Abstract
This study examined whether CD8+ T-cell responses from coronavirus disease 2019 convalescent individuals (n = 30) potentially maintain recognition of the major severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants (alpha, beta, gamma; n = 45 mutations assessed). Only 1 mutation found in Beta variant-spike overlapped with a previously identified epitope (1/52), suggesting that virtually all anti-SARS-CoV-2 CD8+ T-cell responses should recognize these newly described variants.
Keywords: CD8+ T cell, convalescent patients, COVID-19, SARS-CoV-2
Due to the proofreading ability of the coronavirus (CoV) RNA-dependent RNA polymerase, the evolution of the global severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral population during the current pandemic has been relatively constrained as compared with other endemic RNA viruses that do not possess this ability [1]. However, during late 2020, 3 distinct variants that each possessed a significantly increased amount of amino acid polymorphisms were identified in association with spikes in cases of coronavirus disease 2019 (COVID-19) in the United Kingdom (variant B.1.1.7, Alpha), South Africa (variant B.1.351, Beta), and Brazil (variant B.1.1.248, Gamma) [2–4].
These variants all possess the N501Y mutation in the receptor-binding domain (RBD) of the SARS-CoV-2 spike protein, a primary target for neutralizing antibody (NAb) binding. They also all contain unique additional mutations throughout the genome and are not phylogenetically linked, indicating that they evolved independently (Supplementary Table 1). Due in part to the mutations found in the RBD and other areas of the spike protein, these primary viral variants, or pseudoviruses expressing the combination of polymorphisms found in each variant, have been examined for their sensitivity to NAb responses detected in plasma from COVID-19 convalescent donors, preclinical or clinical trial postvaccination plasmas, and monoclonal antibodies [4–7]. These studies have shown that the variants are variably susceptible to neutralization, with the Alpha variant exhibiting only minor decreases in susceptibility to convalescent and postvaccination plasma. In addition, preliminary press reports from ongoing phase 2b/3 vaccine trials performed in the United Kingdom during the rise of the Alpha variant suggest that the efficacy of spike-based vaccines has not diminished significantly; however, these studies have not been published or peer-reviewed. Conversely, the Beta variant has demonstrated a significant increase in resistance to neutralization by some individuals’ convalescent plasma, as well as a decline in neutralization potential for the mRNA-based vaccine–induced NAb responses, although it should be noted that this neutralization potential was still estimated to be high enough to confer complete protection [4–7]. Of greater concern, 2 ongoing phase 2/3 vaccine trials of a recombinant protein–based vaccine and an adenovirus-based vaccine have reported a slight decrease in efficacy of the vaccines in preventing symptomatic COVID-19 in South Africa, where the infections were predominantly caused by the Beta variant. These data have not been published or independently reviewed. Interestingly, these same reports claimed that there was no difference in the effectiveness of the vaccines to prevent serious illness between the 2 countries, suggesting that while protection from initial infection may be somewhat hindered, the vaccines’ ability to prevent further disease progression is preserved.
While the correlates of protection in convalescent individuals and vaccinees are unknown, it is assumed that both a broad humoral response and a cell-mediated immunological response are most likely necessary to fully protect against COVID-19. NAb almost certainly serves as the first line of defense against infection, but the CD8+ T-cell response is also important for prevention of further disease progression.
Previously, our group reported a detailed analysis of the CD8+ T-cell epitopes and cytokine responses to the original strain of SARS-CoV-2 in a collection of convalescent individuals from North America with varying levels of disease and NAb responses [8]. This earlier report identified a broad CD8+ T-cell response in these individuals, with virtually all subjects having detectable responses to several viral epitopes.
METHODS
Detailed methods of the previous study have been published [8]. Briefly, peripheral blood mononuclear cell (PBMC) samples from polymerase chain reaction–confirmed recovered COVID-19 convalescent individuals (n = 30) were collected and examined across 6 different Human Leukocyte Antigen (HLA) haplotypes (HLA-A*01:01, HLA-A*02:01, HLA-A03:01, HLA-A*11:01, HLA-A*24:02, and HLA-B*07:02). A multiplexed peptide-MHC tetramer staining approach permitted the screening of 408 potential SARS-CoV-2 candidate epitopes for CD8+ T-cell recognition. T cells were also evaluated using a 28-marker phenotypic panel. Fifty-two unique epitope responses were found and were directed against several structural and nonstructural viral proteins. For controls, CD8+ T cells were probed for reactivity for up to 20 different SARS-CoV-2-unrelated control peptides per HLA (adenovirus-, CMV-, EBV-, influenza-, and MART-1-derived epitopes).
Amino acid polymorphisms found in the Alpha, Beta, and Gamma variants were mapped to the SARS-CoV-2 genome. The variants were then examined for overlap with the identified epitopes from the previous study.
