Abstract
Background and Objectives:
The kallikrein (KLK) family of genes consists of 15 members, many of which are highly expressed in number of cancers compared to their normal parent tissues. KLK7 was initially characterized as an enzyme implicated in the degradation of intercellular cohesive structures in the stratum corneum of stratified squamous epithelia, preceding desquamation in the skin. It catalyzes the degradation of desmosomes in the outermost layer of skin and permits cell shedding to take place at the skin surface. Overexpression of KLK7 in tumor cells has been reported to significantly enhance the invasive potential in intracranial malignancies and ovarian cancer cells. Thus, KLK7 could contribute to the degradation of extracellular matrices in oral squamous cell carcinoma (OSCC) tissues, promoting invasion of neoplastic cells locally and facilitating metastasis to regional lymph nodes. The objectives of the present study were to compare the expression of KLK 7 in normal subjects and patients with OSCC, to correlate the expression of KLK 7 with respect to the clinical staging of OSCC and to evaluate the expression of KLK 7with respect to different histopathological grades of OSCC.
Materials and Methods:
Thirty cases of OSCC were staged clinically and graded histopathologically. The immunohistochemical method was used to detect the expression of KLK 7 in OSCC. The scores obtained were documented and compared statistically.
Results:
KLK 7 immunoreactivity was noticed in all cases of OSCC. A statistically significant difference was observed in immunoreactivity of KLK 7 between the normal and OSCC (P = 0.0001*) and in different histopathological grades (P = 0.0001*) and in different clinical stages (P = 0.0127*) of OSCC using Kruskal–Wallis analysis of variance test.
Conclusion:
The KLK 7 immunoexpression histopathologically increased from low grade to high grade and clinically from Stage 1 to Stage 4 in OSCC. Hence, increased expression of KLK 7 may be related to poor prognosis in patients with OSCC.
Keywords: Immunohistochemistry, Kallikrein 7, oral squamous cell carcinoma, prognosis
INTRODUCTION
Oral cancer is the most common cancer worldwide, with results in over 200,000 deaths annually and is one of the top eight most frequently diagnosed cancers worldwide.[1]
Oral squamous cell carcinoma (OSCC) is a malignant neoplasm arising from the stratified squamous epithelium of the oral cavity.[2] It can affect any site of the oral mucosa, with a predilection to the floor of the mouth and tongue.[3] The most common risk factors are smoking, tobacco chewing, reverse smoking and alcohol consumption. Less than 10% of cases arise in women. Moreover, it has got a great tendency to produce metastasis in lymph nodes.[4]
The cellular and biochemical factors that underlie locoregional and distant spread of the disease are poorly understood. Invasion and metastasis of OSCC require multiple cellular events including disruption of cell–cell adhesive contacts, cytoskeletal alterations and basement membrane attachment, matrix protein proteolysis and migration.[5,6] Thus, a more detailed analysis of the molecular events that contribute to OSCC metastasis is a necessary prerequisite for the development.
Kallikrein-related peptidase 7 (KLK 7) was originally isolated from the stratum corneum tissue as a serine protease with chymotrypsin-like activity which was involved in the regulated desquamation of terminally differentiated keratinocytes.[7,8] It was also named as stratum corneum chymotryptic enzyme. KLK 7 is primarily expressed in the skin but is also detected at relatively high levels in the esophagus, heart, liver, central nervous system, kidney, pancreas, mammary and salivary glands.[9,10]
In skin disorders, KLK 7 overexpression and/or increased activity result in over-desquamation.[11,12] KLK 7 undergoes differential splicing in ovarian cancer and it displays tumor-associated overexpression according to animal experiments performed.[13] Increased KLK 7 expression levels have been associated with the prognosis in various types of cancers and its high expression correlates with poor survival in cancer patients.[14] However, its contribution to tumor progression at the molecular level remains mainly unclear and will deserve further investigation.
Hence, the present study was undertaken to evaluate the expression of KLK 7 in normal subjects and in patients with OSCC with respect to clinical staging and histopathological grading.
