Abstract
Aims
The COVID-19 pandemic has led to a decline in hospitalizations for non-COVID-19-related conditions. We explored the impact of the COVID-19 pandemic on cardiac operations and interventions undertaken in England.
Methods and results
An administrative database covering hospital activity for England, the Health Episodes Statistics, was used to assess a total of 286 697 hospitalizations for cardiac operations and interventions, as well as 227 257 hospitalizations for myocardial infarction (MI) and 453 799 for heart failure (HF) from 7 January 2019 to 26 July 2020. Over the 3 months of ‘lockdown’, total numbers and mean reductions in weekly rates [n (−%)], compared with the same time period in 2019, were: coronary artery bypass grafting [−2507 (−64%)]; percutaneous coronary intervention [−5245 (−28%)]; surgical [−1324 (−41%)] and transcatheter [−284 (−21%)] aortic valve replacement; mitral valve replacement; implantation of pacemakers [−6450 (−44%)], cardiac resynchronization therapy with [−356 (−42%)] or without [−491 (−46%)] defibrillation devices, and implantable cardioverter-defibrillators [−501 (−45%)]; atrial fibrillation ablation [−1902 (−83%)], and other ablations [−1712 (−64%)] (all P < 0.001). Over this period, there were 21 038 fewer procedures than in the reference period in 2019 (P < 0.001). These changes paralleled reductions in hospitalizations for MI [−10 794 (−27%)] and HF [−63 058 (−28%)] (both P < 0.001).
Conclusions
The COVID-19 pandemic has led to substantial reductions in the number of cardiac operations and interventions undertaken. An alternative strategy for healthcare delivery to patients with cardiac conditions during the COVID-19 pandemic is urgently needed.
Keywords: COVID-19, Myocardial infarction, Heart failure, Aortic valve replacement, Mitral valve replacement, Transcatheter aortic valve implantation, Pacemaker, Cardiac resynchronization therapy, Implantable cardioverter-defibrillator, Cardiac ablation
What’s new?
The first wave of the COVID-19 pandemic led to a dramatic, nationwide reduction in the delivery of cardiac operations and interventions, as well as in the number of hospitalizations for myocardial infarction and heart failure.
The most marked reductions in cardiological practice were observed for cardiac ablation and cardiac implantable electronic device implantation.
An alternative strategy for delivering healthcare to patients with cardiac conditions during the COVID-19 pandemic is urgently needed.
Introduction
In the week commencing the 27 January 2020, the first two cases of COVID-19 were diagnosed in England.1 On 11 March 2020, the World Health Organization declared the COVID-19 pandemic. Following a national ‘lockdown’ announcement on 23 March 2020, hospitalizations for COVID-19 rose to a peak of 3099 on 1 April 2020. In order to meet unprecedented demands, hospitals responded by increasing capacity for COVID-19 patients.2 It is apparent that at least some hospital capacity for COVID-19 was made available by reducing healthcare provision for patients non-COVID-19 conditions.
Cardiovascular disease is major cause of mortality and morbidity worldwide and has been identified as a risk factor for total mortality in COVID-19 patients.3,4 Yet, increasing evidence shows that during the pandemic, patients with cardiac conditions were less likely to attend hospital,5–7 perhaps because of confinement guidelines and/or the perceived risk of contagion. In the ‘first wave’ of the COVID-19 pandemic, reports from the UK,8–10 Italy,5 Austria,11 China,12 and the USA13,14 have shown substantial reductions in cardiac interventions. The objective of the present study was to quantify nationwide changes in the delivery of cardiac operations and interventions in England during the ‘first wave’ of the COVID-19 pandemic.
Methods
This is a retrospective study of hospitalizations for cardiac conditions, operations, and interventions from 7 January 2019 to 26 July 2020, which encompasses the first ‘wave’ of the COVID-19 pandemic. We used the National Health Service Hospital Episode Statistics (HES). These are available to University Hospitals Birmingham under a data-sharing agreement (section 251 of the National Health Service Act 2006), which obviates the need for Ethics Committee approval. The study was approved by the Clinical Audit Department at the University Hospitals Birmingham, Queen Elizabeth, and conforms to the Declaration of Helsinki.
