Abstract
Aims
The coronavirus disease 2019 (COVID-19) pandemic has resulted in the rapid uptake of telemedicine (TM) for routine cardiovascular care. To examine the predictors of TM utilization among ambulatory cardiology patients during the COVID-19 pandemic.
Methods and results
In this single-centre retrospective study, all ambulatory cardiovascular encounters occurring between 16 March and 19 June 2020 were assessed. Baseline characteristics by visit type (in-person, TM phone, TM video) were compared using Chi-square and student t-tests, with statistical significance defined by P-value <0.05. Multivariate logistic regression was used to explore the predictors of TM vs. in-person care. A total of 8446 patients [86% Non-Hispanic (NH) White, 42% female, median age 66.8 ± 15.2 years] completed an ambulatory cardiovascular visit during the study period. TM phone (n = 4981, 61.5%) was the primary mode of ambulatory care followed by TM video (n = 2693, 33.2%). NH Black race [odds ratio (OR) 0.56, 95% confidence interval (CI): 0.35–0.94; P-value = 0.02], Hispanic ethnicity (OR 0.53, 95% CI: 0.29–0.98; P = 0.04), public insurance (Medicaid OR 0.50, 95% CI: 0.32–0.79; P = 0.003, Medicare OR 0.65, 95% CI: 0.47–0.89; P = 0.009), zip-code linked median household income of <$75 000, age >85 years, and patients with a diagnosis of heart failure were associated with reduced access to TM video encounters and a higher likelihood of in-person care.
Conclusions
Significant disparities in TM video access for ambulatory cardiovascular care exist among the elderly, lower income, as well as Black and Hispanic racial/ethnic groups.
Keywords: Telehealth, Social determinants of health, Equity, Disparity, Barriers to access
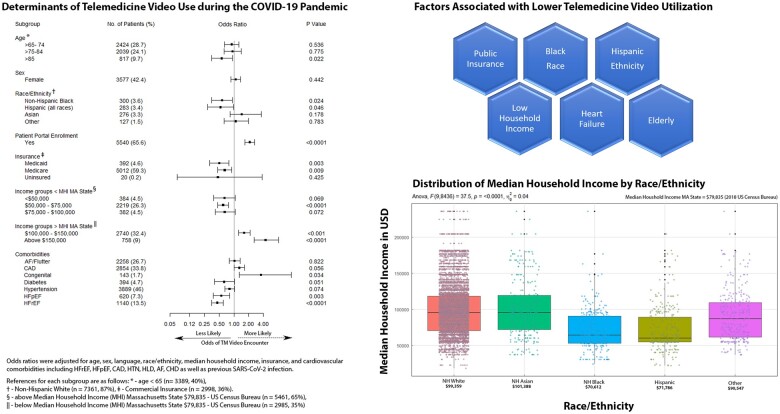
Graphical Abstract
The forest plot (left panel) shows adjusted odds ratios for TM video encounters. The box plot (lower right) shows the relationship of averaged median income in our cardiac population to race/ethnicity. The diagram (upper right) highlights the six factors associated with low TM video use in this cardiac population. AF, atrial fibrillation; CAD, coronary artery disease; CHD, congenital heart disease; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HTN, hypertension.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has led to a paradigm shift in the delivery of ambulatory cardiovascular care.1,2 The enactment of social distancing policies to minimize the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission resulted in the rapid uptake of telemedicine (TM), which now serves as the primary modality by which patients receive outpatient care.2,3 Although up to half of all healthcare institutions in the USA reported TM use prior to the COVID-19 pandemic, its integration into routine care remained exceedingly limited. With the expansion of TM services to all beneficiaries by the Centre for Medicare and Medicaid Services (CMS) and the establishment of payment parity for healthcare providers in response to the COVID-19 pandemic,4 TM is gaining traction as a suitable adjunct to in-person care. Although previously proposed as a mechanism to improve access for underserved populations, there is limited data on the characteristics of patients who engage in TM services, and specifically, on the predictors of use of TM among patients receiving ambulatory cardiovascular care.
Racial and ethnic minorities are adversely impacted by disparities in cardiovascular care.5–8 The higher prevalence of diabetes, obesity, hypertension, and various forms of cardiovascular disease in Black and Hispanic populations alike5 has led to disproportionately poorer clinical outcomes in these and other vulnerable communities during the COVID-19 pandemic.9 This study aims to explore the demographic, socioeconomic, and clinical characteristics of patients who engaged in TM care during the COVID-19 pandemic.
Methods
Study group
This is a retrospective, single-centre study of all adult ambulatory patients (>18 years) who completed at least one outpatient cardiology encounter, either in-person, by TM video, or by TM phone, at the Massachusetts General Hospital (MGH) in Boston, Massachusetts during the initial peak of the COVID-19 pandemic between 16 March and 19 June 2020. This period was defined as coinciding with the Commonwealth of Massachusetts State of Emergency declaration on 10 March 2020, local stay at home orders, and the transition of routine health care services to TM starting on 15 March 2020.10 Whereas nationally, CMS retroactively enacted payment parity for all telehealth visits on 29 April 2020, in the state of MA, payment parity for telehealth services was implemented by the MA state governor on 15 March 2020.10 During the study period, TM became the dominant modality by which patients received ambulatory cardiac care at the MGH. Importantly, these local changes to payment guidelines pre-dated our study period (16 March–19 June 2020), were consistent throughout this interval, and would not have impacted the distribution of patient encounter types.
We also identified all outpatient cardiovascular visits performed during an identical timeframe 1 year prior (16 March 2019 to 19 June 2019) to ascertain there were no significant changes in the demographics of our study cohort and to establish a baseline comparator. Demographic data, including common cardiovascular comorbidities, was collected for all patients. Patients who missed or cancelled visits during this period were excluded from this initial analysis. Data were deduplicated to ensure that each medical record number (MRN) was associated with only one unique outpatient cardiology encounter type, i.e., only one of each (in-person, TM video, or TM phone) were included per MRN during the study period.
