Abstract
The aim of this study was to evaluate the factors affecting the ability and willingness of dentists to work during the COVID-19 pandemic and the effect of this situation on occupational burnout. A 51-question survey, including demographic and pandemic questions and the Maslach Burnout Inventory (MBI), was used as a data collection method and administered to dentists in Turkey via the internet in two stages. A link to the survey (onlineanketler.com) was sent to the participants by e-mail or social media (WhatsApp©). A total of 442 dentists in the first stage and 264 dentists in the second stage answered the questionnaire. The second stage of the survey only applied to dentists who are assigned within the scope of COVID-19 measures in Turkey. Standard descriptive statistics, the chi-square test, independent samples t test and the Kruskal-Wallis test were used for statistical analysis. Most of the participants showed higher stress levels. Occupational burnout levels of participants according to filiation service (serve/FP, did not serve/FN) were 34.4% and 17.6%, respectively. The FP group showed significantly higher stress levels than the FN group. It is important to consider how these results, collected during an infectious disease epidemic, reflect the effects of psychological distress and burnout on dental staff.
Trial Registration Number and Date of Registration: NCT04605692–10/27/2020.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12144-021-01764-x.
Keywords: Burnout, COVID-19, Dentistry, Filiation, Pandemic
Introduction
The coronavirus disease (COVID-19) was first identified during the outbreak of severe acute respiratory syndrome in Wuhan, China, in December 2019 (Organization 2020a). On March 11, 2020, the World Health Organization (WHO) characterized the disease as the first pandemic caused by a coronavirus (Organization 2020b) The disease has spread in more than 200 countries with a mortality rate of about 5.7%. (Baud et al. 2020).
COVID-19 is commonly transmitted through direct contact, contact transmission and a small amount of fecal-oral routes. Healthcare workers are exposed to the virus through blood or other body fluids and airborne infectious agents (Shiao et al., 2007). Considering the transmission mechanism of the virus, aerosols formed as a result of dental procedures are important risk (Lauer et al., 2020). A document prepared by the Occupational Safety and Health Administration (OSHA) divides exposure risk into four categories, and dentistry is in the highest risk category ((OSHA) 2020). Likewise, dentistry received high risk scores on the website Visual Capitalist (Lu, 2020).
The incubation period of the coronavirus is 5 days, and complaints and symptoms develop within 11.5 days in almost all cases. Symptomatic patients are seen as the main source of transmission routes. However, asymptomatic individuals have also been shown to be a source of virus transmission (Lauer et al., 2020). The rate of spread of COVID-19 is higher than other coronaviruses. MERS-CoV is transmitted by consuming the milk or meat of infected animals, the probability of transmission between humans through close contact is not high. SARS CoV and COVID-19 are mainly transmitted through close contact between people. The time to infect the first thousand people was given as 903 days in MERS-CoV, 130 days in SARS CoV and 48 days in COVID-19 (Rabaan et al., 2020). For this reason, quarantine measures have been implemented in many countries to reduce contamination and spread of COVID-19 virus (Mayr et al., 2020; Tian et al., 2020; Wilder-Smith & Freedman, 2020).
Governments rapidly mobilized to minimize transmission of COVID-19 through social distancing and travel restrictions to reduce fatalities and prevent the outstripping of healthcare capacity. Measures, such as the obligation to wear masks, the cancellation of collective events, restrictions for workplaces and the closure of schools and universities were taken (Cheng et al., 2020). “Filiation”, which refers to the connectedness of things that result from one another, is one of the measures taken to reduce the spread rate of the disease in Turkey (Cobbett, 1833). The core idea behind filiation as a precaution against the ongoing COVID-19 outbreak was to prevent the disease by interrupting the chain of transmission with a systematical tracing and isolation of susceptible individuals having contact with any confirmed COVID-19 cases, especially cases who were suspected to be infected or potentially at a higher risk (Demirtas & Tekiner, 2020). This task is being carried out by health care workers, including dentists, in Turkey.
There are many studies showed that the occupational burnout levels of dentists were high even before the epidemic due to various factors such as work environment, repetitive tasks, risk of medical error, one-on-one communication with patients, patient anxiety, long working hours, workload, job dissatisfaction, extraordinary responsibility, working with inadequate qualified dental assistants, uncomfortable physical posture and working environment, economic pressures and demographic characteristics (Ahola et al., 2014; Gorter et al., 2012; Hakanen et al., 2014; Huri et al., 2016; Zini et al., 2013). Besides all these factors, the stress of working during the COVID-19 pandemic can also cause a decrease in the resistance to burnout in dentists, as in all healthcare professionals. In particular, factors such as lack of appreciation, the role confusion due to working in non-branch positions, imbalance in workload, loss of control of the work life, and lack of appreciation of the employee’s labor contribute to the risk of burnout (Çalişkan et al., 2019; Eaton, 2019). Burnout syndrome refers to fatigue for an extended time, reduced levels of motivation and low interest in the job (Embriaco et al., 2007; Goldberg et al., 1996). Burnout in healthcare workers has a direct negative effect, evidenced by fatigue, stress, anxiety, depression, mood disorders, substance abuse, suicide, decreased quality of patient care, early retirement and unexpected resignations (Bakker et al., 2005; Goldberg et al., 1996; Lancee et al., 2008).
This study aimed to evaluate the factors affecting the ability and willingness of dentists to work during the COVID-19 pandemic and the effect of this situation on their occupational burnout. The following conceptual hypotheses were investigated: (1) willingness and ability to work would have no effect on occupational burnout level among dentists during COVID-19 pandemic in Turkey; (2) there would be no difference in terms of occupational burnout between groups that serve and did not serve in filiation service during COVID-19 pandemic.
Subject and Methods
The study was approved by Turkey’s Ministry of Health (approval no: 2020–07-02T14_41_29) and the Akdeniz University Faculty of Medicine Clinical Research Ethics Committee (approval no: KAEK-590).
A pilot study was conducted with 20 dentists to test the questionnaire based on a previous study (Mostafa et al., 2020). In the pilot study, the application aspect of the questionnaire was tested. Also, the answers obtained from the pilot study were evaluated and it was checked whether there were questions that were difficult to understand or answer. The results of the pilot study demonstrated that there is no need to change the questionnaire. The participants of the pilot study were not included in the present study.
The first part of the survey included 29 demographic questions and questions about the participants’ situation before and during the pandemic period. The second part of the survey used the 22-question Maslach Burnout Inventory (MBI) (Maslach & Jackson, 1981). The original MBI has seven options. This version of the inventory has been adapted to Turkish culture and used a survey form with five options (0 = Never, 1 = Very rare, 2 = Sometimes, 3 = Most of the time, 4 = Always).
The number of participants was estimated via a power analysis using the G*Power program package under a power of 95% and an assumed effect size of 0.3, a Type-I error(alpha) of 0.05 and 5 degrees of freedom based on the total target population for dentists in Turkey (n = 19 32.859, according to the data of the Ministry of Health of Turkey). According to the data obtained from the provincial health directorates, 78–90% of the dentists working in the public sector between March–April 2020 took part in filiation serve. Based on these data, a non-response rate of 25% was added for a final sample and minimal sample size necessary for this study determined to be 400 participants for the first stage and 315 participants for the second stage.
A survey was sent to dentists in Turkey via the internet (onlineanketler.com). The link to the questionnaire was sent to the participants by e-mail or social media (WhatsApp©). Eligibility criteria were as follows: being a dentist or specialist dentist, giving consent to participate in the study and questionnaire forms that were completely answered. Exclusion criteria consisted of dentist candidates who have not completed their undergraduate education and retired dentists. Before the participants started to answer the questionnaire, the consent of the participants was obtained with the information text added just initial part of the questionnaire. This consent text included information about the purpose of the study, the security of personal information, the necessary permissions for the study, and that participation in the study was voluntary. For reasons of privacy, no names or other identity information were recorded. Returning the questionnaire was interpreted as indicating a willingness to participate in the study.