Data collection
The HES database, provided by National Health Service Digital, contains data on hospitalizations to all NHS hospitals in England (56.3 M population in 2019). Wales and Scotland are not covered by HES. The main focus in this study was hospitalization for cardiac operations and interventions, rather than on patient-level data. Episodes of care for the different diagnoses, cardiac operations, and interventions were identified using International Classification of Diseases 10th revision (ICD-10) codes and the Office of Population, Censuses and Surveys Classification of Interventions and Procedures version 4. The diagnosis, cardiac operation, or intervention was identified using ‘position 1’ of the hospitalization coding (Supplementary material online, Table S1). The diagnoses included myocardial infarction (MI) or heart failure (HF), whether or not patients underwent an operation or an intervention. Operations and procedures included coronary artery bypass graft (CABG), percutaneous coronary intervention (PCI), surgical aortic valve replacement, mitral valve replacement, transcathether aortic valve implantation, pacemaker implantation, cardiac resynchronization-pacing device implantation, cardiac resynchronization-defibrillation device implantation, implantable cardioverter-defibrillator implantation, ablation for atrial fibrillation, and ablation for conditions other than atrial fibrillation.
Statistical analysis
In analyses of hospitalization numbers, the total number of diagnoses, cardiac operations, and interventions were quantified on a weekly basis. Relative changes in hospitalizations were expressed as the difference in weekly rates during the 3 months after the announcement of the national lockdown (from week beginning on 23 March to week ending 21 June 2020) and the reference period in 2019 (from week beginning on 25 March to week ending on 23 June 2019). The total number of hospitalizations for clinical conditions, cardiac operations, and interventions in these periods was also quantified. Continuous variables are expressed as mean ± 95% confidence intervals (95% CI). Normality was tested using the Shapiro–Wilk test. Student’s t-tests were used to analyse differences between these time periods. Statistical analyses were undertaken using Stata15 (StataCorp, TX, USA).
Results
Cardiac operations and interventions
Data from all 147 NHS hospitals were available from HES. From 7 January 2019 to 26 July 2020, there were 295 640 hospitalizations for cardiac operations and interventions. Weekly rates of cardiac operations and interventions during the reference period in 2019 for all cardiac operations and interventions, as well as for hospitalizations for MI and HF were similar to the weekly rates over the year 2019 (data not shown).
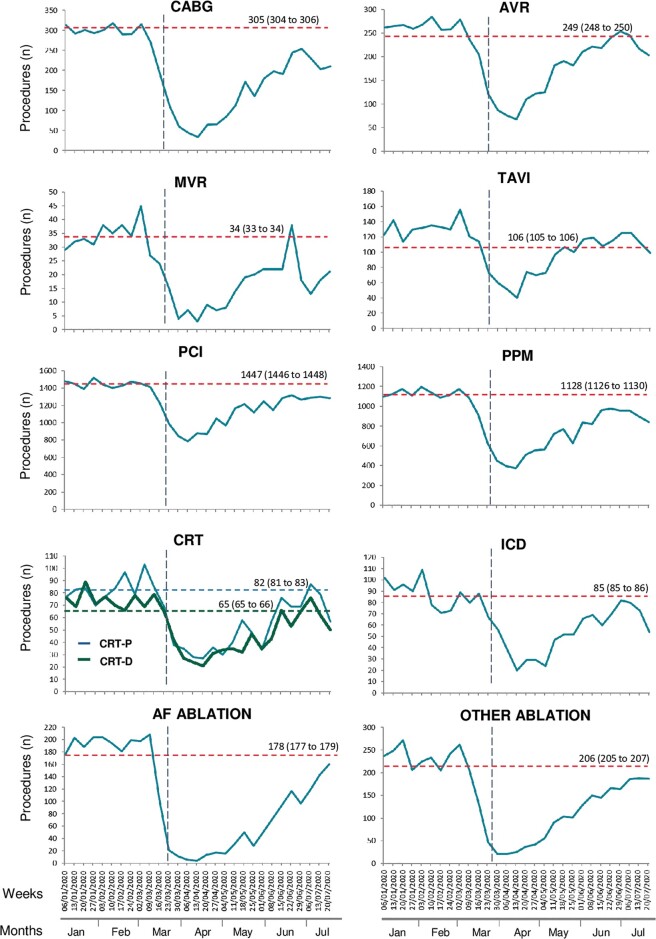
The decline in hospitalizations for cardiac operations and interventions began on the week of 2 March 2020, ∼2 weeks before the lockdown was announced. The most marked reductions in average weekly rates occurred during April 2020: atrial fibrillation ablation (−97%), other ablations (−91%), and mitral valve replacements (−90%) (Figure 1). In the week of 13 April 2020, a gradual increase was observed for all operations and interventions. By the week of 20 July 2020, weekly rates remained below 2019 levels for most operations and interventions.