Sociodemographic characteristics assessed included age, sex, race, ethnicity, preferred language, insurance type/primary payor, patient portal enrolment, and zip-code linked median household income (MHI). MHI used in this study were paired to patient zip code, and local economic data for each zip code were acquired from the US Census Bureau and represents data from year 2018. Comorbidities including atrial fibrillation/atrial flutter, coronary artery disease (CAD), congenital heart disease, diabetes, hyperlipidaemia, hypertension, systolic and diastolic heart failure (HF), obesity, history of SARS-COV-2 infection, substance use disorder, alcohol use disorder, and tobacco use were included a priori using International Statistical Classification of Diseases and Related Health Problems 10th revision (ICD-10) codes. Differences in the clinical and sociodemographic characteristics were then evaluated by visit type with the in-person group held as the reference.
Data management
Data were mined from the MGH Cardiology Telemedicine Registry. The MGH Cardiology TM Registry is an ongoing, single-centre based, observational registry of all ambulatory cardiology patients engaging in care via TM within general cardiology and subspecialty clinics. This registry was approved by the Mass General Brigham Healthcare Institutional Review Board.
Statistical analyses
The association of sociodemographic and socioeconomic determinants with cardiology visit type was examined using Chi-squared χ2 test of proportions and Student’s t-test for categorical and continuous variables, respectively. Quantitative and categorical variables were reported as frequencies and proportions. Two-way analysis of variance was used to compare the averaged median income among racial/ethnic groups and among encounter types. Univariate and multivariate logistic regression was then performed to identify factors that affect the odds of engaging in a TM visit. Models were adjusted for age, sex, race/ethnicity, primary language, insurance type/primary payor, MHI, cardiovascular comorbidities, and history of SARS-COV-2 infection. Income groups ‘below $50 000’ and ‘$50 000–$75 000’ were compared to patients whose MHI were more than the averaged MHI for MA State in 2018 (i.e. >$79 835, US Census Bureau). Income groups ‘$100 000–$150 000’ and ‘above $150 000’ were compared to patients whose MHI were less than the averaged MHI for MA State in 2018 (i.e. <$79 835). Two-tailed P-value <0.05 was determined to be the level statistical significance for all tests. SAS version 9.4 and R (version 4.0.1) programming software were used for all statistical analyses.
Results
Baseline characteristics
A total of 8446 ambulatory cardiology patient encounters were assessed during the height of the COVID-19 pandemic in Massachusetts state (16 March–19 June 2020). The baseline characteristics of all patient encounters assessed during the 2020 study period are detailed in Table 1. Of the 8446 patients [86% non-Hispanic (NH) White, 58% male, median age 66.9 ± 15.2], a majority engaged through TM encounters with phone (n = 4981, 61.5%) and video (n = 2693, 33.2%).
Table 1.
Characteristics of ambulatory cardiology patients seen during the COVID-19 pandemic by encounter type
| March to June 2020 |
||||
|---|---|---|---|---|
| All patients | TM phone | TM video | In-person | |
| N (%) | 8446 | 5076 (60.1) | 2944 (34.9) | 426 (5.0) |
| Age (years), mean ± SD | 66.8 ± 15.2 | 69.7 ± 14.0 | 62.1 ± 16.0 | 65.6 ± 15.5 |
| Sex, n (%) | ||||
| Female | 3577 | 2176 (42.9) | 1233 (41.9) | 168 (39.4) |
| Male | 4869 | 2900 (57.1) | 1711 (58.1) | 258 (60.6) |
| Preferred language, n (%) | ||||
| English | 7961 | 4728 (93.1) | 2839 (96.4) | 394 (92.5) |
| Non-English | 485 | 384 (6.9) | 105 (3.6) | 32 (7.5) |
| Race/Ethnicity, n (%) | ||||
| NH White | 7269 | 4336 (85.4) | 2582 (87.7) | 351 (82.4) |
| NH Black | 300 | 200 (3.9) | 74 (2.5) | 26 (6.1) |
| Hispanic (all races) | 288 | 193 (3.8) | 67 (2.3) | 23 (5.4) |
| NH Asian | 276 | 163 (3.2) | 104 (3.5) | 9 (2.1) |
| NH othera | 127 | 75 (1.5) | 44 (1.5) | 8 (1.9) |
| Declined/unavailable | 191 | 109 (2.2) | 73 (2.5) | 9 (2.1) |
| Patient portal enrolment, n (%) | ||||
| Yes (active) | 5540 | 2965 (58.4) | 2314 (78.6) | 261 (61.3) |
| No (inactive) | 2906 | 2111 (41.6) | 630 (21.4) | 165 (38.7) |
| Insurance, n (%) | ||||
| Commercial | 2998 | 1409 (27.8) | 1450 (49.3) | 139 (32.6) |
| Medicaid | 392 | 245 (4.8) | 114 (3.9) | 33 (7.8) |
| Medicare | 5012 | 3393 (66.8) | 1367 (46.4) | 252 (59.2) |
| Uninsured | 20 | 15 (0.3) | 3 (0.1) | 2 (0.5) |
| Unavailable | 24 | 14 (0.3) | 10 (0.3) | 0 (0.0) |
| Comorbidities, n (%) | ||||
| Atrial fibrillation/atrial flutter | 2258 | 1432 (28.2) | 714 (24.3) | 112 (26.3) |
| Coronary artery disease | 2854 | 1872 (36.9) | 874 (29.7) | 108 (25.4) |
| Congenital heart disease | 143 | 51 (1.0) | 89 (3.0) | 3 (0.7) |
| Hypertension | 3889 | 2547 (50.2) | 1164 (39.5) | 178 (41.8) |
| Systolic heart failure | 1140 | 715 (14.1) | 327 (11.1) | 98 (23.0) |
| Diastolic heart failure | 620 | 433 (8.5) | 146 (5.0) | 41 (9.6) |
| Diabetes | 394 | 258 (5.1) | 109 (3.7) | 27 (6.3) |
| Hyperlipidaemia | 2328 | 1481 (29.2) | 766 (26.0) | 81 (19.0) |
| Obesity | 161 | 84 (1.7) | 74 (2.5) | 3 (0.7) |
| SARS-CoV-2 positive | 51 | 39 (0.8) | 10 (0.3) | 2 (0.5) |
| Substance use disorder | 1 | 0 (0.0) | 1 (0.03) | 0 (0.0) |
| Tobacco | 37 | 25 (0.5) | 12 (0.4) | 0 (0.0) |
| Alcohol use disorder | 3 | 2 (0.04) | 1 (0.03) | 0 (0.0) |
| Median annual household income in USDb | 97 137 ± 35 767 | 94 637 ± 35 151 | 102 692 ± 36 671 | 88 543 ± 31 484 |
NH, non-Hispanic.
