Abstract
We conducted a qualitative review (n = 15 manuscripts) and meta-analysis (n = 9 manuscripts) of the extant literature to evaluate the prevalence and morbidity of subthreshold Attention Deficit Hyperactivity Disorder (ADHD). Our qualitative review showed that a sizable minority (mean: 17.7%) of clinically referred and non-referred children met a priori definitions of subthreshold ADHD. Those affected exhibited significantly higher rates of family dysfunction, cognitive impairment, executive dysfunction, interpersonal and school deficits, temperament problems, psychiatric comorbidity, and juvenile delinquency compared to children with no ADHD symptoms. These deficits were highly consistent with those observed in children with full threshold ADHD. These findings indicate that children with subthreshold ADHD symptoms are at significantly greater risk for negative outcomes in a wide range of non-overlapping functional domains worthy of further clinical and scientific consideration.
Keywords: ADHD, diagnosis, diagnostic criteria, subthreshold
1. Introduction
Attention Deficit Hyperactivity Disorder (ADHD) symptoms are likely to emerge over time as cognitive and educational demands become more prominent. This developmental trajectory predicts that some children with impairing ADHD symptoms may fail to meet full diagnostic threshold for the disorder, hence referred to as subsyndromal. Presently, little is known about subsyndromal manifestations of ADHD.
Previous literature reflects ADHD as a continuously distributed quantitative trait (Larsson et al., 2012). Like many other mental health disorders, ADHD is assessed through binary diagnostics, therefore it’s measures are biased towards high, symptomatic extremes (Greven et al., 2016). This is problematic, as many researchers have ignored meaningful variation in the lower range of scores, lumping those with low extreme ADHD scores with control groups. Researchers such as Larsson et al. (2012) have acknowledged the low extreme ADHD groups as clinically significant, characterizing both low and high extreme ADHD groups with the same etiologic factors, including inattention, hyperactivity, and impulsivity.
In a prospective study conducted by Lecendreux et al. (2015), subsyndromal ADHD symptoms in childhood were an indicator of subsequent full-threshold ADHD in adolescence. Similarly, Faraone and Biederman (2016) argued that in some childhood cases, the onset of symptoms and impairment could separate due to intellectual ability and supportive environments.
Additionally, as argued by Faraone and Biederman (2016), a multifactorial etiology of ADHD would predict a wide variability in initial symptoms and impairments contingent on the accumulation of environmental and genetic risk factors. Those with lower levels of risk will take longer to accumulate sufficient risk factors and longer to develop symptom sand impairment than those with higher levels of such risk factors (Chang et al., 2013). Because these effects are multifactorial, there is no clean separation of etiologic risk factors in individuals below or above symptomatic thresholds (Faraone and Biederman, 2016).
If subthreshold ADHD symptoms are associated with increased negative outcomes, then clinicians may be prompted to consider suitable interventions for such children. Early interventions for subthreshold symptoms of ADHD can help mitigate the progression to a full symptomatic state and obviate the well documented compromised outcomes associated with ADHD (Faraone et al., 2015). Notably, ADHD symptoms may waver around the diagnostic threshold, both increasing and decreasing in severity over time. Some children may never progress to the full clinical presentation, but they should still receive intervention and treatment. Previous research has supported subthreshold symptoms as clinically significant (Biederman et al., 2018): however, more research is needed to understand its impact on global impairment. This knowledge can also improve public health by catalyzing the development of methods to detect subthreshold manifestations of ADHD in schools and community settings.
The main aim of the present study was to evaluate the body of knowledge on the prevalence, morbidity, and dysfunction associated with subthreshold ADHD. To achieve these goals, we conducted a systematic qualitative literature review and meta-analysis of the extant literature on children with subthreshold ADHD.
2. Methods
2.1. Literature review
We performed a systematic literature search through PubMed and PsycINFO utilizing the following search algorithm: (sub threshold or subthreshold or subsyndromal) AND (ADHD or attention deficit hyperactivity disorder or ADD or attention deficit disorder or hyperkinetic syndrome or minimal brain dysfunction) AND (child or children or youth or adolescent or teen or pediatric). Reference lists of retrieved papers were further screened, and papers that possibly met inclusion criteria were retrieved and assessed for inclusion.
2.1.1. Selection criteria
We included original studies that evaluated subthreshold ADHD symptoms. We implemented the following inclusion criteria: (1) original research, (2) includes clear definition of subthreshold ADHD that is mutually exclusive from full threshold ADHD, (3) documents rates of subthreshold ADHD and associated levels of impairment, (4) limits the sample to youth with a mean age ≤ 18, and (5) implements either a cross-sectional or longitudinal design using clinical or epidemiological samples. The following exclusion criteria were also applied: (1) includes cases with a previous full threshold ADHD diagnosis who no longer met full diagnostic criteria, (2) sample size for each of the groups is fewer than 10 children, (3) focus of the study is on other psychiatric, medical or neurological disorders, not specifically ADHD, (4) study methodology is unclear, or (5) the article was not available in English. The senior author (JB), the lead author (AK), and the second author (CK) screened the articles for relevance by examining the abstracts to identify relevant articles in full text and assess their eligibility.
2.1.2. Data extraction
The following variables were extracted: study sample size, proband age range, subthreshold ADHD definition, prevalence rate of subthreshold ADHD, and characteristics that differentiated subjects with symptoms of subthreshold ADHD from those with full syndrome ADHD or those unaffected by ADHD symptomatology.
2.2. Meta-analysis
Means and standard deviations for study outcomes assessing morbidity were extracted when provided and odds ratios were calculated from available data. We meta-analyzed the Standardized Mean Difference (SMD) and Odds Ratios (OR) to assess the difference between subthreshold ADHD and controls, and SMD and risk ratios (RR) to assess the difference between subthreshold ADHD and full threshold ADHD. We used the I2 index to assess the percentage of total variation attributed to heterogeneity. A significant I2 indicates that the degree of heterogeneity is greater than what would be expected by chance. Values range from 0 to 100, with greater percentages indicating greater heterogeneity. Analyses were performed using Stata® (SAS Institute, Cary, N.C.) at the 0.05 alpha level.
3. Results
3.1. Included articles
Figure 1 outlines our process for screening and identifying eligible articles using the algorithm described above. From the database searches, a total of 259 papers were identified and screened by three of the authors (JB, AK, and CK). Two additional papers were added after cross-referencing. After further review, and the removal of 96 duplicates, 150 of the 165 articles were excluded (see Figure 1 for reasons of exclusion).
Figure 1.
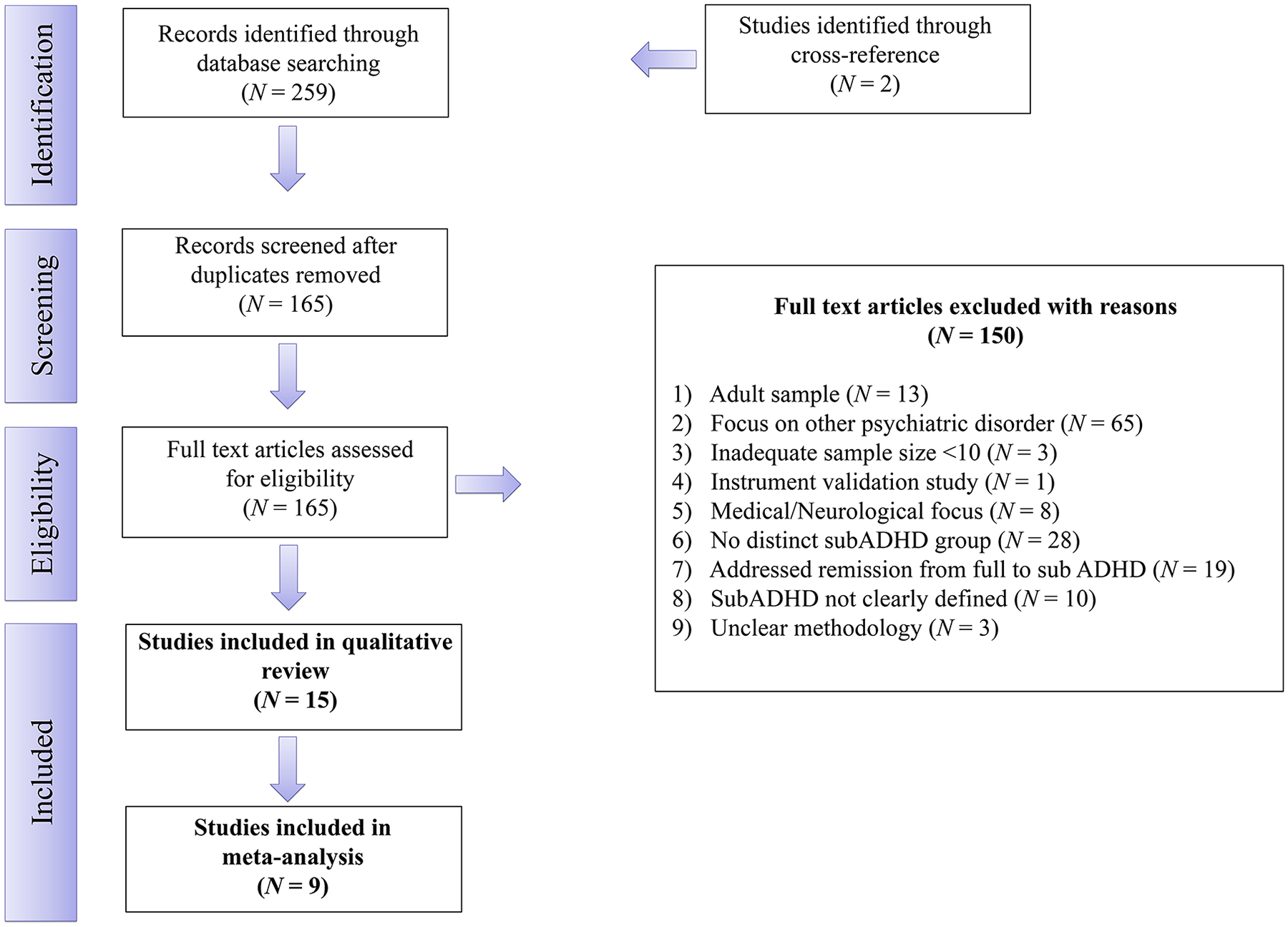
Flow Diagram of Study Selection Process, as Outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement
Fifteen articles met all our inclusion and exclusion criteria and thus were included in the systematic qualitative review. In the meta-analysis, we excluded Kim et al. (2009) because of overlapping data with Cho et al. (2009), and because they assessed too few outcome variables. Similarly, we excluded Shankman et al. (2009) because of overlapping data with Lewinsohn et al. (2004), and because they reported too few outcome variables. Malmberg et al. (2011), DeBono et al. (2012), Larsson et al. (2012), and Roberts et al. (2015) were excluded from the meta-analysis due to one of the following reasons: no control group was included, only odds ratios were reported, or very minimal data on subthreshold ADHD was reported overall. As such, nine of the 15 studies had adequate information and were used to conduct a meta-analysis.