Figure 1.
Number of cardiac operations and interventions in hospitalizations undertaken in England during the COVID-19 pandemic. Dashed horizontal lines indicate the mean weekly rate of procedures during the reference period in 2019. Mean and 95% CI are shown above the lines. The black, vertical, dashed line marks the announcement of the national ‘lockdown’ on 23 March 2020. AF, atrial fibrillation; AVR, surgical aortic valve replacement; CABG, coronary artery bypass graft; CRT-D, cardiac resynchronization therapy-defibrillation; CRT-P, cardiac resynchronization therapy-pacing; ICD, implantable cardioverter-defibrillator; MVR, mitral valve replacement; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; TAVI, transcatheter aortic valve implantation.
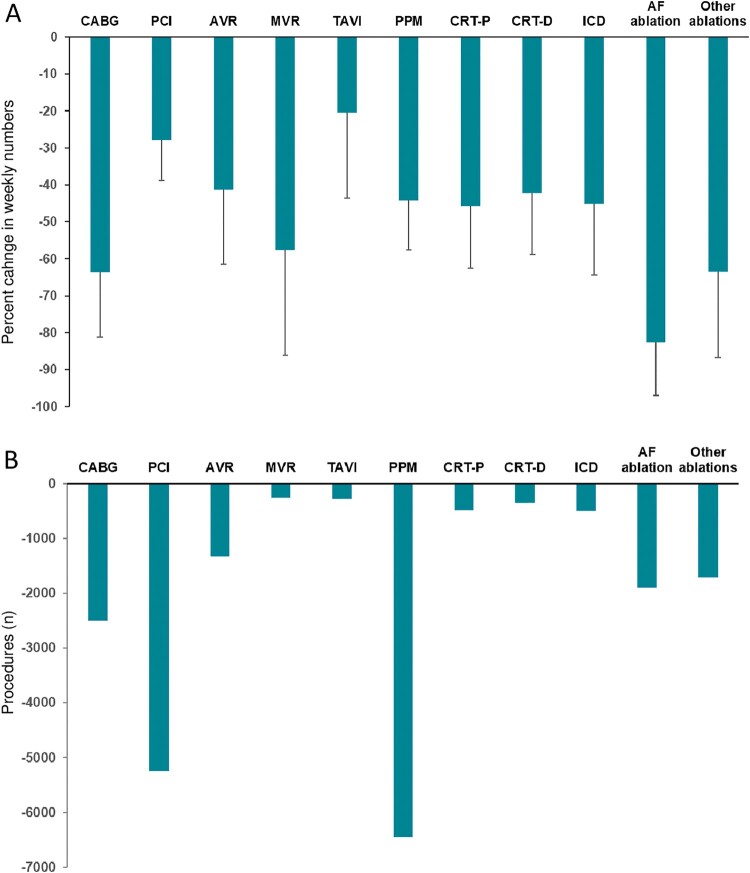
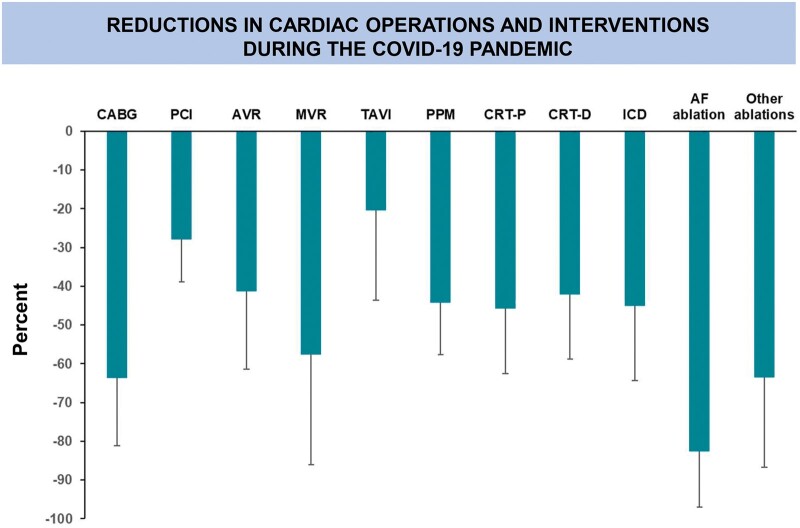
From 7 January 2019 to 26 July 2020, there were 295 640 cardiac operations or interventions. Over the 3 months of lockdown, there was a reduction in hospitalizations for cardiac operations and interventions from 50 508 during the reference period in 2019 to 29 470 (Table 1). In addition, there were 6450 fewer pacemaker implantations, 5245 fewer PCIs, and 2507 fewer CABGs (Table 1). In terms of per cent change in numbers, the most marked reductions were observed for atrial fibrillation ablation [−83% (95% CI 82–83)], other ablations [−64% (95% CI 63–64)], and CABG [64% (95% CI 63–64)] (Figure 2). All comparisons of numbers of cardiac operations and interventions over the 3 months of lockdown with the numbers in the reference period in 2019 were statistically significant (P < 0001).
Table 1.
Hospitalizations for myocardial infarction and heart failure, and number of procedures during the COVID-19 pandemic
| Numbers during 2019 reference period | Numbers during lockdown | Reduction in numbers during lockdown a | Per cent reduction in weekly rate (95% CI) | |
|---|---|---|---|---|
| Cardiac conditions | ||||
