In the Beginning…
The first documented use of telemedicine in orthopaedic surgery was in 1993 between video teleconferencing centers at Tripler Army Medical Center in Oahu, Hawaii and the Kwajalein Atoll in the Republic of the Marshall Islands, connecting two archipelagoes separated by 2200 nautical miles and demonstrating for the first time that telemedicine could be used to provide orthopaedic specialty care across geographical distances [18]. Since then, telemedicine has been used in several aspects of orthopaedic practice, such as remote consultations, postoperative follow-up and rehabilitation, but is not yet standard practice [11, 35, 43, 46].
The most well-established use of telemedicine in orthopaedics is the virtual fracture clinic, pioneered by the Glasgow Royal Infirmary [54]. Standardized, evidence-based protocols are used for a number of stable fractures, and allow many patients to be discharged directly from the emergency department [9, 23, 25, 33, 54]. Patients who might benefit from specialty review are referred to the virtual fracture clinic, where their patient notes and radiographs are reviewed electronically the following day by a multidisciplinary team. Patients then are either discharged directly from the virtual fracture clinic with telephone advice or attend a face-to-face clinic for further review. This has proved to be a clinically acceptable pathway for managing stable injuries and is now used in many orthopaedic departments across the United Kingdom and internationally [32].
The coronavirus disease 2019 (COVID-19) pandemic has forced us to rethink the way that we provide orthopaedic trauma care and new departmental policies have been drawn [1, 7]. Changes initiated by orthopaedic and other surgical specialties are based on guidelines published by the British Association of Oral and Maxillofacial Surgeons in response to the specialties’ high exposure risks [6]. These guidelines aim to reduce the spread of the virus according to four basic principles: personal protective equipment, avoid (contact and transfer of patients), restrict (the number of visits and generation of aerosols), and abbreviate (waiting times and treatment). A critical manifestation of this change has been the rapid extension of telemedicine into many aspects of orthopaedic practice [37, 50]. Video conferencing platforms have allowed departments to perform electronic video consultations for musculoskeletal conditions that do not require in-person evaluation and minimizes viral exposure for both patients and care providers [37, 50].
The Argument
Although telemedicine appears to provide an effective way of continuing vital orthopaedic services throughout the COVID-19 pandemic, a sudden, unregulated increase in remote consultations raises concerns about patient safety, service efficiency, and medicolegal liability. There are some important concerns that must be addressed that are particularly pertinent if physicians are to continue using telemedicine as the pandemic subsides. For example, do we know whether telemedicine is safe, or are we likely to miss some important diagnoses that would have been caught if the patient had been seen in a face-to-face consultation? Furthermore, it is not yet well defined whether there are certain patients who will benefit from telemedicine, and others, who because they may lack access to or familiarity with the technology, may become marginalized as a result.
Along a similar line, it seems likely that some orthopaedic problems will be better suited to telemedicine consultations than others. It is important that we identify these, and more importantly, any that are not. And is telemedicine truly more efficient and cost-effective, or does it depend on the setting in which it is used? It is important that we have answers to these questions going forward so that departments can adapt their use of telemedicine appropriately to their own practices in a way that enhances service efficiency and maintains patient safety.
Essential Elements
We sought to identify all original, prospective (randomized and nonrandomized) and retrospective studies examining the use of telemedicine in trauma and orthopaedic surgery. We searched the terms “orthopaedic” OR “fracture” AND “telemedicine” OR “virtual” OR “telehealth” OR “videoconference” in PubMed and the Cochrane Library between January 1, 2015 and January 5, 2020, yielding 975 articles. Searches were not limited by language.
We followed a Preferred Reporting Items for Systematic Reviews and Meta-analyses-styled search process to analyze results (Fig. 1) [53]. After screening for duplicates using Endnote library (ENDNOTE X3, Thomson Reuters, Carlsbad, CA, USA), we excluded 71 results. We eliminated 845 studies that were not related to the review topic, specifically those about virtual reality, simulation, robotic surgery, three-dimensional printing, and computer-assisted planning. We only included studies in which telemedicine was used for a patient encounter in trauma or elective orthopaedic surgery and assessed patient satisfaction, clinical outcomes, clinical examination or cost-analysis as primary or secondary outcomes.
