Abstract
Treatment of skeletal Class II patients with dual bite and idiopathic condylar resorption (ICR) is challenging for orthodontists because of the unstable position of the mandible as well as skeletal relapse attributed to improper seating of the mandibular condyles. This case report describes the successful treatment of an 18-year-old Mongolian man diagnosed with centric relation–maximum intercuspation discrepancy and ICR. After making a definitive diagnosis from verified centric relation using bilateral manipulation, orthodontic treatment was initiated followed by three-dimensional computer-aided design/computer-aided manufacturing prebent titanium plate–guided sagittal split ramus osteotomy and genioplasty. Postoperative 3D superimposition demonstrated that this surgical guide approach provided accurate repositioning of the condyles, which were well positioned in the fossae. Complete orthodontic and surgical treatment time was 24 months. The patient's facial appearance and occlusion improved significantly, and a stable result was obtained with a 1-year follow-up.
Keywords: Skeletal Class II, ICR, Orthognathic surgery, Computer-aided surgical guide
INTRODUCTION
Idiopathic condylar resorption (ICR), also known as progressive condylar resorption (PCR), is a progressive degenerative disease of the temporomandibular joint (TMJ).1 Resorption in the bilateral condyles usually induces decreased height of the ramus, subsequent opening rotation of the mandible, and decreased chin projection.2 In addition to the skeletal changes, ICR also causes TMJ dysfunction and pain.1 However, Wolford and Cardenas3 showed that 25% patients with ICR have no TMJ symptoms.
Severe skeletal Class II adult ICR patients with mandibular retrusion are often treated by an orthognathic surgical approach (ie, mandibular advancement through sagittal split ramus osteotomy [SSRO]) with the aim of improving both occlusion and facial appearance. SSRO causes a sudden repositioning of the condyle in the fossa, which increases the mechanical load in the joint.1,4 In some patients, the remodeling capacity of their TMJ is exceeded by the functional demands of these sudden changes, and the condyles will resorb.2 To minimize this problem, it is necessary to maintain the position of the condyle to avoid its abnormal rotation while accurately removing surplus bone during surgery.4 As compared with traditional plaster model surgery, three-dimensional (3D) computer-aided simulation and computer-aided design (CAD)/computer-aided manufacturing (CAM) surgical guides ensure highly accurate planned condylar position and bone movements, providing enhanced surgical outcomes.5,6
This case report is of an adult skeletal Class II open bite patient with a centric relation (CR)–maximum intercuspation (MI) discrepancy. The patient was treated orthodontically and surgically guided by preoperative 3D simulation and CAD/CAM prebent titanium plates.
Diagnosis and Etiology
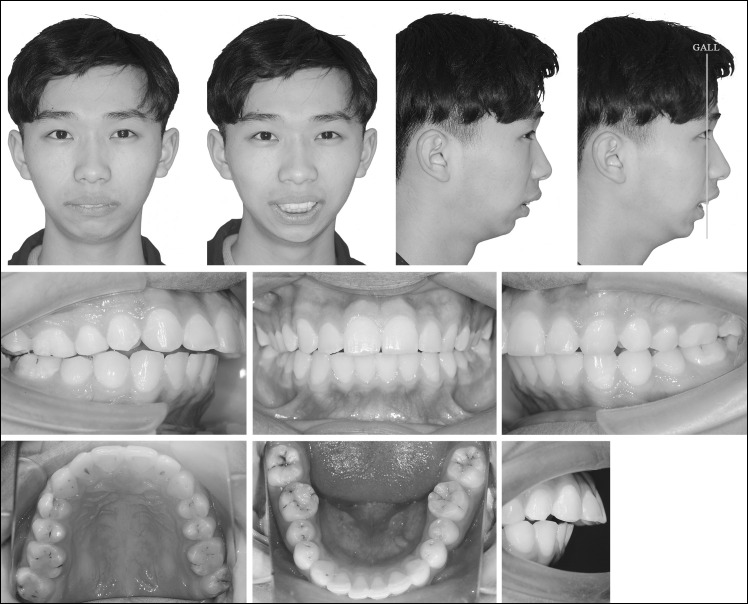
The patient, an 18-year-old Mongolian man, presented to the Department of Orthodontics, West China School of Stomatology. His chief complaint was protrusive profile and a retrusive chin. Facial analysis showed a convex high-angle profile and lower third asymmetry in the frontal view. His maxillary dental midline was coincident with the facial midline, while the mandibular dental midline deviated 1 mm to the right.
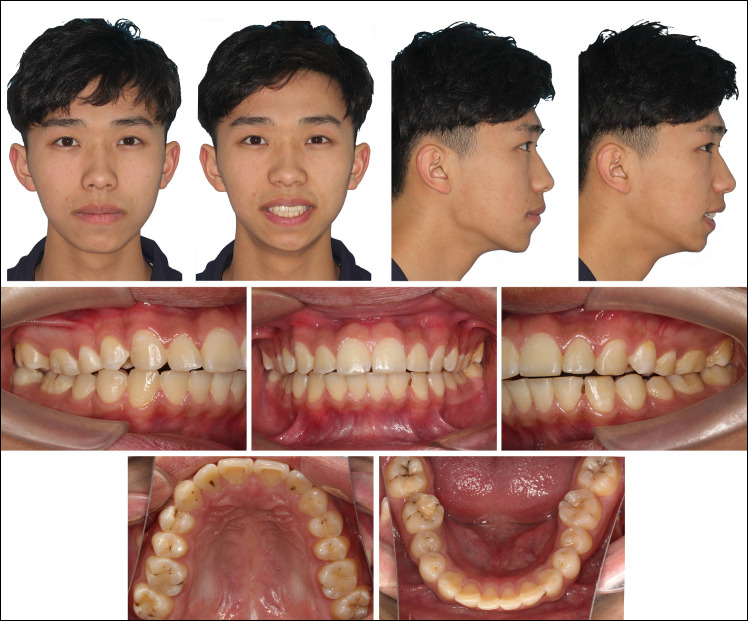
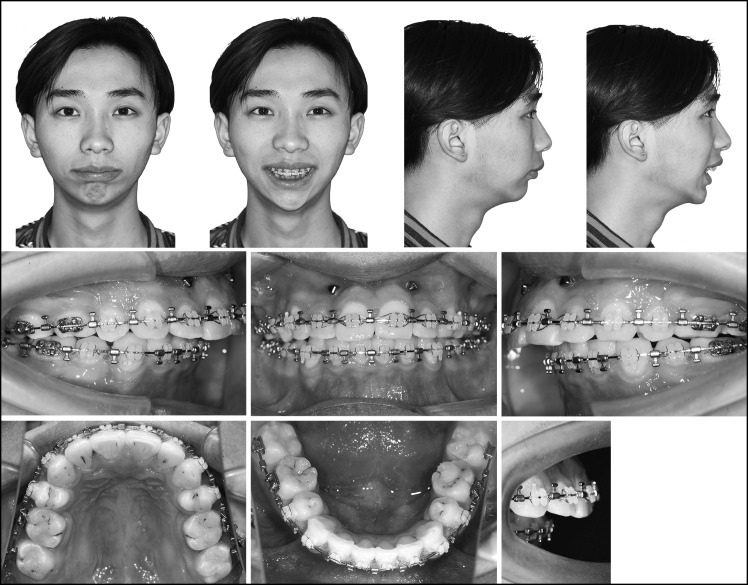
Intraoral analysis demonstrated a lack of occlusal contact from the second premolar to the second premolar with a 1-mm open bite at the incisor region. The periodontium was healthy, whereas extreme attrition was found on the four canines (Figure 1).