MATERIALS AND METHODS
Thirty patients of OSCC visiting the outpatient department of our college were included for the purpose of this study. These cases were staged clinically based on tumor node metastasis staging[15] [Table 1] and graded histopathologically using modified Broder's grading system71 [Table 2]. Thirty apparently normal subjects were included as controls for the study.
Table 1.
Number of cases in each clinical stage of oral squamous cell carcinoma
| Clinical stage | Number of cases |
|---|---|
| Stage I | 10 |
| Stage II | 8 |
| Stage III | 7 |
| Stage IV | 5 |
Table 2.
Number of cases in each histological grade of oral squamous cell carcinoma
| Histopathological grade | Number of cases |
|---|---|
| Grade I | 10 |
| Grade II | 12 |
| Grade III | 8 |
Immunohistochemical study
3–4 μm thickness of paraffin-embedded tissue sections from each block were taken and subjected to immunohistochemistry (IHC). KLK 7 polyclonal antibody was used in the present immunohistochemical study and routine staining protocols were carried out in the immunohistochemical technique for the primary antibody.
Interpretation of staining
The presence of brown-colored end product at the site of the target antigen was indicative of positive immunoreactivity for KLK 7. Skin tissue was taken as a positive control for the antibody with each batch of staining [Figure 1], whereas normal mucosal tissue was taken as a negative control by omitting the primary antibody [Figure 2]. The evaluation of study cases was done subsequently in a similar manner.
Figure 1.
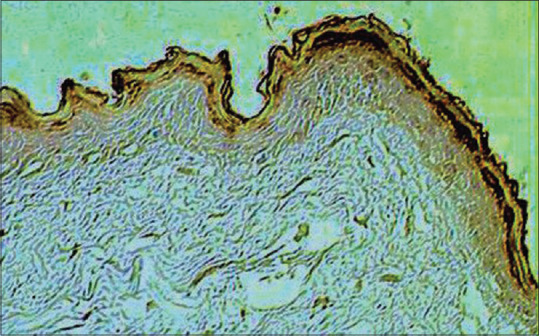
Photomicrograph of skin tissue as a positive control for Kallikrein 7 expression (×10)
Figure 2.
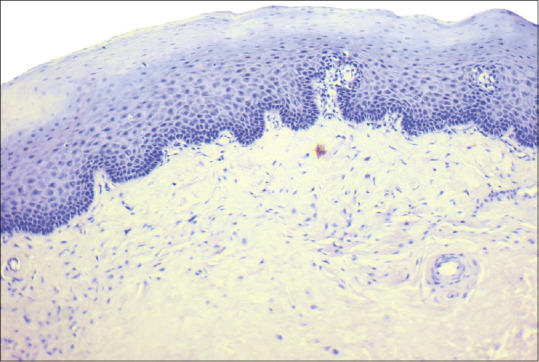
Photomicrograph of normal mucosa as a negative control for Kallikrein 7 expression (×10)
To enumerate the KLK 7 stained slides, 300 cells were examined manually in at least 5 areas and a mean percentage of positive stained slides was determined. Then, each sample was assigned to one of the following staining scores:
0%–25%
26%–50%
51%–75%
76%–100%.
All these observations were carried out by two observers to eliminate interobserver bias and statistical evaluation was done using the SPSS INC; Chicago USA version 17 software.
RESULTS
A total of 60 cases were studied for the immunohistochemical expression of KLK 7 in normal mucosal tissue (n = 30) and OSCC cases (n = 30).
Out of 30 normal subjects, 20 were male and 10 were female. The age distribution was between 18 and 66 years. Out of them, 17 were under 40 years of age and 13 were above 40 years of age.
Out of 30 cases of OSCC, 23 were male and 7 were female. The age distribution was between 30 and 80 years. Out of them, 6 were under 40 years of age and 24 were above 40 years of age.
Table 3 shows a comparison of the expression of KLK 7 in normal mucosa and in patients with OSCC. The mean of IHC score with respect to normal subjects and in patients with OSCC was found to be 0.00 and 2.00, respectively, using independent t-test. Statistically significant difference was observed between normal subjects and in patients with OSCC with respect to the mean of IHC score (P = 0. 0001*).
