Abstract
Background
Rapid and effective emergency response to address health security relies on a competent and suitably trained local and international workforce. The COVID-19 pandemic has highlighted that the health security workforce needs to be well equipped to tackle current and future challenges. In this study, we explored whether training in applied epidemiology was meeting the current needs of the applied epidemiology workforce.
Method
We conducted a cross-sectional online survey that was available in English and French. We used purposive and snowballing sampling techniques to identify potential survey respondents. An online social media advertisement campaign was used to disseminate a REDCap survey link between October 2019 and February 2020 through field epidemiology networks. Survey questions included demographic details of participants, along with their technical background, level of formal education, topics studied during epidemiology training, and years of experience as an epidemiologist. We used Pearson Chi-squared (Chi2) to test the difference between categorical variables, and content analysis to evaluate responses to open-ended questions.
Results
In total, 282 people responded to the survey. Participants had a range of formal public health and epidemiology training backgrounds. Respondents applied epidemiology experience spanned almost 30 years, across 64 countries. Overall, 74% (n = 210) were alumni of Field Epidemiology Training Programs (FETP). Basic outbreak and surveillance training was well reported by respondents, however training in specialised techniques related to emergency response, communication, and leadership was less common. FETP graduates reported higher levels of formal training in all survey topics.
Conclusion
It is critical for the health security workforce to be well-trained and equipped with skills needed to ensure a rapid and effective response to acute public health events. Leadership, communication, interpersonal skills, and specialist training in emergency response are lacking in current training models. Our study has demonstrated that applied epidemiology workforce training must evolve to remain relevant to current and future public health challenges.
Keywords: Epidemiology, Public health practice, Health workforce, Emergency, Education, Emergencies
Background
Rapid and effective emergency response to address health security challenges relies heavily on a competent and suitably trained local and international workforce [1, 2]. The COVID-19 pandemic highlighted the importance of having a well-equipped health security workforce. Future epidemics of emerging infectious disease and other acute public health emergencies will continue to occur. To respond to these events, it is essential that training programs are providing graduates with the skills they need [3].
Well-trained field and applied epidemiologists are a crucial component of the health security workforce to prepare and effectively respond to health emergencies [1, 4]. Applied epidemiologists work in government and non-government organisations to detect, investigate, manage, and control infectious diseases [1, 4, 5], and have been described as “activists” who rapidly transform findings into policy and action [6].
Responsibility for applied epidemiology workforce development varies depending on the country [7, 8]. The Field Epidemiology Training Program (FETP) model [7] is a learn-by-doing training approach [4, 8, 9], where trainees are imbedded within their national health system. FETPs aim to improve public health systems through strengthening disease surveillance for evidence-based decision-making, and enhancing capacity for outbreak prevention, detection and response [8]. This training can vary in duration from 3 months for ‘frontline’ programs through to the 2 years for ‘advanced’ programs and are largely supported by Government health departments [10]. Academic institutions provide Master of Public Health or Epidemiology Programs, offering training in basic or advanced epidemiology, and biostatistics, with some offering specialist training in disaster management and/or humanitarian crisis management [11, 12].
The Ebola outbreak in West Africa, and more recently the COVID-19 pandemic, demonstrated the fragility of national and international public health response models [2]. These public health events have exposed the broader health system and health security implications of under-investing in public health systems and training field epidemiologists [2]. There is an urgent need to review the investment in health security workforce development, to ensure countries have an appropriately skilled and confident workforce to rapidly manage and contain public health emergencies.
In 2019, we interviewed public health experts about the needs and challenges of the epidemiology emergency response workforce. Experts outlined the need for collective competence and discussed the lack of training standardisation, the need for skills in leadership, communication, and also specialist training in emergency response [13]. To understand if current models of applied epidemiology training were meeting the needs of the emergency response workforce and to identify training needs, we conducted an online survey administered to applied epidemiologists. We analysed survey data to understand the knowledge and skills obtained during education and training in applied epidemiology.
Methods
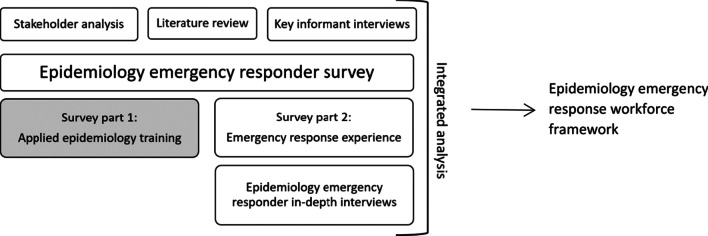
As part of a larger study looking at the effectiveness of the epidemiology workforce during emergency response [14], (Fig. 1) we conducted an online cross-sectional survey to identify training needs from the perspective of applied epidemiologists. For the purposes of this study, the ‘applied epidemiology workforce’ was defined as any person working in an applied or field epidemiology role or acute public health responder role.
Fig. 1.
Epidemiology emergency workforce research study model [14]
Study population
The target population for this survey was the global applied epidemiology workforce. We specifically targeted FETP alumni, however the survey was open to all people who had studied epidemiology and used this training in a practical setting.
Sampling
As there was no defined and reliable sampling frame, a combination of purposive and snowballing sampling techniques was used to identify the target population [15, 16].
Although the size of our study population for this survey was unknown due to our multiple recruitment methods, the primary means for survey distribution was the TEPHIConnect field epidemiology database, with 1700 registered active members as of September 2019. Using this as an indicative sampling frame, and the response rate from a previous unpublished survey by TEPHIConnect of 9.8%, we assessed that the final sample size of 282 in this study would to lead to estimates of a single proportion with a 95% confidence interval, with precision of ± 6%, after employing the finite population correction.
Recruitment
We recruited survey respondents through multiple sources. A YouTube video described the purpose of the study in English; this video included the option of subtitles in English or French. This video formed the basis of a social media recruitment campaign through Twitter, LinkedIn, and our dedicated study Facebook page. We disseminated participation reminders eight times through these social media channels over a 3-month period. We partnered with the global field epidemiology training alumni network, TEPHIConnect, who ran a social media campaign mirroring our campaign. The campaign stated that any person working in an applied epidemiology role could complete the survey. Individuals self-selected based on this criterion.
Postcards advertising the survey were distributed at the 10th TEPHINET Global Scientific Conference, the Australian Communicable Diseases Control Conference 2019, and the European Scientific Conference on Applied Infectious Disease Epidemiology (ESCAIDE 2019). In addition, the study population were directly invited to participate in the survey by email via field epidemiology networks including TEPHIConnect and national FETP networks. We encouraged survey respondents to forward the survey to their personal and professional network.
