Summary
Background
The COVID-19 pandemic is putting health professionals under increasing pressure. This population is already acknowledged to be at risk of burnout.
Aim
We aim to provide a ‘snapshot’ of the levels of burnout, anxiety, depression and distress among healthcare workers during the COVID-19 pandemic.
Methods
We distributed an online survey via social media in June 2020 open to any UK healthcare worker. The primary outcome measure was symptoms of burnout measured using the Copenhagen Burnout Inventory. Secondary outcomes of depression, anxiety, distress and subjective measures of stress were also recorded. Multivariate logistic regression analysis was performed to identify factors associated with burnout, depression, anxiety and distress.
Results
A total of 539 persons responded to the survey; 90% female and 53% nurses. Participants with moderate-to-severe burnout were younger (49% vs. 33% under 40 years, P = 0.004), more likely to have pre-existing comorbidities (21% vs. 12%, P = 0.031), twice as likely to have been redeployed from their usual role (22% vs. 11%; P = 0.042), or to work in an area dedicated to COVID-19 patients (50% vs. 32%, P < 0.001) and were almost 4 times more likely to have previous depression (24% vs. 7%; P = 0.012).
Conclusion
Independent predictors of burnout were being younger, redeployment, exposure to patients with COVID-19, being female and a history of depression. Evaluation of existing psychological support interventions is required with targeted approaches to ensure support is available to those most at risk.
Introduction
Healthcare workers in both the acute and community settings have played a key role in responding to the global COVID-19 pandemic. As person-to-person transmission was confirmed,1 healthcare workers were faced with increased risk of exposure to SARS-CoV-2 and put under considerable psychological stress with the risk of developing adverse mental health outcomes.2 Previous investigations have shown that direct contact with highly infectious patients in the Ebola, H1N1 and SARS epidemics were associated with stress in healthcare workers,3–5 therefore, burnout among this professional group is of great concern. During the COVID-19 pandemic, healthcare staff have been exposed to increased workload, working in unfamiliar areas, returning to clinical practice from non-frontline roles, pervasive media coverage and concerns about access to appropriate personal protective equipment (PPE), layered on top of concerns for the health of family and friends—all factors which could contribute to mental stress. As the well-being of health professionals is likely to influence the care they deliver, caring for staff may also indirectly impact patient outcomes.6
Burnout is characterized by excessive work demands causing stress (exhaustion), a detached attitude toward work and colleagues (depersonalization) and reduced feelings of efficiency and attainment (professional efficacy).7 These feelings may be exacerbated during a pandemic due to the unknown nature of the disease, working with a high volume of infected patients and personal risk of contracting the virus. Burnout also has consequences for patients and colleagues due to higher risk of making poor decisions; possible hostile attitude toward patients; medical errors and difficult relationships with co-workers.8
We aim to provide a ‘snapshot’ of the levels of burnout, anxiety, depression and distress among UK healthcare workers during the COVID-19 pandemic. Identifying factors associated with increased prevalence of these measures will highlight the need for interventions and identify staff groups who may be more at risk of adverse psychological outcomes. This will better inform future government and health board decisions about allocation of resources to staff well-being, and better inform how these resources can be targeted to those with the highest risk of adverse mental-well-being outcomes.9
Materials and methods
Study population
The study was designed to evaluate the impact of the COVID-19 pandemic on the mental-well-being of those working in healthcare in the UK. Anybody working in this sector was eligible for inclusion in the study. Participants were recruited through a non-funded social media campaign initiated by the study investigators (one male and two female) on Twitter using snowball sampling (sharing of the survey link among networks). Twitter was considered the most appropriate platform to initiate sharing of the survey through tagging of professional bodies and healthcare institutions by the study authors. All information was collected anonymously.
Questionnaire design
The questionnaire was administered through onlinesurveys.ac.uk. It collected participant demographics (including age, sex, past medical history, professional role, social living situation and caring responsibilities within the family), concerns over COVID-19 (exposure to patients with COVID-19, access to PPE and sources of stress) and access to health and well-being support (informal team support, professional support offered by the workplace and external professional support). Questions were developed by the team who were working in clinical roles during this period, piloted locally with colleagues and reviewed by a clinical psychologist working within the National Health Service (NHS) in Scotland. In addition, validated measures of burnout, depression, anxiety and distress were used to evaluate the incidence of these factors using the Copenhagen Burnout Inventory (CBI),10 Patient Health Questionnaire-9 (PHQ-9),11 General Anxiety Disorder-7 (GAD-7)12 and the Impact of Event Scale (IES-R),13 respectively. These scales have previously been effective in determining incidence of our chosen outcomes in a healthcare staff population.2,4,14,15 There were no mandatory questions in the survey and participants could end or skip questions if they felt unwilling or unable to answer. A copy of the questionnaire is available from the authors on request.
