Abstract
Aims
TeleCheck-AF is a multicentre international project initiated to maintain care delivery for patients with atrial fibrillation (AF) during COVID-19 through teleconsultations supported by an on-demand photoplethysmography-based heart rate and rhythm monitoring app (FibriCheck®). We describe the characteristics, inclusion rates, and experiences from participating centres according the TeleCheck-AF infrastructure as well as characteristics and experiences from recruited patients.
Methods and results
Three surveys exploring centre characteristics (n = 25), centre experiences (n = 23), and patient experiences (n = 826) were completed. Self-reported patient characteristics were obtained from the app. Most centres were academic (64%) and specialized public cardiology/district hospitals (36%). Majority of the centres had AF outpatient clinics (64%) and only 36% had AF ablation clinics. The time required to start patient inclusion and total number of included patients in the project was comparable for centres experienced (56%) or inexperienced in mHealth use. Within 28 weeks, 1930 AF patients were recruited, mainly for remote AF control (31% of patients) and AF ablation follow-up (42%). Average inclusion rate was highest during the lockdown restrictions and reached a steady state at a lower level after easing the restrictions (188 vs. 52 weekly recruited patients). Majority (>80%) of the centres reported no problems during the implementation of the TeleCheck-AF approach. Recruited patients [median age 64 (55–71), 62% male] agreed that the FibriCheck® app was easy to use (94%).
Conclusion
Despite different health care settings and mobile health experiences, the TeleCheck-AF approach could be set up within an extremely short time and easily used in different European centres during COVID-19.
Keywords: Atrial fibrillation, eHealth, mHealth, Remote monitoring, Telemedicine, TeleCheck-AF, COVID-19
What’s new?
TeleCheck-AF represents an integrated approach for remote management of patients with atrial fibrillation through teleconsultations supported by an on-demand photoplethysmography-based heart rate and rhythm monitoring app.
Despite different health care settings and mHealth experiences, the TeleCheck-AF approach has been set-up within an extremely short time frame using digital channels such as social media and is actively used in different European centres during the COVID-19 pandemic.
The used app was easy to use and easy to install by patients and supported the assessment of rate and rhythm around teleconsultation, which showed that more than half of the patients with a photoplethysmography-detected AF episode were asymptomatic.
The TeleCheck-AF approach presents an alternative and/or supplement to traditional face-to-face consultations with a potential to reduce in-office and unnecessary hospital visits, thereby reducing health care burden.
Introduction
Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia. Patients with uncontrolled AF are considered vulnerable and are at high risk of heart failure, stroke, bleeding, acute coronary syndrome, and adverse effects of antiarrhythmic drugs, all of which may lead to unplanned cardiovascular hospitalization and mortality.1,2 AF management requires a comprehensive approach, including heart rate or rhythm control, stroke prevention with appropriate anticoagulation therapy, treatment of comorbidities, risk factors, and lifestyle modification.2 Traditionally, AF patients are managed through face-to-face consultations in a practice or outpatient clinic by the treating cardiologist, general practitioner, or AF nurse allowing for heart rate and rhythm control through electrocardiogram (ECG). However, during the COVID-19 pandemic, scheduled outpatient consultations were cancelled to keep vulnerable patients out of the hospital, and face-to-face appointments were converted into teleconsultations.3 Although teleconsultation solutions can produce remote situations that are relatively similar to face-to-face interaction,4 the effective remote monitoring and management of AF patients is limited, mainly due to the absence of heart rate and rhythm information of the patient. As a response, different centres all over the world started to combine their teleconsultations with mobile health (mHealth) solutions for remote heart rate and rhythm monitoring.5 With the aim to synchronize activities, to gather data on managed AF patients and to make this approach widely available in European centres, the Cardiology Department of the Maastricht University Medical Centre+ (MUMC+) in Maastricht, the Netherlands, developed a standard operating procedure document describing the TeleCheck-AF approach.6 It incorporates teleconsultations coupled with remote on-demand photoplethysmography (PPG)-based heart rate and rhythm monitoring (FibriCheck®) to allow the treating cardiologist, general practitioner or AF-nurse to comprehensively manage their AF patients through teleconsultation.
Herein, we describe the characteristics of participating centres in the TeleCheck-AF project. We discuss the patient inclusion rate and use of the mHealth infrastructure in the context of centre characteristics and the policy restrictions related to the COVID-19 pandemic in each corresponding country. In addition, we describe centre and patient experiences regarding the TeleCheck-AF infrastructure and self-reported characteristics of recruited patients.
Methods
Project design
The TeleCheck-AF approach is described elsewhere in detail.6 In brief, TeleCheck-AF is an mHealth infrastructure, initially dedicated to maintaining management of AF outpatients during the COVID-19 pandemic. It helps to guarantee the continuity of comprehensive AF management through teleconsultations preceded by remote heart rate and rhythm monitoring using mobile phone app.
One week prior to the scheduled teleconsultation, the patient is provided with an mHealth prescription to use a Conformité Européenne (CE)-marked mobile phone app (www.fibricheck.com) to assess heart rhythm and rate7 three times a day and in case of symptoms through seven days. Additionally, the app provides educational information about AF, its complications and treatment.8 If needed, patients can contact the physician prior to the planned teleconsulatation in case of alarming symptoms. Before the teleconsultation, the treating physician, general practitioner and AF-nurse have access to the cloud to evaluate the measurements.6 During the teleconsultation, similar to standard face-to-face consultation, detailed history taking and adaptation of rate and rhythm control and anticoagulation treatment is performed, as indicated.9 The detailed components of the teleconsultation are described in Supplementary material online, Figure S1. The evaluation of an individualized treatment plan, patient education and medication management is assessed by patient well-being data provided simultaneously with heart rhythm and rate assessment.
Initiation of the project in each centre
One of the biggest advantages of the TeleCheck-AF approach is the broad accessibility of the mobile phone app that allowed a fast implementation of the herein described mHealth infrastructure. In the TeleCheckAF project, fast recruitment of centres was also achieved by using digital channels such as social media.10 All participating centres received a standardized initiation video call to inform and instruct each participating centre based on the detailed standard operating procedure document.6 Additionally, documents with further information regarding the CE mark form were provided. Direct Hotline numbers to the Cardiology Department of the MUMC+ and to FibriCheck® were available throughout the project to answer questions and support with the implementation of the mHealth infrastructure. Each participating centre was provided with the TeleCheck-AF mHealth infrastructure for free throughout the project duration. The centres were updated about the progress of the project and the inclusion rates in a weekly newsletter.
