Abstract
Objective
In response to the rapidly unfolding coronavirus disease 2019 (COVID-19) pandemic in spring 2020, we developed a caregiver-report measure to understand the extent to which children and families were exposed to events related to COVID-19 and their perceptions of its impact. This article reports on the factor structure and psychometric properties of this measure.
Methods
The COVID-19 Exposure and Family Impact Scales (CEFIS) were developed by a multidisciplinary, multi-institutional team using a rapid iterative process. Data from 1805 caregivers recruited from 28 programs at 15 institutions across the United States were collected from May—September 2020. We examined the underlying structure of the CEFIS using exploratory factor analyses and its internal consistency (Cronbach’s alpha).
Results
Participants reported a range of COVID-19-related events (M = 8.71 events of 25). On the bidirectional 4-point impact scale, mean scores were mostly above the midpoint, indicating a slightly negative impact. Cronbach’s alpha was excellent for Exposure (α = .80) and Impact (α = .92). Factor analysis identified six factors for Exposure (COVID-19 experiences, Access to essentials, Disruptions to living conditions, Loss of income, Family caregiving and activities, and Designation as an essential worker). There were three factors for Impact (Personal well-being, Family interactions, and Distress).
Discussion
The CEFIS has strong factors assessing Exposure to events related to COVID-19, and the Impact of these events on families of children in pediatric healthcare. These initial validation data support use of the CEFIS for measuring the effect of the pandemic.
Keywords: COVID-19, pediatric, children, families, caregivers, trauma
The Coronavirus Disease 2019 (COVID-19) global pandemic is having an unprecedented and enduring impact on society and on children and families worldwide. First identified in Wuhan, China in December 2019, the World Health Organization (WHO) declared COVID-19 a global pandemic on March 11, 2020. Mitigation efforts (e.g., closing schools, canceling large events, stay at home orders) began at that time across the United States. A number of papers and reports in the spring and summer of 2020 described increases in mental health problems associated with the health threats and related restrictions on adults, children and families (Brooks et al., 2020; Gassman-Pines et al., 2020; Patrick et al., 2020). Serious health disparities in the incidence and severity of COVID-19 as well as the differential economic impact of the disease also soon became obvious (Laurencin & McClinton, 2020; Valenzuela et al., 2020).
COVID-19-related disruptions to everyday life and associated increased levels of psychological distress have implications for research and pediatric healthcare delivery. There are many potential impacts to ongoing and newly launching research studies requiring reconsideration of strategies for recruitment, data collection, handling of missing data, delivery of interventions, and targeted outcomes (Mara & Peugh, 2020; Stiles-Shields et al., 2020). Particularly relevant is the impact of COVID-19 as an historical confound in ongoing cross-sectional and longitudinal descriptive and interventional studies. We developed a measure that investigators could use to understand the effect of COVID-19 on pediatric patients and their families, both in clinical work and in research.
The COVID-19 Exposure and Family Impact Scales (CEFIS) are based upon a trauma framework (Substance Abuse and Mental Health Services Administration, 2014) and aim to understand how COVID-19 affects families. Similar to other medical traumas (Price et al., 2016), COVID-19 poses one or more potentially traumatic medical events that may be experienced by individuals within the family and the family as a whole (e.g., being in contact with someone with COVID-19, having COVID-19, being hospitalized, dying). Additional important potential traumas relate to widespread attempts to slow transmission of the disease (e.g., disruptions to education, loss of income and housing, etc.). A trauma model predicts (a) that responses to COVID-19 would be related to the amount of exposure to COVID-19-related events, including COVID-19 illnesses, hospitalizations and deaths, and (b) that the impact of these exposures may span multiple domains of child and family functioning, such as accessing healthcare, emotional health, parenting, and safety.
This article describes the psychometric properties of the CEFIS, a caregiver-report measure intended to assess exposure to and impact of COVID-19 on children and their families.
Materials and Methods
Study Overview
The CEFIS is a caregiver-report measure that was developed by a multidisciplinary, multi-institutional team using a rapid iterative process over 22 days (March 26 to April 16, 2020). At that time, the COVID-19 pandemic was unfolding and affecting most, if not all, American families. Communities were under “stay at home” orders, schools were closing, and broad health and financial implications were emerging. Throughout the summer of 2020, states and local communities mandated varying degrees of restriction and mitigation policies.
Availability of the CEFIS was announced on listservs of relevant divisions of the American Psychological Association, specifically Division 54 (Society of Pediatric Psychology) and Division 38 (Society of Health Psychology) on April 17, 2020. It was also distributed through the National Child Traumatic Stress Network at that time. The CEFIS was registered and made widely available on April 22, 2020 with the National Institutes of Health Disaster Information Management Research Center https://disasterinfo.nlm.nih.gov/search/id:22041.