Trial outcomes
The primary outcome was the incidence of moderate or severe burnout of healthcare staff. Secondary outcomes included the incidence of moderate or severe depression, anxiety and distress. A score of 50 or greater on the CBI was used as a threshold to indicate moderate or above burnout (calculated as a mean of the three subscales representing total burnout), whereas scores of greater than 10 were used as a threshold for moderate or above depression or anxiety on the PHQ-9 and GAD-7 scale. A score above 26 indicated at least moderate distress on the IES-R. A breakdown for how the scores were calculated is included in the Supplementary Appendix (Supplementary Table S1). Additional secondary outcomes included subjective measurement of increased stress during the COVID pandemic, and the reasons for this, as well as the reasons participants may not have accessed support services available in the workplace. Emerging data from Singapore, India and China suggests that ∼10% of healthcare professionals managing patients with COVID-19 experience moderate-to-severe anxiety.2,16 We estimate that recruitment of 500 participants into our study will identify at least 50 participants who have at least a moderate level of anxiety.
Ethical approval
The study was reviewed and approved by the University of Edinburgh ethics review panel from the school of Philosophy, Psychology and Language Sciences. Participants indicated that they wished to complete the survey before accessing the content. Consent was therefore implied by accessing and completing the survey content.
Statistical analysis
Baseline characteristics were summarized for the study population and in groups according to the presence or absence of moderate-severe burnout, depression, anxiety and distress. Continuous variables are presented as mean (SD) or median (IQR), as appropriate. Categorical variables are presented as absolute numbers (%). Group-wise comparisons were performed using Chi-square, Kruskal–Wallis or one-way analysis of variance tests as appropriate. Univariable and multivariable logistic regression models were used to estimate the odds of the primary outcome, or either secondary outcome and influence of baseline variables. Baseline variables for the model were selected a priori based on their clinical relevance, including age, sex, past medical history (including known ischemic heart disease or coronary artery disease, diabetes mellitus or immunocompromise), previous history of mental illness, as well as descriptors of their working environment. All analyses were performed in R (Version 3.5.1).
Results
Population demographics
Between 17th and 24th June 2020, 539 participants completed the study questionnaire (90% [480/533] female, 53% [286/539] nurses). The majority of participants lived and worked in Scotland (97%, 512/530) (Supplementary Table S2). Accordingly, the occupation and sex of participants in the study closely reflected the NHS workforce.17 Baseline characteristics of the study population are summarized stratified by the presence or absence of moderate-to-severe burnout (Table 1).
Table 1.
Baseline characteristics of study population stratified by the presence of moderate or severe burnout using the CBI
| Moderate-severe burnout |
||||
|---|---|---|---|---|
| All | Present | Absent | P-value | |
| No. of participants | 539 (100) | 424 (79) | 115 (21) | –– |
| Age (years) | ||||
| 21–30 | 121 (22) | 101 (24) | 20 (17) | 0.012 |
| 31–40 | 122 (23) | 104 (25) | 18 (16) | |
| 41–50 | 141 (26) | 106 (25) | 35 (30) | |
| 51–60 | 126 (23) | 96 (23) | 30 (26) | |
