Abstract
Oceania and South East Asia (OSEA) is a socioeconomically, culturally, and ethnically diverse region facing a rising epidemic of noncommunicable diseases, including chronic kidney disease (CKD). The second iteration of the International Society of Nephrology Global Kidney Health Atlas aimed to provide a comprehensive evaluation of kidney care in OSEA. Of the 30 countries/territories in OSEA, 15 participated in the survey, representing 98.5% of the region’s population. The median prevalence of treated kidney failure in OSEA was 1352 per million population (interquartile range, 966–1673 per million population), higher than the global median of 787 per million population. Although the general availability, access, and quality of kidney replacement therapy (i.e., dialysis and transplantation) was high in OSEA, inequalities in accessibility and affordability of kidney replacement therapy across the region resulted in variability between countries. According to the survey results, in a third of the participating countries (mostly lower-income countries), less than half the patients with kidney failure were able to access dialysis, whereas it was readily available to all with minimal out-of-pocket costs in high-income countries; similar variability in access to transplantation was also recorded. Limitations in workforce and resources vary across the region and were disproportionately worse in lower-income countries. There was little advocacy for kidney disease, moderate use of registries, restricted CKD detection programs, and limited availability of routine CKD testing in some high-risk groups across the region. International collaborations, as seen in OSEA, are important initiatives to help close the gaps in CKD care provision across the region and should continue receiving support from the global nephrology community.
Keywords: dialysis, end-stage kidney disease, global health care, health care delivery, health policy, nephrology, Oceania and South East Asia, surveys and questionnaires
The Oceania and South East Asia region (OSEA) is an International Society of Nephrology (ISN) construct, including countries from the World Health Organization’s regions of South East Asia and Western Pacific. South East Asia is a highly populated region of the world, whereas the Pacific region covers a third of the earth’s surface but <1% of the global population.1,2 In addition to emerging infectious diseases and prevalent outbreak-prone diseases (such as measles and rubella), OSEA is also prone to natural disasters, climate change health impacts, and a rising burden of noncommunicable diseases, including chronic kidney disease (CKD).3,4 Kidney care is highly variable across the region. Nephrology care is well developed in some countries, such as Australia, New Zealand, Singapore, Thailand, Philippines, and Malaysia, whereas in many of the Pacific Island nations, it is almost nonexistent.4,5 In most higher-income countries, dialysis services are readily available and publicly funded. In contrast, in many Pacific Island nations, limited or no dialysis services exist.4,5 In addition, in less well-developed countries, dialysis is only available in user-pay facilities.5 In some lower-income countries, dialysis services represent recent development. For example, in Cambodia, the first hemodialysis (HD) and peritoneal dialysis (PD) treatments were performed in 1997 and 2013, respectively.5 The same limitations in access to transplantation services are also seen across the region, with limited access or unavailability in many lower-income countries and island nations.4,5 Although national registries for dialysis, transplantation, and CKD exist in different OSEA countries, there is no regional registry available.5 Consequently, there remains considerable uncertainty regarding the availability, accessibility, quality, and affordability of kidney care in the OSEA region. Using data from the second iteration of the ISN Global Kidney Health Atlas, we report on these aspects of kidney care in the OSEA region. The methods for this research are described in detail elsewhere.6