When registering to use the CEFIS, users agreed to share de-identified CEFIS data on a monthly basis so that we could establish its psychometric properties and refine the measure. Users were provided with a REDCap data dictionary to facilitate this process. Users specified a priori what participant group(s) would complete the CEFIS. No other data about study participants were provided by CEFIS users.
Sample
The data analyzed in this study are from 1805 caregivers who completed the CEFIS in English. The data are from 28 users at 15 sites in the United States. The sites were located in 12 states and represented the east (DE, NY, and PA) and west (CA, OR, and WA) coasts of the United States, as well as the mid-West (KS, MO, OH, IN, and WI), and south (GA). Three users reported on multisite studies. The majority of participants (N = 1,165, 77.4%) were female; 338 (22.5%) were male.1 The patient groups in the site samples were varied (see Table I). One user indicated that they used the CEFIS clinically while all others used the CEFIS in research.
Table I.
Participant Populations and Settings Included in COVID-19 Exposure and Family Impact Scales Validation
| Group | Number of sites/programs | Number of participants |
|---|---|---|
| Hematology/oncology/stem cell transplant | 10 | 212 |
| Pain | 4 | 523 |
| Overweight/obesity | 3 | 208 |
| General pediatrics | 3 | 147 |
| Community-based | 2 | 578 |
| Diabetes | 2 | 35 |
| Irritable Bowel Syndrome | 2 | 37 |
| Newborns | 1 | 51 |
| ICU | 1 | 14 |
Data collection commenced in May 20202 and closed on September 30, 2020 for this report. The study protocol was reviewed by the Nemours Institutional Review Board and it was determined not to meet the criteria for human subjects research (no. 161342).
Measure
The team that developed the CEFIS included seven psychologists, two pediatricians, a nurse, one postdoctoral fellow, and two stakeholder parents of children with medical conditions, representing four hospitals and universities. The first author (A.E.K.) wrote an initial set of novel questions guided by the trauma (Substance Abuse and Mental Health Services Administration, 2014) and medical trauma literature (Price et al., 2016) and using two domains relevant to a medical traumatic stress framework. The first domain aimed to capture Exposure—the family’s experience of a range of pandemic-related events. The second aimed to capture Impact—the perceived effect of pandemic-related events on functioning and distress. The items were refined during an iterative process of review and discussion via email and videoconferences amongst the team members.
The final English version was translated into Spanish by a native Spanish-speaking member of the research team (G.V.), and was certified as an accurate translation based on independent review by a certified medical interpreter. The CEFIS was distributed through the Center for Pediatric Traumatic Stress (CPTS) and is available free of charge in both languages as a REDCap survey;3 registration is required.
The CEFIS opens with the following general introduction.
Please tell us about your family’s experiences during the novel Coronavirus (COVID-19) pandemic. In answering these questions, please think about what has happened from March 2020 to the present, due to COVID-19. By family we mean people who live in your household, extended family, and close friends who you consider “like family.”
Part 1 (Exposure) consists of 25 items (Yes/No responses) that measure the participants’ “exposure” to COVID-19 and related events (e.g., stay at home orders, school closures, changes in housing, changes in employment, difficulty meeting family needs, missing family events, etc.). This includes a cascading set of five items that ask about a family member: (a) being exposed to someone with COVID-19, (b) having symptoms or being diagnosed with COVID-19, (c) being hospitalized, (d) being admitted to an intensive care unit (ICU), or (e) dying. Open-ended fields allow participants to indicate who in the family was affected for each of these five items. Higher scores indicate greater exposure to COVID-19-related events.
Part 2 (Impact) consists of 12 items that measure the impact of COVID-19 on family relationships, emotional adjustment, and wellbeing. Ten items use a 4-point Likert scale rating (Made it a lot better; Made it a little better; Made it a little worse; and Made it a lot worse). These items also included a “not applicable” option. Two items use a 10-point distress scale. Higher scores denote more negative impact/higher distress.
Using timestamp data from REDCap, the mean time for completion of the CEFIS was 8 min, including comments typed in for an optional open-ended question at the end of the measure.
Procedure
Data collection opened in April 2020, although most sites did not start to use the CEFIS before May, pending IRB approvals for their studies and finalization of data use agreements. Prior to the current data analyses, each site was asked to confirm their patient group(s) and to inform us of any changes to the population(s) with whom they used the measure. Most sites had IRB approved study protocols and confirmed that the participant diagnosis/group data provided at registration remained accurate.
Data Analysis
The distribution of responses and missing data for each CEFIS item was first examined using descriptive statistics and graphs. Free-text responses indicating which family member(s) was exposed to COVID-19, had symptoms/was diagnosed, hospitalized, was admitted to the ICU, or died from the illness were tallied in four categories: self/spouse, child, grandparent, or extended family (which included aunt, uncle, cousin, niece, nephew, friend, and coworker).
