Abstract
Social determinants of health (SDH) are a valuable source of health information which still are not fully utilized in the clinical space. Knowing that a certain patient has trouble finding transportation, has a potentially hazardous relationship with a family member or close relative, is currently unemployed, or various other social factors would allow providers to tailor treatment plans in a way to best help that patient. However, these SDH must be gathered, represented, and stored in a standardized way before they can be leveraged by informatics tools designed for health providers. This process of translating SDH to standardized clinical entities includes two main steps. The first is a collaborative effort to establish an ontology of medical terminology codes (i.e., ICD, SNOMED, LOINC, etc.) which can be used to uniformly represent SDH as coded concepts. The second is a collaborative effort to use the FHIR standard to create profiles and extensions which will allow FHIR resources to be used to store the coded SDH as clinical entities. Each of these steps has their own complexities that must be considered and accounted for in future efforts to create interoperable clinical informatics solutions which utilize SDH.
Keywords: Social determinants of health, FHIR, interoperability, translational informatics
1. Introduction
The World Health Organization (WHO) recommends “systematically addressing” social determinants of health (SDH) to improve the health of the population as a whole [1]. Although there are many medical schools which provide training regarding SDH [2], some research has noted that current training strategies which “focus on knowing rather than acting” cannot effect the change which will reduce health inequity in a meaningful way [3]. One recent study developed five categories of activities which should be used in tandem to fully address social needs. There, the authors describe the need of developing an interoperable digital infrastructure that can easily share data between healthcare and social care organizations. The study also showed awareness as being just the first step in addressing a social issue; the other four categories include adjustment, assistance, alignment, and advocacy [4].
However, despite their potential implications in health, SDH are not a commonly utilized data source in most clinical workflows. Healthcare providers are already collecting some of this data, although this collection often occurs in an inconsistent and unstructured way. A structured, standardized method of SDH data collection by providers could inform individualized treatment, improve care coordination, and allow for a better population-level understanding of social and health equity for policy makers and healthcare system administrators. There are a few current informatics solutions that have sought to utilize SDH within the healthcare provider’s office [5–7]. However, these are specific use-cases implemented among relatively small populations. In order to increase the population sizes included in such studies, interoperability must be a priority. This will allow cross-site deployment and wider-scale evaluation. Additionally, efforts to give these pilot projects an appropriate scope would provide a more solid foundation for subsequent solutions which will use an increasing breadth of determinant phenotypes. One study of SDOH screening and referrals in 13 of Boston’s community health centers finds a wide variation in practice. Researchers identified 16 domains and 78 dimensions of SDH, but housing was the only domain screened in all participating CHCs [8]. Ensuring the interoperability of SDH solutions requires the translation of SDH data to standard clinical terminologies. In this paper we highlight important considerations which relate to this translation process and aim to provide a foundation for those who will utilize SDH in future interoperable clinical informatics solutions.
2. Background
The translation of SDH to standardized clinical entities is a complicated process due to the sheer number of stakeholders (i.e., government organizations, hospital systems, providers, clinical vocabulary creators, etc.) involved in the standardization of any clinical process. However, the informatics solutions discussed here will provide a high-level overview of the domains that decision-makers in SDH clinical implementation projects require.
2.1. Social Determinants of Health
Ninety percent of human health is influenced by factors outside of the traditional healthcare environment. This includes individual behavior, the physical environment, social circumstances, and others [9]. The WHO defines SDH as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life [1].” These SDH create a complicated web of influences outside of classic biology and genomic makeup that determine a patient’s health. Marmot et al. summarized the relation of SDH to health as follows: “The poorest people have high levels of illness and premature mortality—but poor health is not confined to those who are worst off. At all levels of income, health and illness follow a social gradient: the lower the socioeconomic position, the worse the health [3].” Commonly assessed SDH include employment status, education level, food security, access to health services, housing status, income, discrimination, and social support [9].
2.2. FHIR
The HL7 Fast Healthcare Interoperable Resources (FHIR) Specification is an ongoing effort to create a clinical data standard which enables the kind of interoperability which is necessary to fully utilize informatics tools and solutions. It abstracts clinical data concepts into separate resources. These resources are given unique identifiers which are used to string them together in order to represent all possible clinical scenarios [10]. The goal of the FHIR effort is to make a base set of resources available which cover the clinical scenarios which are common to most implementers. It is a powerful specification because a built-in extension system is also provided which allows more nuanced content to be created through a closely-standardized process.