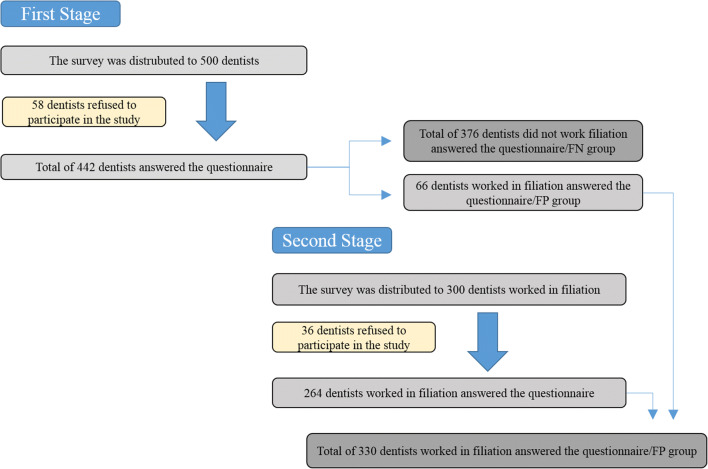
The first stage of the study was carried out between 9 March and 20 April. The survey was distributed to 500 dentists. A total of 442 dentists answered the questionnaire. At this stage, survey was directed to the general dentist population, regardless of their filiation serve status. The status of taking part in the filiation service was asked to the dentists as a question in the survey and grouped according to their responses (serve / FP, did not serve / FN). A questionnaire was sent to only dentists who worked in the filiation service (FP) in the second stage of the study to increase the reliability of the tests by equalizing the number of participants according to power analysis in the comparisons between the groups (FP, FN). For the second stage, eligibility criteria were as follows: being a dentist or specialist dentist who worked in filiation service, giving consent to participate in the study and questionnaire forms that were completely answered. Exclusion criteria consisted of dentist candidates who have not completed their undergraduate education and retired dentist. In the second stage, the survey was distributed to 300 dentists who worked in filiation service from April 29 to May 20. A total of 264 dentists answered the questionnaire. In the first stage of the questionnaire, 66 dentists who stated that they took part in filiation serve were included in the second stage. Flow diagram of the participants was shown in Fig. 1.
Fig. 1.
A flow diagram of the number of dentists participated in the study
MBI scores, for the emotional exhaustion (EE) at work subscale, a combined score of 0–20 for all items was defined as low, 21–30 as moderate, and 31 and above as high. For the depersonalization (DP) subscale, low was defined as a combined score of 0–5, moderate as 6–10, and high as 11 and above. For personal gratification (PG), low was defined as 42 and above, moderate as 36–41 and high as 35 and below. Because the five-option subscale was used to interpret the scores, the values were reduced by 2/7. A combination of high scores on EE and DP, and a low score on PG, correspond to a high level of burnout.
Statistical Analysis
Standard descriptive statistics were used to summarize the responses of all survey questions. The chi-square test and independent sample t test were used to assess the difference of frequencies of burnout, stress levels and related factors using Statistical Package for the Social Science 2.0 (IBM SPSS 22.0, Armonk, NY) program. The Pearson correlation was used to examine the relationship between participant stress levels and subgroup burnout scores. The statistical significance level was accepted as p < 0.05.
Result
A total of 706 participants completed the survey. A flow diagram of the number of dentists participating in the study is shown in Fig. 1. All cases in the sample were valid to be analyzed.
First Stage Results (General Evaluations)
First stage results were obtained on 442 (62.6%) participants, 376 FN dentists and 66 FP dentists. Occupational burnout was observed in 20.4% of the participants. The demographic characteristics of participants and comparisons according to stress levels, burnout and burnout subgroup scores are given in Table 1. Also, general health, smoking, transport, distribution and characteristics of patients treated per week, stress and burnout levels are summarized in Table 1.
Table 1.
First-Stage Participant Characteristics, Burnout-subgroups and Stress levels (n:442)
| Socio-Demographic and Professional Characteristics | Total n (%) |
Emotional exhaustion (MBI) Mean (SD) |
Depersonalization (MBI) Mean (SD) |
Personal gratification (MBI) Mean (SD) |
Burnout (+) n (%) |
Stress level (General) Mean (SD) |
Stress level (Personal) Mean (SD) |
Stress level (Family) Mean (SD) |
Stress lev Mean (SD) el (Patient) |
Stress level (Occupational) Mean (SD) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Female | 338 (76.5) | 19.76 (9.12) | 6.68 (3.65) | 9.26 (4.64) | 64 (71.1) | 7.62 (2.04) | 7.99 (2.19) | 9.02 (1.79) | 7.99 (2.11) | 8.35 (1.86) |
| Male | 104 (23.5) | 19.84 (7.72) | 8.13 (4.40) | 8.50 (4.86) | 26 (28.9) | 6.71 (2.97) | 6.63 (3.04) | 7.90 (2.72) | 6.55 (2.81) | 7.92 (2.99) | |
| p = 0.956 | p = 0.018* | p = 0.309 | p = 0.342 | p = 0.013* | p = 0.001* | p = 0.001* | p = 0.001* | p = 0.213 | |||
| Age (year) | 22–30 | 248 (56.1) | 21.18 (7.30) | 7.60 (3.74) | 9.87 (4.42) | 56 (62.2) | 7.60 (2.24) | 7.96 2.26) | 8.98 (2.17) | 8.02 (0.18) | 8.62 (0.17) |
| 31–40 | 136 (30.8) | 17.38 (8.12) | 6.14 (3.77) | 8.86 (4.88) | 22 (24.4) | 6.88 (2.39) | 7.23 (2.31) | 8.75 (2.25) | 7.25 (0.31) | 7.89 (0.28) | |
| 41 ≤ | 58 (13.1) | 19.72 (9.74) | 6.58 (4.37) | 6.68 (2.39) | 12 (13.3) | 7.79 (2.41) | 7.44 (2.53) | 7.86 (2.49) | 7.03 (0.50) | 7.51 (0.47) | |
| p = 0.223 | p = 0.254 | p = 0.291 | p = 0.573 | p = 0.025* | p = 0.144 | p = 0.007* | p = 0.482 | p = 0.257 | |||
| Marital status | Married | 195 (43.9) | 20.20 (8.38) | 7.10 (3.67) | 8.89 (4.52) | 47 (51.1) | 7.64 (2.26) | 7.75 (2.46) | 8.73 (2.03) | 7.60 (2.34) | 8.24 (2.20) |
| Single/separated/divorced | 247 (56.1) | 19.52 (7.80) | 6.91 (4.14) | 9.22 (4.84) | 43 (48.9) | 7.21 (2.36) | 7.61 (2.49) | 8.79 (2.15) | 7.69 (2.39) | 8.25 (2.17) | |
| p = 0.533 | p = 0.723 | p = 0.607 | p = 0.274 | p = 0.172 | p = 0.679 | p = 0.838 | p = 0.791 | p = 0.971 | |||