Purpose of TeleCheck-AF usage
The TeleCheck-AF approach was initially dedicated to maintaining remote management of AF patients scheduled for a consultation in AF outpatient clinics. The intended use of the TeleCheck-AF project has been expanded over the past months to patient monitoring around AF ablation and/or electrical cardioversion, rate control as part of heart failure management, detection of arrhythmias in patients with palpitations, and other arrhythmia-related symptoms.
Data collection
The results of the three surveys were based on a questionnaire sent via mail to the principal project supervisors (physicians) in each participating centre and recruited patients. The centres’ characteristics survey was sent within the first two weeks after centre inclusion. Centre experience survey was sent at the 28th week of the project duration, and only to centres that completed the first survey. The patient experience survey was sent to each patient within the week following the teleconsultation. Depending on the geographical country localization, centres were categorized into three country groups: Group ‘1’ (Belgium and The Netherlands), Group ‘2’ (Austria, Germany, and Poland), and Group ‘3’ (Denmark, Ireland, Sweden, and UK).
The centre characteristics survey questions concerned type of centre (university, specialized public cardiology, or district hospital), number of weekly performed procedures (physician–patient consultations, Holter monitoring, and AF ablations), presence of AF ablation and AF outpatient clinics and integration of mHealth devices/tools, and remote consultations in the healthcare system. The AF outpatient clinic is defined as an outpatient service that provides complex AF treatment incorporating patient assessment, implementation of an individualized treatment plan, patient education, medication management, and follow-up care,11 whereas the AF ablation clinic is defined as an outpatient service that provides periprocedural AF ablation treatment. The complete questionnaire is provided in Supplementary material online, Figure S2.
The centre experience survey evaluated potential problems or issues during the implementation of the TeleCheck-AF approach in the healthcare system, facility of on-boarding process of centre in the TeleCheck-AF project, facility of cloud infrastructure usage, experience with TeleCheck-AF approach, future challenges of TeleCheck-AF approach implementation in healthcare system, and future TeleCheck-AF approach dedicated group of patients. The complete questionnaire is provided in Supplementary material online, Figure S3.
The patient experience survey encompassed five questions regarding ease of use and installation of the app, usability of daily reminders for heart rate and rhythm assessment, willingness to use the app in the future and whether the patient feels safe while being under heart rate and rhythm control via app. The complete questionnaire is provided in Supplementary material online, Figure S4.
Additionally, the number of daily recruited patients by each centre, patient characteristics and number of heart rate and rhythm measurements was obtained anonymously from the FibriCheck® cloud (status from 9 October 2020). The COVID-19 policy responses in each country were obtained from countries’ government websites supported by information from https://askabout.io/covid-19/ask/what-is-the-global-covid-19-situation/ (accessed on 5 July 2020).
Statistical analysis
All continuous variables were tested for normality with the Shapiro–Wilk test. Variables with normal distribution were expressed as mean ± standard deviation (SD). Nonparametric variables were expressed as median, inter-quartile range (IQR) and categorical variables as counts (n) with percentages (%).To assess correlations with time until the first patient inclusion, time required to ten patients inclusion, number of included patients, procedures performed (Holter monitoring, AF ablations, consultations) and working physicians in AF outpatient clinics in each centre, Pearson’s correlation was calculated. Statistical significance was assumed at a 5% level. For database management and statistical analysis, we used SAS 14.1 (SAS Institute Inc., Cary, NC, USA).
Results
Centre characteristics
The centre characteristics survey was sent to the participating centres at four weeks after commencing the TeleCheck-AF project and was completed by 25 centres across nine countries, including the 23 centres with the highest number of patients included in the TeleCheck-AF project. Twelve additional centres were enrolled at a later stage during the course of the project but did not complete the survey. The characteristics per country are presented in (Supplementary material online, Table S1). Centres were stratified into country groups: Group ‘1’ involved 11 centres (six from the Netherlands, five from Belgium); Group ‘2’ involved seven centres (five from Germany, one from each Poland and Austria); and Group ‘3’ involved seven centres (four from UK and one from each Denmark, Ireland, and Sweden). The characteristics of all centres stratified per country group are presented in Table 1.
Table 1.