Results
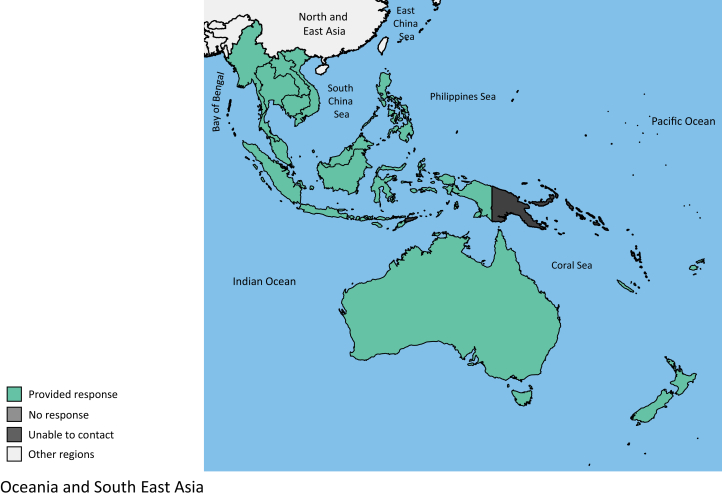
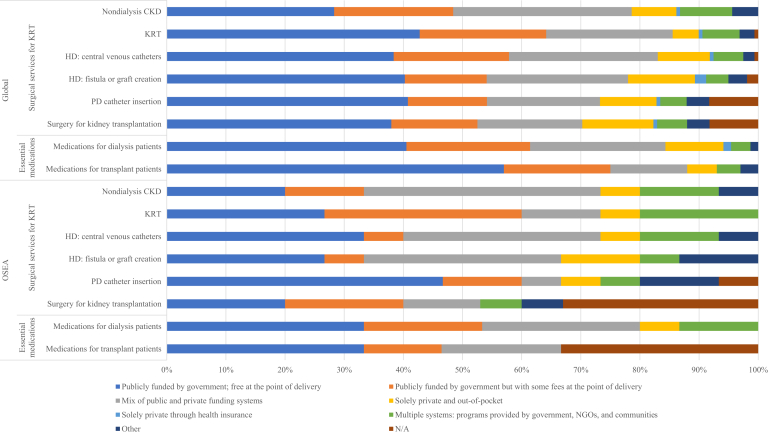
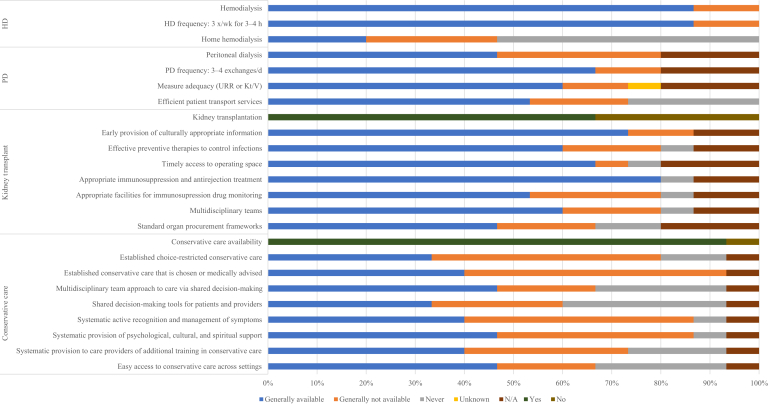
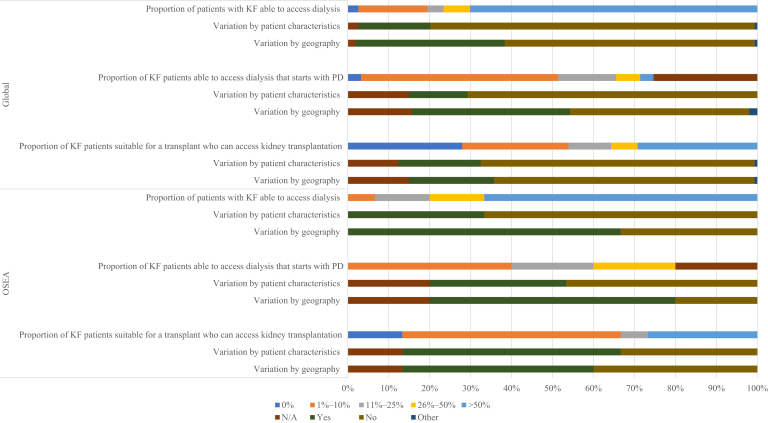
Results of this study are presented in tables and figures and broadly summarized into 2 categories: desk research (Tables 17, 8, 9 and 210, 11, 12, 13, 14, Figure 1, Supplementary Tables S1 and S2, and Supplementary Appendix) and survey administration (Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figures S1–S7).
Table 1.
General demographic and economic indicators of the 15 OSEA countries and territory participating in the ISN-GKHA survey7, 8, 9
| Country/territory | World Bank income level | Area, km2 | Total population (2018)a | GDP (PPP), $ billionb | Total health expenditures, % of GDPb | Annual cost KRTc (US$) and out-of-pocket cost/% paid by patient from total costd |
|||
|---|---|---|---|---|---|---|---|---|---|
| HD | PD | KT |
|||||||
| First year | Later years | ||||||||
| Global median [IQR]e | — | — | — | — | 6.5 [4.9–8.8] | 22,617 [14,882–49,690] | 20,524 [14,305–33,905] | 25,356 [15,913–43,901] | |
| OSEA median [IQR] | — | — | — | 330 [34–933] | 4.4 [3.6–5.7] | 22,601 [10,140–28,559] | 16,479 [14,339–23,464] | 20,070[6588–36,768] | 8003 [5385–16,479] |
| Australia | High | 7,741,220 | 23,470,145 | 1248 | 9.3 | 57,183/1–25 | 49,099/1–25 | 34,894/0 | 10,269/0 |
| Brunei Darussalam | High | 5756 | 450,565 | 34 | 2.3 | 20,205/0 | 23,464/0 | —/0 | —/0 |
| Cambodia | Lower-middle | 181,035 | 16,449,519 | 64 | 6.1 | 8760/100 | — | — | — |
| Fiji | Upper-middle | 18,274 | 926,276 | 9 | 3.6 | —/>75 | —/>75 | — | — |
| Indonesia | Lower-middle | 1,904,569 | 262,787,403 | 3250 | 3.3 | 10,140/26–50 | 8134/1–25 | 19,743/1–25 | 2956/1–25 |
| Lao PDR | Lower-middle | 236,800 | 7,234,171 | 49 | 2.8 | —/26–50 | — | — | — |
| Malaysia | Upper-middle | 329,847 | 31,809,660 | 933 | 4.0 | 10,386/1–25 | 9977/1–25 | 20,396/1–25 | 5385/1–25 |
| Myanmar | Lower-middle | 676,578 | 55,622,506 | 330 | 5.1 | 7169/>75 | 14,339/1–25 | 4302/26–50 | —/26–50 |
| New Caledonia | High | 18,575 | 282,754 | 11 | — | —/0 | —/0 | —/0 | —/0 |
| New Zealand | High | 268,838 | 4,545,627 | 189 | 9.3 | 41,390/1–25 | 28,788/1–25 | 38,642/1–25 | 19,117/1–25 |
| Philippines | Lower-middle | 300,000 | 105,893,381 | 877 | 4.4 | —/26–50 | —/26–50 | —/>75 | —/>75 |
| Samoa | Lower-middle | 2831 | 201,316 | 1 | 5.6 | —/1–25 | — | — | — |
| Singapore | High | 697 | 5,995,991 | 528 | 4.3 | 28,532/26–50 | 15,547/1–25 | 43,901/26–50 | 16,479/26–50 |
| Thailand | Upper-middle | 513,120 | 68,615,858 | 1236 | 3.8 | 24,996/1–25 | 23,267/0 | 8601/26–50 | 5736/26–50 |
| Vietnam | Lower-middle | 331,210 | 97,040,334 | 649 | 5.7 | 28,559/>75 | 16,479/>75 | 4575/>75 | —/>75 |
—, Data not reported/unavailable; GDP, gross domestic product; GKHA, Global Kidney Health Atlas; HD, hemodialysis; IQR, interquartile range; ISN, International Society of Nephrology; KRT, kidney replacement therapy; KT, kidney transplant; OSEA, Oceania and South East Asia; PD, peritoneal dialysis; PDR, People’s Democratic Republic; PPP, purchasing power parity.