| Myocardial infarction | 39 473 | 28 679 | 10 794 | 27 (27–27) |
| Heart failure | 224 650 | 161 592 | 63 058 | 28 (28–28) |
| Total | 264 123 | 190 271 | 73 852 | |
| Cardiac operations | ||||
| CABG | 3961 | 1454 | 2507 | 64 (63–64) |
| Aortic valve replacement | 3240 | 1916 | 1324 | 41 (41–42) |
| Mitral valve replacement | 438 | 172 | 266 | 58 (55–60) |
| Total | 7639 | 3542 | 4097 | |
| Cardiac interventions | ||||
| PCI | 18 815 | 13 570 | 5245 | 28 (28–28) |
| TAVI | 1373 | 1089 | 284 | 20 (19–22) |
| Pacemakers | 14 662 | 8212 | 6450 | 44 (44–44) |
| CRT-pacing | 1067 | 576 | 491 | 46 (45–47) |
| CRT-defibrillation | 846 | 490 | 356 | 42 (41–43) |
| ICD | 1110 | 609 | 501 | 45 (44–46) |
| AF ablation | 2316 | 414 | 1902 | 83 (82–83) |
| Other ablation | 2680 | 968 | 1712 | 64 (63–64) |
| Total | 42 869 | 25 928 | 16 941 |
Compared to the reference period in 2019, all changes compared with the numbers in the reference period in 2019 were statistically significant (P < 0001).
AF, atrial fibrillation; CABG, coronary artery bypass graft; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter-defibrillator; PCI, percutaneous coronary intervention; TAVI, transcatheter aortic valve implantation.
Figure 2.
Number of cardiac operations and interventions during the COVID-19 pandemic. Graphs show (A) mean per cent (SD) change in the weekly number and (B) change in the total number of cardiac operations and interventions during the 3 months of lockdown. In (A), changes in relation to reference period in 2019 were all statistically significant (P < 0.001). AF, atrial fibrillation; AVR, surgical aortic valve replacement; CABG, coronary artery bypass graft; CRT-D, cardiac resynchronization therapy-defibrillation; CRT-P, cardiac resynchronization therapy-pacing; ICD, implantable cardioverter-defibrillator; MVR, mitral valve replacement; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; TAVI, transcatheter aortic valve implantation.
