Abstract
Backgrounds
Although the psychological effects of the COVID-19 pandemic have been investigated, there is no study comparing the effects between the peaks. This study aims to compare the levels of anxiety, depression, and stress of healthcare workers struggling with pandemic between the first and second peaks.
Methods
A total of 2460 healthcare workers, 1051 from the first peak period and 1409 from the second peak period, were included in the study. The first peak measurements of the participants were made between 07.04.2020 and 05.05.2020 and the second peak measurements were made between 22.11.2020 and 20.12.2020 according to the peak period in Turkey. Depression-Anxiety-Stress-21(DASS-21) scale was applied to the participants online by the purpose of the study.
Results
The mean age of the participants was 32.63 ± 7.70, and 66.5% of them were female. A statistically significant difference was found between the income status (p < 0.001), lifestyle (p < 0.001) and COVID-19 test result (p < 0.001), DASS-21 Depression (p < 0.001, t = -5.311), Anxiety (p < 0.001, t = -8.244), Stress (p < 0.001, -10.056) and total(p < 0.001, t = -8.719) scores of the two groups.
Conclusion
The present study results showed that healthcare workers meticulously struggling with the pandemic had increased anxiety, depression, and stress levels at the second peak of the pandemic compared to the first peak.
Keywords: COVID, Peak, Wave, Second, Depression, Psychological
1. Introduction
The novel coronavirus disease 2019 (COVID-19) is a communicable respiratory tract disease that emerged in Wuhan, China in December 2019, spread rapidly to the world and was declared as a pandemic by the World Health Organization (World Health Organization, 2021). Pandemic describes the presence of an unusual situation that has a worldwide impact and affects a large number of people (Porta, 2014). It is predicted that waves and peaks may occur due to the nature of the pandemic based on past experiences, and it is known that these re-increments can change the course, characteristics and consequences of the disease (Temel and Ertin, 2020). Therefore, simulations regarding the future of the pandemic process in the modern world are created and the necessary measures are discussed (Middleton et al., 2020). However, very few of these discussions deal with the psychological effects of fluctuations (Hacimusalar et al., 2020; Middleton et al., 2020).
It is known that the COVID-19 pandemic causes essential problems related to basic needs such as economic, social, shelter and nutrition as well as the physical effects of the disease (Fiorillo and Gorwood, 2020). Also, many studies have shown that it has negative effects on the psychological state of individuals (Fiorillo and Gorwood, 2020; Hacimusalar et al., 2020; Pappa et al., 2020). These studies investigating the psychological effects associated with the COVID-19 pandemic focused on symptoms such as anxiety, depression, stress, hopelessness and fear associated with the disease (Hacimusalar et al., 2020; Pappa et al., 2020; Xiong et al., 2020). However, they focused on the effects of serious measures such as curfews and social isolation in the fight against the pandemic (Roje Đapić et al., 2020). In addition, psychological effects on special groups such as healthcare professionals were also investigated (Hacimusalar et al., 2020). However, as far as we know, there is no study investigating the psychological effects of the wave of the pandemic process and the changes that come with the increase in cases over time.
In general, a COVID-19 pandemic model has been observed in many countries, where the cases seen in the first-period decrease significantly in the spring-summer period and a second case increase occurs with the autumn (World Health Organization, 2021). Similarly, the increasing number of cases in Turkey in the April-May 2020 decreased during the summer months but an increase re-emerged during the November-December 2020 period (Republic of Turkey Ministry of Health, 2021). It is thought that comparing the psychological effects of these increase periods will guide the next case increase periods and preventive psychological health measures to be taken in the current situation. Such studies will also reveal the importance of identifying the psychological effects of pandemic prolongation and evaluating individuals under risk.
Accordingly, the main purpose of the present study is to reveal the changes in anxiety, depression, and stress symptoms of healthcare workers during the two peak periods of the COVID-19 pandemic.
