Abstract
Background:
Around the world, snake bite envenomation remains an underreported human health hazard. Envenomation can cause local and systemic complications, especially when there is a lack of antivenom availability. Although there are established guidelines regarding snake bite management acute care, there is a paucity of data regarding surgical intervention and the plastic surgeon’s role treating this unique patient population.
Methods:
A review was conducted identifying relevant published articles involving snake bite management and treatment in PubMed and EMBASE.
Results:
One hundred ten articles were identified and 77 met inclusion criteria. Snake bite envenomation can result in complications that are dependent upon a variety of variables. The literature has shown the best field treatment to be timely transportation to the nearest medical facility, along with antivenom administration. The cytotoxic, hemotoxic, and neurotoxic effects of venom can cause a variety of local soft tissue and systemic complications. Surgical interventions such as fasciotomies, wound debridements, skin grafts, and tissue flaps may be necessary in these patients to optimize functional and aesthetic outcomes. Disparities in access to care in resource limited settings are discussed.
Conclusions:
Global health disparities and insufficient antivenom distribution create an inequality of care in snake bite patients. Plastic surgeons have an important role in managing acute and chronic complications of snake bite envenomations that can lead to improved patient outcomes.
INTRODUCTION
Snake bite envenomation remains a worldwide health hazard.1 The World Health Organization estimates that of the 5.4 million snake bites that occur annually, 2.7 million are venomous with a 5% fatality rate (137,880 deaths per year).1 Although mortality following envenomation is low, secondary complications are common, ranging from 10% to 44%.2 These include, but are not limited to local tissue pain, swelling, cellulitis, infection, skin necrosis, coagulopathy, compartment syndrome, muscle contracture, and various physical deformities.3 The wide range in complications are primarily attributed to a lack of antivenom availability, healthcare systems infrastructure and patients’ socioeconomic status.1,4,5
Once a snake bite occurs, the first level of management is in the field.1,6,7 This is followed by triage and provision of acute care in a hospital setting with the goal of limiting the local and systemic effects of envenomation.3 Although envenomation is well studied in regards to field treatment and management of acute symptoms, there is a paucity of the literature regarding the management of secondary complications in this select patient population, making treatment guidelines unclear. Resulting wound complications can have permanent and debilitating features such as muscle and tendon contracture, gangrenous and necrotic tissue, osteomyelitis, and chronic wound infection, some of which may require reconstruction.8 To adequately care for patients affected by snake bites, plastic surgeons must be well versed in the acute and long-term management of these wounds.9,10
This article first provides a background and overview of current medical and surgical management in snake bite envenomation. The broad applicability of this practical review is meant to be inclusive and comprehensive for a global plastic surgery audience that might find themselves in a variety of practice environments and scenarios. We also discuss the disparities in global health as related to epidemiology of snake bites and resultant treatments.
METHODS
A scoping review was conducted identifying relevant published articles using the search terms “management” AND “snake bite” AND “surgery.” Initial search of PubMed found a total of 87 review articles, and 44 additional articles via an EMBASE search of “management” AND “snake bite” AND “surgery” along with referenced articles from relevant initial data base search. After removing duplicates, 110 articles were screened for inclusion (Fig. 1). Of these articles, 33 were excluded as they were not evaluating some form of snake bite management. Authors manually evaluated the articles’ suitability for the review and removed any that did not meet inclusion and exclusion criteria. Inclusion criteria included articles that were published between the years 2000 and 2020, published in English, and referenced either some form of snake bite management or factors that attribute to treatment disparities. Articles of all evidence levels were reviewed (Table 1).
Fig. 1.
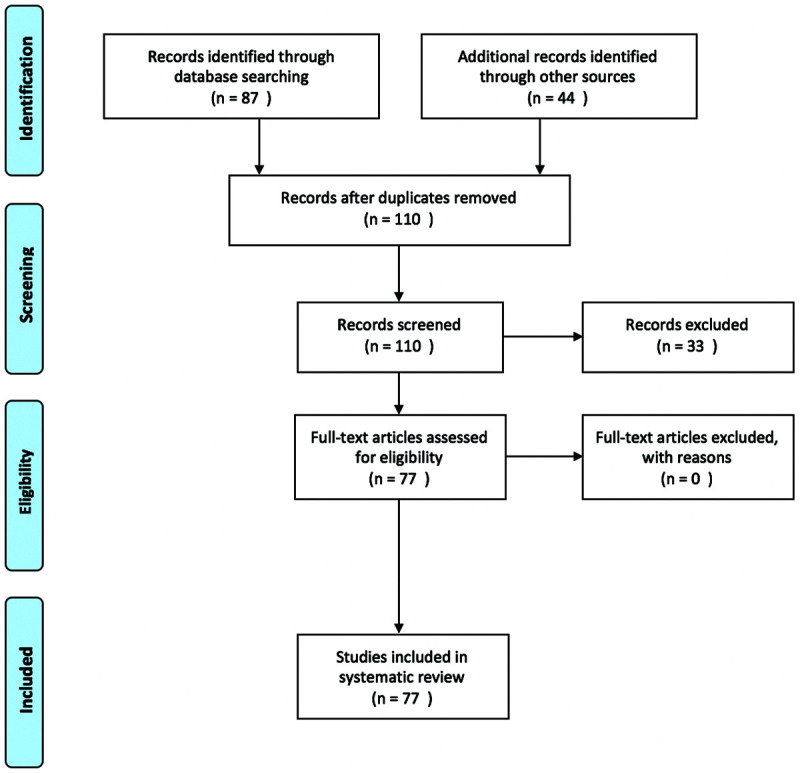
PRISMA flow diagram.
Table 1.
Literature Review
| Article | Type of Study | No. Subjects | Purpose | Results |
|---|---|---|---|---|
| Abbey et al, 201511 | Retrospective review | 90 | Evaluate epidemiology of snake bites in west Texas along with clinical manifestations | 51 were upper extremity, 38 lower extremity. 31 patients had complications and 20 needed surgery. 88 patients received a median of 10 vials antivenom. |
| Ahmad, 200912 | Review | N/A | Evaluate current level of understanding of envenomation among healthcare workers | Suggests training to create better awareness as there is a lack of understanding consequences of snake bites and administration of antivenom. |
| Anz et al13 | Review | N/A | Evaluate management of envenomation injury to the upper extremity | Close observation, thorough physical examination and measurement of intracompartmental pressure are good indicators to if surgical intervention is needed post envenomation. |
| Ashwin et al, 201014 | Case report | 1 | Evaluate rare case of ocular snake bite injury and management | Combination of surgical and laser treatment successfully treated ocular injury. |
| Aziz et al15 | Review | N/A | Assess current management in animal bites | Evidence does not support use of empiric antibiotic. If infection is observed (cellulitis, abscess), culture and specificity. Antivenom is first line. If no response, not an adequate amount administered. |
| Balaji et al, 201516 | Case report | 1 | Evaluate post snake bite cellulitis leading to infected open dislocation of first MCP joint | After debridement, fixation and soft-tissue coverage patient made complete recovery. |
| Bonasso et al, 201517 | Case report | 1 | Evaluate case of osteonecrosis at IP thumb joint post rattlesnake envenomation | One month after the second debridement, patient returned and x-ray showed erosion of IP joint. Patient went back to the OR for further debridement, path confirmed osteonecrosis. |
| Bozkurt et al18 | Retrospective review | 12 | Evaluate 12 hand envenomations from Vipera bite, how to minimize functional impairment and maximize rehabilitation | 3 cases had groin flaps, 2 had full thickness grafts, 3 had thenar flaps, 3 cross finger flaps. This study preferred the use of flaps on volar side of hand along with full-thickness graft on dorsal side of hand as long as bone was not exposed. |
| Campbell et al, 200819 | Retrospective review | 114 | Evaluate cases of pediatric snake bites and evidence-based treatment guidelines | No difference in infectious complications whether or not patient treated with empiric antibiotic. Only 2 patients required fasciotomy. Evaluated based on clinical examination findings and measurement of compartmental pressure |
| Chattopadhyay et al, 200420 | Retrospective review | 58 | Evaluate indications for surgical treatment in snake bites | More antivenin was needed in individuals who required surgery. 28% required local debridement for necrosis, only 5 required skin graft, 1 above knee amputation. |
| Cheng et al, 201921 | Case report | 1 | Evaluate dorsal toe flap post cobra envenomation of great toe | Wound reconstructed using lateral toe pulp flap is a quick 1 step procedure. Great option for distal dorsal defects of great toe. Graft showed initial congestion but survived. |
| Chippaux, 201122 | Meta-analysis | 314,078 | Evaluate the true public health concern and economic impact in sub-Saharan Africa | Reported numbers are not a true representation of the actual epidemiological data as many fatalities, complications and noncomplicated snake bites are underreported. Incidence was inversely correlated with population density, male agricultural or pastoral laborers were most at risk. |
| Corneille et al, 200623 | Retrospective review | N/A | Compare treatment: ovine Fab antivenin (FabAV), antivenin crotalidae polyvalent or no antivenom | FabAV is preferred in treating crotalidae envenomation as there are decreased allergic reactions, high rates of limb salvage, little bleeding but frequent coagulopathy. |