Exploratory factor analysis (EFA) using principal component analysis (PCA) with varimax rotation with Kaiser Normalization was conducted to determine the underlying structure of the subscales of the CEFIS. Because the CEFIS was developed with two distinct theoretical domains (Exposure and Impact), EFA was conducted for each domain separately. For the Impact EFA, the responses on the two distress scale items were converted from a 10 to a 4-point scale (1 = 1; 2–4 = 2; 5–7 = 3; and 8–10 = 4) for consistency across items. In each EFA, to determine the number of factors to extract, a PCA was first conducted without rotation. The resulting scree plot was examined to determine the number of factors to test in subsequent solutions using varimax rotation. Individual items with factor loadings below 0.40 were considered for removal. The number of items retained, interpretability of the factors, and percentage of variance explained by the solution were each considered in deciding upon a final factor structure (Tabachnick & Fidell, 2019).
The internal consistency of the final scales was calculated using Cronbach’s Alpha/Kuder–Richardson Formula 20 and item-total correlations were examined. The correlations among the final factors were also calculated. Across these steps, item removal or replacement were considered to improve the psychometric properties of the CEFIS.
Analysis of variances (ANOVAs) were conducted to explore differences in CEFIS Exposure, Impact and Distress scores across five participant groups. The compared groups included data reported from ≥2 sites and totaling at least 100 participants (see Table I). We also examined gender differences in CEFIS scores. Finally, Pearson Product Moment Correlations were conducted to establish the association among Exposure, Impact, and Distress scores. SPSS v25 and v27 were used for analyses.
Results
Item Inspection and Distributions
The distribution of responses to the dichotomous Exposure items (Yes/No) is presented in Figure 1. Over 90% of the sample reported experiencing stay at home orders and closed schools. In general, most experienced pandemic-related events such as difficulty obtaining essentials including food, medicine, or healthcare due to COVID-19 precautions. A substantial proportion of caregivers reported direct experience with COVID-19 within their families: exposure to someone with COVID-19 (20.8%), symptoms/diagnosis (18.4%), hospitalization (8.0%), ICU admission (7.0%), and death (5.8%). Figure 2 summarizes the free-text responses related to these specific items. Although parents and children in the family were exposed to or may have had symptoms of COVID-19, grandparents and extended family had a broader range of experiences (exposures) including hospitalizations and death.4 Overall, missing data were minimal for the Exposure items (0.5–2.8%).
Figure 1.
Endorsement of CEFIS Exposure items.
Figure 2.

Who in the family experienced COVID-19? Note. Based on data from 15% of the sample who opted to write in a free text field on the five Exposure items related to COVID-19 exposure, illness, hospitalization, ICU admission, or death.
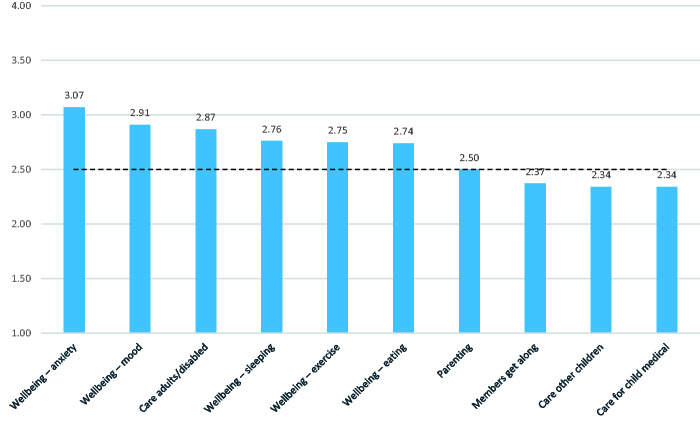
Responses to the Impact items were generally normally distributed utilizing the full range of the 4-point scale (Figure 3). Missing data were within acceptable ranges (5.0–10.0% for most items). However, three items were missing for a larger percentage of families. “Ability to care for your child with [illness/condition]” was not relevant for some samples (e.g., primary care or newborn care settings), and two other items were not applicable to many families (“care for other children” and “care for older adults/people with disabilities”).
Figure 3.
Endorsement (mean values) of CEFIS Impact items. Note. Participants responded on a 4-point scale: 1 = Made it a lot better; 2 = Made it a little better; 3 = Made it a little worse; 4 = Made it a lot worse. Higher scores indicate more negative impact. The range for all items is 1 to 4. The midpoint of the scale (marked above) is 2.5.
The means for most items on the Impact scale were slightly above the midpoint, indicating a mildly negative impact. The impact was rated highest (most negative) on anxiety (M = 3.07, SD = 0.85) and mood (M = 2.91, SD = 0.83). The sample mean for impact on parenting was near the neutral midpoint of the scale (M = 2.50, SD = 0.87) and the mean for COVID-19’s impact on how family members get along tipped slightly positive (M = 2.37, SD = 0.83).
