Abstract
Provision of adequate kidney care for patients with chronic kidney disease or kidney failure (KF) is costly and requires extensive resources. There is an inequality in the global distribution of wealth and resources needed to provide this care. In this second iteration of the International Society of Nephrology Global Kidney Health Atlas, we present data for countries in Eastern and Central Europe. In the region, the median prevalence of chronic kidney disease was 13.15% and treated KF was 764 per million population, respectively, slightly higher than the global median of 759 per million population. In most countries in the region, over 90% of dialysis patients were on hemodialysis and patients with a functioning graft represented less than one-third of total patients with treated KF. The median annual costs for maintenance hemodialysis were close to the global median, and public funding provided nearly universal coverage of the costs of kidney replacement therapy. Nephrologists were primarily responsible for KF care. All countries had the capacity to provide long-term hemodialysis, and 95% had the capacity to provide peritoneal dialysis. Home hemodialysis was generally not available. Kidney transplantation and conservative care were available across most of the region. Almost all countries had official dialysis and transplantation registries. Eastern and Central Europe is a region with a high burden of chronic kidney disease and variable capacity to deal with it. Insufficient funding and workforce shortages coupled with increasing comorbidities among aging patients and underutilization of cost-effective dialysis therapies such as peritoneal dialysis and kidney transplantation may compromise the quality of care for patients with KF. Some workforce shortages could be addressed by improving the organization of nephrological care in some countries of the region.
Keywords: epidemiology, GKHA, hemodialysis, kidney care funding, kidney transplantation, peritoneal dialysis
Thanks to improvements in community health, people are living longer; however, as the population ages, diseases such as diabetes mellitus and hypertension are becoming increasingly prevalent, contributing to the increased incidence of chronic kidney disease (CKD) and kidney failure (KF).1,2 According to the International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA), the global burden of KF is significant due to high treatment costs and its extensive impacts on patient health and well-being.3 Although a variety of treatment options exist, little is known about how access to treatment and characteristics of treatment delivery (e.g., quality indicators, funding mechanisms) vary around the globe. Moreover, the current scope of kidney-specific health information systems (i.e., registries, electronic health records) also remains unknown. Because health priorities and resources differ worldwide, addressing the global burden of CKD and KF requires analyzing data at the regional level and identifying specific aspects to be targeted in specific contexts.
The region designated as Eastern and Central Europe by the ISN includes countries with different demographic and socioeconomic characteristics. It is a complex region characterized by dynamic changes in demographics and health standards over the past 3 decades,4 including a marked increase in CKD and KF that parallels the aging of the population.1 Major etiologies of CKD in the region are diabetes mellitus (24%), hypertension and vascular disease (23%), and glomerulonephritis (14%),1,4,5 reflecting general patterns in the other ISN regions. Unlike other regions, Balkan endemic nephropathy, a chronic interstitial kidney disease with an associated high risk of urothelial tumors, could also be contributing to the rise in unknown causes of patients with KF in Eastern and Central Europe.4 In addition, a high prevalence of behavioral risk factors, including those affecting the kidneys and the urinary tract, may predispose people in the region to chronic diseases.6 For instance, a recent report on the state of health in the European Union revealed that over one-third of Poland’s chronic disease burden can be attributed to risk factors such as smoking, alcohol consumption, and obesity.7 These risk factors also contribute to the high prevalence of diabetes and atherosclerotic cardiovascular diseases, which are well-recognized risk factors for kidney disease. In addition, high levels of environmental pollution in Eastern and Central Europe affect air quality; notably, air pollution was recently identified as a new risk factor for kidney disease.8,9
The resources available for kidney care and opportunities for nephrologists to engage in high-quality clinical practice are improving throughout Eastern and Central Europe, although they continue to lag behind other parts of Europe.4 Different modalities of kidney replacement therapy (KRT; i.e., dialysis and kidney transplantation) are becoming increasingly available, including conservative care.1,5 Despite these improvements, however, high mortality rates are exposing the limitations of health care systems in many countries, which are struggling to cope with CKD and other emerging public health problems. Although annual reports published by the European Renal Association – European Dialysis and Transplant Association include data from national registries in Eastern and Central Europe,1 much uncertainty remains as to the capacity, accessibility, and quality of KF care in the region and the world at large. In this paper, we leverage data from the second iteration of the ISN-GKHA to report on the capacity, accessibility, and quality of KF care in the ISN region of Eastern and Central Europe. The methodology for this research is described in detail elsewhere.10
Results
Results of this study are presented in tables and figures and broadly summarized into 2 categories: desk research (Tables 111, 12, 13, 14, 15 and 215, 16, 17, 18, 19, 20, Figure 1, Supplementary Table S1, and Supplementary Appendix) and survey administration (Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figure S1).
Table 1.