Table 3.
Comparison of kallikrein 7 expression in normal subjects and in patients with oral squamous cell carcinoma with respect to immunohistochemistry score obtained by the number of positive cells per 300 cells counted in random fields
| Groups | Mean | SD | SE | t | P |
|---|---|---|---|---|---|
| OSCC group | 2.00 | 1.34 | 0.24 | 8.1807 | 0.0001* |
| Normal group | 0.00 | 0.00 | 0.00 |
Independent t-test. *P<0.05. OSCC: Oral squamous cell carcinoma, SD: Standard deviation, SE: Standard error
Table 4 shows the comparison of KLK 7 expression with respect to different clinical stages of OSCC. The mean of IHC score in case of Stage I (n = 10), Stage II (n = 8), Stage III (n = 7) and Stage IV OSCC (n = 5) was 1.20, 1.37, 2.29 and 3.60, respectively, using Kruskal–Wallis analysis of variance (ANOVA) test. Statistically significant difference was observed between all the clinical stages of OSCC with respect to the mean of IHC score counted in random fields (P = 0.0127*).
Table-4.
Shows the comparison of Kallikrein 7 expression in different clinical stages of oral squamous cell carcinoma.
| Mean | SD | SE | Sum of ranks | |
|---|---|---|---|---|
| TNM/clinical staging | ||||
| Stage 1 | 1.20 | 0.92 | 0.29 | 105.00 |
| Stage 2 | 1.37 | 1.28 | 0.45 | 109.50 |
| Stage 3 | 2.29 | 1.25 | 0.47 | 124.50 |
| Stage 4 | 3.60 | 0.89 | 0.40 | 126.00 |
| H | 10.8273 | |||
| P | 0.0127* | |||
| Pairwise comparisons by Mann–Whitney U-test | ||||
| Stage 1 versus stage 2 | P=1.0 | |||
| Stage 1 versus stage 3 | P=0.014* | |||
| Stage 1 versus stage 4 | P=0.011* | |||
| Stage 2 versus stage 3 | P=0.019* | |||
| Stage 2 versus stage 4 | P=0.015* | |||
| Stage 3 versus stage 4 | P=0.046* | |||
Kruskal–Wallis ANOVA test. *P=0.0127 – Significant. SD: Standard deviation, SE: Standard error
Table 5 shows the comparison of expression of KLK 7 with respect to different histopathological grades of OSCC. The mean number of IHC score in well-differentiated OSCC (n = 10) [Figure 3], moderately differentiated OSCC (n = 12) [Figure 4] and poorly differentiated (n = 8) [Figure 5] OSCC was found to be 1.10, 2.08 and 3.75, respectively, using Kruskal–Wallis ANOVA test. Statistically significant difference was observed between all the grades of OSCC with respect to the number of IHC score counted in random fields (P = 0.0001*).
Table-5.
Shows the comparison of kallikrein 7 expression in different histopathological grades of oral squamous cell carcinoma.
| Mean | SD | SE | Sum of ranks | |
|---|---|---|---|---|
| Histopathological grading | ||||
| Grade 1 | 1.10 | 0.31 | 0.09 | 55.00 |
| Grade 2 | 2.08 | 0.29 | 57.45 | 199.00 |
| Grade 3 | 3.75 | 0.46 | 74.60 | 211.00 |
| H | 27.0953 | |||
| P | 0.0001* | |||
| Pairwise comparisons by Mann–Whitney U-test | ||||
| Grade 1 versus Grade 2 | 0.0002* | |||
| Grade 1 versus Grade 3 | 0.0004* | |||
Kruskal–Wallis ANOVA test. *P<0.05 – Significant, SD: Standard deviation, SE: Standard error
Figure 3.