3.2. Extracted study variables
Table 1 gives the characteristics of each eligible study: definition of subthreshold ADHD and DSM criteria used, number of subjects, age range, study duration (for longitudinal studies), control group type, rate of subthreshold ADHD, and main findings outlining characteristics that differentiated subjects with subthreshold ADHD from those unaffected by ADHD symptomatology.
Table 1.
Summary of Studies and Extracted Study Variables
| First author, Year | SubADHD Definition | Criteria | N = | Mean Age | Control? Y/N |
Study Length Period | Prevalence Rate of SubADHD | Main Findings and Comments |
|---|---|---|---|---|---|---|---|---|
| Epidemiologic / Cross-Sectional | ||||||||
| Scahill et al. 1999 | Score of 13–18 on ADHD module of DISC-R | DSM-III-R | N = 449 | 9.2 | Y | N/A | 22% (n = 100/449) of subjects met criteria for subADHD | Male sex and family dysfunction were significantly associated with subADHD vs. conrols. SubADHD subjects were similarly likely to have a comorbid disorder as the full ADHD group and both differed from controls. SubADHD and fullADHD had greater cognitive impairment than controls, and the full ADHD group was the most severe. Full ADHD group had significantly higher rates of comorbid externalizing disorders (43%) compared to subADHD (16%). |
| Lewinsohn et al., 2004 | ≥5 total symptoms | DSM-III-R | N = 1704 | 16.6 | Y | N/A | 6% (n=102/1704) of subjects met subADHD criteria | Children with subADHD and full ADHD were more likely to be male vs controls. SubADHD was highly comorbid with other subthreshold disorders, specifically subthreshold MDD, bipolar, eating disorder, anxiety, alcohol and substance abuse/dependence, and conduct. SubADHD was also highly comorbid with the following full-scale disorders: MDD, alcohol abuse/dependence, and conduct. |
| Cho et al., 2009 | ≥ 3 ≤ 5 inattentive and/or hyperactive/impulsive symptoms | DSM-IV | N = 1651 | 9 | Y | N/A | 9% (n=148/1651) of subjects met subADHD criteria | For temperament profiles, subADHD and full ADHD were associated with significantly higher rates of novelty seeking and lower rates of persistence and self-directedness vs. controls. Children with subADHD were at increased risk for externalizing disorders and impaired scores in most individual and aggregate CBCL scales vs. controls, but the full ADHD group was most impaired. SubADHD subjects had 5x greater risk of having externalizing comorbid disorders (Conduct and ODD) vs. controls. The rate of externalizing and internalizing disorders was significantly lower for subADHD group compared to full ADHD. Both subADHD and full ADHD subjects had significantly lower SES vs. controls. The full ADHD group had higher male preponderance than the subADHD group. |
| Kim et al., 2009 | ≥ 3 ≤ 5 inattentive and/or hyperactive/impulsive symptoms | DSM-IV | N = 2673 | 10.7 | Y | N/A | 9% (n=231/2673) of subjects met criteria for subADHD | SubADHD subjects had significantly elevated rates of comorbid anxiety, mood, ODD, conduct, tic disorders, and enuresis vs. controls. SubADHD group had similarly high rates of psychiatric comorbidity as full ADHD group, except for anxiety. Having a non-biological primary caregiver, paternal job loss, and parental marital discord were signiciantly associated with subADHD. Male sex and maternal stress during pregnancy were the main predictors of subADHD vs. controls. Maternal stress, depression and alcohol use during pregnancy were all significantly related to full ADHD. Divorce and changes in caregivers were significantly more common in full ADHD than in subADHD. Subjects with subADHD were more likely to have a higher SES compared to full ADHD subjects. Boys were 4 times more likely to have full ADHD and 1.2 times more likely to have subADHD. |
| Malmberg et al., 2012 | Symptoms slightly below threshold based on K-SADS PL (symptoms marked as either ‘possible’ or ‘certain’) | DSM-IV-TR | N = 312 | 16 | N | N/A | 47% (n=146/312) of subjects met subADHD criteria | Twin study (156 twin pairs) analyzing subADHD combined type. SubADHD Combined was identified in close to 10% of the sample (n=29/312). SubADHD combined was associated with symptoms of depression, mania, psychosis, anxiety, eating problems, and trauma. In boys subADHD was associated with depression and PTSD. |
| Larrson et al., 2012 | 6–7.5 points on the Autism-Tics, ADHD, and other Comorbidities Inventory (A-TAC) | DSM-IV | N = 16,366 | 9–12 | N | N/A | 10% (n=1590/16366) of subjects met subADHD criteria | Findings suggest a strong genetic link between the extreme and the subthreshold range of DSM-IV ADHD symptoms. Study suggests that ADHD is an extreme of a continuous trait. |
| Hong et al., 2014 | ≥ 3 ≤ 5 inattentive and/or hyperactive/impulsive symptoms | DSM-IV | N = 912 | 9 | Y | N/A | 12% (n= 106/912) of subjects met subADHD criteria | SubADHD and full ADHD were both significantly associated with higher ADHD-RS, and more impaired CBCL and Learning Disability Evaluation Scale (LDES) scores vs. controls, although the full ADHD group was significantly impaired vs. both controls and subADHD. Full and SubADHD showed significantly more impaired Stroop scores vs. controls. Full ADHD cases had significantly higher rates of a positive family history of ADHD compared to both subADHD and controls. The rates of Full ADHD (5.2%) and subADHD (16.6%) were higher in children with lower family income vs. children with higher family income. |
| Roberts et al., 2015 | 3 inattentive or hyperactive/impulsive symptoms | DSM-IV | N = 4175 | 11–17 | Y | N/A | 13% (n = 537/4174) of subjects met subADHD criteria | Within the sub ADHD group, the percentage of subADHD cases that reported impairment was 7.3%. The full ADHD cases had significantly higher self-reported impairment than subthreshold ADHD cases. No other information was provided. |
| Clinically Referred / Cross-Sectional | ||||||||
| DeBono et al., 2012 | Symptoms below threshold on K-SADS-PL, no demonstrated evidence of symptomatology across settings, or insufficient impairment to warrant diagnosis | DSM-IV | N = 97 | 15.57 | N | N/A | 27.8% (n=27/97) of subjects met subADHD criteria | Both full ADHD and subADHD groups performed in the average range on all written expression measures (spelling, writing fluency, contextual language, and story construction), except for contextual conventions, which was in the low average range for both groups. Processing speed index also fell in the low average range for both groups. No significant differences were found in age, FSIQ (WAIS-III), cognitive processing (WISC-IV, TOWRE, MAND, TROG-2, TLC-EE), and written expression (WJ-III and TOWL-3) between groups. Proportions of learning disabilities did not differ by diagnostic status (18/70 full ADHD and 6/27 subADHD). Parents and teachers rated inattention higher in full ADHD than subADHD (SWAN). Only parents rated hyperactivity/impulsivity higher in full ADHD than subADHD, not teachers (SWAN). No significant group differences were obtained between ADHD subtypes. |
| Biederman et al., 2018 | Age of onset was ≥ 7 years. Had > 5 < 8 ADHD symptoms using DSM-III-R OR ≥ 4 < 6 ADHD inattentive or hyperactive/impulsive symptoms using DSM-IV | DSM-III-R and DSM-IV | N = 2173 | 11 | Y | N/A | 6% (n=140/2173) met subADHD criteria | Almost half of subADHD had an age onset of >7 years old and 73% had insufficient symptoms (<8 symptoms of DSM-III-R and <6 of DSM-IV). Both ADHD groups had significantly higher rates of all disorders vs. controls. SubADHD differed from controls in the mean number of comorbid disorders, rates of mood, anxiety and elimination disorders, and substance use disorders, all CBCL clinical and social functioning scales, more than half of SAICA scales, rates of requiring extra help in school and being placed in a special class, having lower scores on WISC-R subscales (excluding Digit Span) as well as in Freedom from Distractibility. SubADHD and full ADHD subjects had similarly elevated GAF scores vs controls. SubADHD had fewer perinatal complications, better family functioning scores, and were more likely to be female, older, and to come from higher SES families. |
