Abstract
The COVID-19 pandemic has forced endocrinologists to utilize telemedicine to care for their patients. There is limited information on the experience of endocrinologists in managing patients with thyroid cancer virtually. We sent a 9-item questionnaire to endocrinologists and endocrine surgeons at our institution to better understand the barriers and benefits of caring for patients with thyroid cancer via telemedicine, as well as how we can incorporate telemedicine into our future care of patients with this malignancy. Among the 9 physicians who responded, the majority listed technological issues with the virtual platform as a challenge in caring for patients with thyroid cancer remotely. Additional barriers included difficulty in expressing empathy, decreased ability to coordinate care with the interdisciplinary team, and lack of the physical examination. Benefits included compliance with social distancing measures and convenience for patients with American Thyroid Association (ATA) low-risk thyroid cancer who presented for follow-up visits. Overall, physicians were satisfied or strongly satisfied with caring for patients with thyroid cancer remotely, especially low-risk patients on long-term follow-up. That said, they recommend that some patients be seen in person after the pandemic, including symptomatic patients and ATA high-risk patients. While the COVID-19 pandemic has allowed endocrinologists to manage patients with thyroid cancer remotely, the providers have faced challenges, some of which can be improved upon. Further studies will help determine how telemedicine affects patient outcomes, including satisfaction, disease progression, and survival, which will inform how we may incorporate this practice into our future care of patients with thyroid cancer.
Keywords: well-differentiated thyroid cancer, medullary thyroid cancer, telemedicine, COVID-19
The COVID-19 pandemic has forced all healthcare providers to be adaptive and innovative in their care for their patients so as to maintain adequate social distancing and limit the spread of the SARS-CoV-2 virus. Endocrinologists have embraced telemedicine during this time, both in the outpatient and inpatient setting. In April 2020, just weeks after the first stay-at-home orders were issued in the United States, Madduri et al administered a web-based survey to US endocrinologists who were members of the Facebook group “Endocrinologists” [1]. Of the 181 endocrinologists who responded, almost half of the providers were doing their outpatient visits fully remotely, the majority were doing a mix of telemedicine and in-person visits, and there was only 1 provider who was still seeing outpatients fully in an office setting. This trend toward telemedicine, or a hybrid of telemedicine and in-person visits, continued throughout the summer and into the fall of 2020.
While the experiences of healthcare providers adjusting to telemedicine during the pandemic have been reported, there is limited information on the unique experience of caring for patients with thyroid cancer remotely. Some patients with an underlying malignancy represent a vulnerable population given their immunocompromised state and the fact that they may be on immunosuppressive therapy. In terms of caring for patients with cancer during the pandemic, Tsamakis et al aptly stated in their review paper, “… the cancer community is steering a difficult course amid several challenges: revisiting optimal standards of cancer care, facing persistently evolving shortages, and acknowledging the paradoxical need to keep patients away from healthcare facilities” [2].
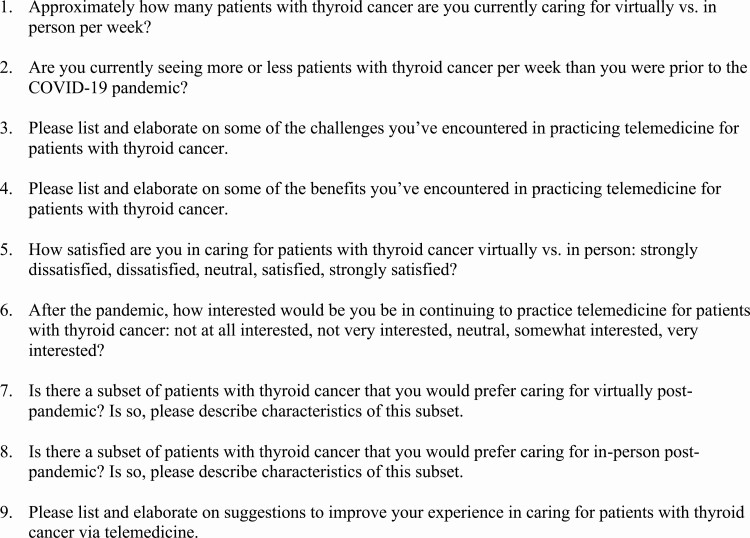
After gaining approval from the Endocrine Service at Memorial Sloan Kettering Cancer Center (MSKCC), we sent an original 9-item questionnaire via e-mail to physicians at our institution who have been caring for patients with thyroid cancer via telemedicine during the pandemic (Fig. 1). Of the 20 physicians who received the questionnaire, 9 providers completed and returned it within the allotted 2-week timeframe in September 2020, all of whom were endocrinologists or endocrine surgeons. The responses to the questionnaire remained anonymous, and no incentive was provided for completion of the survey. Although the questionnaire was specifically focused on the experience of caring for patients with thyroid cancer virtually, several of the providers at MSKCC have interacted with patients both on video and by phone, and their responses to the questionnaire represent this fact. Through our personal experiences, as well as analysis of the questionnaires, we present some of the barriers and benefits of managing patients with thyroid cancer via telemedicine, as well as suggestions about how we may better incorporate telemedicine into our future care for patients with this malignancy.
