Abstract
The COVID-19 pandemic presents a serious public health challenge in all countries. However, repercussions of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections on future global health are still being investigated, including the pandemic’s potential effect on the emergence and spread of global antimicrobial resistance (AMR). Critically ill COVID-19 patients may develop severe complications, which may predispose patients to infection with nosocomial bacterial and/or fungal pathogens, requiring the extensive use of antibiotics. However, antibiotics may also be inappropriately used in milder cases of COVID-19 infection. Further, concerns such as increased biocide use, antimicrobial stewardship/infection control, AMR awareness, the need for diagnostics (including rapid and point-of-care diagnostics) and the usefulness of vaccination could all be components shaping the influence of the COVID-19 pandemic. In this publication, the authors present a brief overview of the COVID-19 pandemic and associated issues that could influence the pandemic’s effect on global AMR.
Introduction and overview of the global COVID-19 pandemic
In December 2019, several cases of atypical pneumonia were reported in Wuhan, China, and later confirmed as severe acute respiratory syndrome (SARS) coronavirus, which was named SARS-Cov-2 because of its genetic relatedness to the 2003 SARS outbreak.1 Subsequent investigations of the novel virus showed a similarity of 79% to SARS-CoV and a 50% similarity to Middle East respiratory syndrome coronavirus (MERS-CoV).2 Initially, on 12 January 2020, WHO named this new virus the 2019-novel coronavirus (2019-nCoV). Later, the Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses (ICTV) proposed the name as SARS-CoV-2.3 On 11 February 2020, WHO officially named the disease caused by this novel coronavirus as COVID-19.
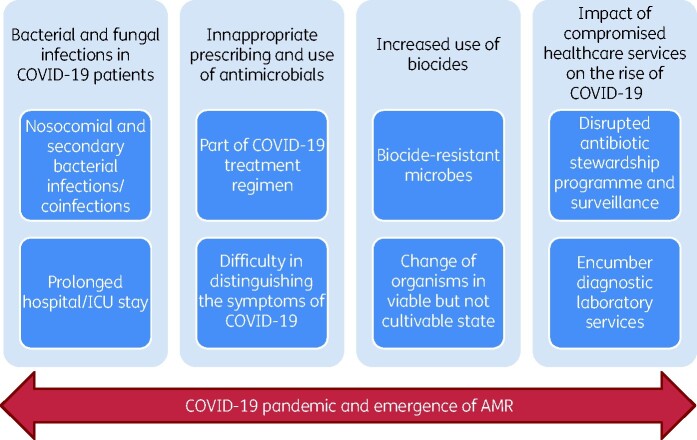
The coronaviruses are enveloped viruses from the Coronaviridae family and possess positive-sense single stranded RNA as genetic material.4 The Coronaviridae family is divided into four genera: α-, β-, γ- and δ-coronaviruses. α- and β-coronaviruses are able to infect mammals, whereas γ- and δ-coronaviruses mainly infect birds, or sometimes mammals.5 In the past 20 years, three outbreaks—including SARS-CoV in 2003, MERS-CoV in 2012 and the much feared COVID-19/SARS-CoV-2 in 2020—have been recorded.3,6–8 Additionally, several other coronaviruses (CoVs) belonging to both α- and β-coronaviruses circulate in humans causing mild respiratory diseases9 and it is estimated that 15%–30% of common colds are caused by CoVs.10 Among the seven human-associated strains (Figure 1), infection with two α-CoVs (HCoV-229E and HCoV-NL63) and two β-CoVs (HCoV-OC43 and HCoV-HKU1) lead to mild respiratory tract infections similar to the common cold, while infection with the three highly pathogenic β-CoVs (SARS-CoV, MERS-CoV and COVID-19/SARS-CoV-2) may result in severe disease.5 At this point, it should be noted that some coronavirus outbreaks trace their origin to animal reservoirs of CoVs, such as the SARS-CoV outbreak in China in 2003,11 and the MERS-CoV causing outbreaks in the Middle East in 2012.12
Figure 1.
Timeline of severe human coronavirus strains.
With specific respect to SARS-CoV-2 and COVID-19, fever and cough have been recorded as the predominant clinical symptoms, with more serious effects among elderly patients and those with underlying comorbidities such as hypertension, COPD, obesity, diabetes and other immunosuppressive conditions.13,14 These patients may develop symptoms such as acute respiratory distress syndrome, septic shock, metabolic acidosis, coagulation dysfunction and in some cases lead to death.15 A study conducted by Guan et al.16 recruiting 1099 laboratory confirmed cases found clinical manifestations such as fever (88.7%), cough (67.8%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), and pneumonia (91.1%) in affected patients. The SARS-CoV-2 virus has also been isolated from rectal swabs of patients with severe pneumonia and gastrointestinal tract symptoms such as diarrhoea, nausea and vomiting. However, only a low proportion of virus-positive rectal swabs have actually been reported (below 10% of patients), suggesting that virus transmissibility through the faecal-oral route is limited.15,17–19 SARS-CoV-2 RNA is detectable 2–3 days prior to the onset of symptoms, but peaks with the start of symptoms (usually in the first week). During the period of overt symptoms, an individual is known to be infectious, with viable virus decreasing in quantity over the following days to weeks. However, although cultivable viable virus may be detected for up to 9 days, viral PCR remains positive for up to 3 months after infection.20 According to the information received on 8 October 2020 [based on the number of total confirmed cases (36 002 827) and total deaths (1 049 810) caused by SARS-CoV-2], the mortality rate has been estimated to be 2.9%,21 which is lower than that found with SARS-CoV (10%)22 and MERS-CoV (37.1%).23 However, the transmissibility of SARS-CoV-2 is much higher when compared with other CoVs.24 Further, there is evidence to suggest that some racial and ethnic populations may be more affected than others.25 Although case fatality rates are difficult to calculate during a pandemic—largely due to the heterogeneity of methodologies used in data collection—it is not unthinkable that a progressive decrease in the COVID-19 mortality rate will be observed as SARS-CoV-2 seroconverts and immunity spreads among the population.
Literature search
To compile the information in preparing this manuscript, a PubMed and Google literature search was conducted by using the key terms ‘COVID-19’, ‘COVID-19 pandemic’, ‘SARS-CoV-2’, ‘SARS-CoV-2019’, ‘coronavirus-2019’, ‘global burden of antimicrobial resistance’, ‘COVID-19 and secondary infections’, ‘COVID-19 and secondary bacterial infections’, ‘COVID-19 and secondary fungal infections’, ‘antimicrobial treatment of COVID-19 patients’, ‘COVID-19 and biocides’, ‘COVID-19 pandemic and biocides’, ‘COVID-19 and healthcare services’, ‘COVID-19 and compromised healthcare services’, ‘COVID-19 and antimicrobial stewardship’, ‘vaccines and antimicrobial resistance’, and ‘COVID-19 vaccines’. The authors included full text articles published in the English language only.