Figure 1.
Initial facial and intraoral photographs.
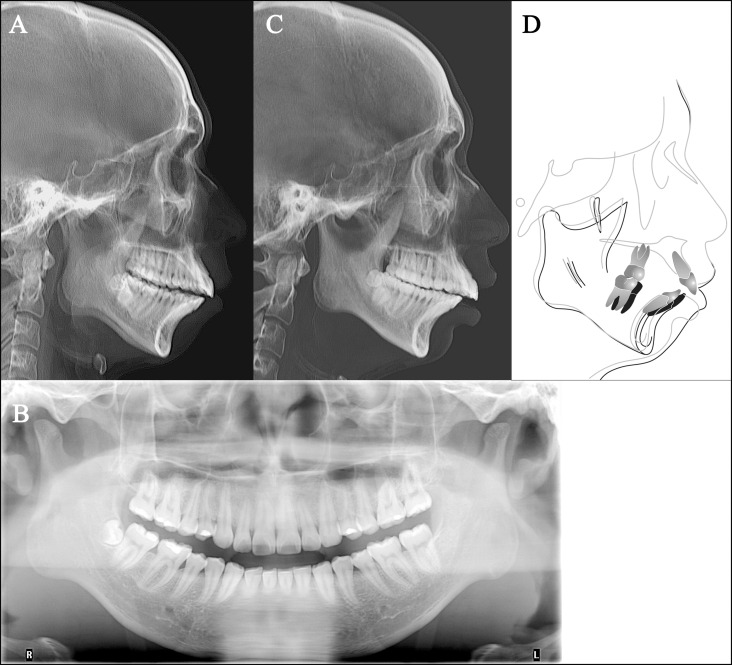
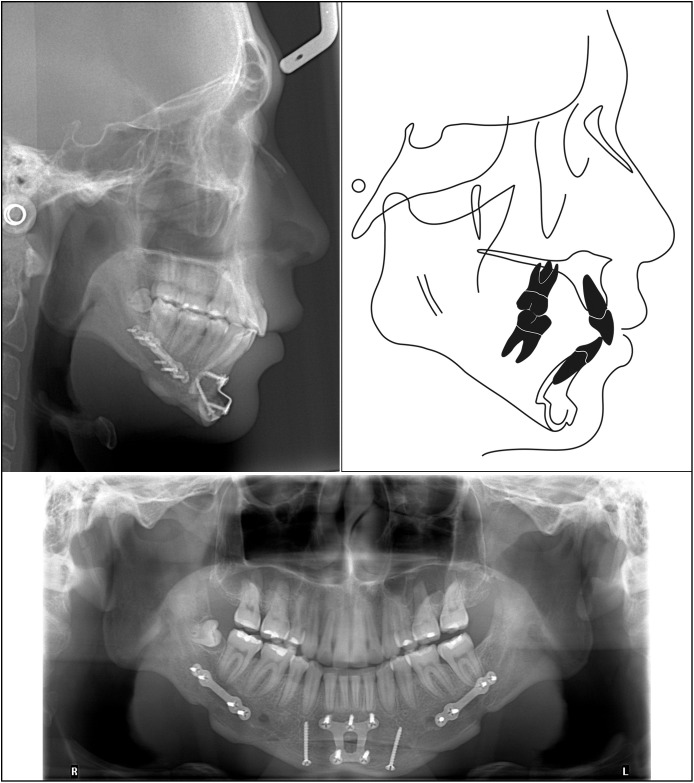
The cephalometric radiograph revealed a retruded mandible and slightly protruded maxilla. The mandibular incisors were severely proclined with relatively well-positioned maxillary incisors, and a hyperdivergent pattern was noticed. The panoramic radiograph indicated right mandibular third molar impaction, bilateral flattened anterosuperior condylar surfaces, and increased antegonial notch depth (Figure 2A,B).
Figure 2.
(A, B), Initial lateral radiograph and panoramic radiograph (in MI). (C) Lateral radiograph in CR. (D) Superimposition of lateral radiographs in CR and MI.