Figure 1.
Questionnaire sent to physicians who care for patients with thyroid cancer at MSKCC.
While most endocrinologists at MSKCC are solely seeing patients with thyroid cancer remotely, the endocrine surgeons are still seeing a significant number of patients with thyroid cancer in person. Furthermore, while some endocrinologists are actually seeing the same number or more patients with thyroid cancer than they were prior to the pandemic, the endocrine surgeons are seeing fewer patients with this condition overall. The increase in patient volume for endocrinologists may be attributed to easier access as well as increased needs and limited staffing at regional medical centers. The decrease in patient volume for endocrine surgeons may be due to postponement of elective procedures, including thyroidectomies, on behalf of the hospital so as to limit inpatient traffic, and on behalf of the patient so as to restrict exposure to healthcare settings. In fact, investigators at the University of Buenos Aires observed an over 98% decrease in the number of procedures performed for thyroid cancer at their hospital over a span of 100 days during their quarantine, including fine needle aspirations, thyroidectomies, lymph node dissections, and resection of brain metastases [3].
When asked about the challenges in caring for patients with thyroid cancer via telemedicine, almost all of the providers at our institution touched upon technological issues. They specifically discussed the inability to complete visits due to poor internet connection or confusion regarding the virtual interface, requiring conversion of the video visit into a telephone encounter or rescheduling of the visit altogether. They also described that while the physician has allotted time to conduct the visit and be present with the patient, the patient may be multitasking during the visit, doing activities such as commuting or shopping for groceries, leading to further connectivity issues as well as distractions and potential breaches of privacy. This can hinder the physician from gathering all of the necessary information to make sound clinical decisions and communicate them effectively to the patient.
An additional technological challenge that the providers noted is the lack of a waiting room, wherein it becomes difficult for a physician to fit a patient into their schedule if the patient “arrived” late or to update a patient if they are behind in their schedule. In his article entitled “Virtual Endocrinology: The Rise of Telehealth During COVID-19,” Derek Bagley describes how the University of Pennsylvania created an interface in which patients can log onto a virtual waiting room, which helps to rectify these issues [4]. Such developments suggest that some of the aforementioned barriers are not intrinsic to telemedicine, but rather, can be improved upon by technological advances.
While these technological challenges have been faced by several groups of providers practicing telemedicine during the pandemic, they become exacerbated when communicating difficult news regarding a new diagnosis of thyroid cancer, progression of disease, or failure of therapy, such as radioactive iodine or radiation. When conveying such sensitive information, it is paramount for the provider to be present for the patient to answer any questions they may have about next steps, provide empathy, or just remain silent as the patient is processing this new and potentially devastating information. In their responses to the questionnaire, 3 of the endocrinologists at our institution specifically stated that they had difficulty connecting with patients on an emotional level on video; these providers listed reasons that included the loss of the human touch, decreased ability to read body language, and miscommunication, the latter of which occurred more frequently with patients whose primary language was not English, requiring the assistance of a virtual translator.
Not only do providers find it difficult to connect with patients using telemedicine, but also with other members of the interdisciplinary thyroid cancer team. Both endocrinologists and endocrine surgeons explained that they previously worked closely with other physicians, nurses, session assistants, and social workers during the patient’s visit so as to provide comprehensive care. With virtual visits, it is not as easy to communicate with one another, wherein care can feel fragmented. For example, it takes additional steps to seek the assistance of Nursing for patient education on certain topics, including the dietary guidelines of radioactive iodine therapy. This disjointed care has also made seemingly simple tasks, such as scheduling follow-up appointments, more complicated.