NH other includes the following racial categories: Native Hawaiian, Pacific Islander, American Indian, and Alaska Native.
Median household income assessed were acquired from US Census Bureau zip code data, 2018.
There was a substantial increase in TM encounters (60% phone, 35% video, 5% in-person visit) in 2020 compared to a similar time frame in 2019 with a quantitative preponderance of patients from Northern and Eastern Massachusetts (Supplementary material online, Figure S1). By comparison, there were 14 428 ambulatory cardiology patient encounters between 16 March and 19 June 2019 with more than 99% of patients seen in-person and 48 total TM visits. Of patients seen in 2020, there were no differences in the sex, age, racial/ethnic demographics, primary language, or insurance type/primary payor when compared with those who engaged in traditional in-person ambulatory cardiovascular care in 2019 (Supplementary material online, Table S1).
Sociodemographic predictors of TM use
Race/ethnicity, age, and patient portal enrolment
NH-Blacks [odds ratio (OR) 0.56, 95% confidence interval (CI): 0.35–0.94; P-value = 0.02] and Hispanics (OR 0.53, 95% CI: 0.29–0.98; P = 0.04) were less likely to have a TM video encounter when compared with NH-Whites (Table 2, Supplementary material online, Table S2). A total of 2944 individuals engaged in TM video visits, of whom 663 (22.5%) of the patients were over the age of 75 years. However, the likelihood of a TM video encounter in individuals over age 85 years was significantly lower when compared with patients less than 65 years of age (OR 0.56, 95% CI: 0.35–0.93; P = 0.01). Individuals above age 75 years had a higher proportion of TM phone over TM video use. There was a trend towards increased video use with decreasing age.
Table 2.
Likelihood telemedicine encounter during the COVID-19 pandemic
| Encounter type |
||||||
|---|---|---|---|---|---|---|
| Video vs. in-person |
Phone vs. in-person |
Telemedicine vs. in-person (phone and video) |
||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (in years, <65 = ref) | ||||||
| >65–74 | 0.90 (0.64–1.27) | 0.536 | 1.13 (0.82–1.56) | 0.443 | 1.02 (0.75–1.41) | 0.880 |
| >75–84 | 0.94 (0.63–1.41) | 0.775 | 1.58 (1.09–2.28) | 0.015 | 1.30 (0.90–1.88) | 0.166 |
| >85 | 0.56 (0.35–0.93) | 0.022 | 1.46 (0.95–2.30) | 0.089 | 1.11 (0.71–1.73) | 0.655 |
| Sex (male = ref) | ||||||
| Female | 1.09 (0.87–1.36) | 0.442 | 1.20 (0.97–1.49) | 0.085 | 1.18 (0.96–1.46) | 0.110 |
|
Race/Ethnicity (NH White = ref) |
||||||
| Hispanic (all races) | 0.53 (0.29–0.98) | 0.046 | 0.89 (0.54–1.52) | 0.655 | 0.78 (0.48–1.33) | 0.344 |
| NH Black | 0.56 (0.35–0.94) | 0.024 | 0.78 (0.51–1.24) | 0.273 | 0.70 (0.46–1.11) | 0.114 |
| NH Asian | 1.65 (0.84–3.64) | 0.178 | 1.63 (0.85–3.51) | 0.173 | 1.65 (0.87–3.53) | 0.157 |
| NH othera | 1.08 (0.63–1.97) | 0.783 | 1.06 (0.64–1.88) | 0.834 | 1.04 (0.63–1.83) | 0.889 |
| Preferred language (English = ref) | ||||||
| Non-English | 0.69 (0.43–1.14) | 0.143 | 1.03 (0.67–1.62) | 0.905 | 0.91 (0.60–1.43) | 0.673 |
| Patient portal enrolment (No = ref) | ||||||
| Yes | 2.09 (1.66–2.63) | <0.0001 | 0.82 (0.66–1.02) | 0.075 | 0.93 (0.75–1.15) | 0.513 |
| Insurance (commercial = ref) | ||||||
| Medicare | 0.65 (0.47–0.89) | 0.009 | 1.06 (0.78–1.44) | 0.689 | 0.87 (0.64–1.18) | 0.388 |
| Medicaid | 0.50 (0.32–0.79) | 0.003 | 0.86 (0.57–1.33) | 0.479 | 0.70 (0.46–1.06) | 0.077 |
| Uninsured | 0.47 (0.73–3.75) | 0.425 | 0.91 (0.24–5.92) | 0.900 | 0.65 (0.18–4.20) | 0.575 |
|
MHI groups below MA state mean MHI (>$79 835 = ref)b |
||||||
| <$50 000 | 0.63 (0.39–1.06) | 0.069 | 0.95 (0.62–1.53) | 0.833 | 0.83 (0.54–1.32) | 0.416 |
| $50 000–$75 000 | 0.59 (0.47–0.77) | <0.0001 | 0.89 (0.71–1.11) | 0.301 | 0.79 (0.63–0.99) | 0.038 |
| $75 000–$100 000 | 0.65 (0.42–1.06) | 0.072 | 0.71 (0.46–1.14) | 0.135 | 0.70 (0.46–1.11) | 0.115 |
|
MHI groups above MA state mean MHI (<$79 835 = ref)b |
||||||
| $100 000–$150 000 | 1.69 (1.30–2.19) | 0.0002 | 1.09 (0.90–1.48) | 0.481 | 1.31 (1.03–1.68) | 0.030 |
| >$150 000 | 4.20 (2.45–7.78) | <0.0001 | 2.29 (1.35–4.20) | 0.004 | 2.94 (1.74–5.37) | <0.001 |
| Comorbidities (No = ref) | ||||||