The global burden of antimicrobial resistance (AMR)—an introduction
Similar to COVID-19, AMR presents a serious challenge to global public health in all countries across the world. In September 2016 (years prior to the emergence of the COVID-19 pandemic), the WHO committed itself to fighting AMR, which had become a problem of global public health importance.26 For example, global infections due to antimicrobial resistant pathogens result in approximately 700 000 deaths annually, which has been estimated to increase to 10 million deaths by the year 2050.27 The Global Antimicrobial Surveillance System (GLASS) of WHO continues to report increasing levels of AMR in a range of pathogens that cause serious or common infections in many regions of the world.28 Recently, an estimated 3 million annual infections in America were reported to be caused by high priority antimicrobial-resistant pathogens.29,30 Moreover, the US CDC previously estimated that approximately 23 000 deaths will occur every year due to infections caused by antimicrobial resistant pathogens in the USA.31 In 2019, ECDC reported the deaths of 25 000 patients in high-income countries of Europe.32 Similarly, in low- and middle-income countries (LMICs) such as India and Thailand, infections caused by antimicrobial-resistant pathogens were responsible for the annual deaths of approximately 58 000 children and 38 000 adults, respectively.33 In the current century, AMR is a substantial and continually growing problem, being considered one of the greatest threats to global health34 with significant global economic burden.35 For example, antimicrobial-resistant infections have been estimated to result in an extra economic burden of $20 billion in the USA alone.31 In the EU and European Economic Area (EEA), AMR results in an extra healthcare cost of €1.1–1.5 billion.32,36 By 2050, there is predicted to be a global loss of 1.1%–3.8% of the global annual gross domestic product due to antimicrobial-resistant infections. It is predicted that, in low-income countries, around 24 million people will be forced into extreme poverty by 2030, and one in six will die due to AMR-related infections.35
The increased incidence of infections by microorganisms resistant to the most recently developed antibiotics, e.g. the carbapenems, or to ‘last resort’ antimicrobial agents, such as colistin, is worrisome. While the emergence of AMR continues to increase, there has been a decline in the availability of newly developed antimicrobial agents on the market. If this continues, most of the currently prescribed antibiotics applied for human and animal infections will be ineffective within a decade, leading to conditions similar to that of the pre-antibiotic era. In this respect, it should be noted that programmes such as the US ‘10 × ’20 initiative’ have been implemented.37 Although the AMR crisis has tended to be more serious in Gram-negative compared with Gram-positive bacterial infections, in recent years, an increased incidence of antibiotic resistant Gram-positive organisms has been reported.38,39 The most serious group of MDR bacteria associated with AMR are those that pose a particular threat to hospitals and nursing homes; referred to by IDSA as ‘ESKAPE’ pathogens, which include Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp.40 In 2017, WHO published its first ‘Priority Pathogens List (PPL)’ in order to help direct efforts into the research and development of new antibiotics. The PPL comprised a catalogue of 12 families of bacteria that pose the greatest threat to mankind, including both Gram-negative and Gram-positive bacteria. The PPL divides pathogens into three categories, namely ‘critical’, ‘high’ and ‘medium’ priority dependent on the urgency of the global need for new antibiotics.41,42 Critical priority species include the carbapenem-resistant A. baumannii, P. aeruginosa, carbapenem-resistant and ESBL-producing Enterobacteriaceae such as Klebsiella spp., Escherichia coli, Serratia spp. and Proteus spp. These are associated with severe infections of the bloodstream and the lower respiratory tract. Bacterial species in the high priority category include vancomycin-resistant E. faecium, MRSA and vancomycin-intermediate/resistant S. aureus, clarithromycin-resistant Helicobacter pylori, fluoroquinolone-resistant Campylobacter spp., Salmonella spp. and cephalosporin- and fluoroquinolone-resistant Neisseria gonorrhoeae. These are commonly associated with the general infections, gastroenteritis and gonorrhoea. Species in the medium priority category include penicillin-resistant Streptococcus pneumoniae, ampicillin-resistant Haemophilus influenzae and fluoroquinolone-resistant Shigella spp.42
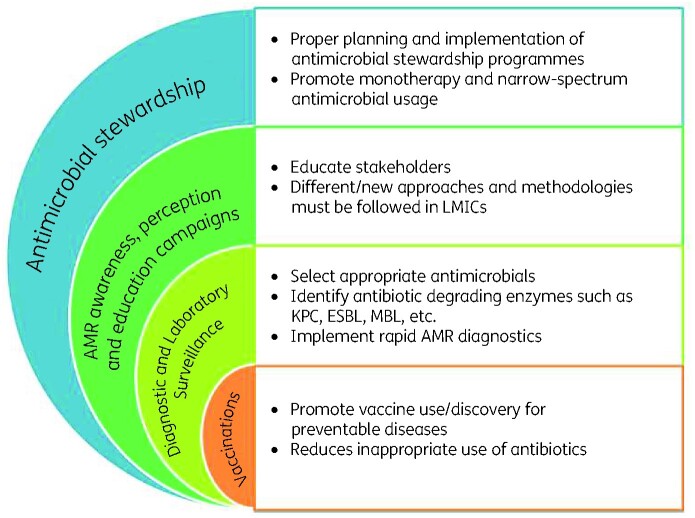
The COVID-19 pandemic and its potential relationship with the emergence of AMR
AMR naturally occurs as a mechanism by which microorganisms adapt to survive in hostile environments, such as those containing antibiotics. The high growth rate of most bacteria combined with microbial genomic mutation and the phenomenon of natural (Darwinian) selection results on the emergence of microorganisms adapted to withstand the presence of these antibiotics. Although this process occurs naturally, the inappropriate (over/misuse) use of antibiotics (and disinfectants/biocides) in many ‘One Health’ areas such as human health and hygiene, agriculture, animal husbandry and food production industries are major contributing factors in the emergence of AMR (or disinfectant/biocide resistance) in the last century.43,44 The various prevention and treatment protocols being used for the management of the COVID-19 pandemic has heightened concern over the development and spread of existing and novel resistance mechanisms associated with pathogenic bacteria. One of the major concerns is the extensive and inappropriate use of antimicrobials in the treatment of critically ill COVID-19 patients.45 However, this is not the only factor potentially linking COVID-19 infections to increasing AMR (and biocides). Details of these factors are provided below (Figure 2).
Figure 2.
The most relevant predictors playing a role in the global development of AMR in the face of the worldwide COVID-19 pandemic.
1. Bacterial and fungal infections in COVID-19 patients
Critically ill COVID-19 patients admitted to the hospital, especially the ICU, suffer more frequent bacterial or fungal nosocomial infections. Patients with underlying risk factors such as advanced age, previous systemic diseases, mechanical ventilation, and prolonged hospital stay are more prone to these complications.15,46 Furthermore, secondary bacterial infections may occur as a consequence of viral respiratory infections, being associated with high morbidity and mortality rates in affected patients.47–49 Although the precise mechanisms facilitating secondary bacterial infections during viral respiratory infection have not been fully elucidated, dysregulation of the immune system,15,50,51 virus-mediated immunosuppression,52 immune response alterations generated towards one pathogen,53 and increased susceptibility of mammalian cells to bacterial attachment when infected by viruses54,55 are some of the published consequences of viral infections that contribute to the development of secondary bacterial infections in affected individuals. However, coinfections with bacterial or fungal pathogens are considered unlikely to be common in patients with mild COVID-19 when compared with those with more severe disease upon hospital admission.56
Mechanical ventilation and prolonged hospitalization or ICU stay has been found to be the most common risk factor for bacterial or fungal superinfections, irrespective of COVID-19 disease.57–59 This fact becomes important as studies from many countries have shown the need for mechanical ventilation in 21%–88% of COVID-19 patients admitted to the ICU.46,60–64 The development of secondary respiratory infection such as ventilator-associated pneumonia is also not surprising, as patients with severe COVID-19 have been reported to show the following: higher pro-inflammatory cytokine levels (e.g. interleukin-2, soluble interleukin-2 receptor, interleukin-6, tumour necrosis factor-alpha), higher levels of anti-inflammatory cytokines (e.g. interleukin-4, interleukin-10), lower CD4 and CD8 cell counts, and decreased expression of interferon-gamma by CD4 cells when compared with those experiencing moderate disease.50,51,65 These changes in inflammatory response are likely to contribute to lung damage that may predispose patients to the abovementioned superinfections.
Initial studies found that 1%–10% of COVID-19 patients developed a secondary bacterial infection.66 However, later studies from several hospitals in Wuhan, China, found that secondary bacterial or fungal infections occurred in 8.5%–42.2% and coinfections occurred in up to 45.4% of COVID-19 patients.67 In a study conducted at two hospitals in New York City, the hospitals reported an associated bacteraemia in 6% of all COVID-19 patients, and in 12% of patients that were on mechanical ventilation.63 Similarly, Zhou et al.68 recruited 191 patients and reported secondary bacterial infections in 28 patients admitted to hospitals in China, with 27 out of 28 patients that developed secondary bacterial infections dying.