Centre characteristics by European geographical location
| Total (n = 25) | Group ‘1’ (n = 11) | Group ‘2’ (n = 7) | Group ‘3’ (n = 7) | |
|---|---|---|---|---|
| NL and BE | DE, AT, and PL | UK, IL, DK, and SE | ||
| Centre characteristics | ||||
| University hospital | 16 (64%) | 4 (36%) | 6 (86%) | 6 (86%) |
| Specialized public cardiology hospital | 6 (24%) | 5 (45%) | 0 (0%) | 1 (14%) |
| District/community hospital | 3 (12%) | 2 (18%) | 1 (14%) | 0 (0%) |
| AF outpatient clinic | 16 (64%) | 8 (73%) | 4 (57%) | 4 (57%) |
| No. of physicians working in AF outpatient clinic | 5 (4–6) | 4 (4–5) | 6 (5–6) | 8 (6–12) |
| AF ablation clinic | 9 (36%) | 4 (36%) | 3 (43%) | 2 (29%) |
| No. of AF consultations performed per week | 50 (30–94) | 50 (30–85) | 40 (33–70) | 100 (59–110) |
| No. of Holter monitoring performed per week | 50 (20–80) | 55 (8–83) | 40 (25–50) | 50 (40–75) |
| No. of AF ablations performed per week | 8 (4–12) | 5 (4–10) | 9 (7–10) | 12 (3–18) |
| Time spent to prepare the consult (min) | 10 (5–10) | 5 (5–13) | 10 (5–10) | 10 (5–11) |
| Time spent to perform the consult (min) | 15 (15–20) | 15 (13–15) | 15 (13–20) | 20 (20–30) |
| Video consultation integrated in healthcare system | 10 (40%) | 3 (27%) | 5 (71%) | 2 (29%) |
| mHealth (app, devices) integrated in healthcare system | 14 (56%) | 9 (82%) | 4 (57%) | 1 (14%) |
| Reasons for mHealth usage by centre before TeleCheck-AF | ||||
| AF control (rate and rhythm) | 8 (57%) | 4 (44%) | 4 (100%) | 0 (0%) |
| Management of rate control | 4 (29%) | 3 (33%) | 1 (25%) | 0 (0%) |
| Management of rhythm control | 5 (36%) | 3 (33%) | 2 (50%) | 0 (0%) |
| Risk assessment of stroke and bleeding risks | 2 (14%) | 2 (22%) | 0 (0%) | 0 (0%) |
| Follow-up after AF ablation | 7 (50%) | 3 (33%) | 4 (100%) | 0 (0%) |
| Other (CIED control, research, patient’s access to medical file) | 5 (36%) | 4 (44%) | 0 (0%) | 1 (100%) |
| Situations for mHealth usage by centre before TeleCheck-AF | ||||
| Prior to consultation | 9 (64%) | 7 (78%) | 2 (50%) | 0 (0%) |
| Post-consultation | 6 (43%) | 4 (44%) | 2 (50%) | 0 (0%) |
| Prior to procedure (ECV/AF ablation) | 2 (14%) | 1 (11%) | 1 (25%) | 0 (0%) |
| Post-procedure (ECV/AF ablation) | 6 (43%) | 3 (33%) | 3 (75%) | 0 (0%) |
| Continuously used by the patient | 2 (14%) | 0 (0%) | 2 (50%) | 0 (0%) |
| On demand of the patient | 6 (43%) | 4 (44%) | 2 (50%) | 0 (0%) |
| Type of mHealth devices used by centre before TeleCheck-AF | ||||
| Kardia Mobile | 7(50%) | 4 (44%) | 3 (75%) | 0 (0%) |
| AppleWatch | 4 (29%) | 2 (22%) | 2 (50%) | 0 (0%) |
| MyDiagnostick | 4 (29%) | 4 (44%) | 0 (0%) | 0 (0%) |
| Fibricheck | 10 (71%) | 8 (89%) | 2 (50%) | 0 (0%) |
| None | 1 (7%) | 0 (0%) | 0 (0%) | 1 (100%) |
| Other (Cube, hospital app) | 2 (14%) | 1 (11%) | 1 (25%) | 0 (0%) |
| Integrated in Electronic Patient System | 2 (14%) | 2 (22%) | 0 (0%) | 0 (0%) |
| Reimbursement | ||||
| Teleconsultation | 15 (65%); n = 23 | 6 (67%); n = 9 | 5 (71%) | 4 (57%) |
| Telemonitoring tools | 1 (5%); n = 20 | 0 (0%); n = 8 | 0 (0%) | 1 (20%); n = 5 |
Number provided after the semicolon indicates the total number of centres available for that variable.
AF, atrial fibrillation; AT, Austria; BE, Belgium; CIED, cardiac implantable electronic device; DE, Germany; DK, Denmark; ECV, electrical cardioversion; IE, Ireland; mHealth, mobile health; NL, The Netherlands; PL, Poland; SE, Sweden.
Overall, most centres were academic hospitals (64%) and the remaining (36%) were specialized public cardiology or district hospitals. This trend was consistent among most countries with the exception of Belgian centres, where specialized public cardiology hospitals made up 60% of all sites (Supplementary material online, Table S1). Most centres had specialized AF outpatient clinics (64%). Only 36% of centres had AF ablation clinics. Additionally, 40% of all centres, particularly in Group ‘2’ (71%), had implemented video consultations in their healthcare system.
More than half of the centres (56%), with 82% of them located in Group ‘1’, already had mHealth solutions (apps and devices) implemented in their healthcare system before the launch of the project. The main reason for use of mHealth solutions before the enrolment in the TeleCheck-AF project was remote AF control (heart rate and rhythm) and follow-up after AF ablation. Among six scenarios for mHealth usage (prior to/post consultation, prior to/post-electrical cardioversion/AF ablation, continuous usage, and on-demand usage), the most common was the period before planned consultations. Continuous mHealth usage occurred in the minority of centres. The type of mHealth devices used before the enrolment in the TeleCheck-AF project showed regional differences—FibriCheck® and MyDiagnostick® were preferred by Group ‘1’ and KardiaMobile by Group ‘2’. Group ‘3’ used remote monitoring by implantable loop recorders but did not use any of the above-mentioned mHealth devices.
Concerning reimbursement, 65% of centres declared that teleconsultations were reimbursed. However, only one single centre from UK reported that mHealth tool usage could be reimbursed, that could be explained by different funding models in particular regions of UK.