Fig. 1.
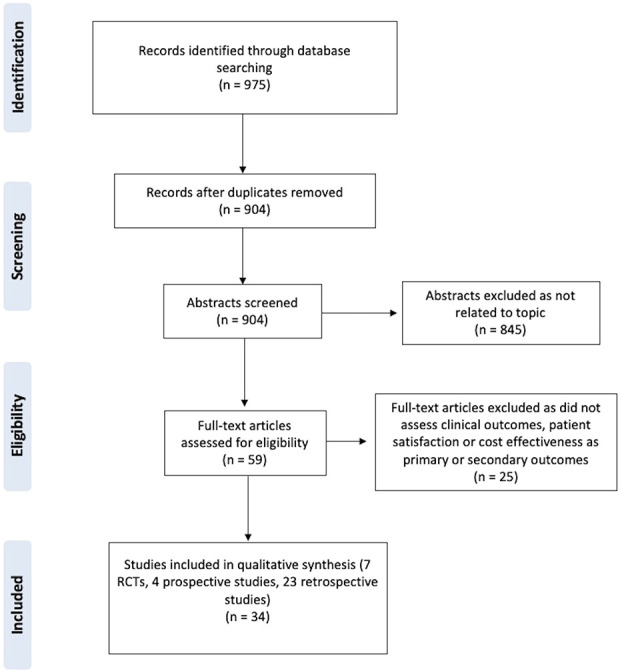
This figure shows the Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram used for our search; RCTs = randomized controlled trials.
We used the World Health Organization (WHO) definition of telemedicine, which is the “delivery of health care services, where patients and providers are separated by distance” [56].
After assessment, we included seven randomized controlled trials [10–12, 35, 47, 48, 55], four prospective studies [19, 27, 45, 49], and 23 retrospective observational studies [2–5, 8, 13, 16, 17, 20–25, 28, 31, 34, 36, 38, 39, 41, 42, 51] with or without control groups, resulting in the inclusion of 34 studies.
We assessed the quality of the evidence of the included studies with the Grading of Recommendations, Assessment, Development, and Evaluations pro-Guideline Development Tool online application using Grading of Recommendations, Assessment, Development, and Evaluations criteria [29]. Based on this assessment, the seven randomized controlled trials included in this review had low-quality evidence and four prospective and 23 retrospective observational studies had very low-quality evidence. The quality of evidence was downgraded for several reasons, most commonly a lack of generalizability and lack of control group. Because of the low number of controlled studies on this topic, we included all studies without controls in the qualitative analysis.
What We (Think) We Know
Clinical Outcomes and Patient Satisfaction
Most evidence for clinical outcomes relating to the use of telemedicine in orthopaedic surgery originates from retrospective studies of virtual fracture clinics, and while they generally demonstrate clinically acceptable outcomes [3–5, 8, 23, 25, 39, 45], most are neither adequately powered nor adequately designed to provide an accurate assessment of safety, with no comparison of diagnoses made (or missed), nor treatments recommended in the virtual setting compared to a controls.
In a retrospective study of 314 patients managed through a virtual fracture clinic pathway for isolated stable Weber B fractures, 99.4% of patients went on to have complete radiological union [3]. Another large study of 618 patients with fifth metatarsal fractures showed no difference in the likelihood of nonunion before and after introduction of a virtual fracture clinic pathway [23]. One prospective observational study looked at outcomes after the introduction of a virtual fracture clinic pathway for the management of stable fractures in 481 patients younger than 16 years of age [45]. One scaphoid fracture was missed on initial radiograph and the patient self-presented to fracture clinic with ongoing pain at 15 days postinjury and went on to heal without complication.