| >60 | 27 (5) | 16 (4) | 11 (10) | |
| Males | 53 (10) | 33 (8) | 20 (18) | 0.004 |
| Females | 486 (90) | 390 (92) | 96 (82) | 0.004 |
| Significant past medical history | 104 (19) | 90 (21) | 14 (12) | 0.04 |
| Coronary artery disease | 12 (2) | 10 (2) | 2 (2) | 1 |
| Malignancy | 7 (1) | 6 (1) | 1 (1) | 1 |
| COPD | 60 (11) | 51 (12) | 9 (8) | 0.27 |
| Diabetes mellitus | 16 (3) | 15 (4) | 1 (1) | 0.236 |
| Immunocompromized | 25 (5) | 21 (5) | 4 (4) | 0.677 |
| Previous mental health diagnosis | 177 (33) | 159 (38) | 18 (16) | <0.001 |
| Previous anxiety | 131 (24) | 119 (28) | 12 (10) | <0.001 |
| Previous depression | 109 (20) | 101 (24) | 8 (7) | <0.001 |
| Other mental health condition | 21 (4) | 18 (4) | 3 (3) | 0.594 |
| Family member at high risk | 99 (19) | 87 (21) | 12 (11) | 0.019 |
| Main carer for another adult | 39 (7) | 35 (8) | 4 (4) | 0.125 |
| Main occupation | ||||
| Allied health professionala | 32 (6) | 24 (6) | 8 (7) | <0.001 |
| Clinical support worker | 54 (10) | 47 (11) | 7 (6) | |
| Doctor | 57 (11) | 34 (8) | 23 (20) | |
| Nurse | 286 (53) | 245 (58) | 41 (36) | |
| Pharmacist | 4 (1) | 2 (1) | 2 (2) | |
| Other | 106 (20) | 72 (17) | 34 (10) | |
| Redeployed from normal workplace | 105 (20) | 93 (22) | 12 (10) | 0.008 |
| Exposure to patients with COVID-19 | ||||
| No known contact | 94 (17) | 62 (15) | 32 (28) | <0.001 |
| Patients with suspected COVID-19 | 64 (12) | 43 (10) | 21 (18) | |
| Patients with confirmed COVID-19 | 131 (24) | 106 (25) | 25 (22) | |
| Work in a dedicated COVID-19 unit | 250 (46) | 213 (50) | 37 (32) | |
| PPE (PPE) | ||||
| Properly trained with PPE | 300 (57) | 232 (55) | 68 (61) | 0.365 |
| Always have access to PPE when needed | 359 (67) | 273 (64) | 86 (75) | 0.047 |
| Properly fitted for specialist PPE if required | 280 (71) | 225 (71) | 55 (73) | 0.868 |
| Feel safe or very safe when using PPE | 234 (43) | 166 (39) | 68 (59) | <0.001 |
| Psychological support | ||||
| Support is available in the workplace | 411 (77) | 308 (73) | 103 (90) | <0.001 |
| Support was accessed from the workplace if available | 91 (22) | 76 (25) | 15 (15) | 0.064 |
| Support accessed exclusively from outside the workplace | 44 (8) | 36 (9) | 8 (7) | 0.999 |
| Rating of support within team median [IQR]b | 3.0 [2.0, 4.0] | 3.0 [2.0, 4.0] | 4.0 [3.0, 5.0] | <0.001 |
Note: Values are expressed as n (%) unless otherwise stated. A P value of <0.05 is considered significant.
Allied health professional group includes dieticians (n = 1), radiographers (n = 4), physiotherapists (n = 11) and occupational therapists (n = 16).
Rating of support within workplace team is on a self-reported integer scale with 1—least supportive to 5—most supportive.
Population with moderate-severe burnout
Burnout was present in the majority of participants (79%, 424/539). Compared to participants who did not have moderate-to-severe burnout, those who met the CBI criteria tended to be younger (49% [206/424] vs. 33% [38/115] under 40 years, P = 0.004) and female (92% vs. 82%, P = 0.004). They were twice as likely to have pre-existing comorbidities [21% vs. 12%, unadjusted odds ratio (OR) 1.9, 95% CI 1.4–2.6, P = 0.031], and were 4-times more likely to have previous mental illness, such as depression (24% vs. 7%, unadjusted OR 4.2, 95% CI 2.6–6.1, P < 0.001). After adjusting for other variables (Table 2), previous depression remained the most powerful independent predictor of moderate-severe burnout, increasing the odds by more than 3-fold (adjusted OR 3.6, 95% CI 2.2–5.9, P = 0.012).
Table 2.