Providers also commented on the change in insurance coverage and reimbursement for visits. As MSKCC is one of the nation’s premier institutions for thyroid cancer, physicians see patients from across the nation and world. However, most insurers, including the Centers for Medicare & Medicaid Services (CMS), mandate that virtual visits be conducted with patients who reside in a state where the provider is licensed or there is no license requirement, which limits the geographic scope of patients who can participate in telemedicine. Billing has also been affected by the transition to telemedicine. For example, if the physician is conducting the virtual visit off-site, the hospital can only bill a professional fee and not the additional facility fee. However, if the physician is conducting the virtual visit on-site, the hospital can charge both professional and facility fees. These policies have affected the financial health of hospitals and clinics alike.
The final, and arguably most important, barrier to caring for patients with thyroid cancer virtually is the inability to perform a physical examination. To start, vital signs provide useful information for patients with thyroid cancer, specifically those with postoperative hypothyroidism secondary to a thyroidectomy. If a patient has gained or lost weight, or if a patient is tachycardic, this may suggest that their dose of thyroid hormone therapy requires adjustment. Furthermore, if a patient is experiencing neck pain, neck fullness, or new lumps on their neck, it is impossible for the endocrinologist to palpate this region of their body to further elucidate these symptoms, and instead, they have to rely entirely on imaging studies. The endocrine surgeons specifically lamented the inability to perform a laryngoscopy if a patient is complaining of hoarseness, wherein they have to see the patient in their office shortly thereafter, undermining the utility of the virtual visit.
In her article entitled “The Importance of Medical Touch,” Caitlin Kelly, who had been diagnosed with ductal carcinoma in situ, discusses the therapeutic role of the human touch. She relates that gentle physical contact during her medical visits helped to calm her nerves and alleviate her anxiety surrounding her diagnosis [5]. She quotes Abraham Verghese, MD, a professor at Stanford University School of Medicine, who, in his TED Talk in 2011, stated, “When we shorten the physical exam, we’re losing a ritual that I believe is transformative, transcendent, and at the heart of the physician patient relationship” [6].
Despite these challenges, there are several benefits to caring for patients with thyroid cancer virtually during the pandemic, safety being first and foremost. As patients with malignancies are at higher risk for developing serious complications from COVID-19, the endocrinologists and endocrine surgeons expressed relief in knowing that they were limiting their patients’ likelihood of contracting the SARS-CoV-2 virus by enabling them to follow stay-at-home orders. They especially underscored the advantage this presented to patients who live far from the hospital, including abroad, and those who depend on public transportation to commute to MSKCC. They noted that an added benefit of telemedicine is that some patients feel less anxious than they normally do, and that others are relieved to include family members in the visit who may have previously been at work during their appointments.
Another advantage that the providers at MSKCC experienced was convenience. They described that for low-risk, asymptomatic patients who had already undergone labs and imaging at an outside institution, the virtual visit was relatively straightforward. Insofar as there were no distractions or technological glitches, providers were able to gain additional information they needed from the encounter itself and did not feel that the visit was lacking. In fact, when asked about their overall satisfaction with telemedicine for patients with thyroid cancer on a 5-point Likert scale ranging from strongly dissatisfied to strongly satisfied, providers were generally satisfied or strongly satisfied, specifically when caring for low-risk patients on long-term follow-up. Furthermore, when asked about their interest in continuing to practice telemedicine after the pandemic on a 5-point Likert scale ranging from not at all interested to very interested, most providers stated they were somewhat interested or very interested, with only 1 provider stating they were not at all interested.
As it relates to the future of telemedicine, Seema Verma, the administrator for CMS, stated the following in a blog post, “With these transformative changes unleashed over the last several months, it’s hard to imagine merely reverting to the way things were before,” suggesting that virtual care is likely here to stay, even after the pandemic [7]. In order to better understand how telemedicine may benefit patients with thyroid cancer after the pandemic, it is important to investigate how virtual visits affect outcomes including progression of disease, disease recurrence, and death, as well as overall patient satisfaction. These findings will help determine the patient population that would be best supported by virtual services in the future.
When providers at MSKCC were asked about the population that would benefit most from telemedicine post-pandemic, they stated patients with well-differentiated thyroid cancer (DTC) or medullary thyroid cancer (MTC) who are ATA low-risk or intermediate-risk with excellent response to therapy, patients who live far from MSKCC, including international patients, and finally, patients who prefer to be seen remotely, as virtual care may enhance their compliance with visits.
In terms of patients with thyroid cancer who would be better cared for in person after the pandemic, providers at our institution stated symptomatic patients, new patients, patients on clinical trials, patients with DTC or MTC who are ATA intermediate-risk with incomplete response to therapy or progressive disease, patients with DTC or MTC who are ATA high-risk, individuals who lack technological skills or adequate internet service, and finally, those who would prefer to be seen in person. We have summarized the characteristics of patients with thyroid cancer who would benefit from being seen via telemedicine versus in person in Table 1.