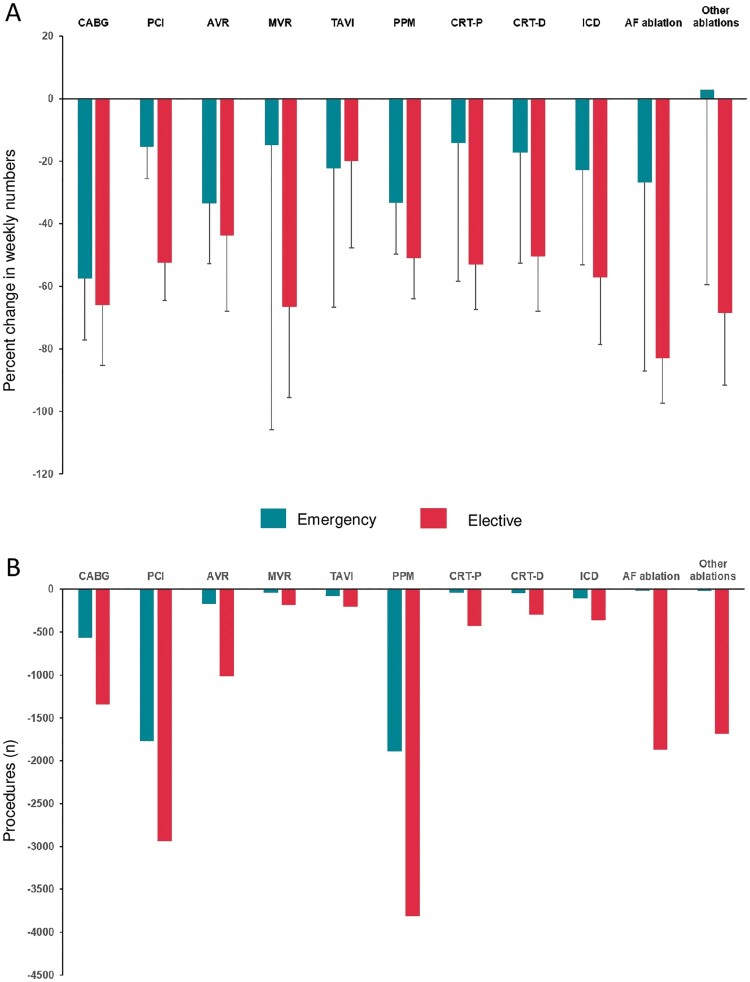
As shown in Figure 3, significant reductions (all P < 0.001) in both emergency and elective hospitalizations were observed for most cardiac operations and interventions in relation to the reference period in 2019. In the case of emergency ablation for conditions other than atrial fibrillation, an overall reduction was also observed (Figure 3), but the weekly rate was highly variable (median change: −7.14%; interquartile range −31.6 to 16.7).
Figure 3.
Number of cardiac operations and interventions during the COVID-19 pandemic according to hospitalization type. Graphs show (A) mean per cent (SD) change in the weekly number and (B) change in the total number of cardiac operations and interventions during the 3 months of lockdown, according to hospitalization type (emergency or elective). In (A), changes in relation to the same time period in 2019 were all significant (P < 0.001), for both emergency and elective hospitalizations. In the case of emergency ablation for conditions other than atrial fibrillation, but weekly rate was highly variable (median reduction: −7.14%; interquartile range −31.6 to 16.7). AF, atrial fibrillation; AVR, surgical aortic valve replacement; CABG, coronary artery bypass graft; CRT-D, cardiac resynchronization therapy-defibrillation; CRT-P, cardiac resynchronization therapy-pacing; ICD, implantable cardioverter-defibrillator; MVR, mitral valve replacement; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; TAVI, transcatheter aortic valve implantation.