| Degree | Dentist | 162 (36.7) | 21.38 (8.35) | 7.51(4.23) | 9.55 (4.65) | 40 (44.4) | 7.41 (2.51) | 7.54 (2.70) | 8.24 (2.53) | 7.44 (2.46) | 8.48 (2.16) |
| MSC/PHD student | 164 (37.1) | 20.24 (7.60) | 7.36 (0.63) | 9.51 (4.50) | 32 (35.6) | 7.64 (2.21) | 8.07 (2.28) | 9.29 (1.52) | 7.89 (2.33) | 8.40 (1.94) | |
| Specialist | 116 (26.2) | 17.05 (7.65) | 5.84 (3.49) | 7.81 (4.87) | 18 (20.0) | 7.05 (2.20) | 7.29 (2.37) | 8.74 (1.96) | 7.62 (2.28) | 7.72 (2.46) | |
| p = 0.498 | p = 0.195 | p = 0.667 | p = 0.404 | p = 0.671 | p = 0.161 | p = 0.319 | p = 0.558 | p = 0.034* | |||
| Specialty | Pediatric dentistry | 57 (12.7) | 18. 89 (8.30) | 6.71 (3.37) | 8.60 (3.37) | 6 (6.7) | 7.39 (2.02) | 8.28 (1.82) | 9.50 (0.96) | 8.28 (1.56) | 7.89 (2.42) |
| Endodontics | 28 (6.3) | 21.64 (7.13) | 8.42 (4.29) | 8.92 (4.02) | 12 (13.3) | 8.00 (2,38) | 8.35 (2.02) | 9.50 (1.34) | 8.00 (2.27) | 8.42 (1.94) | |
| Oral and maxillofacial radiology | 47 (10.9) | 16.04 (7.56) | 4.95 (3.25) | 7.58 (5.23) | 4 (4.4) | 7.04 (2.17) | 6.87 (2.38) | 8.33 (2.35) | 6.83 (2.71) | 7.54 (2.51) | |
| Oral and maxillofacial surgery | 26 (5.9) | 19.61 (7.67) | 7.38 (4.29) | 7.61 (3.35) | 6 (6.7) | 7.76 (2.21) | 7.76 (2.83) | 8.38 (2.56) | 6.84 (2.88) | 8.23 2.71) | |
| Orthodontics | 24 (5.4) | 23.16 (8.38) | 7.41 (4.16) | 11.33 (7.06) | 6 (6.7) | 8.00 (1.27) | 7.76 (2.30) | 8.66 (2.14) | 7.33 (2.87) | 8.83 (1.02) | |
| Periodontology | 58 (13.1) | 16.24 (6.45) | 6.58 (3.46) | 8.68 (5.23) | 8 (8.9) | 6.82 (2.70) | 7.27 (2.73) | 9.37 (1.04) | 7.82 (2.10) | 7.96 (2.44) | |
| Prosthodontics | 30 (6.8) | 20.73 (8.34) | 6.46 (3.02) | 9.20 (3.93) | 4 (4.4) | 7.53 (2.29) | 8.13 (2.32) | 9.13 (1.80) | 8.66 (1.11) | 8.60 (1.24) | |
| Restorative dentistry | 10 (2.3) | 23.40 (2.70) | 9.00 (2.54) | 12.00 (4.94) | 4 (4.4) | 8.00 (2.00) | 9. 00 (1.00) | 9.60 (0.89) | 9.40 (1.34) | 8.80 (0.83) | |
| p = 0.785 | p = 0.393 | p = 0.518 | p = 0.116 | p = 0.285 | p = 0.384 | p = 0.966 | p = 0.083 | p = 0.365 | |||
| Affiliation | Private clinic (single physician) | 44 (10) | 16.22 (6.98) | 6.27 (4.09) | 8.00 (5.43) | 6 (6.7) | 6.22 (2.74) | 6.36 (2.92) | 8.04 (2.51) | 6.13 (2.93) | 7.45 (3.06) |
| Private clinic (multi-physician) | 69 (15.8) | 18.17 (6.90) | 6.22 (3.00) | 8.45 (4.46) * | 6 (6.7) | 6.85 (2.41) | 7.28 (2.62) | 8.40 (2.54) | 7.85 (2.06) | 7.82 (2.83) | |
| Public hospital | 135 (30.3) | 23.08 (8.09) | 7.86 (4.41) | 9.95 (4.93) | 42 (46.7) | 7.83 (2.35) | 7.83 (2.49) | 8.70 (2.12) | 7.59 (2.22) | 8.65 (1.99) | |
| Public university | 169 (38.5) | 18.64 (7.96) | 7.01 (3.74) | 8.96 (4.58) | 32 (35.6) | 7.54 (2.15) | 7.95(2.24) | 9.09 (1.76) | 7.958 (2.31) | 8.21 (1.80) | |
| Foundation university | 25 (5.4) | 21.33(8.11) | 7.02 (3.88) | 9.08 (4.69) | 4 (4.4) | 7.40 (2.32) | 7.67 (2.47) | 8.76 (2.09) | 7.65 (2.37) | 8.25 (2.18) | |
| p = 0.128 | p = 0.104 | p = 0.036* | p = 0.066 | p = 0.040* | p = 0.004* | p = 0.131 | p = 0.674 | p = 0.136 | |||
| Years of experience | 0–1 | 18 (4.1) | 19.55 (5.74) | 6.00 (4.69) | 10.44 (3.43) | 4 (4.4) | 8.00 (1.73) | 7.55 (2.29) | 7.88 (3.10) | 7.33 (2.64) | 8.44 (1.33) |
| 2–5 | 194 (43.9) | 21.76 (7.31) | 7.72 (3.74) | 10.13 (4.43) | 44 (48.9) | 7.59 (2.19) | 8.06 (2.26) | 9.15 (1.58) | 7.97 (2.10) | 8.79 (1.67) | |
| 6–10 | 137 (31.2) | 18.00 (8.30) | 6.71 (3.84) | 9.00 (4.84) | 26 (28.9) | 7.10 (2.49) | 7.28 (2.55) | 8.71 (2.24) | 7.46 (2.47) | 7.84 (2.43) | |
| 11 ≤ | 93 (20.8) | 18.84 (8.9) | 6.21 (3.91) | 6.71 (4.46) | 16 (17.8) | 7.34 (2.44) | 7.45 (2.77) | 8.19 (2.44) | 7.32 (2.66) | 7.69 (2.62) | |
| p = 0.204 | p = 0.517 | p = 0.128 | p = 0.876 | p = 0.220 | p = 0.233 | p = 0.008* | p = 0.749 | p = 0.091 | |||
| General health | Excellent | 48 (10.9) | 17.62 (8.48) | 7.25 (4.18) | 7.95 (4.82) | 12 (13.3) | 6.00 (3.09) | 6.58 (3.18) | 8.70 (2.31) | 6.79 (2.79) | 8.20 (2.28) |
| Very Good | 122 (27.6) | 17.65 (6.68 | 6.72 (3.43) | 9.26 (5.32) | 10 (11.1) | 6.93 (2.42) | 7.08 (2.59) | 8.42 (2.22) | 7.29 (2.66) | 7.81 (2.57) | |
| Good | 185 (47.2) | 19.17 (7.79) | 6.81 (3.76) | 8.6. (4.35) | 36 (40.0) | 7.58 (1.96) | 7.76 (2.20) | 8.74 (2.19) | 7.73 (2.07) | 8.22 (2.09) | |
| Fair | 79 (17.6) | 25.05 (7.56) | 7.56 (4.69) | 10.61 (4.32) | 6 (6.7) | 8.48 (1.80) | 8.87 (1.96) | 9.25 (1.46) | 8.33 (2.10) | 8.89 (1.53) | |
| Poor | 8 (1.8) | 30.25 (6.55) | 9.75 (1.89) | 9.00 (2.82 | 26 (28.9) | 8.50 (1.50) | 9.50 (0.50) | 10.00 (0.00 | 10.00 (0.00) | 9.50 (1.00) | |
| p = 0.154 | p = 0.380 | p = 0.333 | p = 0.004* | p = 0.003* | p = 0.001* | p = 0.903 | p = 0.090 | p = 0.528 | |||
| Smoking | Yes | 103 (23.1) | 21.09 (8.61) | 8.33 (4.07) | 8.76 (4.91) | 28 (31.1) | 7.19 (2.60) | 7.29 (2.77) | 8.45 (2.58) | 7.45 (2.81) | 8.19 (2.62) |
| No | 339 (76.9) | 19.44 (7.84) | 6.62 (3.74) | 9.17 (4.64) | 62 (68.9) | 7.47 (2.24) | 7.78 (2.38) | 8.85 (1.92) | 7.71 (2.22) | 8.27 (2.04) | |
| p = 0.198 | p = 0.006* | p = 0.584 | p = 0.152 | p = 0.461 | p = 0.213 | p = 0.224 | p = 0.482 | p = 0.831 | |||
| Public transport | Yes | 94 (21.3) | 24.14 (2.8) | 8.42 (1.04) | 10.57 (0.84) | 24 (26.7) | 7.57 (2.25) | 8.08 (2.01) | 8.97 (2.02) | 7.91 (2.16) | 8.87 (1.67) |
| No | 348 (78.7) | 20.89 (1.59) | 8.15 (1.19) | 8.84 (0.95) | 66 (73.3) | 7.36 (2.35) | 7.56 (2.58) | 8.70 (2.11) | 7.58 (2.42) | 8.08 (2.27) | |
| p = 0.062 | p = 0.868 | p = 0.017* | p = 0.321 | p = 0.580 | p = 0.201 | p = 0.432 | p = 0.400 | p = 0.028 | |||
| Serving COVID-19 patients | Yes | 82 (18.6) | 23.75 (4.76) | 8.50 (2.21) | 9.00 (1.77) | 22 (24.4) | 7.65 (2.25) | 7.85 (2.47) | 8.46 (2.39) | 7.60 (2.32) | 8.68 (1.80) |
