.2196/11271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Vettese LC, Toneatto T, Stea JN, et al. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy 2009;23(3):198–225. doi: 10.1891/0889-8391.23.3.198. [DOI] [Google Scholar]
- 106. Parsons CE, Crane C, Parsons LJ et al. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants' mindfulness practice and its association with outcomes. Behav Res Ther 2017;95:29–41. doi: 10.1016/j.brat.2017.05.004 [published online first: May 21, 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Berghoff CR, Wheeless LE, Ritzert TR et al. Mindfulness meditation adherence in a college sample: comparison of a 10-min versus 20-min 2-week daily practice. Mind 2017;8:1513–21. doi: 10.1007/s12671-017-0717-y. [DOI] [Google Scholar]
- 108. van der Velden AM, Kuyken W, Wattar U et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev 2015;37:26–39. [DOI] [PubMed] [Google Scholar]
- 109. Alsubaie M, Abbott R, Dunn B et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev 2017;55:74–91. [DOI] [PubMed] [Google Scholar]
- 110. Hölzel BK, Lazar SW, Gard T et al. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 2011;6:537–59. [DOI] [PubMed] [Google Scholar]
- 111. Leyland A, Rowse G, Emerson L-M. Experimental effects of mindfulness inductions on self-regulation: systematic review and meta-analysis. Emotion 2019;19:108. [DOI] [PubMed] [Google Scholar]
- 112. McConnell PA, Froeliger B. Mindfulness, mechanisms and meaning: perspectives from the cognitive neuroscience of addiction. Psychol Inq 2015;26:349–57. doi: 10.1080/1047840X.2015.1076701 [published online first: March 1, 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Garland EL, Farb NA, Goldin P et al. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq 2015;26:293–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Boccia M, Piccardi L, Guariglia P. The meditative mind: a comprehensive meta-analysis of MRI studies. BioMed Research International 2015;2015:419808 doi: 10.1155/2015/419808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Vignaud P, Donde C, Sadki T et al. Neural effects of mindfulness-based interventions on patients with major depressive disorder: a systematic review. Neurosci Biobehav Rev 2018;88:98–105. [DOI] [PubMed] [Google Scholar]
- 116. Fox KC, Dixon ML, Nijeboer S et al. Functional neuroanatomy of meditation: a review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev 2016;65:208–28. [DOI] [PubMed] [Google Scholar]
- 117. Lomas T, Ivtzan I, Fu CHY. A systematic review of the neurophysiology of mindfulness on EEG oscillations. Neurosci Biobehav Rev 2015;57:401–10. doi: 10.1016/j.neubiorev.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 118. Fox KC, Nijeboer S, Dixon ML et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev 2014;43:48–73. [DOI] [PubMed] [Google Scholar]
- 119. Marchand WR. Neural mechanisms of mindfulness and meditation: evidence from neuroimaging studies. World J Radiol 2014;6:471–9. doi: 10.4329/wjr.v6.i7.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Black DS, Slavich GM. Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann N Y Acad Sci 2016;1373:13–24. doi: 10.1111/nyas.12998 [published online first: January 23, 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Pascoe MC, Thompson DR, Jenkins ZM et al. Mindfulness mediates the physiological markers of stress: systematic review and meta-analysis. J Psychiatr Res 2017;95:156–78. [DOI] [PubMed] [Google Scholar]
- 122. Schutte NS, Malouff JM, Keng SL. Meditation and telomere length: a meta-analysis. Psychol Health 2020;1–15. doi: 10.1080/08870446.2019.1707827. [DOI] [PubMed] [Google Scholar]
- 123. Heckenberg RA, Eddy P, Kent S et al. Do workplace-based mindfulness meditation programs improve physiological indices of stress? A systematic review and meta-analysis. J Psychosom Res 2018;114:62–71. [DOI] [PubMed] [Google Scholar]
- 124. Baer R. Ethics, values, virtues, and character strengths in mindfulness-based interventions: a psychological science perspective. Mind 2015;6:956–69. [Google Scholar]
- 125. Ruedy NE, Schweitzer ME. In the moment: the effect of mindfulness on ethical decision making. J Bus Ethics 2010;95:73–87. doi: 10.1007/s10551-011-0796-y. [DOI] [Google Scholar]
- 126. Wong SYS, Chan JYC, Zhang DX et al. The safety of mindfulness-based interventions: a systematic review of randomized controlled trials. Mind 2018;9:1344–57. doi: 10.1007/s12671-018-0897-0. [DOI] [Google Scholar]
- 127. Anālayo B. The insight knowledge of fear and adverse effects of mindfulness practices. Mind 2019;10:2172–85. [Google Scholar]
- 128. Anderson T, Suresh M, Farb NA. Meditation benefits and drawbacks: empirical codebook and implications for teaching. Journal of Cognitive Enhancement 2019;3:207–20. [Google Scholar]
- 129. Britton W. Can mindfulness be too much of a good thing? The value of a middle way. Current Opinion in Psychology 2019;28:159–65. doi: 10.1016/j.copsyc.2018.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Britton WB. Can mindfulness be too much of a good thing? The value of a middle way. Curr Opin Psychol 2019;28:159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Falick M. Mindfulness and the need to minimize the risk of harm: a proposal to implement and enforce standards for secular mindfulness practice. Mindfulness Studies Theses 2020:33. https://digitalcommons.lesley.edu/mindfulness_theses/33. [Google Scholar]
- 132. Schlosser M, Sparby T, Vörös S et al. Unpleasant meditation-related experiences in regular meditators: prevalence, predictors, and conceptual considerations. PLoS ONE 2019;14:e0216643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Lustyk MK, Chawla N, Nolan R et al. Mindfulness meditation research: issues of participant screening, safety procedures, and researcher training. Adv Mind Body Med 2009;24:20–30. [PubMed] [Google Scholar]
- 134. Spijkerman M, Pots WTM, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin Psychol Rev 2016;45:102–14. [DOI] [PubMed] [Google Scholar]
- 135. Toivonen KI, Zernicke K, Carlson LE. Web-based mindfulness interventions for people with physical health conditions: systematic review. J Med Internet Res 2017;19:17. doi: 10.2196/jmir.7487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Wong SY, Sun YY, Chan AT et al. Treating subthreshold depression in primary care: a randomized controlled trial of behavioral activation with mindfulness. The Annals of Family Medicine 2018;16:111–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Zelazo PD, Forston JL, Masten AS et al. Mindfulness plus reflection training: effects on executive function in early childhood. Front Psychol 2018;9:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Astin JA, Berman BM, Bausell B et al. The efficacy of mindfulness meditation plus qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J Rheumatol 2003;30:2257–62. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There are no new data associated with this article.