Table 1.
Characteristics of patients with thyroid cancer who would benefit from telemedicine versus in-person visits post-pandemic
| Telemedicine visits | In-person visits |
|---|---|
| Patients with DTC or MTC who are ATA low-risk or intermediate-risk with excellent response to therapy; patients who live far from the hospital, including international patients; patient preference |
Symptomatic patients; new patients; patients on clinical trials; patients with DTC or MTC who are ATA intermediate-risk with incomplete response to therapy or progressive disease; patients with DTC or MTC who are ATA high-risk; patients who lack technological skills or adequate internet service; patient preference |
Abbreviations: ATA, American Thyroid Association; DTC, well-differentiated thyroid cancer; MTC, medullary thyroid cancer.
In a review article on the potential challenges in caring for patients with any malignancy during the COVID-19 pandemic, the investigators discussed the role of telemedicine [8]. They stated that cancer patients who have previously benefited from telemedicine include those who are not on active therapy as well as those who are receiving palliative care or survivorship care. This aligned with the feedback from the physicians at MSKCC, who indicated that patients with thyroid cancer who are not on active therapy (eg, patients with DTC or MTC who are ATA low-risk with excellent response to therapy) could be cared for adequately via telemedicine. In the aforementioned study, the authors also listed limitations to caring for patients with cancer virtually during the pandemic, including the legal boundaries of telemedicine, limited training on telemedicine tools, the lack of the physical exam, and issues relating to reimbursement, all of which were barriers that the endocrinologists and endocrine surgeons mentioned in our correspondence with them.
The final topic that we covered in our questionnaire was potential changes that would enhance the providers’ experiences with telemedicine moving forward. When asked about this subject, most of the physicians discussed the virtual platform. Several suggested updating the interface to include a virtual waiting room, similar to the platform used by providers at the University of Pennsylvania, so as to maximize the number of patients that can be seen and allow for better communication with patients throughout the day [4]. They also recommended a feature to enable screen sharing so they could walk their patients through their laboratory and imaging findings. Additionally, they proposed new functionality that would enable physicians and nurses to collaborate on issues including pre-visit assessments and post-visit education. Finally, they hoped insurers would loosen restrictions that hinder patients from being seen virtually so as to promote healthcare access for all.
The pandemic has necessitated that providers and patients adapt to telemedicine in an effort to flatten the curve and decrease the spread of SARS-CoV-2. A favorable outcome of this change is that physicians have a new way of delivering care, one that will continue to benefit a subset of our population in years to come. We look forward to conducting and reviewing outcomes-based research, building upon our technology, negotiating with policy makers, and considering the experiences of all individuals so as to best incorporate telemedicine into our future care of patients with thyroid cancer and beyond.
Acknowledgments
Sources of funding: None.
Glossary
Abbreviations
- DTC
well-differentiated thyroid cancer
- MSKCC
Memorial Sloan Kettering Cancer Center
- MTC
medullary thyroid cancer
Additional Information
Disclosures: The authors have nothing to disclose.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1. Madduri S, Chowdhary R, Sethu Reddy S. Telehealth Adoption Among Endocrinologists During the Covid-19 Pandemic. Endocr Pract. 2020;26(8):846-856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tsamakis K, Gavriatopoulou M, Schizas D, et al. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett. 2020;20(1):441-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smulever A, Abelleira E, Bueno F, Pitoia F. Thyroid cancer in the Era of COVID-19. Endocrine. 2020;70(1):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bagley D. Virtual endocrinology: the rise of telehealth during COVID-19. Endocrine News. July 2020. Accessed October 2, 2020. https://endocrinenews.endocrine.org/virtual-endocrinology-the-rise-of-telemedicine-during-covid-19/ [Google Scholar]
- 5. Kelly C. The importance of medical touch.New York Times. October 8, 2018. Accessed October 25, 2020. https://www.nytimes.com/2018/10/08/well/live/the-importance-of-medical-touch.html [Google Scholar]
- 6. Verghese A. A doctor’s touch. Presented at TEDGlobal2011; September 27, 2011; Edinburgh, Scotland. Accessed October 20, 2020. https://www.ted.com/talks/abraham_verghese_a_doctor_s_touch/transcript?language=en [Google Scholar]
- 7. Verma S. Early impact of CMS expansion of Medicare telehealth during COVID-19.Health Affairs. July 15, 2020. Accessed October 20, 2020. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/ [Google Scholar]
- 8. Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist. 2020;25(6):e936-e945. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.