| First author, Year | SubADHD Definition | Criteria | N = | Initial Age – Final Age | Control? Y/N |
Study Length Period | Prevalence Rate of SubADHD | Main Findings and Comments |
| Epidemiologic / Longitudinal | ||||||||
| Kadesjö & Gillberg, 2001 | 5 ≤ 7 of the 14 DSM-III-R symptoms | DSM-III-R | N = 409 | 7 – 11 | Y | 4 years | 10% (n = 42/409) of subjects met subADHD criteria | Children with subthreshold ADHD had much higher rates of comorbid diagnoses, including externalizing, learning, and developmental disorders compared to controls. The rate of school adjustment, learning, and behavior problems at follow-up was very high in both ADHD groups. |
| Shankman et al., 2009 | ≥5 total symptoms | DSM-III-R and DSM-IV | N = 1505 | 16.6 – 30.4 | N | 15 years | 6% (n=86/1505) of subjects met subADHD criteria. | 72% of subADHD subjects had at least one comorbid subthreshold disorder and 36% had a comorbid full syndrome disorder. Although none converted to full ADHD during the 15-year follow-up period, subjects with subADHD diagnosis at baseline were likely to develop alcohol, substance, and conduct disorder at follow up. Males were more likely to have subADHD (64%) than females. |
| Bussing et al., 2010 | ≥ 3 ≤ 5 inattentive and/or hyperactive/impulsive symptoms | DSM-IV | N = 332 | 5 to 11 – 13 to 19 | Y | 8 years | 23% (n=75/332) of youth identified at “high risk for ADHD” met subADHD criteria during childhood | SubADHD was associated with similarly greater risk for grade retention and graduation failure as full ADHD relative to controls. Both full and subADHD groups had lower grades and lower achievement scores on standardized tests of reading and math. Full ADHD and subADHD diagnoses tripled the odds of juvenile justice involvement and the odds of developing ODD, depression and anxiety vs. controls. |
| Fergusson et al., 2010 | ≥1 ADHD symptom met on DSM criteria | DSM-IV | N = 995 | 14 to 16 – 18 to 25 | Y | 11 years | 61% (n=609/995) of subjects met subADHD criteria | In all ADHD cases, clinical subjects had the worst outcomes, those with subclinical symptoms had intermediate outcomes, and controls had the best outcomes. SubADHD subjects were more likely to commit crime (property and violent crime) compared to controls and less likely compared to full ADHD subjects. SubADHD subjects were more likely to develop substance use and mental health issues (major depression, anxiety, antisocial personality disorder, suicide attempts) compared to controls and less likely compared to full ADHD subjects. SubADHD subjects were also more likely to have issues with pregnancy, parenthood, partnership, education, employment, and lower average income compared to controls and less likely compared to full ADHD subjects. |
| Selinus et al., 2016 | 6–7.5 points on the Autism-Tics, ADHD, and other Comorbidities Inventory (A-TAC) | DSM-IV | N = 4635 | 9 or 12 – 15 or 18 | Y | 6 years | Rate of subADHD for 9 yo twins was 4% (102/2640); Rate of subADHD for 12 yo twins was also 4% (81/1987) | In both the full ADHD and subADHD groups for both twin samples, severity of ADHD symptoms was associated with a higher likelihood for all adverse outcomes (school problems, internalizing, antisocial behavior) in both males and females. Females with subADHD had higher rates of internalizing problems (anxiety, depression, psychosomatic symptoms) vs. controls and vs. the full ADHD group. More girls than boys reported internalizing problems (all levels) and risky drug use (screen-intermediate and screen- positive only). More boys reported antisocial behavior at the screen- negative and screen-intermediate levels, but at the screen-positive level, similar proportions of girls and boys displayed antisocial behavior. |
3.3. Meta-analysis
The final meta-analysis dataset compiled from the nine eligible studies consisted of 11,111 participants, 2,173 of which were clinically referred pediatric participants and the rest were non-referred. The breakdown of the participants was: 2,488 with full threshold ADHD, 1,505 with subthreshold ADHD symptoms, and 7,118 controls. The overall rates of full threshold ADHD and subthreshold ADHD were 9.8% and 18.5%, respectively. The overall rate of ADHD (both subthreshold and full threshold cases) was 30.1%. The control groups included children without full or subthreshold ADHD. Seven of the nine studies included children without subthreshold or full threshold ADHD, but with other psychiatric disorders in the control group (Kadesjo and Gillberg, 2001; Cho et al., 2009; Kim et al., 2009; Shankman et al., 2009; Fergusson et al., 2010; Noren Selinus et al., 2016; Biederman et al., 2018). The other two studies included only healthy children with neither full nor subthreshold psychiatric disorders (Scahill et al., 1999; Bussing et al., 2010).
The results of all analyses for subthreshold ADHD versus controls and for subthreshold ADHD versus full threshold ADHD are summarized in Tables 2 and 3, which report tests of heterogeneity and the variation in SMD, OR and RR attributable to heterogeneity (I2).
Table 2.
Summary of results of continuous outcomes showing tests of heterogeneity and the variation in SMD attributable to heterogeneity (I2) for the following subgroups in the meta-analysis: 1) Subthreshold ADHD vs. Controls, and 2) Subthreshold ADHD vs. Full ADHD.
| Subthreshold ADHD vs. Controls | ||||
|---|---|---|---|---|
| Study | Heterogeneity Statistic | Degrees of Freedom | p | I2 |
| Scahill 1999 | 45.2 | 10 | >0.01 | 77.9% |
| Bussing 2010 | 41.3 | 8 | >0.01 | 80.6% |
| Fergusson 2010 | 27.5 | 6 | >0.01 | 78.2% |
| Hong 2014 | 348.7 | 28 | >0.01 | 92.0% |
| Biederman 2018 | 1150.4 | 40 | >0.01 | 96.5% |
| Overall | 2176.6 | 96 | >0.01 | 95.6% |
| Subthreshold ADHD vs. Full ADHD | ||||
| Scahill 1999 | 54.4 | 10 | >0.01 | 81.6% |
| Bussing 2010 | 16.3 | 8 | 0.04 | 51.0% |
| Fergusson 2010 | 45.8 | 6 | >0.01 | 86.9% |
| Hong 2014 | 63.1 | 28 | >0.01 | 55.6% |
| Biederman 2018 | 161.6 | 40 | >0.01 | 80.7% |
| Overall | 160.1 | 96 | >0.01 | 70.0% |
Table 3.
Summary of results for binary outcomes showing tests of heterogeneity and the variation in OR and RR attributable to heterogeneity (I2) for the following subgroups in the meta-analysis: 1) Subthreshold ADHD vs. Controls, and 2) Subthreshold ADHD vs. Full ADHD.
| Subthreshold ADHD vs. Controls | ||||
|---|---|---|---|---|
| Study | Heterogeneity Statistic | Degrees of Freedom | p | I2 |
| Scahill 1999 | 0.0 | 1 | 0.9 | 0.0% |
| Kadesjö 2001 | 5.0 | 6 | 0.5 | 0.0% |
| Lewinsohn 2004 | 9.2 | 15 | 0.9 | 0.0% |
| Bussing 2010 | 85.2 | 19 | <0.01 | 77.7% |
| Fergusson 2010 | 12.3 | 5 | 0.03 | 59.5% |
| Selinus 2016 | 43.6 | 6 | <0.01 | 86.2% |
| Biederman 2018 | 61.1 | 11 | <0.01 | 82.0% |
| Overall | 556.4 | 69 | <0.01 | 87.6% |
| Subthreshold ADHD vs Full ADHD | ||||
| Scahill 1999 | 2.2 | 1 | 0.14 | 53.6% |
| Kadesjö 2001 | 8.9 | 6 | 0.18 | 32.5% |
| Lewinsohn 2004 | 12.6 | 6 | 0.05 | 52.3% |
| Cho 2009* | 7.9 | 12 | 0.80 | 0.0% |
| Bussing 2010 | 61.3 | 19 | <0.01 | 69.0% |
| Fergusson 2010 | 33.7 | 5 | <0.01 | 85.1% |
| Selinus 2016 | 1.8 | 6 | 0.94 | 0.0% |
| Biederman 2018 | 39.5 | 11 | <0.01 | 72.2% |
| Overall | 251.0 | 73 | <0.01 | 70.9% |
Cho 2009 did not report data on controls for the extracted outcome variables and therefore is only included in the Subthreshold ADHD vs. Full ADHD subgroup meta-analysis.