2. Method
2.1. Sample
The sample of this cross-sectional study consisted of physicians, nurses and allied frontline health workers the COVID-19 in the forefront during the two COVID-19 peaks according to the confirmed cases. Accordingly, 1051 healthcare workers from the first peak period and 1409 health workers from the second peak period were included in the study. Participants were invited to the study through an online survey. The inclusion criteria were determined to be between the ages of 18–65, to have no major psychiatric illness, to have been actively working in the pandemic unit (in direct contact with COVID-positive patients, such as inpatient service, intensive care clinic, outpatient follow-up unit) for at least 15 days, and to be a volunteer. Consent of all participants who accepted to participate in the study was obtained through online methods, and only the participants who gave consent were able to access the scales and repeated participation was prevented through the system. In the subsequent examinations, scales that were filled in incomplete or out of instruction were excluded from the study. The study was conducted under the supervision of the Department of Psychiatry, Kırıkkale Yüksek İhtisas Hospital . Local ethics committee approval was obtained for the study (05.05.2020-2020/181, 2020-21/401) and all stages were completed in accordance with the principles of the Declaration of Helsinki.
2.2. Study Design
Participants were reached via online forms, and they were asked to fill in an anonymous form including the consent form, sociodemographic data form, and the Depression-Anxiety-Stress-21 Scale (DASS-21). Forms that did not meet the inclusion criteria and were not filled properly were excluded from the study. The forms were evaluated and scored according to their instructions, recorded in the data set, and statistically analyzed.
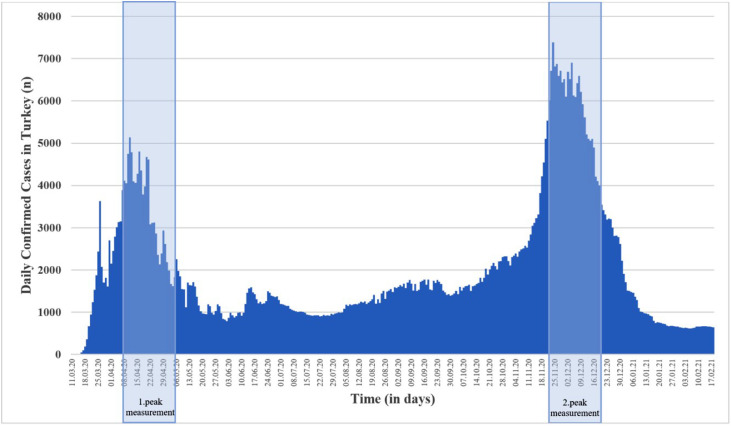
This study, which is planned to compare the levels of depression, anxiety, and stress among healthcare workers between COVID-19 peaks, aims to evaluate the same healthcare workers at different peak periods. However, due to the rotational work of healthcare professionals in COVID-related units, the healthcare workers' levels of depression, anxiety and stress in general during peak periods were found suitable to be evaluated. The peak period was determined based on the number of cases taken from the daily announcements of the Ministry of Health of the Republic of Turkey (Republic of Turkey Ministry of Health, 2021). The distribution of the number of cases in Turkey and measurement times are presented in Fig. 1 . Accordingly, the first peak measurements were done between 07.04.2020 and 05.05.2020, and the second peak measurements were done between 22.11.2020 and 20.12.2020.
Fig. 1.
The number of confirmed coronavirus disease (COVID-19) cases per day in Turkey.
2.3. Data Collection Tools
2.3.1. Sociodemographic data form
The researchers developed it in accordance with the purpose of the study. Demographic data of the participants such as age, gender, profession, education level, income level and place of residence were questioned.