| AF/flutter | 1.03 (0.80–1.33) | 0.822 | 1.14 (0.90–1.46) | 0.266 | 1.08 (0.86–1.37) | 0.509 |
| CAD | 1.28 (1.00–1.65) | 0.056 | 1.57 (1.24–1.99) | 0.0002 | 1.45 (1.15–1.84) | 0.002 |
| Congenital | 3.55 (1.29–14.07) | 0.035 | 1.59 (0.57–6.61) | 0.440 | 2.51 (0.93–10.24) | 0.119 |
| SARS-CoV-2 | 1.00 (0.23–6.93) | 0.999 | 2.19 (0.65–13.7) | 0.287 | 1.71 (0.51–10.64) | 0.463 |
| Diabetes | 0.63 (0.40–1.02) | 0.051 | 0.70 (0.46–1.09) | 0.098 | 0.66 (0.44–1.03) | 0.056 |
| Hyperlipidaemia | 1.28 (0.97–1.70) | 0.086 | 1.53 (1.17–2.01) | 0.002 | 1.45 (1.12–1.90) | 0.006 |
| Hypertension | 0.81 (0.65–1.02) | 0.074 | 1.14 (0.92–1.41) | 0.220 | 1.02 (0.83–1.26) | 0.865 |
| Diastolic HF | 0.55 (0.38–0.82) | 0.003 | 0.75 (0.53–1.08) | 0.107 | 0.67 (0.48–0.97) | 0.026 |
| Systolic HF | 0.46 (0.35–0.61) | <0.0001 | 0.66 (0.51–0.85) | 0.001 | 0.59 (0.46–0.76) | <0.0001 |
| Obesity | 3.21 (1.16–13.3) | 0.052 | 2.78 (1.02–11.46) | 0.085 | 2.88 (1.08–11.74) | 0.073 |
Odds ratios adjusted for age, sex, race/ethnicity, primary language, MHI, insurance type/primary payor, and co-morbidities including AF/flutter, CAD, SARS-CoV-2, congenital heart disease, diabetes, diastolic and systolic heart failure, hyperlipidaemia, hypertension, and obesity.
AF, atrial fibrillation; CAD, coronary artery disease; HF, heart failure; MHI, Median Household Income; NH, Non-Hispanic.
NH other includes the following racial categories: Native Hawaiian, Pacific Islander, American Indian, and Alaska Native.
Median household income assessed were acquired from US Census Bureau zip code data, 2018. Massachusetts State mean household income used as reference ($79 835).
During both time periods (2019 and 2020), two-thirds of the patients who engaged in any ambulatory cardiovascular care were enrolled in the patient portal (a requisite for TM video visits). Individuals above 85 years had disproportionately lower patient portal enrolment (OR 0.56, 95% CI: 0.35–0.93; P = 0.02) when compared with patients less than 65 years (Table 3, Supplementary material online, Table S3). Additionally, Hispanic ethnicity, NH-Black race, non-English preferred language, Medicare, Medicaid, MHI <$75 000 were also independently associated with lower patient portal enrolment (Supplementary material online, Table S3).
Table 3.
Characteristics of ambulatory cardiology patients seen during the COVID-19 pandemic stratified by age
| Age strata, n (%) |
||||
|---|---|---|---|---|
| <65 | >65–74 | >75–84 | >85 | |
| March–June 2020 | 3166 (37.5) | 2424 (28.7) | 2039 (24.1) | 817 (9.7) |
| Sex, n (%) | ||||
| Female | 1378 (43.5) | 983 (40.6) | 827 (40.6) | 389 (47.6) |
| Male | 1788 (56.5) | 1441 (59.4) | 1212 (59.4) | 428 (52.4) |
| Visit type, n (%) | ||||
| In-person | 169 (5.3) | 129 (5.3) | 87 (4.3) | 41 (5.0) |
| Telemedicine phone | 1538 (48.6) | 1473 (60.8) | 1434 (70.3) | 631 (77.2) |
| Telemedicine video | 1459 (46.1) | 822 (33.9) | 518 (25.4) | 145 (17.8) |
| Preferred language, n (%) | ||||
| English | 3004 (94.9) | 2286 (94.3) | 1910 (93.7) | 761 (93.1) |
| Non-English | 162 (5.1) | 138 (5.7) | 129 (6.3) | 56 (6.9) |
| Race/Ethnicity, n (%) | ||||
| NH White | 2526 (79.8) | 2133 (88.0) | 1858 (91.1) | 752 (92.0) |
| NH Black | 168 (5.3) | 77 (3.2) | 43 (2.1) | 12 (1.5) |
| Hispanic (all races) | 177 (5.6) | 67 (2.8) | 29 (1.4) | 10 (1.2) |
| NH Asian | 131 (4.1 | 70 (2.9) | 57 (2.8) | 18 (2.2) |
| NH othera | 71 (2.2) | 30 (1.2) | 16 (0.8) | 10 (1.2) |
| Declined/unavailable | 93 (2.9) | 47 (1.9) | 36 (1.8) | 15 (1.8) |
| Patient portal enrolment, n (%) | ||||
| Yes (active) | 2152 (68.0) | 1695 (69.9) | 1293 (63.4) | 400 (49.0) |
| No (inactive) | 1014 (32.0) | 729 (30.1) | 746 (36.6) | 417 (51.0) |
| Insurance, n (%) | ||||
| Commercial | 2407 (76.0) | 443 (18.3) | 115 (5.6) | 33 (4.0) |
| Medicaid | 342 (10.8) | 22 (0.9) | 20 (1.0) | 8 (1.0) |
| Medicare | 383 (12.1) | 1950 (80.4) | 1904 (93.4) | 775 (94.9) |
| Uninsured | 17 (0.5) | 3 (0.1) | 0 (0.0) | 0 (0.0) |
| Unavailable | 17 (0.5) | 6 (0.3) | 0 (0.0) | 1 (0.1) |
| Median annual household income in USDb | 94 713 ± 35 579 | 96 104 ± 34 673 | 100 675 ± 36 523 | 100 770 ± 36 852 |
NH, non-Hispanic.