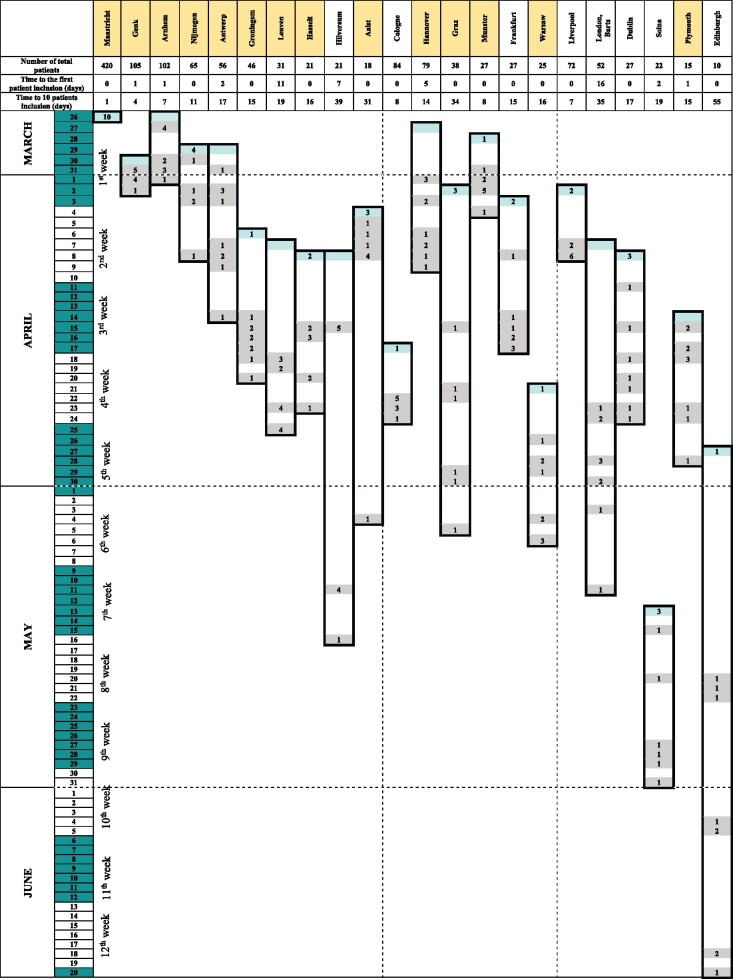
Timeline of centre activations in the TeleCheck-AF project
Distribution of centres by country and number of included patients per centre within 28 weeks is presented in Figure 1. The timeline from the centre activation to the first ten patients enrolment with a focus on centre experience with mHealth solutions is presented in Figure 2. Only centres which enrolled the largest number of patients are presented in the graph. The centres included in this analysis joined the TeleCheck-AF project within seven weeks of the project duration and 17 of them were participants from the very beginning of the study (from the first two weeks of project duration on). In most cases (82%), the time of centre enrolment correlated with the number of recruited patients per centre. However, there were no statistically significant differences between mHealth experienced and inexperienced centres according to median time required to 10th patient’s inclusion [15 (8–17) vs. 16 (9–27) days, P = 0.46], the first patient enrolment [0.5 (0–2) vs. 1 (0–12) days], P = 0.57) and median of included patients [42 (25–79) vs. 27 (22–62) patients, P = 0.42]. Time to first patient inclusion correlated with the number of physicians working in the AF outpatient clinic (rp=0.49, P = 0.02).
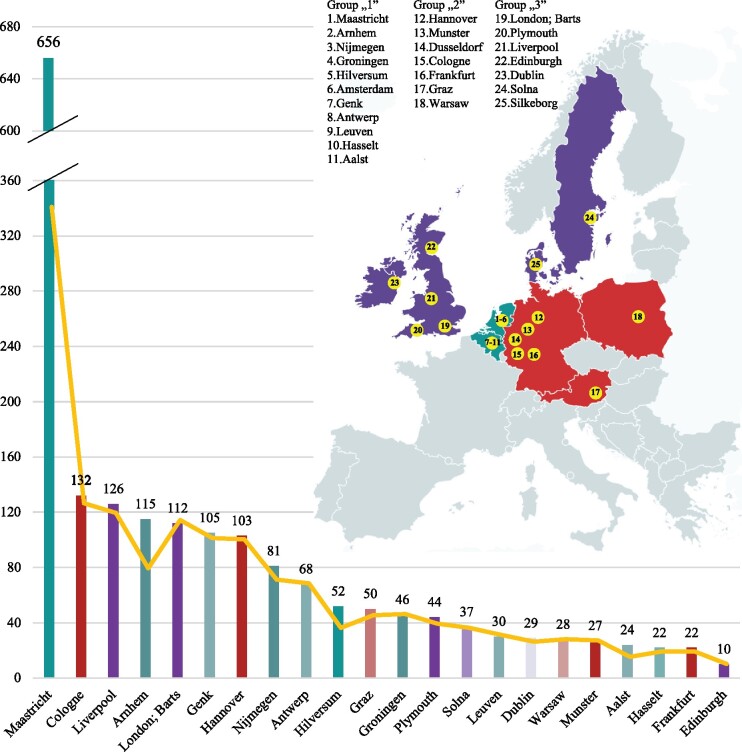
Figure 1.
Number of recruited patients per clinical centre and European geographical location of centres. Inclusion rates apply to centres that included ten or more patients. Columns showed number of recruited patients; yellow line showed the real number of patients that started heart rhythm and rate monitoring (status from 9 October 2020).
Figure 2.
Timeline from centre inclusion to first ten patients’ enrolment. Centres with previous experience with mHealth (yellow), dates of centre inclusion (blue), and days of patients’ enrolment (grey) are highlighted. The date of 26 March was chosen as start of the ‘first week’ as the first centre joined the project, beside Maastricht centre, and official date of TeleCheck-AF was announced at 4 April, therefore first week counts nine instead of seven days.
Timeline of patient inclusion in the TeleCheck-AF project
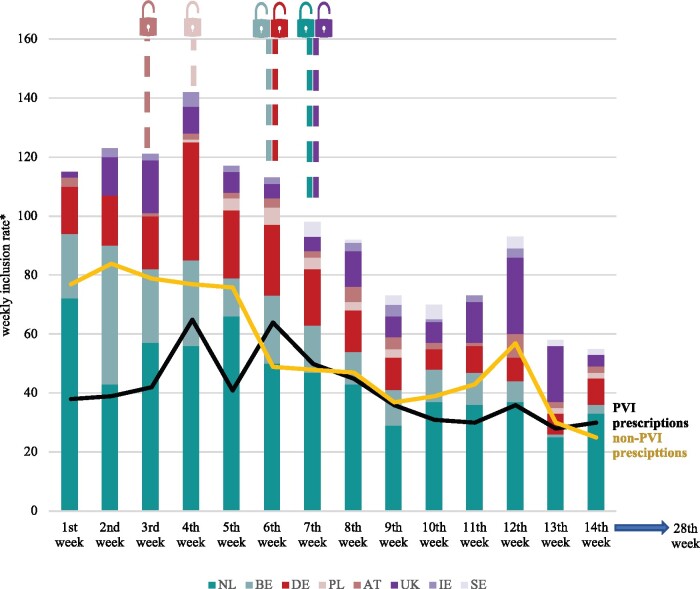
Within 28 weeks, 1930 AF patients were recruited within the TeleCheck-AF approach by included centres. Overall, the average inclusion rate was highest during the lockdown restrictions (until Week 7 of the project) and reached a steady state at a lower level after easing the restrictions (188 vs. 52 weekly recruited patients) (Figure 3).
Figure 3.