2.3.2. The Depression-Anxiety-Stress Scale-21 (DASS-21)
It was used to evaluate the severity of depressive, anxiety and stress symptoms of the participants during the two peak periods. The short form of the scale with 21 items was used (Lovibond and Lovibond, 1995). The scale is a 4-point Likert-type scale and consists of seven items that evaluate depression, anxiety, and stress. The score obtained from the scale varies between 0-21 for each subscale. For the depression subscale, 0–4 points are scored as normal, 5–6 points as mild depression, 7–10 points as moderate depression, 11–13 points as severe depression, and 14 and above as very severe depression. For the anxiety subscale, these scores are 0–3 points are scored as normal, 4–5 points as mild, 6–7 points as moderate, 8–9 points as severe, 10 and above as very severe. For the stress subscale, these scores are 0–7 points are scored as normal, 8-9 points as mild, 10–12 points as moderate, 13–16 points as severe, 17 and above as very severe . The Turkish validity and reliability study of the scale was conducted by Sarıçam et al (Saricam, 2018).
2.4. Statistical Analysis
Statistical analysis of the study was performed using SPSS 22.0 (Statistical Package for Social Sciences, IBM Inc., Chicago, IL, USA). The conformity of the data to normal distribution was evaluated with Kolmogorov-Smirnov, Skewness and Kurtosis values. Descriptive data are presented as mean and standard deviation for continuous variables and as frequency and percentage for categorical variables. To compare categorical data between two peak groups, Pearson Chi-square analysis was used. In comparing the continuous variables between the two peak groups, student's T-test analysis was used after testing the compatibility with parametric assumptions. The statistical significance was p < 0.05
3. Results
The present study was conducted with a total of 2460 volunteers, including 1637 (66.5%) women and 823 (33.5%) men. The mean age of the participants was 32.63 ± 7.70 years. Of the participants, 37.6% (n = 926) were physicians, 41.2% (n = 1013) were nurses and 21.2% (n = 521) were other healthcare professionals. The comparison of the sociodemographic data of the two peak groups is presented in Table 1 . Accordingly, the two peak groups were not statistically different in terms of age, gender, marital status, educational status, and profession variables. However, there was a significant difference between the two groups in terms of income status (x 2 = 52.743, df = 2, p < 0.001), lifestyle (χ2 = 167.045, df = 2, p < 0.001) and COVID-19 test result (x 2 = 230.793, df = 1, p < 0.001) variables.
Table 1.
Comparison of the sociodemographic data of the participants according to COVID-19 peaks.
| Variable | Group |
t/χ2 | df | pvalue | |
|---|---|---|---|---|---|
| Peak(n = 1051) | Peak(n = 1409) | ||||
| Age; mean±SD (year) | 32.94 ± 7.82 | 32.40 ± 7.60 | t = 1.688 | 2394 | 0.092 |
| Gender; n (%) | |||||
| Female | 685 (65.2) | 952 (67.6) | χ2 = 1.544 | 1 | 0.214 |
| Male | 366 (34.8) | 457 (32.4) | |||
| Marital Status; n (%) | χ2 = 2.330 | 2 | 0.312 | ||
| Married | 543 (51.7) | 766 (54.4) | |||
| Single | 392 (37.3) | 508 (36.1) | |||
| Other | 116 (11.0) | 135 (9.6) | |||
| Education Status; n (%) | χ2 = 1.405 | 2 | 0.495 | ||
| High School | 33 (3.1) | 57 (4.0) | |||
| University | 554 (52.7) | 734 (52.1) | |||
| Postgraduate | 464 (44.1) | 618 (43.9) | |||
| Income status, n(%) | χ2 = 52.743 | 2 | <0.001* | ||
| Income less than the expense | 70 (6.7) | 199 (14.1) | |||
| Expense equals income | 447 (42.5) | 662 (47.0) | |||
| Income more than the expense | 534 (50.8) | 548 (38.9) | |||
| Job title, n (%) | χ2 = 3.099 | 2 | 0.212 | ||
| Doctor | 381 (36.3) | 545 (38.7) | |||
| Nurse | 454 (43.2) | 559 (39.7) | |||
| Other health care workers | 216 (20.6) | 305 (21.6) | |||
| Life style, n (%) | χ2 = 167.045 | 2 | <0.001* | ||
| Family | 527 (50.1) | 1025 (72.7) | |||
| Single | 331 (31.5) | 312 (22.1) | |||
| Other (hostel vb.) | 193 (18.4) | 72 (5.1) | |||
| COVID-19 Test, n (%) | χ2 = 230.793 | 1 | <0.001* | ||
| Positive | 24 (2.3) | 343 (24.3) | |||
| Negative | 1027 (97.7) | 1066 (75.7) | |||
:p ≤ 0.05, t: Student-T test, χ2: Pearson Chi-square test.