The total Oceania and South East Asia region population in 2018 was 691,621,337 people, of which participating countries accounted for 98.5%.
Estimates are in US$ 2017.
Detailed reference list on annual cost of KRT is available in the Supplementary Appendix.
Costs are in US$ 2016.
Median and interquartile range are calculated from the participating countries in the ISN-GKHA survey only.
Table 2.
Kidney replacement therapy and nephrology workforce statistics in the 15 OSEA countries and territory participating in the ISN-GKHA survey10, 11, 12, 13, 14
| Country/territory | World Bank income level | Treated KF, pmp, 2018 |
Prevalence of long-term dialysis, pmp, 2018 |
Long-term dialysis centers, pmp |
Kidney transplantation, pmp, 2018 |
Nephrology workforce, pmp |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | Prevalence | HD | PD | Total (HD + PD)a | HD | PD | Incidence | Prevalence | Centers | Nephrologists | Nephrology trainees | ||
| Global median [IQR]b | — | 142 [106–193] | 787 [522–1047] | 310.0 [99.0–597.0] | 25.0 [2.0–56.0] | 359.0 [112.0–636.0] | 4.5 [1.2–9.9] | 1.3 [0.4–2.5] | 14.0 [5.0–36.0] | 269.0 [66.0–468.0] | 0.4 [0.2–0.7] | 10.0 [1.2–22.7] | 1.4 [0.4–3.7] |
| OSEA median [IQR]b | — | 259 [135–338] | 1352 [966–1673] | 682.0 [411.0–970.0] | 101.0 [10.0–175.0] | 887.0 [320.0–1235.0] | 5.7 [1.5–14.4] | 2.2 [0.6–3.3] | 4.7 [2.5–12.6] | 268.0 [58.0–461.0] | 0.4 [0.1–0.7] | 5.7 [1.1–16.6] | 1.1 [0.3–4.5] |
| Australia | High | 117 | 988 | 425.5 | 101.1 | 527.0 | 4.3 | 4.3 | 45.0 | 461.0 | 0.9 | 21.3 | 5.0 |
| Brunei Darussalam | High | 393 | 1673 | 1064.6 | 170.4 | 1235.0 | 14.4 | 3.3 | — | — | 2.2 | 28.9 | 11.1 |
| Cambodia | Lower-middle | — | — | — | — | — | 0.6 | — | — | — | — | 0.9 | 0.3 |
| Fiji | Upper-middle | — | — | — | — | — | 6.5 | 2.2 | — | — | — | 1.1 | 1.1 |
| Indonesia | Lower-middle | 135 | 323 | — | 3.3 | 320.0 | 2.5 | 0.2 | 2.0 | — | 0.0 | 0.5 | 0.2 |
| Lao PDR | Lower-middle | — | — | — | — | — | 1.2 | — | — | — | — | — | 11.3 |
| Malaysia | Upper-middle | 259 | 1352 | 970.0 | 95.0 | 1295.0 | 23.6 | 1.4 | 2.5 | 58.0 | 0.1 | 5.7 | 1.1 |
| Myanmar | Lower-middle | — | — | — | 0.0 | — | 1.5 | 0.1 | 0.0 | — | 0.1 | 0.5 | 0.3 |
| New Caledonia | High | 338 | 2542 | 1770.0 | 251.0 | 2021.0 | 47.7 | 26.5 | — | 521.0c | —c | 40.7 | 0.0 |
| New Zealand | High | 119 | 966 | 410.6 | 175.4 | 586.0 | 2.4 | 2.4 | 39.8 | 380.0 | 0.7 | 15.4 | 4.5 |
| Philippines | Lower-middle | 172 | 319 | 69.2 | 10.1 | 314.0 | 5.7 | — | 4.7 | 5.0 | 0.3 | 5.7 | 0.9 |
| Samoa | Lower-middle | — | — | — | — | — | 9.9 | — | — | — | — | 5.0 | 0.0 |
| Singapore | High | 333 | 2076 | 681.9 | 158.3 | 1188.9 | 19.4 | 0.9 | 12.6 | 267.5 | 0.4 | 16.6 | 3.5 |
| Thailand | Upper-middle | 346 | 1515 | 823.5 | 369.0 | 1192.5 | 10.7 | 3.2 | 9.4 | 114.1 | 0.4 | 11.7 | 1.3 |
| Vietnam | Lower-middle | — | — | 41.7 | 11.5 | 53.2 | 1.3 | 0.6 | 2.9 | — | 0.2 | 3.1 | 0.5 |
—, Data not reported/unavailable; GKHA, Global Kidney Health Atlas; HD, hemodialysis; IQR, interquartile range; ISN, International Society of Nephrology; KF, kidney failure; OSEA, Oceania and South East Asia; PD, peritoneal dialysis; PDR, People’s Democratic Republic; pmp, per million population.
The total number of dialysis patients might not correspond to the sum of HD and PD patients if numbers for HD, PD, and total dialysis patients were obtained from different data resources.
Median and interquartile range are calculated from the countries participating in the ISN-GKHA survey.
In New Caledonia, patients can receive a kidney transplantation in France and, since 2012, a local kidney transplantation program is also available with transplantation being performed in Sydney, Australia.
