Learning points for clinicians
It has been well established in the literature that those with COVID-19 are at increased risk of thrombotic disease, however, research into the best modalities to therapeutically anti-coagulate patients in this population is on-going. This case series highlights concerns with regard to possible increased rates of life-threatening bleeding in this population.
Introduction
Since its emergence in late 2019, COVID-19 (caused by the SARS-CoV-2 virus) has affected over 100 million people worldwide to date.1 COVID-19 has been associated with a significant increase in thrombosis, particularly in patients requiring hospitalization, where it is estimated that up to 33% of patients have thrombotic events. The incidence is higher in those that are critically-ill with COVID-19 as per a recent JAMA paper which showed that in a US registry of patients with COVID-19, thrombotic complications occurred in 2.6% of 229 non-critically ill hospitalized patients and in 35.3% of 170 hospitalized critically ill patients.2
Intravascular coagulation resulting from endovascular disruption is a major contributor to patient mortality.3 As such, several studies, including the REMAP-CAP trial, ATTACC and ACTIV-4 trials are currently investigating the role for empiric therapeutic anti-coagulation in all patients with severe COVID-19 disease. However, therapeutic anti-coagulation is not without risk. This limited case series describes a single center, inpatient service experience of bleeding complications secondary to therapeutic anti-coagulation in the setting of COVID-19 infection, wherein 3 patients over a 6-week period suffered spontaneous bleeding into either rectus sheath or retroperitoneum.
Patient 1
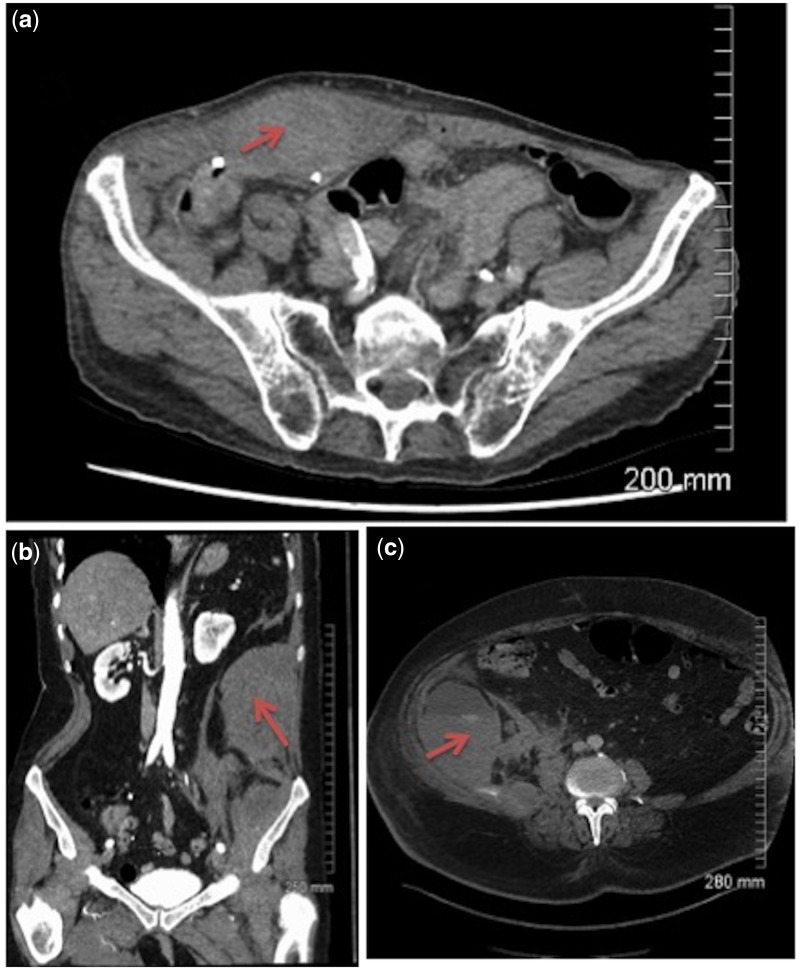
An 88-year-old gentleman with vascular dementia, atrial flutter and ischemic heart disease was admitted to hospital with Covid-19 infection. The patient’s regular oral anticoagulant was switched to a dose-adjusted therapeutic enoxaparin (adjusted for renal function) for the duration of his inpatient stay. On the 10th day of admission, the patient noted new right lower abdominal pain, with evidence of a palpable mass in the right iliac fossa on clinical examination. CT abdomen-pelvis revealed a 9 cm × 4 cm × 3 cm rectus sheath hematoma (Figure 1a), without evidence of extravasation on CT angiography. Anti-coagulation was reversed with protamine sulfate and the patient’s pain resolved over several days.