NH other includes the following racial categories: Native Hawaiian, Pacific Islander, American Indian, and Alaska Native.
Median household income assessed were acquired from US Census Bureau zip code data, 2018.
Primary language and interpreter services use
Patients requiring the use of interpreter services were also assessed. 94% of patients cited English as their primary/preferred language. The primary languages requested for interpreter services were Spanish (n = 158), followed by Mandarin (n = 33), Italian (n = 33), Portuguese (n = 28), and Russian (n = 26). Interpreter services were used more frequently during TM phone vs. TM video visits (33% vs. 8% of visits). Of individuals who engaged in a TM phone visit, 70% had previously used formal interpreter services, while 52% of TM video visit users had previous experience with interpreter services. There were many individuals who utilized family members for interpretation despite readily available services. This was true in 31.9% of all TM phone encounters and in 45.8% of all TM video encounters. Non-English speakers were less likely to use TM video visits compared with English speakers (unadjusted OR 0.46, 95% CI: 0.31–0.70; P < 0.001); however, these differences became non-significant when adjusted for insurance, MHI, sex, age, cardiovascular comorbidities, and history of SARS-CoV-2 infection (Table 2, Supplementary material online, Tables S2 and S4).
Socioeconomic predictors of TM use
Of the 8446 patients assessed, most were insured (58% Medicare, 37% commercial, 4.6% Medicaid). Carriers of public insurance (Medicaid OR 0.50, 95% CI 0.32–0.79; P = 0.003, Medicare OR 0.65, 95% CI: 0.47–0.89; P = 0.009) had a lower likelihood of a TM video encounter compared to carriers of commercial insurance. There was an equal distribution of TM phone and TM video encounters (47% vs. 48%) for carriers of commercial insurance. The uninsured population had a non-significant trend towards higher utilization of in-person visits during the 2020 timeframe. NH-Blacks (OR 1.68, 95% CI: 1.05–2.61; P = 0.02) and Hispanics (OR 2.70, 95% CI: 1.63–4.40; P < 0.0001) were more likely to carry Medicaid when compared with NH-Whites.
Average MHI was lowest in the in-person encounter group and highest in the TM video encounter group (in-person: $88 543, TM phone: $94 637, and TM video: $102 692, P < 0.0001). Average MHI was also lowest for NH-Blacks ($70 612 ± 27342, mean ± SD) and Hispanics ($71 786 ± 31027). Individuals with an MHI $50 000–$75 000 (OR 0.65, 95% CI: 0.47–0.77; P < 0.0001) were less likely to have a TM video visit when compared with those earning more than Massachusetts state MHI ($79 835). This was also true for MHI <$50 000 but became non-significant after multivariate assessment. Furthermore, individuals within the income bracket $50 000–$75 000 were slightly more likely to have an in-person visit (OR 1.26, 95% CI: 1.01–1.59; P = 0.04) when compared with those earning more than state MHI ($79 835). Individuals with MHI $100 000–$150 000 (OR 1.69, 95% CI: 1.30–2.19; P = 0.0002) and MHI >$150 000 (OR 4.20, 95% CI: 2.45–7.78; P < 0.0001) had a very high likelihood of a TM video encounter when compared with those making less than state MHI ($79 835).
Clinical predictors of TM use
Medical comorbidities with a higher likelihood of a TM visit (phone and video) included CAD (OR 1.45, 95% CI: 1.15–1.84; P = 0.002) and HLD (OR 1.45, 95% CI: 1.12–1.90; P = 0.006). Patients with congenital heart disease had a higher likelihood of a TM video encounter (OR 3.55, 95% CI: 1.29–14.07; P = 0.03). Of note, there was a lower likelihood of a TM video encounter in individuals with HF with preserved ejection fraction (HFpEF) (OR 0.55, 95% CI: 0.38–0.82; P = 0.003) and HF with reduced ejection fraction (HFrEF) (OR 0.46, 95% CI: 0.35–0.61; P < 0.0001) and a higher likelihood of an in-person encounter in patients with HFrEF (OR 1.70, 95% CI: 1.32–2.18; P < 0.0001) and HFpEF (OR 1.48, 95% CI: 1.03–2.08; P = 0.03).[AQ: Please spell out HLD (if necessary).]
On further assessment, NH-Black race, Hispanic ethnicity, carriers of public insurance (Medicaid and Medicare), uninsured patients, and MHI income $50 000–$75 000 were associated with higher likelihood of carrying a diagnosis of systolic HF. Age >65, female sex, public insurance, MHI <$50 000, diagnosis of atrial fibrillation, and hypertension were associated with a higher likelihood of carrying a diagnosis of diastolic HF (Supplementary material online, Table S5).