Weekly inclusion rate per country. *Weekly inclusion rate of the ‘first week’ was calculated for nine days instead of seven days. Inclusion rate was highest during the lockdown restrictions (n=829; 188 per week) lasting for 1st to 7th weeks and reached a steady state at a lower level after easing the restrictions (n=1101; 52 per week) lasting from 8th to 28th weeks (status from 9 October 2020). To simplify calculations, the border between the ‘lockdown’ and ‘easing the restrictions’ was chosen for the 7th week as it was the week in which the last country introduced the easing the restrictions. AT, Austria; BE, Belgium; DE, Germany; IE, Ireland; NL, The Netherlands; PL, Poland; PVI, pulmonary vein isolation; SE, Sweden.
Expected and observed FibriCheck® usage during the TeleCheck-AF project
At the initiation of the TeleCheck-AF project, centres were asked about the likelihood for mHealth usage during the COVID-19 pandemic. The usage of mHealth for follow-up of patients after AF ablation was expected to be most likely (44%) followed by the monitoring of heart rhythm control (20%), rate control (16%) and remote AF control (heart rate and rhythm) (12%). Risk assessment (8%) was not considered to be an important reason for mHealth usage during the COVID-19 pandemic. This trend was similar for all three groups of centres (Supplementary material online, Figure S5).
The survey-based expectations for mHealth use during the COVID-19 pandemic (i.e. follow-up of patients after AF ablation) are in line with the observed usage of the mHealth infrastructure. Within the TeleCheck-AF project, 575 (42%) patients were managed by FibriCheck® for heart rhythm monitoring around AF ablation procedure. Of note, 430 (31%) patients were monitored remotely by FibriCheck® within the TeleCheck-AF approach for remote AF control (heart rate and rhythm) around teleconsultations in AF outpatient clinics. Additional scenarios for the usage of FibriCheck® were heart rhythm monitoring around electrical cardioversion [119 patients (9%)] and assessment of AF-related symptoms [252 patients (18%)] (Supplementary material online, Figure S6).
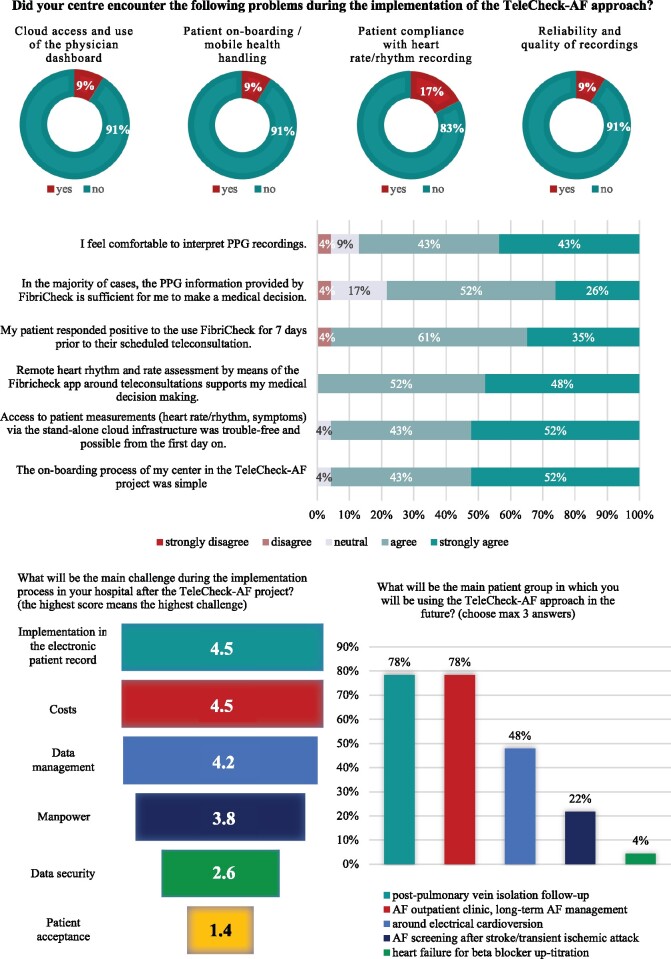
Centre experiences
From the 25 centres that completed the centre characteristics survey, 23 centres across nine countries also completed the centre experience survey. The majority (>80%) of centres reported no problems (concerning cloud access, patient compliance, or quality of recordings) during the initial implementation of the TeleCheck-AF approach. Centres agreed that the on-boarding process of their centre in the TeleCheck-AF project was simple and access to the patients measurements via stand-alone cloud infrastructure was trouble-free and possible from the first day on. They also agreed that remote heart rate and rhythm assessment by the FibriCheck® app around teleconsulatation supported their medical decision making; that their patients responded positively to use FibriCheck® for seven days; and that they felt comfortable to interpret PPG recordings. In their opinion, the main challenges during the permanent introduction of such a mHeath solution after the TeleCheck-AF project will be implementation of mHealth data in the electronic patient record followed by costs and data management. Most centres predict that mHealth approaches such as TeleCheck-AF will be used for follow-up after AF ablation and management of patients referred to AF outpatient clinics in the future. The results of the centre experience survey are presented in Figure 4.
Figure 4.
Centre experiences (n = 23). AF, atrial fibrillation; PPG, photoplethysmography.
Patient characteristics
Overall, 1480 (77% of recruited patients) started heart rate and rhythm monitoring. One-third of patients was in the age range 60–69 years (Supplementary material online, Figure S7) and this trend was consistent among most countries. The most common encountered comorbidity was hypertension (42% of all patients). More than 70% of patients were treated with oral anticoagulation with the higher rate within Group ‘2’, which was also characterized by the highest AF knowledge rate (91% of patients).