3.3.1. Meta-analysis results for continuous outcomes
For continuous outcomes, the pooled SMD was significant, indicating an increased impairment associated with subthreshold ADHD relative to controls (SMD=0.83, 95% CI=0.72–0.95). Overall heterogeneity was high and significant. Figure 2 displays the forest plot for SMDs with 95% confidence intervals (CI). The pooled SMD was also significant for the full threshold ADHD versus subthreshold ADHD comparison, indicating an increased impairment associated with full threshold ADHD compared to subthreshold ADHD (SMD=0.27, 95% CI=0.34–0.41). Heterogeneity was high and significant. Figure 3 displays the forest plot for SMDs with 95% confidence intervals (CI).
Figure 2.
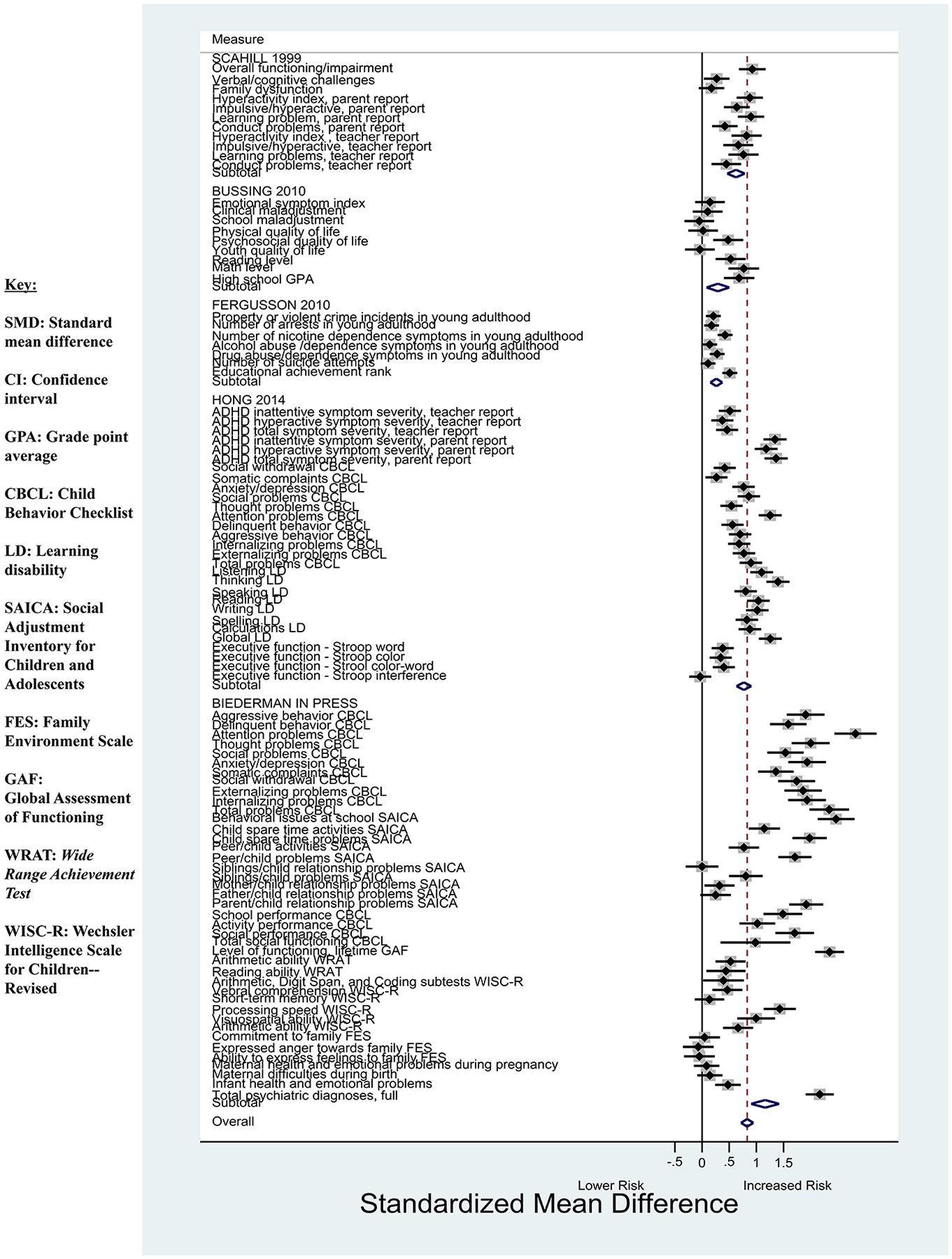
Forest plot showing the SMD and 95% CI for continuous outcome variables between the subthreshold ADHD group and controls.
*The area of each square is proportional to the sample size for that particular variable included in the meta-analysis.
Figure 3.
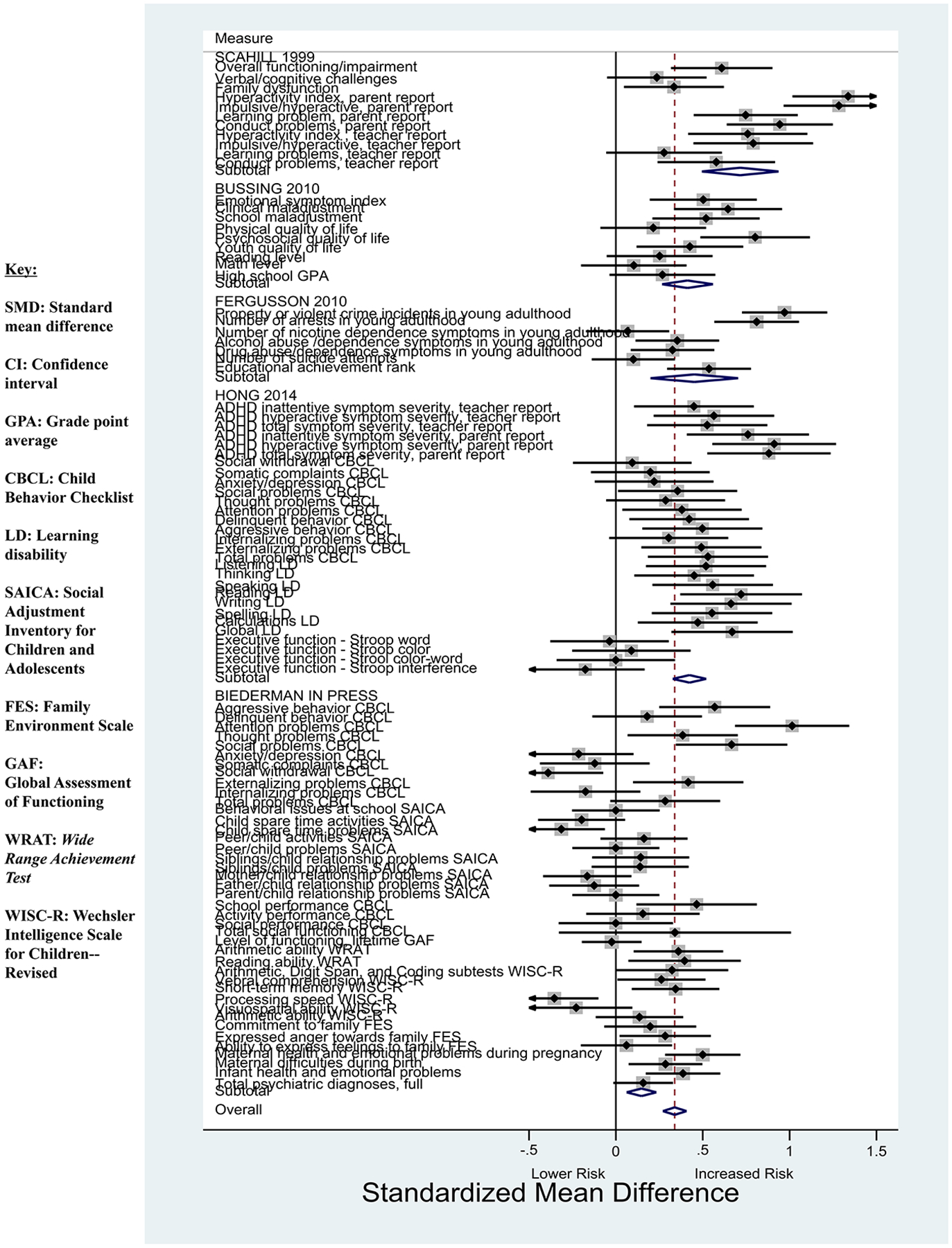
Forest plot showing the SMD and 95% CI for continuous outcome variables between the subthreshold ADHD group and full ADHD.
*The area of each square is proportional to the sample size for that particular variable included in the meta-analysis.