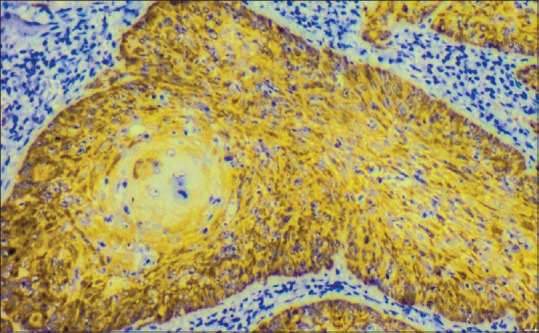
Photomicrograph showing Kallikrein 7 expression in welldifferentiated oral squamous cell carcinoma (×40)
Figure 4.
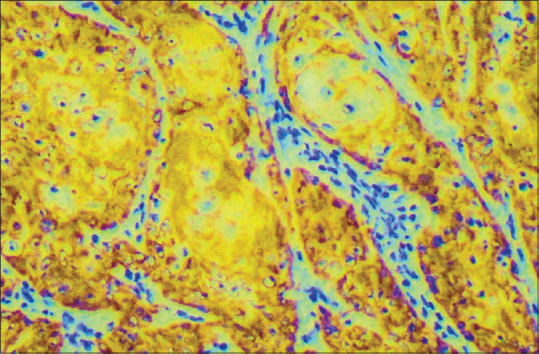
Photomicrograph showing Kallikrein 7 expression in moderately differentiated oral squamous cell carcinoma (×40)
Figure 5.
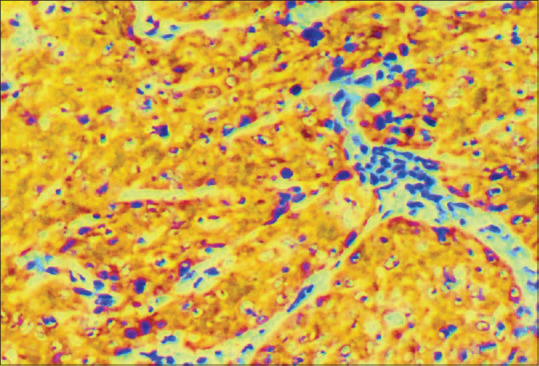
Photomicrograph showing Kallikrein 7 expression in poorly differentiated oral squamous cell carcinoma (×40)
DISCUSSION
Oral cancers currently represent approximately 3% of all cancer deaths. The 5-year survival after diagnosis has remained at a dismal 50% for the past several decades, carrying one of the worse prognoses of all cancers. Poor prognosis is directly related to advanced-stage, metastatic disease at the time of diagnosis.[4] These data highlight the need for new biomarkers in diagnosing OSCC.
The KLK family constitutes the largest cluster of proteases within the human genome and all 15 KLK genes are encoded in tandem on chromosome 19q13.3-13.4. All KLKs share similarities in their DNA sequences and tertiary structures suggesting conserved function among the encoded proteins.[16] They have been reported to play important roles in physiological pathways, such as blood pressure control, semen liquefaction, skin desquamation and innate immunity.[17] KLK s have also been implicated in pathologic processes. Studies have shown that KLKs also influence tumorigenesis through their effects on epithelial-to-mesenchymal transition (EMT), disruption of normal oxygen balance, degradation of the extracellular matrix (ECM) and involvement in tumor cell proliferation.[10]
KLKs participate in many stages of the metastatic cascade by facilitating tumor-cell detachment; by enabling invasion through multiple ECM barriers, independently and in collaboration with other extracellular proteases and potentially by contributing to the metastatic spread. Tumor cells detach, invade local tissues and metastasize by undergoing EMT, through which they attain a malignant phenotype. EMT is characterized by extensive changes in the expression of adhesion molecules, including the loss of an E-cadherin-mediated cell–cell adhesion and de novo expression of mesenchymal cadherins such as N-cadherin. Loss of E-cadherin facilitates tumor-cell detachment and N-cadherin promotes cell motility and migration.[18]
Thereby, KLK 7 plays an important role in tumor invasion and progression which attracted many investigators to evaluate its role in cancer growth.[19]
Pettus et al. examined KLKs 5, 7, 8 and 10 expressions in squamous cell carcinoma of the oral cavity. They demonstrated that serial sections showed specific cytoplasmic staining for each KLK in 100% of tumor samples analyzed and results from the present study showed an increased expression of Kallikrein 7 with respect to various clinical stages and histopathological grades respectively.[20]
Zhao et al. conducted a study on the correlation of the expression of human KLK-related peptidases 4 and 7 with the prognosis in OSCC. They observed that both KLK s were expressed strongly in the majority of tumor cells in 68 of 80 cases; these were mostly moderately or poorly differentiated neoplasms. The results of the present study were in accordance with Zhao et al.[21]
The results of the present study were found to be statistically significant with P value of 0.0001 in various clinical stages of OSCC. In the present study, there is an increased expression of KLK 7 in clinical Stages III and IV as compared with clinical Stages I and II. Thus, increased expression of KLK 7 was seen in the advanced clinical stages, thereby predicting the worst prognosis of OSCC patients.