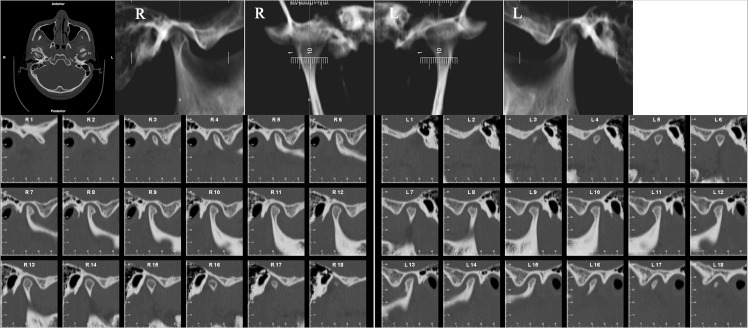
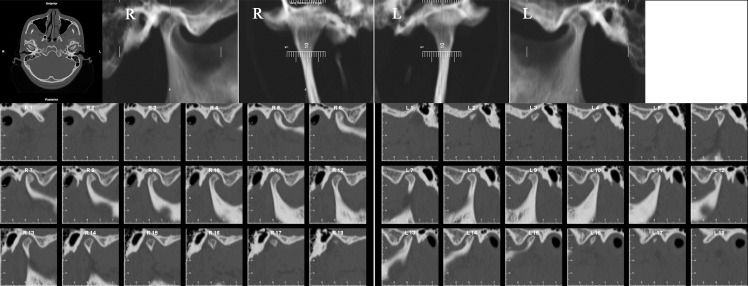
Considering that intracapsular temporomandibular disorders (TMDs) usually cause progressive anterior open bite and extreme attrition,7 the status and function of the patient's TMJ were carefully evaluated based on guidelines established by Dawson.7 Functional assessment illustrated a smooth mouth opening-and-closing pattern and adequate muscle relaxation. Limitations of mouth opening and muscle disharmonies were not observed, and the patient had no functional disorders such as pain or clicking sounds of the TMJ. After determining and verifying the CR using bilateral manipulation and load testing,7 a CR-MI discrepancy was detected. After the condylar position was seated in the CR, facial analysis indicated a severely convex profile, attributable to a retrognathic mandible and chin. Cone-beam computed tomography (CBCT) of the TMJ showed a cup-shaped defect in the superior surface of the left condyle (Figure 3), which indicated a vulnerable stage.8
Figure 3.
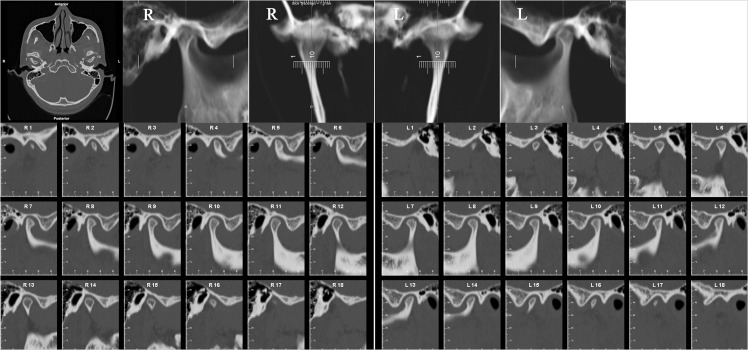
Initial bilateral TMJ radiograph.
After five monthly standard examinations for TMJ and occlusion, it was ascertained that the patient's condylar position had been stabilized without any other TMD symptoms or signs. TMJ radiograph indicated the superior surface of the left condyle had a cortex, but the cortex was not consecutive, suggesting a relatively radiographically stable stage (Figure 4).8 One month later, detailed records for an accurate diagnosis were taken. Casts mounted in CR on the semiadjustable articulator demonstrated a lack of occlusal contact from the left second premolar to the right second premolar with a 1.5-mm open bite at the incisors. Occlusal examination revealed stable contact at the bilateral molars. The molar and canine relationships were end-on Class II on the left and complete Class II on the right (Figure 5). The cephalometric superimposition of CR and MI showed that the mandible was retruded and rotated clockwise, resulting in a more severe skeletal Class II pattern in CR (Figure 2C,D). Facial analysis illustrated a normal gingival display when smiling (not shown in the figure), lip incompetence at rest, and upper incisors protruded by 1 mm in relation to the goal anterior limit line (Figure 6).
Figure 4.
Bilateral TMJ radiograph: 1 month before initiation of treatment.
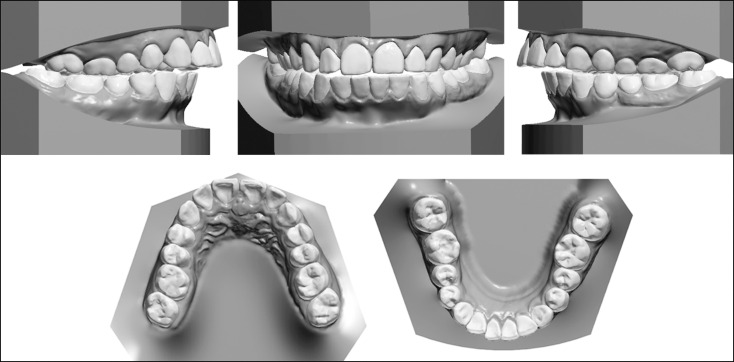
Figure 5.
Digitized dental casts mounted in CR.
Figure 6.
Facial and intraoral photographs in CR.
Treatment Objectives
Because of the potentially destructive phase of the left condyle and CR-MI discrepancy on the first visit, the primary treatment objective was to ascertain the stable conditions of the TMJ and the occlusion.8 After the condylar position had been stable, the following treatment objectives were set in CR: (1) establish ideal functional and stable occlusion and (2) improve soft-tissue esthetics.
Treatment Alternatives
Because of the severity of the skeletal Class II malocclusion, orthodontic treatment alone would not solve the patient's problem. After comprehensive assessment of the surgical simulations for both single-jaw and bimaxillary surgeries, it was determined that both options could improve facial appearance. The bimaxillary surgery option consisted of maxillary impaction with advancement of the mandible. The single-jaw surgery option was mandibular advancement.
According to the cephalometric analysis, the maxilla was relatively well positioned sagittally and vertically without vertical excess, and because the mandible predominantly contributed to this severe jaw discrepancy and facial asymmetry, single-jaw surgery would improve facial appearance and occlusion significantly, comparable with the bimaxillary surgery. In addition, the frontal photograph demonstrated an average smile without gingival exposure. Maxillary impaction would result in the upper lip covering the upper incisors and would be unattractive.9 Because lip coverage of the maxillary incisors tends to increase with age, the bimaxillary surgery could reduce oral esthetics in the long term.10 In addition, because of concerns of the surgery-related risks and treatment costs, the patient decided on an extraction, single-jaw surgery approach: orthodontic treatment with the extraction of four premolars prior to the mandibular advancement surgery using bilateral SSRO combined with genioplasty to correct the retrusive chin. Considering the maxillary incisors were just slightly protruded and there was no severe crowding, extraction of maxillary second premolars was planned. To retract the proclined mandibular anterior teeth and obtain sufficient space for mandibular advancement, mandibular first premolars were also extracted.