As shown in Figure 2, subthreshold ADHD was associated with a significantly increased risk for several negative continuous outcomes relative to controls including: lower overall functioning and global impairment (Scahill et al., 1999; Biederman et al., 2018); academic, learning, and cognitive challenges (Scahill et al., 1999; Hong et al., 2014; Biederman et al., 2018); conduct problems and behavioral concerns (Scahill et al., 1999; Fergusson et al., 2010; Hong et al., 2014; Biederman et al., 2018); infant health and emotional problems (Biederman et al., 2018); higher scores on the Conner’s Teacher and Parent Questionnaires (CTQ and CPQ) (Conners, 1969; Conners, 1995) on ADHD (Scahill et al., 1999); lower psychosocial quality of life indicated on the Child Health Questionnaire (CHQ) (Landgraf, 1995; Bussing et al., 2010); elevated scores on the ADHD Rating Scale (ADHD-RS) (DuPaul et al., 1998) Parent and Teacher reports (Hong et al., 2014); impaired scores on all Child Behavior Checklist (CBCL) domains (Achenbach, 1991; Hong et al., 2014; Biederman et al., 2018); impaired scores on a majority of the Social Adjustment Inventory for Children and Adolescents (SAICA) domains (Biederman et al., 2018); impaired scores on the Learning Disability Evaluation Scale (McCarney, 1996) domains (Hong et al., 2014); and impaired executive functioning as indicated by various Stroop tasks (Hong et al., 2014). Longitudinal data also showed a significantly increased risk for the following negative outcomes in young adulthood: lower educational achievement, crime and arrests, nicotine dependence, and drug abuse and dependence (Fergusson et al., 2010).
As shown in Figure 3, full threshold ADHD was associated with a significantly increased risk for several negative continuous outcomes relative to subthreshold ADHD including: lower overall functioning and global impairment (Scahill et al., 1999), family dysfunction (Scahill et al., 1999), cognitive impairment (Biederman et al., 2018), conduct problems and behavioral concerns (Scahill et al., 1999; Fergusson et al., 2010; Hong et al., 2014; Biederman et al., 2018), maternal/infant health and emotional problems (Biederman et al., 2018), maternal problems during birth (Biederman et al., 2018), higher scores on the CPQ and CTQ on ADHD and conduct problems (Scahill et al., 1999; Hong et al., 2014), elevated self-reported measures on the Behavioral Assessment System for Children (BASC) (Reynolds and Kamphaus, 2002) emotional index, clinical and school maladjustment (Bussing et al., 2010), lower psychosocial and youth quality of life indicated on the Youth Quality of Life (YQOL) (Edwards et al., 2002) questionnaire and CHQ (Bussing et al., 2010), elevated scores on the ADHD-RS Parent and Teacher reports (Hong et al., 2014), impaired scores on at least a third of CBCL domains (Hong et al., 2014; Biederman et al., 2018), and impaired scores on all LDES domains (Hong et al., 2014). Longitudinal data also showed a significantly increased risk for the following outcomes in young adulthood: lower educational achievement, crime and arrests, and alcohol and drug abuse/dependence (Fergusson et al., 2010). There were fewer negative outcomes that were significant compared to the subthreshold ADHD vs. controls binary analysis. Analyses were more varied in the Biederman et al. (2018) data for the full threshold ADHD versus subthreshold ADHD group comparison than in the subthreshold ADHD versus controls analysis. For example, there was a significantly decreased risk for the following negative outcomes in the full threshold ADHD group compared to the subthreshold ADHD group: social withdrawal (CBCL), child spare time problems (SAICA), and processing speed (WISC-R). Although some variables assessed in the subthreshold group were more impaired than in the full threshold cases most likely due to chance, the overall interpretation of the findings is that subthreshold cases were similarly morbid to the full threshold cases.
3.3.2. Meta-analysis results for binary outcomes
For binary outcomes, the pooled OR was significant, indicating an increased risk for negative outcomes associated with subthreshold ADHD relative to controls (OR=5.71, 95% CI=4.33–7.54). Overall heterogeneity was high and significant. Figure 4 displays the forest plot for ORs with 95% confidence intervals. The pooled risk ratio (RR) was also significant, indicating an increased risk for negative outcomes for full threshold ADHD compared to subthreshold ADHD (RR=1.45, 95% CI=1.31–1.61). Figure 5 displays the forest plot for ORs with 95% confidence intervals. Heterogeneity was high and significant.
Figure 4.
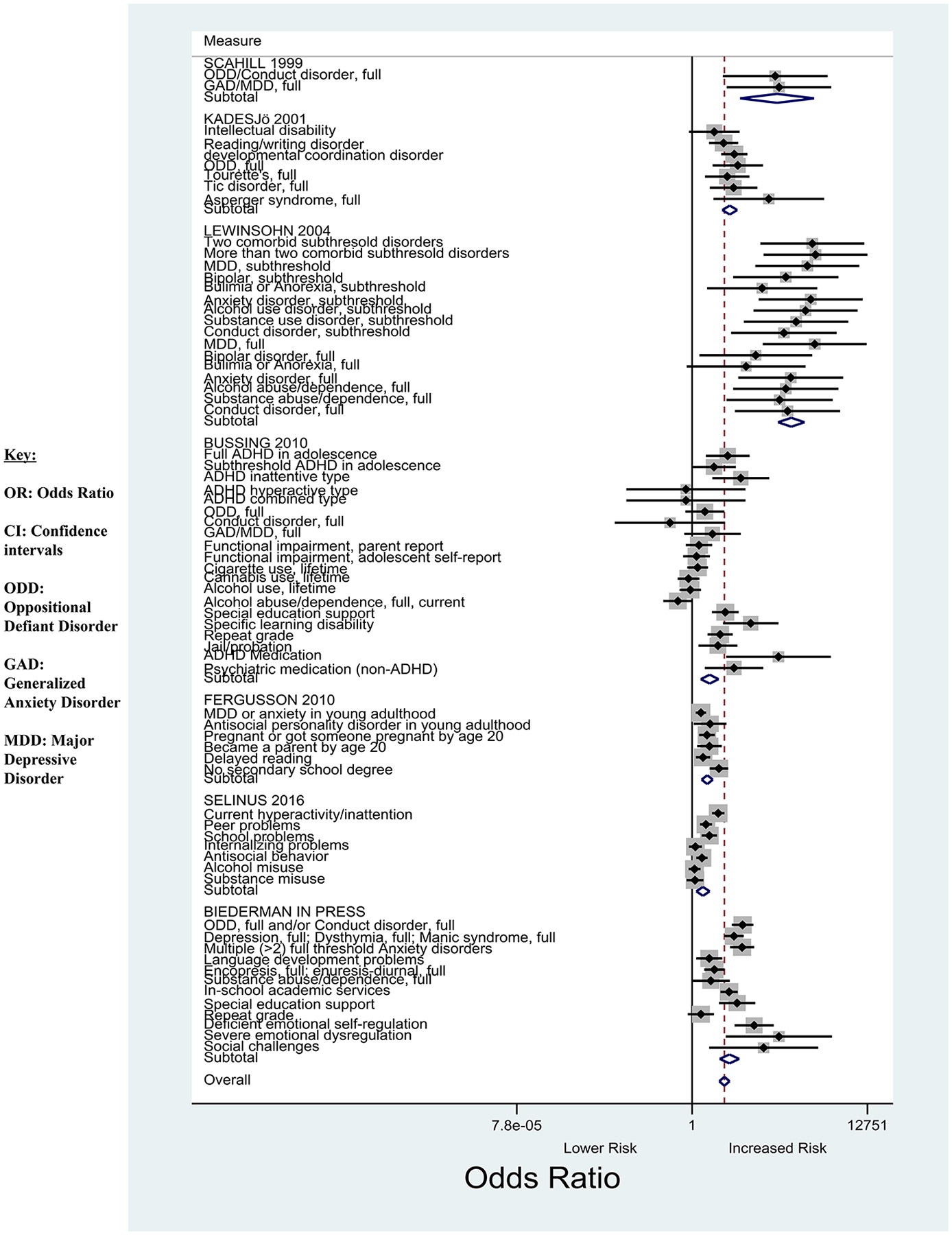
Forest plot showing the OR and 95% CI for binary outcome variables between the subthreshold ADHD group and controls.
*The area of each square is proportional to the sample size for that particular variable included in the meta-analysis.
Figure 5.