2.3. Translational Informatics and clinical information modeling
The branch of translational informatics is becoming an increasingly important aspect of health informatics research. As its name suggests, translational informatics is the process of translating data from its original form to another using informatics methods. In health informatics, this has enabled various data sources to be utilized by informatics solutions in the clinical space in a standardized way. A sampling of these data sources includes environmental sensors, wearable health tools, imaging devices, various -omics databases, and detailed drug pharmaceutical research resources [11–14]. In each case, the data is not formatted for clinical use and must be translated to a common clinical data standard before it can be used for interoperable clinical informatics solutions. Because these data are so potentially useful in clinical use, translational informatics has been named as an important milestone in achieving a nationwide learning health system [15].
3. Methods
The standardized representation of social determinants of health as clinical entities is a classic case of translational informatics. This means that it follows roughly the same protocol as other instances of translational informatics.
3.1. Representing SDH as coded concepts
In the United States, the HITECH act requires health providers to use systems that capture specific patient data in standardized formats to enable interoperable data exchange with other systems. These programs require that EHRs use a common clinical data set (CCDS) [16] which use specific medical codes to represent concepts such as race, ethnicity, and preferred language. While these guidelines include only limited requirements in regards to representing other social concepts, the maturation of clinical SDH use should emphasize these same principles. This means that the first step in a translational informatics approach to standardize the clinical use of SDH is to establish a shared ontology which coordinates the representation of any single determinant as a coded concept. This ontology could draw from established clinical coding systems such as SNOMED CT or ICD-10. Creating an ontology would allow separate efforts to build on each other rather than duplicate work.
One study worked to create a compendium of structured, codable social risk factors from common medical terminologies (i.e., SNOMED, LOINC, and ICD) [17]. Subsequent efforts should build upon such efforts in a collaborative way to achieve a robust CCDS of SDH which can be formally adopted and used for future SDH clinical solutions. Another recent effort out of Boston Medical Center focused on generating ICD-10 codes for SDH gathered from eligible patients through a screening process. These codes were used to create referrals for available resources in connection with the determinant(s) identified [18]. Coding the determinants is the first step to various downstream interventions which enhance the value of care provided to patients. Standardizing the coding process with a shared ontology will result in a uniform knowledge source.
3.2. Standardizing the storage of coded SDH
While mapping SDH to clinical codes is an important first step, it must be coupled with a standardized approach to storing them as clinical data entities. The clinical standard most suited for this purpose is the HL7 FHIR specification which is comprised of detailed resources (e.g. Observation, Condition, etc...). These resources require concepts to be coded to medical terminologies. However, each of these base resources would need to be properly extended in order to ensure that different research efforts would be able to maintain interoperability. This extension process relies on FHIR profiles to be created and published which specify how the relevant resource would need to be adapted to accurately represent the specific new data type in question. These efforts are typically undertaken by coordinated working groups and result in a FHIR Implementation Guide (IG) [19]. The IG walks future implementers through the process of creating the specific resources and extensions.
4. Results and Discussion
As is the case in any informatics efforts, collaboration and standardization are the catalysts for real progress. The creation of a robust ontology of SDH medical terminology codes, and the utilization of the FHIR standard for the standardized clinical representation of SDH, is a vast undertaking. The following considerations are additional points which should be carefully considered by those who join this effort.
4.1. FHIR profiles for SDH
A working group, known as the Gravity Project, has recently been announced which will tackle the complex issue of specifying FHIR profiles and extensions which can be used to store SDH [20]. Their coordinated efforts to profile various SDH will result in an IG to assist in the standardized adoption of FHIR resources to represent SDH. Because SDH represent a wide spectrum of information, there are some which have already been profiled because of their connection with other clinical use-cases. For example, smoking status is an SDH which has implications in various clinical contexts. Since it is a commonly-gathered data point, it has already been scoped as a FHIR profile [21]. This example is a good illustration of the fact that SDH are varied and many FHIR profiles may already exist for certain determinants. Care should be taken by researchers to ensure that existing work is built upon and only modified if necessary. These more common determinants can also serve as a valuable starting point while the efforts of working groups for profiling the bulk of other determinants is ongoing.
4.2. FHIR Questionnaire resource for interoperable SDH collection
FHIR can also provide important interoperability and standardization to the process of SDH collection. The FHIR Questionnaire resource is a versatile option for representing SDH-gathering questionnaires or question sets [22]. It allows each question to be internally represented with a corresponding clinical code. SDH have historically been gathered through sets of questions which probe the patient’s lifestyle and other aspects typically associated with SDH. Due to the nature of SDH data, its collection often requires patient self-reporting. For example, although patient addresses are frequently used to infer socio-economic standing from census tracts, ZIP codes, and other community area designations, this method is dependent on survey and census material which is often outdated [23]. To assume that the patient is poor, based on that address alone, would result in incomplete information for that determinant. Since most approaches to clinical SDH gathering will use direct questions to avoid that unreliability, using FHIR Questionnaire resources would allow questionnaires to be used across institutions.