Internal Reliability and Structure of the CEFIS
Exposure
Cronbach’s alpha for the Exposure scale was excellent (α = .80).
The final factor structure for the Exposure items converged in five rotations (Table II).
Table II.
COVID-19 Exposure and Family Impact Scales Exposure Items and Factor Structure
| Exposure items (scale α = .80) | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| We had a “stay at home” order | −0.025 | −0.001 | 0.110 | 0.045 | 0.402 | −0.080 |
| Our schools/child care centers were closed | −0.032 | −0.035 | −0.057 | −0.054 | 0.535 | −0.078 |
| Our child/rens education was disrupted | −0.020 | 0.012 | −0.080 | 0.056 | 0.615 | −0.105 |
| We were unable to visit or care for a family member | −0.008 | 0.134 | 0.128 | 0.053 | 0.535 | 0.176 |
| Our family lived separately for health, safety or job demands | 0.092 | 0.208 | 0.569 | 0.153 | 0.066 | 0.176 |
| Someone moved into (or back into) our home | 0.142 | 0.019 | 0.606 | 0.022 | 0.084 | −0.076 |
| We had to move out of our home | 0.293 | 0.275 | 0.549 | 0.111 | −0.072 | 0.050 |
| Someone in the family kept working outside the home (essential personnel) | 0.092 | 0.038 | −0.138 | 0.089 | −0.011 | 0.809 |
| Someone in the family is a healthcare provider/first responder providing direct care | 0.121 | 0.044 | 0.331 | 0.079 | −0.057 | 0.654 |
| We had difficulty getting food | 0.097 | 0.753 | 0.122 | 0.141 | −0.044 | 0.039 |
| We had difficulty getting medicine | 0.198 | 0.668 | 0.253 | 0.121 | 0.048 | 0.020 |
| We had difficulty getting healthcare when we needed it | 0.133 | 0.683 | 0.180 | 0.066 | 0.127 | 0.014 |
| We had difficulty getting other essentials | 0.071 | 0.753 | 0.028 | 0.063 | 0.039 | 0.051 |
| We self−quarantined due to travel or possible exposure | 0.051 | 0.081 | 0.625 | 0.004 | 0.072 | 0.101 |
| Our family income decreased | 0.026 | 0.101 | 0.112 | 0.788 | 0.066 | 0.028 |
| A member of the family had to cut back hours at work | 0.025 | 0.087 | 0.002 | 0.814 | 0.052 | 0.107 |
| A member of the family was required to stop working (expect to be called back) | 0.103 | 0.148 | 0.203 | 0.692 | 0.029 | 0.012 |
| A member of the family lost their job permanently | 0.214 | 0.131 | 0.482 | 0.325 | −0.033 | −0.018 |
| We lost health insurance/benefits | 0.331 | 0.287 | 0.451 | 0.237 | −0.096 | −0.044 |
| We missed an important family event or it was canceled | 0.024 | 0.037 | 0.017 | 0.016 | 0.518 | 0.123 |
| Someone in the family was exposed to someone with COVID-19 | 0.439 | 0.069 | 0.332 | −0.071 | 0.050 | 0.364 |
| Someone in the family had symptoms or was diagnosed with COVID-19 | 0.612 | 0.088 | 0.185 | −0.072 | 0.088 | 0.245 |
| Someone in the family was hospitalized for COVID-19 | 0.808 | 0.136 | 0.186 | 0.096 | −0.049 | 0.021 |
| Someone in the family was in the ICU for COVID-19 | 0.784 | 0.152 | 0.155 | 0.091 | −0.038 | 0.021 |
| Someone in the family died from COVID-19 | 0.805 | 0.109 | 0.072 | 0.103 | −0.029 | 0.014 |
| Eigenvalue | 5.42 | 1.94 | 1.46 | 1.39 | 1.20 | 1.16 |
| Percent variance accounted for | 21.67 | 7.76 | 5.83 | 5.55 | 4.78 | 4.62 |
| Mean | 0.59 | 0.85 | 0.82 | 1.28 | 4.09 | 0.84 |
| SD | 1.16 | 1.20 | 1.03 | 1.16 | 1.05 | 0.75 |
Note. Factor 1: COVID-19 experiences (α = .78); Factor 2: access to essentials (α = .75); Factor 3: disruptions to living conditions (α = .69); Factor 4: loss in income (α = .71); Factor 5: family caregiving and activities (α = .38) Factor 6: designation as an essential worker (α = .45).