| No | 360 (81.4) | 21.40 (1.45) | 8.18 (1.00) | 9.36 (0.83) | 68 (75.6) | 7.35 (2.34) | 7.63 (2.48) | 8.83 (2.02) | 7.66 (2.38) | 8.15 (2.25) | |
| p = 0.026 | p = 0.195 | p = 0.125 | p = 0.255 | p = 0.445 | p = 0.609 | p = 0.309 | p = 0.890 | p = 0.163 | |||
| Getting Covid-19 test | Yes | 77 (17.2) / positive:2 | 20. 57 (8.95) | 7.65 (4.85) | 8.47 (4.81) | 20 (22.2) | 6.89 (2.58) | 7.07 (2.66) | 8.10 (2.61) | 7.07 (2.56) | 8.21 (2.49) |
| No | 365 (82.8) | 19.66 (7.87) | 6.89 (3.64) | 9.20 (4.67) | 70 (77.8) | 7.51 (2.26) | 7.79 (2.42) | 8.90 (1.95) | 7.77 (2.31) | 8.26 (2.12) | |
| p = 0.526 | p = 0.268 | p = 0.382 | p = 0.317 | p = 0.136 | p = 0.104 | p = 0.082 | p = 0.099 | p = 0.895 | |||
| Current working status | Full-time | 274 (62.0) | 19.89 (8.52) | 6.92 (3.98) | 8.64 (4.78) | 50 (55.6) | 7.37 (2.42) | 7.51 (2.64) | 8.67 (2.26) | 7.62 (2.49) | 8.17 (2.29) |
| Part-time | 18.83 (1.11) | 18.83 (7.74) | 6.95 (3.65) | 9.96 (4.60) | 24 (26.7) | 7.00 (2.21) | 7.52 (2.23) | 8.50 (2.13) | 7.52 (2.06) | 8.08 (2.17) | |
| Emergency patient only | 38 (8.6) | 23.57 (5.38) | 8.78 (4.04) | 9.84 (3.83) | 12 (13.3) | 7.94 (2.04) | 8.47 (2.03) | 9.47 (1.12) | 7.84 (2.38) | 8.73 (1.62) | |
| Not working | 32 (7.2) | 18.18 (6.45) | 6.31 (2.93) | 10.50 (4.96) | 4 (4.4) | 8.06 (1.94) | 8.37 (2.09) | 9.43 (0.81) | 7.93 2.29) | 8.81 (1.86) | |
| Unpaid vacation/fired | 2 (0.5) | 13 | 1 | 4 | 0 | 10 | 10 | 10 | 10 | 10 | |
| p = 0.500 | p = 0.213 | p = 0.824 | p = 0.964 | p = 0.835 | p = 0.951 | ||||||
| Filiation service | Yes (FY) | 66 (14.9) | 22.51 (8.98) | 8.51 (4.49) | 9.96 (4.59) | 24 (26.7) | 7.45 (2.59) | 7.33 (2.55) | 8.39 (2.29) | 7.24 (2.30) | 8.60 (2.06) |
| No (FN) | 376 (85.1) | 19.35 (7.80) | 6.76 (3.71) | 8.92 (4.71) | 66 (73.3) | 7.39 (2.28) | 7.73 (2.46) | 8.82 (2.06) | 7.72 (2.37) | 8.19 (2.20) | |
| p = 0.037* | p = 0.240 | p = 0.016* | p = 0.013* | p = 0.900 | p = 0.393 | p = 0.272 | p = 0.278 | p = 0.316 | |||
| Patients’ distribution (9 >) | 0 | 156 (35.5) | 19.17 (7.39) | 7.41 (3.67) | 9.34 (4.39) | 36 (40.0) | 7.37 (2.37) | 7.66 (2.41) | 8.82 (1.15) | 7.74 (2.25) | 8.15 (1.86) |
| ≤ 25 | 197 (44.3) | 20.26 (8.24) | 6.72 (4.07) | 9.00 (5.19) | 38 (42.2) | 7.33 (2.44) | 7.48 (2.70) | 8.65 (2.21) | 7.56 (2.60) | 8.52 (2.23) | |
| 26–50 | 40 (9.0) | 22.20 (8.40) | 7.55 (4.08) | 9.20 (4.59) | 10 (11.1) | 7.80 (1.93) | 7.75 (2.33) | 8.40 (2.47) | 6.75 (2.24) | 7.65 (2.81) | |
| 51–75 | 25 (5.9) | 18.07 (10.37) | 6.30 (4.04) | 7.26 (3.78) | 4 (4.4) | 6.92 (2.56) | 8.07 (2.25) | 8.84 (1.46) | 7.92 (1.65) | 7.07 (2.84) | |
| 76 ≤ | 24 (5.4) | 18.33 (6.99) | 6.83 (3.24) | 9.25 (3.64) | 2 (2.2) | 8.08 (1.08) | 8.66 (1.15) | 9.83 (0.57) | 9.08 (1.24) | 9.00 (1.04) | |
| p = 0.364 | p = 0.916 | p = 0.823 | p = 0.746 | p = 0.665 | p = 0.836 | p = 0.856 | p = 0.127 | p = 0.026* | |||
| Patients distribution (65 <) | 0 | 86 (19.5) | 20.55 (8.26) | 6.88 (3.63) | 9.76 (5.82) | 10 (11.1) | 7.58 (1.80) | 8.06 (1.91) | 9.18 (1.45) | 7.90 (2.30) | 8.13 (2.11) |
| ≤ 25 | 170 (38.5) | 19.22 (8.35) | 6.96 (4.01) | 9.47 (4.54) | 38 (42.2) | 7.02 (2.37) | 7.29 (2.60) | 8.44 (2.40) | 7.32 (2.37) | 8.16 (2.13) | |
| 26–50 | 136 (30.8) | 19.77 (7.74) | 7.23 (3.90) | 9.02 (4.56) | 34 (37.8) | 7.60 (2.45) | 7.82 (2.50) | 8.97 (1.76) | 8.00 (2.21) | 8.50 (2.14) | |
| 51–75 | 44 (10.0) | 21.59 (7.78) | 7.13 (3.97) | 6.81 (3.81) | 6 (6.7) | 7.72 (2.67) | 7.68 (2.88) | 8.36 (2.75) | 7.09 (3.23) | 8.04 (2.81) | |
| 76 ≤ | 6 (1.4) | 18.66 (8.14) | 5.00 4.35) | 6.00 (6.08) | 2 (2.2) | 9.00 (1.00) | 9.33 (0.57) | 10.00 (0.00) | 9.96 (0.57) | 8.33 (0.57) | |
| p = 0.665 | p = 0.669 | p = 0.586 | p = 0.398 | p = 0.656 | p = 0.730 | p = 0.891 | p = 0.276 | p = 0.506 | |||
| Number of patients treated per week (before COVID-19) | ≤ 10 | 32 (7.2) | 14.37 (6.83) | 5.87 (3.36) | 8.25 (6.04) | 2 (2.2) | 6.93 (1.80) | 6.75 (2.17) | 7.81 (2.31) | 7.62 (1.99) | 8.00 (1.96) |
| 11–50 | 177 (40.3) | 19.22 (7.36) | 7.04 (3.77) | 9.58 (4.64) | 36 (40.0) | 7.23 (2.36) | 7.64 (2.46) | 8.91 (1.96) | 7.76 (2.22) | 8.23 (2.06) | |
| 51–100 | 126 (28.5) | 19.96 (8.09) | 6.57 (3.46) | 8.53 (4.26) | 18 (20.0) | 7.65 (2.17) | 7.92 (2.50) | 9.00 (1.98) | 7.84 (2.46) | 8.14 (2.34) | |
| 101–150 | 49 (10.9) | 23.04 (7.90) | 8.83 (4.15) | 9.79 (4.74) | 18 (20.0) | 7.95 (2.71) | 8.41 (2.30) | 9.00 (2.06) | 7.79 (2.41) | 8.75 (1.98) | |
| 150–200 | 24 (5.4) | 24.33 (7.76) | 7.66 (4.39) | 10.08 (4.16) | 10 (11.1) | 7.75 (2.49) | 7.00 (3.04) | 8.16 (2.65) | 7.08 (2.53) | 8.08 (2.50) | |
| 200< | 34 ( | 19.82 (10.08) | 6.64 (5.07) | 7.52 (5.31) | 6 (6.7) | 6.82 (2.42) | 7.23 (2.43) | 8.11 (2.44) | 6.64 (2.91) | 8.41 (2.57) | |
| p = 0.289 | p = 0.673 | p = 0.224 | p = 0.048 | p = 0.280 | p = 0.220 | p = 0.166 | p = 0.665 | p = 0.595 | |||
| Number of patients treated per week (after COVID-19) | ≤ 10 | 164 (37.1) | 17.82 (7.17) | 6.41 (3.75) | 8.98 (4.78) | 26 (28.9) | 7.46 (2.21) | 7.81 (2.40) | 8.89 (0.21) | 7.96 (1.91) | 8.35 (1.90) |
| 11–50 | 210 (47.5) | 21.31 (7.93) | 7.44 (3.71) | 9.40 (4.40) | 50 (55.6) | 7.45 (2.13) | 7.61 (2.40) | 8.67 (2.16) | 7.56 (2.26) | 8.21 (2.16) | |
| 51–100 | 52 (11.8) | 21.19 (9.69) | 7.53 (4.69) | 7.61 (4.11) | 12 (13.3) | 7.30 (3.15) | 7.73 (2.93) | 9.23 (1.77) | 7.84 (2.73) | 8.65 (2.41) | |
| 101–150 | 12 (2.7) | 18.00 (9.03) | 6.83 (4.30) | 11.50 (8.59) | 2 (2.2) | 6.16 (3.37) | 6.33 (2.94) | 6.83 (3.60) | 5.16 82.71) | 6.83 (3.18) | |