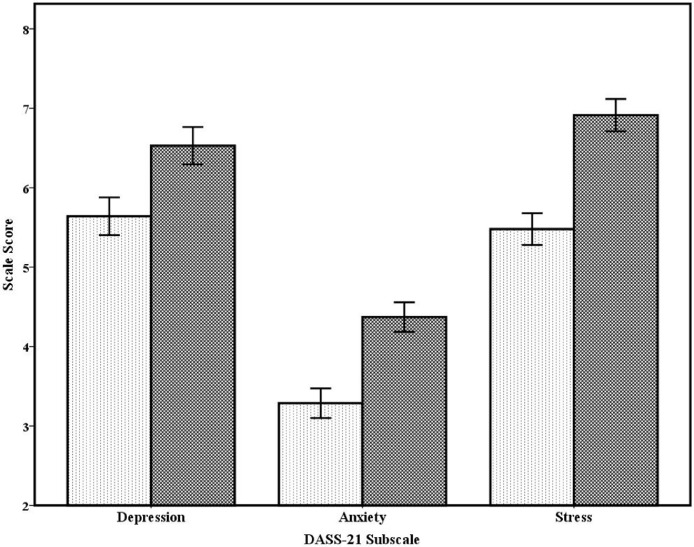
The comparison of the depression, anxiety, and stress levels between the two peak groups is presented in Table 2 and Fig. 2 . Accordingly, there was a significant difference between the two groups in terms of the scores on the depression subscale (t = 5.311, df = 2398, p < 0.001), scores on the anxiety subscale (t = -8.244, df = 2402, p < 0.001), scores on the stress subscale (t = -10.056, df = 2418, p < 0.001) of DASS-21, and the total DASS-21 scores (t = -8.719, df = 2427, p < 0.001) (Fig. 2). In addition, a statistical difference was found in the comparison of the severity of depression (x2 = 28.368, df = 4, p < 0.001), anxiety (χ2 = 69.390, df = 4, p < 0.001) and stress (χ2 = 103.298, df = 4, p < 0.001) between the two groups.
Table 2.
Comparison of the Depression, Anxiety and Stress feature of the participants according to the COVID-19 peaks.