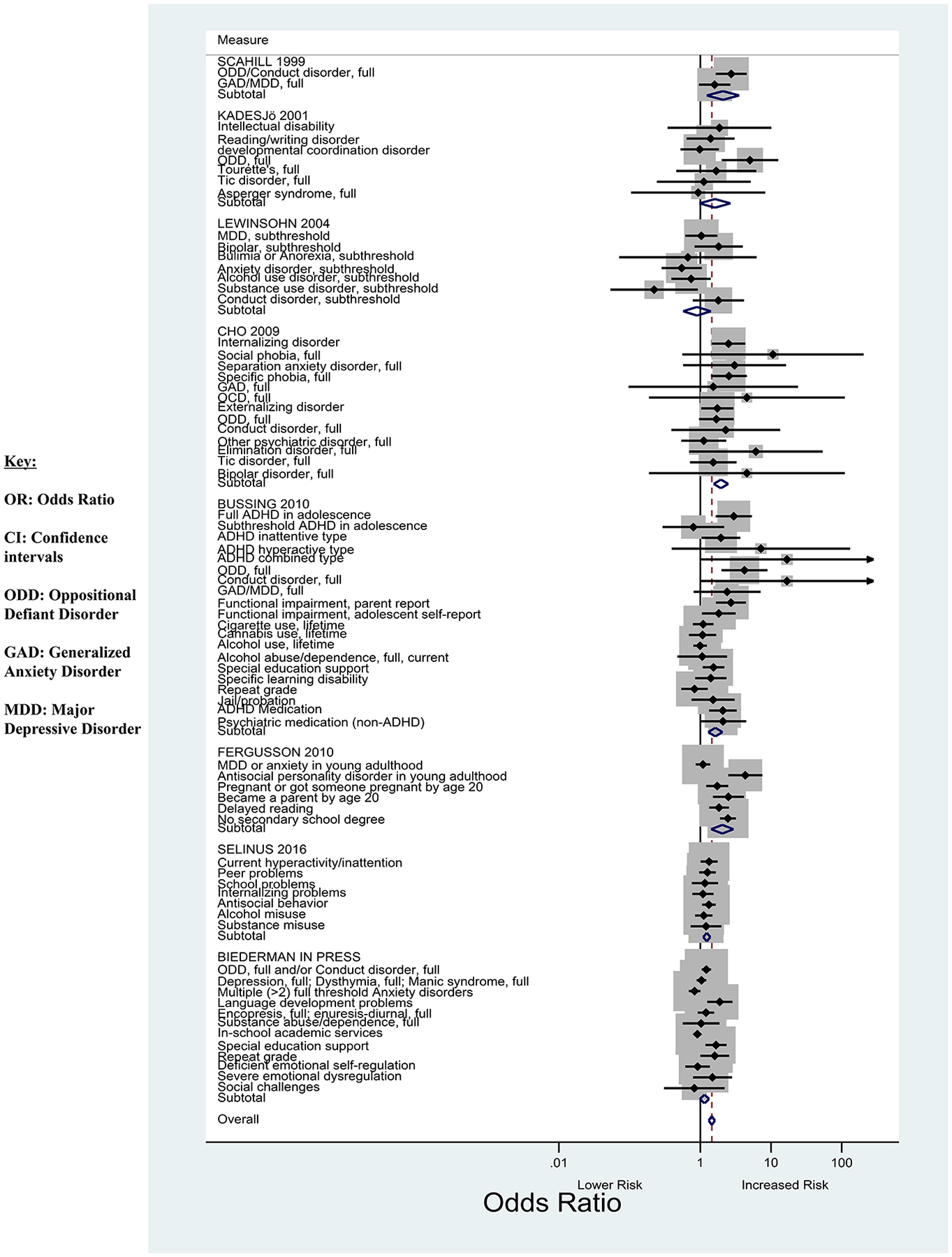
Forest plot showing the OR and 95% CI for binary outcome variables between the subthreshold ADHD and full ADHD group.
*The area of each square is proportional to the sample size for that particular variable included in the meta-analysis.
As shown in Figure 4, subthreshold ADHD was associated with a significantly increased risk for several negative binary outcomes relative to controls including: both full threshold and subthreshold externalizing psychiatric disorders (Scahill et al., 1999; Kadesjo and Gillberg, 2001; Lewinsohn et al., 2004; Biederman et al., 2018) both full threshold and subthreshold internalizing psychiatric disorders (Scahill et al., 1999; Kadesjo and Gillberg, 2001; Lewinsohn et al., 2004; Biederman et al., 2018) intellectual and learning disabilities (Kadesjo and Gillberg, 2001; Bussing et al., 2010; Noren Selinus et al., 2016; Biederman et al., 2018), grade retention (Bussing et al., 2010), and juvenile system involvement (Bussing et al., 2010). Longitudinal data also showed a significantly increased risk for the following outcomes in young adulthood: pregnancy and parenthood by age 20; no secondary degree by young adulthood; and MDD, anxiety, and anti-social personality disorder diagnoses (Fergusson et al., 2010). Of note, Noren Selinus et al. (2016) and Bussing et al. (2010) did not find significantly increased risks for similar outcome variables such as internalizing problems and alcohol/substance abuse and dependence.
As shown in Figure 5, full threshold ADHD was associated with a significantly increased risk for only a small number of negative binary outcomes relative to subthreshold ADHD, including: full threshold ODD and Conduct disorders (Scahill et al., 1999; Kadesjo and Gillberg, 2001; Bussing et al., 2010), poor language development and special education support (Biederman et al., 2018), internalizing psychiatric disorders such as specific phobia (Cho et al., 2009), and parent reports of functional impairment on the Columbia Impairment Scale (CIS) (Bird et al., 1993; Bussing et al., 2010). Longitudinal data also showed a significantly increased risk for the following outcomes in young adulthood: pregnancy and parenthood by age 20, no secondary degree by young adulthood, delayed reading, and anti-social personality disorder diagnosis (Fergusson et al., 2010).
3.4. Qualitative review summary
The mean prevalence of subthreshold ADHD across all 15 studies was 17.7% (range 4.0–61.2%). All but two of the studies included in this review were epidemiologic studies that reported on prevalence rates, and most studies also included outcomes related to the morbidity of subthreshold ADHD. Biederman et al. (2018) and DeBono et al. (2012) analyzed data from clinically-referred youth. The rate of subthreshold ADHD was the lowest in a twin longitudinal study (4.0%) (Noren Selinus et al., 2016), and highest in the study by Fergusson et al. (2010) (61.2%), most likely due to their loose subthreshold inclusion criteria (presence of one or more ADHD symptoms).
3.4.1. Sex effects on rates of ADHD
Five studies reported higher rates of subthreshold ADHD among males than females (Scahill et al., 1999; Lewinsohn et al., 2004; Kim et al., 2009; Shankman et al., 2009; Biederman et al., 2018). Three of the studies reported that both the full threshold ADHD and subthreshold ADHD groups had more males than females, but there was a difference in the sex distributions between the subthreshold ADHD and full threshold ADHD groups; the boy to girl ratio was much larger in the full threshold ADHD group (Cho et al., 2009; Kim et al., 2009; Biederman et al., 2018). Biederman et al. (2018) analyzed data from clinically-referred children and found a significantly larger proportion of females in the subthreshold ADHD compared to the full threshold ADHD group. The rest of the studies did not find sex differences in the rates of subthreshold ADHD.
3.4.2. Social class effects
Three studies reported that children with subthreshold ADHD came from lower social class strata than controls (Cho et al., 2009; Hong et al., 2014; Biederman et al., 2018). Biederman et al. (2018), however, also reported higher social class in the subthreshold ADHD group compared to the full threshold ADHD group. A longitudinal study conducted by Fergusson et al. (2010) found that increasing severity of ADHD in adolescence was directly correlated with lower earned income by mid-twenties. The other studies in the qualitative review failed to find meaningful differences based on social class.
3.4.3. Differences between subthreshold ADHD and controls
Compared to controls, children with subthreshold ADHD notably had higher rates of maternal stress during pregnancy and family dysfunction (Scahill et al., 1999; Kim et al., 2009), cognitive impairment (Hong et al., 2014; Biederman et al., 2018), executive function deficits (Hong et al., 2014), temperament problems (Cho et al., 2009; Biederman et al., 2018), psychiatric comorbidity for both internalizing and externalizing full and subthreshold disorders (Lewinsohn et al., 2004; Cho et al., 2009; Kim et al., 2009; Shankman et al., 2009; Bussing et al., 2010; Fergusson et al., 2010; Malmberg et al., 2011; Noren Selinus et al., 2016; Biederman et al., 2018), greater risk for grade retention and graduation failure (Fergusson et al., 2010; Biederman et al., 2018), school problems including lower grades and lower achievement scores on standardized tests of reading and math (Bussing et al., 2010; Noren Selinus et al., 2016), juvenile justice system involvement (Bussing et al., 2010), and more impaired scores on clinical scales including the SAICA (Biederman et al., 2018) and the CBCL (Cho et al., 2009; Hong et al., 2014; Biederman et al., 2018).
3.4.4. Similarities and differences between subthreshold ADHD and full syndrome ADHD
Most of the reviewed papers (10/15) found that subthreshold and full threshold ADHD groups were significantly more impaired versus controls across several social, interpersonal, emotional, academic, and cognitive domains. The full threshold ADHD group had the most impaired outcomes across studies, but it is notable that in some cases the full threshold and subthreshold ADHD groups did not differ significantly. The full threshold ADHD and subthreshold ADHD subjects from DeBono et al. (2012) performed similarly on cognitive processing and written expression measures. Both groups performed in the low average range for processing speed and contextual conventions. Kim et al. (2009) reported that subthreshold ADHD and full threshold ADHD subjects had similarly elevated rates of comorbid anxiety, ODD, conduct, tic disorders and enuresis that were significantly different from controls. Scahill et al. (1999) also found that subthreshold ADHD and full threshold ADHD groups were similarly likely to have a comorbid psychiatric disorder and that they had similar rates of internalizing disorders (GAD and MDD). When assessing the mean number of comorbid psychiatric disorders, Biederman et al. (2018) also reported that both ADHD groups had similar rates of comorbidity, which were significantly elevated compared to controls. The two ADHD groups also had similar rates of mood, anxiety, elimination, and substance use disorders. In Biederman et al. (2018), both subthreshold ADHD subjects and full threshold ADHD subjects received significantly more extra help in school and were placed more often in special classes compared to controls. Biederman et al. (2018) also found that full threshold ADHD and subthreshold ADHD subjects had greater cognitive impairment than controls. However, subthreshold ADHD subjects had more severe impairment in processing speed and memory (WISC-R Digit Symbol subscale) compared to healthy controls and full threshold ADHD group.