Treatment Progress
Initially, the patient was referred to specialists for the evaluation of his periodontal condition, caries, and extraction of four premolars. Subsequently, ceramic 0.022-inch preadjusted brackets (Clarity ADVANCED; 3M, St. Paul, MN) were bonded. After alignment and leveling, 0.018 × 0.025-inch stainless-steel wires were applied to close the space in both arches (Figure 7). Space closure involved controlled lingual tipping movement of the maxillary incisors and retraction of the proclined mandibular incisors. However, it also resulted in a gummy smile with extrusion of the maxillary incisors. To achieve frontal smile esthetics and avoid premature contact of the incisors after surgery, two miniscrews were placed in the maxillary incisor area for intrusion of the incisors.
Figure 7.
Facial and intraoral photographs: space closure.
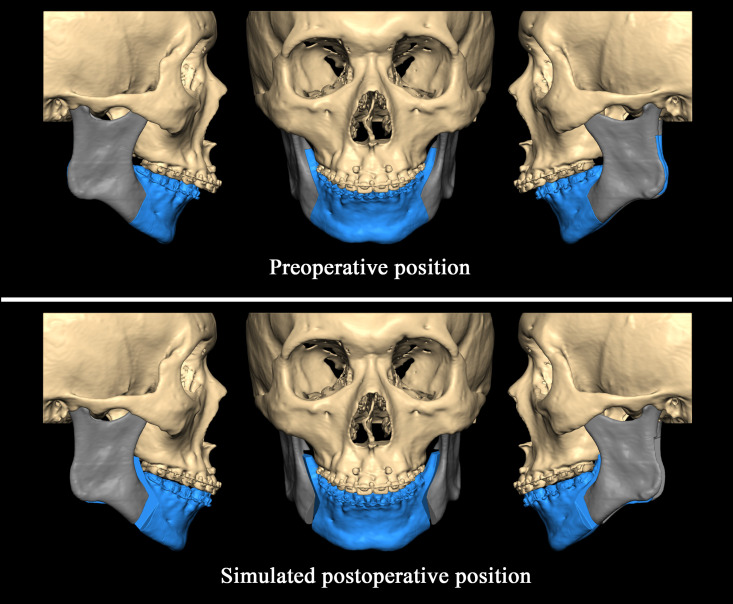
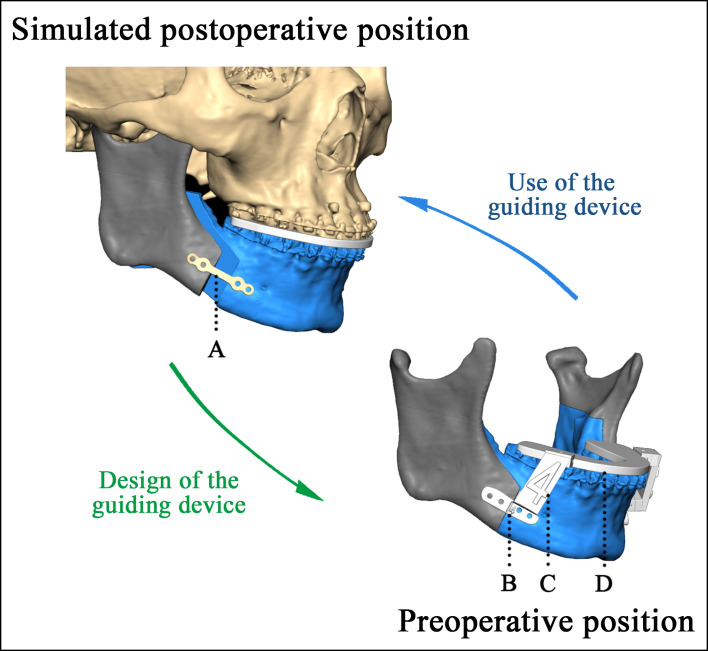
Thirteen months after initial bonding, orthognathic surgery was scheduled. A preoperative 3D model of the skull merged with the models' digital data sets in Mimics (version 10.01; Materialise, Leuven, Belgium) was constructed. A 3D global coordinate system was used to quantify the spatial changes of the bony segments. The final position of the mandibular dentition was based on the position of the maxillary dentition to achieve an Angle Class I relationship, and the bilateral SSRO was performed virtually using Freeform software (version 12.0; Geomagic Studio, Research Triangle Park, NC). The spatial movements of the distal segment were calculated in three dimensions, and interferences between bony segments were simulated and avoided (Figure 8; Table 1). The final occlusal splint, guiding templates, guiding splint, and connecting cylinders were designed and printed out in three dimensions. Meanwhile, the digitized, four-screw titanium plates were prebent according to the 3D-printed resin models (Figure 9).
Figure 8.
Virtual surgical planning: frontal and lateral 3D images.
Table 1.
Spatial Movements of Distal Segmentsa
| Measurement |
Preoperative to Simulated |
| RL, mm | 1.50 |
| AP, mm | 7.32 |
| SI, mm | 3.41 |
| P, ° | −0.20 |
| R, ° | 0.75 |
| Y, ° | 0.34 |
AP indicates anterior-posterior translation; P, pitch; R, roll; RL, right-left translation; SI, superior-inferior translation; Y, yaw. The reference bony landmark for translation (RL, AP, SI) and orientation (P, R, Y) is Pogonion. For RL, “>0” indicates the right direction. For AP, “>0” indicates the anterior direction. For SI, “>0” indicates the superior direction. For P, “<0” indicates the anterior of the distal segment rotated downward. For R, “>0” indicates the left of the distal segment rotated upward. For Y, “>0” indicates the anterior of the distal segment turned left.
Figure 9.