Six factors were identified among the 25 items that accounted for 50.2% of the variance. The factors are: (a) COVID-19 experiences (five items; α = .78). These cascading items measure direct family experiences with COVID-19—exposure, symptoms/diagnosis, hospitalization, ICU admission, and death—in any family member; (b) access to essentials (four items; α = .75). These items assess difficulty in obtaining food, medicine, healthcare, or other essentials; (c) disruptions to living conditions (six items; α = .69). The items on this factor capture the experiences of living separately, moving, permanent job loss, and needing to self-quarantine; (d) loss of income (three items; α = .71). These three items related to temporary loss of employment and reduction in income; (e) Disruptions in family caregiving and activities (five items; α = .38). The items on this factor relate to disruptions in educational activities, caring for other family members, and important family events; and (f) Designation as an essential worker (two items; α = .45). These items capture having a family member who was categorized as an essential worker or was a healthcare provider or first responder providing direct patient care.
Impact
Cronbach’s alpha for the Impact scale was excellent (α = .92). The final factor structure for the Impact items resulted in three factors that converged after four iterations (Table III) and accounted for 73.3% of the variance.
Table III.
COVID-19 Exposure and Family Impact Scales Impact Items and Factor Structure
| Impact items (scale α = .92) | 1 | 2 | 3 |
|---|---|---|---|
| Parenting | 0.320 | 0.774 | 0.099 |
| How family members get along with each other | 0.306 | 0.682 | 0.091 |
| Ability to care for your child with [add illness/condition] | 0.168 | 0.838 | 0.192 |
| Ability to care for other children in your family | 0.181 | 0.863 | 0.137 |
| Ability to care for older adults or people with disabilities in your family | 0.289 | 0.635 | 0.179 |
| Your physical wellbeing—exercise | 0.774 | 0.250 | 0.095 |
| Your physical wellbeing—eating | 0.783 | 0.281 | 0.146 |
| Your physical wellbeing—sleeping | 0.858 | 0.196 | 0.207 |
| Your emotional wellbeing—anxiety | 0.796 | 0.265 | 0.259 |
| Your emotional wellbeing—mood | 0.769 | 0.361 | 0.215 |
| Distress caregiver | 0.384 | 0.159 | 0.806 |
| Distress child | 0.146 | 0.228 | 0.893 |
| Eigenvalue | 6.30 | 1.44 | 1.05 |
| Percent variance accounted for | 52.50 | 12.02 | 8.75 |
| Mean | 2.85 | 2.49 | 5.71 |
| SD | 0.72 | 0.73 | 2.21 |
Note. Factor 1: personal well-being; (α = .86); Factor 2: family interactions (α = .86); Factor 3: distress (α = .76).
The factors are: (a) personal well-being (five items; α = .86) pertaining to physical and emotional wellness of the responding caregiver (i.e., exercise, eating, sleeping, anxiety, and mood); (b) family interactions (five items; α = .86) describing the impact of COVID-19 on family interactions such as parenting and caring for children and elderly family members or family members with disabilities; and, (c) distress (two items; α = .76) comprising the two items that ask about the caregiver’s and the children’s distress.
Intercorrelations Among Exposure, Impact, and Distress and Subscales
The relation between Exposure and Impact is of low magnitude although statistically significant (r = .11, p < .0001). Distress is significantly correlated with both Exposure (r = .40, p < .0001) and Impact (r = .46, p < .0001). Distress is also significantly associated with all of the subscales. Table IV presents the full correlation matrix of the subscales.
Table IV.
Correlation Matrix of COVID-19 Exposure and Family Impact Scales Exposure and Impact Subscales
| Exposure impact | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| COVID-19 experience | Access to essentials | Disruptions living | Loss of income | Family caregiving | Essential worker | Personal wellbeing | Family interaction | Distress | |
| COVID-19 experience | 1 | .361** | .455** | .199** | −.064** | .249** | .095** | .165** | .299** |
| .000 | .000 | .000 | .007 | .000 | .000 | .000 | .000 | ||
| 1,799 | 1,799 | 1,800 | 1,801 | 1,791 | 1,764 | 1,751 | 1,794 | ||
| Access to essentials | 1 | .421** | .329** | .087** | .143** | .117** | .181** | .360** | |
| .000 | .000 | .000 | .000 | .000 | .000 | .000 | |||
| 1,798 | 1,799 | 1,800 | 1,790 | 1,762 | 1,749 | 1,792 | |||
| Disruptions living | 1 | .297** | .074** | .225** | −.043 | .041 | .263** | ||
| .000 | .002 | .000 | .072 | .084 | .000 | ||||
| 1,799 | 1,800 | 1,791 | 1,762 | 1,749 | 1,793 | ||||
| Loss of income | 1 | .125** | .153** | .014 | .008 | .223** | |||
| .000 | .000 | .558 | .731 | .000 | |||||
| 1,801 | 1,790 | 1,763 | 1,750 | 1,793 | |||||
| Family caregiving | 1 | .030 | .077** | .033 | .116** | ||||
| .201 | .001 | .162 | .000 | ||||||
| 1,793 | 1,765 | 1,753 | 1,795 | ||||||
| Essential worker | 1 | .027 | .092** | .087** | |||||
| .252 | .000 | .000 | |||||||
| 1,754 | 1,743 | 1,786 | |||||||
| Personal wellbeing | 1 | .593** | .418** | ||||||
| .000 | .000 | ||||||||
| 1,737 | 1,763 | ||||||||
| Family interaction | 1 | .381** | |||||||
| .000 | |||||||||
| 1,750 | |||||||||
| Distress | 1 | ||||||||
| 1,796 | |||||||||
Note. Correlations are Pearson Product Moment Correlations.