Studies examining the use of video consultations in orthopaedics are less consistent with limited assessment of patient safety, but there is some evidence supporting their utility in remote geographic areas and for those undergoing elective procedures [11, 12, 35, 48]. One randomized control trial evaluated the quality of care provided to 400 patients who were assigned to receive either a video consultation or standard face-to-face appointment in a Norwegian tertiary orthopaedic center with a catchment area of 112,975 km2 [11]. Patients in the video consultation group attended their local hospital and accessed the appointment via a video link with a nurse present, who had been trained in physical examination and casting techniques. There was no difference in re-referrals between groups within 2 years. Of those in the video consultation group, 86% said they would prefer a video consultation for their next appointment compared with 63% of patients who were seen in a face-to-face appointment, with 82% reporting a shorter travel time as the reason for their preference.
In a randomized controlled trial of 52 pediatric patients with stable Type 1 supracondylar fractures, parents were either coached to remove casts at home via video consultation or attended a standard face-to-face appointment for cast removal at 4 weeks postinjury. There was no difference in fracture displacement, ROM, or pain scores between groups at 8-week follow-up. Interestingly, parent satisfaction was almost identical between the two groups until those in the face-to-face group were made aware of the reduced consultation times for patients in the video consultation group, at which point satisfaction decreased in parents allocated to the face-to-face group [48].
The use of video consultations for patients undergoing elective procedures has recently been evaluated in a randomized controlled trial of 66 patients who underwent arthroscopic rotator cuff surgery [35]. No difference in pain scores was reported between the video consultation and face-to-face groups. Patients in the video consultation group had a stronger preference for future video consultations than did those in the face-to-face group. In a randomized control trial of 72 patients who underwent THA, patients either received postoperative care at home via a novel telehealth system or via standard fast-track THA pathway [55]. The authors found reduced length of stay in the telehealth group compared with the standard fast-track group, with no differences in health-related quality of life, anxiety levels, timed up-and-go test results and Oxford hip scores between the two groups.
Clinical Examination
One concern for surgeons using video consultations is the limited ability to examine patients [11]. In a study measuring ROM in 52 elbows, each measurement was recorded in person, through teleconferencing and still-shot photography by two researchers trained in goniometry and showed that teleconference goniometry had a high agreement with clinical goniometry [19]. Teleconference measurements tended to underestimate ROM, which could be explained by the difficulty in identifying bony landmarks without palpating the elbow. However, measurements were still under the clinically accepted range of 5°.
A prospective study used video conferencing with smartphones to assess shoulder function in 51 patients attending a shoulder clinic with a variety of complaints. These patients underwent face-to-face and video consultation in alternating order, with no difference in mean Constant scores between the two methods. [27].
Cost Analysis and Efficiency
Several studies show that telemedicine results in financial savings in areas such as departmental spending, Trust or Clinical Commissioning Group spending (statutory bodies responsible for the planning and commissioning of national health care services for their local area in England), patient travel expenditure, and socioeconomic savings such as less time off work or school [2, 3, 10, 16, 34, 35, 39, 41, 45, 49]. However, although cost and efficiency studies generally can analyze the raw expenditures associated with using telemedicine, and some have compared them with those of in-person clinics, true assessment of cost-effectiveness cannot be done without better evaluation of the risks and potential costs associated with missed diagnoses and/or inappropriate treatments.
Cost analyses of virtual fracture clinics found that they cost less than traditional face-to-face clinics [2, 3, 34, 39, 41, 45] and reduce the number of patients attending traditional fracture clinics [4, 34, 39]. One study showed that a new virtual fracture clinic pathway for stable fractures resulted in fewer patients seen in the traditional fracture clinic, decreased wait times, and an increase in the proportion of patients seen within 72 hours [39]. A further study used a stochastic discrete event simulation model to estimate a cost saving of 38% from a new virtual fracture clinic pathway [2]. In addition, they estimated that their department saved 30 hours of consultant-led specialist services that have gradually been reinvested in the development of subspecialty services. Although using a simulation for cost comparison may result in a less-robust model, it provides the most comprehensive analysis of costs to date, including staff resources (medical, nursing, and administrative) and equipment.