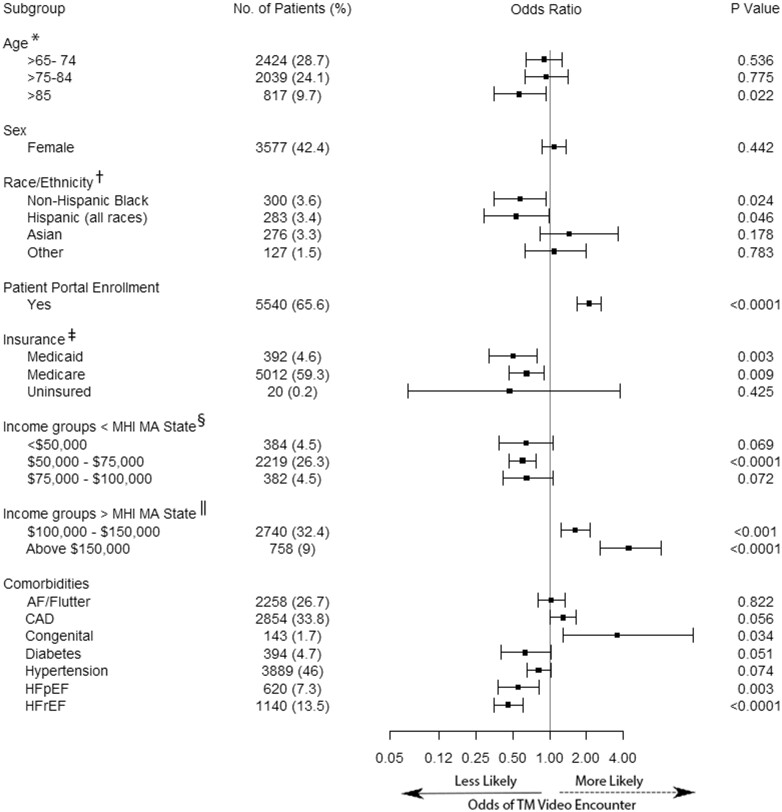
Overall, NH-Black race, Hispanic ethnicity (all races), age >85 years, MHI less than state average, public insurance, and patients with a diagnosis of HF (diastolic or systolic) were associated with a lower likelihood of TM video encounter during the COVID-19 pandemic (Table 2, Supplementary material online, Table S2, Figure 1).
Figure 1.
Determinants of telemedicine video use during the COVID-19 pandemic. Odds ratios were adjusted for age, sex, language, race/ethnicity, median household income, insurance, and cardiovascular comorbidities including HFrEF, HFpEF, CAD, HTN, HLD, AF, CHD, as well as previous SARS-CoV-2 infection. References for each subgroup are as follows: aAge < 65 (n = 3389, 40%). bNon-Hispanic White (n = 7361, 87%). cCommercial Insurance (n = 2998, 36%). dAbove Median Household Income (MHI) Massachusetts State $79 835—US Census Bureau (n = 5461, 65%). eBelow Median Household Income (MHI) Massachusetts State $79 835—US Census Bureau (n = 2985, 35%). AF, atrial fibrillation; CAD, coronary artery disease; CHD, congenital heart disease; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HTN, hypertension.
Discussion
The findings in this study show that pervasive inequities in access to TM care disparately impact cardiovascular patients based on socioeconomic, demographic, and clinical factors. We found that older age (particularly >85 years), NH-Black and Hispanic race/ethnicity, low MHI, public insurance, and patients with a diagnosis of systolic or diastolic HF were independently associated with lower TM utilization, and particularly lower TM video encounters (Graphical abstract). Our work adds to prior observations on disparities in TM in ambulatory cardiology11 and is among the first to describe specific clinical cardiology determinants of TM utilization.
Elderly patients were found to have decreased access to TM video encounters during the COVID-19 pandemic. In addition to an independently lower odds of TM video engagement in patients older than age 85, there was also a linear trend towards TM video underutilization as age increased, disproportionately affecting patients older than age 75 years. Concurrently, there was a greater likelihood of TM phone utilization in patients older than 75 years. Although socioeconomic status may contribute to lack of device ownership12 and broadband access,13 lack of digital literacy and hesitancy to adopt new health technology due to insufficient dexterity, visual impairment, and cognitive dysfunction may also contribute to decreased TM utilization in the elderly.14,15 Within our cohort, 33.8% of patients seen were within susceptible age groups associated with reduced TM engagement (particularly those above 75 years).
In our cohort of ambulatory cardiology patients, NH-Black race and Hispanic ethnicity were also associated with significantly lower TM video use. It is well established that socioeconomic adversity leads to poorer cardiovascular outcomes and reduced lifespan in certain vulnerable patient groups.5,8,16 Furthermore, the association between health care disparities and social determinants of health has been heightened by the disproportionate impact of COVID-19 on Black and Hispanic communities.9,17 To this end, socioeconomic status may serve as a more significant driver of reduced access to health technology, reduced engagement in TM, and poor adoption of digital health among NH-Black and Hispanic patients.17
While investigating the impact of socioeconomic status on TM use, we found that MHI less than the Massachusetts state average and public health insurance (Medicaid and Medicare) were independently associated with lower access to TM video care and TM use overall. Additionally, NH-Black and Hispanic patients were demonstrated to have the lowest average MHI within our cohort of cardiovascular patients and were also more likely to use Medicaid as a primary payor. Although outside the scope of this article, we recognize the impact of housing and neighbourhood socioeconomics on cardiovascular health outcomes and the crucial effect of MHI on housing stability and resource accessibility.18 Lower MHI, for example, has been directly linked to limited access to broadband internet,17 a requisite for TM video participation. As of 2019, an estimated 21.3 million people completely lacked broadband internet access according to the Federal Communications Commission (FCC). As efforts are being made to understand and improve the digital divide, socioeconomic inequality remains a significant contributor to uneven access to health technology across vulnerable communities.19,20
The use of TM video specifically for patients with HF has yet to be thoroughly investigated and is the subject of ongoing study in our cohort. This study reveals disproportionate underutilization of TM amongst patients with both diastolic and systolic HF. Black patients of both sexes face higher HF-related hospitalization and a disproportionately higher mortality rate compared to other races and ethnicities. This is particularly true among younger age groups (35–64 years).7,21 Our results agree with prior studies demonstrating that NH-Black, Hispanics, and patients with low income were more likely to carry a diagnosis of HF in our cohort.5,7 Structured telephone and video support coupled with telemonitoring may prove a cost-effective approach to reductions in HF-related hospitalizations.22,23 Although there is a clinical need for greater objectivity when assessing patients with HF (especially during titration of medications and optimization of volume status), the coupling of TM and remote monitoring may introduce an opportunity to address access barriers and improve HF outcomes.