In total, 59.858 heart rate and rhythm measurements were recorded by 1480 patients. The highest average number of measurements per patient was seen within the age range ≥80years. In the vast majority (82%), only one heart rate and rhythm measurement was needed to receive good quality recording. During the 1-week FibriCheck® use, patient adherence was high. Patients performed between two and five recordings a day and the median number of measurements per patient was 21 (15–29) (Table 2).
| Total (n = 1480) | Group ‘1’ (n = 796) | Group ‘2’ (n = 346) | Group ‘3’ (n = 338) | |
|---|---|---|---|---|
| NL and BE | DE, AT, and PL | UK, IL, DK, and SE | ||
| Demographics | ||||
| Percentage men | 915 (62%) | 476 (60%) | 206 (60%) | 233 (69%) |
| Age (median) | 64 (55–71) | 65 (57–72) | 62 (54–72) | 64 (54–70) |
| Age | ||||
| <30 | 506 (2%) | 60 (2%) | 94 (2%) | 352 (2%) |
| 30–39 | 1456 (5%) | 236 (4%) | 333 (6%) | 887 (5%) |
| 40–49 | 3565 (8%) | 518 (7%) | 880 (11%) | 2167 (9%) |
| 50–59 | 13 148 (21%) | 1659 (18%) | 2086 (23%) | 9403 (25%) |
| 60–69 | 21 351 (33%) | 2466 (34%) | 3940 (31%) | 14 945 (33%) |
| 70–79 | 16 810 (27%) | 2013 (29%) | 2059 (22%) | 12 738 (25%) |
| >80 | 3023 (4%) | 106 (5%) | 581 (4%) | 2336 (2%) |
| Age of oldest participant | 92 | 92 | 85 | 86 |
| Medical history | ||||
| Pacemaker |
64 (5%) n = 1386 |
21 (3%) n = 751 |
15 (5%) n = 328 |
18 (6%) n = 307 |
| Heart failure |
248 (18%) n = 1385 |
198 (26%) n = 749 |
18 (6%) n = 329 |
32 (10%) n = 307 |
| Coronary artery disease |
175 (13%) n = 1387 |
79 (11%) n = 752 |
56 (17%) n = 328 |
40 (13%) n = 307 |
| Hypertension |
581 (42%) n = 1388 |
293 (39%) n = 752 |
181 (55%) n = 328 |
107 (35%) n = 308 |
| Diabetes |
135 (10%) n = 1388 |
79 (11%) n = 751 |
24 (7%) n = 329 |
32 (10%) n = 308 |
| Treatment with oral anticoagulants |
1017 (73%) n = 1400 |
548 (72%) n = 766 |
252 (77%) n = 328 |
217 (71%) n = 306 |
| Heart rhythm and rate recordings | ||||
| Average number of measurements per patient | 40 | 54 | 28 | 21 |
| Median number of measurements per patient | 21 | 22 | 21 | 18 |
| Average number of measurements per age | ||||
| <30 | 15 | 19 | 12 | 10 |
| 30–39 | 20 | 25 | 15 | 14 |
| 40–49 | 29 | 40 | 24 | 17 |
| 50–59 | 43 | 66 | 26 | 20 |
| 60–69 | 43 | 55 | 36 | 22 |
| 70–79 | 43 | 55 | 27 | 24 |
| >80 | 49 | 57 | 39 | 18 |
| Number of attempts of measurements | ||||
| 1 | 49 319 (82%) | 34 962 (56%) | 8100 (81%) | 5930 (84%) |
| 2 | 3291 (6%) | 23 301 (37%) | 491 (5%) | 437 (6%) |
| >3 | 1340 (2%) | 937 (2%) | 172 (2%) | 198 (3%) |
| NA/0 | 5908 (10%) | 4095 (7%) | 1210 (12%) | 492 (7%) |
AT, Austria; BE, Belgium; DE, Germany; DK, Denmark; IE, Ireland; NA, no applicable; NL, The Netherlands; PL, Poland; SE, Sweden.
More than half of the recordings showed sinus rhythm (54%) followed by AF (28%), extrasystoles (7.2%) and other rhythms, e.g. bradycardia or tachycardia (2.8%). The most common AF-related symptom was palpitations (10%). Noteworthy, more than half of the patients (54%) with a PPG-detected AF episode by FibriCheck® were asymptomatic (Supplementary material online, Figure S8). Just 65% of all symptom-triggered events were associated with PPG recordings suggestive for AF (Supplementary material online, Figure S9).
The patient characteristics of all centres and stratified per country group are present in Table 2 and characteristics per country are present in Supplementary material online, Table S2.
Patient experiences
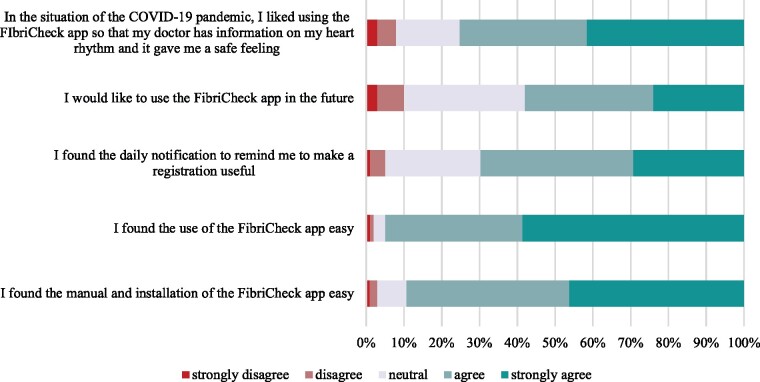
Patients agreed that the FibriCheck® app was easy to use (94%) and easy to install (89%). The app gave patients a safe feeling (74%) due to being in constant heart rate and rhythm control. More than half of the patients (58%) agreed or strongly agreed that they would like to use the FibriCheck® app in the future. They also found the automated reminders useful (64%). The results of the patient experience survey are present in Figure 5.
Figure 5.
Patient experiences (n = 826).
Discussion
The TeleCheck-AF project was officially announced early April 2020 and made mHealth-supported teleconsultations widely available in European centres aiming to maintain AF care during the COVID-19 pandemic, whilst keeping patients out of hospital.5,10,12 During the initial two weeks the infrastructure was implemented in 17 centres from six different countries. Currently, 37 international centres from 13 different countries are participating in this European mHealth project.
The novel component of the TeleCheck-AF approach is the on-demand mHealth infrastructure, incorporating the app-based remote collection of heart rate and rhythm information for one week prior to a scheduled teleconsultation.6 This is a short-term on-demand mHealth approach (prescribed seven days prior to teleconsultation) that prevents unnecessary data overload requiring work-intensive and expensive data management infrastructures. Dealing with amounts of unnecessary information coming from mHealth technology was recently identified as one major hurdle for mHealth implementation in the wEHRAbles survey conducted in a total of 417 physicians from 42 countries.13 Additionally, information about strategies to educate and empower patients to self-manage the on-demand mHealth application and the required care coordination, including implementation of the approach in clinical practice, were provided.8 The standardized instruction for all participating centres through an initiation call with a simultaneous discussion of the TeleCheck-AF project rationale appeared to facilitate the mHealth usage in the included centres.