In the present study, the results were found to be statistically significant with P value of 0.0001 within various histological grades of OSCC. The results of the present studies were in accordance with previous studies by Shan et al.[22] and Zhao et al.[21] where they demonstrated that poorly differentiated OSCC shows increased expression of KLK 7 when compared to well-differentiated OSCC.
The significant expression of KLK 7 in patients with OSCC as compared to normal subjects suggests its role as a diagnostic biomarker. Statistically significant expression of KLK 7 in patients with OSCC with respect to clinical staging and histopathological grading suggests its role as a prognostic indicator.
CONCLUSION
On the basis of these study findings, we suggest that KLK7 has the potential to become a useful diagnostic/prognostic tool for identifying OSCC, monitoring response to therapy as well as serve as a novel target antigen for the treatment of OSCC refractory to standard treatment modalities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49:33–64, 1. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 2.Rivera C, Venegas B. Histological and molecular aspects of oral squamous cell carcinoma (Review) Oncol Lett. 2014;8:7–11. doi: 10.3892/ol.2014.2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feller LL, Khammissa RR, Kramer BB, Lemmer JJ. Oral squamous cell carcinoma in relation to field precancerisation: Pathobiology. Cancer Cell Int. 2013;13:31. doi: 10.1186/1475-2867-13-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doshi NP, Shah SA, Patel KB, Jhabuawala MF. Histological grading of oral cancer: A comparison of different systems and their relation to lymph node metastasis. Natl J Community Med. 2011;2:136–42. [Google Scholar]
- 5.Shi Z, Stack MS. Urinary-type plasminogen activator (uPA) and its receptor (uPAR) in squamous cell carcinoma of the oral cavity. Biochem J. 2007;407:153–9. doi: 10.1042/BJ20071037. [DOI] [PubMed] [Google Scholar]
- 6.Shi Z, Stack MS. Molecules of cell adhesion and extracellular matrix proteolysis in oral squamous cell carcinoma. Histol Histopathol. 2010;25:917–32. doi: 10.14670/HH-25.917. [DOI] [PubMed] [Google Scholar]
- 7.Egelrud T, Lundström A. A chymotrypsin-like proteinase that may be involved in desquamation in plantar stratum corneum. Arch Dermatol Res. 1991;283:108–12. doi: 10.1007/BF00371618. [DOI] [PubMed] [Google Scholar]
- 8.Lundström A, Egelrud T. Cell shedding from human plantar skin in vitro: Evidence of its dependence on endogenous proteolysis. J Invest Dermatol. 1988;91:340–3. doi: 10.1111/1523-1747.ep12475679. [DOI] [PubMed] [Google Scholar]
- 9.Shaw JL, Diamandis EP. Distribution of 15 human kallikreins in tissues and biological fluids. Clin Chem. 2007;53:1423–32. doi: 10.1373/clinchem.2007.088104. [DOI] [PubMed] [Google Scholar]
- 10.Yousef GM, Scorilas A, Magklara A, Soosaipillai A, Diamandis EP. The KLK7 (PRSS6) gene, encoding for the stratum corneum chymotryptic enzyme is a new member of the human kallikrein gene family-Genomic characterization, mapping, tissue expression and hormonal regulation. Gene. 2000;254:119–28. doi: 10.1016/s0378-1119(00)00280-8. [DOI] [PubMed] [Google Scholar]