Responses to these questionnaires can be represented as FHIR QuestionnaireResponse resources. While using a FHIR Questionnaire ensures that the SDH are captured as coded concepts, an additional step is necessary to create a profiled FHIR resource for each relevant question response. For example, although a positive response to question on smoking history would result in a corresponding coded SDH within the QuestionnaireResponse, an additional step would be required to create a profiled FHIR Observation resource to represent that information. An informaticist querying for information on that patient’s smoking history will be guided by the smoking status profile and will look for that corresponding resource, not for an obscure response within an QuestionnaireResponse resource. Coding a patient’s smoking history as a FHIR Observation resource would allow for the data to be queried by relevant CDS solutions for all subsequent patient interactions. This method also enables patient-level, system-level, or population-level analysis of both the questionnaires and the unique, standardized clinical concepts.
4.3. Terminology overlap for representing SDH
The creation of an SDH ontology will be further complicated by the fact that there is a high level of overlap between the common medical terminologies. Reconciling this overlap will require collaboration and iterative feedback from relevant stakeholders. However, it is a crucial first step because despite the clinical standardization available through FHIR, the value is lost if the underlying representation of SDH is ambiguous.
5. Conclusion
Clinical informatics is a field which continues to present new opportunities for utilizing nontraditional medical data sources. Combining clinical informatics and translational informatics can be a powerful source of innovation. SDH represent a vast and varied source of data which can have important implications for health services. However, in order to use SDH in a clinical setting, they must be translated to standardized clinical entities. Following our approach will require a collaborative effort to curate a robust SDH ontology and to create the necessary FHIR profiles and extensions to store SDH in the clinical space. As this work moves forward, it will allow health professionals to provide more informed care for their patients and will likely inform later efforts to create new interoperable clinical informatics solutions which use other nontraditional data sources.
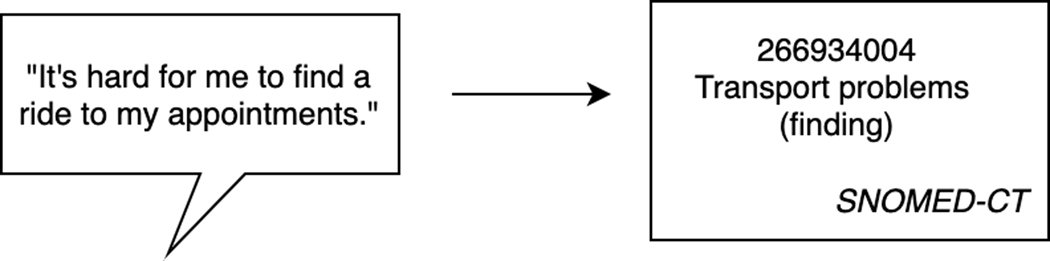
Figure 1.
Example of representing an SDH as a coded concept.
Table 1.
Overlapping terminology codes for representing employment status [17]
| ICD | SNOMED | LOINC | |||
|---|---|---|---|---|---|
| Z56.0 | Unemployment, unspecified | 7348004 | Unemployed | LA 17956–6 | Unemployed |
| Z56.1 | Change of job | 276068009 | Changed job | LAI 7957–4 | Employed full time |
| Z56.2 | Threat of job loss | 266956001 | Dismissed from job | LAI 7958–2 | Employed part time |
| Z56.3 | Stressful work schedule | 360484006 | Loss of job | LA 17959–0 | Homemaker |
| Z56.4 | Discord with boss and | 160905000 | Absenteeism at work | LA 17960–8 | Retired due to |
| workmates | 105496009 | Work maladjustment | age/preference | ||
| Z56.5 | Uncongenial work environment | problem | LA 17961–6 | Retired due to disability | |
6. Acknowledgments
The work of this paper was supported in part by a World Health Organization WHO/PAHO, IS4H joint grant, between the University of Utah in the USA, and the National Institute of Health in Peru.