| Correa et al24 | Retrospective review | 150 | Evaluate use of antivenom, antibiotics, and diagnostics in pediatric population in SW Texas | Morbidity is rare, low envenomation score gave no antivenom, high score gave antivenom. 4 patients required surgery. 52 received CroFab, 1 allergic reaction. |
| Cumpston, 201125 | Systematic review | N/A | Evaluate the role of fasciotomies in crotalinae envenomation in North America | Immediate CroFab antivenom should be administered in suspected envenomations. |
| Dart and McNally, 200126 | Review | N/A | Evaluate efficacy and safety of antivenom in the United States | Newer antivenoms are more stable, predictable and less likely to cause a reaction. |
| Dijkman et al, 201627 | Case report | 1 | Evaluate case of Crotalus durissus envenomation | Treatment with cross polyvalent antivenom primarily used for Crotalus durissus can be used to successfully treat Crotalus durissus unicolor. |
| Edgerton and Koepplinger10 | Review and case report | 1 | Evaluate previous envenomation treatment and outcomes to positively affect patient care | Critical to receive critical care and antivenom administration if envenomation occurs. Surgical intervention necessary in the development of compartment syndrome, tissue necrosis, or compromised vascularity. |
| Farrar et al, 201228 | Retrospective review | 82 | Evaluate pediatric populations response to CroFab antivenom | Overall, pediatric population tolerated CroFab well. 6/82 developed an allergic reaction but all reactions were mild and did not affect course of treatment. |
| Fry et al, 200329 | Systematic review | 0 | Evaluate global state of snake envenomation | The snake bite crisis is ignored and underreported. Poor disbursement of antivenom and lack of adequately trained medical personnel. Continues to be an economic burden. |
| Gold et al30 | Review article | N/A | Overview envenomation diagnosis, treatment and management | Timely transport to hospital is imperative to be further assessed by a medical professional. |
| Greene et al, 201731 | Case report | 1 | Evaluate case of Cryptelytrops albolabris envenomation on distal thumb | Patient successfully managed with 2 rounds of 5 vials antivenin specific for the viper. Important in identifying proper snake to treat appropriately with antivenin |
| Griffin et al32 | Systematic review | NA | Evaluate the different options and techniques available to correct soft-tissue defects of the upper extremity | One must consider the nature of the defect and type of flap that is needed to properly restore form and function for optimal outcomes. |
| Hamdi et al, 201033 | Case report | 1 | Evaluate compartment syndrome post adder envenomation to thenar eminence | Documented increased compartment pressure. Received fasciotomy. Patient had full recovery. |
| Heiner et al, 201334 | Retrospective review | 17 | Evaluate clinical significance of antivenom in the US military personnel in Afghanistan | All bites to extremity. 10 cases received polyvalent antivenom for coagulopathy (no adverse effects). 6 received additional antivenom. None required surgery. All had resolution of coagulopathy, swelling, and pain at discharge. |
| Hernandez et al35 | Retrospective review | 72 | Evaluate the management and outcome of pediatric population in KwaZulu-Natal, South Africa | Early time to treatment and antivenom administration will reduce need for surgery. Hemoglobin <11 mg/dL, leukocytosis, INR >1.2 were associated with fasciotomy independently. |
| Rha et al, 201536 | Retrospective review | 111 | Evaluate validity and safety of surgical management in snake bite patients | Group A received only debridement and group B received antivenom and debridement. Of the 10 patients in A, 2 developed cellulitis, 1 skin necrosis resulting in skin graft. Of 36 pts in B, 19 cellulitis, 2 skin necrosis one of which received a graft. CS found in 1 patient in which fasciotomy and graft were performed. |
| Hon et al, 200537 | Case report | 1 | Evaluate patient who had to stop antivenom due to development of anaphylaxis | Patient subsequently developed compartment syndrome and required fasciotomy. |
| Hsieh et al38 | Retrospective review | N/A | Evaluate factors that contribute to complications post envenomation | Use of antivenin, antibiotics, and timely presentation to hospital post envenomation improved outcomes. Bites by Taiwan cobra lead to more complications, tissue necrosis, infection and necrotizing fasciitis. |
| Hsu et al39 | Retrospective review | 136 | Evaluate factors responsible for compartment syndrome post envenomation | Post envenomation patients should be observed for at least 48 h. Increased WBC and AST levels indicate higher likelihood of compartment syndrome. |
| Ince and Gundesliog, 201440 | Retrospective review | 23 | Evaluate Viperidae bites, single-center review | Only 1 needed surgical intervention. Sufficient antivenom must be used to reduce further complications. |
| Irion et al, 201641 | Retrospective review | N/A | Evaluate management post envenomation and need to transfer to tertiary care hospital | If rural hospital has enough experience and antivenom availability, it can be medically managed. |
| Jeng et al, 200742 | Prospective | 44 | Evaluate patients with soft-tissue loss who received integra for complex reconstruction | Long-term follow-up showed persistence of integra collagen fibers in healing wound, also stated, “large volume loss wounds benefited from the ability to fill voids with multilayered applications.” |
| Juckett and Hancox6 | Systematic review | N/A | Evaluate management and treatment of envenomations | At the hospital, a thorough workup and use of a grading scale I–IV to guide antivenom administration. Evaluation of fasciotomy is necessary but rare. |
| Kang et al43 | Retrospective review | 49 | Evaluate the use of free flaps in lower extremity reconstruction | With careful planning and proper debridement, free flaps provide a great choice for wound coverage and restoration of form and function in the lower extremity. |
| Karlo et al, 201144 | Retrospective review | 93 | Evaluate envenomations in Croatian North Dalmatia region | Most common symptoms were pain and swelling (93), then hematomas and ecchymosis (87) and compartment syndrome (8). |
| Kim et al9 | Retrospective review | 59 | Evaluate if fasciotomy is necessary post envenomation with elevated compartment pressure | Found 10.8% of all their snake bite victims needed fasciotomy. All had intracompartmental pressures measured. Mean of 49, range of 37–88. |
| Kleinschmidt et al45 | Review | 373 | Evaluation of acute adverse events associated with CroFab antivenom | 2.7% of patients had adverse reactions, most common was rash, severe adverse events in 1.1% of patients. |
| Korambayi et al7 | Prospective | 112 | Evaluate multidisciplinary approach to envenomation, specifically plastic surgery | Hyperbaric oxygen improves outcome of snake bite management in extremities. 50 cellulitis, 24 with CS, 38 needed soft-tissue coverage of extremity, 77 involved LE and 35 involved UE. |
| Laohawiriyakamol et al46 | Retrospective review | 58 | Evaluate role of surgery in pediatric snake bite patients | Surgery is needed post envenomation, especially in cobra bites that more commonly cause tissue necrosis. Surgery in 13/58 patients. Common procedures: serial debridement, skin grafting. 1 toe amputation. CS suspected in 2 patients. |
| Larson et al, 201647 | Retrospective review | 32 | Compare those who did and did not receive CroFab following Agkistrodon bite and subsequent tissue loss | CroFab provided patient better comfort and pain control. No difference was observed in tissue loss between the groups. |
| Lavonas et al, 202045 | Double-blinded clinical trial | 72 | Evaluate Fab antivenom vs placebo in copperhead envenomation | Men recovered better than women; however, treatment with Fab was similar in terms of recovery across all subgroups. |
| Lee and Yao, 201049 | Case report | 1 | Evaluate rare case of stenosing flexor tendon tenosynovitis post envenomation | Patient would have significantly benefited from immediate administration of antivenom as missed diagnosis caused patient to present 1 wk post envenomation. |
| Liu et al, 201850 | Basic science | N/A | Evaluate use of ELISA and lateral flow strip assays to diagnose envenomation | Could be of use in ED when determining what antivenom to administer. |
| Mao et al52 | Retrospective review | 183 | Evaluate management of Naja atra snake bite | Median dose of antivenom to treat symptoms was 10 vials. Debridement in 74 patients, fasciotomy in 46, finger or toe amputation in 7. Most were not operated on until 3.5 d post envenomation. |