Predictors of moderate-severe burnout
| Univariate OR for type moderate-severe burnout (95% CI) | P-value for term | Multivariate OR for type moderate-severe burnout (95% CI) | P-value for term | |
|---|---|---|---|---|
| Age 20–30 | –– | –– | –– | –– |
| 31–40 | 1.1 (0.8–1.6) | 0.703 | 1.2 (0.8–1.8) | 0.64 |
| 41–50 | 0.6 (0.4–0.8) | 0.102 | 0.9 (0.6–1.4) | 0.869 |
| 51–60 | 0.6 (0.5–0.9) | 0.156 | 0.6 (0.4–0.9) | 0.24 |
| 61–70 | 0.3 (0.2–0.5) | 0.007 | 0.4 (0.2–0.8) | 0.174 |
| Sex (M) | 0.4 (0.3–0.5) | 0.003 | 0.3 (0.2–0.5) | 0.003 |
| Significant past medical historya, including immunocompromised | 1.9 (1.4–2.6) | 0.031 | 1.6 (1.1–2.4) | 0.215 |
| Previous anxiety | 3.3 (2.4–4.6) | <0.001 | 1.8 (1.2–2.7) | 0.128 |
| Previous depression | 4.2 (2.8–6.1) | <0.001 | 3.6 (2.2–5.9) | 0.012 |
| Other previous significant mental health condition | 1.7 (0.9–3.1) | 0.426 | 0.9 (0.4–1.9) | 0.856 |
| Family member in a high-risk category of COVID | 2.2 (1.6–3.1) | 0.015 | 1.9 (1.3–2.8) | 0.117 |
| Main carer for another adult | 2.5 (1.4–4.2) | 0.092 | 2.3 (1.1–4.6) | 0.246 |
| Redeployed from normal working role | 2.4 (1.7–3.4) | 0.007 | 2.2 (1.5–3.3) | 0.042 |
| Exposure level to COVID-19 in working role (per unit increase, scale 1–4) | 1.5 (1.4–1.6) | <0.001 | 1.6 (1.4–1.8) | <0.001 |
| Workplace support available | 0.3 (0.2–0.4) | <0.001 | 0.7 (0.4–1) | 0.314 |
| Supportive workplace team environment (per unit increase, scale 1–4) | 0.5 (0.5–0.6) | <0.001 | 0.6 (0.5–0.7) | <0.001 |
| PPE (PPE): | ||||
| Adequate training received in use of PPE (Yes) | 0.8 (0.6–1) | 0.311 | 0.8 (0.6–1.1) | 0.482 |
| Access to PPE (scale 1–5) | 0.7 (0.6–0.8) | 0.001 | 0.9 (0.8–1.1) | 0.709 |
| Feeling of safety when using supplied PPE (scale 1–5) | 0.7 (0.6–0.7) | <0.001 | 0.9 (0.8–1) | 0.355 |
Multivariate logistic regression model adjusted for all variables described with univariate and multivariate odds ratios. A P value of < 0.05 is considered significant.
An odds ratio of >1 is a predictor of burnout, whereas an odds ratio of <1 is protective against burnout. For example, a supportive workplace team is protective against burnout.
Significant past medical history includes participants with diabetes mellitus, chronic cardiovascular disease, chronic airways disease, current malignancy and those receiving oral or intravenous steroids, or immunotherapy agents.
Participant occupation and working environment also had a significant impact on the incidence of burnout (Table 2). Those with moderate-severe burnout were twice as likely to have been redeployed from their normal place of work (22% vs. 11%, adjusted OR 2.2, 95% CI 1.5–3.3, P = 0.042), and work in an area dedicated to treating patients with confirmed COVID-19 infection (50% vs. 32%, adjusted OR 1.6, 95% CI 1.4–1.8, P < 0.001). Participants with burnout also had less frequent access to all of the PPE required to work safely (64% vs. 75% always having access to PPE, P = 0.047); however, in adjusted models, this association was attenuated. A supportive workplace team and male sex were both powerful independent predictors protecting against burnout, reducing the odds by 40% (adjusted OR 0.6, 95% CI 0.5–0.7, P < 0.001) and 70% (adjusted OR 0.3, 95% CI 0.2–0.5, P = 0.003), respectively.
Secondary outcomes of moderate-severe depression, anxiety and distress
Baseline characteristics stratified by the presence of moderate-severe depression, anxiety and distress are summarized in Supplementary Table S3. In participants with moderate or severe depression, as classified by the PHQ-9 score, treating patients with confirmed COVID-19 infection (adjusted OR 1.3, 95% CI 1.1–1.4, P = 0.023) and previous depression (adjusted OR 3.6, 95% CI 2.6–4.9, P < 0.001), were important independent predictors of the odds of depression. Similar results were seen in models to predict moderate-severe anxiety (Supplementary Table S4). A supportive workplace team was protective against depression (adjusted OR 0.7, 95% CI 0.7–0.8, P = 0.001). Only 5/539 participants scored above the threshold for moderate distress as classified by IES-R (Supplementary Table S3).