To start understanding and ultimately target systems-based factors that contribute to reduced TM access, we assessed patient portal enrolment in our cohort of cardiovascular patients. Here, we demonstrate that NH-Blacks and Hispanics, individuals above age 85 years, those who preferred a non-English language, carriers of Medicare and Medicaid, as well as patients with an average MHI less than $75 000 had a disproportionately lower likelihood of being enrolled in the patient portal. In a cross-sectional analysis of personal health record adoption that included our healthcare system, NH-Blacks, Hispanics, and patients of lower socioeconomic status were less likely than Whites to access their personal health records.24 We show here that these disparities appear to persist nearly a decade later. If patient portal activation is required for patient engagement in TM video visits, lack of enrolment may stand yet another targetable barrier to dismantling equities in TM access.
In addition to patient portal enrolment, we sought to assess the effect of primary/preferred language on TM use. Although non-English language was not independently associated with TM use after multivariable analysis, there was a trend towards reduced utilization in our univariate evaluation. We also found that use of interpreter services was far higher in our TM phone group when compared with the video cohort. Notably, patients whose preferred language was other than English were under-represented within our study cohort. Nonetheless, we noted only 33% with TM phone visits and 8% of TM video visits of non-English speaking patients received formal hospital-provided interpretation services during their encounter and a higher proportion received interpretation assistance from a family member instead (Supplementary material online, Table S3). Prior studies have shown that use of professional interpreters not only increases patient satisfaction, but also improves adherence and outcomes, and reduces adverse events.25,26
The dynamic and co-dependent determinants of TM utilization described herein including socioeconomic status (MHI and primary payor), age above 85 years, Black race, Hispanic ethnicity, non-English language, and diagnosis of HF all have a direct and potentially additive impact on access to TM care during the COVID-19 pandemic and could lead to worse longitudinal cardiovascular outcomes in these already vulnerable groups.
Strengths and limitations
There are several limitations to this study. It is a retrospective study at a single academic medical centre with a largely NH-White population and high state median income. Nonetheless, our large TM registry provided a very robust set of data to perform multivariate evaluation of TM utilization amongst cardiovascular patients seen during the COVID-19 pandemic. Although our study also did not assess clinical outcome data or follow up and was not designed to evaluate differences in the quality of healthcare delivered to patients via TM, to our knowledge, we are the first to find that a diagnosis of HF was associated with lower TM engagement. This study revealed that older adults and certain racial and ethnic minorities had reduced access to TM care. Concomitantly, we recognize that these populations were also disproportionately affected by COVID-19, which may have influenced their attempts to access ambulatory care, but during our study period, 51 patients out of 8449 had a history of SARS-CoV-2 infection and had no impact on adjusted ORs reported here. Importantly, we recognize the need for community-based intervention, and while subsequent analyses from our group will aim to use zip-code linked MHI to investigate the direct impact of neighbourhood socioeconomics and housing on TM engagement, these factors were not within the scope of our study. Furthermore, while our zip-code linked MHI data may give insight into regional socioeconomic vulnerabilities, it lacks precision for individual/patient-based MHI. Differential access to internet services, smartphones, and devices compatible with TM applications may have contributed to the differences in TM usage and is an area of already planned future studies by our Telemedicine Equity Task Force. Lastly, we did not assess educational level, health and digital literacy, and trust in the medical community in these populations which may also affect their ability to access care.
Clinical implications
As practice patterns evolve over the coming months and years to integrate more digital platforms, providers will need to reassess potential barriers to effectively deliver equitable cardiovascular care. For example, lack of access to hardware and broadband internet, poor digital literacy, and limited English proficiency may foster bias, decrease TM access, exacerbate inequities in care delivery, and worsen clinical outcomes in marginalized populations.8 Once the predictors that impact equitable TM access in ambulatory cardiovascular care delivery are well understood, a framework can be developed for implementation strategies to dismantle the sociodemographic and technological barriers affecting healthcare access for vulnerable populations in this era of rapidly evolving TM uptake.
Conclusion
NH-Black race, Hispanic ethnicity, age above 85 years, public insurance (Medicaid/Medicare), MHI of <$75 000, and a diagnosis of HF were all independently associated with a lower likelihood of TM video engagement during the COVID-19 pandemic. Our findings call to action the dismantling of sociodemographic, socioeconomic, and technological barriers to healthcare access for vulnerable patient groups to improve the delivery of equitable TM care.
Supplementary material
Supplementary material is available at European Heart Journal – Digital Health online.
Supplementary Material
Acknowledgements
Joseph Locascio, PhD (biostatistics support).
Conflict of interest: J.P.S.: has consulted for Biotronik, Boston Scientific Corp, Medtronic Inc, Abbott Inc, Cardiologs, Microport Inc, EBR Inc, Impulse Dynamics, Nopras Inc, New Century Health, OrchestraBioMed Inc, Sanofi Inc and Toray Inc. A.B.B.: has consulted for EkoHealth, AstraZeneca, Bristol Myers Squibb, and Novartis. All other authors have declared no conflict of interest.