The respiratory system has been reported to be the most affected system associated with COVID-19 related secondary infections, e.g. bacterial and fungal pneumonia, especially ventilator-associated pneumonias.69 Bloodstream and urinary tract infections appear to be less frequent. Most of the bacterial pathogens isolated were found to produce antibiotic-degrading enzymes such as carbapenemases and ESBLs, which confer resistance to the carbapenem and cephalosporin groups of antibiotics, respectively. Among pathogens causing secondary infections, the pandrug resistant (PDR) A. baumannii, carbapenemase- and ESBL-producing K. pneumoniae, ESBL-producing Pseudomonas aeruginosa, Enterobacter cloacae, Serratia marcescens, Mycoplasma species and H. influenzae were the bacterial pathogens most often observed, whereas Aspergillus fumigatus, Aspergillus flavus, Candida albicans, Candida glabrata, and Candida auris were the most common fungal pathogens reported.17,60,67,70–73
Although it is widely debated as to when a blood culture should be requested in patients with lower respiratory tract bacterial infections such as bacterial pneumonia, microbiological studies using sputum microscopy and culture, pleural effusion microscopy and culture, blood culture, urinary antigen tests and serology are all included in the management of bacterial pneumonia.74 Blood culture reports offer additional information regarding whether an antibiotic treatment should be implemented or not. De-escalation of the antibiotic prescription in special cases plays an important role in decreasing AMR. However, among several studies conducted to evaluate secondary bacterial pneumonia in COVID-19 patients, only a few included blood culture processing.67 Despite this fact, it has been widely recognized by the medical community that antibiotics have been overprescribed for the management of COVID-19 patients.
There is currently a paucity of data on the association between increased respiratory bacterial and/or fungal respiratory coinfections and the frequent use of broad-spectrum empirical antimicrobial medications in patients with COVID-19 infections. Data from such studies are required in order to generate scientific evidence to support the development of (inter)national antimicrobial stewardship practices and policies targeted to COVID-19 and future pandemic infections.75
2. Inappropriate prescribing and use of antimicrobials
Inappropriate prescribing and use of antimicrobials are the most common factors fuelling the development of AMR across the globe. It is estimated by experts that at least 50% of the antimicrobial medications currently used to treat infectious diseases worldwide are unnecessary or inappropriate.76 In this respect, the COVID-19 pandemic may be contributing to worsening the scope of AMR globally through the non-rational use of antibiotics as part of preventive and therapeutic management of COVID-19. In fact, repeated warnings have been raised about the role of the COVID-19 pandemic causing an increase in antimicrobial drug resistant bacteria which is an additional burden on already overwhelmed healthcare systems.77,78 In this line, WHO released guidance discouraging the use of antibiotics in the treatment of patients with mild or moderate symptoms of COVID-19 unless indicated by established laboratory culture susceptibility testing protocols.79
In the face of the COVID-19 pandemic the tendency to prescribe antimicrobial medications by healthcare workers is very high. This is partly due to the difficulty in distinguishing the symptoms of COVID-19 from those of other respiratory diseases or even hospital-acquired or ventilator-associated pneumonia, particularly among hospitalized patients.1,68,71,80 Several studies have observed a comparative increase in the use of antibiotics while treating COVID-19 patients, despite relatively low number of confirmed cases of secondary bacterial or fungal infection. For example, the International Severe Acute Respiratory and Emerging Infections Consortium (ISARIC) reported that 62% of COVID-19 patients in their study had received antimicrobial therapy.81 Other studies have also found widespread use of antibiotics (80%–100%) and antifungals (7.5%–15%) in critically ill COVID-19 patients admitted to ICUs in China.15,16,61,70,71,82 Another study highlighted the administration of antibacterial therapy to 72% of COVID-19 patients even though only 8% of patients were confirmed to have bacterial or fungal infections.83 In this respect, the most common antibiotics prescribed for empirical therapy in Chinese hospitals were fluoroquinolones, cephalosporins, carbapenems, azithromycin, vancomycin and linezolid.46,61,70,71,84 However, the extensive and widespread use of antimicrobials to treat COVID-19 patients was also reported outside the Asian continent. A study conducted in France highlighted the use of antimicrobial medications for the treatment of COVID-19 patients, with the use of various combinations of meropenem, tigecycline, levofloxacin, aerosolized colistimethate, voriconazole and/or isavuconazole being reported.72 In a meta-analysis of 154 studies (30 623 patients), Langford et al.67 found a prevalence of antibiotic prescribing of 74.6% (95% CI 68.3%–80.0%). A Dutch retrospective observational study conducted in four hospitals also reported high prevalence of antimicrobial use (60.1%; range 33.3%–73.4%) in the absence of corresponding level of laboratory confirmed bacterial coinfection (1.2%).85 One option to address this high level of non-rational antimicrobial use is to expedite the prompt and accurate diagnosis of viral/bacterial coinfection. For example, triage (based on clinical symptoms) combined with the measurement of inflammatory biomarkers such as C-reactive protein (CRP),86,87 procalcitonin (PCT) or commercially available assays88—e.g. the FebriDx rapid test (Lumos Diagnostics, The Netherlands)89—could be more efficiently implemented. In 2020, Mason et al.90 concluded that the absence of both elevated baseline white cell counts and antibiotic-related decrease in CRP in COVID-19 infections could help exclude bacterial coinfection. A recent systematic review and meta-analysis of 26 studies showed that the use of PCT to guide initiation and duration of antibiotic treatment reduces the risk of mortality, lowers antibiotic consumption and decreases the risk of antibiotic-related side effects.91 A study conducted in England evaluated the usefulness of PCT in antimicrobial stewardship. The study reported reduced antibiotic consumption (without an increase in mortality) and a reduction in admission-related carbapenem prescribing for COVID-19 patients presenting with a negative PCT test.92
Undoubtedly, antimicrobial therapy is important in the management of suspected or confirmed cases of bacterial or fungal coinfections or secondary infections whether community-acquired or nosocomial infections.93 However, determining the role of antibiotic treatment in the efficient management of COVID-19 patients still requires more evidence-based research.
3. Increased use of biocides
Significantly less is known about the mechanisms and extent of microbial resistance to biocides than is known about microbial resistance to antibiotics. In this respect, the word ‘biocides’ refers to compounds with antiseptic, disinfectant or preservative activity.94 Due to the current COVID-19 pandemic, the use of biocides has hugely increased in private, community and hospital settings. Interestingly, improved hygiene practices involving biocides may actually reduce the transmission of antimicrobial-resistant pathogens that are found on our hands, but paradoxically may at the same time select for antimicrobial-resistant pathogens, thereby having an unknown impact on global AMR.95–99 Additionally, the intensive use of surface disinfectants and household cleaners contribute to an increased concentration of these substances in wastewater treatment plants and receiving waters, altering the normal ecosystem and potentially favouring the emergence of AMR due to biocide-related selection pressure.100,101 Moreover, in densely populated countries, where the use of disinfectants was mostly confined to the clinical/healthcare settings, the increased use of hand sanitizers and disinfectants might potentially impact on the human microbiome, which contributes to maintaining homeostasis in and on its host. According to the Scientific Advisory Board of the British Institute of Cleaning Sciences, the killing activity of alcohol-based sanitizers for SARS-CoV-2 has not yet been proven. The overuse of these sanitizers may assist alcohol-resistant organisms, in particular the spore-forming Bacillus spp. found on the hands, to escape and survive antibiotics, leading to creation of even more harmful resistant microbes.102 Furthermore, the increased use of disinfectants may induce organisms to a viable but non-cultivable state, becoming undetectable using standard culture-based detection methods.103,104 These conditions may alter the isolation and antimicrobial susceptibility patterns of microbial pathogens, potentially giving rise to new AMR traits.
In this context, evidence-based data are required to evaluate the impact of the intensive use of sanitizers during the COVID-19 pandemic on the selection and acquisition of AMR genes, as well as on the viability, detection and transmission of antimicrobial-resistant microorganisms in private, community, hospital and environmental situations. This approach should take into consideration a One Health approach and not just focus on hospital-based AMR.