| 150–200 | 4 (0.9) | 11.00 (2.82) | 3.50 (3.53) | 7.50 (9.19) | 0 | 7.50 (2.12) | 8.00 (2.82) | 8.00 (2.82) | 5.00 (5.65) | 5.00 (5.65) | |
| p = 0.131 | p = 0.845 | p = 0.004 | p = 0.649 | p = 0.195 | p = 0.647 | p = 0.242 | p = 0.011* | p = 0.112 | |||
| Occupational risk in COVID-19 pandemic | Extremely | 288 (65.2) | 21.01 (8.07) | 7.06 (4.06) | 9.06 (4.47) | 66 (73.3) | 7.94 (1.93) | 8.29 (2.08) | 9.22 (1.57) | 8.11 (2.11) | 8.59 (1.85) |
| High | 134 (30.3) | 17.46 (7.25) | 6.80 (3.44) | 8.85 (4.54) | 20 (22.2) | 6.53 (2.58) | 6.77 (2.65) | 8.26 (2.42) | 7.10 (2.53) | 7.71 (2.53) | |
| Moderate | 12 (2.7) | 17.16 (10.77) | 6.66 (3.61) | 7.00 (6.89) | 2 (2.2) | 6.33 (3.14) | 5.33 (3.01) | 6.16 (2.78) | 5.50 (1.87) | 7.33 (2.42) | |
| Low | 4 (0.9) | 28.00 (5.65) | 11.50 (7.77) | 16.00 (7.07) | 2 (2.2) | 4.00 (0.00) | 3.50 (0.50) | 4.50 (1.50) | 4.50 (4.94) | 9.50 (0.70) | |
| No risk | 4 (0.9) | 13.00 (2.82) | 7.50 (0.70) | 17.00 (9.89) | 2 (2.2) | 4.50 (3.50) | 4.50 (3.50) | 4.50 (3.50) | 3.00 (2.82) | 3.50 (2.50) | |
| p = 0.568 | p = 0.000* | p = 0.000* | p = 0.486 | p = 0.000* | p = 0.000* | p = 0.000* | p = 0.000* | p = 0.015* | |||
| Working knowledge about COVID-19 pandemic | Yes | 298 (67.4) | 18.91 (7.86) | 6.82 (3.91) | 8.73 (4.65) | 64 (71.1) | 7.18 (2.34) | 7.36 (2.52) | 8.57 (2.23) | 7.50 (2.43) | 8.06 (2.21) |
| No | 144 (32.6) | 21.70 (8.15) | 7.43 (3.79) | 9.79 (4.74) | 26 (28.9) | 7.87 (2.32) | 8.30 (2.27) | 9.16 (1.71) | 7.97 (2.20) | 8.65 (2.08) | |
| p = 0.015* | p = 0.18 | p = 0.278 | p = 0.554 | p = 0.037 | p = 0.008* | p = 0.030* | p = 0.169 | p = 0.059 | |||
A statistically significant decrease in the number of patients treated by participants per week was found after the pandemic (p < 0.001). When the dental treatments provided by the participants are evaluated, 24.4% of the participants stated that they did not perform aerosol-generating procedures. The proportions of the participants who performed intraoral examination, radiographic examination, and aerosol-generating procedure were 61.1%, 42.1% and 66.1%, respectively. Of the participants who performed aerosol-generating procedures, 67.8% (n = 198) used an N95 or an FFP3 mask. Personal protective equipment used rates were as following: surgical mask 92.3%, protective goggles 68.8%, gloves 97.3%, box 91%, face visor 93.7%, bonnet 81.4% and N95 / FFP3 mask 63.8%. The burnout and stress levels of participants who used N95 masks in clinical procedures were twice as high as the others.
Pearson’s correlations showed that EE was moderately positively correlated with general, personal and occupational stress levels (Table 2).
Table 2.
Correlation matrix between MBI subgroup scores and participants stress levels
| Stress Levels | |||||
|---|---|---|---|---|---|
| Subgroups | General | Personal | Occupational | Family | Patient |
| EE |
r = 0.510 p < 0.01 |
r = 0.467 p < 0.01 |
r = 0.487 p < 0.01 |
r = 0.248 p < 0.01 |
r = 313 p < 0.01 |
| DP |
r = 0.239 p < 0.01 |
r = 0.200 p < 0.01 |
r = 0.317 p < 0.01 |
r = 0.088 p < 0.01 |
r = 0.125 p < 0.01 |
| PG |
r = 0.188 p < 0.01 |
r = 0.213 p < 0.01 |
r = 0.222 p < 0.01 |
r = 0.150 p < 0.01 |
r = 165 p < 0.01 |
Second Stage Results (Comparative Evaluations)
The FP group contained 330 dentists, and the FN group contained 376 dentists. The age range of the FP dentists was significantly higher than the FN dentists (p < 0.001). All the FP dentists served in a public hospital, and most of them were not specialists (75.8%). A statistically significant difference was found between the FP and FN groups according to academic degree and filiation (p < 0.001). Most participants of both groups (63.6% of FP and 68.1% of FN) stated that they had sufficient knowledge about the COVID-19 pandemic.
A statistically significant decrease was noted in the number of patients treated by participants per week after the pandemic in the FP group (p < 0.001). Dentists in the FP group were statistically significantly more likely to avoid aerosol-generating procedures. The COVID-19 test and positivity rates were six times higher in the FP group than the FN group.
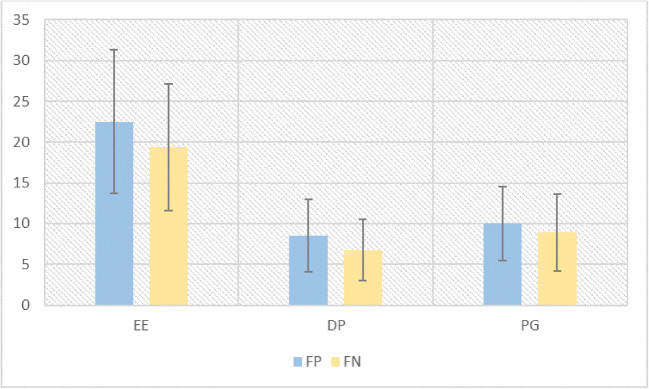
The FP group showed significantly higher stress levels than the FN group (Table 3). Occupational burnout levels were 34.4% for the FP group and 17.6% for the FN group. The distribution of burnout subgroups according to filiation service is shown in Fig. 2. A statistically significant difference was found between the burnout levels of participants according to filiation service (p < 0.001) (Table 3).
Table 3.
Burnout-subgroups and Stress levels scores of participants according to filiation serve (n: 706)
| n (%) | Emotional exhaustion (MBI) Mean (SD) |
Depersonalization (MBI) Mean (SD) |
Personal gratification (MBI) Mean (SD) |
Burnout n (%) |
Stress level (General) Mean (SD) |
Stress level (Personal) Mean (SD) |
Stress level (Family) Mean (SD) |
Stress level (Patient) Mean (SD) |
Stress level (Occupational) Mean (SD) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| FP | 330 (46.7) | 22.51 (8.87) | 8.51 (4.43) | 9.96 (4.53) | 120 (64.5) | 8.45 (2.56) | 8.85 (2.52) | 8.39 (2.26) | 7.24 (2.27) | 9.10 (2.03) |
| FN | 376 (53.3) | 19.35 (7.80) | 6.76 (3.71) | 8.92 (4.71) | 66 (35.5) | 7.36 (2.28) | 7.73 (2.46) | 8.82 (2.06) | 7.72 (2.37) | 8.19 (2.20) |
| p = 0.000* | p = 0.000* | p = 0.035* | p = 0.000* | p = 0.000* | p = 0.000* | p = 0.059 | p = 0.051 | p = 0.000* |
Fig. 2.