Data availability
Data that support the findings in this study are available on reasonable request from corresponding author.
References
- 1. Webster P. Virtual health care in the era of COVID-19. Lancet 2020;395:1180–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay R, Rasmusson K, et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the Heart Failure Society of America. J Card Fail 2020;26(6):448–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ateev Mehrotra MC, David L, Hilary H, David C. “What Impact Has COVID-19 Had on Outpatient Visits?” Commonwealth Fund, 19 May 2020, www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits. (Accessed 12 April 2021).
- 4.Center for Medicare & Medicaid Services (CMS). “Press Release CMS Approves Medicaid Section 1135 Waivers for 11 Additional States in Response to COVID-19.” CMS, 23 Mar. 2020, www.cms.gov/newsroom/press-releases/cms-approves-medicaid-section-1135-waivers-11-additional-states-response-covid-19. (Accessed 12 April 2021).
- 5.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics—2020 update: a report from the American Heart Association. Circulation 2020;141:e139–e596. [DOI] [PubMed] [Google Scholar]
- 6. Mensah GA, Roth GA, Fuster V.. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol 2019;74:2529–2532. [DOI] [PubMed] [Google Scholar]
- 7. Nayak A, Hicks AJ, Morris AA.. Understanding the complexity of heart failure risk and treatment in black patients. Circ Heart Fail 2020;13:e007264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council Social determinants of risk and outcomes for cardiovascular disease. Circulation 2015;132:873–898. [DOI] [PubMed] [Google Scholar]
- 9. Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. [DOI] [PubMed] [Google Scholar]
- 10. Baker CD, Polito KE. “March 15 2020 Telehealth Order.”. Mass.gov, 15 Mar. 2020, www.mass.gov/doc/march-15-2020-telehealth-order. (Accessed 12 April 2021).
- 11.Eberly LA, Khatana SAM, Nathan AS, Snider C, Julien HM, Deleener ME, Adusumalli S Telemedicine outpatient cardiovascular care during the COVID-19 pandemic. Circulation. 2020;142:510–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pew Research Center. “Demographics of Mobile Device Ownership and Adoption in the United States.” Pew Research Center: Internet, Science & Tech, 7 Apr. 2021, www.pewinternet.org/fact-sheet/mobile. (Accessed 12 April 2021).
- 13.FCC. “2020 Broadband Deployment Report.” Federal Communications Commission FCC 20-50. 24 Apr. 2020, docs.fcc.gov/public/attachments/FCC-20-50A1.pdf. (Accessed 12 April 2021).
- 14.Krishnaswami A, Beavers C, Dorsch MP, Dodson JA, Masterson Creber R, Kitsiou S, Goyal P, Maurer MS, Wenger NK, Croy DS, Alexander KP, Batsis JA, Turakhia MP, Forman DE, Bernacki GM, Kirkpatrick JN, Orr NM, Peterson ED, Rich MW, Freeman AM, Bhavnani SP; Innovations, Cardiovascular Team and the Geriatric Cardiology Councils, American College of Cardiology. Gerotechnology for older adults with cardiovascular diseases: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;76:2650–2670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Levy H, Janke AT, Langa KM.. Health literacy and the digital divide among older Americans. J Gen Intern Med 2015;30:284–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, Yancy CW; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Functional Genomics and Translational Biology; and Stroke Council. Cardiovascular Health in African Americans: a scientific statement from the American Heart Association. Circulation 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 17.Nouri S, Khoong EC, Lyles CR, Karliner L. “Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic.” NEJM Catalyst Innovations in Care Delivery, 4 May 2020, catalyst.nejm.org/doi/full/10.1056/CAT.20.0123. (Accessed 12 April 2021).
- 18.Sims M, Kershaw KN, Breathett K, Jackson EA, Lewis LM, Mujahid MS, Suglia SF; American Heart Association Council on Epidemiology and Prevention and Council on Quality of Care and Outcomes Research. Importance of housing and cardiovascular health and well-being: a scientific statement from the American Heart Association. Circ Cardiovasc Qual Outcomes 2020;13:e000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson M, Kumar M. “Digital Divide Persists Even as Lower-Income Americans Make Gains in Tech Adoption.” Pew Research Center, 30 May 2020, www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/. (Accessed 12 April 2021).
- 20. Zhai Y. A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom 2021;90:64–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Glynn P, Lloyd-Jones DM, Feinstein MJ, Carnethon M, Khan SS.. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol 2019;73:2354–2355. [DOI] [PubMed] [Google Scholar]
- 22. Brahmbhatt DH, Cowie MR.. Remote management of heart failure: an overview of telemonitoring technologies. Card Fail Rev 2019;5:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stehlik J, Schmalfuss C, Bozkurt B, Nativi-Nicolau J, Wohlfahrt P, Wegerich S, Rose K, Ray R, Schofield R, Deswal A, Sekaric J, Anand S, Richards D, Hanson H, Pipke M, Pham M. Continuous wearable monitoring analytics predict heart failure hospitalization. Circ Heart Fail 2020;13:e006513. [DOI] [PubMed] [Google Scholar]
- 24. Yamin CK, Emani S, Williams DH, Lipsitz SR, Karson AS, Wald JS, Bates DW. The digital divide in adoption and use of a personal health record. Archiv Intern Med 2011;171:568–574. [DOI] [PubMed] [Google Scholar]
- 25. Juckett G, Unger K.. Appropriate use of medical interpreters. Am Fam Physician 2014;90:476–480. [PubMed] [Google Scholar]
- 26. Lindholm M, Hargraves JL, Ferguson WJ, Reed G.. Professional language interpretation and inpatient length of stay and readmission rates. J Gen Intern Med 2012;27:1294–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data that support the findings in this study are available on reasonable request from corresponding author.