| Mao et al, 201652 | Retrospective review | 112 | Identify bacteriology of Naja atra snake bite wounds | 86 developed suspected infections, 61 of which required surgery due to tissue necrosis, finger/toe gangrene, necrotizing fasciitis. From most to least common bacteria found: Marganella morganii, Proteus spp., Aeromonas hydrophila, Pseudomonas aeruginosa, Providencia spp. |
| Mao et al, 202053 | Retrospective review | 186 | Evaluate Protobothrops mucrosquamatus envenomation and factors that lead to surgical intervention | Bite to finger or toe should be carefully inspected for tissue necrosis and infection as prompt surgery is needed to salvage. |
| McBride et al, 201754 | Case report | 1 | Evaluate compartment syndrome post eastern diamondback envenomation | Treatment with multiple doses of CroFab and transfusions corrected coagulation values after patient had compartment syndrome in the right leg with “delayed recurrent coagulopathy.” |
| Michael et al55 | Cross-sectional multicenter study | 374 | Evaluation of knowledge and management of healthcare professionals in Nigeria | 52.9% had “adequate” overall knowledge of snake bites. Clinicians need more education and training for treating snake bites. |
| Mohan et al, 201956 | Review and case report | 1 | Evaluate the efficacy of plasmapheresis and its use in post snake bite management | Plasmapheresis should be used as an adjunctive treatment post envenomation. |
| Nazim et al3 | Retrospective review | 25 | Evaluate snake bite envenomations | Envenomation patients should be comprehensively reviewed and observed for a minimum of 24 h at any sign of envenomation. |
| Norris et al57 | Case report | 1 | Evaluate case of patient who died from coral snake bite | Coral snake antivenom that is commercially available along with proper medical treatment would have greatly benefited this patient. |
| Palappallil, 201558 | Retrospective review | 313 | Evaluate use of antibiotics post envenomation. Study in Kerala (developing country) | Classically if infection was suspected, ampicillin alone was used or in combination empirically with cloxacillin prophylactically, or piperacillin or tazobactam for established infections. |
| Poryazogulu et al, 201259 | Case report | 7 | Evaluate case reports of 7 pit viper envenomations in military personnel | Hematologic complications were the most likely abnormality, grafts and flaps were utilized in cases where primary wound care was not sufficient. |
| Pulimaddi et al, 201760 | Retrospective review | 100 | Evaluate AKI in snake bite victims along with incidence, clinical symptoms, and outcomes | Early presentation to hospital along with adequate antivenom and supportive care offers a favorable outcome for these patients. Of all patients, 86 recovered, 6 died, 8 developed chronic kidney disease. |
| Ramirez et al, 201561 | Case report | 2 | Evaluate pediatric finger envenomation resulting in chondrolysis and epiphysiolysis | One patient received PIP joint fusion and other managed conservatively. |
| Rha et al62 | Retrospective review | 111 | Evaluate safety and efficacy of surgical management post envenomation | 46 of 111 required debridement. Of those who received antivenom, 19 developed cellulitis, 2 skin necrosis, one of which needed a skin graft, and 1 had CS which required fasciotomy and skin graft. |
| Ruha et al8 | Retrospective review | 450 | Evaluate database to explore epidemiology, clinical course, and management of snake bites in North America | 54% LE injury, 27% of which had no shoes on. Common symptoms were erythema, edema. 84% of bites received antivenom. |
| Severyns, 201863 | Case report | 1 | Evaluate case of Bothrops lanceolatus envenoming and its subsequent secondary complications | Surgical intervention (fasciotomy and debridement) is needed for established necrotizing fasciitis with empiric third generation cephalosporins and ICU management. |
| Sharma et al, 200864 | Review and case report | 1 | Evaluate venomous snakes in India with a focus on levantine viper case report | Identification of the snake is essential as traditional antivenom used for the “big 4” is not effective with the levantine viper. The correct antivenom is essential to successfully manage these bites. |
| Shaw and Hosalkar, 200265 | Retrospective review | 19 | Evaluate if high-dose antivenom is effective in children | In children, adequate doses of antivenom should be administered before considering surgical treatment as 16/19 avoided surgery. Of the 3 that needed surgery, there were 2 debridements and 1 fasciotomy. |
| Strickland et al66 | Basic science | N/A | Evaluate the phenotypic variation within rattlesnake venom | Variation within venom blurs true classification of venom dichotomy. |
| Su et al, 201667 | Retrospective review | 28 | Evaluate ways to predict patient who will need surgery in Naja atra envenomation | Necrotizing fasciitis was main reason for surgery. If patient presents with skin ecchymosis or need for high dose antivenom, they should be looked at for early surgical intervention. |
| Taieb et al68 | Randomized controlled trial | 98 | Evaluate current healthcare worker knowledge of treating snake bites before and after information course | Statistically significant improvement in knowledge along with correction of common treatment myths. |
| Tincu et al, 201769 | Case report | 1 | Evaluate case of rattlesnake bite in which DVT and compartment syndrome developed | If high clinical suspicion for CS, early intervention is needed to improve outcome in these patients. Rattlesnake venom can cause prothrombotic state, leading to a DVT and CS. |
| Tochie et al5 | Review | N/A | Evaluate disease burden and management of snake bites in Cameroon | Poor disease surveillance, lack of patients who seek medical attention, lack of widely distributed antivenom and high cost. Need to revise policy, price of antivenom, and education and medical centers. |
| Tokish et al, 200170 | Retrospective review | 164 | Evaluate the management of snake bite envenomations in southern Arizona | Determined incision and suction, tourniquets, and cryotherapy increase risk of needing surgery. Recommend the use of an objective envenomation scale to guide treatment and antivenom use. |
| Toschlog et al, 201371 | Review | N/A | Evaluate the best form of surgical management in North American crotalinae envenomations | With the use of antivenom, urgent surgical intervention in crotalinae envenomation is rare. |
| Tucker & Josty72 | Case report | 1 | Evaluate the case of adder bite to the hand | Compartment pressure was 48 in thenar eminence and 59 in thumb. Warranted fasciotomy due to compartment syndrome. 5 mo later have full recovery and movement of all digits. |
| Türkmen and Temel, 201673 | Retrospective review | 37 | Evaluate criteria for fasciotomy post envenomation | Fasciotomy should not be performed unless intracompartmental pressure measurement is greater than 55 mmHg. |
| Wagener et al, 201774 | Prospective audit | 164 | Determine offending bacteria of infection secondary to snake bite | Common bacteria found in wounds were Enterobacteriaceae and enterococci. Strongly advocate for good antibiotic policy at the hospital. |
| Wu et al, 200175 | Case report | 1 | Evaluate the case of snake bite with Vibrio vulnificus infection | 79-y-old man had snake bite on palm of the hand. Presented with rapidly enlarging bullae, compartment syndrome necrotizing fasciitis, and septic shock. Had debridement and several reconstructions. |
| Yildrim et al, 200676 | Retrospective review | 20 | Evaluate if plasmapheresis in snake bite patients is beneficial | Plasmapheresis should be considered for treatment of snake bit management as it is safe and effective. Rapidly resolved hematologic parameters that were off. |
| Yuenyongviwat et al, 201477 | Review and case report | 1 | Evaluate Calcific myonecrosis in post snake bite patient | 66-y-old patient who was bit by Malayan pit viper at 14 y old has had 10 y history of progressively enlarged mass in the left leg. Broke through the skin when became infected. Excision followed by antibiotics was treatment. |
| Zengin et al, 201378 | Retrospective review | 37 | Evaluate if plasma exchange is beneficial in acute treatment of envenomation | Plasma exchange should be considered in ED for rapid resolution of patient symptoms, especially in hematologic abnormalities, limb salvage. |
AKI, acute kidney injury; AST, aspartate aminotransferase; CS, compartment syndrome; DVT, deep vein thrombosis; ICU, intensive care unit; INR, international normalized ratio; IP, interphalangeal; MCP, metacarpophalangeal; OR, operating rooml PIP, proximal interphalangeal joint; UE, upper extremity; WBC, white blood cell.