There is difficulty in generalizing cost savings because of variations in the way healthcare systems are funded worldwide. However, one study estimated that participating providers could see three pediatric patients in the virtual fracture clinic in the time it takes to see one patient in the traditional fracture clinic, estimating the savings to the clinical commissioning groups at USD 56,450 and to the hospital at USD 132,920 per year [45]. Norway has a national health service that reimburses patients for public transportation expenditure, constituting 3.2% of the total health budget per year [30]. The cost of establishing a video consultation pathway for a tertiary referral was examined [10]. Additional costs were incurred for establishing the video consultation service, including equipment purchase, initial training, and a nurse at the local site for cast change and suture removal. However, when travel costs and time off work are considered, video consultations costs USD 74 less than face-to-face consultations per patient with no difference in quality adjusted life years between the two groups, and so was found to be cost-effective if 151 consultations are made each year.
Video consultations may have a greater role in postoperative follow-up; patients can be familiarized with the process beforehand and access their video consultation in their own homes, reducing the need for travel. In patients who were randomly assigned to receive video consultation follow-up after elective arthroscopic rotator cuff surgery (accessed via a patient’s smartphone or tablet), appointments were less time-consuming and patients required less time off work than did those in the face-to-face consultation group [35].
Knowledge Gaps and Unsupported Practices
Although the evidence appears to consistently support the use of telemedicine in a range of clinical settings, it must be borne in mind that the GRADE quality for all studies in this review is low to very low. Low-quality studies tend to overestimate the benefit of an intervention, which means that telemedicine may have more risks, fewer benefits, and be less cost-effective than the evidence we have cited in this paper.
Safety is also poorly assessed in the source studies. Many studies make claims of safety based on no adverse events in a small population sample during the assessment period. Larger studies are required to make a confident assessment of safety for the use of telemedicine across a range of clinical settings. Most studies also had relatively short follow-up periods, no follow-up or patient-led follow-up, with patients being advised to attend a face-to-face clinic if they had ongoing symptoms. Therefore, it is likely that there were some delayed diagnoses or late complications not captured by these studies if they occurred beyond the follow-up period, or if patients re-presented to a different hospital.
In addition, many studies in this review used nonvalidated patient satisfaction tools to quantify satisfaction with telemedicine encounters. Factors that influence patient satisfaction can vary widely between patients and attempts to measure this parameter can be misleading, so we have avoided reporting any nonvalidated outcomes here [44]. We have, however, reported differences in satisfaction scores when compared with control groups because we believe this represents a more relevant assessment of patient experience.
Barriers and How to Overcome Them
The main factor restricting high-level, clear evidence for the use of telemedicine in orthopaedic surgery is its limited generalizability. The most consistent and translatable evidence is in support of a virtual fracture clinic pathway for acute injuries. Within the limits of the available evidence, it does appear to be a cost-saving and efficient method of managing a range of stable, nonoperative fractures. Protocols exist that can be adapted to different healthcare systems worldwide [3–5, 8, 23, 25, 39, 45]. However, we recommend careful department-specific cost analysis to ensure that funding is not reduced because of a reduction in face-to-face consultations. Furthermore, stringent and long-term follow-up is required for those patients managed through virtual fracture clinic pathways to provide a more accurate assessment of safety, and we recommend further research in this area.
Video consultations for acute fractures appears to have the most benefit in remote geographic areas, for which face-to-face consultations require substantial travel [11, 12, 38]. For elective follow-up whereby patients can access appointments from home on their tablet or phone, the cost of service provision is minimal, in addition to reducing the length of stay and attendance at face-to-face clinics [35]. This appears to be a promising option for following patients with an uncomplicated postoperative course as elective operations are resumed.
Patients who undergo telemedicine consultations have a higher preference for it in future consultations, and satisfaction with face-to-face consultations is reduced once patients are aware of the benefits of telemedicine [11, 48, 55]. These findings suggest that as patients become more familiar with telemedicine during the COVID-19 pandemic, more patients will prefer remote consultations in the future, and we should have pathways in place to facilitate this. Furthermore, having telehealth support systems that reduce hospital length of stay could help expedite the return to elective operations, in which safeguarding hospital beds for patients with COVID-19 remains a priority [55].