Surgical guiding device. (A) Prebent titanium plate. (B) Guiding template. (C) Connection cylinder. (D) Guiding splint.
Orthognathic surgery was performed one month later. Stainless steel rectangular archwires of 0.019 × 0.025 inches with surgical lugs were placed for intermaxillary fixation (Figure 10). After the mandibular ramus had been exposed, the guiding template on the right side connected to the guiding splint by the cylinder was placed on the mandible (Figure 11). With all holes drilled and vertical cutting lines marked on the mandible according to the marks on the template, the template was removed. This was then repeated on the left side. After mandibular advancement and maxillomandibular fixation with the final splint, the screw holes on the prebent titanium plates were aligned with the screw holes on the corresponding proximal and distal segments. Then, the screws were tightened fully, and the final occlusion was verified and found to be satisfactory and repeatable. Advancement genioplasty was also performed. Light-guiding elastics were placed, and the patient was extubated without complication. Postsurgical orthodontic treatment was started 2 weeks after surgery and continued for 5 months to detail the occlusion (Figure 12).
Figure 10.
Facial and intraoral photographs: just before surgery.
Figure 11.
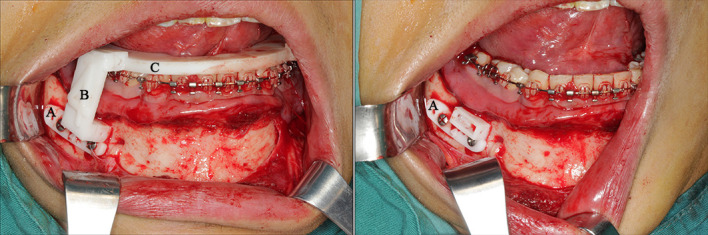
Surgical photographs showing (A) Guiding template, (B) Connection cylinder, and (C) Guiding splint.
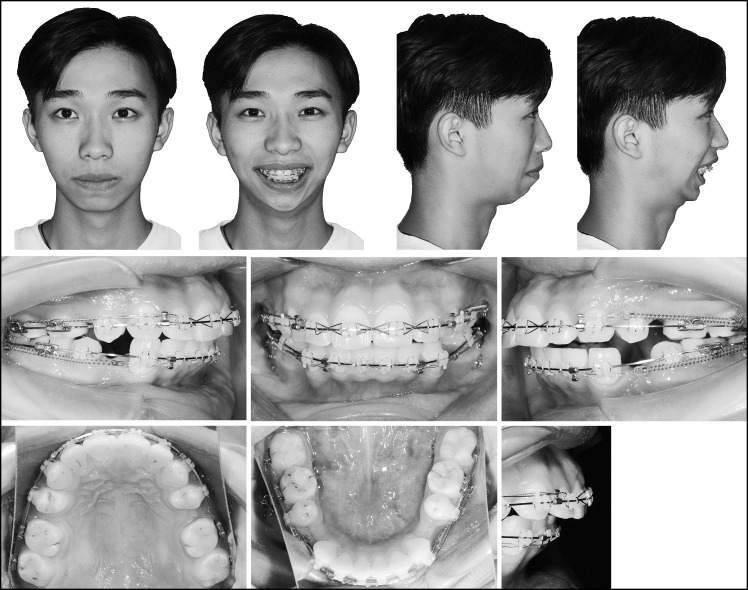
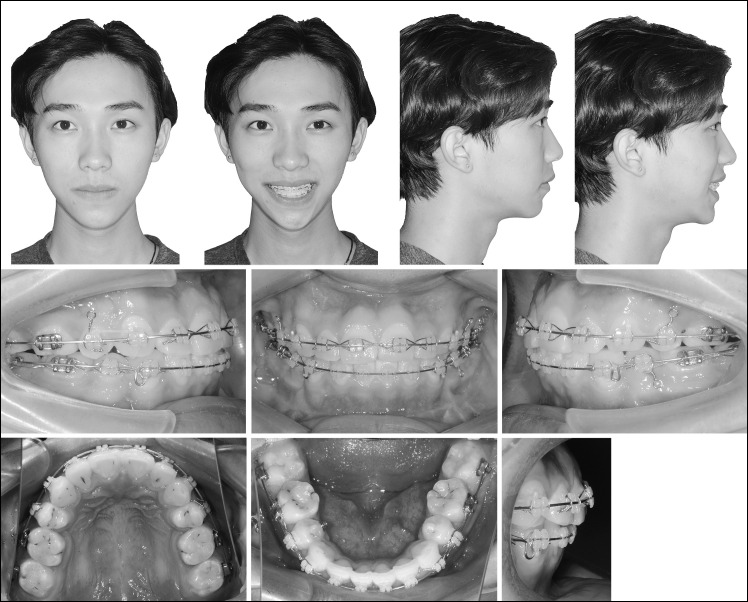
Figure 12.
Facial and intraoral photographs: postsurgical orthodontic correction.
Treatment Results
The posttreatment records revealed significant improvements in the patient's soft-tissue profile and occlusion. Intraorally, acceptable overjet and overbite and an Angle Class I molar relationship were all achieved. The profile was more harmonious, with lip competence and a better chin-to-lip contour. The maxillary incisor exposure during smiling was considered to be within the normal range, and the maxillary dental midline was coincident with the facial midline (Figures 13 and 14). Skeletally, the superimposed tracing showed advancement of the mandible with an increased SNB and decreased ANB. The panoramic radiograph showed good overall root parallelism without evidence of root resorption (Figures 15 and 16; Table 2). The CR-MI discrepancy was eliminated, and no TMJ symptoms were observed throughout active orthodontic treatment. Considerable bone remodeling and cortical continuity was observed on the left condyle, and the right condyle shape was maintained without any significant change (Figure 17).
Figure 13.
Posttreatment facial and intraoral photographs.