RESULTS
No level I randomized control studies involving snake bite envenomation were identified. This review also found relatively few level II studies classified as nonrandomized control trials or prospective studies. The majority of articles were classified as below level II quality of evidence and included retrospective reviews, systematic reviews, and case reports. One meta-analysis was identified.
Venom
Common symptomatology can be identified across snake species.3 Presenting symptoms of any envenomation can include generalized weakness, numbness, paresthesia, and pain.79 A snake’s venom is composed of a variety of enzymes and proteins that are responsible for both local tissue damage and systemic manifestations. Each species has altering levels of gene expression that control which proteins and enzymes are expressed. For example, certain species’ venom primarily expresses metalloproteinases, which can lyse membranes and cellular adhesions, causing rubor, calor, tumor, and tissue necrosis.6,80 This can present clinically as tachycardia, petechia, confusion, vomiting, disseminated intravascular coagulation, acute renal failure, shock, and compartment syndrome.6 Commonly, laboratory values show depleted fibrin levels, anemia (intravascular hemolysis), thrombocytopenia, and elevated BUN, creatinine, and prothrombin time/partial thromboplastin time.10
Alternatively, gene expression of either alpha protein or phospholipase A2 can give the venom a neurotoxic effect in which presynaptic or postsynaptic blockade prevents signal transmission. This can lead to visual disturbance (ptosis and diplopia), dysphagia, diaphoresis, peripheral nerve palsy, diminished reflexes, and in severe cases, respiratory depression, and paralysis.6,66
Field Management
When in the field, accurate assessment of the wound is difficult, as there are no immediate differentiating symptoms between a snake bite with or without envenomation.81 The focus of first aid has shifted from field treatment to timely transport to the nearest medical facility.30 Once at the hospital, further assessment, additional resources, and treatment options can be offered.
After sustaining a snake bite, victims and bystanders should move out of the snake’s striking distance and take a picture of the snake, if possible.2,6 The victim’s airway, breathing, and circulation should be assessed as envenomation can affect these vital functions within minutes.10 Current recommendations for field treatment include limiting the victim’s activity while lying them flat and keeping the bitten extremity immobilized at heart level.82 If local swelling, erythema, or pain are progressing, the affected extremity can be elevated as long as no systemic symptoms are present.81 Importantly, the medical facility should be called in advance to allow enough time for the antivenom to be prepared or transferred as it is not universally stocked.6 Antivenom is costly and not available in most low-middle income countries (LMICs).
Common misconceptions about snake bite management abound. The use of a tourniquet, thought to reduce the return of venom to the central circulation, actually restricts essential blood flow to the affected tissue, increasing local edema and potentiating the venom’s local effects.82 A venous tourniquet can be beneficial when kept below a pressure of 30 mm Hg (2 fingers under band), limiting spread of systemic absorption; however, improper application limits its use in the field.6,13 Wound compression, which involves wrapping the affected extremity distal to proximal at an optimal pressure of 55 mm Hg, has been shown to be error prone and is not recommended.57 Initial treatment of wound incision and suction or suction alone was thought to withdraw a portion of the venom load, thus limiting the quantity of absorbed venom; however, studies have shown it can actually worsen patient outcomes and is therefore no longer recommended.83 Application of medicinal herbs, chemicals, and intense scrubbing/cleaning of the wound is also not recommended.1
Antivenom
The mainstay of medical management is antivenom administration. Antivenom is made up of purified IgG antibodies from venom injected into animal hosts. Adverse reactions range from mild (rash, diarrhea, diaphoresis, and pain) to severe (anaphylactic shock, bronchospasm, angioedema, and hypotension).45 A hospital should be aware of the most common envenomations to obtain the most needed antivenoms. Antivenom can be stored in lipophilic or liquid form and has to be refrigerated.84 If an adverse reaction is detected upon administration, immediate antivenom discontinuation is followed by antihistamines, corticosteroids, or a combination of both should follow.12,84 Epinephrine can be used in severe cases with bronchospasm, angioedema, and hypotension.84
Antivenom is indicated when there is a progression of local symptoms. This includes swelling that is either rapidly expanding, encompassing more than half an extremity, or present at the digits or toes.85 Antivenom is also given at any sign of systemic illness including any laboratory derangements (Table 3).10,45,84,20,21 Studies have found early intervention (within 4 hours of envenomation) along with higher doses of antivenom offer more favorable patient outcomes and a decreased risk of requiring surgical intervention.6,35,86,23,24 However, antivenom can be given within 24 hours of envenomation and still provide beneficial effects.6,87 As there is no maximum dose of antivenom—the medication should be given until clinical and laboratory derangements are corrected.1,85,87 Some studies report the use of an envenomation scale to aid in this decision.24 Initial infusion of antivenom should occur at a rate of 2 ml/min or diluted bolus with 5–10 ml/kg of isotonic saline administered at a fixed rate over 1–2 hours.84,87,25 With a slower rate of antivenom infusion, adverse effects are less likely to occur.45,88,27
Table 3.
Venom
| Primary Affect | Effect at Cellular Level | Clinical Symptoms | Altered Laboratory Values |
|---|---|---|---|
| Hemotoxic | Metalloproteinases and other cytotoxic enzymes lyse membranes and cellular adhesions, leading to rubor, tumor, and tissue necrosis | Tachycardia, petechia, confusion, vomiting, disseminated intravascular coagulation, acute renal failure, shock and compartment syndrome | Depleted fibrin levels, anemia (intravascular hemolysis, thrombocytopenia, elevated BUN, elevated creatinine, elevated prothrombin time, elevated partial thromboplastin time |
| Neurotoxic | Inhibit neurotransmission signals in different ways to disrupt neurologic function. Alpha protein binds post synaptic nicotinic acetylcholine receptors. Mojave toxin irreversibly binds presynaptic nerve receptors, inhibiting the influx of calcium ions. Phospholipase A2 inhibits neuronal activity at the presynaptic terminal | Paresthesia, numbness, visual disturbance (ptosis, diplopia), dysphagia, diaphoresis, diminished reflexes, peripheral nerve palsy, respiratory depression, paralysis | Patient can have hematologic effects as mentioned in “hemotoxic” row, however, less commonly altered laboratory values and more neurological sequelae |
Acute Hospital Treatment
Upon arrival to the hospital, intravenous access should be obtained and fluids administered, this is provider and patient dependent, as 500–1000 ml bolus of lactated ringers or normal saline is typically infused in adult patients.84 Current literature does not recommend prophylactic antibiotics, but if signs of infection are present, cultures and sensitivities of the wound and blood should be obtained to target the offending bacteria.15 A full patient workup should be performed, along with irrigation and careful inspection of the wound.10,83 The border of swelling and erythema should be marked and observed every 30 minutes to monitor progression.3 Consistent monitoring of clinical symptoms along with serial laboratory draws (CBC, CMP, coagulation studies, and liver function tests) should be performed every 2–3 hours to evaluate possible progression of systemic complications.6,8
An identified envenomation with primarily hematological sequelae and no signs of secondary complications should be monitored for a minimum of 12 hours to ensure no development or progression of symptoms.8 If bitten by a snake and neurological symptoms are present, a minimum observation period of 24 hours is required with specific neurological monitoring to ensure no further progression of symptoms (Table 4).3,90
Table 4.
