Abstract
Coronavirus disease 2019 has been a worldwide pandemic since early 2020 with New York City being the epicenter in the United States during early 2020. Although cases of decreased coronavirus disease 2019 during the summer, cases began to rise once more in the fall-winter period. Little is known about trends in patient characteristics, medical care, and outcome between these time periods. We report initial patient characteristics and outcomes from a large quaternary referral center in New York City between Spring (March to June), Summer (July to September), and Winter (October to December), including prevalence of renal failure, respiratory failure, and mortality; stratified across several key populations of interest including all patients, ICU patients, those requiring of noninvasive positive pressure ventilation and high-flow nasal cannula, and those intubated in each time period.
Keywords: coronavirus disease 2019, intubation rate, mortality, renal failure, second wave
To the Editor:
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus continues to infect thousands of Americans daily, with exponentially rising case counts during the end of fall (1). New York City became the center of the pandemic in the United States in March and April of 2020, accounting for more than 30% of all U.S. cases at that time (2). The initial surge of patients resulted in significant morbidity and mortality, especially among those requiring invasive mechanical ventilation (2). After the initial surge in the spring, a second, albeit smaller, rise in cases was observed in the city during the fall (3). We report initial patient characteristics and outcomes in a large quaternary referral center in New York City between three distinct time periods of coronavirus disease 2019 (COVID-19) pandemic.
METHODS
The study population consists of all adult inpatients admitted to or transferred to the Mount Sinai Hospital, with COVID-19 identified by positive SARS-CoV-2 polymerase chain reaction on that admission or clinical documentation of infection. Patients are separated into three periods based on visual analysis of the epidemic curve: Spring (March 1, 2020, to June 30, 2020), Summer (July 1, 2020, until September 30, 2020), and Winter (October 1 to December 25); all patients included in this study were followed for outcomes through January 24, 2021. Similar to other studies, patients admitted after December 25, 2020, were censored to ensure most patients had known disposition (4). Comparisons between periods was done at the level of all patients versus those who required ICU level of care and among patients who used noninvasive respiratory support with noninvasive positive pressure ventilation (NIPPV) or high-flow nasal cannula (HFNC) but were never intubated versus those who required invasive mechanical ventilation. The use of respiratory support, including low flow nasal cannula and HFNC, mechanical ventilators, d-dimer levels, Sequential Organ Failure Assessment (SOFA) scores, and creatinine elevations were compared between groups. Data preprocessing was performed in Python version 3.7.3 (Python Software Foundation, Wilmington, DE, https://www.python.org/), and analysis was completed in R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria, https://www.R-project.org/) with RStudio version 1.2.5001 (RStudio PBC, Boston MA, http://www.rstudio.com/). The study was reviewed by the Mount Sinai Hospital Institutional Review Board number 20-0054.
RESULTS
The temporal distribution of admissions is shown in Figure 1A. A total of 3,088 inpatient admissions were included in this analysis; 2,305 in the spring cohort, 217 in the summer cohort, and 566 in the winter cohort (Table 1). Patients were slightly younger in the summer (mean age 61 yr spring, 57 yr summer, 60 yr winter; p = 0.014) and were more likely to be male in all time periods (55%, 55%, 59%; p = 0.036). ICU utilization was similar in all time periods (25%, 22%, 21%; p = 0.11), but intubation rate declined with time (17%, 9.7%, 8.8%; p < 0.001). Mean and peak SOFA scores declined with time (mean SOFA 2.06, 1.62, 1.45; p < 0.001), as did mean and peak d-dimer (mean d-dimer 3.7, 3.3, 3.1; p < 0.001). Although there was no significant difference in admission creatinine between time periods (1.72, 1.68, 1.24; p = 0.092), there was a decline in acute kidney injury (AKI) as identified by 150% increase in creatinine through admission (19%, 13%, 10%; p < 0.001).
Figure 1.