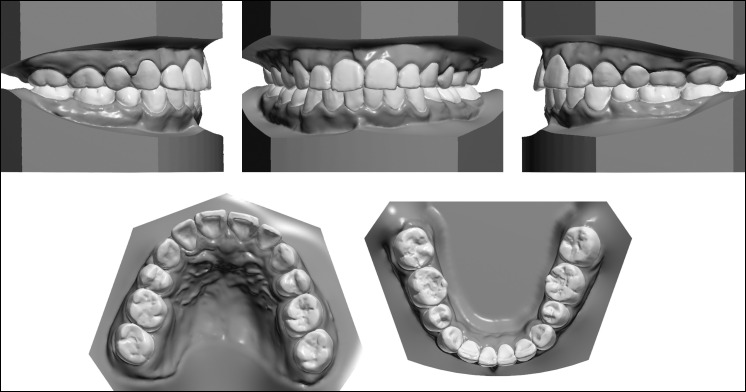
Figure 14.
Posttreatment dental casts.
Figure 15.
Posttreatment lateral radiograph, lateral radiograph tracing, and panoramic radiograph.
Figure 16.
Superimposition of pretreatment (in CR) and posttreatment lateral radiographs.
Table 2.
Cephalometric Analysis
| Measurement |
Norm |
Pretreatment (in CR) |
Posttreatment |
| SNA, ° | 81.7 | 84.9 | 83.9 |
| SNB, ° | 78.9 | 73.1 | 78.5 |
| ANB, ° | 2.8 | 11.8 | 5.4 |
| SN-MP, ° | 32.9 | 37.1 | 39.9 |
| U1-SN, ° | 103.8 | 107.2 | 101.2 |
| L1-MP, ° | 95.4 | 123.1 | 104.2 |
| U1-L1, ° | 123.2 | 92.6 | 114.7 |
| U1-NA, mm | 4.1 | 6.2 | 3.1 |
| U1-NA, ° | 21.5 | 22.3 | 18.4 |
| L1-NB, mm | 5.7 | 16.7 | 8.2 |
| L1-NB, ° | 28.1 | 53.3 | 41.5 |
| LAFH/TAFH | 55.0 | 53.8 | 53.9 |
Figure 17.
Posttreatment bilateral TMJ radiograph.
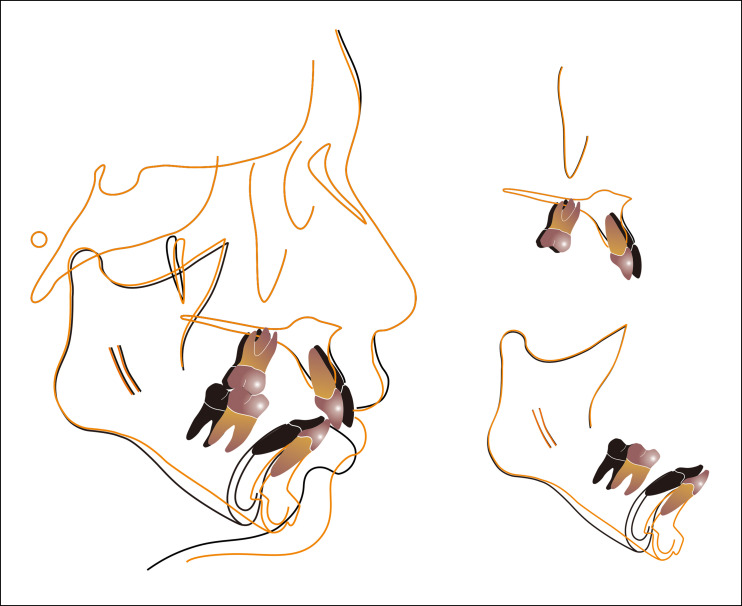
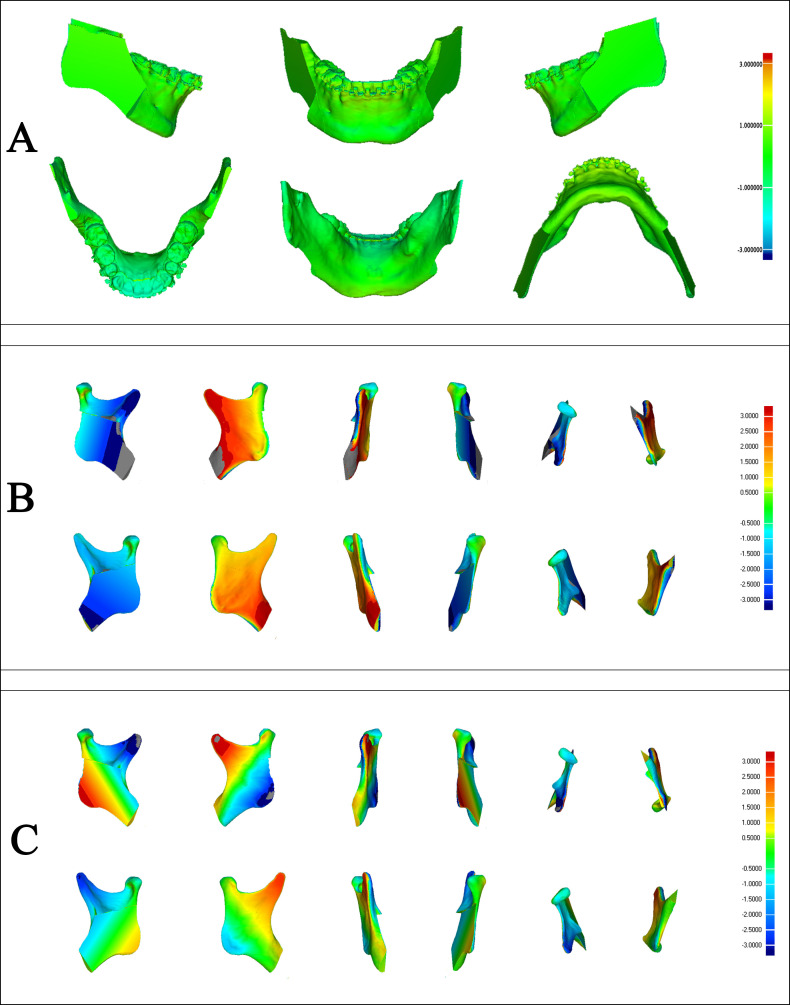
The surface deviation between the simulated and postoperative distal segments are shown on the colored map (Figure 18A). To compare the deviations with a clinically acceptable error, the absolute values of the deviation were compared with 1 mm in translation or 1° in rotation. As the colored map shows, the mean (SD) displacement was 0.016 (0.491) mm, which indicated an acceptable and accurate clinical reproduction of the virtually planned distal segment.