RESULTS
As previously described, 60% of individuals included in the analysis were male, and samples were collected a median (interquartile range) of 42.5 (37.5–48.0) days from initial diagnosis [8]. The group was selected evenly from tertiles (10 each) according to their overall anti-SARS-CoV-2 immunoglobulin G (IgG) titers [8, 9]. Among the convalescent individuals, there were 132 SARS-CoV-2-specific CD8+ T-cell responses corresponding to 52 unique epitope reactivities directed against several structural and nonstructural target epitopes from the entire proteome.
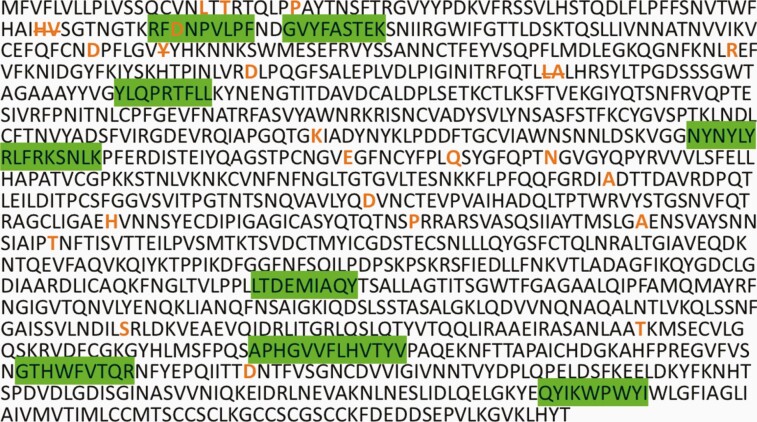
Of all the mapped mutations, insertions, and deletions (n = 45) (Supplementary Table 1), only 1 mutation was found to fall within 1 of the 52 unique epitopes identified in the previous study (Figure 1; Supplementary Figure 1). This mutation is the D80A mutation in the spike protein, and it occurs in the third residue of the RFDNPVLPF epitope. This is an HLA*A24:02-restricted epitope, for which a CD8+ T-cell response was detected in 1 of the 5 HLA*A24:02+ individuals and at a low frequency (0.005 of total CD8+ T cells), indicating that this is not a high-prevalence epitope within the studied cross-sectional sample. The individual in whom this epitope response was detected was part of the high-IgG tertile.
Figure 1.
Spike Protein CD8 Epitopes and Mutations. Severe acute respiratory syndrome coronavirus 2 Wuhan variant spike protein amino acid sequence with CD8+ T-cell epitopes highlighted in green, and all mutation and deletion sites (strikethrough) for variants Alpha, Beta, and Gamma indicated in bold orange.
DISCUSSION
As the global SARS-CoV-2 pandemic continues, it is inevitable that new viral variants will emerge. Many of these variants will disappear unnoticed due to a combination of incomplete or nonexistent genotypic surveillance, changes that have a deleterious impact on viral fitness, and conditions that do not promote their further spread in the population. However, some variants, like the 3 examined here, will emerge in situations where continued spread is possible due to either differences in underlying infectivity of the variant, large founder effects, incomplete treatment interventions, immunocompromised patient groups, low levels of societal physical interventions, or a combination of all or some of these factors. Understanding the extant immunity in previously infected individuals to any new variant is of critical importance to properly estimate what effect these variants may have in the global pandemic [10].
This analysis identified only 1 mutation from the 3 most prominent global SARS-CoV-2 variants that overlapped with 52 CD8+ T-cell epitopes previously identified in a group of convalescent individuals. Additionally, this mutation was found on the third residue of the epitope, and given that the predicted anchor residues for HLA binding of this epitope are residues 2 and 9, one could speculate that this mutation may not significantly affect HLA binding and subsequent TCR recognition [11].
The data on CD8+ T-cell responses from these 30 convalescent individuals are also in line with another recent report showing that the great majority of CD4+ and CD8+ T-cell epitopes from the spike protein of the SARS-CoV-2 variants are also conserved in vaccinated individuals [12, 13]. Yet it should be noted that new variants are continuing to be identified all over the world, and it will be important to continually examine these for the possible accumulation of T-cell escape mutations.
The preliminary analyses of NAb responses to the Alpha, Beta, and Gamma have yielded varied outcomes, with some reduced efficacy of monoclonal antibody therapeutics and a significant decrease in the neutralization capacity of plasma from convalescent and vaccinated individuals to the Beta variant. The vaccines that have been tested thus far against the Beta variant in South Africa demonstrate reduced protective efficacy against COVID-19, but do seem to reduce the number of cases of severe disease at an equivalent level as they do against other strains [4–7]. Yet, it must be highlighted many of these results have not been published in full detail or peer-reviewed. This possible prevention of severe disease may be due in part to the cell-mediated immunity generated due to natural COVID-19 infection or vaccination, which the results presented here would suggest are minimally affected by the mutations found in these variants.