Acute Hospital Treatment
| Symptoms | Observation | Laboratories | Hospital Course | Complications |
|---|---|---|---|---|
| Hematologic | Monitor at least 12 h. | CBC | Patient receives supportive treatment and appropriate amount of antivenom. If secondary sequelae are absent, there is no progression of local symptoms and local erythema/swelling is controlled with no proximal progression, patient can be discharged with follow up laboratory tests | If new symptoms arise (fever, SOB, dizziness, nausea, vomiting), return to hospital for further evaluation and treatment |
| CMP | ||||
| Coagulation studies | ||||
| Liver function tests | ||||
| Neurologic | Monitor at least 24 h. | CBC | Patient receives supportive treatment and appropriate amount of antivenom. Specific monitoring of neurological functioning is performed. If secondary sequelae are absent, there is no progression of local symptoms and an improvement of neurological symptoms, patient can be discharged with follow-up laboratory tests | If new symptoms arise (visual disturbance (ptosis, and diplopia), dysphagia, diaphoresis, peripheral nerve palsy, diminished reflexes, and in severe cases, respiratory depression and paralysis), return to hospital for further evaluation |
| CMP | ||||
| Coagulation studies | ||||
| Liver function tests | ||||
| Respiratory function tests |
If compartment syndrome is clinically suspected, action needs to be taken in a timely manner as ignoring the need for a fasciotomy can lead to further tissue necrosis, ischemic complications and even loss of limb.9,39 The patient will present with pain that is disproportional to examination, diminished peripheral pulses and paresthesia, increased firmness upon palpation, or have a sustained intracompartmental pressure greater than the normal values of 0–8 mm Hg.13,86,90,23,31 In children, more accurate signs and symptoms that identify acute compartment syndrome are agitation, anxiety, and analgesia.91 The literature has reported independent risk factors associated with a patient needing a fasciotomy such as a hemoglobin <11 mg/dL, leukocytosis and an INR >1.2.39
Physician disagreement regarding fasciotomy post envenomation centers around local tissue complications (pain, tense, and numb) that can potentially mimic compartment syndrome.10,86 In the past, this has led to unnecessary fasciotomies.9 To further ensure a true compartment syndrome, several studies have used various cutoffs (30, 40, 45, and 55 mm Hg) indicating a need for fasciotomy.9,39,90,92,30,31,33 Current literature, however, supports serial clinical evaluation with an accompanying clinical picture of compartment syndrome.93 The definitive role of measurements of elevated intracompartmental pressure to confirm compartment syndrome and the need for a fasciotomy is unclear; however, criteria may vary by institution.9,72,93
Surgical Interventions
Overall, the true incidence of envenomation injuries requiring some kind of formal reconstruction is unknown. Post envenomation, plastic surgeons are frequently consulted regarding wounds where restoration of form and function are desired.13 Surgical interventions are more common for certain envenomations such as the cobra, as its venom is known for causing higher rates of tissue necrosis.46 These surgical interventions include but are not limited to fasciotomies, wound debridement, tissue grafts, local and free tissue flaps, and rarely amputations.9 Resulting sequelae of snake bite envenomation that prompt surgical intervention includes infection, tissue necrosis, compartment syndrome, necrotizing fasciitis, chronic wounds, and ischemic contracture.13,62,37 In the past, delayed wound debridement has been recommended to prevent the unnecessary removal of viable tissue.94 However, more recent techniques utilizing autolytic and enzymatic debridement, as well as topical wound staining that specifically targets dead tissue, may help prevent the removal of healthy tissue.95 Locoregional tissue grafts and flaps can be utilized to restore previous form and function of smaller defects.94,96,40 Occasionally, free flaps are required when there is insufficient soft tissue available for locoregional flaps.96 When selecting a flap, it is important to consider matching skin, bulk, composition, and size of vessels, to the recipient defect.94
Upper Extremity Envenomation
Envenomation of the upper extremity and hand often requires a graft or flap in a complex reconstruction to allow for the return of form and function.10 Soft-tissue dysfunction within the hand can be debilitating, as many people rely on their function to perform activities of daily living, as well as occupations.10 Grafts and flaps must be utilized to reduce contracture of the affected area while maintaining mobility and function.10 The volar and dorsal hand require different flap characteristics (Table 2) as the dorsal hand has little subcutaneous and adipose tissue that easily exposes tendon and bone upon envenomation induced tissue necrosis.13,43,41 A variety of flaps can also be used in reconstruction of the upper extremity that closely matches the missing tissue defect (Table 2).18,94,42 In any hand or upper extremity injury, early rehabilitation is key to making a full recovery.18,32,43
Table 2.
Location Dependent Reconstructive Options
| Upper Extremity | Reconstructive Options | Comment |
|---|---|---|
| Digit | • Cross finger flap (transposition) | Lacks excess tissue for reconstruction, limited blood supply, restoration of function is important for many occupations and daily life. Z plasty can be utilized to break up contracted scar |
| • V-Y advancement flap | ||
| • Homodigital island flap | ||
| Hand—dorsal | • Full-thickness skin graft | A full-thickness skin graft or flap is often required to survive on top of the easily exposed bone and tendon. Muscle flaps are generally avoided on the dorsal hand as the muscle fibers tend to integrate with the underlying tissue, limiting extensor tendon function and possibly compromising existing vasculature |
| • Posterior interosseous artery perforator propeller flap | ||
| • Radial forearm flap (free or pedicled) | ||
| Hand—volar | • Groin flap | Important to match similar skin characteristics |
| • Cross finger flap | ||
| • Thenar flap | ||
| Forearm/arm | • Posterior interosseous artery perforator propeller flap | A variety of flaps can be implemented depending on the severity of the defect and extent of tissues involved. Lateral arm flap utilizes the posterior collateral radial artery and can be pedicled. The thoracodorsal flap can be pedicled or free (muscle, myocutaneous) and provide a large area of coverage for upper arm |
| • Radial forearm flap (free or pedicled) | ||
| • Lateral arm flap | ||
| • ALT flap | ||
| • Latissimus dorsi flap | ||
| Lower Extremity | Reconstructive Options | Comment |
| Toes | • Lateral toe pulp flap | As they are distally located, lack sufficient collateral blood supply and tissue. Challenge to have successful flap vascularization and survival |
| Foot—plantar | • Latissimus dorsi muscular flap (larger defect) | The plantar surface and heel of the foot need special consideration as it is more glabrous kin that is responsible for weight bearing pressure. To sustain eventual force, larger muscle flap is needed to be able to sustain |
| • Medial plantar myocutaneous flap (smaller defect) | ||
| • Lateral calcaneal | ||
| • Reverse sural | ||
| Foot—dorsal | • Scapular flap (fascial or fasciocutaneous or osteocutaneous) | Dorsum of foot does not have excess subcutaneous or adipose tissue. Therefore, flaps with less bulk are typically used unless there is a large defect that needs to be covered |
| • Latissimus dorsi muscular flap (if larger defect) | ||
| • ALT fasciocutaneous flap | ||
| Leg | • Scapular osteocutaneous flap | Anterior leg is bony and also has little subcutaneous and adipose tissue. This allows for underlying structures to be more easily affected. Osteocutaneous flaps are useful in this area |
| • Fibular osteocutaneous flap | ||
| • Iliac osteocutaneous flap, | ||
| • Gastrocnemius or soleus muscle flap | ||
| • Perforator flap (propeller or keystone) | ||
| Thigh | • ALT flap | More surrounding soft tissue to use for local grafts and flaps depending on severity of defect. Bulkier flaps can be used to fill in severe defects |
| • Latissimus dorsi muscle, fascial or fasciocutaneous flap | ||
| Face | Reconstructive Options | Comment |
| Face | • Local V-Y advancement flaps | Depending on location of defect, can use any of the mentioned flaps. Median forehead flap utilized in nasal reconstruction. Parascapular, rectus abdominis, and radial forearm flaps can all be used in larger soft-tissue defects of the face |
| • Rotational flaps (single/bilobed flap) and transposition flaps (Limberg flap) | ||
| • Median forehead flap | ||
| • Parascapular flap | ||
| • Rectus abdominis flap | ||
| • Radial forearm flap |
ALT, anterolateral thigh.