Despite the standardized instruction of all centres, the temporal enrolment pattern of patients varied in the different country groups. Factors such as experiences with mHealth solutions, older software systems in some hospital sites and the indication and motivation to perform heart rate and rhythm monitoring (e.g. long-term AF management in AF outpatient clinics vs. follow-up after AF ablation) may have contributed to this observation. Additionally, the dynamics in the COVID-19 pandemic may have impacted the use of the TeleCheck-AF approach. Accordingly, inclusion rates were highest during the lockdown restrictions (until Week 7) and reached a steady state at a lower level after easing the restrictions. One important additional factor in patient inclusion rates is the level of mHealth experience before COVID-19, and even more specifically, experience with PPG-based technology, in each centre. The countries in group ‘1’ (Belgium and The Netherlands) had the highest rate of mHealth integration (including FibriCheck® in 89% of centres) in their healthcare system and already enrolled their first patients in the week of program inclusion. However, some countries in Group ‘2’ (Austria, Germany, and Poland) and Group ‘3’ (Denmark, Ireland, Sweden, and UK) without having previously dealt with mHealth tools/applications included more patients than centres that were enrolled earlier in the project. The material provided at the initiation of a new centre and the stand-alone cloud-based mHealth infrastructure of the TeleCheck-AF approach without the need of installation of programs on computers or complete implementation in the electronic health record system may explain the accelerated implementation of the TeleCheck-AF infrastructure despite the absence of existing mHealth infrastructures and the lack in mHealth experience. In addition to differences in centre mHealth experience, also differences in patient mHealth experience might have impacted the implementation process of the TeleCheck-AF approach. However, this needs to be investigated in future prospective studies. Overall, patients agreed that the FibriCheck® app was easy to use.
The COVID-19 pandemic is not over yet,14 and the continuing need for social distancing still puts restrictions on the numbers of patients visiting the hospital and consequently face to face consultations. Implementation of mHealth infrastructures for remote heart rate and rhythm monitoring, such as TeleCheck-AF, even in countries beyond Europe, may contribute to managing the potentially increased number of patients presenting with AF episodes during the COVD-19 pandemic.15 However, despite the potential impact of COVID-19 on AF arrhythmogenesis,16 a Danish nationwide registry reported a decrease in new-onset AF by 47%, but a 41% increase in ischaemic stroke or all-cause death during the first three weeks of the national lockdown compared with the same period in the previous year.17 Patients with first symptoms of AF may have delayed or refused care as they were afraid to contact medical services due to the potential contamination. Whether implementation of an infrastructure allowing remote AF monitoring through a mHealth app and using teleconsultation, such as the TeleCheck-AF approach, may potentially prevent this patient preventive behaviour, however this warrants further investigation.
A PPG-based mHealth solution has advantages and limitations. PPG-based mHealth-solutions can discriminate slow from fast rhythms and regular from irregular. The wide accessibility and low cost of this technology that needs nothing more than a smartphone makes it an interesting tool for remote heart rate and rhythm monitoring. Although PPG technology is nearly as accurate as ECG to detect AF,18 the diagnosis of AF still requires an ECG documentation of the arrhythmia.1 Therefore, FibriCheck in the TeleCheck-AF approach is mainly used to remotely detect AF episodes and assess heart rates in patients who have been diagnosed for AF by ECG before. Additionally, FibriCheck® also represents a good tool to test for symptom-rhythm correlation. In TeleCheck-AF, more than half of the patients with a PPG detected AF episode by FibriCheck® were asymptomatic and just 65.4% of all symptom-triggered events were associated with PPG recordings suggestive for AF. In general, the TeleCheck-AF approach could be also performed by using ECG-based mHealth solutions instead of PPG-based apps to overcome some of the above mentioned limitations in specific patients requiring for example remote QRS width or QT-interval monitoring during antiarrhythmic drug treatment.
Perspectives and challenges
We showed that the TeleCheck-AF mHealth infrastructure could be set-up within a short time frame during the COVID-19 pandemic. Participating European cardiology centres and recruited patients could easily use the infrastructure and consider the TeleCheck-AF approach as an alternative to face-to-face consultations in the future. Additionally, higher age is no obstacle for mHealth use. One-third of patients was in the age range 60–69 years and the highest average number of measurements per patient was performed by patients older than 80 years of age.
However, several remaining challenges need to be addressed, before mHealth infrastructures such as TeleCheck-AF can be implemented in clinical care. The implementation in electronic patient records and reimbursement were identified as the main barrier to a more widespread adoption of mHealth solutions in healthcare systems by centres participating in the TeleCheck-AF project. Without financial support provided by government or private insurances, mHealth apps or devices will be limited to those patients who may be willing to pay out-of-pocket for access to telemedicine solutions.19 Additionally, due to the current fee for service model in some countries, reducing clinical face-to-face appointments and hospitalizations may not be in the best interest of physicians. This may prevent healthcare innovations in the field of remote AF management and telemedicine. Also other mHealth infrastructures for AF management, which may similarly support the remote care of AF patients, are available.20 However, TeleCheck-AF is the only mHealth approach which has been proven feasible to be set up within a short period of time (e.g. number of days/weeks) during the global COVID-19 pandemic. Until now, no outcome data for the TeleCheck-AF approach is available yet. The standardized inclusion and instruction of centres in TeleCheck-AF allow further retrospective analysis to obtain a real-world picture of AF care through the TeleCheck-AF approach during the COVID-19 pandemic.
Conclusions
Despite different existing infrastructures, mHealth experiences and motivation to use mHealth, the TeleCheck-AF approach using FibriCheck® was set up in a short time frame and was actively used in numerous European cardiology centres during the COVID-19 pandemic, and beyond. FibriCheck® was easy to use and easy to install by patients and supported the assessment of rate and rhythm around teleconsultation. A detailed retrospective analysis of the data collected within the TeleCheck-AF project is currently performed and used to guide discussions concerning reimbursement with insurances. Additionally, the retrospective analysis allows an informed preparation of the TeleCheck-AF Study: a prospective randomized trial to assess whether mHealth-supported teleconsultation is non-inferior to current standard AF care guided by face-to-face consultations.