4. The impact of compromised healthcare services on the rise of COVID-19
Regular surveillance and monitoring of AMR through antimicrobial stewardship has provided insights into some of the key mechanisms associated with the increasing prevalence of antimicrobial-resistant organisms. In turn, this knowledge permits the development of targeted AMR guidelines and strategic plans to combat the further emergence and transmission of AMR.105 Unfortunately however, the COVID-19 pandemic has disrupted healthcare services in many countries and potentially impacted on the microbiological diagnostic laboratory systems that conduct routine screening and surveillance for antibiotic-resistant organisms.106 This disruption in services is further worsened by the excess pressure on the existing workforce and competing manpower needs. The impact of these changes on the maintenance of antimicrobial stewardship and antibiotic resistance monitoring programmes is likely to contribute to the further transmission of AMR in affected healthcare settings.107 The impact of the COVID-19 pandemic in many hospitals, across the UK, was a reduction in antimicrobial stewardship activities, with 64% (61/95) of respondents reporting that COVID-19 had a negative impact on routine antimicrobial stewardship activities.108 Further, the COVID-19 pandemic may interrupt the routine healthcare services associated with antimicrobial stewardship and infection control practices, including the isolation and treatment of patients infected/colonized with AMR bacteria, for example, patients infected with MDR TB or HIV.75,109 Knock-on effects may also be experienced via the disruption of infectious disease vaccination programmes and services.109 The use of technology may assist in reducing some of the difficulties being encountered by antimicrobial stewardship teams during the COVID 19 pandemic, as virtual meetings and ward rounds are increasingly being used in stewardship activities in the UK.75
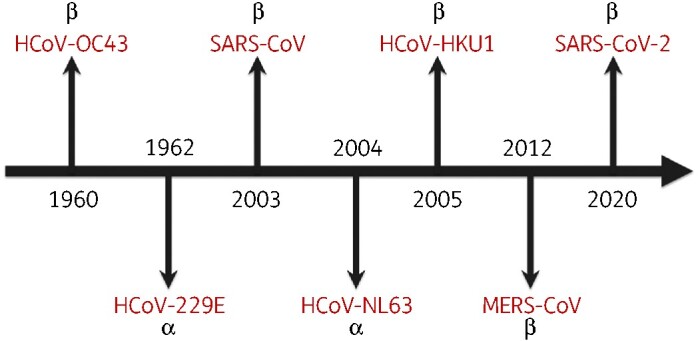
Opportunities for controlling AMR in the COVID-19 era (including in LMICs)
Although the emergence of AMR is a great challenge, the implementation of the following strategies could potentially help minimize the emergence of AMR during the COVID-19 pandemic era (Figure 3).
Figure 3.
The key points to AMR control strategies in the age of COVID-19.
1. Antimicrobial stewardship
To decrease the spread of AMR, it is necessary to discourage and curtail inappropriate prescribing and use of antimicrobials in COVID-19 patients with mild symptoms (see also sections 2 and 4 above). This is achievable through the application of properly articulated and carefully implemented hospital-wide antimicrobial stewardship programmes such as drug, dose, duration, de-escalation and diagnosis protocols.110 In this respect, the most accurate antimicrobial (such as the antimicrobial with the narrowest spectrum), at the right dose adjusted for patient weight and assessed with its renal toxicity, should be prescribed by all clinicians. Likewise, the correct duration of antimicrobial prescribing (e.g. successful treatment within the shortest amount of time) is also the most important factor for effective antimicrobial stewardship programs.110 The de-escalation of antimicrobial medication during the treatment of COVID-19 should not only be encouraged among clinicians/therapists, but medical personnel should also be regularly updated on this practice by AMR taskforces across the globe. The use of broad-spectrum antimicrobials and combination therapy are likely to be more prevalent among critically ill patients. However, it is necessary to carefully de-escalate the use of broad-spectrum antimicrobials and combination therapy in order to focus treatment towards using narrow-spectrum antimicrobials and monotherapy and minimize the emergence of AMR.111,112 There is no sufficient evidence to favour the use of combination therapy over monotherapy for the management of ventilator-associated pneumonia. Moreover, combination therapy has apparently no beneficial effects in decreasing superinfections or the emergence of AMR in pathogens.113–117 Additionally, lower rates of superinfections have been observed using monotherapy rather than combination antibiotic therapy.118
2. AMR awareness, perception and education campaigns
Public and clinician awareness, perceptions and education are important interventions in promoting behavioural change towards the use of antibiotics in order to prevent AMR, also during periods of viral-related pandemics.119 There should be continuous educational campaigns to educate healthcare workers and patients on the need for the appropriate prescribing and use of antimicrobial medications. Such campaigns targeting the general public and the healthcare workers have been organized and implemented using different approaches and methodologies, although mainly involving high-income countries.120
In most LMICs, lack of national policies and poor regulation of the distribution and use of antimicrobials means that many antibiotics can easily be purchased ‘over the counter’ without a prescription. Further, the relatively high rates of HIV infection, TB and malaria among patients of LMIC hospitals means that antibiotics may be intensively administered as a proactive preventive measure to try to avoid bacterial or fungal infections.121–123 Also, in LMIC settings there may be poor levels of healthcare and limited antimicrobial stewardship programmes, which are often linked to lack of resources such as trained personnel and to under-equipped diagnostic laboratories.124,125 Faced with the above-mentioned challenges, physicians may find it difficult to follow evidence-based antimicrobial prescribing practices,126,127 the consequence of which may be higher AMR prevalence in affected LMIC settings.128,129
Sustained public awareness campaigns on the ineffectiveness of antibiotics to treat viral infections (including pandemic respiratory viruses, respiratory infections caused by ‘common cold’ viruses and viral diarrhoea) should be instigated and implemented in order to reduce unnecessary antimicrobial prescription, self-medication and potential unwanted side effects.130,131 Medical professionals themselves also need to be educated about the non-rational use of antibiotics. For example, a randomized controlled trial conducted within primary care environments in 12 European countries recruited 1023 patients with acute cough syndrome—the result indicated no clear advantage of the use of amoxicillin over placebo.132 For both public and medical professionals, scientific-based evidence is essential in the development of appropriate health educational campaigns.
