Editor
Non-emergency services offered by the National Health Service were significantly affected during the COVID-19 pandemic1. Concerns were raised about the impact on care of other groups of patients who require time-critical intervention, such as those with suspected colorectal cancer2. These patients are referred through rapid-access pathways for diagnostic investigations, according to certain criteria specified by national guidelines3. It is feared that this pathway was compromised during the COVID-19 period. This study examined the impact of the COVID-19 pandemic on the (colorectal cancer) early diagnostic pathway, and subsequent delays in diagnosis and treatment of these patients in Kettering General Hospital.
Patients referred with suspected colorectal cancer via the 2-week wait pathway, between 1 March and 31 July 2020, were compared with those referred during the equivalent period in 2019. The following parameters were compared: total number of referrals, time to first appointment, time from referral to diagnosis, and percentage of patients who achieved a diagnosis within 28 days and referral to treatment (RTT).
A total of 460 patients were included in the 2020 cohort, compared with 808 in the 2019 cohort (43.1 per cent drop). The most significant decrease was noticed in April 2020 during the peak of the pandemic.
Some 90.0 per cent of first appointments were conducted within 2 weeks of referral in 2020 compared with 97.0 per cent in 2019. It is worth highlighting that half of the clinic appointments were made virtual (49.0 per cent) to mitigate the impact of COVID-19.
The diagnosis target was achieved in 70.4 per cent of patients in 2020 versus 88.0 per cent in 2019. The mean time from referral to diagnosis was significantly higher in the COVID cohort (Fig. 1). The total number of delays was 136 (29.6 per cent) in 2020 compared with 97 (12.0 per cent) in 2019. COVID-19 was the documented reason for delay in 78 (57.4 per cent) of the pandemic cohort. This meant that 10 of 22 patients requiring cancer treatment missed their RTT target of 62 days in the COVID-19 cohort compared with only 2 of 14 in the pre-COVID-19 cohort. Surprisingly, the yield of cancer diagnosis increased by 35.4 per cent during the COVID-19 period despite the reduced number of referrals. This may indicate that the fear of missing a cancer diagnosis might be exaggerated. However, this assumption must be examined cautiously by future studies to detect surges in patients with delayed presentations.
Fig. 1.
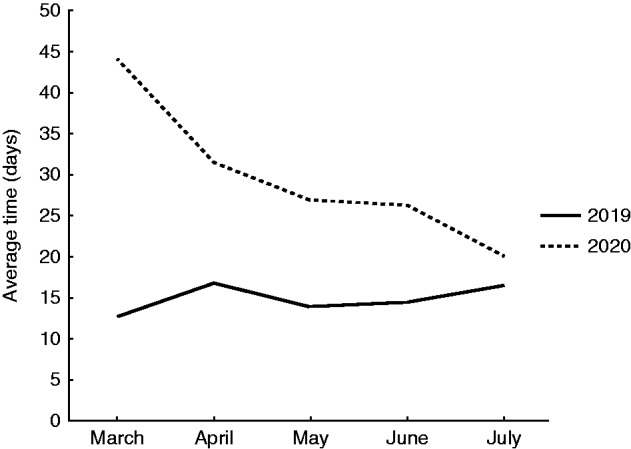
Mean time from referral to diagnosis for each month
The delay in diagnosis and starting treatment is definitely a big concern. Sud and colleagues4 reported that a 3-month delay in diagnosis of colorectal cancer would result in at least a 10.0 per cent drop in 10-year survival rates.
Lessons should be learnt from the first-wave experience to mitigate the impact of any future lockdowns. Developing triage systems using alternative tests, such as the faecal immunochemical test, in primary care helped stratify patients into highest or lowest risk of bowel cancer5. Virtual clinics and telemedicine were introduced across the country to help tackle similar problems. Straight to test is another channel that general practitioners (GPs) can use in patients with strongly suspected pathology. To a similar extent, educational media campaigns to urge people to seek help when needed are vital to prevent patients delaying presentation to a GP.
Disclosure
The authors declare no conflict of interest.
References
- 1. Courtney A, Howell AM, Daulatzai N, Savva N, Warren O, Mills S et al. Colorectal cancer services during the COVID‐19 pandemic. Br J Surg 2020;107:e255–e256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020;21:1023–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Institute for Health and Care and Excellence (NICE). Colorectal Cancer: Diagnosis and Management . London: NICE, 2014. [Google Scholar]
- 4. Sud A, Torr B, Jones ME, Broggio J, Scott S, Loveday C et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol 2020;21:1035–1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee YH, Kung PT, Wang YH, Kuo WY, Kao SL, Tsai WC. Effect of length of time from diagnosis to treatment on colorectal cancer survival: a population-based study. PLoS One 2019;14:e0210465. [DOI] [PMC free article] [PubMed] [Google Scholar]