There is difficulty in generalizing cost savings because of variations in the way healthcare systems are funded worldwide. For example, the National Health Service in the United Kingdom funds services using a national tariff, whereby acute services are paid according to activity level. Lower tariffs are paid for nonface-to-face appointments and must be negotiated with clinical commissioning groups. However, video consultations are shorter than face-to-face consultations, which can result in more patients being seen per session and higher tariffs overall [45].
In the United States, physicians are reimbursed less for non-face-to-face consultations. During the COVID-19 pandemic, temporary legislation (such as a 1135 waiver) has been enacted, allowing for telehealth parity during the crisis [14]. The Centers for Medicare and Medicaid Services will reimburse physicians for services rendered through telehealth at the same rate as in-person visits for all diagnoses and easing “originating site” requirements to allow telemedicine for patients not in rural locations or in another healthcare facility. Interstate licensing laws have been suspended, paving the way for states to allow providers to practice telemedicine across state lines [15]. It is unclear whether any of these changes will remain in the long-term, and issues with billing could be a persistent barrier to widespread adoption of telemedicine in private health care systems.
Another factor that may limit wider application of telemedicine within orthopaedic surgery is the inability of surgeons to examine patients. Research on the efficacy of upper limb examinations through video consultations seems to be promising and could be beneficial postoperatively in assessing ROM in patients who undergo uncomplicated elective procedures [19, 27]. However, evidence is extremely limited and further robust research is required in this area, particularly for lower limb and spinal conditions which might be less amenable to remote assessment.
Although familiarity with telemedicine platforms will have increased during the pandemic, concerns regarding data sharing and indemnity may hinder the widespread use of telemedicine in the future. In the United States, several platforms have been developed to be Health Insurance Portability and Accountability Act (HIPAA) compliant, such as American Well (Amwell, Boston, MA, USA), MDLink (MDLink, Ltd, Kingston, Jamaica), Polycom RealPresence (Plantronics, Santa Cruz, CA, USA), and Snap MD (SnapMD, Glendale, CA, USA) and are integrated with the patient's medical record for documentation and billing. In the United Kingdom, National Health Service Digital recommends using Microsoft Teams (Microsoft, Redmond, WA, USA), which is available through mail from the National Health Service [40]. The General Medical Council, a public body that governs the United Kingdom’s medical register, has produced good practice guidance on remote consultations that should be followed, and we recommend that only HIPAA-supported platforms should be used [26].
We also acknowledge that the COVID-19 pandemic and the specialties’ role in its management is rapidly changing, making it difficult to publish recommendations that remain relevant for any length of time. However, given the obvious benefits, it is almost certain that telemedicine will continue to be used in our everyday practice. As the pandemic subsides, the balance of risk benefit to patients will change and the temporary legislative cover and indemnity arrangements that have protected physicians throughout the pandemic will disappear. It is therefore vital that physicians continue to use telemedicine appropriately, in line with evidence-based practice to maximize efficiency, ensure patient safety, and protect ourselves. It is also important to identify where further research is required so that we can work to fill in those gaps in the future.
5-year Forecast
We believe that the use of telemedicine in trauma and orthopaedic surgery will be more widespread in the coming years. Studies suggest that patients who wish to undergo telemedicine appointments rate it very highly, and those who have used it before are more likely to prefer remote consultations in the future [11, 35, 48]. It is important to identify those patients who may benefit, such as patients with long travel times, those with inflexible working hours, those with careers, those who are comfortable with and have access to technology, patients with an uncomplicated postoperative course, and patients older than 60 years with comorbidities (who constitute a large proportion of patients who undergo arthroplasty). As patients become increasingly familiar with telemedicine during the COVID-19 pandemic, the demand for remote consultations will continue to rise and the specialty should be prepared to provide them.
Cost-efficiency will be at the forefront of health service provision for the foreseeable future, with many countries predicted to enter a prolonged period of economic recession because of the COVID-19 lockdown [52]. Orthopaedic departments will be expected to streamline spending if we hope to return to the same standard and volume of service provided before. Developing a novel telehealth pathway for patients who undergo elective surgery that reserves inpatient beds for patients with COVID-19, minimizes the number of hospital attendances by vulnerable patients, and reduces department spending will help facilitate our return to elective operations in the protracted post-COVID-19 period.