References
- [1].WHO | about social determinants of health. (2017). Retrieved from https://www.who.int/social_determinants/sdh_definition/en/
- [2].Sharma M, Pinto A, & Kumagal A. (2018). From Making Lists to Making Change. Public Health Post, 1–3. Retrieved from https://www.publichealthpost.org/research/teaching-social-determinants-of-health-making-change/ [Google Scholar]
- 3.Marmot M, Friel S, Bell R, Houweling TA, Taylor S, & Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet, 372(9650), 1661–1669. doi: 10.1016/S01406736(08)61690-6 [DOI] [PubMed] [Google Scholar]
- 4.Bibbins-Domingo K. (2019). Integrating social care into the delivery of health care. Jama, doi: 10.1001/jama.2019.15603 [DOI] [PubMed] [Google Scholar]
- 5.de la Vega Buitron, Pablo, Losi S, Sprague Martinez L, Bovell-Ammon A, Garg A, James T, . . . Kressin NR. (2019). Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Medical Care, 57, S133–S139. doi: 10.1097/MLR.0000000000001029 [DOI] [PubMed] [Google Scholar]
- 6.Kasthurirathne SN, Vest JR, Menachemi N, Halverson PK, & Grannis SJ (2018). Assessing the capacity of social determinants of health data to augment predictive models identifying patients in need of wraparound social services. Journal of the American Medical Informatics Association, 25(1), 47–53. doi: 10.1093/jamia/ocx130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bettencourt-Silva J, Mulligan N, Cullen C, & Kotoulas S. (2018). Bridging Clinical and Social Determinants of Health Using Unstructured Data. Studies in Health Technology and Informatics, 255, 70–74. 10.3233/978-1-61499-921-8-70 [DOI] [PubMed] [Google Scholar]
- 8.Slabodkin G. (2019, May 14). SDOH screening differs widely among community health centers. Retrieved from https://www.healthdatamanagement.com/news/sdoh-screening-differs-widely-among-community-health-centers
- 9.NCHHSTP Social Determinants of Health. (2014, March 10). Retrieved from https://www.cdc.gov/nchhstp/socialdeterminants/faq.html
- 10.FHIR Overview. (2018, December 27). Retrieved from https://www.hl7.org/fhir/overview.html
- 11.Shameer K, Badgeley MA, Miotto R, Glicksberg BS, Morgan JW, & Dudley JT (2017). Translational bioinformatics in the era of real-time biomedical, health care and wellness data streams. Briefings in Bioinformatics, 18(1), 105–124. doi: 10.1093/bib/bbv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geis JR (2007). Medical imaging informatics: How it improves radiology practice today. Journal of Digital Imaging, 20(2), 99–104. doi: 10.1007/s10278-007-9010-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tenenbaum JD (2016). Translational bioinformatics: Past, present, and future. Genomics, Proteomics & Bioinformatics, 14(1), 31–41. doi: 10.1016/j.gpb.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cantor MN (2012). Translational informatics: An industry perspective. Journal of the American Medical Informatics Association : JAMIA, 19(2), 153–155. doi: 10.1136/amiajnl-2011-000588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedman CP, Wong AK, & Blumenthal D. (2010). Achieving a nationwide learning health system. Science Translational Medicine, 2(57), 57cm29. doi: 10.1126/scitranslmed.3001456 [DOI] [PubMed] [Google Scholar]
- 16.2015 Edition Common Clinical Data Set (CCDS) Reference Document. (2018, February 22). Retrieved from https://www.healthit.gov/sites/default/files/ccds_reference_document_v1_1.pdf
- 17.Arons A, DeSilvey S, Fichtenberg C, Gottlieb L. (2018) Compendium of Medical Terminology Codes for Social Risk Factors. San Francisco, CA: Social Interventions Research and Evaluation Network; 2018. Available at: http://sirenetwork.ucsf.edu/tools-resources/mmi/compendium-medical-terminology-codes-social-risk-factors [Google Scholar]
- 18.Slabodkin G. (2019, May 17) Boston Medical Center implements SDOH screening tool in EHR. Retrieved from https://www.healthdatamanagement.com/news/boston-medical-center-implements-sdoh-screening-tool-in-ehr
- 19.FHIR Implementation Guides (2019, January 28). Retrieved from https://wiki.hl7.org/index.php?title=FHIR_Implementation_Guides
- 20.Lovett L. (2019, 21 August) Social determinants of health program Gravity Project joins HL7 FHIR accelerator. Retrieved from https://www.mobihealthnews.com/news/north-america/social-determinants-health-program-gravity-project-joins-hl7-fhir-accelerator
- 21.StructureDefinition-us-core-smokingstatus (2019, June 19) Retrieved from https://www.hl7.org/fhir/us/core/StructureDefinition-us-core-smokingstatus.html
- 22.Resource Questionnaire - Content. (2018, December 27) Retrieved from https://www.hl7.org/fhir/questionnaire.html
- 23.Shavers VL (2007). Measurement of Socioeconomic Status in Health Disparities Research. Journal of the National Medical Association, 99(9), 1013–1023. [PMC free article] [PubMed] [Google Scholar]