3. Diagnostics and laboratory surveillance
Diagnostic and laboratory surveillance systems are crucial components of the AMR mitigation response. Robust diagnostic and laboratory surveillance systems are needed to guide the accurate diagnosis of infectious diseases, ensure proper selection of antimicrobial medications (targeted therapy) and monitor the performance of antimicrobial stewardship programmes within the healthcare system. In order to attain the United Nations Sustainable Development Goals to achieve universal health coverage and access to quality healthcare, countries globally need to have access to diagnostics.133 The CEO of the Foundation for Innovative Diagnostics (FIND), Catharina Boehme, describes comprehensive diagnostic services as a requirement to strengthen the function and efficiency of health systems.134 The COVID-19 pandemic has served to highlight the lack of access to diagnostics in many LMICs; with research showing that LMICs have lower rates of COVID-19 testing per 100 000 of their population, compared with COVID-19 testing rates in higher-income countries.135 The lack of diagnostics in LMICs in general is also apparent in the limited participation of LMICs in WHO’s GLASS surveillance programme for monitoring AMR.28
Finally, the willingness of healthcare authorities to develop, fund and implement rapid diagnostic testing [including point-of-care (POC) testing] against COVID-19 should be matched by a concerted effort to develop, fund and implement rapid bacterial infectious disease and POC testing to combat AMR. This effort, can be augmented via the use of a ‘mix and match’ implementation package directed at the individual stakeholders involved in the development and use of rapid diagnostics.136
4. Vaccinations
One of the main focuses for stopping the spread of infectious diseases, including SARS-CoV-2 is vaccination. The use of vaccines (viral and bacterial) has a clear positive impact on global health, as mass vaccination helps reduce the prevalence of infectious diseases and subsequently the number of infections that are unnecessarily treated using antibiotics. Vaccination can have a major impact on the spread of AMR.137 For example, several studies have found decreased incidence in antibiotic-resistant S. pneumoniae isolated from acute otitis media and acute bacterial rhinosinusitis since the introduction of 7-valent pneumococcal vaccine.138,139 Other studies have found a reduced incidence of penicillin resistance in S. pneumoniae strains when collected before and after the use of a 7-valent pneumococcal vaccine.140,141
The successful implementation of vaccination against SARS-CoV-2 will help reduce the global prevalence of COVID-19 disease, thereby reducing the (inappropriate) use of antibiotics and potentially reducing the global burden of AMR. Additionally, there may be knock-on effects on the willingness of the public to accept vaccination even among ‘anti-vaxers’.142 For example, there is evidence to suggest that a high influenza vaccine uptake may lead to fewer COVID-19 deaths.143 Also an increased acceptance of influenza vaccination is being reported with potentially fewer respiratory tract infections and (inappropriate) antibiotic use likely.144 Currently more than 100 COVID-19 vaccines are at various stages of their development and several candidates have been approved for emergency use. Among the COVID-19 vaccines that have been approved, the adenovirus-vectored ChAdOx1 nCoV-19 vaccine (AZD1222)—which is a replication-deficient chimpanzee adenoviral vector (ChAdOx1) that contains the structural surface glycoprotein (spike protein) gene of SARS-CoV-2—showed an efficacy of 70.4% with an acceptable safety profile.145 An mRNA-based vaccine, i.e. the Pfizer-BioNTech COVID-19 (mRNA-BNT162b2) vaccine (Pfizer Inc, Philadelphia, PA, USA)—which is a lipid nanoparticle based nucleoside-modified mRNA vaccine that encodes the pre-fusion spike glycoprotein of SARS-CoV-2—was approved for emergency use by FDA on 11 December 2020 and has been shown to be 95% effective.146,147 Another mRNA-based vaccine, mRNA-1273 (Moderna Inc., Cambridge, MA, USA)—which is a lipid nanoparticle-encapsulated mRNA-based vaccine encoding the pre-fusion stabilized full-length spike protein—has been found to be 94.1% effective in preventing COVID-19 related illnesses including severe disease.148 Unfortunately however, it is not yet obvious what the effects of new COVID-19 variants (including the UK, Brazilian and South African variants) will be on the success of COVID-19 vaccination campaigns and ultimately on the development and spread of AMR.149
Conclusions
WHO has placed AMR among the top 10 most urgent global health threats of the 21st century and provided advice on how to tackle the problem. However, the emergence of the COVID-19 pandemic has further complicated the current and future landscape of global AMR. To confront this issue, there is a need for global coordination, especially in developing relevant guidelines for the management of COVID-19 using diagnostics, novel antimicrobials, biocides and vaccines. In addition, continuing education of all stakeholders (healthcare workers, the general public and politicians) about the dangers associated with inappropriate use of antimicrobials and biocides should be made mandatory. The role of antimicrobial stewardship cannot be overemphasized; mechanisms should be instituted to commence stewardship programmes where lacking and made more functional when the implementation of such programmes is suboptimal. Finally, there is a need for LMICs to invest in diagnostics (including rapid and POC diagnostics) and to ensure vaccination of a significant proportion of their population within the shortest possible time frame.
AMR Insights Ambassador Network
The first author and all co-authors are members of the Global AMR Insights Ambassador Network. The AMR Insights Ambassador Network consists of an integrated global and cross-professional community discussing, devising and driving actions to combat AMR. The Network aims to inspire, connect and empower the Ambassadors to take individual and collective actions to curb AMR. For more information about the Network: https://www.amr-insights.eu/about-us/ambassadors.
Acknowledgements
We would like to express our sincere thanks to the following members of the Global AMR Insights Ambassador Network for supporting us in preparing this manuscript: Herman W. Barkema, Steffanie Strathdee, Emmanuel Benyeogor, Uzairue Leonard Ighodalo, Kurcheti Pani Prasad, Carlos M., Yoshiaki Gu, Sabiha Essack, Dilan de Silva, Akke Vellinga, Wagih Mommtaz Ghannam, Najib Auwal Tsoho, M. H. F. Sakeena, Rhoda Ilenwabor, Dhanuraj (Raj) Shetty, Arnold Ayebare, Zoumana Isaac Traore, Ola Henry, Amritanjali Kiran, Rhoda Ilenwabor, Luisa Fernanda Toro, Adil Smail, Anne Amulele, Luria Leslie Founou, Prathamesh S. Sawant, Esther Buregyeya, Enrique Castro-Sanchez, Javier Moreno-Morales, Mina Izadjoo, Andrea Gori, Debra Goff, Arielle Blocker, Giovanna Forte, Muhammad Farooq Tahir, Mathew Diggle, Dipanjan Chakraborty, Anita E. Asamoah and Humphrey Aberi.
Funding
This study was supported by internal funding.
Transparency declarations
None to declare.
Footnotes
For more information on Global AMR Insights Ambassador Network and for the acknowledged members of the Network see underneath the article.
Contributor Information
Global AMR Insights Ambassador Network:
Herman W Barkema, Steffanie Strathdee, Emmanuel Benyeogor, Uzairue Leonard Ighodalo, Kurcheti Pani Prasad, Carlos M, Yoshiaki Gu, Sabiha Essack, Dilan de Silva, Akke Vellinga, Wagih Mommtaz Ghannam, Najib Auwal Tsoho, M H F Sakeena, Rhoda Ilenwabor, Dhanuraj (Raj) Shetty, Arnold Ayebare, Zoumana Isaac Traore, Ola Henry, Amritanjali Kiran, Rhoda Ilenwabor, Luisa Fernanda Toro, Adil Smail, Anne Amulele, Luria Leslie Founou, Prathamesh S Sawant, Esther Buregyeya, Enrique Castro-Sanchez, Javier Moreno-Morales, Mina Izadjoo, Andrea Gori, Debra Goff, Arielle Blocker, Giovanna Forte, Muhammad Farooq Tahir, Mathew Diggle, Dipanjan Chakraborty, Anita E Asamoah, and Humphrey Aberi
References
- 1. Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lu R, Zhao X, Li J et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395: 565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 2020; 5: 536–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sola I, Almazan F, Zuniga S et al. Continuous and discontinuous RNA synthesis in coronaviruses. Annu Rev Virol 2015; 2: 265–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018; 23: 130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anthony SJ, Johnson CK, Greig DJ et al. Global patterns in coronavirus diversity. Virus Evol 2017; 3: vex012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 2019; 17: 181–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ren LL, Wang YM, Wu ZQ et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J (Engl) 2020; 133: 1015–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Makela MJ, Puhakka T, Ruuskanen O et al. Viruses and bacteria in the etiology of the common cold. J Clin Microbiol 1998; 36: 539–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fung TS, Liu DX. Human coronavirus: host-pathogen interaction. Annu Rev Microbiol 2019; 73: 529–57. [DOI] [PubMed] [Google Scholar]
- 11. Li W, Shi Z, Yu M et al. Bats are natural reservoirs of SARS-like coronaviruses. Science 2005; 310: 676–9. [DOI] [PubMed] [Google Scholar]
- 12. Corman VM, Ithete NL, Richards LR et al. Rooting the phylogenetic tree of Middle East respiratory syndrome coronavirus by characterization of a conspecific virus from an African bat. J Virol 2014; 88: 11297–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hatmi ZN. A systematic review of systematic reviews on the COVID-19 pandemic. SN Compr Clin Med 2021; 3: 419–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Badawi A, Vasileva D. Comparative profile for COVID-19 cases from China and North America: clinical symptoms, comorbidities and disease biomarkers. World J Clin Cases 2021; 9: 118–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guan WJ, Ni ZY, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen N, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang W, Du RH, Li B et al. Molecular and serological investigation of 2019-nCoV infected patients: implication of multiple shedding routes. Emerg Microbes Infect 2020; 9: 386–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Novazzi F, Cassaniti I, Piralla A et al. SARS-CoV-2 positivity in rectal swabs: implication for possible transmission. J Glob Antimicrob Resist 2020; 22: 754–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tirupathi R, Ramparas TR, Wadhwa G et al. Viral dynamics in the upper respiratory tract (URT) of SARS-CoV-2. Infez Med 2020; 28: 486–99. [PubMed] [Google Scholar]
- 21. WHO. Coronavirus Disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=EAIaIQobChMIpdPJzaLy6wIVtsEWBR2-NAKfEAAYASAAEgI6B_D_BwE.