Consent
Participation in this study was voluntary; participants were directed to plain language information sheets, available online in French and English, prior to being able to access the survey. Each participant provided online consent prior to obtaining access to the survey questions. Respondents had the option to navigate the survey and remove or change answers prior to submission.
Ethics
This survey was approved by the Australian National University Human Research Ethics Committee, ID 2019-068.
Data collection
We used findings from key informant interviews conducted in 2019 [13, 17] and literature reviews to develop survey questions [18]. The questionnaire was reviewed by key informants and pre-tested with 11 individuals representative of the target population to test for construct and content validity.
The survey was divided into three modules: demographics, epidemiology training, and deployment experience. This paper reports findings from the first two modules. The demographics module included age, gender identity, citizenship, formal education, technical background, years of epidemiology experience, and emergency response experience. For FETP trainees and graduates, we asked about their highest FETP level achieved, based on the globally recognised categories of frontline (≤ 6 months), intermediate (9 months–1 year), and advanced (2 years) tiers [9].
The survey module on epidemiology training included five broad areas, each with a checkbox list of specific training items: surveillance (6 items), data analysis and assessment (15 items), leadership (9 items), social and communication skills (11 items), and emergency response (14 items). We termed what is commonly known as ‘soft skills’ or ‘interpersonal skills’ [19] as ‘social and communication skills’. The variation in terminology for this set of skills varied across the literature with little consensus, either too narrow in definition for this study or unclearly defined.
This module captured qualitative data via open-ended questions with free-text fields where respondents could identify further training gaps for each area, provide further comments, or list additional training received. Respondent were also asked to comment on whether the knowledge and skills gained during their training, and were appropriate and adequate for emergency response.
We developed and tested the survey in English, which was then translated into French. A native French-speaker re-checked the translation to ensure accuracy of meaning. The survey was self-administered online by respondents via REDCap (Research Electronic Data Capture) [20] between October 2019 and February 2020. No incentives were provided for participation.
Data analysis
Survey data were analysed descriptively in Microsoft Excel (2016) and Stata15 (TX:StataCorp) [21]. Data were analysed to explore associations within and between respondents. We compared self-recounted epidemiology training between FETP and non-FETP and gender. Reported FETP levels were not sub-analysed due to low numbers of respondents from frontline and intermediate programs. We used Pearson Chi-squared (Chi2) to test for significant differences between categorical variables. Answers to open-ended questions were analysed using Nvivo11 [22], data familiarisation led to open-coding of text; common categories were created iteratively and merged or expanded as needed [23, 24].
We used the six World Health Organization (WHO) regions to categorise respondents from different geographical areas according to: the Regional Office for Africa (AFRO), Regional Office for the Eastern Mediterranean (EMRO), the Regional Office for Europe (EURO), Pan American Health Organization (PAHO), South-East Asia Regional Office (SEARO), and the Western Pacific Region Office (WPRO) [25].
Results
Three hundred and thirty individuals consented to participate, of whom 282 (85%) completed the survey; 268 (95%) in English and 14 (5%) in French.
Respondents were able to select multiple options regarding how they were informed of the survey, 104 (32%) indicated Facebook, Twitter, and/or LinkedIn, similarly 105 (32%) indicated the TEPHINET/TEPHIConnect alumni network, 71 (22%) indicated they were notified through their country specific FETP network and 42 (13%) through personal or professional contact snowballing sampling.
Demographics
Gender distribution of respondents was similar, 51% female (n = 144/282). The median age of respondents was 39 (range: 23–77 years) (Table 1). Gender, age distribution, and education level were similar between FETP and non-FETP respondents.
Table 1.
Demographic characteristics of epidemiology emergency response survey respondents, 2019–2020 (n = 282)
| Category | Variable | Number (%) |
|---|---|---|
| Gender | ||
| Female | 144 (51.1%) | |
| Male | 135 (47.9%) | |
| Non-conforming | 0 (0%) | |
| Prefer not to answer | 3 (1.1%) | |
| Age (years) | ||
| < 20 | 0 (0%) | |
| 20–29 | 18 (6.4%) | |
| 30–39 | 140 (49.6%) | |
| 40–49 | 78 (27.7%) | |
| 50–59 | 37 (13.1%) | |
| 60–69 | 7 (2.5%) | |
| 70 + | 2 (0.7%) | |
| Technical backgrounda | ||
| Epidemiology | 225 (79.8%) | |
| Public Health | 158 (56%) | |
| Medicine | 70 (24.8%) | |
| Laboratory | 35 (12.4%) | |
| Nursing | 25 (8.9%) | |
| Data science | 21 (7.4%) | |
| Veterinary | 19 (6.7%) | |
| Social Science | 14 (5.0%) | |
| Other | 23 (8.2%) | |
aMultiple technical backgrounds per respondent
The majority of respondents reported a professional or technical background in epidemiology (79.8% n = 225/282, Table 1) with postgraduate or doctorate-level qualifications (91.5% n = 258/282, Table 2). When disaggregated by gender, there were twice as many male laboratory specialists (65.7% n = 23/35 p = 0.028) and significantly more female social scientists (78.5% n = 11/14 p = 0.038). There were more females who identified as epidemiologists (53% n = 120/225), nurses (64% n = 16/25), and public health specialists (53% n = 84/158), however, a statistically significant difference was not detected.
Table 2.