Footnotes
Both authors certify that neither he nor she, nor any members of his or her immediate family, has any commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
The opinions expressed are those of the writers, and do not reflect the opinion or policy of CORR® or The Association of Bone and Joint Surgeons®.
References
- 1.American Academy of Orthopaedic Surgeons. Guidelines for Elective Surgery. Available at: https://www.aaos.org/about/covid-19-information-for-our-members/aaos-guidelines-for-elective-surgery/. Accessed May 8, 2020.
- 2.Anderson GH, Jenkins PJ, McDonald DA, Van Der Meer R, Morton A, Nugent M, Rymaszewski LA. Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow hospital. BMJ Open. 2017;7:e014509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellringer SF, Brogan K, Cassidy L, Gibbs J. Standardised virtual fracture clinic management of radiographically stable Weber B ankle fractures is safe, cost effective and reproducible. Injury. 2017;48:1670–1673. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya R, Jayaram PR, Holliday R, Jenkins P, Anthony I, Rymaszewski L. The virtual fracture clinic: Reducing unnecessary review of clavicle fractures. Injury. 2017;48:720–723. [DOI] [PubMed] [Google Scholar]
- 5.Breathnach O, O’Reilly M, Morrissey K, Conlon B, Sheehan E. Electronic referrals for virtual fracture clinic service using the National Integrated Medical Imaging System (NIMIS). Ir J Med Sci . 2019;188:371–377. [DOI] [PubMed] [Google Scholar]
- 6.British Association of Oral and Maxillofacial Surgeons. BAOMS and COVID-19. Available at: https://www.baoms.org.uk/professionals/baoms_and_covid-19.aspx. Accessed May 8, 2020. [DOI] [PubMed]
- 7.British Orthopaedic Association. BOAST - Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html. Accessed May 8, 2020.
- 8.Brogan K, Bellringer S, Akehurst H, Gee C, Ibrahim N, Cassidy L, Rogers B, Gibbs J. Virtual fracture clinic management of fifth metatarsal, including Jones’, fractures is safe and cost-effective. Injury. 2017;48:966–970. [DOI] [PubMed] [Google Scholar]
- 9.Brooksbank K, Jenkins PJ, Anthony IC, Gilmour A, Nugent MP, Rymaszewski LA. Functional outcome and satisfaction with a “self-care” protocol for the management of mallet finger injuries: a case-series. J Trauma Manag Outcomes. 2014;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J. Med. Internet Res. 2019;21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res . 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare 2019;25:451–459. [DOI] [PubMed] [Google Scholar]
- 13.Caffery LJ, Taylor M, North JB, Smith AC. Tele-orthopaedics: A snapshot of services in Australia. J Telemed Telecare. 2017;23:835–841. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed May 7, 2020.
- 15.Centers for Medicare and Medicaid Services. Novel Coronavirus (COVID-19) Medicare Provider Enrollment Relief Frequently Asked Questions (FAQs). Available at: https://www.cms.gov/files/document/provider-enrollment-relief-faqs-covid-19.pdf. Accessed May 7, 2020.