Demographics, health expenditures, and kidney replacement therapy costs in Eastern and Central European countries that participated in the ISN-GKHA survey11, 12, 13, 14, 15
| Country | World Bank income level | Area (km2) | Total population (2018) | GDP (PPP), $ billiona | Total health expenditures, % of GDPa | Annual cost KRTb (US$) and out-of-pocket cost/% paid by patient from total costc |
||
|---|---|---|---|---|---|---|---|---|
| HD | PD | KT (first year) | ||||||
| Global, median [IQR] | — | — | — | — | 6.5 [4.9–8.8] | 22,617 [14,882–49,690] | 20,524 [14,305–33,905] | 25,356 [15,913–43,901] |
| Eastern and Central Europe, median [IQR] | — | 2,169,274 | 209,784,111 | 81 [34–235] | 6.9 [6.1–8.2] | 20,077 [16,516–27,153] | 21,137 [17,199–25,744] | 37,003 [23,673–76,112] |
| Albania | Upper-middle | 28,748 | 3,057,220 | 36.0 | 6.8 | 15,081/100 | 11,078/100 | —/100 |
| Bosnia and Herzegovina | Upper-middle | 51,197 | 3,849,891 | 44.8 | 9.2 | 17,536/1–25 | 41,029/1–25 | —/0 |
| Bulgaria | Upper-middle | 110,789 | 7,057,504 | 153.5 | 8.2 | 26,598/1–25 | 26,871/0 | —/0 |
| Croatia | High | 56,594 | 4,270,480 | 102.1 | 7.2 | 27,015/100 | 22,644/100 | —/100 |
| Cyprus | High | 9251 | 1,237,088 | 31.8 | 6.9 | —/0 | —/0 | —/0 |
| Czech Republic | High | 78,867 | 10,686,269 | 375.9 | 7.1 | 21,709/0 | 24,296/0 | —/0 |
| Estonia | High | 45,228 | 1,244,288 | 41.7 | 6.7 | 36,349/1–25 | 47,893/1–25 | —/1–25 |
| Hungary | High | 93,028 | 9,825,704 | 289.6 | 7.2 | 12,673/1–25 | 14,155/1–25 | 43,045/1–25 |
| Kosovo | Upper-middle | 10,887 | 1,907,592 | 19.6 | — | —/100 | —/100 | —/51–75 |
| Latvia | High | 64,589 | 1,923,559 | 54.0 | 5.8 | 15,456/0 | 16,187/0 | —/0 |
| Lithuania | High | 65,300 | 2,793,284 | 91.5 | 6.5 | 16,907/1–25 | 20,104/1–25 | —/1–25 |
| Macedonia | Upper-middle | 25,713 | 2,118,945 | 31.0 | 6.1 | 16,133/1–25 | 18,210/1–25 | —/1–25 |
| Moldova | Lower-middle | 33,851 | 3,437,720 | 23.7 | 10.2 | —/100 | —/100 | —/100 |
| Montenegro | Upper-middle | 13,812 | 614,249 | 11.1 | 6.0 | — | — | — |
| Poland | High | 312,685 | 38,420,687 | 1126.0 | 6.3 | 16,899/1–25 | 21,488/1–25 | —/1–25 |
| Romania | Upper-middle | 238,391 | 21,457,116 | 483.4 | 5.0 | 18,445/0 | 14,271/0 | —/0 |
| Serbia | Upper-middle | 77,474 | 7,078,110 | 105.7 | 9.4 | 31,269/— | 18,258/— | 16,385/— |
| Slovakia | High | 49,035 | 5,445,040 | 179.7 | 6.9 | 21,744/0 | 24,617/0 | —/0 |
| Slovenia | High | 20,273 | 2,102,126 | 71.2 | 8.5 | 49,720/0 | 33,644/0 | 109,180/0 |
| Turkey | Upper-middle | 783,562 | 81,257,239 | 2186.0 | 4.1 | 27,290/1–25 | 20,786/1–25 | 30,962/1–25 |
—, Data not reported/unavailable; GDP, gross domestic product; GKHA, Global Kidney Health Atlas; HD, hemodialysis; IQR, interquartile range; ISN, International Society of Nephrology; KRT, kidney replacement therapy; KT, kidney transplants; PD, peritoneal dialysis; PPP, purchasing power parity.
Estimates are in US$ 2017.
Detailed reference list on annual cost of KRT is available in the Supplementary Appendix.
Costs are in US$ 2016.
Table 2.