Figure 1.
Countries and territory participating in the International Society of Nephrology (ISN) Global Kidney Health Atlas survey in the ISN Oceania and South East Asia region.
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT) care reported by the countries and territory participating in the International Society of Nephrology Global Kidney Health Atlas survey. Values represent absolute number of countries in each category, expressed as a percentage of total number of participating countries. In Oceania and South East Asia (OSEA), when peritoneal dialysis/transplantation is not available, funding structure is listed as N/A. HD, hemodialysis; NGOs, nongovernmental organizations; PD, peritoneal dialysis.
Figure 3.
Availability of choice in kidney replacement therapy or conservative care for patients with kidney failure reported by the 15 Oceania and South East Asia countries and territory participating in the International Society of Nephrology Global Kidney Health Atlas survey. In some countries, kidney transplantation is not available locally, but some services related to transplantation are available. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
Figure 4.
Accessibility of kidney replacement therapy for patients with kidney failure (KF), reported by the countries and territory participating in the International Society of Nephrology Global Kidney Health Atlas survey. In some Oceania and South East Asia (OSEA) countries, kidney transplantation is not available locally, but some services related to transplantation are available. N/A, not provided; PD, peritoneal dialysis.
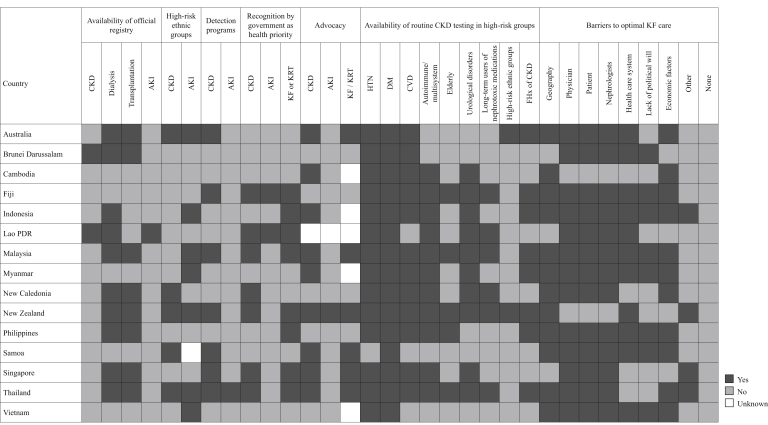
Figure 5.
Country-level scorecard for registries, national policies, advocacy, and barriers to optimal kidney care in the International Society of Nephrology Oceania and South East Asia region. AKI, acute kidney injury; CKD, chronic kidney disease; CVD, cardiovascular disease; DM, diabetes mellitus; FHx, family history; HTN, hypertension; KF, kidney failure; KRT, kidney replacement therapy; PDR, People’s Democratic Republic.
Setting
A total of 30 countries and territories are listed as part of the ISN OSEA region.3 It includes South East Asian countries (Indonesia, Myanmar, Thailand, Timor-Leste [World Health Organization’s South East Asia1]; Brunei Darussalam, Cambodia, Lao People’s Democratic Republic (PDR), Malaysia, Philippines, Singapore, Vietnam [World Health Organization’s Western Pacific2]), Australia, and New Zealand and a large group of Pacific Island nations, including the countries of Kiribati, Marshall Islands, Federated States of Micronesia, Fiji, Nauru, Palau, Papua New Guinea, Samoa, Solomon Islands, Tonga, Tuvalu, and Vanuatu; the French territories of French Polynesia and New Caledonia; and the US territories of American Samoa, Guam, and Northern Mariana Islands. The total population of the OSEA region is 692 million, Indonesia being the most populous (263 million). The region covers a total area of 12.8 million square kilometers. Australia represents 61% of that area while being home to about 3% of the population of the region. In comparison, South East Asian countries cover 33% of the OSEA area but represent 94% of the population.7 Most South East Asian and Pacific Island countries are listed as middle-income countries. Singapore, Australia, and New Zealand are ranked as high-income countries, as are most French and American Pacific territories.15 Diverse economies are seen across the OSEA region, with different health funding schemes.
Characteristics of participating countries
Thirty-six respondents, representing 14 countries and 1 territory (New Caledonia) in the ISN OSEA region, completed the online questionnaire (Figure 1). Most respondents were nephrologists (n = 29 [81%]), and other respondents included 2 policy makers (6%), 1 nonnephrologist physician (3%), 1 nonphysician health professional (3%), and 3 in other roles (8%). The overall response rate for this region was 81.8%. Participating countries jointly represented a population of 681.3 million. Most OSEA countries were classified as lower-middle income (n = 7), followed by high income (n = 5) and upper-middle income (n = 3).15 As a proportion of gross domestic product, health expenditures in participating countries ranged from 2.3% in Brunei Darussalam to 9.3% in both Australia and New Zealand (Table 1).7, 8, 9 General demographics, economic indicator, and burden of CKD in the 15 OSEA countries and territories that did not participate in the ISN Global Kidney Health Atlas survey are listed in Supplementary Table S1.
Burden of CKD and kidney failure in OSEA
World Health Organization data on the burden of CKD in the OSEA region were available for all participating countries, except the territory of New Caledonia. The median prevalence of CKD in OSEA for participating countries was 10.8% (95% confidence interval, 9.8%–11.4%), ranging from 8% in Cambodia to 13.9% in Thailand. The highest proportions of deaths and disability-adjusted life years attributed to CKD were found in lower middle-income countries, including Samoa and the Philippines (Supplementary Table S2).