- 11.Hachem JP, Wagberg F, Schmuth M, Crumrine D, Lissens W, Jayakumar A, et al. Serine protease activity and residual LEKTI expression determine phenotype in Netherton syndrome. J Invest Dermatol. 2006;126:1609–21. doi: 10.1038/sj.jid.5700288. [DOI] [PubMed] [Google Scholar]
- 12.Komatsu N, Saijoh K, Kuk C, Liu AC, Khan S, Shirasaki F, et al. Human tissue kallikrein expression in the stratum corneum and serum of atopic dermatitis patients. Exp Dermatol. 2007;16:513–9. doi: 10.1111/j.1600-0625.2007.00562.x. [DOI] [PubMed] [Google Scholar]
- 13.Prezas P, Scorilas A, Yfanti C, Viktorov P, Agnanti N, Diamandis E, et al. The role of human tissue kallikreins 7 and 8 in intracranial malignancies. Biol Chem. 2006;387:1607–12. doi: 10.1515/BC.2006.200. [DOI] [PubMed] [Google Scholar]
- 14.Shan SJ, Scorilas A, Katsaros D, Rigault de la Longrais I, Massobrio M, Diamandis EP. Unfavorable prognostic value of human kallikrein 7 quantified by ELISA in ovarian cancer cytosols. Clin Chem. 2006;52:1879–86. doi: 10.1373/clinchem.2006.071456. [DOI] [PubMed] [Google Scholar]
- 15.Edge SB. AJCC Cancer Staging Manual. American Cancer Society; 2010. AJCC Cancer Staging Handbook. [Google Scholar]
- 16.Yousef GM, Diamandis EP. The new human tissue kallikrein gene family: Structure, function, and association to disease. Endocr Rev. 2001;22:184–204. doi: 10.1210/edrv.22.2.0424. [DOI] [PubMed] [Google Scholar]
- 17.Lawrence MG, Lai J, Clements JA. Kallikreins on steroids: Structure, function, and hormonal regulation of prostate-specific antigen and the extended kallikrein locus. Endocr Rev. 2010;31:407–46. doi: 10.1210/er.2009-0034. [DOI] [PubMed] [Google Scholar]
- 18.Descargues P, Deraison C, Prost C, Fraitag S, Mazereeuw-Hautier J, D'Alessio M, et al. Corneodesmosomal cadherins are preferential targets of stratum corneum trypsinand chymotrypsin-like hyperactivity in Netherton syndrome. J Invest Dermatol. 2006;126:1622–32. doi: 10.1038/sj.jid.5700284. [DOI] [PubMed] [Google Scholar]
- 19.Du JP, Li L, Zheng J, Zhang D, Liu W, Zheng WH, et al. Kallikrein-related peptidase 7 is a potential target for the treatment of pancreatic cancer. Oncotarget. 2018;9:12894–906. doi: 10.18632/oncotarget.24132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pettus JR, Johnson JJ, Shi Z, Davis JW, Koblinski J, Ghosh S, et al. Multiple kallikrein (KLK 5, 7, 8, and 10) expression in squamous cell carcinoma of the oral cavity. Histol Histopathol. 2009;24:197–207. doi: 10.14670/hh-24.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao H, Dong Y, Quan J, Smith R, Lam A, Weinstein S, et al. Correlation of the expression of human kallikrein-related peptidases 4 and 7 with the prognosis in oral squamous cell carcinoma. Head Neck. 2011;33:566–72. doi: 10.1002/hed.21496. [DOI] [PubMed] [Google Scholar]
- 22.Shan SJ, Scorilas A, Katsaros D, Diamandis EP. Transcriptional upregulation of human tissue kallikrein 6 in ovarian cancer: clinical and mechanistic aspects. British journal of cancer. 2007;96(2):362–72. doi: 10.1038/sj.bjc.6603556. [DOI] [PMC free article] [PubMed] [Google Scholar]