Kidney replacement therapy services and nephrology workforce statistics in Eastern and Central European countries15, 16, 17, 18, 19, 20
| Country | Treated KF (pmp) |
Prevalence of long-term dialysis (pmp) |
Long-term dialysis centers (pmp) |
Kidney transplantation (pmp) |
Nephrology workforce (pmp) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | Prevalence | HD | PD | Total (HD + PD) | HD | PD | Prevalence | Centers | Nephrologists | Nephrology trainees | |
| Global, median [IQR] | 142 [106–193] | 787 [522–1047] | 310.0 [99.0–597.0] | 25.0 [2–56] | 359.0 [112.0–636.0] | 4.5 [1.0–10.0] | 1.3 [0.4–2.5] | 269.0 [66.0–468.0] | 0.4 [0.2–0.7] | 10.0 [1.2–22.9] | 1.4 [0.3–3.7] |
| East and Central Europe, median [IQR] | 170 [114–190] | 788 [684–999] | 512.0 [300.3–608.8] | 37 [21.4–54.3] | 609.1 [335.0–655.0] | 9.2 [6.5–10.8] | 2.5 [1.3–3.8] | 230.5 [98.4–302] | 0.7 [0.5–0.8] | 25.6 [15.5–36.7] | 3.3 [1.6–4.4] |
| Albania | 90 | 547 | — | — | 335.0 | 3.9 | 0.3 | 80.0 | 0.8 | 54.0 | 4.4 |
| Bosnia and Herzegovina | 108 | 749 | 627.6 | 24.4 | 652.0 | 7.0 | 1.3 | 96.9 | 0.8 | 15.6 | 2.6 |
| Bulgaria | 170 | 627 | 300.3 | 21.4 | 528.0 | 11.4 | 2.3 | 83.0 | 0.4 | 31.9 | 8.5 |
| Croatia | 191 | 1248 | 610.7 | 54.3 | 620.3 | 10.8 | 5.9 | — | 0.9 | 39.8 | 10.0 |
| Cyprus | 236 | — | 21.0 | 2.5 | 23.5 | 4.0 | 4.0 | — | 0.8 | 20.2 | 2.4 |
| Czech Republic | 232 | 1176 | 505.9 | 45.2 | 632.0 | 10.3 | 4.7 | — | 0.5 | 28.1 | 3.7 |
| Estonia | 66 | 720 | 260.7 | 41.8 | 302.5 | 7.2 | 2.4 | 396.0 | 0.8 | 14.5 | 2.8 |
| Hungary | 222 | 999 | 512.0 | 68.3 | 655.0 | 6.5 | 3.1 | 344.0 | 0.4 | 30.5 | 1.0 |
| Kosovo | 190 | 319 | — | — | — | 4.7 | 3.7 | — | — | 22.5 | 3.7 |
| Latvia | 114 | 684 | 156.8 | 49.5 | 275.5 | 12.5 | 2.6 | 285.0 | 0.5 | 23.4 | 1.6 |
| Lithuania | 120 | 796 | 364.6 | 16.8 | 491.2 | 22.2 | 1.1 | 288.0 | 0.7 | 50.1 | 3.9 |
| Macedonia | 181 | 871 | 608.8 | 13.8 | 721.0 | 9.9 | 0.7 | 102.0 | 0.7 | 12.3 | 2.8 |
| Moldova | — | — | 66.6 | 0.5 | 67.1 | 2.9 | — | — | 0.3 | 11.6 | 1.5 |
| Montenegro | — | — | — | — | — | — | — | — | — | — | — |
| Poland | 170 | 788 | 407.0 | 28.8 | 524.0 | 6.5 | 1.3 | 282.0 | 0.6 | 26.0 | 6.5 |
| Romania | 187 | 1143 | 973.2 | 70.2 | 1043.4 | 6.5 | 1.9 | 98.4 | 0.2 | 25.6 | 3.3 |
| Serbia | 100 | 712 | 536.3 | 61.8 | 598.1 | 9.2 | 4.7 | 112.8 | 0.7 | 15.5 | 0.7 |
| Slovakia | 170 | 655 | 532.1 | 37.0 | 620.0 | 13.4 | 3.7 | 302.0 | 0.7 | 36.7 | 3.7 |
| Slovenia | 126 | 1008 | 654.9 | 25.2 | 680.1 | 9.5 | 3.8 | 328.2 | 0.5 | 40.4 | 14.3 |
| Turkey | 146 | 957 | 531.2 | 81.6 | 754.0 | 10.5 | 1.2 | 179.0 | 0.8 | 8.0 | 1.1 |
—, Data not reported/unavailable; HD, hemodialysis; IQR, interquartile range; KF, kidney failure; PD, peritoneal dialysis; pmp, per million population.