It should be noted that this study had several limitations including the relatively small size of the population examined. In addition, the participants in the study were all from North America and were selected in part on the presence of 1 or more of the target HLA types examined (73% coverage of the continental US population). It will also be important to examine for T-cell escape in more diverse HLA types moving forward.
These data highlight the potential significant role of a multi-epitope T-cell response in limiting viral escape and partly mediating protection from disease caused by SARS-CoV-2 variants. It is important that vaccines used for widespread campaigns generate strong multivalent T-cell responses in addition to NAb and other humoral responses in order to optimize efficacy against the current SARS-CoV-2 and emerging variants. It will be important to continue to monitor the breadth, magnitude, and durability of the anti-SARS-CoV-2 T-cell responses in recovered and vaccinated individuals as part of any assessment to determine if booster vaccinations are needed.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
The authors would like to thank the CCP study and laboratory teams and all the donors for the generous participation in the study.
Financial support. This work was supported in part by National Institute of Allergy and Infectious Diseases (NIAID) grants R01AI120938, R01AI120938S1, and R01AI128779 (A.A.R.T.); the Division of Intramural Research, NIAID, National Institutes of Health (O.L., A.R., T.Q.); and National Heart Lung and Blood Institute grant 1K23HL151826-01 (E.M.B.).
Potential conflicts of interest. H.K., B.A., A.N., and M.F. are shareholders and/or employees of ImmunoScape Pte Ltd. A.N. is a Board Director of ImmunoScape Pte Ltd. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Patient consent. All study participants provided informed consent. This study was approved by the Johns Hopkins Institutional Review Board.
References
- 1. Hillen HS, Kokic G, Farnung L, Dienemann C, Tegunov D, Cramer P. Structure of replicating SARS-CoV-2 polymerase. Nature 2020; 584:154–6. [DOI] [PubMed] [Google Scholar]
- 2. Faria NR, Claro IM, Candido D, et al. Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings. 2021. Available at: https://virological.org/t/genomic-characterisation-of-an-emergent-sars-cov-2-lineage-in-manaus-preliminary-findings/586. Accessed 1 February 2021.
- 3. Public Health England. Investigation of novel SARS-COV-2 variant: variant of concern 202012/01. 2020. Available at: https://www.gov.uk/government/publications/investigation-of-novel-sars-cov-2-variant-variant-of-concern-20201201. Accessed 5 February 2021.
- 4. Cele S, Gazy I, Jackson L, et al. Escape of SARS-CoV-2 501Y.V2 variants from neutralization by convalescent plasma. medRxiv 2021.01.26.21250224 [Preprint]. 27 February 2021. Available at: 10.1101/2021.01.26.21250224. [DOI] [Google Scholar]
- 5. Muik A, Wallisch A-K, Sänger B, et al. Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera. bioRxiv 2021.01.18.426984 [Preprint]. 19 January 2021. Available at: 10.1101/2021.01.18.426984. Accessed 5 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu K, Werner AP, Moliva JI, et al. mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv 2021.01.25.427948 [Preprint]. 25 January 2021. Available at: http://www.ncbi.nlm.nih.gov/pubmed/33501442. Accessed 5 February 2021.
- 7. Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv 2021.01.18.427166 [Preprint]. 1 March 2021. Available at: 10.1101/2021.01.18.427166. [DOI] [PubMed]
- 8. Kared H, Redd AD, Bloch EM, et al. SARS-CoV-2-specific CD8+ T cell responses in convalescent COVID-19 individuals. J Clin Invest 2021; 131:e145476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Klein SL, Pekosz A, Park HS, et al. Sex, age, and hospitalization drive antibody responses in a COVID-19 convalescent plasma donor population. J Clin Invest 2020; 130:6141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Agerer B, Koblischke M, Gudipati V, et al. SARS-CoV-2 escapes CD8 T cell surveillance via mutations in MHC-I restricted epitopes. bioRxiv 2020.12.18.423507 [Preprint]. 20 December 2020. Available at: 10.1101/2020.12.18.423507. Accessed 9 February 2021. [DOI]
- 11. Ibe M, Ikeda Moore Y, Miwa K, Kaneko Y, Yokota S, Takiguchi M. Role of strong anchor residues in the effective binding of 10-mer and 11-mer peptides to HLA-A(*)2402 molecules. Immunogenetics 1996; 44:233–41. [DOI] [PubMed] [Google Scholar]
- 12. Tarke A, Sidney J, Kidd CK, et al. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Reports Med 2021. ; 2:100204.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tarke A, Sidney J, Methot N, et al. Negligible impact of SARS-CoV-2 variants on CD4 + and CD8 + T cell reactivity in COVID-19 exposed donors and vaccinees. bioRxiv 2021.02.27.433180 [Preprint]. 16 February 2021. Available at: 10.1101/2021.02.27.433180. Accessed 7 March 2021. [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.