Correlation is significant at the .01 level (two-tailed).
Condition Differences
Five conditions were compared on CEFIS scores—General pediatrics (N = 147), a community-based sample (N = 578), pain (N = 523), hematology/oncology/stem cell transplantation (N = 212), and overweight/obesity (N = 208). ANOVAs indicated statistically significant differences among the conditions on Exposure, F (4, 1,663) = 53.11, p < .001, Impact F (4, 1,458) = 9.32, p < .001, and Distress, F (4, 1,654) = 25.89, p < .001. As is summarized in Table V, there is diversity in scores across the groups. In particular, the community sample had the highest scores on Exposure and Distress.
Table V.
COVID-19 Exposure and Family Impact Scales Scores by Participant Condition
| Hem/Onc/SCT (N = 212) | Pain (N = 523) | Obesity (N = 208) | General pediatrics (N = 147) | Community (N = 578) | F | |
|---|---|---|---|---|---|---|
| Exposure, M (SD) | 6.97 (2.72) | 8.25 (2.86) | 7.70 (2.50) | 7.76 (2.96) | 10.64 (5.43) | 53.11*** |
| Impact, M (SD) | 2.54 (0.67) | 2.83 (0.59) | 2.67 (0.61) | 2.73 (0.65) | 2.62 (0.69) | 9.32*** |
| Distress, M (SD) | 4.95 (2.22) | 5.94 (1.98) | 5.42 (1.86) | 5.05 (2.33) | 6.38 (2.25) | 25.89*** |
Note. Hem/Onc/SCT = Hematology/Oncology/Stem Cell Transplantation. Post-hoc analyses using least significant difference tests show significant differences among most groups for Exposure and Distress. The community sample had significantly higher Exposure (p < .001) and Distress (p < .001) scores than all the other groups. Families of patients with pain issues had significantly higher scores on Impact than the Hem/Onc/SCT and Community (p < .001) and Obesity (p < .01) groups.
p < .001.
Gender Differences
Male caregivers in the sample had significantly higher scores than female caregivers on Exposure (Mmale = 10.43, SD = 5.56; Mfemale = 8.33, SD = 3.69; F = 107.72, df = 1, 1,501, p = .0001). There were no significant differences for Impact (Mmale = 2.59, SD= 0.66; Mfemale = 2.65, SD = 0.65; F = 1.53, df = 1, 1,297, p = .22) or Distress (Mmale = 6.19, SD = 2.50; Mfemale = 5.84, SD = 2.37; F = 2.95, df = 1,494, p = .086).
Scoring the CEFIS
The CEFIS was designed to produce scores for COVID-19 Exposure and Impact. Although the factor structure of the Exposure subscale is interesting and robust, some factor-derived subscales (Disruptions in family caregiving and activities, Designation as an essential worker) have few items and low internal consistencies in our sample.
The total Exposure Score was calculated as a count of “yes” responses. Scores range from 0 to 25 with higher scores indicating greater exposure. The mean Exposure Score in our sample was 8.71 (SD = 4.07, median = 8.00, and range = 0–25).
Use of the mean for the Impact items (with the exception of the Distress items) allows for quick interpretation of the value by dichotomizing at the midpoint (positive valence if ≤ 2.5; negative valence if > 2.5). The mean Impact Score in our sample was 2.68 (SD = 0.65 and median = 2.75).
Based upon the factor structure and response scales for the Impact items, the Distress Score should be scored separately. The Distress Score may be expressed as an average (to estimate family-level distress) or the items can be used individually for caregiver and child distress. The mean for caregiver self-reported distress in our sample was 5.95 (SD = 2.34, median = 6, range = 1–10) and, for caregiver report of child distress, 5.44 (SD = 2.55, median = 6, range = 1–10).
Discussion
With the vast majority of children and families continuing to be impacted by COVID-19 and related efforts to mitigate the pandemic, it is important for researchers and clinicians to have a means of assessing and understanding these events. Besides the very real direct effects of COVID-19 illness on families, the process of accessing healthcare and assuring the wellbeing of children and other family members has challenged caregivers and healthcare providers as they grapple with the uncertainties imposed on them. Understanding the extent to which families are exposed to COVID-19-related events and how they appraise the impact of these events could help guide efforts to assure the delivery of high-quality pediatric healthcare. The impact of COVID-19 on research, particularly in studies where outcomes include psychosocial or behavioral factors, is likely significant, and the historical complications of a pandemic in the course of a study can threaten the validity of its findings.