Figure 18.
(A) Deviation of distal segment between simulation and postsurgery. (B) Deviation of the condyle and the proximal segment between presurgery and postsurgery. (C) Deviation of the condyle and the proximal segment between simulation and postsurgery.
Spatial movements of the condyle were measured with a 3D vector using a reversed routine described previously (Figure 18B,C).11 The values of ML, AP, and SI (preoperative to postoperative and from simulation to postoperative) were less than 1 mm, and the values of P (simulation to postoperative) were less than 1°, which suggests that the condyle and proximal segment were well controlled (Table 3). The postoperative positions of the screws were compared with the planned positions, and they were all accurately located. After 1 year of retention, the corrected occlusion and natural smile were well maintained (Figure 19).
Table 3.
Spatial Movements of the Condyle and the Proximal Segmenta
| Measurement |
Preoperative to Postoperative |
Simulated to Postoperative |
||
| Left Condyle |
Right Condyle |
Left Condyle |
Right Condyle |
|
| ML, mm | −0.33 | −0.58 | −0.33 | −0.58 |
| AP, mm | −0.08 | 0.15 | −0.08 | 0.15 |
| SI, mm | −0.90 | −0.61 | −0.90 | −0.61 |
| P, ° | 1.88 | 1.68 | −0.61 | −0.75 |
| R, ° | −0.68 | −1.25 | 4.02 | 1.91 |
| Y, ° | 5.2 | 1.41 | 6.34 | 3.05 |
AP, anterior-posterior translation; ML, Medial-lateral translation; P, pitch; R, roll; SI, superior-inferior translation; Y, yaw. The reference landmarks for translation (ML, AP, SI) and orientation (P, R, Y) are centers of both condyles. For ML, “<0” indicates the lateral direction. For AP, “>0” indicates the anterior direction, “<0” indicates the posterior direction. For SI, “<0” indicates the inferior direction. For P, “>0” indicates upward rotation, and “<0” indicates downward rotation around the transverse axis. For R, “>0” indicates that the lateral condyle rotated upward, and “<0” indicates that the medial condyle rotated upward around the sagittal axis. For Y, “>0” indicates that the anterior condyle turned outward around the vertical axis.
Figure 19.
Facial and intraoral photographs: 1 year after treatment.
DISCUSSION
ICR is an uncommon, aggressive, degenerative disease of the TMJ in normal orthodontic practice. Treatment of orthodontic patients with ICR is challenging for clinicians because of the constantly changing occlusion caused by an unstable condylar position.12 This patient showed an unstable dual bite, which indicated a CR-MI discrepancy, and his occlusion was not reliable for making a definitive diagnosis on the first visit. The elimination of occlusal interferences and achievement of an occlusion with no shift between CR and MI should be the primary goals of orthodontic treatment.13
During the active phase of ICR, the TMJs are vulnerable to biomechanical interactions; therefore, irreversible occlusal treatment, such as orthodontic treatment, should be avoided.8 To find a stable mandibular position and observe changes in condylar resorption, treatment was postponed. After 6 months, a CBCT of the bilateral TMJs indicated cortical continuity and the appearance of an osteophyte on the anterior aspect of the condyle, which was thought to be a radiographically stable stage of ICR.8 Because a stable mandibular position was acquired and no TMD-related symptoms were observed, the orthodontic treatment was then initiated.
Occlusal splints are suggested in ICR cases to stabilize the condylar position before surgery and when there is pain or dysfunction in the joint.4 However, this patient had no such complaints at the initial clinical examination and did not show any TMD-related symptoms throughout active orthodontic treatment. Considering his adequate muscle relaxation and stable CR verified by load testing before bonding and before surgery, he did not receive any splint treatment.
Most severe Class II patients would benefit from mandibular advancement surgery to improve their facial profile. However, ICR is an irreversible complication and a factor in the development of late skeletal relapse after surgery.14 For example, Scheerlink et al.15 showed that surgical mandibular advancement of 5–10 mm can lead to 10% of patients developing significant condylar resorption.
The etiology of ICR is still unclear. Current theories for explaining the onset of ICR include a combination of chemical transduction and mechano-transduction processes.8 The basic concept is that mandibular advancement causes a sudden repositioning of the condyle in the fossa, which increases the mechanical load in the joint.1,4 Without reestablishing the preoperative condylar position after SSRO, the remodeling capacity of the TMJ in some patients is exceeded by the functional demands of these sudden changes, and the condyles will resorb.2
Because immediate postsurgical relapse has also been mainly attributed to improper seating of the condyles, various authors stressed avoiding condylar displacement to prevent relapse and complications.16,17 To ensure highly accurate planned condylar position and bone movements, the CAD/CAM prebent titanium plate approach was designed. During orthognathic surgery, the condyle position can be altered by various factors, such as the surgeon's experience, bony segment interference, and positioning of the proximal and distal segments.18 In the course of the preoperative preparation, bony interferences by mediolateral translation and yaw of the distal segment was avoided with appropriate rolling and lateral translation of the proximal segments. In the operation, experience-based maneuvers were simplified, and guiding templates and CAD/CAM prebent plates ensured the planned postoperative position of the proximal and distal segments. All of these measures provided assurance for the correct position of the condyle. Objective evaluation and 1-year follow-up suggested that the proposed guide had allowed for accurate repositioning of the distal segment and that the proximal segment (condyle) was well positioned.
With the prerequisite of clinical effectiveness assured, simple preparation and a short duration of operation would be beneficial for clinical use. When compared with the relative CAD/CAM guides, this guide simplified the fabrication procedures of transferring screw holes from titanium plates to guiding plates.6 In addition, the bulk of the guide was minimized, split into parts to simplify the operation, and eliminated the procedure of deforming the titanium plates to fit the bone.5 This may not decrease the duration of the operation for an experienced surgeon, but better familiarity using surgical simulation does help surgeons to handle a complicated operation.