| Variable | Group |
t/χ2 | df | p | |
|---|---|---|---|---|---|
| Peak(n = 1051) | Peak(n = 1409) | ||||
| DASS-21 Depression Score; mean±SD | 5.64 ± 3.85 | 6.52 ± 4.41 | t = -5.311 | 2398 | <0.001* |
| Depression Severity; n (%) | χ2 = 28.368 | 4 | <0.001* | ||
| Normal | 437 (41.6) | 506 (35.9) | |||
| Mild | 209 (19.9) | 236 (16.7) | |||
| Moderate | 289 (27.5) | 414 (29.4) | |||
| Severe | 69 (6.6) | 146 (10.4) | |||
| Extremely severe | 47 (4.5) | 107 (7.6) | |||
| DASS-21 Anxiety Score; mean±SD | 3.28 ± 3.02 | 4.37 ± 3.48 | t = -8.244 | 2402 | <0.001* |
| Anxiety Severity; n (%) | χ2 = 69.390 | 4 | <0.001* | ||
| Normal | 671 (63.8) | 680 (48.3) | |||
| Mild | 164 (15.6) | 234 (16.6) | |||
| Moderate | 129 (12.3) | 253 (18.0) | |||
| Severe | 34 (3.2) | 116 (8.2) | |||
| Extremely severe | 53 (5.0) | 126 (8.9) | |||
| DASS-21 Stress Score; mean±SD | 5.47 ± 3.23 | 6.91 ± 3.82 | t = -10.056 | 2418 | <0.001* |
| Stress Severity; n (%) | χ2 = 103.298 | 4 | <0.001* | ||
| Normal | 838 (79.7) | 860 (61.0) | |||
| Mild | 97 (9.2) | 220 (15.6) | |||
| Moderate | 99 (9.4) | 251 (17.8) | |||
| Severe | 13 (1.2) | 58 (4.1) | |||
| Extremely severe | 4 (0.4) | 20 (1.4) | |||
| DASS-21 Total Score; mean±SD | 14.40 ± 8.80 | 17.81 ± 10.55 | t = -8.719 | 2427 | <0.001* |
:p ≤ 0.05, DASS-21: Depression-Anxiety-Stress Scale-21, t: Student-T test, χ2: Pearson Chi-Square test.
Fig. 2.
The Comparison of Anxiety, Depression and Stress Symptoms Levels of Healthcare Workers between the First and Second COVID-19 Peaks
4. Discussion
The most important result of this study, which aimed to compare the anxiety, depression and stress levels of healthcare workers fighting against the pandemic at the forefront, is revealing that anxiety, depression and stress levels of healthcare workers increase in the second peak compared to the first peak. In addition, another important result is that the economic status of the participants in the second peak was lower than the first peak. It is thought that the results of this study are important as they compared two different peaks and the mental states between this duration for the first time.
The negative effects of the COVID-19 pandemic on anxiety, depression and stress have been shown in numerous articles (Fiorillo and Gorwood, 2020; Hacimusalar et al., 2020; Pappa et al., 2020; Xiong et al., 2020). In addition, many negative mental effects such as despair, sleep disorders, post-traumatic stress disorder symptoms, psychosomatic symptoms, and burnout have been reported (Hacimusalar et al., 2020; Shevlin et al., 2020; Spoorthy et al., 2020; Wang et al., 2020; Zhang et al., 2020). In the current study, it was found that the anxiety, depression and stress symptoms and levels of healthcare workers who took part in the COVID-19 pandemic were higher in the second peak compared to the first peak. The prolongation of the COVID-19 pandemic may be related to the fact that people's long and intense working hours have caused an increase in burnout and chronic fatigue levels (Matsuo et al., 2020). The fact that some healthcare workers left their jobs and some died during this period may have increased the mental and physical workload of healthcare workers(Abuown et al., 2020). In addition, traumatic events such as the loss of relatives in this period and COVID-19 infection may have contributed to this result (Zhang et al., 2020). In this context, it is seen that COVID-19 infection among healthcare workers increased ten times in the six-month period examined in this study. On the other hand, it is a fact that uncertainties such as the uncertainty of the pandemic period, when it will end and when people will return to the pre-pandemic period may adversely affect the mental state of individuals (Vaishnav et al., 2020). The fact that the mutations of the Coronavirus have emerged may cause the psychological effects between peaks to increase exponentially. In the pandemic period, the restrictions applied to prevent infection may prevent individuals from taking mental rehabilitation methods such as walking, exercising, spending time with their loved ones, and on the contrary, the compelling effects such as not being able to leave the house or socialize may negatively affect anxiety, depression and stress (Mucci et al., 2020). Restrictions may be an obstacle to self-spiritual intervention and spiritual help. The effort of the healthcare professionals, who constitute the population of the study, to stay away from their families and loved ones due to the risk of infection increase the emotional burden on them and should be considered as another reason (Souadka et al., 2020). The increasing social and economic effects of the pandemic period may also be a reason for the worsening of individuals' mental states (Di Tella et al., 2020). Considering so many reasons together, the result that the level of "being psychologically affected" of the healthcare workers increases as the pandemic period prolongs seems to be normal.