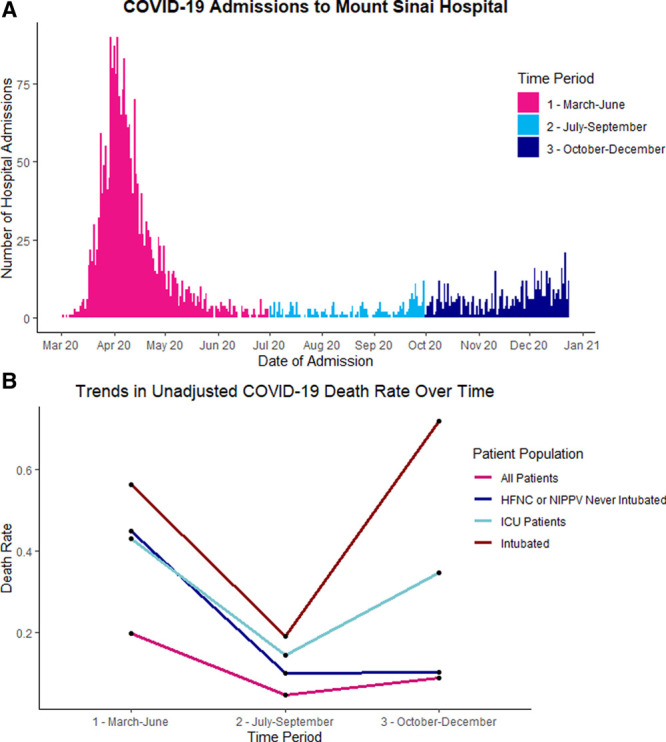
A, Admissions of coronavirus disease 2019 (COVID-19) patients to Mount Sinai Hospital per day from February 2020 to January 2020. B. Unadjusted mortality comparing Spring, Summer, and Winter for different groups of COVID-19 patients admitted to Mount Sinai Hospital. HFNC = high-flow nasal cannula, NIPPV = noninvasive positive pressure ventilation.
TABLE 1.
Patient Characteristics and Outcomes for Coronavirus Disease 2019 Patients Admitted to Mount Sinai Hospital Comparing All Admissions With ICU Admissions Between the Spring, Summer, and Winter Time Periods
| Characteristics | All Admissions | Patients Admitted to ICU Only | ||||||
|---|---|---|---|---|---|---|---|---|
| 1—March to June, n = 2,305 | 2—July to September, n = 217 | 3—October to December, n = 566 | pa | 1—March to June, n = 573 | 2—July to September, n = 48 | 3—October to December, n = 118 | pa | |
| Age, mean (sd) | 61 (18) | 57 (18) | 60 (18) | 0.014 | 61 (16) | 59 (16) | 66 (17) | 0.001 |
| Gender, n (%) | 0.036 | 0.7 | ||||||
| Female | 1,030 (45) | 96 (44) | 232 (41) | 219 (38) | 16 (33) | 42 (36) | ||
| Male | 1,275 (55) | 120 (55) | 333 (59) | 354 (62) | 32 (67) | 76 (64) | ||
| Unknown | 0 (0) | 1 (0.5) | 1 (0.2) | 0 (0) | 0 (0) | 0 (0) | ||
| Hospital length of stay (d), mean (sd) | 11 (13) | 10 13) | 10 (11) | < 0.001 | 21 (20) | 22 (20) | 21 (16) | 0.3 |
| Ever intubated, n (%) | 390 (17) | 21 (9.7) | 50 (8.8) | < 0.001 | 390 (68) | 21 (44) | 50 (42) | < 0.001 |
| Received ICU level of care, n (%) | 573 (25) | 48 (22) | 118 (21) | 0.11 | ||||
| Highest SOFA score during admission, mean (sd) | 3.30 (3.34) | 2.70 (2.98) | 2.43 (2.72) | < 0.001 | 7.07 (3.04) | 6.44 (2.79) | 6.11 (2.70) | < 0.001 |
| Mean SOFA score, mean (sd) | 2.06 (2.84) | 1.62 (2.37) | 1.45 (2.35) | < 0.001 | 5.0 (3.6) | 4.2 (3.2) | 4.1 (3.5) | 0.045 |
| Admission d-dimer, mean (sd) | 2.9 (3.7) | 2.2 (3.3) | 1.7 (2.7) | < 0.001 | 4.0 (4.7) | 3.7 (4.9) | 2.4 (3.3) | < 0.001 |
| Peak d-dimer, mean (sd) | 5.0 (5.4) | 3.5 (4.7) | 3.1 (4.5) | < 0.001 | 8.7 (6.3) | 7.1 (6.4) | 6.5 (6.2) | < 0.001 |
| Admission creatinine, mean (sd) | 1.72 (2.50) | 1.68 (2.22) | 1.24 (1.45) | 0.092 | 1.72 (2.22) | 2.12 (2.39) | 1.32 (1.16) | 0.5 |