- 22. WHO Summary of Probable SARS Cases With Onset of Illness from 1 November 2002 to 31 July 2003. https://www.who.int/csr/sars/country/table2004_04_21/en/.
- 23. WHO Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Monthly Summary, November 2019. https://www.who.int/emergencies/mers-cov/en/.
- 24. Standl F, Jöckel KH, Brune B et al. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis 2020; doi:10.1016/S1473-3099(20)30648-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tirupathi R, Muradova V, Shekhar R et al. COVID-19 disparity among racial and ethnic minorities in the US: a cross sectional analysis. Travel Med Infect Dis 2020; 38: 101904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. WHO. United Nations High-Level Meeting on Antimicrobial Resistance. https://www.who.int/antimicrobial-resistance/events/UNGA-meeting-amr-sept2016/en/.
- 27. O’Neill J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations 2016. https://www.biomerieuxconnection.com/wp-content/uploads/2018/04/Tackling-Drug-Resistant-Infections-Globally_-Final-Report-and-Recommendations.pdf.
- 28. WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report Early Implementation 2017–2018. https://www.who.int/glass/resources/publications/early-implementation-report-2017-2018/en/.
- 29. Jernigan JA, Hatfield KM, Wolford H et al. Multidrug-resistant bacterial infections in U.S. hospitalized patients, 2012-2017. N Engl J Med 2020; 382: 1309–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. CDC. Antimicrobial Resistance Threats in the United States, 2019. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf.
- 31. CDC. Antibiotic Resistance Threats in the United States, 2013. https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf.
- 32. ECDC. The Bacterial Challenge: Time to React. https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/0909_TER_The_Bacterial_Challenge_Time_to_React.pdf.
- 33. Central for Disease Control and Prevention. Infographic: Antibiotic Resistance: The Global Threat. https://www.cdc.gov/globalhealth/infographics/antibiotic-resistance/antibiotic_resistance_global_threat.htm.
- 34. WHO. Antimicrobial Resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
- 35. The World Bank. Drug-Resistant Infections: A Threat to Our Economic Future. http://documents.worldbank.org/curated/en/323311493396993758/final-report.
- 36. ECDC. Antimicrobial Resistance: Tackling the Burden in the European Union. https://www.oecd.org/health/health-systems/AMR-Tackling-the-Burden-in-the-EU-OECD-ECDC-Briefing-Note-2019.pdf.
- 37. Antibiotic Development: The 10 x ’20 Initiative. https://www.idsociety.org/policy–advocacy/antimicrobial-resistance/antibiotic-development-the-10-x-20-initiative/.
- 38. Exner M, Bhattacharya S, Christiansen B et al. Antibiotic resistance: what is so special about multidrug-resistant Gram-negative bacteria? GMS Hyg Infect Control 2017; 12: Doc05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kulkarni AP, Nagvekar VC, Veeraraghavan B et al. Current perspectives on treatment of Gram-positive infections in India: what is the way forward? Interdiscip Perspect Infect Dis 2019; 2019: 7601847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis 2008; 197: 1079–81. [DOI] [PubMed] [Google Scholar]
- 41. Tacconelli E, Carrara E, Savoldi A et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis 2018; 18: 318–27. [DOI] [PubMed] [Google Scholar]
- 42. WHO. Report on Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. https://www.who.int/medicines/publications/global-priority-list-antibiotic-resistant-bacteria/en/.
- 43. Buckner MMC, Ciusa ML, Piddock LJV. Strategies to combat antimicrobial resistance: anti-plasmid and plasmid curing. FEMS Microbiol Rev 2018; 42: 781–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Venter H, Henningsen ML, Begg SL. Antimicrobial resistance in healthcare, agriculture and the environment: the biochemistry behind the headlines. Essays Biochem 2017; 61: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nieuwlaat R, Mbuagbaw L, Mertz D et al. COVID-19 and antimicrobial resistance: parallel and interacting health emergencies. Clin Infect Dis 2020; doi:10.1093/cid/ciaa773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wang D, Hu B, Hu C et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mallia P, Footitt J, Sotero R et al. Rhinovirus infection induces degradation of antimicrobial peptides and secondary bacterial infection in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012; 186: 1117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol 2017; 8: 1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang H, Anthony D, Selemidis S et al. Resolving viral-induced secondary bacterial infection in COPD: A concise review. Front Immunol 2018; 9: 2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chen G, Wu D, Guo W et al. Clinical and immunologic features in severe and moderate coronavirus disease 2019. J Clin Invest 2020; 130: 2620–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pedersen SF, Ho YC. SARS-CoV-2: a storm is raging. J Clin Invest 2020; 130: 2202–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kim YG, Park JH, Reimer T et al. Viral infection augments Nod1/2 signaling to potentiate lethality associated with secondary bacterial infections. Cell Host Microbe 2011; 9: 496–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hendaus MA, Jomha FA, Alhammadi AH. Virus-induced secondary bacterial infection: a concise review. Ther Clin Risk Manag 2015; 11: 1265–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nyangacha RM, Odongo D, Oyieke F et al. Secondary bacterial infections and antibiotic resistance among tungiasis patients in Western, Kenya. PLoS Negl Trop Dis 2017; 11: e0005901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pittet LA, Hall-Stoodley L, Rutkowski MR et al. Influenza virus infection decreases tracheal mucociliary velocity and clearance of Streptococcus pneumoniae. Am J Respir Cell Mol Biol 2010; 42: 450–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Mehta OP, Bhandari P, Raut A et al. Coronavirus disease (COVID-19): comprehensive review of clinical presentation. Front Public Health 2021; 8: 582932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kalil AC, Metersky ML, Klompas M et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 2016; 63: e61–e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Reignier J, Mercier E, Le Gouge A et al. Effect of not monitoring residual gastric volume on risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA 2013; 309: 249–56. [DOI] [PubMed] [Google Scholar]
- 59. Seguin P, Laviolle B, Dahyot-Fizelier C et al. Effect of oropharyngeal povidone-iodine preventive oral care on ventilator-associated pneumonia in severely brain-injured or cerebral hemorrhage patients: a multicenter, randomized controlled trial. Crit Care Med 2014; 42: 1–8. [DOI] [PubMed] [Google Scholar]
- 60. Yang X, Yu Y, Xu J et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Du Y, Tu L, Zhu P et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med 2020; 201: 1372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Grasselli G, Zangrillo A, Zanella A et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020; 323: 1574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Goyal P, Choi JJ, Pinheiro LC et al. Clinical characteristics of Covid-19 in New York City. N Engl J Med 2020; 382: 2372–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Arentz M, Yim E, Klaff L et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA 2020; 323: 1612–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Lu L, Zhang H, Zhan M et al. Preventing mortality in COVID-19 patients: which cytokine to target in a raging storm? Front Cell Dev Biol 2020; 8: 677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lai CC, Shih TP, Ko WC et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020; 55: 105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Langford BJ, So M, Raybardhan S et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect 2020; 26: 1622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zhou F, Yu T, Du R et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Zhang H, Zhang Y, Wu J et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect 2020; 9: 1958–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chen T, Wu D, Chen H et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020; 368: m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wang Z, Yang B, Li Q et al. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis 2020; 71: 769–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Lescure FX, Bouadma L, Nguyen D et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis 2020; 20: 697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chowdhary A, Tarai B, Singh A et al. Multidrug-resistant Candida auris infections in critically ill coronavirus disease patients, India, April-July 2020. Emerg Infect Dis 2020; 26: 2694–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Mandell LA, Wunderink RG, Anzueto A et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44: S27–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Rawson TM, Ming D, Ahmad R et al. Antimicrobial use, drug-resistant infections and COVID-19. Nat Rev Microbiol 2020; 18: 409–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Dryden MS, Cooke J, Davey P. Antibiotic stewardship–more education and regulation not more availability? J Antimicrob Chemother 2009; 64: 885–8. [DOI] [PubMed] [Google Scholar]
- 77. Osterholm MT. Preparing for the next pandemic. N Engl J Med 2005; 352: 1839–42. [DOI] [PubMed] [Google Scholar]
- 78. Talbot GH, Jezek A, Murray BE et al. The Infectious Diseases Society of America’s 10 × ’20 initiative (10 new systemic antibacterial agents US Food and Drug Administration approved by 2020): is 20 × ’20 a possibility? Clin Infect Dis 2019; 69: 1–11. [DOI] [PubMed] [Google Scholar]
- 79. WHO. Clinical Management of COVID-19: Interim Guidance. https://www.who.int/publications/i/item/clinical-management-of-covid-19.