Supplementary material
Supplementary material is available at Europace online.
Supplementary Material
Acknowledgements
The mHealth infrastructure was provided for free within the TeleCheck-AF project by the MUMC+ and additionally supported by FibriCheck® and Biosense Webster®.
Conflict of interest: J.M.H. was supported by a Future Leader Fellowship provided by the National Heart Foundation of Australia. D.D. received lecture honorary, travel grants, and/or a fellowship grant from Abbott, Astra Zeneca, Bayer, Biotronik, Boehringer Ingelheim, Boston Scientific, Medtronic, Microport, Pfizer, and Zoll. M.M. has received speaker honoraria and/or travel grants from Biosense Webster, Abbott, Biotronik, Zoll, Boston Scientific, Daiichi Sankyo, Bayer, Amomed, Pfizer and research grants from Biosense Webster. H.H. has no personal honararia constituting a conflict of interest. His institutions received a COVID-19 Innovation Prize by the city of Antwerp for the rapid implementation of teleconsultations, including FibriCheck, for AF patients, and have institutional clinical investigator contracts with Qompium (the company providing Fibricheck). P.L. has received a speaker honorarium from Bayer, Boehringer Ingelheim, and Pfizer. D.L. has no personal honararia constituting a conflict of interest. His institutions received support by the Netherlands Enterprise Agency for the implementation of teleconsultations supported by a remote heart rate and rhythm monitoring, including FibriCheck, for AF patients. The University of Maastricht has received on his behalf lecture and/or consulting fees and/or research grants from Bayer, Biosense-Webster, Medtronic, LivaNova, RespiCardia, Medtronic, and ResMed. The other authors have no conflict of interest to declare.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1.Nieuwlaat R, Prins MH, Le Heuzey JY, Vardas PE, Aliot E, Santini M. et al. Prognosis, disease progression, and treatment of atrial fibrillation patients during 1 year: follow-up of the Euro Heart Survey on atrial fibrillation. Eur Heart J 2008;29:1181–9. [DOI] [PubMed] [Google Scholar]
- 2.Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J 2021;42:373–498. [DOI] [PubMed] [Google Scholar]
- 3.Varma N, Marrouche NF, Aguinaga L, Albert CM, Arbelo E, Choi JI. et al. HRS/EHRA/APHRS/LAHRS/ACC/AHA worldwide practice update for telehealth and arrhythmia monitoring during and after a pandemic. Europace 2021;23:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hermans ANL, Velden RMJ, Gawalko M, Verhaert DVM, Desteghe L, Duncker D. et al. ; TeleCheck‐AF investigators. On-demand mobile health infrastructures to allow comprehensive remote atrial fibrillation and risk factor management through teleconsultation. Clin Cardiol 2020;43:1232–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pluymaekers N, Hermans ANL, van der Velden RMJ, den Uijl DW, Vorstermans B, Buskes S. et al. On-demand app-based rate and rhythm monitoring to manage atrial fibrillation through tele-consultations during COVID-19. Int J Cardiol Heart Vasc 2020;28:100533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pluymaekers N, Hermans ANL, van der Velden RMJ, Gawalko M, den Uijl DW, Buskes S. et al. Implementation of an on-demand app-based heart rate and rhythm monitoring infrastructure for the management of atrial fibrillation through teleconsultation: TeleCheck-AF. Europace 2021;23:345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Sullivan JW, Grigg S, Crawford W, Turakhia MP, Perez M, Ingelsson E. et al. Accuracy of smartphone camera applications for detecting atrial fibrillation: a systematic review and meta-analysis. JAMA Netw Open 2020;3:e202064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Velden RMJ, Hermans ANL, Pluymaekers NAHA, Gawałko M, Vorstermans B, Martens H. et al. Coordination of a remote mHealth infrastructure for atrial fibrillation management during COVID-19 and beyond: teleCheck-AF. Int J Care Coord 2020;23:65–70. [Google Scholar]
- 9.Hendriks JL, Nieuwlaat R, Vrijhoef HJ, de Wit R, Crijns HJ, Tieleman RG.. Improving guideline adherence in the treatment of atrial fibrillation by implementing an integrated chronic care program. Neth Heart J 2010;18:471–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.m-Health: Apps to the Rescue – Maastricht, The Netherlands. https://www.escardio.org/Education/COVID-19-and-Cardiology/m-health-apps-to-the-rescue-maastricht-the-netherlands (15 August 2020, date last accessed).
- 11.Hendriks JML, Tieleman RG, Vrijhoef HJM, Wijtvliet P, Gallagher C, Prins MH. et al. Integrated specialized atrial fibrillation clinics reduce all-cause mortality: post hoc analysis of a randomized clinical trial. Europace 2019;21:1785–92. [DOI] [PubMed] [Google Scholar]
- 12.Linz D, Pluymaekers N, Hendriks JM.. TeleCheck-AF for COVID-19. Eur Heart J 2020;41:1954–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manninger M, Kosiuk J, Zweiker D, Njeim M, Antolic B, Kircanski B. et al. Role of wearable rhythm recordings in clinical decision making-The wEHRAbles project. Clin Cardiol 2020;43:1032–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coronavirus disease (COVID-19). Situation Report – 189. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200727-covid-19-sitrep-189.pdf?sfvrsn=b93a6913_2 (27 July 2020, date last accessed).
- 15.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G. et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020;75:2352–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gawałko M, Kapłon-Cieślicka A, Hohl M, Dobrev D, Linz D.. COVID-19 associated atrial fibrillation: incidence, putative mechanisms and potential clinical implications. Int J Cardiol Heart Vasc 2020;30:100631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holt A, Gislason GH, Schou M, Zareini B, Biering-Sorensen T, Phelps M.. New-onset atrial fibrillation: incidence, characteristics, and related events following a national COVID-19 lockdown of 5.6 million people. Eur Heart J 2020;41:3072–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan PH, Wong CK, Poh YC, Pun L, Leung WW, Wong YF. et al. Diagnostic performance of a smartphone-based photoplethysmographic application for atrial fibrillation screening in a primary care setting. J Am Heart Assoc 2016;5:e003428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M.. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018;24:4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W. et al. Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol 2020;75:1523–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.