Just over half of the participating countries in OSEA, including Australia, Brunei Darussalam, Indonesia Malaysia, New Zealand, the Philippines, Singapore, Thailand, and New Caledonia, had data available on the frequency of treated kidney failure (KF). The median prevalence of treated KF in OSEA was 1352 per million population (pmp) (interquartile range [IQR], 966–1673 pmp) compared with the global median of 787 pmp. The prevalence was 3- to 6-fold higher observed in high- and upper-middle income countries (n = 6; 988–2076 pmp), compared with lower middle-income countries (n = 2; 320 pmp) (Table 2).10, 11, 12, 13, 14 The median number of new cases of treated KF in the region (259 pmp; IQR, 135–338 pmp) was also higher than the global median (142 pmp), with this growing burden mainly present in Brunei Darussalam, Thailand, and Singapore.
Health finance and service delivery
Government funding was provided for nondialysis CKD in only one-third of OSEA countries, compared with 48% of countries globally (Figure 2). Among the 15 participating countries/territories, 10 (67%) had data available for the annual costs of dialysis. Median annual costs (in 2016 US$) per person for maintenance HD ($22,601; IQR, $10,140–$28,559) were similar to the global median ($22,617), whereas PD costs ($16,479; IQR, $14,339–$23,464) were below the global median ($20,524) (Table 1).7, 8, 9 The lowest HD costs were reported from the lower-middle income countries of Myanmar and Cambodia ($7169 and $8760, respectively), where >75% and 100% of total costs, respectively, were covered by patients (out-of-pocket costs). On the contrary, in Australia and New Zealand, annual costs for HD were $57,183 and $41,390, respectively, but out-of-pocket costs only represented 1% to 25% of total costs. Lower costs for PD compared with HD were seen in all countries, with the exceptions of Brunei Darussalam ($20,205 for HD vs. $23,464 for PD) and Myanmar ($7169 for HD vs. $14,339 for PD). Of note, in Myanmar, only 1% to 25% of PD costs were out of pocket for patients compared with >75% for HD. Data on the annual cost of kidney transplantation in the first year were available in 8 of the 10 countries where transplantation was available, with a 10-fold range in costs (from $4302 in Myanmar to $43,901 in Singapore). Out-of-pocket costs for transplantation accounted for 1% to 50% of total costs in most countries, except for Australia (0%) and Vietnam (>75%) (Table 1).7, 8, 9
Health workforce for nephrology care
In keeping with the global trend, nephrologists were primarily responsible for KF care in OSEA (n = 14 countries [93%]), with support from primary care physicians (n = 5), multidisciplinary teams (n = 5), and nurse practitioners or specialized nurses (n = 5). In Lao PDR, health officers or extension workers bore the primary clinical responsibility for the delivery of KF care. The median number of nephrologists (5.66 pmp; IQR, 1.08–16.59 pmp) in OSEA was much lower than the median number worldwide (9.95 pmp), whereas the median number of nephrology trainees (1.08 pmp; IQR, 0.30–4.51 pmp) was similar to the global trend (1.42 pmp) (Table 2).10, 11, 12, 13, 14 Overall, the number of nephrologists was higher in high-income countries (15–41 nephrologists pmp), whereas some lower-middle income countries (Myanmar, Indonesia, and Cambodia) had <1 nephrologist pmp. The most commonly reported workforce shortages were for nephrologists, dialysis nurses, and vascular access coordinators, as reported by all countries but Australia, New Caledonia, and New Zealand (80% of countries). Surgeons and interventional radiologists for dialysis access, transplant surgeons and coordinators, dialysis technicians, and counselors/psychologists were also in shortage in 60% to 73% of countries. Most lower-income countries reported substantially more workforce shortages than high-income countries (Supplementary Figure S1). Australia was the only country reporting no shortage in kidney replacement therapy (KRT; dialysis and/or transplantation) providers. New Caledonia reported no shortage besides transplant surgeons as transplantation was performed in Australia.
Essential medications and health product access for KF care
Dialysis
Long-term HD was available and the predominant form of dialysis in all participating countries, and was the sole KRT modality in Cambodia, Lao PDR, and Samoa. However, in Fiji and Myanmar, HD was generally not available to patients (Figure 3). The median number of HD centers was 5.67 pmp (n = 15; IQR, 1.49–14.43), with the highest densities in New Caledonia and Malaysia (47.74 and 23.58 pmp, respectively) and the lowest in Cambodia and Lao PDR (0.61 and 1.24 pmp, respectively) (Table 2).10, 11, 12, 13, 14 Home HD was readily available in Australia, New Zealand, and New Caledonia only. In lower-middle income countries (Cambodia, Indonesia, Lao PDR, Myanmar, Philippines, and Vietnam), between 51% and 75% of patients began treatment with a temporary dialysis catheter. In Fiji, >75% of patients started HD with a tunneled dialysis catheter, whereas New Caledonia reported 51% to 75% of patients having a functioning vascular access (arteriovenous fistula or graft) at dialysis commencement (Supplementary Figure S2).
PD was available in 80% of countries (n = 12), with just over half of these countries (n = 7) offering it to all suitable patients (Figure 3). The proportion of dialysis patients on PD was highest in Thailand and New Zealand (31% and 30%, respectively), but represented <10% in Indonesia, Philippines, and Malaysia. The median number of PD centers in the region was 2.16 pmp (n = 11; IQR, 0.57–3.33) and higher than the global average. Indonesia and Myanmar had the lowest PD capacity (Table 2).10, 11, 12, 13, 14 Of the 12 countries, 10 (83%) were able to offer adequate frequency of exchanges (3–4 manual exchanges per day or equivalent cycles on automated PD), and 9 of those (75%) had the capacity to measure PD adequacy (via measurement of urea reduction ratio or measure of dialysis adequacy [Kt/V]) (Figure 3).