- 16.Cota A, Tarchala M, Parent-Harvey C, Engel V, Berry G, Reindl R, Harvey EJ. Review of 5.5 Years’ Experience Using E-mail-Based Telemedicine to Deliver Orthopedic Care to Remote Communities. Telemed J E Health. 2017;23:37–40. [DOI] [PubMed] [Google Scholar]
- 17.Cottrell MA, O’Leary SP, Swete-Kelly P, Elwell B, Hess S, Litchfield M-A, McLoughlin I, Tweedy R, Raymer M, Hill AJ, Russell TG. Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract. 2018;38:99–105. [DOI] [PubMed] [Google Scholar]
- 18.Delaplain CB, Lindborg CE, Norton SA, Hastings JE. Tripler pioneers telemedicine across the Pacific. Hawaii Med J . 1993;52:338–339. [PubMed] [Google Scholar]
- 19.Dent PA, Wilke B, Terkonda S, Luther I, Shi GG. Validation of Teleconference-based Goniometry for Measuring Elbow Joint Range of Motion. Cureus. 2020;12:e6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans D, Hardman J, Middleton SD, Anakwe RE. Developing a virtual fracture clinic for hand and wrist injuries. J Hand Surg Eur Vol. 2018;43:893–894. [DOI] [PubMed] [Google Scholar]
- 21.Fenelon C, Murphy EP, Galbraith JG, O’Sullivan ME. Telesurveillance: Exploring the use of mobile phone imaging in the follow-up of orthopedic patients with hand trauma. Telemed J E Health. 2019;25:1244–1249. [DOI] [PubMed] [Google Scholar]
- 22.Ferdinandus S, Smith LK, Pandit H, Stone MH. Setting up an arthroplasty care practitioner-led virtual clinic for follow-up of orthopaedic patients. Br J Nurs . 2019;28:1326–1330. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson KB, McGlynn J, Jenkins P, Madeley NJ, Kumar CS, Rymaszewski L. Fifth metatarsal fractures - Is routine follow-up necessary? Injury. 2015;46:1664–1668. [DOI] [PubMed] [Google Scholar]
- 24.Fisher R, Hamilton V, Reader S, Khatun F, Porteous M. Virtual arthroplasty follow-up: five-year data from a district general hospital. Ann R Coll Surg Engl . 2020;102:220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gamble D, Jenkins PJ, Edge MJ, Gilmour A, Anthony IC, Nugent M, Rymaszewski LA. Satisfaction and functional outcome with “self-care” for the management of fifth metacarpal fractures. Hand . 2015;10:607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.General Medical Council. Remote consultations. Available at: https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations. Accessed May 5, 2020.
- 27.Goldstein Y, Schermann H, Dolkart O, Kazum E, Rabin A, Maman E, Chechik O. Video examination via the smartphone: A reliable tool for shoulder function assessment using the constant score. J Orthop Sci. 2019;24:812–816. [DOI] [PubMed] [Google Scholar]
- 28.Gupta S, Jones G, Shah S. Optimising orthopaedic follow-up care through a virtual clinic. Int J Orthop Trauma Nurs . 2018;28:37–39. [DOI] [PubMed] [Google Scholar]
- 29.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol . 2011;64:383–394. [DOI] [PubMed] [Google Scholar]
- 30.Helsedirektoratet. SAMDATA - Spesialisthelsetjenesten. Available at: https://www.helsedirektoratet.no/rapporter/samdata-spesialisthelsetjenesten. Accessed May 2, 2020.
- 31.Holderried M, Schlipf M, Höper A, Meier R, Stöckle U, Kraus TM. [Chances and risks of telemedicine in orthopaedics and trauma surgery] [in German]. Z Orthopadie Unfallchirurgie . 2018;156:68–77. [DOI] [PubMed] [Google Scholar]
- 32.Holgate J, Kirmani S, Anand B. Virtual fracture clinic delivers British Orthopaedic Association compliance. Ann R Coll Surg Engl . 2017;99:51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jayaram PR, Bhattacharyya R, Jenkins PJ, Anthony I, Rymaszewski LA. A new “virtual” patient pathway for the management of radial head and neck fractures. J Shoulder Elbow Surg . 2014;23:297–301. [DOI] [PubMed] [Google Scholar]
- 34.Jenkins PJ, Morton A, Anderson G, Van Der Meer RB, Rymaszewski LA. Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care. Bone Joint Res. 2016;5:33–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kane LT, Thakar O, Jamgochian G, Lazarus MD, Abboud JA, Namdari S, Horneff JG. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg . 2020;29:775–783. [DOI] [PubMed] [Google Scholar]
- 36.Kelly M, O’Keeffe N, Francis A, Moran C, Gantley K, Doyle F, Kenny P. Connolly Hospital Trauma Assessment Clinic (TAC): a virtual solution to patient flow. Ir J Med Sci . 2020;189:425–429. [DOI] [PubMed] [Google Scholar]
- 37.Mauffrey C, Trompeter A. Lead the way or leave the way: leading a Department of Orthopedics through the COVID-19 pandemic. Eur J Orthop Surg Traumatol. 2020; 30:555-557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKerrow M, North J. Clavicle fracture management: A comparison of a tertiary hospital and rural telehealth sites. J Telemed Telecare. 2017;23:856–860. [DOI] [PubMed] [Google Scholar]
- 39.McKirdy A, Imbuldeniya AM. The clinical and cost effectiveness of a virtual fracture clinic service: An interrupted time series analysis and before-and-after comparison. Bone Joint Res. 2017;6:259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.NHS Digital. Messaging tool for NHS to support remote working during coronavirus outbreak. Available at: https://digital.nhs.uk/news-and-events/news/messaging-tool-for-nhs-to-support-remote-working-during-coronavirus-outbreak. Accessed May 11, 2020.