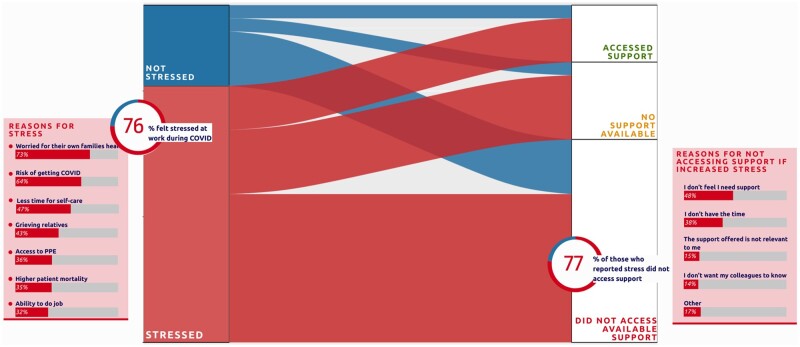
Stress and workplace staff support
The majority of participants (76%, 408/539) recorded increased stress (Figure 1), primarily because of concern about their family’s health (73%, 296/408), or their own risk of contracting COVID-19 (64%, 262/408). Other reasons for increased stress included concern about access to PPE (36% 148/408), their ability to do their job properly (32%, 131/408) and having to cope with higher patient mortality (35%, 144/408), with nearly one-third of participants remarking that these reasons had caused them concern. Only a minority of participants who reported stress had accessed local workplace support (23%, 70/306). The most common reason for not doing so was not feeling a need for support, despite increased stress (48%, 113/236), although 38% (89/236) felt they needed support but did not have time, while 1 in 7 participants felt that they needed support but they did not want their colleagues to know (14%, 34/236) or that the support was not relevant to them (15%, 36/236). Dedicated workplace support was not available to one in four participants (25%, 102/408).
Figure 1.
Alluvial diagram showing proportion of participants with increased stress during the COVID-19 pandemic, causes of stress and whether workplace support was available and accessed. Causes of stress are shown as a stacked bar chart, with size of bar representing proportion, with participants able to select multiple responses.
Discussion
Prior to COVID-19, burnout among healthcare workers was already a concern. While estimates vary, systematic reviews have reported a prevalence of 11% among nurses, and between 31% and 54% among UK doctors.18,19 Irregular hours, understaffing, physical and psychological stress and the provision of complex care are all elements thought to contribute to the development of burnout.19 We report that the independent predictors of overall burnout among our sample population are being younger, female, redeployed to a new working area, working with patients with confirmed COVID-19 infection, concerns over access to adequate PPE and a prior history of depression. Our findings are consistent with other studies reporting a higher incidence of burnout among women and those with younger age,2,20–22 those working in areas with high COVID-19 exposure, concerns over PPE provision and a history of pre-existing psychological problems.23–25
Previous work has suggested that women in healthcare may be at higher risk of burnout due to the large proportion involved in front line care in the nursing profession thereby increasing their exposure to COVID-19.2 It is also possible that the large proportion of nurses in this study represent a younger population, who often have less experience in their respective positions and who may therefore be at increased risk of adverse psychological outcomes.
At the start of a healthcare crisis, there is an initial sense of eagerness to contribute to the healthcare effort and a sense of obligation to work through the pandemic.26 Staff volunteered to work in roles, or were redeployed to roles, that were unfamiliar to them as regular NHS services were paused. These redeployed staff are also identified as a high-risk group so should be a target for health and well-being interventions. Interventions can be focused at the level of the individual or within organizational structures. Organization directed interventions (teamwork, leadership, workload and shift rotation) were seen to reduce physician burnout more than individual directed interventions.27 Examples of organization directed interventions are prioritizing staff safety (access to PPE), organizing rotas to maintain existing teams, supporting staff to implement recommendations and ensuring visibility of managers.28 These are all modifiable factors that if addressed could prevent the development of burnout.25 Telephone helplines are an example of an individual targeted intervention and while staff appreciated the availability of this service, it could also be viewed as too impersonal to be an effective support mechanism.29
In addition to burnout, we recorded subjective measures of stress. More than three quarters of the workforce surveyed reported feeling heightened stress levels at work during the COVID-19 pandemic, but fewer than one in four of those with stress had accessed workplace support. The main reason reported was that support was not required, despite feeling heightened stress levels. This phenomenon is not unusual amongst healthcare workers with a delay between event-timing, and reflective practice that allows staff to acknowledge the emotional impact of their work.29 As not all of those recognizing their need for support accessed support, this suggests that the structure through which the support is being offered may not be meeting the needs of those it is intended to serve. Inadequate time, and not wanting colleagues to know they were seeking support were two of the main barriers to access. Digital platforms are effective in delivering psychological treatment,30 therefore can be offered by organizations and accessed discreetly at an appropriate time for the individual. One of the few factors found to be protective against burnout, depression and anxiety was feeling supported at work. Peer supervision and strong teamwork have been previously shown to strengthen workplace well-being.31 Healthcare employers could support service leads, ward managers, senior nurses and local supervisors to understand their critical role in supporting their staff to prevent the development of burnout.