| Peak creatinine, mean (sd) | 2.53 (3.38) | 2.06 (2.68) | 1.52 (1.87) | < 0.001 | 3.65 (3.54) | 3.17 (2.96) | 2.15 (1.93) | < 0.001 |
| 150% increase in creatinine during admission, n (%) | 414 (19) | 25 (13) | 55 (10) | < 0.001 | 274 (48) | 15 (31) | 42 (36) | 0.005 |
| Died, n (%) | 456 (20) | 10 (4.6) | 51 (9.0) | < 0.001 | 247 (43) | 7 (15) | 41 (35) | < 0.001 |
| Discharged alive to home, n (%) | 1,475 (64) | 175 (81) | 474 (84) | < 0.001 | 196 (34) | 28 (58) | 58 (49) | < 0.001 |
| Discharged alive to facility, n (%) | 366 (16) | 31 (14) | 24 (4.2) | < 0.001 | 130 (23) | 13 (27) | 10 (8.5) | 0.001 |
SOFA = Sequential Organ Failure Assessment.
aStatistical tests performed: Kruskal-Wallis test; χ2 of independence.
Six-hundred eighty-seven patients were admitted to an ICU; 573 in the spring, 48 in the summer, and 66 in the winter. ICU patients showed similar trends over time in age, intubation rate, SOFA scores, and d-dimers; however, rates of AKI did not fall as much as in the total patient cohort (48%, 31%, 36%; p = 0.005) (Table 1).
Changes in use of respiratory support over time are shown in Figure 2. Use of HFNC significantly increased through the pandemic (15% of all patients in spring, 18% in summer, and 25% in winter p < 0.001), along with a decreasing intubation rate (17%, 9.7%, 8.8%; p < 0.001). Summary data for patients who required HFNC or NIPPV but never invasive mechanical ventilation versus those who did are shown in Table 2. Patients who required HFNC or NIPPV did not demonstrate declining SOFA scores (mean SOFA 1.85, 1.57, 1.45; p = 0.6) but had similar trends in rate of AKI to the general population. Patients who were intubated did not demonstrate a decline in SOFA (mean SOFA 6.4, 6.6, 7.1; p = 0.3, or rate of AKI (65%, 52%, 62%; p = 0.5).
Figure 2.
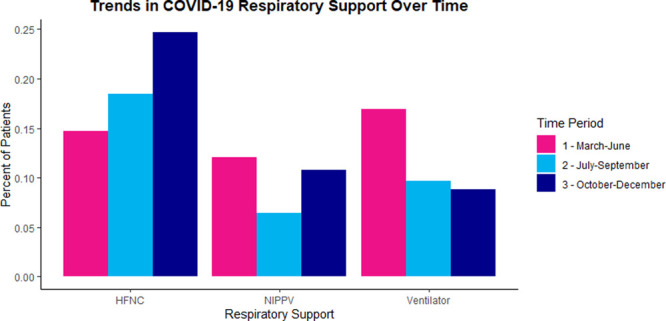
Supplemental oxygen device utilization comparing Spring, Summer, and Winter for different groups of coronavirus disease 2019 (COVID-19) patients admitted to Mount Sinai Hospital. HFNC = high-flow nasal cannula, NIPPV = noninvasive positive pressure ventilation.
TABLE 2.