- 41.O’ Reilly M, Breathnach O, Conlon B, Kiernan C, Sheehan E. Trauma assessment clinic: Virtually a safe and smarter way of managing trauma care in Ireland. Injury. 2019;50:898–902. [DOI] [PubMed] [Google Scholar]
- 42.Parkes RJ, Palmer J, Wingham J, Williams DH. Is virtual clinic follow-up of hip and knee joint replacement acceptable to patients and clinicians? A sequential mixed methods evaluation. BMJ Open Qual. 2019;8:e000502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res . 2017;19:e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ring D, Leopold SS. Editorial—Measuring satisfaction: Can it be done? Clin Orthop. 2015;473:3071–3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robinson PM, Sim F, Latimer M, Mitchell PD. Paediatric fracture clinic re-design: Incorporating a virtual fracture clinic. Injury. 2017;48:2101–2105. [DOI] [PubMed] [Google Scholar]
- 46.Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am . 2011;93:113–120. [DOI] [PubMed] [Google Scholar]
- 47.Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma . 2015;29:e139-145. [DOI] [PubMed] [Google Scholar]
- 48.Silva M, Delfosse EM, Aceves-Martin B, Scaduto AA, Ebramzadeh E. Telehealth: a novel approach for the treatment of nondisplaced pediatric elbow fractures. J Pediatr Orthop B. 2019;28:542–548. [DOI] [PubMed] [Google Scholar]
- 49.Sinha N, Cornell M, Wheatley B, Munley N, Seeley M. Looking through a different lens: Patient satisfaction with telemedicine in delivering pediatric fracture care. J Am Acad Orthop Surg Glob Res Rev . 2019;3:e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stinner DJ, Lebrun C, Hsu JR, Jahangir AA, Mir HR. The orthopaedic trauma service and COVID-19 - Practice considerations to optimize outcomes and limit exposure. J Orthop Trauma . 2020;34:333-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sultan AA, Acuña AJ, Samuel LT, Rabin JM, Grits D, Gurd DP, Kuivila TE, Goodwin RC. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: A comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. [Published online ahead of print March 31, 20]. DOI: 10.1097/BPO.0000000000001553. [DOI] [PubMed]
- 52.The World Bank. Pandemic, recession: the global economy in crisis. Glob Econ PROSPECTS. 2020;1:66. [Google Scholar]
- 53.University of Oxford. PRISMA Statement. Available at: http://www.prisma-statement.org/PRISMAStatement/. Accessed May 11, 2020.
- 54.Vardy J, Jenkins PJ, Clark K, Chekroud M, Begbie K, Anthony I, Rymaszewski LA, Ireland AJ. Effect of a redesigned fracture management pathway and ‘virtual’ fracture clinic on ED performance. BMJ Open. 2014;4:e005282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vesterby MS, Pedersen PU, Laursen M, Mikkelsen S, Larsen J, Søballe K, Jørgensen LB. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop . 2017;88:41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.World Health Organization. Global health observatory data 2016: Telehealth. Available at: http://www.who.int/gho/goe/telehealth/en/. Accessed May 8, 2020.