In a third of the participating countries in the survey, less than half the patients with KF were able to access dialysis (Figure 4). This was the case for Fiji (1%–10%), Lao PDR and Myanmar (11%–25%), and Cambodia and Samoa (25%–50%). Two-thirds of countries reported variability in dialysis accessibility based on geography (n = 10 [66.7%]), and 5 of those countries also reported variation based on patient characteristics. The proportion of people undergoing PD varied widely across countries and within countries, depending on geographic factors and patient characteristics (Figure 4). Efficient patient transport services for dialysis were reported as generally available in just over half of the participating countries and never available in about a quarter of countries (Figure 3).
Kidney transplantation
Kidney transplantation was available in two-thirds of participating countries/territories, with a regional median of 0.36 transplant center pmp (n = 16; IQR, 0.13–0.66), similar to the global median of 0.42 pmp (IQR, 0.20–0.72 pmp) (Table 2).10, 11, 12, 13, 14 Brunei Darussalam had the highest number of transplantation centers (2.22 transplant centers pmp), whereas Indonesia had the lowest (0.02 pmp). For Fiji and New Caledonia, kidney transplantation was only available overseas (India and Australia), with follow-up provided by these nations.16 Patients living with a functioning graft represented a large proportion (20%–47%) of patients on KRT in high-income countries, except in Brunei Darussalam (Table 2).10, 11, 12, 13, 14 In Brunei, Indonesia, and Myanmar, only living donation was available, whereas all other countries with transplantation capacity performed a combination of deceased and living donor kidney transplantation. National deceased donor kidney transplant waitlists were available in 60% of transplanting countries, whereas others had regional lists only, except for the Philippines, where no waitlist was recorded. Provision of early and culturally appropriate information about transplantation to patients was available in all countries providing kidney transplantation, including New Caledonia, through the remote transplant program (Figure 3). Most of these countries also provided effective infection control measures, timely access to operating space, and appropriate immunosuppression and antirejection treatment. In Myanmar, Philippines, and Vietnam, however, appropriate facilities for immunosuppression drug monitoring were reported as generally not available (Figure 3).
Transplantation was unavailable in a third of countries, and 6 other countries reported that transplantation was accessible to only 1% to 10% (Indonesia, Malaysia, Philippines, Thailand, and Vietnam) or 11% to 25% (Myanmar) of the population. More than half of suitable patients had access to transplantation in high-income countries (Australia, Brunei Darussalam, New Zealand, and Singapore) (Figure 3).
Conservative kidney management
Conservative care was available in all OSEA countries, except Cambodia (Figure 3). In 30% to 40% of countries (mostly high-income countries), a multidisciplinary approach to care via shared decision making, shared decision-making tools for patients and providers, systematic active recognition and management of symptoms, systematic provision of psychological, cultural, and spiritual support, and systematic provision to care providers of additional training in conservative care were available (Figure 3).
Most services to diagnose and treat complications of KF were available in most OSEA countries (Supplementary Figure S3).
Reporting of KRT quality indicators
In all countries, quality indicators were monitored and reported if the treatment modality was available (Supplementary Figure S4). For patients on dialysis, blood pressure, hemoglobin/hematocrit, and solute clearance were monitored in >75% of the centers in most countries. Patient survival was monitored in all countries for each available modality, except for Cambodia and Vietnam, where patient survival on HD was not reported. The least reported quality indicator was patient-reported outcome measures, particularly in transplantation (Supplementary Figure S4).
Health information systems, statistics, and national health policy
Most OSEA countries had official registries for dialysis (n = 10; 90% national) and transplantation (n = 8; all national), reporting on modality of dialysis/transplant source, etiology of KF, mortality, and process-based measures (Supplementary Figure S5). Only 2 countries (Lao PDR and Brunei Darussalam) had registries covering the whole spectrum of CKD (stages 1–5). Hospitalizations and quality of life were rarely recorded in the various registries. No official registries were reported in Cambodia, Fiji, Myanmar, Samoa, and Vietnam. Participation in registries was mandatory for the 2 CKD registries and for 70% and 50% of dialysis and transplant registries (Supplementary Figure S5). Only Lao PDR had a local, voluntary, acute kidney injury (AKI) registry, reporting on risk factors, etiology, and incidence of AKI and patient outcome measures (hospitalizations and requirement for KRT).
Routine testing for kidney disease was available in most OSEA countries for patients with diabetes, hypertension, cardiovascular disease, autoimmune/multisystem diseases, and urological disorders (Figure 5). Five countries identified specific ethnic groups present in that country considered to be at increased risk for CKD, but routine testing for those groups was only available in 2 countries (Australia and New Zealand). Almost half the countries (n = 7 [47%]) had a CKD detection program, but only Thailand had an AKI detection program (Figure 5).
National strategies to improve care for patients with CKD were available in 9 countries covering more frequently the non–dialysis-dependent CKD population (n = 6 [66.7%]) than the kidney transplantation/long-term dialysis population (n = 3 [33.3%]) (Supplementary Figures S6 and S7). Recognition of kidney disease by the government as a health priority was much more common for KF (53%) and CKD (47%) than for AKI (13%) (Figure 5). In comparison, advocacy groups were more frequent for CKD (60%), followed by KF (40%) and AKI (7%) (Figure 5). The most commonly cited barriers to optimal kidney care were the physician, the patient, and the nephrologists (87% of countries), followed by geography (80%), health care system and economic factors (73%), and lack of political will (53%) (Figure 5).