Patient Characteristics and Outcomes for Coronavirus Disease 2019 Patients Admitted to Mount Sinai Hospital Comparing Noninvasive Positive Pressure Ventilation/High-Flow Nasal Cannula With Intubated Patients Between the Spring, Summer, and Winter Time Periods
| Characteristics | High-Flow Nasal Cannula or Noninvasive Positive Pressure Ventilation But Never Intubated | Intubated Patients | ||||||
|---|---|---|---|---|---|---|---|---|
| 1—March to June, n = 249 | 2—July to September, n = 30 | 3—October to December, n = 107 | pa | 1—March to June, n = 390 | 2—July to September, n = 21 | 3—October to December, n = 50 | pa | |
| Age, mean (sd) | 68 (16) | 57 (16) | 65 (16) | 0.001 | 62 (14) | 62 (10) | 69 (14) | < 0.001 |
| Gender, n (%) | 0.023 | 0.6 | ||||||
| F | 108 (43) | 5 (17) | 38 (36) | 147 (38) | 9 (43) | 16 (32) | ||
| M | 141 (57) | 25 (83) | 68 (64) | 243 (62) | 12 (57) | 34 (68) | ||
| Unknown | 0 (0) | 0 (0) | 1 (0.9) | 0 (0) | 0 (0) | 0 (0) | ||
| Hospital length of stay (d), mean (sd) | 15 (12) | 13 (7) | 15 (11) | 0.3 | 25 (22) | 34 (23) | 28 (19) | 0.012 |
| Highest SOFA score during admission, mean (sd) | 3.83 (2.71) | 3.63 (2.87) | 3.46 (2.48) | 0.6 | 8.66 (1.18) | 8.67 (0.80) | 8.40 (1.20) | 0.2 |
| Mean SOFA score, mean (sd) | 1.71 (1.85) | 1.49 (1.57) | 1.43 (1.45) | 0.6 | 6.4 (3.1) | 6.6 (3.1) | 7.1 (3.1) | 0.3 |
| Admission d-dimer, mean (sd) | 3.6 (4.3) | 1.7 (2.1) | 1.8 (2.8) | < 0.001 | 4.3 (4.9) | 5.6 (6.2) | 2.8 (4.0) | 0.018 |
| Peak d-dimer, mean (sd) | 6.8 (5.8) | 3.4 (4.5) | 3.6 (4.5) | < 0.001 | 10.1 (6.1) | 10.1 (6.5) | 9.9 (6.8) | > 0.9 |
| Admission creatinine, mean (sd) | 1.98 (2.62) | 1.86 (2.80) | 1.10 (0.87) | < 0.001 | 1.73 (1.97) | 2.47 (2.74) | 1.52 (1.07) | 0.3 |
| Peak creatinine, mean (sd) | 2.67 (3.38) | 2.12 (3.37) | 1.33 (1.19) | < 0.001 | 4.32 (3.51) | 4.21 (3.13) | 3.01 (1.98) | 0.2 |
| 150% increase in creatinine during admission, n (%) | 47 (19) | 3 (10) | 9 (8.4) | 0.025 | 250 (65) | 11 (52) | 31 (62) | 0.5 |
| Died, n (%) | 112 (45) | 3 (10) | 11 (10) | < 0.001 | 220 (56) | 4 (19) | 36 (72) | < 0.001 |
| Discharged alive to home, n (%) | 106 (43) | 23 (77) | 84 (79) | < 0.001 | 76 (19) | 8 (38) | 5 (10) | 0.023 |
| Discharged alive to facility, n (%) | 31 (12) | 3 (10) | 8 (7.5) | 0.4 | 94 (24) | 9 (43) | 6 (12) | 0.017 |
SOFA = Sequential Organ Failure Assessment.
aStatistical tests performed: Kruskal-Wallis test; χ2 of independence.
Overall death rate declined dramatically through the pandemic (Fig. 1B). Among all patients, 20% of spring admissions, 4.6% of summer admissions, and 9.0% of winter admissions died during follow-up (p < 0.001); at the time of analysis, disposition was known for greater than 97% of patients in every time period. ICU patients had a similar trend with higher mortality than all patients (43% spring, 31% summer, 35% fall; p < 0.001). Patients requiring HFNC or NIPPV but not mechanical ventilation also had significant reduction in mortality rate over time and by winter was similar to the general population (45% spring, 10% summer, 10% winter; p < 0.001). Intubated patients had a high mortality which rose in the winter cohort (56% spring, 19% summer, 72% winter; p < 0.001).
DISCUSSION AND CONCLUSIONS
In the current report, we find a greater than 50% reduction in death rate over time for patients admitted for COVID-19 in a large hospital system in New York City. We note a large first peak in the spring followed by a large drop during the summer and steady but slower rise of cases during the winter. Despite increasing case count, mortality in the winter months remains lower than at the beginning of the pandemic. In general, patients admitted with COVID-19 in the winter, compared with the spring, are similar in age but have lower SOFA scores, lower d-dimer levels, and lower prevalence of AKI. These differences persisted among ICU patients, suggesting that their degree of illness is lower than the patients admitted to ICU in the early days of COVID-19.