Professional background characteristics of epidemiology emergency response survey respondents, 2019–2020 (n = 282)
| Category | Variable | Number (%) |
|---|---|---|
| Epidemiology and Public heath traininga | n = 282 | |
| Master of Public Health (or similar) | 92 (32.6%) | |
| Other relevant Masters | 13 (4.6%) | |
| Public Health Physician training | 10 (3.5%) | |
| PhD | 18 (6.4%) | |
| Field Epidemiology Training Program (FETP) | 210 (74.5%) | |
| FETP | n = 282 | |
| Yes | 178 (63.1%) | |
| Trainee at time | 32 (11.3%) | |
| No | 72 (25.5%) | |
| FETP level | n = 210 (including trainees) | |
| Advanced (2 years) | 189 (90%) | |
| Intermediate (9 months – 1 year) | 7 (3.4%) | |
| Frontline (< 6 months) | 7 (3.4%) | |
| Unanswered | 7 (3.4%) | |
| Years since FETP graduation | n = 210 | |
| 10 or less | 157 (74.8%) | |
| 10 + | 37 (17.6%) | |
| Unanswered | 16 (7.6%) | |
| Epidemiology experience | n = 282 | |
| < 1 years | 12 (4.3%) | |
| 1– < 2 years | 23 (8.2%) | |
| 2– < 5 years | 77 (27.3%) | |
| 5– < 8 years | 64 (22.7%) | |
| 8– < 12 years | 42 (14.9%) | |
| 12+ years | 59 (20.9%) | |
| Not applicable | 4 (1.4%) | |
| Unanswered | 1 (0.4%) | |
aMultiple training types per respondent
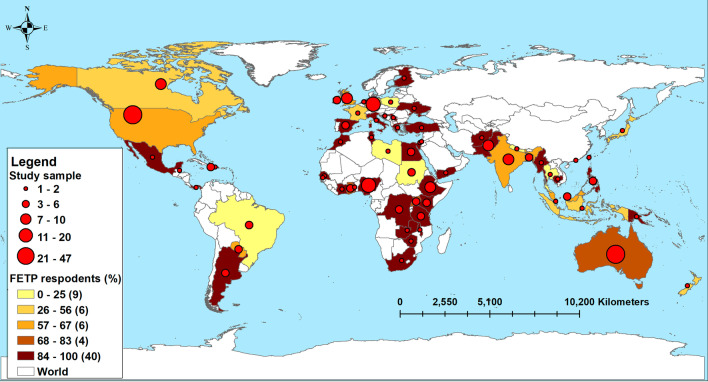
Respondents came from 64 countries, with the highest proportion from the United States of America (16.7% n = 47/282), Australia (13.8% n = 39/282), and Nigeria (7.1% n = 20/282). When stratified by WHO regions, the highest response was from the America’s (PAHO) (Fig. 2). Respondents in AFRO and SEARO were more likely to be male (76% n = 51/67, 85% n = 23/27, respectively), with a higher proportion of female respondents in PAHO and WPRO (69% n = 53/76, 71% n = 41/57, respectively). Gender distribution within EMRO and EURO respondents was similar. Age distribution across all regions was similar and FETP respondents made up between 65% and 89% of respondents (Fig. 2).
Fig. 2.
Distribution of epidemiology emergency response survey respondents by country and training type, 2019–2020 (n = 282)
Respondents reported a variety of formal public health and epidemiology training, including, FETP, postgraduate master’s programs, doctorate programs, physician public health training, and short courses in specified public health and epidemiology topics (Table 2). The majority of respondents (74%, n = 210/282) indicated they were graduates or trainees of an FETP, 90% (n = 189/210) of whom reported to have studied the advanced program (Table 2). Respondents had predominately (74.8%, n = 157/210) graduated from their FETP within the past 10 years (Table 2), with the earliest graduation being 1992. Professional epidemiology experience varied with 40% (n = 112/282) of respondents reporting less than 5 years, and 20% (n = 59/282) reporting more than 12 years of experience (Table 2).
Epidemiology training
Outbreak and surveillance
Six outbreak and surveillance categories were listed in the survey (Table 3a). Training in general outbreak and surveillance was commonly reported by the respondents, however less commonly reported was targeted training in emergency response surveillance, community-based surveillance or syndromic surveillance (Table 3a). When comparing the respondents who had completed an FETP with those who had not participated in an FETP, FETP graduates reported higher levels of formal training in all surveillance and outbreak investigation categories (Table 3a).
Table 3.
Reported epidemiology training, comparison between FETP and non-FETP epidemiology emergency response survey respondents, 2019–2020 (n = 282)
| Section | Category | Topic | Total n = 282 | Total % | Non-FETP n = 72 | Non-FETP% | FETP n = 178 | FETP% |
|---|---|---|---|---|---|---|---|---|
| a | Training in outbreak and surveillance | |||||||
| Basic principles of surveillance | 262 | 92.9 | 58 | 80.6 | 173 | 97.2 | ||
| Syndromic surveillance | 165 | 58.5 | 23 | 31.9 | 118 | 66.3 | ||
| Community-based surveillance | 157 | 55.7 | 34 | 47.2 | 104 | 58.4 | ||
| Emergency response surveillance | 168 | 59.6 | 29 | 40.3 | 119 | 66.8 | ||
| Outbreak investigation steps | 250 | 88.7 | 51 | 70.8 | 168 | 94.4 | ||
| Outbreak investigation methods | 238 | 84.4 | 47 | 65.3 | 160 | 89.9 | ||
| b | Training in analysis and epidemiology methods | |||||||
| Rapid survey | 162 | 57.4 | 35 | 48.6 | 107 | 60.1 | ||
| Mortality survey | 84 | 29.8 | 21 | 29.2 | 51 | 28.6 | ||
| Nutrition survey | 52 | 18.4 | 13 | 18.1 | 32 | 18 | ||
| Other survey | 107 | 37.9 | 17 | 23.6 | 75 | 42.1 | ||
| Denominator estimation | 83 | 29.4 | 20 | 27.8 | 52 | 29.2 | ||
| Needs assessment | 101 | 35.8 | 24 | 33.3 | 66 | 34.1 | ||
| Risk assessment | 152 | 53.9 | 34 | 47.2 | 98 | 55.1 | ||
| Managing complex datasets | 78 | 27.7 | 23 | 31.9 | 47 | 26.4 | ||
| R | 34 | 12.1 | 12 | 16.7 | 18 | 10.1 | ||
| Stata | 123 | 43.6 | 28 | 38.9 | 79 | 44.4 | ||
| Epi Info | 205 | 72.7 | 31 | 43.1 | 149 | 83.7 | ||
| Excel | 187 | 66.3 | 35 | 48.6 | 131 | 73.6 | ||
| Data visualisation | 112 | 39.7 | 26 | 36.1 | 67 | 37.6 | ||
| Transmission trees | 36 | 12.8 | 11 | 15.3 | 20 | 11.2 | ||
| Spatial analysis | 71 | 25.2 | 19 | 26.4 | 38 | 21.4 | ||
| c | Training in leadership and management | |||||||
| Evidence-based decision-making | 159 | 56.4 | 35 | 48.6 | 108 | 60.7 | ||
| Mentoring | 98 | 34.8 | 10 | 13.9 | 74 | 41.6 | ||
| Leadership | 130 | 46.1 | 19 | 26.4 | 91 | 51.1 | ||
| Managing a team | 119 | 42.2 | 20 | 27.8 | 85 | 47.8 | ||
| Peer teaching | 93 | 33 | 9 | 12.5 | 70 | 39.3 | ||
| Team work | 184 | 65.2 | 33 | 45.8 | 126 | 70.8 | ||
| Prioritisation | 87 | 30.9 | 17 | 23.6 | 60 | 33.7 | ||
| Delegating responsibility | 73 | 25.9 | 13 | 18.1 | 52 | 29.2 | ||
| Partner coordination | 84 | 29.8 | 15 | 20.8 | 60 | 33.7 | ||
| Reflective practices | 33 | 11.7 | 8 | 11.1 | 21 | 11.8 | ||