Consistent with the trauma framework used to develop the CEFIS, EFAs support the Exposure scale as a means of tabulating the extent to which families have experienced potentially traumatic events related to COVID-19. The factors include direct COVID-19 exposures, access to essentials (e.g., food, medication, healthcare), disruptions to the family’s living conditions, losses associated with employment and income, and disruptions in the family’s caregiving and other activities. Scores on the Exposure items reflect a range of exposures, from those that are common (e.g., stay at home orders, schools closed) to those that impacted at least half the sample (e.g., decreased family income, missed events) and some that are less common (e.g., hospitalization, death). Of course, the uncommon exposures (e.g. deaths) are likely to have significant traumatic potential. The correlations amongst Exposure, Impact, and Distress, and the positive associations among the subscales and distress, indicate the clinical utility of the CEFIS as well as the association of outcomes with extent of exposure, consistent with a trauma model. We suggest relying on the Exposure, Impact, and Distress scores and using subscales cautiously, given lower internal consistency values in the Disruptions in family caregiving and activities and the Designation as an essential worker factors.
In addition to examining a family’s experiences related to COVID-19, understanding caregiver appraisal of the impact of the pandemic is important. Results suggest that the CEFIS Impact scale is reflecting valid assessment of impact on personal well-being and family interactions. In general, the most endorsed negative impact of COVID-19 was on caregiver anxiety and mood, a finding that is consistent with other studies of the pandemic (Gassman-Pines et al., 2020; Patrick et al., 2020). This is not surprising but raises questions about how caregivers and families are handling the many stressors associated with the ongoing pandemic and surges in illness and related restrictions. It also emphasizes the importance of attention to caregiver anxiety in delivering care. Given the chronicity and uncertain course of the pandemic, anticipating and appreciating the long-term effects on children, caregivers, and families at large will continue to be important (Christakis, 2020). With half of the families indicating a decrease in income and a quarter reporting problems obtaining essentials and accessing healthcare, CEFIS data could be used to help ensure the responsiveness of healthcare systems to the realities of families’ experiences.
Although the means for most of the Impact items indicated negative consequences, the full range of response options was used for all items, and most was only slightly above the midpoint, indicating signs of positive coping. Many families are demonstrating resilience in coping with the effects of the pandemic. It may be that families were making an effort to build new family routines and rituals and to reframe potential negative effects as more positive. Amongst the items rated most positively are those related to caring for the child with a health condition as well as other children in the family. This is consistent with evidence from The Netherlands that quality of life in families of children with cancer remained consistent between 2019 and 2020 (van Gorp et al., 2020). It is possible that families recruited from healthcare samples are more accustomed to restrictions in their daily lives (e.g., due to their child’s immunocompromised health status) or that families who are treated in centers with psychosocial services and resources may feel more connected to support from their healthcare teams in managing the strains of the pandemic. Alternatively, some of the samples may have included patients with relatively lower levels of health impact (e.g., cancer survivors as opposed to those in active treatment). The community-based groups reported higher levels of exposure to COVID-19-related events than the other groups, and higher levels of distress. This highlights the importance of understanding experiences of COVID-19 in a broad group of families, including those who may not be directly accessing healthcare. Within the healthcare groups, the higher levels of impact in the pain groups suggest the importance of evaluating the impact of COVID-19 with these patients and families.
We developed and distributed the CEFIS quickly and conclude that it is an innovative and helpful caregiver-report measure that can be easily integrated into ongoing and new research studies. The CEFIS can document the extent to which research participants have been exposed to COVID-19-related events. It can also provide data to help understand, or control for, how these exposures and related mitigation efforts may influence psychosocial and behavioral outcomes. The strengths of the CEFIS include the incorporation of both exposure and impact as well as consideration of the impact on the caregiver, child, and family as a whole. The impact scale also allows for indications of resilience as well as distress. The CEFIS was made available quickly (within weeks of major mitigation efforts), and we were able to amass a large sample and establish strong internal consistency of the scales. This article also provides normative data for users. The national sample supports its generalizability in that it allowed for inclusion of participants from a variety of states and localities with different, and changing, mitigation directives.
It will be important to continue the process of establishing the validity of the CEFIS. Convergent- and criterion-related validity will help establish its association with other measures and relevant outcomes, including those with clinical utility. A limitation of the CEFIS data included in this report is the absence of demographic- and disease-related characteristics of participants. Because we moved very quickly to develop and evaluate the CEFIS, we made it as easy as possible for sites to provide deidentified data for these initial analyses. We anticipate that subsequent papers from CEFIS users will provide this important information and perspective on exposure and impact for subgroups of the pediatric population, including examining exposure and impact by patient groups, socioeconomic status, changes over the course of the pandemic, and race and ethnicity. Given the health disparities apparent in the pandemic, the CEFIS has the potential to identify factors that may influence inequities, thus providing avenues for addressing these disparities.