Myocardial infarction and heart failure
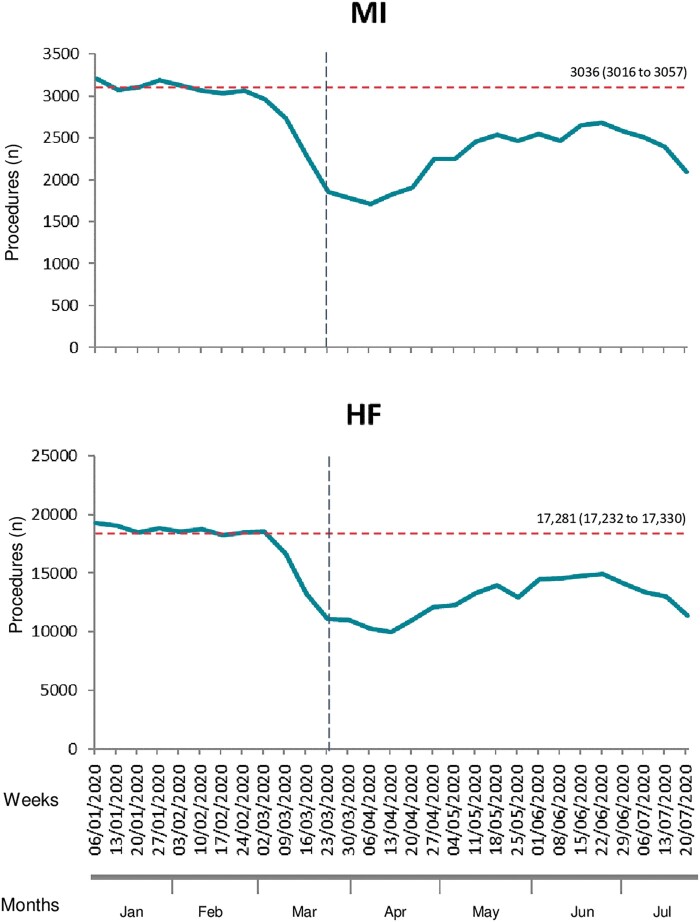
As in the case of cardiac operations and interventions, the decline in hospitalizations for MI and HF also began on the week of 2 March 2020, ∼2 weeks before announcement of the lockdown (Figure 4). The greatest reduction in weekly rates for MI and HF hospitalizations were observed on the week of 6 April 2020 (45% and 42%, respectively). Weekly rates began to return towards 2019 levels by the week of 13 April 2020 for MI and 20 April for HF. By the week of 20 July, weekly rates remained below 2019 levels for both MI (27%) and HF (−33%).
Figure 4.
Hospitalizations for myocardial infarction and heart failure in England during the COVID-19 pandemic. Graphs show weekly numbers of hospitalizations. Dashed horizontal lines indicate the mean weekly number of hospitalizations during the reference period in 2019. Mean (95% CI) are shown above the lines. The black, vertical, dashed line marks the announcement of the national ‘lockdown’, on 23 March 2020. Changes in weekly rates in relation corresponding weeks during the reference period in 2019 were all statistically significant (P < 0.001).
From 7 January 2019 to 26 July 2020, there were 227 257 hospitalizations for MI and 453 799 for HF. Over the 3 months of lockdown, there was a reduction in hospitalizations for MI from 50 508 during the reference period in 2019 to 39 473. Similarly, there was a reduction in hospitalizations for HF from 224 650 in the 3-month reference period in 2019 to 161 592 during the 3 months of lockdown (Table 1). In terms of per cent change, hospitalizations decreased by 27% (95% CI 27–27) for MI and by 28% (95% CI 28–28) for HF. Changes in the total number of hospitalizations for MI and HF were statistically significant (P < 0001). Changes in weekly rates during the 3 months of lockdown in relation the reference period in 2019 were also statistically significant (P < 0.001).
Discussion
This study explores the nationwide impact of the COVID-19 pandemic on the delivery of cardiac operations and interventions. The main finding was a dramatic reduction in the number of cardiac operations and interventions undertaken during the ‘first wave’. Over the 3 months of lockdown, there were 63% fewer operations and interventions than in the same period in 2019. These changes occurred in parallel with nearly 11 000 fewer hospitalizations for MI and over 63 000 fewer hospitalizations for HF. These findings are consistent with those of Mohamed et al.,8 who also used HES data. The present study adds further data on the nature of the hospitalization (emergency or elective), hospitalizations for MI and HF, as well as the types of cardiac ablation procedure and cardiac devices.