Figure 1.
(a) (Patient 1)—Heterogenous expansion of the right rectus abdominis muscle on portal venous phase CT images of the lower abdomen, consistent with rectus sheath hematoma. (b) (Patient 2)—Portal venous phase images of left sided retroperitoneal hematoma arising from the iliacus muscle. (c) (Patient 3)—Arterial phase image demonstrating expansion of the left iliacus muscle with evidence of focal hyperdense blush and layering hyperdensity, suggestive of active hemorrhage and subsequent retroperitoneal hematoma formation.
Patient 2
An 85-year-old woman was admitted with respiratory failure secondary to Covid-19 viral pneumonitis. A high d-dimer and worsening hypoxemia prompted therapeutic anti-coagulation pending CT Pulmonary Angiogram (CTPA). CTPA revealed no evidence of Pulmonary Embolism (PE), however, it revealed a left sided retroperitoneal mass. Further imaging of the abdomen with CT angiography revealed a large left retroperitoneal hematoma, with evidence of active extravasation (as seen in Figure 1b, below). This was treated conservatively, with blood transfusion and anti-coagulation was stopped.
Patient 3
A 66-year-old gentleman with obstructive sleep apnea, pulmonary hypertension, chronic obstructive pulmonary disease, atrial fibrillation and elevated BMI acquired nosocomial transmitted Covid-19 infection. The patient’s pre-admission oral anticoagulant was switched to a dose-adjusted therapeutic enoxaparin (adjusted for renal function and BMI) for the duration of his inpatient stay. On the 29th day of his admission, the patient became hypotensive with a corresponding drop in his hemoglobin. A CT angiogram revealed a large retroperitoneal hematoma (Figure 1c, above). The patient was resuscitated with IV fluids, blood products and reversal of anti-coagulation but despite the above he died later that day.
Discussion
Spontaneous rectus sheath hematomas and retroperitoneal hematomas are recognized, though rare, complications of therapeutic anti-coagulation, including low molecular weight heparin4 and carry a mortality of up to 20%.5
Though reports in the literature of these spontaneous bleeds occurring in patients with COVID 19 remain scarce, with isolated case reports of spontaneous bleeding requiring embolization,6 increased prescription of therapeutic anti-coagulation in those at high risk of thrombotic events will almost certainly result in higher rates of bleeding events. Randomized controlled trials establishing risks of bleeding from therapeutic anti-coagulation in patients with COVID-19 are lacking to date, and these authors postulate that there may be an increased bleeding risk in this patient population, whether secondary to direct endothelial damage by the SARS-CoV-2 Virus, or other factors yet to be established. Appropriate weight and renal function based dosing of therapeutic LWMH remains crucial in reducing bleeding risk in all cohorts.
Conflict of interest. None declared.
References
- 1. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [cited 2021 Jan 30]. https://covid19.who.int.
- 2. Piazza G, Campia U, Hurwitz S, Snyder JE, Rizzo SM, Pfeferman MB, et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol 2020; 76:2060–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Salabei JK, Fishman TJ, Asnake ZT, Ali A, Iyer UG.. COVID-19 coagulopathy: current knowledge and guidelines on anticoagulation. Heart Lung [Internet]. 2021; [cited 2021 Jan 30]; http://www.sciencedirect.com/science/article/pii/S014795632100011X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Agarwal S, Lamani YP, Goudar BV, Kalburgi EB, Bhavi BK.. Rectus sheath haematoma secondary to enoxaparin injection—a rare case report. J Clin Diagn Res 2017; 11:PD11–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. González C, Penado S, Llata L, Valero C, Riancho JA.. The clinical spectrum of retroperitoneal hematoma in anticoagulated patients. Medicine (Baltimore) 2003; 82:257–62. [DOI] [PubMed] [Google Scholar]
- 6. Roomi SS, Saddique M, Ullah W, Haq S, Ashfaq A, Madara J, et al. Anticoagulation in COVID-19: a single-center retrospective study. J Commun Hosp Intern Med Perspect 2021; 11:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]