- 80. Huttner BD, Catho G, Pano-Pardo JR et al. COVID-19: don’t neglect antimicrobial stewardship principles! Clin Microbiol Infect 2020; 26: 808–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. International Severe Acute Respiratory and Emerging Infection Consortium. COVID-19 Report: 08 April 2020. https://media.tghn.org/medialibrary/2020/04/ISARIC_Data_Platform_COVID-19_Report_8APR20.pdf.
- 82. Dong X, Cao YY, Lu XX et al. Eleven faces of coronavirus disease 2019. Allergy 2020; 75: 1699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Rawson TM, Moore LSP, Zhu N et al. Bacterial and fungal co-infection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis 2020; 71: 2459–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Cao J, Tu W-J, Cheng W et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clin Infect Dis 2020; 71: 748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Karami Z, Knoop BT, Dofferhoff ASM et al. Few bacterial co-infections but frequent empiric antibiotic use in the early phase of hospitalized patients with COVID-19: results from a multicentre retrospective cohort study in The Netherlands. Infect Dis (Lond) 2021; 53: 102–10. [DOI] [PubMed] [Google Scholar]
- 86. Potempa LA, Rajab IM, Hart PC et al. Insights into the use of C-reactive protein as a diagnostic index of disease severity in COVID-19 infections. Am J Trop Med Hyg 2020; 103: 561–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Feng X, Li S, Sun Q et al. Immune-inflammatory parameters in COVID-19 cases: a systematic review and meta-analysis. Front Med 2020; 7: 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Dhesi Z, Enne VI, O’Grady J et al. Rapid and point-of-care testing in respiratory tract infections: an antibiotic guardian? ACS Pharmacol Transl Sci 2020; 3: 401–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Self WH, Rosen J, Sharp SC et al. Diagnostic accuracy of FebriDx: a rapid test to detect immune responses to viral and bacterial upper respiratory infections. J Clin Med 2017; 6: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Mason CY, Kanitkar T, Richardson CJ et al. Exclusion of bacterial co-infection in COVID-19 using baseline inflammatory markers and their response to antibiotics. J Antimicrob Chemother 2021; doi:10.1093/jac/dkaa563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Schuetz P, Wirz Y, Sager R et al. Procalcitonin to initiate or discontinue antibiotics in acute respiratory tract infections. Cochrane Database Syst Rev 2017; issue 10: CD007498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Williams EJ, Mair L, Silva TI d et al. Evaluation of procalcitonin as a contribution to antimicrobial stewardship in SARS-CoV-2 infection: a retrospective cohort study. J Hosp Infect 2021; 110: 103–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Gautret P, Lagier J-C, Parola P et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020; 56: 105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 94. Russel AD. Mechanism of antimicrobial action of antiseptics and disinfectants: an increasingly important area of investigation. J Antimicrob Chemother 2002; 49: 597–9. [DOI] [PubMed] [Google Scholar]
- 95. Buffet-Bataillon S, Tattevin P, Bonnaure-Mallet M et al. Emergence of resistance to antibacterial agents: the role of quaternary ammonium compounds–a critical review. Int J Antimicrob Agents 2012; 39: 381–9. [DOI] [PubMed] [Google Scholar]
- 96. Levy SB. Active efflux, a common mechanism for biocide and antibiotic resistance. Symp Ser Soc Appl Microbiol 2002; 31: 655–715. [PubMed] [Google Scholar]
- 97. Maillard JY. Antimicrobial biocides in the healthcare environment: efficacy, usage, policies, and perceived problems. Ther Clin Risk Manag 2005; 1: 307–20. [PMC free article] [PubMed] [Google Scholar]
- 98. Pal C, Bengtsson-Palme J, Kristiansson E et al. Co-occurrence of resistance genes to antibiotics, biocides and metals reveals novel insights into their co-selection potential. BMC Genomics 2015; 16: 964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Webber MA, Whitehead RN, Mount M et al. Parallel evolutionary pathways to antibiotic resistance selected by biocide exposure. J Antimicrob Chemother 2015; 70: 2241–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. McBain AJ, Rickard AH, Gilbert P. Possible implications of biocide accumulation in the environment on the prevalence of bacterial antibiotic resistance. J Ind Microbiol Biotechnol 2002; 29: 326–30. [DOI] [PubMed] [Google Scholar]
- 101. Fouz N, Pangesti KNA, Yasir M et al. The contribution of wastewater to the transmission of antimicrobial resistance in the environment: implications of mass gathering settings. Trop Med Infect Dis 2020; 5: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Coronavirus Warning: Mass Use of Hand Gels Could CREATE Unstoppable Superbugs - Expert. https://www.express.co.uk/news/uk/1329220/coronavirus-superbug-warning-hand-gels-health-danger-andrew-kemp-covid-19.
- 103. Robben C, Fister S, Witte AK et al. Induction of the viable but non-culturable state in bacterial pathogens by household cleaners and inorganic salts. Sci Rep 2018; 8: 15132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Gupte AR, de Rezende CLE, Joseph SW. Induction and resuscitation of viable but nonculturable Salmonella enterica serovar Typhimurium DT104. Appl Environ Microbiol 2003; 69: 6669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. WHO. Prioritization of Pathogens to Guide Discovery, Research and Development of New Antibiotics for Drug Resistant Bacterial Infections, Including Tuberculosis. https://www.who.int/medicines/areas/rational_use/prioritization-of-pathogens/en/.