It is known that the pandemic has socioeconomic consequences as well as physical and mental effects (Nicola et al., 2020). Economic consequences like this can affect all economies from the smallest to the largest (Fernandes, 2020; Nicola et al., 2020). Similar to the findings in the literature, it is observed in this study that the economic status of healthcare workers worsened in the second peak compared to the first peak. This situation may have very different reasons. First, even if there is no unemployment among health workers, the decrease in income may be a reason. However, increases in the amount of expenditure due to inflation and pandemic conditions may be effective in this result (Binder, 2020). In addition, it should be remembered that the unemployment of spouses and relatives due to the pandemic could be another reason (Kartseva and Kuznetsova, 2020). When considered within the general objectives of the study, it should not be forgotten that economic deterioration will have negative effects on the mental health of individuals.
This study has some limitations as well as significant strengths such as the large sample size. The most important limitation of this study is that it has a cross-sectional design. The continuity problem of healthcare professionals who are fighting against the pandemic in the front line has led the researchers to design the study in this way. It will be useful for the upcoming studies to be follow-up studies. On the other hand, the fact that this study was conducted with healthcare professionals may be an obstacle regarding the generalization of the results. Another limitation is that the online self-report scale was used, and it prevented conducting an objective evaluation.
5. Conclusion
The current study has shown that healthcare workers fighting against the pandemic in the foreground had increased levels of anxiety, depression, and stress at the second peak of the pandemic. These results are important because they demonstrate the negative psychological effects of the prolonging period for the first time. The results of the study reveal the necessity of individual and group mental support programs for healthcare professionals who show great devotion in combating against the pandemic. Additionally, it would be appropriate to identify the negative mental effects of the pandemic period and to implement preventive mental and socioeconomic interventions as soon as possible.
Funding
This research received no specific grant and financial support from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions
Category 1
Conception and design of study: İbrahim Gündoğmuş, Cansu Ünsal, Abdullah Bolu, Sabri Berkem Ökten, Mikail Burak Aydın, Hüseyin Uçar, Anıl Gündüz, Ayşegül Taşdelen Kul
Aquisition of data (laboratory or clinical): İbrahim Gündoğmuş, Abdullah Bolu, Taha Takmaz, Mikail Burak Aydın, Hüseyin Uçar, Anıl Gündüz
Data analysis and/or interpretation: İbrahim Gündoğmuş, Abdullah Bolu, Taha Takmaz, Hüseyin Uçar, Ayşegül Taşdelen Kul
Category 2
Drafting of manuscript and/or critical revision: İbrahim Gündoğmuş, Cansu Ünsal, Abdullah Bolu, Taha Takmaz, Sabri Berkem Ökten, Mikail Burak Aydın, Hüseyin Uçar, Anıl Gündüz, Ayşegül Taşdelen Kul
Category 3
Approval of final version of manuscript: İbrahim Gündoğmuş, Cansu Ünsal, Abdullah Bolu, Taha Takmaz, Sabri Berkem Ökten, Mikail Burak Aydın, Hüseyin Uçar, Anıl Gündüz, Ayşegül Taşdelen Kul
Declaration of Competing Interest
The authors declare that there is no conflict of interest.
Acknowledgments
All persons who have made substantial contributions to the work reported in the manuscript (e.g., tecnical help, writing and editing assistance, general support), but who do not meet the criteria for authorship are named in the Acknowledgments and have given us their written permission to be named. If we have not included an Acknowledgments in our manuscript, then that indicates that we have not received substantial contributions from non-authors
References
- Abuown A., Taube C., Koizia L.J. Impact of COVID-19 second wave on healthcare worker staffing levels. Infect. Control Hosp. Epidemiol. 2020 doi: 10.1017/ice.2020.353. 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binder C. Coronavirus fears and macroeconomic expectations. Rev. Econ. Stat. 2020;102(4):721–730. [Google Scholar]
- Di Tella M., Romeo A., Benfante A., Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020;26(6):1583–1587. doi: 10.1111/jep.13444. [DOI] [PubMed] [Google Scholar]
- Fernandes, N., 2020. Economic effects of coronavirus outbreak (COVID-19) on the world economy. Available at SSRN 3557504.