Comparison of burnout subgroups
Discussion
This study was designed to evaluate the factors affecting the ability and willingness of dentists to work during the COVID-19 pandemic and the effect of this situation on their occupational burnout. Results of this study show that approximately 20.83 ± 8.46, 7.58 ± 4.15, 9.41 ± 4.65 of the study population experienced EE, DP and PG, respectively. In addition, 20% of the dentists suffered from burnout. Based on these results, the first hypothesis was rejected. Additionally, the occupational burnout levels of the dentists serve in filiation service were significantly higher than the dentists who were not serve. Hence, the second hypothesis was also rejected. The reason for this situation may be the fact that dentists have been burdened with a mission that is not in the job description, the increased risk of contamination and the change in working conditions.
The pandemic affected the field of dentistry as well as many professional groups. Both individuals and the government have implemented many changes in working conditions (Schiff et al., 2020; Şahin et al., 2020). Healthcare workers are affected by epidemics and pandemics, especially those working with infected patients. During the outbreak of the severe acute respiratory syndrome (SARS) epidemic in 2003, the H1N1 pandemic in 2009, MERS-CoV in 2014 and recently, COVID-19 in 2020, researchers observed that members of the healthcare community experienced high levels of psychological stress and occupational burnout (Memish et al., 2014; Mobaraki & Ahmadzadeh, 2019; Shacham et al., 2020a, b; Sim & Chua, 2004).
Studies evaluating the stress levels of dental staff during COVID-19 period indicate that stress levels vary between 11.5% and 81.5% (Duruk et al., 2020; Shacham et al., 2020a, b; Şahin et al., 2020; Özdede & Sahin, 2020). This broad range may be due to the uncertainty about the ongoing management of COVID-19 in many countries and the diversity of possible risk factors evaluated in the studies. In a study evaluating the concerns about the COVID-19 pandemic of dental students in Turkey, high level of anxiety was reported (Özdede & Sahin, 2020). This study revealed that most dentists have high stress levels. In line with current research, another study showed that psychological distress level of dentists ranging from 55.6% to 81.5% (Duruk et al., 2020). Another study conducted during COVID-19 pandemic period showed that the dentists had the “extremely stress” from infecting their families (Sarialioglu et al., 2021).
MBI and Copenhagen Burnout Inventory (CBI) are two different scales specially adapted for those working in the healthcare sector and proved by validity and reliability tests to comply with Turkish culture. A study comparing these two scales showed that MBI only deals with burnout at occupational level. For these reasons, MBI, whose validity and reliability study were conducted by Ergin et al. in 1992, was used to determine occupational burnout in this study (Çapri, 2006; Çapri et al., 2011; Ergin, 1992; Yildirim & İçerli, 2010). According to MBI results, in this study, occupational burnout was observed in 20% of the dentists in this study. To our knowledge, this is the first study focusing on and comparing the occupational burnout frequency and related factors of dentists during COVID-19 pandemic in Turkey. In studies examining the occupational burnout of dentists/dental students/dental personnel before COVID-19 pandemic in Turkey, the occupational burnout rate varied between 8% and 29% (Eren et al., 2016; Huri et al., 2017; Huri et al., 2016). Recent estimates about the prevalence of burnout among healthcare professionals, including dentists, put the prevalence between 8 and 36% before the COVID-19 pandemic in the world (Collin et al., 2019). According to these results, the prevalence of occupational burnout in dentistry before and during the COVID-19 pandemic is parallel. Although it has been reported that the stress and burnout rates of other healthcare professionals have increased compared to the pre-pandemic period, these rates did not show remarkable variation in dentistry (Barello et al., 2020; Matsuo et al., 2020). The fact that dentists were working under harsh conditions and their long-term and stressful working conditions before the pandemic may have facilitated their adaptation to pandemic conditions.
Anxiety and stress in physicians during the epidemic were found to have a positive correlation with MBI scores (Patel et al., 2018; Shah, Kamrai, et al., 2020). Lack of control over procedures, infection control measures, incorrect concepts of security measures, poor communication and directives, lack of preparedness and emotional support, inadequate personal protective equipment, and perceived death are among the factors that cause burnout. In addition, new policies and procedures, the stress of both staff and patients, and the possibility that infected individuals (staff or patients) can be detected at any time in the workplace can be a source of burnout (Shah, Kamrai, et al., 2020). In addition, studies show that perceived job insecurity and fear of COVID-19 are positively associated with depressive symptoms (Gasparro et al., 2020). In the United States, about 54.4% of physicians have shown at least one symptom of burnout in the form of EE, DP, or reduced senses of accomplishment during the COVID-19 pandemic period (Shah, Chaudhari, et al., 2020). According to the results of a survey given to Italian healthcare workers, the level of EE was higher than normative values (Barello et al., 2020). In this study, most of the participants showed a high level of EE, a moderate level of DP and a low level of PG.
In studies evaluating the level of burnout of healthcare workers during COVID-19 pandemic, female have been shown to higher levels of EE than male (Barello et al., 2020; Matsuo et al., 2020). In this study, a significant difference was observed in DP level depending on gender. In addition, all stress levels were significantly higher in female except occupational stress. In pre-pandemic period, in a study that evaluate the levels of burnout among dentist in Turkey, EE and DP levels were significantly higher in female. In the same study, the most emotionally depleted group was dentists in the 36–45 age group, while those in the 46–55 age group showed the highest increasing DP scores (Huri et al., 2016). In this study, no significant difference was observed among age groups. The reason for this situation may be that the age groups are categorized differently. It has been shown in many studies that an academic degree affects the level of burnout (Divaris et al., 2012; Hakanen et al., 2014; Huri et al., 2016; Reyes-Torres et al., 2012; Vered et al., 2014; Zini et al., 2013). This study was performed in COVID-19 pandemic process in Turkey, and health workers were summoned to duty regardless of academic degrees. This may be the reason why there is no difference in burnout levels. On the other hand, a significant difference was observed in occupational stress levels depending on the academic degree. Similar to the results of this study, authors stated that there is more EE and DP in dentists working in the public sector compared to dentists working in the private sector (de Ruijter et al., 2015; Hakanen et al., 2014; Vered et al., 2014; Zini et al., 2013).
Oral and dental health service is not only related to the knowledge and skills of the dentist, but also to the order and continuity of the work of all dental staff. A healthy continuation of the workflow requires sharing of responsibility and teamwork of all the dental staff working with the dentist (Yener et al., 2012). Severe conditions such as a pandemic can negatively affect the coping mechanisms and work stress of all dental staff, causing burnout. A recent study found among Israeli dental staff a positive link between subjective overload and psychological distress (M. Shacham et al., 2020a and b). Also, it was stated that dentists in different countries will exhibit different levels of subjective overload due to their healthcare systems’ instructions, which in turn may affect their psychological distress and burn out (Mijiritsky et al., 2020).
During dental treatments, strong saliva ejectors and personal protective equipment reduce the risk of contamination (Samaranayake et al., 1989). Minimizing the use of ultrasonic instruments, high-speed handpieces, and 3-way syringes may also reduce the risk of contaminated aerosols (Ather et al., 2020). If adequate precautions are not taken, visits to the dental office can potentially expose patients to cross contamination. A study reported that while 63.79% of Turkish dentists used strong dental suction during dental procedures, 49.95% avoided performing aerosol-forming procedures as much as possible (Duruk et al., 2020). In this study, the rate of dentists who did not perform the procedures containing aerosol was 24% and 67.8% of the dentists who performed the procedures containing aerosol were using N95 / FFP3 masks. In the aforementioned study, the rate of using N95 masks was reported as 12.36% of the dentists (Duruk et al., 2020). The differences can be attributed to the fact that the studies were conducted at different times during the pandemic period, and the dentists’ knowledge about the disease increased. In this study, the burnout level was twice as high in dentists who did not use N95 masks. However, the continuous use of personal protective equipment contributes to physical fatigue and mental pressures in healthcare workers (Al-Rabiaah et al., 2020).
