Dear Editor
COVID-19 has caused significant disruption to National Health Service (NHS) services, with resources redirected to combat the virus pandemic1. This has had a knock-on effect on other patient groups, such as those with cancer. There are reports of an increase in the number of avoidable deaths from cancer during the pandemic2. Cancer multidisciplinary team (MDT) meetings form a crucial part of the cancer care pathway. The effects of the pandemic on MDT function need to be explored as this may have direct implications for the quality of a patient’s cancer care.
A service evaluation was used to assess the impact of COVID-19 on cancer MDT function at Leeds Teaching Hospitals NHS Trust in the UK. This is a cancer care provider to 4.5 million people. Mixed methods were employed for analysis of both routinely collected MDT activity data and questionnaires of staff experiences. Three time frames were assessed: period 1, before any impact of COVID-19 (January to February 2020); period 2, full lockdown owing to COVID-19 (April to May 2020); and period 3, recovery when NHS functioning had been reinstated (July to August 2020). The transition intervals between these time periods (March and June) were excluded to ensure clear separation of data.
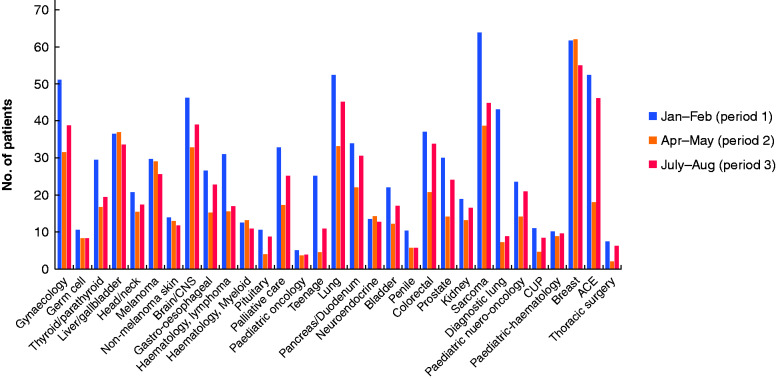
Thirty-one different cancer MDTs were included. Analysis demonstrated a 37 per cent reduction in total number of patients discussed weekly between period 1 (874) and period 2 (548) (Fig. 1). An increase in numbers of patients discussed was observed in period 3 (679), although these were still only 78 per cent of pre-COVID levels. Marked differences were observed between teams, which may reflect different challenges in terms of diagnostic availability, clinical teams or patient groups (Fig. 1).
Fig. 1.
Total number of patients discussed each week in cancer multidisciplinary team meetings
CUP, cancer of unknown primary; ACE, accelerate, coordinate evaluate.
A total of 90 MDT members completed the survey (response rate 35 per cent). The results demonstrated a drop in the number of MDTs continuing with face-to-face meetings (63 per cent), with the majority making changes including limiting attendees, social distancing, use of face masks, and use of virtual software. Feedback on the experience of virtual MDT meetings was that 79 per cent of respondents found them less interactive and 80 per cent reported that communication was disadvantaged. Some 63 per cent of those surveyed believed that IT support was inadequate. Indeed, half of respondents felt that a virtual MDT hampered the decision-making process and 66 per cent believed that COVID-19 had resulted in delays in the diagnosis or management of patients with cancer. The pandemic also affected MDT members directly, with 62 per cent of respondents reporting a drop in meeting attendance because of members self-isolating or COVID-related sickness.
This study provides further insight into the effect of the COVID-19 pandemic on the delivery of cancer services. It represents a service evaluation in one region; implementation of COVID-19 restrictions in other regions and indeed countries may have a different impact. The authors have, however, demonstrated that COVID-19 has had a substantial impact on the cancer MDT meeting process, which is of concern, considering its key role in the provision of cancer care in the NHS. Not only has there been a fall in the numbers of patients discussed, but also the quality of discussion has been hampered. The medium–longer-term impact of this damage to diagnostic and therapeutic interprofessional decision-making in terms of cancer survival has yet to be fully ascertained.
Promisingly, actions in the authors’ hospital Trust have led to upgrades of IT systems and technology in MDT meeting rooms, and also further efforts from the cancer care teams to increase patient support. Further improvements and innovations are, however, needed throughout the NHS and other healthcare systems to mitigate some of the current deficits. The changes to healthcare provision owing to COVID-19 can also be seen as an opportunity to improve patient care and efficiency while maintaining high quality of care3,4.
Disclosure. The authors declare no conflict of interest.
References
- 1. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 2020;107:1440–1449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020;21:1023–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wallis C, Catto J, Finelli A, Glaser A, Gore J, Loeb S et al. The impact of the COVID-19 pandemic on genitourinary cancer care: re-envisioning the future. Eur Urol 2020;78:731–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nunoo-Mensah J, Giordano P, Chung-Faye G. COVID-19: an opportunity to reimagine colorectal cancer diagnostic testing—a new paradigm shift. Clin Colorectal Cancer 2020;19:227–230 [DOI] [PMC free article] [PubMed] [Google Scholar]