Rates of cardiac operations and interventions began to fall in advance of the announcement of the lockdown, mirroring the situation reported in the USA.15 The inflexion point of the weekly rate curve occurred in the 2nd week of March. These changes are likely to reflect increasing public awareness of the COVID-19, most likely triggered by reports of severe acute respiratory syndrome coronavirus 2 in China and Northern Italy. In addition, an NHS declaration of a Level 4 national incident in England on 30 January 2020,2 prepared hospitals for the pandemic. The lowest weekly rates of cardiac operations and interventions occurred in April 2020. Cardiac ablation for atrial fibrillation was the worst hit, followed by other ablations, mitral valve replacements, and coronary artery bypass surgery. For most operations and interventions, a gradual recovery was observed after 13 April. By late July 2020, none had returned to levels observed in the reference period in 2019. Over the 3 months of lockdown, there were 21 038 fewer operations or interventions, compared to the same period in 2019 (Figure 5).
Figure 5.
Per cent reduction in weekly number of cardiac operations and interventions during the COVID-19 pandemic. Graph shows mean percent (SD) reduction in the weekly number of cardiac operations and interventions during the 3 months of lockdown. AF, atrial fibrillation; AVR, surgical aortic valve replacement; CABG, coronary artery bypass graft; CRT-D, cardiac resynchronization therapy-defibrillation; CRT-P, cardiac resynchronization therapy-pacing; ICD, implantable cardioverter-defibrillator; MVR, mitral valve replacement; PCI, percutaneous coronary intervention; PPM, permanent pacemaker; TAVI, transcatheter aortic valve implantation.
We found substantial reductions in hospitalizations for MI and HF. This is consistent with data from the USA showing that during the early phase of the pandemic, cardiac catheterization laboratory activation for ST-segment elevation MI decreased by 38%.13 Braiteh et al.14 also reported a drop of 41% in admissions for acute coronary syndromes in New York State. In a nationwide survey in Italy reported a 47% reduction in HF hospitalizations during the pandemic.7 Similar reports emerged from China.12 As to the causes for the reductions in hospitalizations for MI and HF, a change in the incidence of cardiac disease during the COVID-19 pandemic is an unlikely explanation. More likely is that fewer patients attended hospital, perhaps because of fear of contagion.
As well as a decline in emergency patient attendances as a cause of reduction in cardiac operations and interventions, we should also consider reductions in elective hospital capacity. In this respect, most hospitals redeployed cardiac surgeons and cardiologists away from their specialties to deal with COVID-19 patients. Hospital beds, intensive care unit beds as well as operating theatre and cardiac catheterization laboratory capacity were also re-directed to deal with COVID-19 patients.2 The British Cardiovascular Intervention Society had also recommended that PCI should be used instead of coronary artery bypass grafting in order to reduce inpatient stays.16 This is likely to contribute for our findings of more marked reductions in coronary artery bypass grafting and valve surgery, compared to PCI and transcatheter aortic valve implantation. The shortage of intensive care beds, which are required for all patients undergoing cardiac surgery, is a continuing challenge.
We observed significant reduction in both elective and emergency hospitalizations during the lockdown period. This is perhaps not surprising, given the observed reduction in the number of hospitalizations of patients with MI and HF. This is also consistent generalized reduction in attendances to hospital observed by others.5–7 Further studies are needed to determine to what extent the ‘excess deaths’ reported in national figures are due to underprovision of cardiac operations and procedures.
The operations and procedures described herein are for patients with conditions that carry a major threat to survival and quality of life. In this regard, there is a 44% mortality in 1 year for untreated symptomatic severe aortic stenosis17 and a 22% mortality in 1 year for severe untreated mitral stenosis.18 With respect to MI, West et al.19 found that in England, the 30-day all-cause mortality rate for hospitals performing PCI on >25% of ST-elevation MI patients was almost double that of hospitals performing it on more than 75%. The survival benefits of cardiac device implantation, including pacemakers, cardiac resynchronization therapy, and implantable cardioverter-defibrillator therapy have also been clearly established.20 It follows that not undertaking these operations or procedures or delaying them is likely to translate into poor patient outcomes.
The fluid nature of the pandemic makes it difficult to predict the long-term impact of the COVID-19 pandemic on the delivery of cardiac operations and interventions. Within the time window of the present study, none of the cardiac operations or interventions returned to ‘baseline’ levels by late July 2020. Whilst the repercussions from other ‘waves’ are likely to be less acute, a less acute but more sustained reduction may well exceed the impact observed during the ‘first wave’, particularly over the winter months.