Researchers reported that fear of transmitting the virus to family and coworkers was the top concern of dentists and frontline healthcare workers (Ahmed et al., 2020). In another study conducted in Turkey, more than 90% of dentists are concerned about COVID-19 contamination, and 95% are concerned about carrying this virus to their families (Duruk et al., 2020). In this study, no significant difference was observed between stress levels in the general, personal, patient, and occupational categories, while the highest rate was observed in the family-related stress level.
The level of professional burnout was higher in dentists who worked in the filiation service (34.4%). Dentists involved in filiation are more likely to have direct contact with patients with COVID-19, and changes in working conditions may cause an increase in burnout rate. The COVID-19 knowledge levels of both FP and FN dentists were similar. Other factors, including age, academic degree, patients treated per week before and after the pandemic, COVID-19 test positivity rates, and willingness to perform aerosol-generating procedures, supported the high levels of burnout and stress.
Factors that may contribute to reducing burnout include creating up-to-date guidelines specific to the unit where healthcare professionals work, having adequate and accessible personal protective equipment, and increasing the employment of auxiliary and administrative staff for non-clinical duties to alleviate the burden of physicians, as can ensuring the safety and health of all staff members by periodical screening of vital signs, possible symptoms of infection, and signs of burnout. Psychiatric support can be provided in addition to these screenings (Shah, Chaudhari, et al., 2020).
This study has several limitations. The survey used in this study was delivered to the participants via the internet. Although participants were assured of their anonymity, worry about identification may have caused participants to reduce their score on burnout questions. Moreover, even with an 88.25% response rate, selection bias may have skewed our results if very distressed staff members or those with little distress chose not to participate. Finally, it is important to state that the survey was conducted at a certain point in the pandemic. In these aspects, the generalization of the findings and comparison with normative data may be limited.
Burnout and stress levels are multifaceted, and more detailed studies are needed to address all aspects.
Conclusion
According to the results of this study evaluating the burnout level of dentists in Turkey during COVID-19 pandemic, 20% of participants were seen in occupational burnout. This rate was significantly higher for dentists serve in filiation service.
The COVID-19 pandemic has strained the entire healthcare system. It is vital to remediate the burnout issue among healthcare workers, including dentists, with concrete actions to avoid potential short-term and long-term adverse outcomes. Dentists are in the high-risk group, and personal protective equipment, support and updated information can reduce one possible cause of burnout. It is important to inform physicians before their service and to take preventive measures to reduce the effect of sudden changes in working conditions, such as dentists’ working on the filiation service. On the other hand, dentists must be prepared to take a different role in the public health emergency management system and tackle life-threatening diseases.
Supplementary Information
(XLSX 257 kb)
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Merve Özarslan and Secil Caliskan. All authors read and approved the final manuscript.
Funding
The authors did not receive support from any organization for the submitted work.
Data Availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics Approval
The study was approved by Turkey’s Ministry of Health and the Akdeniz University Faculty of Medicine Clinical Research Ethics Committee (approval no: KAEK-590). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, Khurshid Z. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. International Journal of Environmental Research and Public Health. 2020;17(8):2821. doi: 10.3390/ijerph17082821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahola K, Hakanen J, Perhoniemi R, Mutanen P. Relationship between burnout and depressive symptoms: A study using the person-centred approach. Burnout Research. 2014;1(1):29–37. doi: 10.1016/j.burn.2014.03.003. [DOI] [Google Scholar]
- Al-Rabiaah A, Temsah M-H, Al-Eyadhy AA, Hasan GM, Al-Zamil F, Al-Subaie S, Alsohime F, Jamal A, Alhaboob A, Al-Saadi B. Middle East respiratory syndrome-Corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. Journal of Infection and Public Health. 2020;13(5):687–691. doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. Journal of Endodontics. 2020;46(5):584–595. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. Journal of Advanced Nursing. 2005;51(3):276–287. doi: 10.1111/j.1365-2648.2005.03494.x. [DOI] [PubMed] [Google Scholar]
- Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Research. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baud, D., Qi, X., Nielsen-Saines, K., Musso, D., Pomar, L., & Favre, G. (2020). Real estimates of mortality following COVID-19 infection. The Lancet infectious diseases, 20(7), 773. [DOI] [PMC free article] [PubMed]
- Cheng C, Barceló J, Hartnett AS, Kubinec R, Messerschmidt L. COVID-19 government response event dataset (CoronaNet v. 1.0) Nature Human Behaviour. 2020;4(7):756–768. doi: 10.1038/s41562-020-0909-7. [DOI] [PubMed] [Google Scholar]
- Cobbett W. A new French and English dictionary. 1833. [Google Scholar]
- Collin V, Toon M, O'Selmo E, Reynolds L, Whitehead P. A survey of stress, burnout and well-being in UK dentists. British Dental Journal. 2019;226(1):40–49. doi: 10.1038/sj.bdj.2019.6. [DOI] [PubMed] [Google Scholar]
- Çalişkan, S., Delikan, E., & Kizilaslan, S (2019). Dental hemşirelerin mesleki tükenmişlik düzeylerinin değerlendirilmesi. Journal of Biotechnology and Strategic Health Research, 3(3), 192–196.
- Çapri, B. (2006). Tükenmişlik ölçeğinin Türkçe uyarlaması: Geçerlik ve güvenirlik çalışması. Mersin Üniversitesi Eğitim Fakültesi Dergisi, 2(1).
- Çapri, B., Gündüz, B., & Gökçakan, Z. (2011). Maslach tükenmişlik envanteri-öğrenci formu'nun (mte-öf) Türkçe'ye uyarlamasi: Geçerlik ve güvenirlik çalişmasi. Cukurova University Faculty of Education Journal, 40(1).
- de Ruijter RA, Stegenga B, Schaub RM, Reneman MF, Middel B. Determinants of physical and mental health complaints in dentists: A systematic review. Community Dentistry and Oral Epidemiology. 2015;43(1):86–96. doi: 10.1111/cdoe.12122. [DOI] [PubMed] [Google Scholar]
- Demirtas T, Tekiner H. Filiation: A historical term the COVID-19 outbreak recalled in Turkey. Erciyes Medical Journal. 2020;42(3):354–359. [Google Scholar]
- Divaris K, Polychronopoulou A, Taoufik K, Katsaros C, Eliades T. Stress and burnout in postgraduate dental education. European Journal of Dental Education. 2012;16(1):35–42. doi: 10.1111/j.1600-0579.2011.00715.x. [DOI] [PubMed] [Google Scholar]
- Duruk, G., Gümüşboğa, Z. Ş., & Çolak, C. (2020). Investigation of Turkish dentists’ clinical attitudes and behaviors towards the COVID-19 pandemic: A survey study. Brazilian Oral Research, 34. [DOI] [PubMed]
- Eaton L. Health workforce burn-out. World Health Organization. Bulletin of the World Health Organization. 2019;97(9):585–586. doi: 10.2471/BLT.19.020919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embriaco N, Papazian L, Kentish-Barnes N, Pochard F, Azoulay E. Burnout syndrome among critical care healthcare workers. Current Opinion in Critical Care. 2007;13(5):482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- Eren H, Huri M, Bagis N, Basibuyuk O, Sahin S, Umaroglu M, Orhan K. Burnout and occupational participation among Turkish dental students. The Southeast Asian Journal of Tropical Medicine and Public Health. 2016;47(6):1343–1352. [PubMed] [Google Scholar]
- Ergin, C. (1992). Doktor ve hemsirelerde tukenmislik ve Maslach tukenmislik olceginin uyarlanmasi. VII. Ulusal Psikoloji Kongresi, 22th September 1992 Ankara (Turkey).