| d | Training in social and communication skills | |||||||
| Basic scientific communication skills | 244 | 86.5 | 48 | 66.7 | 166 | 93.3 | ||
| Practical field communication skills | 149 | 52.8 | 24 | 33.3 | 107 | 60.1 | ||
| Media communication | 136 | 48.2 | 24 | 33.3 | 94 | 52.8 | ||
| Cultural competency | 72 | 25.5 | 22 | 30.6 | 42 | 23.6 | ||
| Participant consent | 152 | 53.9 | 30 | 41.7 | 100 | 56.2 | ||
| Stress management | 60 | 21.3 | 9 | 12.5 | 43 | 24.2 | ||
| Social media | 32 | 11.3 | 5 | 6.9 | 22 | 12.4 | ||
| Interview techniques | 144 | 51.1 | 31 | 43.1 | 95 | 53.4 | ||
| Ethics | 169 | 59.9 | 40 | 55.6 | 111 | 62.4 | ||
| Relationship building | 62 | 22 | 14 | 19.4 | 38 | 21.3 | ||
| e | Training in emergency response training | |||||||
| Role of the epidemiologist during emergency response | 169 | 59.9 | 33 | 45.8 | 113 | 63.5 | ||
| Epidemiology of public health disasters | 166 | 58.9 | 32 | 44.4 | 114 | 64 | ||
| Humanitarian principles | 67 | 23.8 | 18 | 25 | 42 | 23.6 | ||
| Principles of escalation/scaling a response | 45 | 16 | 9 | 12.5 | 30 | 16.9 | ||
| Methods of data collection in an emergency | 147 | 52.1 | 31 | 43.1 | 96 | 53.9 | ||
| Ethics during emergencies | 82 | 29.1 | 18 | 25 | 53 | 29.8 | ||
| IMS—Incident Management System | 73 | 25.9 | 14 | 19.4 | 46 | 25.8 | ||
| EOC role—Emergency Operations Centre | 93 | 33 | 17 | 23.6 | 63 | 35.4 | ||
| IHR—International Health Regulations | 121 | 42.9 | 15 | 20.8 | 87 | 48.9 | ||
| HeRAMS: Health Resources Availability Monitoring System | 11 | 3.9 | 1 | 1.4 | 8 | 4.5 | ||
| EWARS: Early Warning, Alert and Response System (EWARS in a box) | 79 | 28 | 12 | 16.7 | 58 | 32.6 | ||
| Personal safety (use of PPE—personal protective equipment) | 130 | 46.1 | 26 | 36.1 | 88 | 49.4 | ||
| Border control (POE—point of entry) | 46 | 16.3 | 8 | 11.1 | 30 | 16.9 | ||
Respondents highlighted the need for additional opportunities for knowledge consolidation and skill development in both outbreak and surveillance, specifying the need for teaching grounded within the political and social context (Box 1). Additional training was requested on responding to less common events such as environmental, chemical and radiological disasters (Box 1).
Box 1. Outbreak and surveillance training gaps reported by epidemiology emergency response survey respondents, 2019–2020
| Application of practical skills | “I feel we were given enough knowledge but did not apply it in practice.” |
| “I believe that I wanted to have more opportunities to apply in practice what I learned theoretically.” | |
| “While we acquire lots of knowledge, the practical competencies could be more developed by being in the field during the training program” | |
| Course relevance | [training] “was mostly based around field epidemiology in stable, developing world settings. It's mostly related to the work of government departments.” |
| “The knowledge and skills learnt were more geared toward outbreak response … Even then, looking back they were somewhat outdated and didn't necessarily reflect the political culture within which outbreaks occur.“ | |
| Knowledge | [I wanted training] “related to chemical, radiological and explosive emergencies” |
Data analysis and epidemiology methods
Fifteen emergency response training categories were listed in the survey (Table 3b). Reported training in specific methodology and data analysis skills needed during emergency response was limited. Training on estimation of population size during emergencies was reported by 29.4% (n = 83/282), which was similar for both FETP (29.2% n = 52/178) and non-FETP (27.8% n = 20/72) respondents. Thirty-six percent (n = 101/282) of respondents reported receiving training on how to conduct a needs assessment, and 53.9% (n = 152/282) on how to conduct a risk assessment. Training in survey development and implementation of specialised survey methods, such as nutrition and mortality surveys, were uncommonly reported (18.4% n = 52/282, and 29.8% n = 84/282, respectively), as were analytical techniques such as transmission trees (12.8% n = 36/282) and spatial analysis (25.2% n = 71/282) (Table 3b). Only 28% (n = 78/282) of respondents had received training in managing complex datasets.
The most common statistical and data management packages that respondents reported learning during their training was Epi Info™ (72.7% n = 205/282), followed by Microsoft Excel (66.3% n = 187/282) and Stata Statistical Software (43.6% n = 123/282) (Table 3b). A higher proportion of FETP graduates were trained in statistical packages compared to non-FETP graduates, with 83.7% (n = 149/178) of FETP trained respondents taught Epi Info™ compared to 43.1% (n = 31/72) non-FETP. Microsoft Excel training was reported by 73.6% (n = 131/178) of FETP trained respondents compared to 48.6% (n = 35/752) of non-FETP respondents.
Respondents highlighted additional training needs in specific software increasingly used in applied field epidemiology; specifically, training in R statistical software, population denominator estimation, spatial analysis, and geo-spatial mapping.
Leadership and management
Ten leadership and management training categories were listed in the survey (Table 3c) Sixty-five percent (n = 184/282) of respondents reported having received training in teamwork, and 56.4% (n = 159/282) reported training in evidence-based decision-making. Responses to the remaining eight items in the leadership and management module of the survey indicated that these were missing from most training programs. Less than 50% of respondents reported having learnt leadership and management skills during their applied epidemiology training (Table 3c). For example, only 11.7% (n = 33/282) of respondents reported training in skill development related to reflective practices.