As expected, findings reflected that children who met criteria for full threshold ADHD had the most severe outcomes compared to both the subthreshold ADHD and control groups. DeBono et al. (2012) reported that parents rated the full threshold ADHD group higher in inattention and hyperactivity/impulsivity compared to the subthreshold ADHD group on the Strengths and Weakness of ADHD-symptoms and Normal Behavior Scale (SWAN). In addition to noting similarities between the subthreshold ADHD and full threshold ADHD groups, Scahill et al. (1999) found that the full threshold ADHD group had significantly higher rates of comorbid externalizing disorders (43%) compared to both the subthreshold ADHD group (16%) and controls. Similarly, Cho et al. (2009) found that while both full threshold ADHD and subthreshold ADHD had higher rates of comorbid internalizing and externalizing disorders relative to controls, the rates of comorbid disorders were higher in the full threshold ADHD group compared to the subthreshold group. While Biederman et al. (2018) found that the two ADHD groups had similar rates of several psychiatric disorders, they reported that the full threshold ADHD group had the highest rate of disruptive behaviors and language disorders. Scahill et al. (1999) also found that full threshold ADHD and subthreshold ADHD cases had significantly greater cognitive impairment than controls, with cognitive impairment being the most severe for the full threshold ADHD group. While Cho et al. (2009), Hong et al. (2014) and Biederman et al. (2018) all found that the subthreshold and full threshold ADHD groups had significant impairments across many of the CBCL Clinical and Social Functioning scales, children with full threshold ADHD had the most severe impairment. Hong et al. (2014) also reported that the full threshold ADHD group had the most impaired scores on the ADHD-RS and LDES, and that a positive family history of ADHD was only strongly correlated with the full threshold ADHD group.
All five longitudinal studies (Kadesjo and Gillberg, 2001; Shankman et al., 2009; Bussing et al., 2010; Fergusson et al., 2010; Noren Selinus et al., 2016) found that subthreshold ADHD and full threshold ADHD diagnoses in childhood and adolescence were associated with a number of negative outcomes in late adolescence and early adulthood. With regards to academic challenges, Bussing et al. (2010) found that both the full threshold ADHD and subthreshold ADHD groups had lower grades and lower achievement scores on mathematic and reading standardized tests compared to controls. Similar findings were reported by longitudinal studies done by Fergusson et al. (2010) and Noren Selinus et al. (2016) using self-reported measures. Regarding social and interpersonal outcomes, Fergusson et al. (2010) associated subthreshold ADHD and full threshold ADHD in adolescence with several negative self-reported outcomes in young adulthood, including: crime and arrest, substance abuse/dependence, mental health issues (anxiety, MDD, suicide attempts, and anti-social personality disorder), no secondary degree, young pregnancy/parenthood, and lower earned income. In these areas, the full threshold ADHD group had the worst outcomes overall.
4. Discussion
Our systematic literature review and meta-analysis results indicate that subthreshold ADHD is a prevalent and morbid condition worthy of further clinical and scientific consideration. The results show that a sizeable minority of non-referred and referred children failed to meet full threshold diagnosis for ADHD while exhibiting significant functional impairment. Children with subthreshold symptoms of ADHD have patterns of morbidity and dysfunction that are significantly worse than children without ADHD and that closely resemble the patterns identified in children with full threshold ADHD. Children with subthreshold ADHD symptoms showed higher rates of comorbid psychopathology, as well as increased deficits in cognitive, interpersonal, and school functioning deficits relative to unaffected children.
The findings of subthreshold ADHD cases have a very similar pattern of comorbidity and spectrum of functional impairments as full threshold ADHD cases on several outcome variables. Data from several studies showed that both subthreshold ADHD and full threshold ADHD groups had similarly high rates of psychiatric comorbidities that were significantly different from controls (Scahill et al., 1999; Kim et al., 2009; Biederman et al., 2018). Additionally, both the subthreshold ADHD and full threshold ADHD groups had a greater risk for grade retention and graduation failure relative to controls (Bussing et al., 2010), and they were more likely to be placed in a special class or to receive extra help in school (Biederman et al., 2018). Notably, participants with full threshold ADHD and subthreshold ADHD also showed similar patterns of cognitive impairment and executive dysfunction (Scahill et al., 1999; DeBono et al., 2012; Hong et al., 2014; Biederman et al., 2018). It is notable that there were significant differences between the subthreshold ADHD and control groups given that many of the studies (7/9) included control group participants who had other psychopathologies. We would expect even more stark differences between these two groups if the controls had included only children with ADHD and no other psychopathologies. Taken together, these results support the notion that psychiatric and cognitive impairments are strongly associated with the symptomatic picture of ADHD whether at or below the diagnostic threshold.
On the other hand, some noteworthy differences between full and subthreshold ADHD were identified. Subthreshold ADHD subjects were more likely to come from higher socioeconomic backgrounds, had more even sex distribution, and had less disruptive behavior disorders than full threshold ADHD subjects (Cho et al., 2009; Kim et al., 2009; Hong et al., 2014; Biederman et al., 2018). These finding suggest that environmental factors, subject sex, and fewer disruptive disorders may exert protective effects that may inhibit the display of full-blown ADHD symptoms in some children. While these findings may inhibit the display of full-blown ADHD symptoms in some children, the patterns observed could be due to selection bias. More research is needed to confirm these findings before firm conclusions can be drawn.
The findings of similarly high levels of morbidity and dysfunction seen in subthreshold and full threshold ADHD are consistent with genetic data. Twin and population studies emphasize the genetic significance of subthreshold ADHD. Larsson et al. (2012)’s large twin data set found comparable group heritability estimates for full and subthreshold ADHD. Malmberg et al. (2011)’s twin study found that subthreshold ADHD was associated with higher rates of mood and anxiety disorders, psychosis, eating problems, and trauma than in controls. Noren Selinus et al. (2016)’s twin study reported that subsyndromal ADHD in childhood was associated with higher proportions of self-reported negative psychosocial and psychiatric outcomes in adolescence. In addition to these twin studies, a French population study found that subthreshold ADHD was morbid and predicted the onset of the full diagnosis during follow-up (Lecendreux et al., 2015). On the other hand, Shankman et al. (2009) failed to see a conversion of subthreshold ADHD cases to full threshold ADHD over the course of the study but did note that adolescents with subthreshold ADHD were likely to develop alcohol, substance, and conduct disorder at follow up (late adolescence/young adulthood).
Findings showing that perinatal factors were more closely related to full threshold ADHD than to subthreshold ADHD support the idea that perinatal complications could mediate the development of the full syndrome in children at genetic risk for the disorder (Kim et al., 2009; Biederman et al., 2018). These findings are consistent with the hypothesis that ADHD symptoms and impairment emerge due to the accumulation of both environmental and genetic risk factors (Faraone et al., 2015). Individuals with lower levels of risk at birth will take longer to accumulate sufficient risk factors, thus will have a later age of onset with symptoms and impairment (Biederman et al., 2018).
The finding that subthreshold ADHD symptoms are associated with negative outcomes has important implications. Clinicians may want to consider early intervention for children experiencing subsyndromal symptoms of ADHD. Such intervention can help mitigate the progression into a full syndromatic state and obviate the well documented compromised outcomes associated with ADHD (Faraone et al., 2015). Additionally, from a public health perspective, this knowledge may catalyze the development of methods to detect subsyndromal manifestations of ADHD in schools and community settings for early intervention efforts.
Our findings need to be viewed considering certain limitations, most notably that the literature on subthreshold ADHD is relatively sparse. Additionally, because there was substantial heterogeneity in the samples, our results may not easily generalize to all samples. The heterogeneity observed is likely a result of the differences in the methodologies amongst the studies, specifically when it came to the definition of subthreshold ADHD classification. Additionally, a couple of the studies used healthy controls as the comparison group while other studies included children with other psychiatric disorders other than ADHD. Another limitation stems from the fact that all the studies except for Biederman et al. (2018) based the subthreshold ADHD symptoms on insufficient symptoms only. However, symptoms of subthreshold ADHD can also be met by a later age of onset. The definition of subthreshold ADHD does not depend on degree of impairment, but that the impairment experienced is enough to meet partial diagnostic criteria. The available literature does not provide adequate information on the rate of conversion from subthreshold to full threshold ADHD. Although many gaps remain in the literature, the current study hopes to address these gaps by consolidating available data to make sense of the disorder’s presentation and pervasiveness. Finally, the available literature had large variability between the studies making meta-analytic results more tentative.
Despite these considerations, our systematic qualitative literature review and meta-analysis demonstrates that children failing to meet full threshold diagnosis for ADHD have highly similar patterns of impairment compared to those with the full syndrome, including high rates of comorbid disorders, as well as interpersonal, cognitive, and school functioning deficits. Female sex, higher SES status, fewer disruptive behavior disorders, and fewer perinatal complications distinguished subthreshold from full threshold ADHD cases. Taken together, these results support the high morbidity and disability associated with subthreshold ADHD worthy of further scientific and clinical considerations. Our meta-analysis results further highlight the increased risk of numerous negative outcomes for subthreshold ADHD relative to controls.