Change in practice pattern regarding use of noninvasive respiratory support is seen with an increasing utilization of HFNC and NIPPV with falling intubation rate. Anecdotally, this may reflect lower concern among providers regarding the aerosolizing potential of noninvasive modalities and a switch to a later intubation strategy. Patients who require noninvasive respiratory support have similar outcomes to the general population; however, those who were intubated had high rates of mortality.
Studies of publicly available datasets from the World Health Organization (WHO) and private companies have suggested there is a decreasing case fatality rate of COVID-19 worldwide (4,5). Fan showed a median reduction of 38.3% in case fatality rate between first and second waves using WHO data aggregated across 53 countries, including a 67% reduction in case fatality rate in the United States. Auld reported an almost 50% reduction in mortality among intubated patients, but not among patients overall at a single center in July compared with March (5). Dennis et al (6) showed a consistent improvement in survival through each week of the COVID-19 pandemic in United Kingdom from March to June but were unable to examine kidney injury or use of mechanical ventilation. Horwitz et al (7) demonstrated a decline in crude and risk-adjusted mortality among patients admitted to another large New York health system through August 2020 but did not assess other outcomes such as rate of intubation or AKI. To our knowledge, no other study has analyzed outcomes of patients with COVID-19 admitted once cases began to rise once more in the winter and fall.
To our knowledge, this is the first attempt at in-depth comparison of patients admitted for COVID-19 between three time periods in the United States and with the longest period of follow-up extending into winter. Although mortality is significantly lower in the winter compared with the spring of the pandemic, due to the retrospective nature of this review, it is difficult to determine the cause of this improvement. Several hypotheses have been put forward, including a “harvesting” bias where the most susceptible patients died early on in the course of the pandemic (4); a reduction in hospital overcrowding resulting in more optimal patient outcomes (8); a decrease in level of illness among admitted patients or less ill patients presenting to hospital; or evolution in therapeutics including the routine use of anticoagulation, steroids, and antivirals (6).
In conclusion, it is found that outcomes in patients admitted to a large referral center for COVID-19 are improving after over the time period of the pandemic, with clinically and statistically significantly lower rates of respiratory failure and death for all admitted patients. This benefit persists among those who require HFNC or NIPPV but do not require intubation; however, the smaller subset of patients who progress to severe disease requiring intubation and mechanical ventilation remain with similarly elevated mortality. Although the cause of these changes is not yet fully understood, a careful follow-up analysis is planned to explore several proposed hypotheses.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Duca LM, Coyle J, McCabe C, et al. COVID-19 Stats: COVID-19 incidence, by urban-rural classification — United States, January 22–October 31, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S, Hirsch JS, Narasimhan M, et al. ; the Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized With COVID-19 in the New York City Area. JAMA. 2020; 323:2052–2059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.New York City Department of Health: COVID-19 Data: Long-Term Trends - Cases, Hospitalizations, and Deaths. Available at: https://www1.nyc.gov/site/doh/covid/covid-19-data-trends.page#epicurve. Accessed January 12, 2021
- 4.Fan G, Yang Z, Lin Q, et al. Decreased case fatality rate of COVID-19 in the second wave: A study in 53 countries or regions. Transbound Emerg Dis. 2020; 00:1–3 [DOI] [PubMed] [Google Scholar]
- 5.Auld SC, Caridi-Scheible M, Robichaux C, et al. Declines in mortality over time for critically ill adults with coronavirus disease 2019. Crit Care Med. 2020; 48:e1382–e1384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dennis JM, McGovern AP, Vollmer SJ, et al. Improving survival of critical care patients with coronavirus disease 2019 in England: A National Cohort Study, March to June 2020. Crit Care Med. 2020; 49:209–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horwitz LI, Jones SA, Cerfolio RJ, et al. Trends in COVID-19 risk-adjusted mortality rates. J Hosp Med. 2021; 16:90–92 [DOI] [PubMed] [Google Scholar]
- 8.Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006; 184:208–212 [DOI] [PubMed] [Google Scholar]