Although leadership training was not widely reported, FETP trained respondents reported a higher percentage of training in all leadership categories compared to non-FETP, especially in mentoring and peer teaching (Table 3c). Within each category in this section, males reported much higher leadership and management exposure, with the exception of peer teaching. Of note, during training 45.9% (n = 62/135) of male respondents reported having been taught mentoring, compared to 24.3% (n = 35/144) of female respondents, 61.5% (n = 83/135) of males reported training in leadership skills compared to 31.3% (n = 45/144) of females, and 34.1% (n = 46/135) of males reported training in delegation skills compared to 17.4% (n = 25/144) of females (Table 4).
Table 4.
Reported training in leadership and management, comparison of epidemiology emergency response survey by gender, 2019–2020 (n = 282)
| Topic | Female n = 144 (%) | Male n = 135 (%) |
|---|---|---|
| Evidence-based decision-making | 77 (53.5%) | 80 (59.3%) |
| Mentoring | 35 (24.3%) | 62 (45.9%) |
| Leadership | 45 (31.3%) | 83 (61.5%) |
| Managing a team | 45 (31.3%) | 72 (53.3%) |
| Peer teaching | 51 (35.4%) | 42 (31.1%) |
| Team work | 89 (61.8%) | 92 (68.1%) |
| Prioritisation | 38 (26.4%) | 47 (34.8%) |
| Delegating responsibility | 25 (17.4%) | 46 (34.1%) |
| Partner coordination | 37 (25.7%) | 45 (33.3%) |
Social and communication skills
Ten training categories were listed in the survey under social and communication skills (Table 3d). The majority (86.5% n = 244/282) of respondents reported training in basic scientific communication such as report writing and presentation preparation. Training in other communication techniques was less frequently reported; including training in practical communication in the field (52.8% n = 149/282), media communication (48.2% n = 136/282), cultural competence (25.5% n = 72/282), and social media communication (11.3% n = 32/282) (Table 3d). Approximately 20% of respondents reported training in stress management (n = 60/282) and relationship building (n = 62/282). Interview techniques, issues related to consent, and practical ethical approaches to field work were reported by just over half of the respondents (Table 3d). With the exception of cultural competence, non-FETP trained participants reported less training than FETPs to each category in this section (Table 3d).
Free text responses highlighted the need for more training in social and communication skills, (Box 2). Additionally, respondents indicated the need for further training in traditional media and social media. (Box 2). Respondents also stated that training with a focus on cultural, political, and contextual understanding was needed, as was training on qualitative research methods, stress management, and prioritisation (Box 2).
Box 2. Social and communication training gaps reported by epidemiology emergency response survey respondents, 2019–2020
| Communication | “I think a really valuable skill that should be taught in epidemiology is how to influence others with the data story. This isn't about most fancy, complicated analysis, but about working out what's important in the data for decision-making” |
| Social science and anthropological skills | “My training as an anthropologist and social scientist significantly enhanced my skills as an epidemiologist. These are new concepts and under recognized and underused” |
| “I will welcome more knowledge in behavioural change and anthropology during the training” |
Emergency response
Fourteen emergency response training items were listed in the survey with half (n = 7) of them reported by less than 30% of respondents each (Table 3e). Non-FETP respondents reported less training than FETP graduates in each of these emergency response categories (Table 3e).
When respondents were asked whether they believed emergency response training should be a core component of applied epidemiology training, almost 75% (n = 211/282) replied yes, and 18% (n = 50/282) suggested it should be optional.
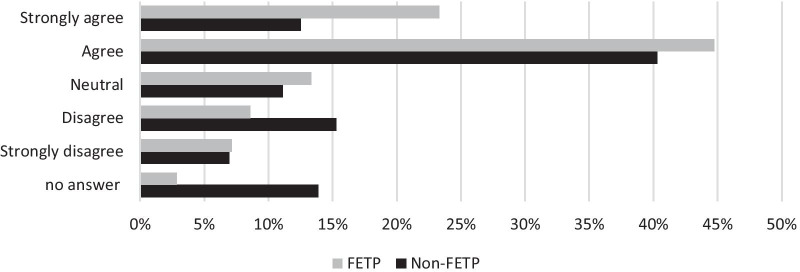
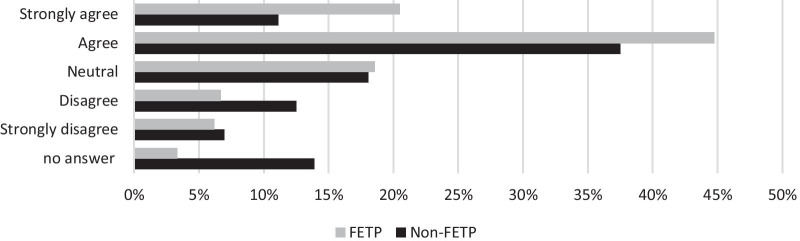
Despite relatively low proportions of respondents having received formal training in the listed emergency response categories, 64% (n = 181/282) agreed or strongly agreed that their epidemiology training gave them the required knowledge to work as an epidemiologist during emergency response (Fig. 3). Additionally, 65% (n = 172/282) believed they had learnt the required skills for epidemiology emergency response (Fig. 4). FETP respondents were more likely to answer positively to these questions than non-FETP (Figs. 3 and 4).
Fig. 3.
FETP and non-FETP respondents' perceptions of epidemiology training providing the knowledge required for emergency responses (n = 282)
Fig. 4.
FETP and non-FETP respondents' perceptions of epidemiology training providing the skill required for emergency responses (n = 282)
Respondents requested additional training on the role of an epidemiologist during emergency response, personal and professional characteristics needed during a response, epidemiology methods in emergency response, humanitarian principles, as well as training on the emergency response structure (Box 3).