Discussion
This study brings to light several important aspects of kidney care in OSEA. Inequalities in accessibility and affordability of KRT across the region resulted in highly variable prevalence of treated KF between countries, although the general availability, access, and quality of KRT was high in OSEA. The workforce and availability of resources varied across the region and were disproportionately worse in lower-income countries. There was little advocacy for kidney disease, moderate use of registries, restricted CKD detection programs, and limited availability of routine CKD testing in some high-risk groups across the region.
Although CKD prevalence across the OSEA region was about 11%, few data were available for half of the jurisdictions included in the OSEA region, particularly for Pacific Islands nations. A lack of data on disease prevalence, incidence, resource use, and quality of care in lower-income countries limits the ability to monitor the care provided and evaluate resource availability. Furthermore, it makes it harder for governments and providers to predict the appropriate allocation of health care resources, including KRT facilities, medicines, and health care professionals. For example, in an assessment of the capacity of clinical systems to address the burden of noncommunicable diseases in American Samoa in 2011, a 33% increase in the number of patients receiving HD was noted between 2006 and 2010. The identification of the burden of disease and the agencies and programs responsible for delivery of care were highlighted as priority areas.17 Similarly, in 2012, a review of laboratory results and detailed audit of medical records in Fiji estimated a crude KF incidence rate of 753 pmp, indicating that CKD was a substantial public health problem, likely attributable to an increasing prevalence of obesity, diabetes, and hypertension in the Fijian population.18 It concluded that improvement in kidney disease screening and management was warranted to mitigate adverse impacts on life expectancy and quality of life.18
Although KRT availability, access, and quality were overall high in participating OSEA countries, they were substantially higher and more affordable for patients in high-income countries. Transplantation was available in two-thirds of participating OSEA countries, although rates of transplantation were much lower in countries where only living-related transplantation was available (Brunei Darussalam19 and Indonesia and Myanmar20). HD was available in all countries, but home HD was only available in 3 high-income countries. PD was available in most countries, but only 83% of those reported an ability to provide adequate exchanges. In some countries, the funding structure of KF care had an impact on dialysis modality selection. For example, in Thailand, the universal coverage system followed a PD-first policy, which has resulted in a steady increase in PD uptake over time.20 In addition to cost savings, promoting PD use could also improve access to dialysis in rural areas in countries where the funding models favor urban settings for HD centers, as described in Malaysia21 and Indonesia.22
Compared with the dominant public funding system for CKD care globally, government funding was responsible for nondialysis CKD care in only a third of OSEA countries and for KRT in 60% of countries. Changes toward public funding and government financial support of KRT over the last decade have been associated with a substantial increase in dialysis treatment rates in some OSEA countries, including Malaysia, Philippines, Indonesia, and Thailand.20 In Cambodia and Lao PDR, there are no national health insurance systems and, therefore, patients of lower socioeconomic status only come to the HD center when they can afford a session.23
Important workforce limitations, especially for nephrologists, were also highlighted in this study. The nephrologist density of OSEA was lower than that worldwide overall (5.7 vs. 9.1 pmp10). Efforts to increase the nephrologist workforce in most countries in OSEA are important. In addition, promoting multidisciplinary teams of nurses, pharmacists, dietitians, and other physicians to provide kidney care could help alleviate the shortages in nephrologists. In Indonesia, for example, both internists and general practitioners with at least 3 months of HD training are involved in standard dialysis units.23 Moreover, telemedicine may be another useful tool to diminish the discrepancies in care across the regions. In a study comparing HD care provision of 2 French overseas territories, monthly physical consultation provided to patients on the main island of New Caledonia compared with monthly teleconsultation and quarterly on-site consultation to patients based on Wallis Island showed no differences in dialysis adequacy, vascular access complications, 1- and 6-year survival, and number of patients being transplanted between the 2 cohorts.24
Limitations in infrastructure and workforce are important issues in lower-income countries. Support from higher-income countries has been beneficial in many instances and should be promoted. In Laos PDR, the first dialysis center was established in 1989 with the support of the Vietnamese government and, following its closure from 1993 to 1997, reopened with support from Japan and Thailand.23 Japan has also assisted in the establishment of the Cambodian Association of Nephrology,5 supports activities in arteriovenous fistula creation in Cambodia,25 offers training in dialysis therapy in Myanmar, and created the dialysate purification project in Vietnam, Cambodia, and Myanmar.22,26 Other training programs, such as the ISN’s Continuing Medical Education and Fellowship Programs or visiting Educational Ambassador Program, and collaborations between countries through the Sister Renal Center Program are important initiatives to help close the gaps in CKD care provision across the region.5,27
Little advocacy for kidney disease is seen across OSEA, with just over half the countries reporting advocacy for KF. Increasing the awareness in kidney disease and promoting its prevention and treatment through accessible guidelines and policies with an increase of government prioritization could help mitigate the burden and consequences of KF, particularly in countries with limited resources.
In conclusion, OSEA is a vast and diverse region combining highly populated neighbor Asian countries, small remote island nations, and large countries with much lower population densities. Each country’s socioeconomic situation, geographic location, and funding structure of CKD management impact availability, access, and quality of kidney care. International collaborations and assistance, added to ISN programs, have been successful in improving kidney care in the region and should continue receiving support from the global nephrology community.
Disclosure
DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care, travel sponsorship from Amgen, personal fees from Astra Zeneca, AWAK, and Ono, and grants from National Health and Medical Research Council of Australia, outside the submitted work. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. All the other authors declared no competing interests.
Acknowledgements
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
We thank Kara Stephenson Gehman in International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA) for carefully editing the English text of a draft of this article. We thank Jo-Ann Donner, coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements; and Sandrine Damster, senior research project manager at the ISN, and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support. We also thank the ISN headquarters staff, including the Executive Director, Charu Malik, and the Advocacy team. We also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey.