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacimusalar Y., Kahve A.C., Yasar A.B., Aydin M.S. Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. J. Psychiatr. Res. 2020;129:181–188. doi: 10.1016/j.jpsychires.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kartseva M.A., Kuznetsova P.O. The economic consequences of the coronavirus pandemic: which groups will suffer more in terms of loss of employment and income? Popul. Econ. 2020;4:26. [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Matsuo T., Kobayashi D., Taki F., Sakamoto F., Uehara Y., Mori N., Fukui T. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw. Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.17271. e2017271–e2017271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middleton J., Lopes H., Michelson K., Reid J. Planning for a second wave pandemic of COVID-19 and planning for winter. Int. J. Public Health. 2020;65(9):1525–1527. doi: 10.1007/s00038-020-01455-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucci F., Mucci N., Diolaiuti F. Lockdown and isolation: psychological aspects of COVID-19 pandemic in the general population. Clin. Neuropsychiatry. 2020;17(2):63–64. doi: 10.36131/CN20200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta M. Oxford university press; 2014. A dictionary of epidemiology. [Google Scholar]
- Republic of Turkey Ministry of Health . Republic of Turkey Ministry of Health; 2021. COVID-19 Information Page, General Coronavirus Table.https://covid19.saglik.gov.tr/EN-69532/general-coronavirus-table.html [Google Scholar]
- Roje Đapić M., Buljan Flander G., Prijatelj K. Children behind closed doors due to COVID-19 isolation: abuse, neglect and domestic violence. archives of psychiatry research. Int. J. Psychiatry Related Sci. 2020;56(2):181–192. [Google Scholar]
- Saricam H. The psychometric properties of Turkish version of Depression Anxiety Stress Scale-21 (DASS-21) in health control and clinical samples. J. Cogn. Behav. Psychother. Res. 2018;7(1):19–30. [Google Scholar]
- Shevlin M., Nolan E., Owczarek M., McBride O., Murphy J., Gibson Miller J., Hartman T.K., Levita L., Mason L., Martinez A.P. COVID-19-related anxiety predicts somatic symptoms in the UK population. Br. J. Health Psychol. 2020 doi: 10.1111/bjhp.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souadka A., Essangri H., Benkabbou A., Amrani L., Majbar M.A. COVID-19 and Healthcare worker's families: behind the scenes of frontline response. E. Clin. Med. 2020:23. doi: 10.1016/j.eclinm.2020.100373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temel M.K., Ertin H. Lessons from the 1918 Influenza Pandemic for the COVID-19 Pandemic. Anadolu Kliniği Tıp Bilimleri Dergisi. 2020;25:63–78. (Special Issue on COVID 19) [Google Scholar]
- Vaishnav M., Dalal P., Javed A. When will the pandemic end? Indian J. Psychiatry. 2020;62(Suppl 3):S330. doi: 10.4103/psychiatry.IndianJPsychiatry_1030_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S., Xie L., Xu Y., Yu S., Yao B., Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. (Lond.) 2020 doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO; 2021. 2021. WHO Coronavirus Disease (COVID-19) Dashboard. [Google Scholar]; https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Shi Y., Jing P., Zhan P., Fang Y., Wang F. Posttraumatic stress disorder symptoms in healthcare workers after the peak of the COVID-19 outbreak: a survey of a large tertiary care hospital in Wuhan. Psychiatry Res. 2020;294 doi: 10.1016/j.psychres.2020.113541. [DOI] [PMC free article] [PubMed] [Google Scholar]