5. Declaration of Interest
Dr. Joseph Biederman is currently receiving research support from the following sources: AACAP, Feinstein Institute for Medical Research, Food & Drug Administration, Genentech, Headspace Inc., Lundbeck AS, Neurocentria Inc., NIDA, Pfizer Pharmaceuticals, Roche TCRC Inc., Shire Pharmaceuticals Inc., Sunovion Pharmaceuticals Inc., and NIH. Dr. Biederman has a financial interest in Avekshan LLC, a company that develops treatments for attention deficit hyperactivity disorder (ADHD). His interests were reviewed and are managed by Massachusetts General Hospital and Partners HealthCare in accordance with their conflict of interest policies. Dr. Biederman’s program has received departmental royalties from a copyrighted rating scale used for ADHD diagnoses, paid by Bracket Global, Ingenix, Prophase, Shire, Sunovion, and Theravance; these royalties were paid to the Department of Psychiatry at MGH. In 2019, Dr. Biederman is a consultant for Akili, Jazz Pharma, and Shire. Through MGH corporate licensing, he has a US Patent (#14/027,676) for a non-stimulant treatment for ADHD, and a patent pending (#61/233,686) on a method to prevent stimulant abuse. In 2018, Dr. Biederman was a consultant for Akili and Shire.
Dr. Stephen Faraone, in the past year, has received income, potential income, travel expenses continuing education support and/or research support from Lundbeck, Rhodes, Arbor, KenPharm, Ironshore, Shire, Akili Interactive Labs, CogCubed, Alcobra, VAYA, Sunovion, Genomind and Neurolifesciences. With his institution, he has US patent US20130217707 A1 for the use of sodium-hydrogen exchange inhibitors in the treatment of ADHD. In previous years, he received support from: Shire, Neurovance, Alcobra, Otsuka, McNeil, Janssen, Novartis, Pfizer and Eli Lilly. Dr. Faraone receives royalties from books published by Guilford Press: Straight Talk about Your Child’s Mental Health, Oxford University Press: Schizophrenia: The Facts and Elsevier: ADHD: Non-Pharmacologic Interventions. He is principal investigator of www.adhdinadults.com. Dr. Faraone is supported by the K.G. Jebsen Centre for Research on Neuropsychiatric Disorders, University of Bergen, Bergen, Norway, the European Union’s Seventh Framework Programme for research, technological development and demonstration under grant agreement no 602805, the European Union’s Horizon 2020 research and innovation programme under grant agreement No 667302 and NIMH grants 5R01MH101519 and U01 MH109536-01.
Ms. Anna-Mariya Kirova, Ms. Caroline Kelberman, Ms. Barbara Storch, Mrs. Maura DiSalvo and Ms. Yvonne Woodworth have no conflicts of interest.
6. Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Achenbach TM, 1991. Manual for the Child Behavior Checklist/4–18 and the 1991 Profile. University of Vermont, Department of Psychiatry, Burlington, VT. [Google Scholar]
- Biederman J, Fitzgerald M, Kirova A, Woodworth KY, Biederman I, Faraone SV, 2018. Further evidence of morbidity and dysfunction associated with subsyndromal ADHD in clinically referred children. J Clin Psychiatry 79. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza BM, 1993. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child and Adolescent Psychiatry 32, 361–368. [DOI] [PubMed] [Google Scholar]
- Bussing R, Mason DM, Bell L, Porter P, Garvan C, 2010. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J Am Acad Child Adolesc Psychiatry 49, 595–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Z, Lichtenstein P, Asherson PJ, Larsson H, 2013. Developmental twin study of attention problems: high heritabilities throughout development. JAMA Psychiatry 70, 311–318. [DOI] [PubMed] [Google Scholar]
- Cho SC, Kim BN, Kim JW, Rohde LA, Hwang JW, Chungh DS, et al. , 2009. Full syndrome and subthreshold attention-deficit/hyperactivity disorder in a Korean community sample: comorbidity and temperament findings. Eur Child Adolesc Psychiatry 18, 447–457. [DOI] [PubMed] [Google Scholar]
- Conners CK, 1969. A teacher rating scale for use in drug studies with children. American Journal of Psychiatry 126, 884–888. [DOI] [PubMed] [Google Scholar]
- Conners CK, 1995. The conners rating scales: instruments for the assessment of childhood psychopathology. [Google Scholar]
- DeBono T, Hosseini A, Cairo C, Ghelani K, Tannock R, Toplak M, 2012. Written expression performance in adolescents with attention-deficit/hyperactivity disorder (ADHD). Read Writ 25, 1403–1426. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos A, Reed R, 1998. The ADHD Rating Scale-IV Checklist, Norms and Clinical Interpretation. Guilford Press, New York, NY. [Google Scholar]
- Edwards TC, Huebner CE, Connell FA, Patrick DL, 2002. Adolescent quality of life, part I: conceptual and measurement model. J Adolesc 25, 275–286. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, et al. , 2015. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers 1, 15020. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, 2016. Can attention-deficit/hyperactivity disorder onset occur in adulthood? JAMA Psychiatry 73, 655–656. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ, 2010. Classification of behavior disorders in adolescence: scaling methods, predictive validity, and gender differences. J Abnorm Psychol 119, 699–712. [DOI] [PubMed] [Google Scholar]
- Greven CU, Merwood A, van der Meer JM, Haworth CM, Rommelse N, Buitelaar JK, 2016. The opposite end of the attention deficit hyperactivity disorder continuum: genetic and environmental aetiologies of extremely low ADHD traits. J Child Psychol Psychiatry 57, 523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong SB, Dwyer D, Kim JW, Park EJ, Shin MS, Kim BN, et al. , 2014. Subthreshold attention-deficit/hyperactivity disorder is associated with functional impairments across domains: a comprehensive analysis in a large-scale community study. Eur Child Adolesc Psychiatry 23, 627–636. [DOI] [PubMed] [Google Scholar]
- Kadesjo B, Gillberg C, 2001. The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry 42, 487–492. [PubMed] [Google Scholar]
- Kim HW, Cho SC, Kim BN, Kim JW, Shin MS, Kim Y, 2009. Perinatal and familial risk factors are associated with full syndrome and subthreshold attention-deficit hyperactivity disorder in a Korean community sample. Psychiatry investigation 6, 278–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landgraf J, 1995. Child Health Questionnaire-Parent form CHQ-PF 50. The Health Institute of New England Medical Center, Boston. [Google Scholar]
- Larsson H, Anckarsater H, Rastam M, Chang Z, Lichtenstein P, 2012. Childhood attention-deficit hyperactivity disorder as an extreme of a continuous trait: a quantitative genetic study of 8,500 twin pairs. J Child Psychol Psychiatry 53, 73–80. [DOI] [PubMed] [Google Scholar]
- Lecendreux M, Konofal E, Cortese S, Faraone SV, 2015. A 4-year follow-up of attention-deficit/hyperactivity disorder in a population sample. J Clin Psychiatry 76, 712–719. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Shankman SA, Gau JM, Klein DN, 2004. The prevalence and co-morbidity of subthreshold psychiatric conditions. Psychol Med 34, 613–622. [DOI] [PubMed] [Google Scholar]
- Malmberg K, Edbom T, Wargelius HL, Larsson JO, 2011. Psychiatric problems associated with subthreshold ADHD and disruptive behaviour diagnoses in teenagers. Acta Paediatr 100, 1468–1475. [DOI] [PubMed] [Google Scholar]
- McCarney S, 1996. The Learning Disability Evaluation Scale - Renormed. Hawthorne Educational Services, Inc., Columbia, MO. [Google Scholar]
- Noren Selinus E, Molero Y, Lichtenstein P, Anckarsater H, Lundstrom S, Bottai M, et al. , 2016. Subthreshold and threshold attention deficit hyperactivity disorder symptoms in childhood: psychosocial outcomes in adolescence in boys and girls. Acta Psychiatr Scand 134, 533–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW, 2002. The clinician’s guide to the Behavior Assessment System for Children (BASC). Guilford Press, New York. [Google Scholar]
- Roberts RE, Fisher PW, Turner JB, Tang M, 2015. Estimating the burden of psychiatric disorders in adolescence: the impact of subthreshold disorders. Soc Psychiatry Psychiatr Epidemiol 50, 397–406. [DOI] [PubMed] [Google Scholar]
- Scahill L, Schwab-Stone M, Merikangas KR, Leckman JF, Zhang H, Kasl S, 1999. Psychosocial and clinical correlates of ADHD in a community sample of school-age children. J Am Acad Child Adolesc Psychiatr 38, 976–984. [DOI] [PubMed] [Google Scholar]
- Shankman SA, Lewinsohn PM, Klein DN, Small JW, Seeley JR, Altman SE, 2009. Subthreshold conditions as precursors for full syndrome disorders: a 15-year longitudinal study of multiple diagnostic classes. J Child Psychol Psychiatry 50, 1485–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]