Face Envenomation
Snake bite envenomation of the face often occurs in children or agricultural workers working close to the ground. Envenomation to the face can cause tissue necrosis, contracture, and deformity making reconstruction essential.37,36,62 Depending on the extent of damage, local or free flaps can be used in a range of defects (Table 2).94
Lower Extremity Envenomation
Envenomation of the lower extremity is most common.6,13 The foot and toes are most often involved, especially if the victim is not wearing shoes.6 Envenomation of the lower extremity can be difficult for reconstruction as neither the foot nor the toes have abundant tissue or a robust blood supply to utilize for local grafts and flaps.43 Flaps are selected based on where the defect is located, along with the defect characteristics, making each reconstruction unique and individualized.43 Defects to the plantar surface and heel of the foot need special consideration as this region contains thick tissue with glabrous skin to sustain ambulation and weight bearing.43 A variety of flaps can be used to reconstruct defects of the anterior leg and thigh as well (Table 2).43
DISCUSSION
Snake bite envenomation is an underreported global health crisis.68 True incidence is likely underreported due to lack of contact with healthcare system for less severe snake bites.5,55 Multiple studies support the use of early and sufficient doses of antivenom administration to reduce the need for surgical intervention. However, there is a sparse availability of antivenom in rural and resource poor areas, especially in LMICs as the price of antivenom is cost prohibitive. Socioeconomic factors and a lack of access to resources also preclude timely treatment of snake bites in LMICs.5,45,55,68 This results in higher rates of secondary complications than seen in HICs, indicating even more of a need for plastic surgeons to treat the resulting sequelae in this patient population. Efforts in LMICs should be focused on envenomation education as treatment myths can potentiate local effects of the venom’s cytotoxic enzymes, worsening local tissue injury, and patient outcomes. Although antivenom availability can be limited in LMICs, receiving treatment at a healthcare facility should be encouraged.
Plastic surgeons are well suited to care for the acute and chronic management of snake bite victims through reconstructive procedures.17,13,51 These procedures are essential for allowing patients to regain their normal life.10 Post envenomation, wound debridement was among the most cited procedures which is essential to any successful reconstructive outcome. Although fasciotomies are a controversial intervention post envenomation, they cannot be ignored as there are severe consequences if true compartment syndrome is not acted upon in a timely manner. Studies also showed that overall amputations are most common in envenomation to the digits or toes, especially if antivenom is not administered. After the effects of envenomation have been controlled, reconstructive options post envenomation should be evaluated as any other soft-tissue defect, paying special attention to proper debridement.
Patient education is important to provide the general population with knowledge about treatment post envenomation. Further global effort is needed among private companies and governments to provide effective and affordable antivenom that is widely distributed and readily available to those who need it most.
This study is limited by the level of evidence of available studies; many case reports and single-center retrospective reviews composed the literature search.
CONCLUSIONS
Plastic surgery has an important role in snake bite management and the resulting complications. Published reports have demonstrated multiple ways to manage envenomation with a variety of techniques in an effort to reduce these secondary complications and improve patient outcomes.8 Timing of plastic surgery intervention can range from immediate (fasciotomy) to days, weeks, or years (debridement, scar contracture release, and flap) which is unique to each patient's situation, geographic location, and timing of presentation. Victims of snake bite envenomation need a multidisciplinary team that understands the underlying pathophysiology and potential complications to avoid a delay in treatment. It is essential for plastic surgeons to take responsibility for these patients to help restore both form and function.
Footnotes
Published online 29 April 2021.
Disclosure: Dr. Janis received royalties from Thieme and Springer publishing. The other authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.World Health Organization. Snake bite envenomation. 2019. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/snakebite-envenoming. Accessed April 29, 2020. [Google Scholar]
- 2.Prevention CfDCa. Venomous snakes. 2018. National Institute for Occupational Safety and Health. Available at: https://www.cdc.gov/niosh/topics/snakes/default.html. Accessed April 29, 2020. [Google Scholar]
- 3.Nazim MH, Gupta S, Hashmi S, et al. Retrospective review of snake bite victims. W V Med J. 2008; 104:30–34. [PubMed] [Google Scholar]
- 4.Johnson DSA. Frequently asked questions about venomous snakes. 2020. University of Florida. Available at: https://ufwildlife.ifas.ufl.edu/venomous_snake_identification.shtml. Accessed April 29, 2020. [Google Scholar]
- 5.Tochie JN, Temgoua MN, Njim T, et al. The neglected burden of snakebites in Cameroon: a review of the epidemiology, management and public health challenges. BMC Res Notes. 2017; 10:405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Juckett G, Hancox JG. Venomous snakebites in the United States: management review and update. Am Fam Physician. 2002; 65:1367–1374. [PubMed] [Google Scholar]
- 7.Korambayil PM, Ambookan PV, Abraham SV, et al. A multidisciplinary approach with hyperbaric oxygen therapy improve outcome in snake bite injuries. Toxicol Int. 2015; 22:104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruha AM, Kleinschmidt KC, Greene S, et al. ; ToxIC Snakebite Study Group. The epidemiology, clinical course, and management of snakebites in the North American Snakebite Registry. J Med Toxicol. 2017; 13:309–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim YH, Choi JH, Kim J, et al. Fasciotomy in compartment syndrome from snakebite. Arch Plast Surg. 2019; 46:69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edgerton MT, Koepplinger ME. Management of snakebites in the upper extremity. J Hand Surg Am. 2019; 44:137–142. [DOI] [PubMed] [Google Scholar]
- 11.Abbey JM, Jaffar NA, Abugrara HL, et al. Epidemiological characteristics, hospital course and outcome of snakebite victims in West Texas. Hosp Pract (1995). 2015; 43:217–220. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad Z. A study of the knowledge and attitudes of emergency physicians and plastic surgeons in the management of snakebites. Eur. J. Plast. Surg. 2009; 32:141–145. [Google Scholar]
- 13.Anz AW, Schweppe M, Halvorson J, et al. Management of venomous snakebite injury to the extremities. J Am Acad Orthop Surg. 2010; 18:749–759. [DOI] [PubMed] [Google Scholar]
- 14.Ashwin PT, Mehta P, Tailor R, et al. Challenges in the management of ocular snake-bite injuries. Int Ophthalmol. 2010; 30:633–635. [DOI] [PubMed] [Google Scholar]
- 15.Aziz H, Rhee P, Pandit V, et al. The current concepts in management of animal (dog, cat, snake, scorpion) and human bite wounds. J Trauma Acute Care Surg. 2015; 78:641–648. [DOI] [PubMed] [Google Scholar]
- 16.Balaji G, Kumar A, Menon J. Snake bite induced cellulitis leading to infected open dislocation of the first metacarpophalangeal joint - A rare complication. J Clin Orthop Trauma. 2015; 6:195–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonasso P, Lucke-Wold B, Jacob G. Osteonecrosis of interphalangeal joint of thumb two months after rattlesnake bite. Hand Surg. 2015; 20:330–332. [DOI] [PubMed] [Google Scholar]