Box 3 Emergency response training gaps reported by epidemiology emergency response survey respondents, 2019–2020
| Emergency response | “Being fit for the field, i.e. not everyone who has completed the program should be in the field” |
| “Specific things like bioterrorism and natural disasters and hurricane response” | |
| “Critical skills to data analysis and collection during an emergency, rarely having a denominator, working with dirty data, working with MoH's [Ministry of Health] without statistical packages” | |
| “Did not learn enough about the different approaches and methods that are/should be used in an emergency setting vs a regular ongoing surveillance or outbreak response setting” | |
| “Thinking systems in the middle of an emergency” | |
| “A session on the realities of an emergency situation would be useful” | |
| “There was minimal relevant to emergency response or low resource settings” | |
| Response structure | “How humanitarian responses are structured—what is happening around you in such a response and concrete feedback about where epi skills and information can serve those components |
| “There were no emergency response topics covered in my epi training… no mention of IHR [International Health Regulations]” “ | |
| Roles and responsibilities | Role of Field Epidemiologist during Humanitarian crisis still confuses me” |
| “Even at the advanced level and despite being "on the ground", does not have the capacity of those trained in the roles of the epidemiologist in emergency situations or health crises, in rapid interventions” | |
| “In a situation with an environmental disaster (e.g. air pollution), the epidemiologist has no preparation on his role in such an event. Other areas: Mass casualty, major water contamination, exposure to chemicals due to explosions, etc... responders are prepared, but the epidemiologist is not” |
Discussion
Our survey on epidemiology training for emergency response identified core training needs of the applied epidemiology workforce. Our findings indicate that respondents believe their training in outbreak and surveillance, regardless of different training models, was sufficient. Respondents did, however, identify training gaps in the areas of social and communication skills, leadership and management, data analysis, epidemiology methods, and emergency response. Additionally, respondents identified that training methods needed to focus more on application of practical skills.
The COVID-19 pandemic has been another reminder of the importance of communication skills in connecting with the public during a public health emergency and the essential role of effective communication in the successful implementation of control measures [26–28]. Applied epidemiologists are often required to draw on a variety and diverse range of communication skills in order to effect change. These skills range from communicating risk to the public, communicating methods and findings to peers and designing messages that will support policy and decision-makers to implement an effective public health response. As the applied epidemiology definition by Thacker and Buffington [6] states, applied epidemiology is about “transforming findings to policy and action”, and as one of the respondents wrote, “it is not just about collecting data but it is about influencing others with the story”. Our survey identified gaps in applied epidemiology training in the areas of cultural competence, understanding the socio-political context, and anthropological principles. This training deficit was documented in a study of emergency response epidemiologists who responded to the 2014–2016 West Africa Ebola crisis [19], and a study looking to understand outbreak investigation training [29]. Despite the crucial need for these skills to function optimally as applied epidemiologists, survey respondents highlighted that these skills were not routinely taught in their applied epidemiology training.
Leadership and management skills are crucial for responding effectively and efficiently to public health events. One of the primary aims of FETPs is to train future public health leaders [8, 30, 31], with leadership and management listed as a core FETP competency. However, all training categories in the leadership and management section of our survey were uncommonly reported by respondents, with the exception of working in a team. Holding et al. [19] study post the West Africa Ebola crisis found a similar deficit in leadership training, as did Samet and Brownson [32] in their study of epidemiology graduates in the United States. A key characteristic of applied epidemiology is making evidence-based decisions, however only about half of respondents reported having received training on this.
While we did not identify any significant difference between respondents in regards to gender, level of education, or type of education, we identified significant difference in leadership and decision-making training between males and females. In this self-reported survey, this raises questions on whether leadership has the same meaning or interpretation across genders. The difference in response between genders may be linked to stereotypes and individual definitions around what constitutes leadership [33–35]. Traditionally, leadership has been linked to masculine traits, which then also devalue the feminine style of leadership [34, 35]. Johnson and Blair discuss how COVID-19 is shifting this understanding of leadership [34]. This concept of gender is important for leadership in emergencies and associated training needs further exploration through operational research.
When focusing on technical epidemiological skills, few respondents reported training in estimation of population density or specialised surveys such as mortality or nutrition surveys. Médecins Sans Frontières (MSF) have listed key competencies for epidemiologists in emergency response; including experience in practical applied research methods, as well as survey development and implementation (including mortality and nutritional surveys) [36]. Few respondents reported having received training in these specialised skills. Graduates of FETP programs who are trained to respond to public health events, without training in population estimation, population surveys, risk and needs assessment, would struggle to respond effectively to public health emergencies. Standardisation of FETP curriculum and core concepts regarding emergency response is urgently needed [37].
In addition, respondents to our survey highlighted the need to further understand the role of an epidemiologist during an emergency response, and the emergency response structure. Emergency response, whether it be a local or international public health emergency, should be a core competency of applied epidemiologists, who are often early responders. To be adequately equipped, this workforce needs more specialised skills in emergency response which appear to be neglected in the current models of applied epidemiology training. Continuous professional development activities should be considered for this workforce to ensure skills and knowledge is maintained, developed and responsive to changes in the field epidemiology emergency response landscape.
In our survey, there was an evident lack of training in practices that support the applied epidemiology workforce to remain strong and healthy and prevent burnout, such as stress management and reflective practices. Many countries struggle to retain field epidemiologists due to occupational burnout or career path limitations [7, 31, 38]. Ryu et al. [7] study on field epidemiology occupational stress, suggests that burnout is a very real concern given the frontline nature of outbreak and emergency response.
Although this survey focused on individuals’ training experience, our findings may be used to explore challenges to the broader workforce. We need to consider what capacities are required for the management and control of public health emergencies, not just the individual needs of each trainee [39]. Investment in a resilient applied epidemiology workforce means ensuring the workforce have the skills and knowledge needed to fulfil the various health security roles they will play now and in the future [5, 29, 32, 37].
Study limitations
It is important to recognise some limitations with this study that may impact on our findings. We collected data through an opt-in self-administered online survey. The survey was not offered in any other format, therefore those without internet access were not able to participate, which means we may have excluded people working at the community level. We attempted to limit the effect of selection-biases introduced because of our approach to sampling by using multiple sources and methods to recruit participants. We offered the survey in two languages, French and English, as these are the common languages used during recent international emergency responses. We are cautious in generalising our findings to the applied epidemiology workforce, however, our sample size was large enough to identify common categories.
It was difficult for us to identify an accurate study target population sampling frame. The applied epidemiology workforce in most countries is informal and often poorly documented with the definition of ‘epidemiologist’ varying between individuals and organisations. The work title of an epidemiologist is largely through self-identification. Due to this limitation, we designed a cross-sectional survey distributed through professional networks. The study target population was defined as anyone who self-identified as having worked in an applied epidemiology role. However, because of this design we are unable to comment on how survey respondents differed from non-respondents.
As the timing of the survey was not during or immediately after the respondents’ training in epidemiology, recall bias may have affected the information obtained. Respondents also had varying years and types of experience and time since graduation. This gap between training and our survey may have been advantageous as respondents may have had time to reflect on what went well and what could be improved [40, 41].