In conclusion, the CEFIS appears to be a psychometrically sound instrument that measures families’ exposure to potentially traumatic aspects of the COVID-19 pandemic and the impact of the COVID-19 pandemic on family functioning. These findings provide the foundation for future research that will examine the convergent and criterion validity of the CEFIS. The CEFIS may also possess clinical utility in that it is brief and can therefore be administered in fast-paced healthcare and other community settings. It can also provide clinicians with valuable information about how the ongoing COVID-19 pandemic has impacted families and guide the focus of clinic appointments and referrals to psychosocial services as needed.
Acknowledgements
We thank Lisa Schwartz, PhD, Alexandra Psihogios, PhD, and Janet Deatrick, PhD for their feedback during the development process. We appreciate the helpful feedback provided by Darlene Barkman and Kerry Doyle-Shannon and thank the sites that contributed deidentified data for this project.
Footnotes
One site did not collect data on participant sex.
A small number of surveys (N = 11) were returned in late April and were combined with the May data. Three surveys returned in early October were combined with September data.
This paper reports on data from the English version of the CEFIS due to a much smaller number of completed Spanish forms at the time this article was prepared.
These free text responses were not required in completing the CEFIS but were reported by 15% of the sample.
Contributor Information
Anne E Kazak, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Melissa Alderfer, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Paul T Enlow, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Amanda M Lewis, Nemours Children’s Health System.
Gabriela Vega, Nemours Children’s Health System.
Lamia Barakat, Children’s Hospital of Philadelphia; Perelman School of Medicine of the University of Pennsylvania.
Nancy Kassam-Adams, Children’s Hospital of Philadelphia; Perelman School of Medicine of the University of Pennsylvania.
Ahna Pai, Cincinnati Children’s Hospital Medical Center.
Kimberly S Canter, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Aimee K Hildenbrand, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Glynnis A McDonnell, Nemours Children’s Health System.
Julia Price, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Corinna Schultz, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Erica Sood, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Thao-Ly Phan, Nemours Children’s Health System; Sidney Kimmel Medical College of Thomas Jefferson University.
Funding
This research is supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (U54GM104941) and the State of Delaware. Additional support is provided by the Center for Pediatric Traumatic Stress (U79SM080048) and the Nemours Center for Healthcare Delivery Science.
Conflicts of interest: None declared.
References
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis D. (2020). Pediatrics and COVID-19. JAMA, 324(12), 1147–1148. [DOI] [PubMed] [Google Scholar]
- Gassman-Pines A., Ananat O., Henley J. (2020). COVID-19 and parent-child psychological well-being. Pediatrics, 146(4), e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurencin C., McClinton A. (2020). The COVID-19 pandemic: A call to action to identify and address racial and ethnic disparities. Journal of Racial and Ethnic Health Disparities, 7(3), 398–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mara C., Peugh J. (2020). Validity of data collected from randomized behavioral clinical trials during the COVID-19 pandemic. Journal of Pediatric Psychology, 45(9), 971–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S., Henkhaus L., Zickafoose J., Lovell K., Halvorson A., Loch S., Letterie M., Davis M. (2020). Well-being of parents and children during the COVID-19 pandemic: A National Survey. Pediatrics, 146(4), e2020016824. [DOI] [PubMed] [Google Scholar]
- Price J., Kassam-Adams N., Alderfer M., Christofferson J., Kazak A. (2016). An integrative model of pediatric medical traumatic stress: An update based on a systematic literature review. Journal of Pediatric Psychology, 41(1), 86–97. [DOI] [PubMed] [Google Scholar]
- Stiles-Shields C., Plevinsky J., Psihogios A., Holmbeck G. (2020). Considerations and future directions for conducting research with pediatric populations during the COVID-19 pandemic. Journal of Pediatric Psychology, 45(7), 720–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA), pp. 14–4884. Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2019). Multivariate statistics, 7th ed. Pearson. [Google Scholar]
- Valenzuela J., Crosby L., Harrison R. (2020). Commentary: Reflections on the COVID-19 pandemic and health disparities in pediatric psychology. Journal of Pediatric Psychology, 45(8), 839–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gorp M., Maurice-Stam H., Teunissen L., van de Peppel-van der Meer W., Huussen M., Schouten-van Meeteren A., Grootenhuis M. (2020). No increase in psychosocial stress of Dutch Children and their caregivers during the first months of the COVID-19 pandemic. Pediatric Blood and Cancer, 68, e28827. [DOI] [PMC free article] [PubMed] [Google Scholar]