- 18.Bozkurt M, Kulahci Y, Zor F, et al. The management of pit viper envenomation of the hand. Hand (N Y). 2008; 3:324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campbell BT, Corsi JM, Boneti C, et al. Pediatric snakebites: lessons learned from 114 cases. J Pediatr Surg. 2008; 43:1338–1341. [DOI] [PubMed] [Google Scholar]
- 20.Chattopadhyay A, Patra RD, Shenoy V, et al. Surgical implications of snakebites. Indian J Pediatr. 2004; 71:397–399. [DOI] [PubMed] [Google Scholar]
- 21.Cheng LF, Lee JT, Wu MS. Lateral toe pulp flap used in reconstruction of distal dorsal toe defect: case report and review of the literature. Ann Plast Surg. 2019; 82(1S Suppl 1):S136–S139. [DOI] [PubMed] [Google Scholar]
- 22.Chippaux JP. Estimate of the burden of snakebites in sub-Saharan Africa: a meta-analytic approach. Toxicon. 2011; 57:586–599. [DOI] [PubMed] [Google Scholar]
- 23.Corneille MG, Larson S, Stewart RM, et al. A large single-center experience with treatment of patients with crotalid envenomations: outcomes with and evolution of antivenin therapy. Am J Surg. 2006; 192:848–852. [DOI] [PubMed] [Google Scholar]
- 24.Correa JA, Fallon SC, Cruz AT, et al. Management of pediatric snake bites: are we doing too much? J Pediatr Surg. 2014; 49:1009–1015. [DOI] [PubMed] [Google Scholar]
- 25.Cumpston KL. Is there a role for fasciotomy in Crotalinae envenomations in North America? Clin Toxicol (Phila). 2011; 49:351–365. [DOI] [PubMed] [Google Scholar]
- 26.Dart RC, McNally J. Efficacy, safety, and use of snake antivenoms in the United States. Ann Emerg Med. 2001; 37:181–188. [DOI] [PubMed] [Google Scholar]
- 27.Dijkman MA, Damhuis DE, Meulenbelt J, et al. Clinical presentation and management of an Aruban rattlesnake bite in the Netherlands. Clin Toxicol (Phila). 2016; 54:447–449. [DOI] [PubMed] [Google Scholar]
- 28.Farrar HC, Grayham T, Bolden B, et al. The use and tolerability of Crotalidae Polyvalent Immune FAB (Ovine) in pediatric envenomations. Clin Pediatr (Phila). 2012; 51:945–949. [DOI] [PubMed] [Google Scholar]
- 29.Fry BG, Wüster W, Ryan Ramjan SF, et al. Analysis of Colubroidea snake venoms by liquid chromatography with mass spectrometry: evolutionary and toxinological implications. Rapid Commun Mass Spectrom. 2003; 17:2047–2062. [DOI] [PubMed] [Google Scholar]
- 30.Gold BS, Barish RA, Dart RC. North American snake envenomation: diagnosis, treatment, and management. Emerg Med Clin North Am. 2004; 22:423–443, ix. [DOI] [PubMed] [Google Scholar]
- 31.Greene S, Galdamez LA, Tomasheski R. White-lipped tree viper (cryptelytrops albolabris) envenomation in an American Viper Keeper. J Emerg Med. 2017; 53:e115–e118. [DOI] [PubMed] [Google Scholar]
- 32.Griffin M, Hindocha S, Malahias M, et al. Flap decisions and options in soft tissue coverage of the upper limb. Open Orthop J. 2014; 8:409–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamdi MF, Baccari S, Daghfous M, et al. Upper limb compartment syndrome after an adder bite: a case report. Chin J Traumatol. 2010; 13:117–119. [PubMed] [Google Scholar]
- 34.Heiner JD, Bebarta VS, Varney SM, et al. Clinical effects and antivenom use for snake bite victims treated at three US hospitals in Afghanistan. Wilderness Environ Med. 2013; 24:412–416. [DOI] [PubMed] [Google Scholar]
- 35.Hernandez MC, Traynor M, Bruce JL, et al. Surgical considerations for pediatric snake bites in low- and middle-income countries. World J Surg. 2019; 43:1636–1643. [DOI] [PubMed] [Google Scholar]
- 36.Rha JH, Kwon SM, Oh JR, et al. Snakebite in Korea: A guideline to primary surgical management. Yonsei Med J. 2015; 56:1443–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hon KL, Chow CM, Cheung KL, et al. Snakebite in a child: could we avoid the anaphylaxis or the fasciotomies? Ann Acad Med Singap. 2005; 34:454–456. [PubMed] [Google Scholar]
- 38.Hsieh YH, Hsueh JH, Liu WC, et al. Contributing factors for complications and outcomes in patients with snakebite: experience in a medical center in Southern Taiwan. Ann Plast Surg. 2017; 78(3 Suppl 2):S32–S36. [DOI] [PubMed] [Google Scholar]
- 39.Hsu CP, Chuang JF, Hsu YP, et al. Predictors of the development of post-snakebite compartment syndrome. Scand J Trauma Resusc Emerg Med. 2015; 23:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ince B, Gundeslioglu AO. The management of viper bites on the hand. J Hand Surg Eur Vol. 2014; 39:642–646. [DOI] [PubMed] [Google Scholar]
- 41.Irion VH, Barnes J, Montgomery BE, et al. Presentation and management of venomous snakebites: should all patients be transferred to a tertiary referral hospital? J Surg Orthop Adv. 2016; 25:69–73. [PubMed] [Google Scholar]
- 42.Jeng JC, Fidler PE, Sokolich JC, et al. Seven years’ experience with Integra as a reconstructive tool. J Burn Care Res. 2007; 28:120–126. [DOI] [PubMed] [Google Scholar]
- 43.Kang MJ, Chung CH, Chang YJ, et al. Reconstruction of the lower extremity using free flaps. Arch Plast Surg. 2013; 40:575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karlo R, Dželalija B, Zupančić B, et al. Venomous snakebites in the Croatian North Dalmatia region. Wien Klin Wochenschr. 2011; 123:732–737. [DOI] [PubMed] [Google Scholar]
- 45.Kleinschmidt K, Ruha AM, Campleman S, et al.; ToxIC North American Snakebite Registry Group. Acute adverse events associated with the administration of Crotalidae polyvalent immune Fab antivenom within the North American Snakebite Registry. Clin Toxicol (Phila). 2018; 56:1115–1120. [DOI] [PubMed] [Google Scholar]
- 46.Laohawiriyakamol S, Sangkhathat S, Chiengkriwate P, et al. Surgery in management of snake envenomation in children. World J Pediatr. 2011; 7:361–364. [DOI] [PubMed] [Google Scholar]
- 47.Larson KW, Schaefer KR, Austin C, et al. Management of tissue loss after agkistrodon snakebite: appropriate use of crotalidae-fab antivenin. J Trauma Nurs. 2016; 23:169–172. [DOI] [PubMed] [Google Scholar]
- 48.Lavonas EJ, Burnham RI, Schwarz J, et al. Recovery from copperhead snake envenomation: role of age, sex, bite location, severity, and treatment. J Med Toxicol. 2020; 16:17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee L, Yao J. Stenosing flexor tenosynovitis following a rattlesnake bite. Orthopedics. 2010; 33:515. [DOI] [PubMed] [Google Scholar]
- 50.Liu CC, Yu JS, Wang PJ, et al. Development of sandwich ELISA and lateral flow strip assays for diagnosing clinically significant snakebite in Taiwan. Plos Negl Trop Dis. 2018; 12:e0007014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mao YC, Liu PY, Chiang LC, et al. Naja atra snakebite in Taiwan. Clin Toxicol (Phila). 2018; 56:273–280. [DOI] [PubMed] [Google Scholar]
- 52.Mao YC, Liu PY, Hung DZ, et al. Bacteriology of Naja atra Snakebite Wound and its implications for antibiotic therapy. Am J Trop Med Hyg. 2016; 94:1129–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mao YC, Liu PY, Chiang LC, et al. Clinical manifestations and treatments of Protobothrops mucrosquamatus bite and associated factors for wound necrosis and subsequent debridement and finger or toe amputation surgery. Clin Toxicol (Phila). 2020:1–10. [DOI] [PubMed] [Google Scholar]
- 54.McBride KM, Bromberg W, Dunne J. Thromboelastography utilization in delayed recurrent coagulopathy after severe eastern diamondback rattlesnake envenomation. Am Surg. 2017; 83:332–336. [PubMed] [Google Scholar]
- 55.Michael GC, Grema BA, Aliyu I, et al. Knowledge of venomous snakes, snakebite first aid, treatment, and prevention among clinicians in northern Nigeria: a cross-sectional multicentre study. Trans R Soc Trop Med Hyg. 2018; 112:47–56. [DOI] [PubMed] [Google Scholar]