Footnotes
Table S1. General demographics, economic indicators, and burden of chronic kidney disease in the Oceania and South East Asia countries and territories not participating in the ISN-GKHA survey.
Table S2. Burden of chronic kidney disease and its risk factors in the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Figure S1. Shortage in kidney care providers identified by the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Figure S2. Proportion of patients starting dialysis with different forms of vascular access and adequate education in countries and territory participating in the ISN-GKHA survey.
Figure S3. Availability of services to diagnose and treat complications of kidney failure reported by the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Figure S4. Quality indicators monitored and reported by the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Figure S5. Registry characteristics for the Oceania and South East Asia countries and territory that have reported having ≥1 in the ISN-GKHA survey.
Figure S6. National strategies available in countries reported by the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Figure S7. Population covered under national noncommunicable disease and chronic kidney disease strategies reported by the 15 Oceania and South East Asia countries and territory participating in the ISN-GKHA survey.
Supplementary Appendix. Reference list for annual cost of kidney replacement therapy (for Table 1).
Supplementary Material
References
- 1.World Health Organization South-East Asia. https://www.who.int/southeastasia Available at:
- 2.World Health Organization Western Pacific. https://www.who.int/westernpacific/ Available at:
- 3.Bello A., Levin A., Lunney M. International Society of Nephrology; Brussels, Belgium: 2019. Global Kidney Health Atlas: A Report by the International Society of Nephrology on the Global Burden of End-Stage Kidney Disease and Capacity for Kidney Replacement Therapy and Conservative Care Across World Countries and Regions. [Google Scholar]
- 4.Cho Y., Palmer S., Johnson D.W. Chapter 81. Global considerations in kidney disease: Oceania region. In: Yu A., Chertow G., Luyckx V., editors. Brenner & Rector’s the Kidney. 11th ed. Elsevier; Philadelphia, PA: 2019. pp. 2588–2607. [Google Scholar]
- 5.Kerr P.G., Tran H.T.B., Ha Phan H.A. Nephrology in the Oceania–South East Asia region: perspectives and challenges. Kidney Int. 2018;94:465–470. doi: 10.1016/j.kint.2018.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11:e4–e10 [Google Scholar]
- 7.Central Intelligence Agency The world factbook. Published 2019. https://www.cia.gov/the-world-factbook/ Available at:
- 8.World Health Organization The Global Health Observatory. https://www.who.int/gho/en/ Available at:
- 9.van der Tol A., Lameire N., Morton R. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bello A.K., Levin A., Lunney M. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:15873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 11.GODT Global Observatory on Donation and Transplantation summary. http://www.transplant-observatory.org/summary/ Available at:
- 12.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 14.USRDS. United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
- 15.World Bank GDP ranking, June 2019. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at:
- 16.Agence de la Biomédecine Rapport annuel 2017: réseau epidémiologie et information en néphrologie. https://www.francerein.org/files/France%20Rein/mediatheque/rapport-rein-2017.pdf Avaliable at:
- 17.Ichiho H.M., Roby F.T., Ponausuia E.S. An assessment of non-communicable diseases, diabetes, and related risk factors in the territory of American Samoa: a systems perspective. Hawai’i J Med Public Heal. 2013;72(suppl 1):10–18. [PMC free article] [PubMed] [Google Scholar]
- 18.Krishnan A., Chandra Y., Malani J. End-stage kidney disease in Fiji. Intern Med J. 2019;49:461–466. doi: 10.1111/imj.14108. [DOI] [PubMed] [Google Scholar]
- 19.Farah S.S., Alhaji M.M., Ahmed D. Barriers to kidney transplantation as a choice of renal replacement therapy. Transplant Proc. 2018;50:3165–3171. doi: 10.1016/j.transproceed.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Tang S.C.W., Yu X., Chen H.C. Dialysis care and dialysis funding in Asia. Am J Kidney Dis. 2020;75:772–781. doi: 10.1053/j.ajkd.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Surendra N.K., Manaf M.R.A., Hooi L.S. Cost utility analysis of end stage renal disease treatment in Ministry of Health dialysis centres, Malaysia: hemodialysis versus continuous ambulatory peritoneal dialysis. PLoS One. 2019;14:1–16. doi: 10.1371/journal.pone.0218422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Afiatin, Khoe L.C., Kristin E. Economic evaluation of policy options for dialysis in end-stage renal disease patients under the universal health coverage in Indonesia. PLoS One. 2017;12:1–10. doi: 10.1371/journal.pone.0177436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hyodo T., Fukagawa M., Hirawa N. Present status of renal replacement therapy in Asian countries as of 2016: Cambodia, Laos, Mongolia, Bhutan, and Indonesia. Ren Replace Ther. 2019;5:1–11. [Google Scholar]
- 24.Michel LM, Barroux N, Frimat L, et al. Telenephrology and on-site nephrology: comparable adequate dialysis care to patients living in remote Pacific Islands [epub ahead of print]. J Telemed Telecare. https://doi.org/10.1177/1357633X19896680. Accessed September 18, 2020. [DOI] [PubMed]
- 25.Naganuma T., Takemoto Y. Prospects for vascular access education in developing countries: current situation in Cambodia. Blood Purif. 2017;44:52–54. doi: 10.1159/000479620. [DOI] [PubMed] [Google Scholar]
- 26.Naramura T., Hyodo T., Kokubo K. Dialysis and quality of dialysate in Southeast Asian developing countries. Nephron Extra. 2014;4:64–69. doi: 10.1159/000362454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.International Society of Nephrology Programs. https://www.theisn.org/about-isn/supporting-groups/programs-supporting-groups Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.