In recent years, FETP training has expanded to three levels including a frontline and intermediate program, although few representatives from these programs accessed the survey. Future applied epidemiology workforce surveys should be targeted at graduates of these programs. Despite these limitations, our study offers insight into gaps in training for applied epidemiologists, which is supported by other operational research.
Conclusion
Our survey identified that applied epidemiology training needs to evolve to provide capacity and skills to respond to dynamic and complex public health emergencies. There is a need to address the identified training gaps in leadership, communication and social skills, as well as emergency response. This will strengthen the applied epidemiology workforce, as well as the health systems they function within and the local, national, regional and global emergencies they respond to. Continuous professional development activities must also be available to support the current workforce adapt, as well as augment new graduates to be suitably skilled for the challenges ahead.
Acknowledgements
Thank you to the survey respondents for sharing your knowledge and experience. Thank you to TEPHIConnect, FETP program directors, and TEPHINET networks, for distributing the survey to members and for support with recruitment. Thank you also to Dr Kinley Wangdi for support with mapping, and Dr Alice Richardson for statistical advice. Finally, thank you for the constructive comments made by our reviewers to strengthen this paper.
Abbreviations
- AFRO
Regional Office for Africa
- COVID-19
Coronavirus Disease 2019
- EMRO
Regional Office for the Eastern Mediterranean
- EOC
Emergency Operations Centre
- ESCAIDE
European Scientific Conference on Applied Infectious Disease Epidemiology
- EURO
Regional Office for Europe
- EWARS
Early Warning, Alert, and Response System
- FETP
Field Epidemiology Training Program
- HeRAMS
Health Resources Availability Monitoring System
- IHR
International Health Regulations
- IMS
Incident management systems
- MPH
Master of Public Health
- MSF
Médecins Sans Frontières
- PAHO
The Pan American Health Organization
- POE
Point of Entry
- PPE
Personal protective equipment
- REDCap
Research Electronic Data Capture
- SEARO
South-East Asia Regional Office
- TEPHINET
Training Programs in Epidemiology and Public Health Interventions Network
- TEPHIConnect
TEPHINET alumni network
- WHO
World Health Organization
- WPRO
Western Pacific Region Office
Authors' contributions
AP wrote the manuscript and is leading the study; TH, BO, DD, MK supported study design development, TH, BO, DD, MK, SC supported data analysis interpretation and revised the manuscript critically. All authors read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. AP receives Commonwealth and ANU science merit scholarships, along with funding from the Australian National Health. AP and SC are funded through the Medical Research Council (NHMRC) Integrated Systems for Epidemic Response (APP1107393). MK is supported by an NHMRC fellowship (APP1145997) and receives funding from the NHMRC for Integrated Systems for Epidemic Response. The funders did not have any role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Availability of data and materials
All data relevant to this manuscript are included within the manuscript tables, figures and/or reference links.
Declarations
Ethics approval and consent to participate
This survey was approved by the Australian National University Human Research Ethics Committee, ID 2019-068. Each participant completed a consent form prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amy Elizabeth Parry, Email: amy.parry@anu.edu.au.
Martyn D. Kirk, Email: martyn.kirk@anu.edu.au
David N. Durrheim, Email: David.Durrheim@newcastle.edu.au
Babatunde Olowokure, Email: olowokureb@who.int.
Samantha M. Colquhoun, Email: samantha.colquhoun@anu.edu.au
Tambri Housen, Email: Tambri.Housen@newcastle.edu.au.
References
- 1.O’Carroll P, Kirk M, Baggett K, Herrera D. The global field epidemiology roadmap. 2018 (cited 2020 Sep 9). https://www.tephinet.org/sites/tephinet/files/content/attachment/2018-11-26/The%20Global%20Field%20Epidemiology%20Roadmap_11.26.18.FINAL_.pdf.
- 2.World Health Organization. Working for health and growth: investing in the health workforce. World Health Organization; 2016 (cited 2020 Sep 11). Report No.: ISBN 978 92 4 151130 8. https://apps.who.int/iris/bitstream/handle/10665/250047/9789241511308-eng.pdf;jsessionid=935A6223EF4D1BFCE447E2ABDD915AC3?sequence=1.
- 3.Dhama K, Patel SK, Sharun K, Pathak M, Tiwari R, Yatoo MI, et al. SARS-CoV-2 jumping the species barrier: Zoonotic lessons from SARS, MERS and recent advances to combat this pandemic virus. Travel Med Infect Dis. 2020;37:101830. doi: 10.1016/j.tmaid.2020.101830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nsubuga P, White M, Fontaine R, Simone P. Training programmes for field epidemiology. Lancet. 2008;371(9613):630–631. doi: 10.1016/S0140-6736(08)60281-0. [DOI] [PubMed] [Google Scholar]
- 5.Bensyl DM, King ME, Greiner A. Applied epidemiology training needs for the modern epidemiologist. Am J Epidemiol. 2019;188(5):830–835. doi: 10.1093/aje/kwz052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thacker SB, Buffington J. Applied epidemiology for the 21st Century. Int J Epidemiol. 2001;30(2):320–325. doi: 10.1093/ije/30.2.320. [DOI] [PubMed] [Google Scholar]
- 7.Ryu S, Kim YW, Kim S, Liao Q, Cowling BJ, Lee C-S. Occupational stress among field epidemiologists in field epidemiology training programs from the public health sector. Int J Environ Res Public Health. 2019;16(18):3427. doi: 10.3390/ijerph16183427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider D, Evering-Watley M, Walke H, Bloland PB. Training the global public health workforce through applied epidemiology training programs: CDC’s experience, 1951–2011. Public Health Rev. 2011;33(1):190–203. doi: 10.1007/BF03391627. [DOI] [Google Scholar]
- 9.Training Programs | TEPHINET (cited 2020 Sep 30). https://www.tephinet.org/training-programs.
- 10.Traicoff DA, Walke HT, Jones DS, Gogstad EK, Imtiaz R, White ME. Replicating success: developing a standard FETP curriculum. Public Health Rep. 2008;123(Suppl 1):28–34. doi: 10.1177/00333549081230S109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riley M, Health JBS of P. Concentrations. Johns Hopkins Bloomberg School of Public Health (cited 2020 Oct 24). https://www.jhsph.edu/academics/degree-programs/master-of-public-health/curriculum/concentrations.html.
- 12.London School Hygiene and Tropical Medicine. LSHTM MSc Public Health, programme handbook 2020–21 (cited 2020 Oct 24). https://www.lshtm.ac.uk/files/ph-handbook.pdf.