Heavy emotional burden has been previously shown to be a predictor of burnout among healthcare workers.14,32 Working in COVID-19 designated areas with a high concentration of critically ill and dying patients with relatives unable to visit has placed an even higher emotional demand on staff which may be a contributing cause to burnout seen in this staff group.
As well as a professional identity, healthcare workers also occupy multiple other identities including that of parents, children, siblings and friends. The major causes of stress among those surveyed were fears for personal health and that of the family. Previous studies have reported that prioritizing well-being of family members represented a barrier to working during an influenza pandemic with degree of worry related to intentional absenteeism.26,33 With burnout currently present in the majority (79%) of survey participants, employers risk losing staff during subsequent waves if not supported adequately. As current health and well-being interventions do not appear to be optimized, employers should aim to revise the support offered through thorough evaluation with intended service users and target future interventions to staff groups most at risk.
Limitations
This study has several limitations. The majority of respondents were female, which is perhaps not unsurprising given than more than half were from the nursing profession where 89% of the workforce are women.17 We did not collect data on ethnicity of respondents. As it is now known that black and ethnic minority groups are more adversely affected by COVID-19 this may have an impact on mental health outcomes among these staff groups. However, in Scotland, 96% of the population identify as white34 therefore it is unlikely we could have performed analyses stratified by ethnicity in our respondent population. Additionally, it is possible that a mental health social media survey has captured the responses of those that are already engaged with the topic and may therefore overestimate the prevalence burnout, anxiety and depression in the target population.
Supplementary material
Supplementary material is available at QJMED online.
Funding
This study was supported by the British Heart Foundation through a Senior Clinical Research Fellowship (FS/16/14/32023) and a Research Excellence Award (RE/18/5/34216).
Data sharing
A de-identified data set can be made available for sharing upon request.
Author’s contribution
A.F., R.W. and F.S. designed the study and carried out the initial acquisition, analysis or interpretation of data. All authors were involved in drafting and revising the manuscript and have given final approval of the version to be published.
Transparency declaration
The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Conflict of interest. None declared.
Supplementary Material
References
- 1. Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet 2020; 395:1137–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3:e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smith MW, Smith PW, Kratochvil CJ, Schwedhelm S.. The psychosocial challenges of caring for patients with Ebola virus disease. Health Security 2017; 15:104–9. [DOI] [PubMed] [Google Scholar]
- 4. Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatr Clin Neurosci 2012; 66:353–60. [DOI] [PubMed] [Google Scholar]
- 5. Nickell L, Crighton E, Shawn Tracy C, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effect of SARS on hospital staff: survey on a large tertiary care institution. Can Med Assoc J 2004; 170:793–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Waqas A, Ahmad W, Haddad M, Taggart FM, Muhammad Z, Bukhari MH, et al. Measuring the well-being of health care professionals in the Punjab: a psychometric evaluation of the Warwick-Edinburgh mental well-being scale in a Pakistani population. PeerJ 2015; 3:e1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Koutsimani P, Montgomery A, Georganta K.. The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol 2019; 10:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kumar S. Burnout and Doctors: prevalence, prevention and Intervention. Healthcare (Basel )2016; 4:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Academy of Medical Sciences. Preparing for a Challenging Winter 2020-2021. 2020; https://acmedsci.ac.uk/file-download/51353957 (7 July 2020, date last accessed).