Limitations
This study has several limitations. Importantly, it is based on an administrative rather than on a clinical database. Whilst this approach is rich in numbers, it is scant in clinical detail. Nevertheless, an administrative database is more apt to capture hospitalization episodes more reliably than a clinical database. We cannot reliably model what may happen in the long term, as the pandemic may involve additional ‘waves’. As this dataset only captures in-hospital activity, we cannot quantify out of hospital activity, such as out of hospital cardiac arrests and events which did not necessarily lead to a hospitalization.
Conclusions
The ‘first wave’ of the COVID-19 pandemic has led to a substantial reduction in the number of cardiac operations and interventions undertaken in England. These findings, which are consistent with studies from other countries, pose a challenge to the provision of healthcare to patients with cardiac conditions, during and after the pandemic.
Supplementary material
Supplementary material is available at Europace online.
Funding
Boston Scientific provided an unrestricted educational grant to fund the Chief Statistician (T.Q.) and had no role in hypothesis generation, study design, data collection, data analyses, data interpretation, or writing of the manuscript. The authors had full access to all data and take responsibility for the decision to publish.
Conflict of interest: none declared.
Data availability
The data underlying this article were accessed from NHS Digital. The summary data generated in this research will be shared on reasonable request to the corresponding author.
Supplementary Material
References
- 1. Moss P, Barlow G, Easom N, Lillie P, Samson A.. Lessons for managing high-consequence infections from first COVID-19 cases in the UK. Lancet 2020;395:e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stevens S, Pritchard A.. Next Steps on NHS Response to COVID-19. NHS England and NHS Improvement. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf (Accessed 19 August 2020).
- 3. Banerjee A, Pasea L, Harris S, Gonzalez-Izquierdo A, Torralbo A, Shallcross L. et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet 2020;395:1715–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW. et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 2020;8:e1003–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A. et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;383:88–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bromage DI, Cannatà A, Rind IA, Gregorio C, Piper S, Shah AM. et al. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail 2020;22:978–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. De Rosa S, Spaccarotella C, Basso C, Calabro MP, Curcio A, Filardi PP. et al. , Società Italiana di Cardiologia and the CCU Academy investigators group. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mohamed MO, Banerjee A, Clarke S, de Belder M, Patwala A, Goodwin AT. et al. Impact of COVID-19 on cardiac procedure activity in England and associated 30-day mortality. Eur Heart J Qual Care Clin Outcomes 2020;doi: 10.1093/ehjqcco/qcaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M. et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020;396:381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kwok CS, Gale CP, Kinnaird T, Curzen N, Ludman P, Kontopantelis E. et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 2020;106:1805–11. [DOI] [PubMed] [Google Scholar]
- 11. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ.. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M. et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv 2020;doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S. et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Braiteh N, Rehman WU, Alom M, Skovira V, Breiteh N, Rehman I. et al. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J 2020;226:147–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH. et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med 2020;383:691–3. [DOI] [PubMed] [Google Scholar]
- 16.British Cardiovascular Intervention Society. Cardiology Services during the Coronavirus Pandemic. http://file:///C:/Users/Owner/Downloads/specialty-guide-cardiolgy-coronavirus-v1-20-march.pdf (Accessed 29 August 2020).
- 17. Shareghi S, Rasouli L, Shavelle DM, Burstein S, Matthews RV.. Current results of balloon aortic valvuloplasty in high-risk patients. J Invas Cardiol 2007;19:1–5. [PubMed] [Google Scholar]
- 18. Pasca I, Dang P, Tyagi G, Pai RG.. Survival in patients with degenerative mitral stenosis: results from a large retrospective cohort study. J Am Soc Echocardiogr 2016;29:461–9. [DOI] [PubMed] [Google Scholar]
- 19. West RM, Cattle BA, Bouyssie M, Squire I, de Belder M, Fox KA. et al. Impact of hospital proportion and volume on primary percutaneous coronary intervention performance in England and Wales. Eur Heart J 2011;32:706–11. [DOI] [PubMed] [Google Scholar]
- 20. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA. et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013;15:1070–118. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were accessed from NHS Digital. The summary data generated in this research will be shared on reasonable request to the corresponding author.