Since the mandible was repositioned to its physiologic position, the newly acquired occlusion enabled stability of the mandibular position at the end of treatment, which would contribute to long-term stability and retention of the occlusion. One year of retention showed a stable outcome for both occlusion and the profile. However, skeletal relapse after mandibular advancement has been a major issue because of stretching of suprahyoid muscles and adverse effects on the TMJ. In a case with previous condylar resorption, the increased joint loading may lead to PCR.14 It needs to be noted that although most cases of PCR are expected to initiate during the first year after surgery, late PCR is possible after the first year.19 Furthermore, in view of the significant advancement of the mandibular body more than 7 mm, the risk in the condyle may not be excluded because the movement was made against soft-tissue surroundings on the labial side.15 Compared with low-angle patients, high-angle patients show a more continuous relapse pattern occurring 1 to 3 years in the follow-up period.20 Based on the above-mentioned factors, long-term follow-up of this hyperdivergent skeletal Class II patient is needed.
CONCLUSIONS
Because the ICR often causes occlusal and skeletal changes, precise diagnosis and accurate implementation of the surgical plan is essential. In this case report, the treatment process of a skeletal Class II deficiency associated with ICR was demonstrated.
A 3D simulation of the surgical process and a prebent titanium plate guide were applied in combination to resolve esthetic and functional concerns.
ACKNOWLEDGMENT
The guided device is protected by a license of invention patent (No. 201510204862.0) and patent for utility models (No. 201520260791.1) in PRC.
REFERENCES
- 1. .Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 2. .Handelman CS, Greene CS. Progressive/idiopathic condylar resorption: an orthodontic perspective. Semin Orthod. 2013;19:55–70. [Google Scholar]
- 3. .Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116:667–677. doi: 10.1016/s0889-5406(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 4. .Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion-idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996;110:117–127. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- 5. .Abdel-Moniem Barakat A, Abou-ElFetouh A, Hakam MM, El-Hawary H, Abdel-Ghany KM. Clinical and radiographic evaluation of a computer-generated guiding device in bilateral sagittal split osteotomies. J Craniomaxillofac Surg. 2014;42:e195–e203. doi: 10.1016/j.jcms.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 6. .Bai S, Shang H, Liu Y, Zhao J, Zhao Y. Computer-aided design and computer-aided manufacturing locating guides accompanied with prebent titanium plates in orthognathic surgery. J Oral Maxillofac Surg. 2012;70:2419–2426. doi: 10.1016/j.joms.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 7. .Dawson PE. Functional Occlusion From TMJ to Smile Design. St Louis, Mo: Mosby; 2006. [Google Scholar]
- 8. .Hatcher DC. Progressive condylar resorption: pathologic processes and imaging considerations. Semin Orthod. 2013;19:97–105. [Google Scholar]
- 9. .Guo J, Gong H, Tian W, Tang W, Bai D. Alteration of gingival exposure and its aesthetic effect. J Craniofac Surg. 2011;22:909–913. doi: 10.1097/SCS.0b013e31820f7f7a. [DOI] [PubMed] [Google Scholar]
- 10. .Vig RG, Brundo GC. The kinetics of anterior tooth display. J Prosthet Dent. 1978;39:502–504. doi: 10.1016/s0022-3913(78)80179-6. [DOI] [PubMed] [Google Scholar]
- 11. .Xue C, Tian Y, Wang L, Yang X, Luo E, Bai D. Surgical guide and CAD/CAM prebent titanium plate for sagittal split ramus osteotomy in the correction of mandibular prognathism. Br J Oral Maxillofac Surg. 2018;56:586–593. doi: 10.1016/j.bjoms.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 12. .Lee GH, Park JH, Lee SM, Moon DN. Orthodontic treatment protocols for patients with idiopathic condylar resorption. J Clin Pediatr Dent. 2019;43:292–303. doi: 10.17796/1053-4625-43.4.12. [DOI] [PubMed] [Google Scholar]
- 13. .Roth RH. Functional occlusion for the orthodontist. J Clin Orthod. 1981;15:32–40. 44–51. [PubMed] [Google Scholar]
- 14. .Kobayashi T, Izumi N, Kojima T, Sakagami N, Saito I, Saito C. Progressive condylar resorption after mandibular advancement. Br J Oral Maxillofac Surg. 2012;50:176–180. doi: 10.1016/j.bjoms.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 15. .Scheerlinck JP, Stoelinga PJ, Blijdorp PA, Brouns JJ, Nijs ML. Sagittal split advancement osteotomies stabilized with miniplates: a 2-5-year follow-up. Int J Oral Maxillofac Surg. 1994;23:127–131. doi: 10.1016/s0901-5027(05)80285-1. [DOI] [PubMed] [Google Scholar]
- 16. .Epker BN, Wylie GA. Control of the condylar-proximal mandibular segments after sagittal split osteotomies to advance the mandible. Oral Surg Oral Med Oral Pathol. 1986;62:613–617. doi: 10.1016/0030-4220(86)90251-3. [DOI] [PubMed] [Google Scholar]
- 17. .Lake SL, McNeill RW, Little RM, West RA. Surgical mandibular advancement: a cephalometric analysis of treatment response. Am J Orthod. 1981;80:376–394. doi: 10.1016/0002-9416(81)90173-1. [DOI] [PubMed] [Google Scholar]
- 18. .Kim HM, Baek SH, Kim TY, Choi JY. Evaluation of three-dimensional position change of the condylar head after orthognathic surgery using computer-aided design/computer-aided manufacturing-made condyle positioning jig. J Craniofac Surg. 2014;25:2002–2007. doi: 10.1097/SCS.0b013e3182a246f1. [DOI] [PubMed] [Google Scholar]
- 19. .Hoppenreijs TJM, Maal T, Xi T. Evaluation of condylar resorption before and after orthognathic surgery. Semin Orthod. 2013;19:106–115. [Google Scholar]
- 20. .Mobarak KA, Espeland L, Krogstad O, Lyberg T. Mandibular advancement surgery in high-angle and low-angle class II patients: different long-term skeletal responses. Am J Orthod Dentofacial Orthop. 2001;119:368–381. doi: 10.1067/mod.2001.110983. [DOI] [PubMed] [Google Scholar]