- 10. Kristensen TS, Borritz M, Villadsen E, Christensen KB.. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress 2005; 19:192–207. [Google Scholar]
- 11. Spitzer RL, Kroenke K, Williams JBW, Löwe B.. A brief measure for assessing general anxiety disorder. The GAD-7. Arch Intern Med 2006; 166:1092–7. [DOI] [PubMed] [Google Scholar]
- 12. Kroenke K, Spitzer RL, Williams JB.. The PHQ-9 validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Weiss D, Marmer C.. The impact of event scale—revised. In: Wilson J, Keane T, eds. Assessing Psychological Trauma and PTSD: A Practitioners Handbook. New York, Guilford Press, 1997, 399–411. [Google Scholar]
- 14. Creedy DK, Sidebotham M, Gamble J, Pallant J, Fenwick J.. Prevalence of burnout, depression, anxiety and stress in Australian midwives: a cross-sectional survey. BMC Preg Childbirth 2017; 17:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chen C-S, Yang P, Yen C-F, Wu H-Y.. Validation of Impact of Events Scale in nurses under threat of contagion by severe acute respiratory syndrome. Psychiatr Clin Neurosci 2005; 59:135–9. [DOI] [PubMed] [Google Scholar]
- 16. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020; 88:559–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Public Health Scotland. NHS Scotland Workforce Information, 2019. https://www.isdscotland.org/Health-Topics/Workforce/Publications/data-tables2017.asp (8 July 2020, date last accessed).
- 18. Imo U. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bull 2017; 41:197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Woo T, Ho R, Tang A, Tam W.. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res 2020; 123:9–20. [DOI] [PubMed] [Google Scholar]
- 20. Matsuo T, Kobayashi D, Taki F, Sakamoto F, Uehara Y, Mori N, et al. Prevalence of health care worker burnout during the Coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw Open 2020; 3:e2017271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Khasne RW, Dhakulkar BS, Mahajan HC.. Burnout among Healthcare Workers during COVID-19 pandemic in India: results of a questionnaire-based survey. Ind J Crit Care Med 2020; 24:664–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moitra M, Rahman M, Collins PY, Gohar F, Weaver M, Kinuthia J.. Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for LMICs. Front Psychiatr 2021; 12:602–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lasalvia A, Amaddeo F, Porru S, Carta A, Tardivo S, Bovo C, et al. Levels of burnout among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open 2021; 11:e045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. de Wit K, Mercuri M, Wallner C, Clayton N, Archambault P, Ritchie K, et al. , for the Network of Canadian Emergency Researchers. Canadian emergency physician psychological distress and burnout during the first 10 weeks of COVID-19: a mixed-methods study. J Am Coll Emerg Phys Open 2020; 1:1030–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gemine R, Davies GR, Tarrant S, Davies RM, James M, Lewis K.. Factors associated with work-related burnout in NHS staff during COVID-19: a cross-sectional mixed methods study. BMJ Open 2021; 11:e042591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ives J, Greenfield S, Parry JM, Draper H, Gratus C, Petts JI, et al. Healthcare workers’ attitudes to working during pandemic influenza: a qualitative study. BMC Public Health 2009; 9:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. De Simone S, Vargas M, Servillo G.. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res 2019; doi:10.1007/s40520-019-01368-3. [DOI] [PubMed] [Google Scholar]
- 28. Walton M, Murray E, Christian MD.. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care 2020; 9:241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Billings J, Chi Fung Ching B, Gkofa V, Greene T, Bloomfield M. Healthcare workers’ experiences of working on the frontline and views about support during COVID-19 and comparable pandemics: a rapid review and meta-synthesis. 2020; doi:10.1101/2020.06.21.20136705. [DOI] [PMC free article] [PubMed]
- 30. Chandrashekar P. Do mental health mobile apps work: evidence and recommendations for designing high-efficacy mental health mobile apps. Mhealth 2018; 4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jarden RJ, Sandham M, Siegert RJ, Koziol-McLain J.. Strengthening workplace well-being: perceptions of intensive care nurses. Nurs Crit Care 2019; 24:15–23. [DOI] [PubMed] [Google Scholar]
- 32. Le Blanc PM, Bakker AB, Peeters MCW, van Heesch NCA, Schaufeli WB.. Emotional job demands and burnout among oncology care providers. Anxiety Stress Coping 2001; 14:243–63. [Google Scholar]
- 33. Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T.. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis 2010; 10:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clark D. Distribution of non-white ethnic backgrounds in Scotland in 2018. 2019; https://www.statista.com/statistics/367842/scotland-ethnicity-of-population/ (15 July 2020, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.