- 13.Parry, Amy Elizabeth, Kirk, MD, Durrheim, DN, Olowokure, B, Colquhoun S, Housen T. Emergency response and the need for collective competence in epidemiological teams. Bull World Health Organ. 2021 (cited 2021 Mar 20); early release. https://cdn.who.int/media/docs/default-source/bulletin/online-first/blt.20.276998.pdf?sfvrsn=e2e61bf0_5. [DOI] [PMC free article] [PubMed]
- 14.Parry AE, Kirk MD, Durrheim DN, Olowokure B, Housen T. Study protocol: building an evidence base for epidemiology emergency response, a mixed-methods study. BMJ Open. 2020;10(6):e037326. doi: 10.1136/bmjopen-2020-037326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deborah K. Padget. SAGE Publications: Qualitative and Mixed Methods in Public Health; 2012. [Google Scholar]
- 16.Teddlie C, Yu F. Mixed methods sampling: a typology with examples. J Mix Methods Res. 2007;1(1):77–100. doi: 10.1177/1558689806292430. [DOI] [Google Scholar]
- 17.Parry AE, Kirk MD, Colquhoun SM, Housen T. Enhancing the effectiveness of the epidemiology workforce responding to Covid-19. BMJ. 2020 (cited 2020 Jul 21);368(m1075). https://www.bmj.com/content/368/bmj.m1075/rr-0.
- 18.David de Vaus. Surveys in Social Research. 6th edition. Allen & Unwin - Australia; 2014.
- 19.Holding M, Ihekweazu C, Stuart JM, Oliver I. Learning from the epidemiological response to the 2014/15 ebola virus disease outbreak. J Epidemiol Glob Health. 2019;9(3):169–175. doi: 10.2991/jegh.k.190808.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.About-REDCap (cited 2020 Sep 30). https://projectredcap.org/about/
- 21.StataCorp. Stata Statistical Software. College Station, TX: StataCorp LLC; 2017.
- 22.QSR International Pty Ltd. NVivo 11. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home.
- 23.Liamputtong P. Qualitative Research Methods. South Melbourne, Vic., Oxford University Press; 2009 (cited 2018 Jul 25). https://trove.nla.gov.au/work/7394612.
- 24.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 25.Regional offices (cited 2020 Sep 30). https://www.who.int/about/who-we-are/regional-offices.
- 26.Rubinelli S, Myers K, Rosenbaum M, Davis D. Implications of the current COVID-19 pandemic for communication in healthcare. Patient Educ Couns. 2020;103(6):1067–1069. doi: 10.1016/j.pec.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooley L. Trust and communication: responding to uncertainty. J Patient Exp. 2020;7(3):277–278. doi: 10.1177/2374373520938476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finset A, Bosworth H, Butow P, Gulbrandsen P, Hulsman RL, Pieterse AH, et al. Effective health communication—a key factor in fighting the COVID-19 pandemic. Patient Educ Couns. 2020;103(5):873–876. doi: 10.1016/j.pec.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forbes O, Davis S, Dyda A, Rosewell A, Williams S, Moffatt C, et al. Expert perspectives on outbreak investigation training: a quality improvement exercise. Glob Biosecurity. 2020 (cited 2020 Oct 29);1(4). http://jglobalbiosecurity.com/articles/53/print/.
- 30.Training programmes for field epidemiology—the Lancet (cited 2020 Oct 27). https://www.thelancet.com/journals/lancet/article/PIIS0140673608602810/fulltext?rss=yes.
- 31.Jones DS, Dicker RC, Fontaine RE, Boore AL, Omolo JO, Ashgar RJ, et al. Building global epidemiology and response capacity with field epidemiology training programs. Emerg Infect Dis. 2017;23(Suppl 1):S158–S165. doi: 10.3201/eid2313.170509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Samet JM, Brownson RC. Epidemiology in a changing world. Am J Prev Med. 2014;47(5):S383–S385. doi: 10.1016/j.amepre.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 33.Dhatt R, Theobald S, Buzuzi S, Ros B, Vong S, Muraya K, et al. The role of women’s leadership and gender equity in leadership and health system strengthening. Glob Health Epidemiol Genomics. 2017 ed (cited 2020 Oct 27);2. https://www.cambridge.org/core/journals/global-health-epidemiology-and-genomics/article/role-of-womens-leadership-and-gender-equity-in-leadership-and-health-system-strengthening/A6AEB63AFE17295E0EF9E40741A2EC5B. [DOI] [PMC free article] [PubMed]
- 34.Johnson C, Williams B. Gender and political leadership in a time of COVID. Polit Gend. 2020. pp. 1–8.
- 35.Randell S, Yerbury H. An exploration of the metaphors and images used to describe leadership in two different cultural contexts. Front Educ. 2020 (cited 2020 Oct 31);5. https://www.frontiersin.org/articles/10.3389/feduc.2020.00151/full?utm_source=F-AAE&utm_medium=EMLF&utm_campaign=MRK_1411754_21_Educat_20200825_arts_A.
- 36.Médecins Sans Frontières (MSF) International. Who we are. Médecins Sans Frontières (MSF) International (cited 2019 Jul 15). https://www.msf.org/who-we-are.
- 37.Thoroughman D. Applied epidemiology competencies: experience in the field. Public Health Rep. 2008;123(Suppl 1):8–10. doi: 10.1177/00333549081230S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pourshaban D, Basurto-Dávila R, Shih M. Building and sustaining strong public health agencies: determinants of workforce turnover. J Public Health Manag Pract JPHMP. 2015;21(Suppl 6):S80–90. doi: 10.1097/PHH.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 39.Gebbie KM. The public health workforce: key to public health infrastructure. Am J Public Health. 1999;89(5):660–661. doi: 10.2105/AJPH.89.5.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bernard AW, Gorgas D, Greenberger S, Jacques A, Khandelwal S. The use of reflection in emergency medicine education. Acad Emerg Med. 2012;19(8):978–982. doi: 10.1111/j.1553-2712.2012.01407.x. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization. Guidance for after action review (AAR) Geneva, Switzerland: World Health Organization; 2019 (cited 2019 Oct 8). Report No.: WHO/WHE/CPI/2019.4. https://apps.who.int/iris/bitstream/handle/10665/311537/WHO-WHE-CPI-2019.4-eng.pdf?sequence=1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to this manuscript are included within the manuscript tables, figures and/or reference links.