- Gasparro R, Scandurra C, Maldonato NM, Dolce P, Bochicchio V, Valletta A, Sammartino G, Sammartino P, Mariniello M, Di Lauro AE. Perceived job insecurity and depressive symptoms among Italian dentists: The moderating role of fear of COVID-19. International Journal of Environmental Research and Public Health. 2020;17(15):5338. doi: 10.3390/ijerph17155338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg R, Boss RW, Chan L, Goldberg J, Mallon WK, Moradzadeh D, Goodman EA, McConkie ML. Burnout and its correlates in emergency physicians: Four years' experience with a wellness booth. Academic Emergency Medicine. 1996;3(12):1156–1164. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- Gorter R, Jacobs B, Allard R. Low burnout risk and high engagement levels among oral and maxillofacial surgeons. European Journal of Oral Sciences. 2012;120(1):69–74. doi: 10.1111/j.1600-0722.2011.00923.x. [DOI] [PubMed] [Google Scholar]
- Hakanen JJ, Perhoniemi R, Bakker AB. Crossover of exhaustion between dentists and dental nurses. Stress and Health. 2014;30(2):110–121. doi: 10.1002/smi.2498. [DOI] [PubMed] [Google Scholar]
- Huri M, Bağiş N, Eren H, Başibüyük O, Şahin S, Umaroğlu M, Orhan K. Burnout and occupational participation among dentists with teaching responsibilities in universities. Psychology, Health & Medicine. 2017;22(6):693–700. doi: 10.1080/13548506.2016.1210177. [DOI] [PubMed] [Google Scholar]
- Huri M, Bağış N, Eren H, Umaroğlu M, Orhan K. Association between burnout and depressive symptoms among Turkish dentists. Journal of Dental Sciences. 2016;11(4):353–359. doi: 10.1016/j.jds.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee WJ, Maunder RG, Goldbloom DS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, Azman AS, Reich NG, Lessler J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Annals of Internal Medicine. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu M. Visual Capitalist. 2020. The front line: Visualizing the occupations with the highest COVID-19 risk. [Google Scholar]
- Maslach, C. & S.E. Jackson, (1981). The measurement of experienced burnout. Journal of Organizational Behavior, 2(2), 99–113.
- Matsuo T, Kobayashi D, Taki F, Sakamoto F, Uehara Y, Mori N, Fukui T. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Network Open. 2020;3(8):e2017271–e2017271. doi: 10.1001/jamanetworkopen.2020.17271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayr V, Nußbaumer-Streit B, Gartlehner G. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review (review) Gesundheitswesen (Bundesverband der Arzte des Offentlichen Gesundheitsdienstes (Germany)) 2020;82(6):501–506. doi: 10.1055/a-1164-6611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish Z, Al-Tawfiq J, Makhdoom H, Al-Rabeeah A, Assiri A, Alhakeem R, AlRabiah F, Al Hajjar S, Albarrak A, Flemban H. Screening for Middle East respiratory syndrome coronavirus infection in hospital patients and their healthcare worker and family contacts: A prospective descriptive study. Clinical Microbiology and Infection. 2014;20(5):469–474. doi: 10.1111/1469-0691.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mijiritsky, E., Hamama-Raz, Y., Liu, F., Datarkar, A. N., Mangani, L., Caplan, J., Shacham, A., Kolerman, R., Mijiritsky, O., Ben-Ezra, M., & Shacham, M. (2020). Subjective overload and psychological distress among dentists during COVID-19. International Journal of Environmental Research and Public Health, 17(14). 10.3390/ijerph17145074. [DOI] [PMC free article] [PubMed]
- Mobaraki, K., & Ahmadzadeh, J. (2019). Current epidemiological status of Middle East respiratory syndrome coronavirus in the world from 1.1. 2017 to 17.1. 2018: A cross-sectional study. BMC Infectious Diseases, 19(1), 1–5. [DOI] [PMC free article] [PubMed]
- Mostafa A, Sabry W, Mostafa NS. COVID-19-related stigmatization among a sample of Egyptian healthcare workers. PLoS One. 2020;15(12):e0244172. doi: 10.1371/journal.pone.0244172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W.H. Q&A on coronaviruses (COVID-19) (2020a). Retrieved from: www.who.int/ news-room/q-a-detail/q-a-coronaviruses.
- Organization, W.H . Director-General’s opening remarks at the media briefing on COVID-19. 2020. [Google Scholar]
- OSHA (2020). Worker Exposure Risk to COVID-19. Retrieved from: https://www.osha.gov/Publications/OSHA3993.pdf
- Özdede M, Sahin S. Views and anxiety levels of Turkish dental students during the COVID-19 pandemic. Journal of Stomatology. 2020;73(3):123–128. doi: 10.5114/jos.2020.96867. [DOI] [Google Scholar]
- Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A review. Behavioral Sciences. 2018;8(11):98. doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabaan AA, Al-Ahmed SH, Haque S, Sah R, Tiwari R, Malik YS, Dhama K, Yatoo MI, Bonilla-Aldana DK, Rodriguez-Morales AJ. SARS-CoV-2, SARS-CoV, and MERS-COV: A comparative overview. Le Infezioni in Medicina. 2020;28(2):174–184. [PubMed] [Google Scholar]
- Reyes-Torres M, Ríos-Santos JV, López-Jiménez A, Herrero-Climent M, Bullón-Fernández P. Job satisfaction and depression in SEPA members, and their relation to the burnout syndrome-creation of a structural model. Med Oral Pat Oral Cir Bucal. 2012;17:e821–e824. doi: 10.4317/medoral.17478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samaranayake LP, Reid J, Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC Journal of Dentistry for Children. 1989;56(6):442–444. [PubMed] [Google Scholar]
- Sarialioglu Gungor, A., Donmez, N., & Uslu, Y. S. (2021). Knowledge, stress levels, and clinical practice modifications of Turkish dentists due to COVID-19: A survey study. Brazilian Oral Research, 35. 10.1590/1807-3107bor-2021.vol35.0048. [DOI] [PubMed]
- Schiff, M., Zasiekina, L., Pat-Horenczyk, R., & Benbenishty, R. (2020). COVID-related functional difficulties and concerns among university students during COVID-19 pandemic: A binational perspective. Journal of Community Health, 1–9. [DOI] [PMC free article] [PubMed]
- Shacham M, Hamama-Raz Y, Kolerman R, Mijiritsky O, Ben-Ezra M, Mijiritsky E. COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. International Journal of Environmental Research and Public Health. 2020;17(8):2900. doi: 10.3390/ijerph17082900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shacham, M., Hamama-Raz, Y., Kolerman, R., Mijiritsky, O., Ben-Ezra, M., & Mijiritsky, E. (2020b). COVID-19 factors and psychological factors associated with elevated psychological distress among dentists and dental hygienists in Israel. International Journal of Environmental Research and Public Health, 17(8). 10.3390/ijerph17082900. [DOI] [PMC free article] [PubMed]
- Shah, K., Chaudhari, G., Kamrai, D., Lail, A., & Patel, R. S. (2020). How essential is to focus on physician's health and burnout in coronavirus (COVID-19) pandemic? Cureus, 12(4). [DOI] [PMC free article] [PubMed]
- Shah, K., Kamrai, D., Mekala, H., Mann, B., Desai, K., & Patel, R. S. (2020). Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus, 12(3). [DOI] [PMC free article] [PubMed]
- Shiao JS-C, Koh D, Lo L-H, Lim M-K, Guo YL. Factors predicting nurses' consideration of leaving their job during the SARS outbreak. Nursing Ethics. 2007;14(1):5–17. doi: 10.1177/0969733007071350. [DOI] [PubMed] [Google Scholar]
- Sim K, Chua HC. The psychological impact of SARS: A matter of heart and mind. Cmaj. 2004;170(5):811–812. doi: 10.1503/cmaj.1032003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. Journal of Community Health. 2020;45(6):1168–1177. doi: 10.1007/s10900-020-00921-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, Chen H, Wang D, Liu N, Liu D. Characteristics of COVID-19 infection in Beijing. Journal of Infection. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vered Y, Zaken Y, Ovadia-Gonen H, Mann J, Zini A. Professional burnout: Its relevance and implications for the general dental community. Quintessence International. 2014;45(1):87–90. doi: 10.3290/j.qi.a30763. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. Journal of Travel Medicine. 2020;27(2):taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yener, Ö., Torumtay, G., & Doğan, B. (2012). Diş hekimliğinde yardimci personel eğitimi: Dental implantlar ve biyomateryaller üzerine bir pilot çalişma. Balıkesir Sağlık Bilimleri Dergisi, 1(2), 59–64.
- Yildirim MH, İçerli L. Tükenmişlik Sendromu: Maslach ve Kopenhag Tükenmişlik Ölçeklerinin Karşılaştırmalı Analizi. Organizasyon ve Yönetim Bilimleri Dergisi. 2010;2(1):123–131. [Google Scholar]
- Zini A, Zaken Y, Ovadia-Gonen H, Mann J, Vered Y. Burnout level among general and specialist dentists: A global manpower concern. Occup Med Health Aff. 2013;1(128):e31. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX 257 kb)
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].