- 106. Chibabhai V, Duse AG, Perovic O et al. Collateral damage of the COVID-19 pandemic: exacerbation of antimicrobial resistance and disruptions to antimicrobial stewardship programmes? S Afr Med J 2020; 110: 572–3. [DOI] [PubMed] [Google Scholar]
- 107. Liew Y, Lee WHL, Tan L et al. Antimicrobial stewardship program, a vital resource for hospitals during the global outbreak of coronavirus disease 2019 (COVID-19). Int J Antimicrob Agents 2020; 56: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Ashiru-Oredope D, Kerr F, Hughes S et al. Assessing the impact of COVID-19 on antimicrobial stewardship activities/programs in the United Kingdom. Antibiotics (Basel) 2021; 10: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Getahun H, Smith I, Trivedi K et al. Tackling antimicrobial resistance in the COVID-19 pandemic. Bull World Health Organ 2020; 98: 442–442A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. American College of Emergency Physicians. Antimicrobial stewardship. Ann Emerg Med 2020; 76: e109–e112. [DOI] [PubMed] [Google Scholar]
- 111. Huttner B, Jones M, Rubin MA et al. Double trouble: how big a problem is redundant anaerobic antibiotic coverage in Veterans Affairs medical centres? J Antimicrob Chemother 2012; 67: 1537–9. [DOI] [PubMed] [Google Scholar]
- 112. Drew RH, White R, MacDougall C et al. Insights from the Society of Infectious Diseases Pharmacists on antimicrobial stewardship guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Pharmacotherapy 2009; 29: 593–607. [DOI] [PubMed] [Google Scholar]
- 113. Dellit TH, Owens RC, McGowan JE Jr et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007; 44: 159–77. [DOI] [PubMed] [Google Scholar]
- 114. Aarts MA, Hancock JN, Heyland D et al. Empiric antibiotic therapy for suspected ventilator-associated pneumonia: a systematic review and meta-analysis of randomized trials. Crit Care Med 2008; 36: 108–17. [DOI] [PubMed] [Google Scholar]
- 115. De Waele JJ, Ravyts M, Depuydt P et al. De-escalation after empirical meropenem treatment in the intensive care unit: fiction or reality? J Crit Care 2010; 25: 641–6. [DOI] [PubMed] [Google Scholar]
- 116. Johnson SJ, Ernst EJ, Moores KG. Is double coverage of gram-negative organisms necessary? Am J Health Syst Pharm 2011; 68: 119–24. [DOI] [PubMed] [Google Scholar]
- 117. Niederman MS, Soulountsi V. De-escalation therapy: is it valuable for the management of ventilator-associated pneumonia? Clin Chest Med 2011; 32: 517–34. [DOI] [PubMed] [Google Scholar]
- 118. Bliziotis IA, Samonis G, Vardakas KZ et al. Effect of aminoglycoside and β-lactam combination therapy versus β-lactam monotherapy on the emergence of antimicrobial resistance: a meta-analysis of randomized, controlled trials. Clin Infect Dis 2005; 41: 149–58. [DOI] [PubMed] [Google Scholar]
- 119. Chandy SJ, Mathai E, Thomas K et al. Antibiotic use and resistance: perceptions and ethical challenges among doctors, pharmacists and the public in Vellore, South India. Indian J Med Ethics 2013; 10: 20–7. [DOI] [PubMed] [Google Scholar]
- 120. Huttner B, Saam M, Moja L et al. How to improve antibiotic awareness campaigns: findings of a WHO global survey. BMJ Glob Health 2019; 4: e001239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Okoth C, Opanga S, Okalebo F et al. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: findings and implications. Hosp Pract (1995) 2018; 46: 128–36. [DOI] [PubMed] [Google Scholar]
- 122. Saleem Z, Hassali MA, Versporten A et al. A multicenter point prevalence survey of antibiotic use in Punjab, Pakistan: findings and implications. Expert Rev Anti Infect Ther 2019; 17: 285–93. [DOI] [PubMed] [Google Scholar]
- 123. Anand Paramadhas BD, Tiroyakgosi C, Mpinda-Joseph P et al. Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Expert Rev Anti Infect Ther 2019; 17: 535–46. [DOI] [PubMed] [Google Scholar]
- 124. Pierce J, Apisarnthanarak A, Schellack N et al. Global antimicrobial stewardship with a focus on low- and middle-income countries. Int J Infect Dis 2020; 96: 621–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Fadare JO, Ogunleye O, Iliyasu G et al. Status of antimicrobial stewardship programmes in Nigerian tertiary healthcare facilities: Findings and implications. J Glob Antimicrob Resist 2019; 17: 132–6. [DOI] [PubMed] [Google Scholar]
- 126. Mendelson M, Røttingen J-A, Gopinathan U et al. Maximizing access to achieve appropriate human antimicrobial use in low-income and middle-income countries. Lancet 2016; 387: 188–98. [DOI] [PubMed] [Google Scholar]
- 127. Cox JA, Vlieghe E, Mendelson M et al. Antibiotic stewardship in low- and middle-income countries: the same but different? Clin Microbiol Infect 2017; 23: 812–8. [DOI] [PubMed] [Google Scholar]
- 128. Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One 2017; 12: e0189621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Laxminarayan R, Duse A, Wattal C et al. Antibiotic resistance- the need for global solutions. Lancet Infect Dis 2013; 13: 1057–98. [DOI] [PubMed] [Google Scholar]
- 130. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020; 382: 1679–81. [DOI] [PubMed] [Google Scholar]
- 131. Llor C, Moragas A, Bayona C et al. Efficacy of anti-inflammatory or antibiotic treatment in patients with non-complicated acute bronchitis and discoloured sputum: randomised placebo controlled trial. BMJ 2013; 347: f5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Little P, Stuart B, Moore M et al. Amoxicillin for acute lower-respiratory-tract infection in primary care when pneumonia is not suspected: a 12-country, randomised, placebo-controlled trial. Lancet Infect Dis 2013; 13: 123–9. [DOI] [PubMed] [Google Scholar]
- 133. United Nations’ Sustainable Development Goals. Take Action for the Sustainable Development Goals. https://www.un.org/sustainabledevelopment/health/.
- 134. WHO. WHO and FIND Formalize Strategic Collaboration to Drive Universal Access to Essential Diagnostics. https://www.who.int/news-room/detail/10-02-2020-who-and-find-formalize-strategic-collaboration-to-drive-universal-access-to-essential-diagnostics.
- 135. Developing Countries Face Diagnostic Challenges as the COVID-19 Pandemic Surges. https://cen.acs.org/analytical-chemistry/diagnostics/Developing-countries-face-diagnostic-challenges/98/i27.
- 136. Hays JP, Mitsakakis K, Luz S et al. The successful uptake and sustainability of rapid infectious disease and antimicrobial resistance point-of-care testing requires a complex ‘mix-and-match’ implementation package. Eur J Clin Microbiol Infect Dis 2019; 38: 1015–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Hjálmarsdóttir MÁ, Haraldsson G, Quirk SJ et al. Reduction of antimicrobial resistant pneumococci seven years after introduction of pneumococcal vaccine in Iceland. PLoS One 2020; 15: e0230332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Brook I, Gober A. Bacteriology of spontaneously draining acute otitis media in children before and after the introduction of pneumococcal vaccination. Pediatr Infect Dis J 2009; 28: 640–2. [DOI] [PubMed] [Google Scholar]
- 139. Park SY, Moore MR, Bruden DL et al. Impact of conjugate vaccine on transmission of antimicrobial-resistant Streptococcus pneumoniae among Alaskan children. Pediatr Infect Dis J 2008; 27: 335–40. [DOI] [PubMed] [Google Scholar]
- 140. Casey JR, Pichichero ME. Changes in frequency and pathogens causing acute otitis media in 1995–2003. Pediatr Infect Dis J 2004; 23: 824–8. [DOI] [PubMed] [Google Scholar]
- 141. Garbutt J, Rosenbloom I, Wu J et al. Empiric first-line antibiotic treatment of acute otitis in the era of the heptavalent pneumococcal conjugate vaccine. Pediatrics 2006; 117: e1087–94. [DOI] [PubMed] [Google Scholar]
- 142. Understanding Opposition to Vaccines. https://www.healthline.com/health/vaccinations/opposition.
- 143. Marín-Hernández D, Schwartz RE, Nixon DF. Epidemiological evidence for association between higher influenza vaccine uptake in the elderly and lower COVID-19 deaths in Italy. J Med Virol 2021; 93: 64–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Bachtiger P, Adamson A, Chow J-J et al. The impact of the Covid-19 pandemic on uptake of influenza vaccine: a UK-wide observational study. medRxiv2020; doi:10.1101/2020.10.01.20205385. [DOI] [PMC free article] [PubMed]
- 145. Voysey M, Clemens SAC, Madhi SA et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 2021; 397: 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. FDA. Pfizer-BioNTech COVID-19 Vaccine: Emergency Use Authorization. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine.
- 147. Oliver SE, Gargano JW, Marin M et al. The Advisory Committee on Immunization Practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 1922–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Baden LR, El Sahly HM, Essink B et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021; 384: 403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Covid Variants: what are they and will vaccines work? https://www.bbc.com/news/health-55659820.