- 56.Mohan G, Guduri PR, Shastry S. Role of therapeutic plasma exchange in snake bite associated thrombotic microangiopathy-A case report with review of literature. J Clin Apher. 2019; 34:507–509. [DOI] [PubMed] [Google Scholar]
- 57.Norris RL, Ngo J, Nolan K, et al. Physicians and lay people are unable to apply pressure immobilization properly in a simulated snakebite scenario. Wilderness Environ Med. 2005; 16:16–21. [DOI] [PubMed] [Google Scholar]
- 58.Palappallil DS. Pattern of use of antibiotics following snake bite in a tertiary care hospital. J Clin Diagn Res. 2015; 9:OC05–OC09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Poyrazoglu Y, Toygar M, Turk Y, et al. Pit viper envenomation in military personnel. TAF Preventive Medicine Bulletin. 2012; 11:127. [Google Scholar]
- 60.Pulimaddi R, Parveda AR, Brahmanpally B, et al. Incidence & prognosis of acute kidney injury in individuals of snakebite in a tertiary care hospital in India. Indian J Med Res. 2017; 146:754–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramirez RN, Umberhandt R, Oishi SN, et al. Digital chondrolysis and epiphysiolysis associated with snakebite: a report of 2 cases. J Pediatr Orthop. 2015; 35:e60–e64. [DOI] [PubMed] [Google Scholar]
- 62.Rha JH, Kwon SM, Oh JR, et al. Snakebite in Korea: a guideline to primary surgical management. Yonsei Med J. 2015; 56:1443–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Severyns M, Nevière R, Resiere D, et al. Case report: bothrops lanceolatus snakebite surgical management-relevance of fasciotomy. Am J Trop Med Hyg. 2018; 99:1350–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sharma LR, Lal V, Simpson ID. Snakes of medical significance in India: the first reported case of envenoming by the Levantine viper (Macrovipera lebetina). Wilderness Environ Med. 2008; 19:195–198. [DOI] [PubMed] [Google Scholar]
- 65.Shaw BA, Hosalkar HS. Rattlesnake bites in children: antivenin treatment and surgical indications. J Bone Joint Surg Am. 2002; 84:1624–1629. [PubMed] [Google Scholar]
- 66.Strickland JL, Mason AJ, Rokyta DR, et al. Phenotypic variation in mojave rattlesnake (Crotalus scutulatus) venom is driven by four toxin families. Toxins (Basel). 2018; 10:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Su HY, Wang MJ, Li YH, et al. Can surgical need in patients with Naja atra (Taiwan or Chinese cobra) envenomation be predicted in the emergency department? Hong Kong Med J. 2016; 22:435–444. [DOI] [PubMed] [Google Scholar]
- 68.Taieb F, Dub T, Madec Y, et al. Knowledge, attitude and practices of snakebite management amongst health workers in Cameroon: Need for continuous training and capacity building. Plos Negl Trop Dis. 2018; 12:e0006716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tincu RC, Ghiorghiu Z, Tomescu D, et al. The compartment syndrome associated with deep vein thrombosis due to rattlesnake bite: a case report. Balkan Med J. 2017; 34:367–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tokish JT, Benjamin J, Walter F. Crotalid envenomation: the southern Arizona experience. J Orthop Trauma. 2001; 15:5–9. [DOI] [PubMed] [Google Scholar]
- 71.Toschlog EA, Bauer CR, Hall EL, et al. Surgical considerations in the management of pit viper snake envenomation. J Am Coll Surg. 2013; 217:726–735. [DOI] [PubMed] [Google Scholar]
- 72.Tucker SC, Josty I. Compartment syndrome in the hand following an adder bite. J Hand Surg Br. 2005; 30:434–435. [DOI] [PubMed] [Google Scholar]
- 73.Türkmen A, Temel M. Algorithmic approach to the prevention of unnecessary fasciotomy in extremity snake bite. Injury. 2016; 47:2822–2827. [DOI] [PubMed] [Google Scholar]
- 74.Wagener M, Naidoo M, Aldous C. Wound infection secondary to snakebite. S Afr Med J. 2017; 107:315–319. [DOI] [PubMed] [Google Scholar]
- 75.Wu CH, Hu WH, Hung DZ, et al. Snakebite complicated with Vibrio vulnificus infection. Vet Hum Toxicol. 2001; 43:283–285. [PubMed] [Google Scholar]
- 76.Yildirim C, Bayraktaroğlu Z, Gunay N, et al. The use of therapeutic plasmapheresis in the treatment of poisoned and snake bite victims: an academic emergency department’s experiences. J Clin Apher. 2006; 21:219–223. [DOI] [PubMed] [Google Scholar]
- 77.Yuenyongviwat V, Laohawiriyakamol T, Suwanno P, et al. Calcific myonecrosis following snake bite: a case report and review of the literature. J Med Case Rep. 2014; 8:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zengin S, Yilmaz M, Al B, et al. Plasma exchange as a complementary approach to snake bite treatment: an academic emergency department’s experiences. Transfus Apher Sci. 2013; 49:494–498. [DOI] [PubMed] [Google Scholar]
- 79.Russell FE. Snake venom poisoning in the United States. Annu Rev Med. 1980; 31:247–259. [DOI] [PubMed] [Google Scholar]
- 80.Minton SA, Weinstein SA. Geographic and ontogenic variation in venom of the western diamondback rattlesnake (Crotalus atrox). Toxicon. 1986; 24:71–80. [DOI] [PubMed] [Google Scholar]
- 81.Currie BJ. Treatment of snakebite in Australia: the current evidence base and questions requiring collaborative multicentre prospective studies. Toxicon. 2006; 48:941–956. [DOI] [PubMed] [Google Scholar]
- 82.McKinney PE. Out-of-hospital and interhospital management of crotaline snakebite. Ann Emerg Med. 2001; 37:168–174. [DOI] [PubMed] [Google Scholar]
- 83.Alberts MB, Shalit M, LoGalbo F. Suction for venomous snakebite: a study of “mock venom” extraction in a human model. Ann Emerg Med. 2004; 43:181–186. [DOI] [PubMed] [Google Scholar]
- 84.Warrell DA. Guidelines for the management of snake-bites. 2010. World Health Organization. Available at: https://www.who.int/snakebites/resources/9789290225300/en/. Accessed May 8, 2020.
- 85.Sheikh S, Leffers P, Nusbaum J, et al. Points & pearls: emergency department management of North American snake envenomations. Emerg Med Pract. 2018; 20(19 Suppl):1–2. [PubMed] [Google Scholar]
- 86.Fry BG. Snake bite: when the human touch becomes a bad touch. Toxins (Basel). 2018; 10:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Barish RA. Snake bites. 2020. Merck & Co., Inc. Merck Manuals Web site. Available at: https://www.merckmanuals.com/home/injuries-and-poisoning/bites-and-stings/snakebites. Accessed May 11, 2020. [Google Scholar]
- 88.Rudolph R, Neal GE, Williams JS, et al. Snakebite treatment at a southeastern regional referral center. Am Surg. 1995; 61:767–772. [PubMed] [Google Scholar]
- 89.Parrish HM, Khan MS. Bites by coral snakes: report of 11 representative cases. Am J Med Sci. 1967; 253:561–568. [PubMed] [Google Scholar]
- 90.Matsen FA, 3rd, Winquist RA, Krugmire RB, Jr. Diagnosis and management of compartmental syndromes. J Bone Joint Surg Am. 1980; 62:286–291. [PubMed] [Google Scholar]
- 91.Livingston KS, Glotzbecker MP, Shore BJ. Pediatric acute compartment syndrome. J Am Acad Orthop Surg. 2017; 25:358–364. [DOI] [PubMed] [Google Scholar]
- 92.Mubarak SJ, Owen CA, Hargens AR, et al. Acute compartment syndromes: diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978; 60:1091–1095. [PubMed] [Google Scholar]
- 93.Tillinghast CM, Gary JL. Compartment syndrome of the lower extremity. In: Mauffrey C, Hak DJ, Martin IM, eds. Compartment Syndrome: A Guide to Diagnosis and Management. Cham, CH: Springer; 2019:67–81. [Google Scholar]
- 94.Panse N, Sahasrabudhe P. Free style perforator based propeller flaps: Simple solutions for upper extremity reconstruction! Indian J Plast Surg. 2014; 47:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Anghel EL, DeFazio MV, Barker JC, et al. Current concepts in debridement: science and strategies. Plast Reconstr Surg. 2016; 138(3 Suppl):82S–93S. [DOI] [PubMed] [Google Scholar]
- 96.Janis JE, Kwon RK, Attinger CE. The new reconstructive ladder: modifications to the traditional model. Plast Reconstr Surg. 2011; 127(Suppl 1):205s–212s. [DOI] [PubMed] [Google Scholar]