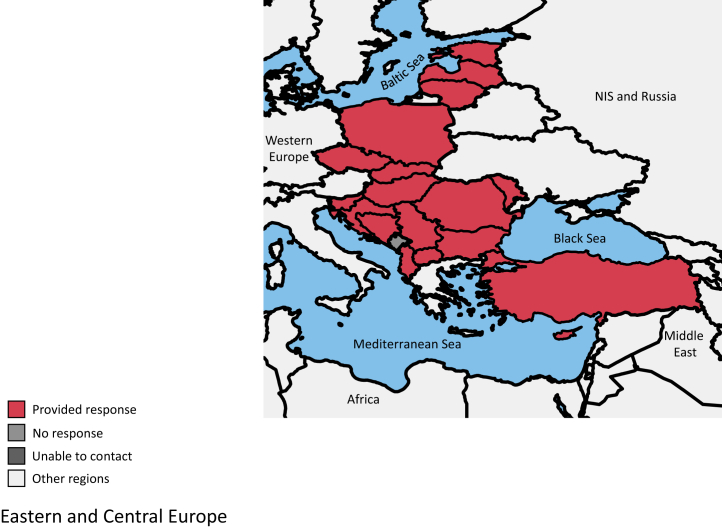
Figure 1.
Eastern and Central Europe countries participating in the International Society of Nephrology Global Kidney Health Atlas survey. NIS, Newly Independent States.
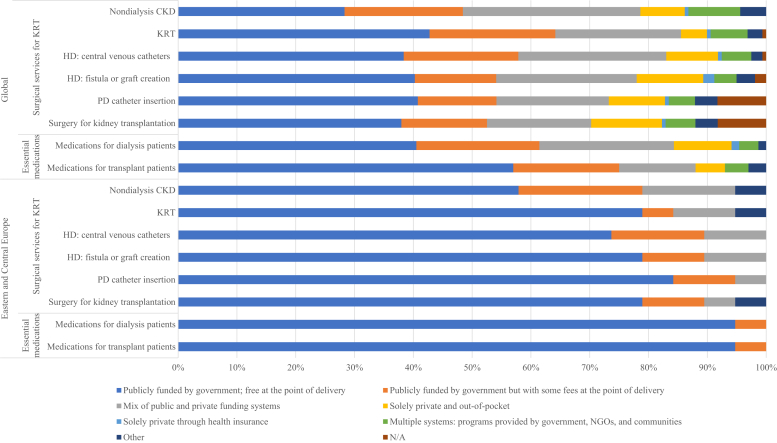
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT) care in Eastern and Central Europe. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; N/A, not provided; NGOs, nongovernmental organizations; PD, peritoneal dialysis.
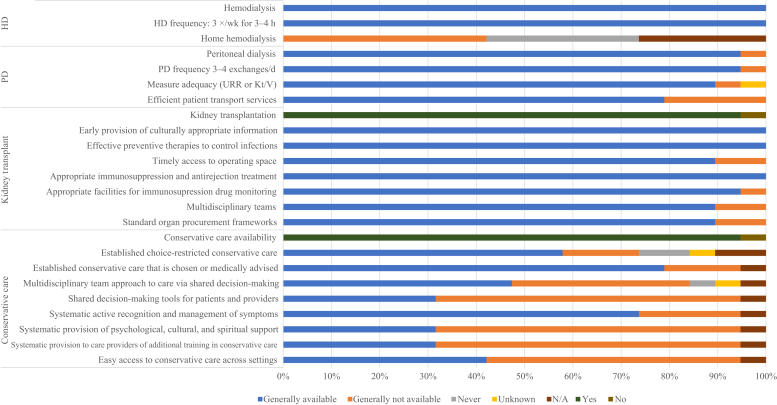
Figure 3.
Availability of choice in kidney replacement therapy or conservative care for patients with kidney failure. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
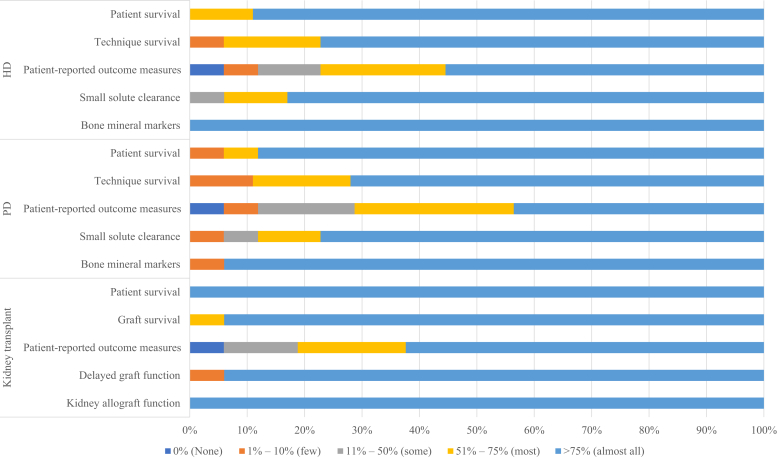
Figure 4.
Quality indicators monitored and reported by countries that participated in the International Society of Nephrology Global Kidney Health Atlas survey. HD, hemodialysis; PD, peritoneal dialysis.
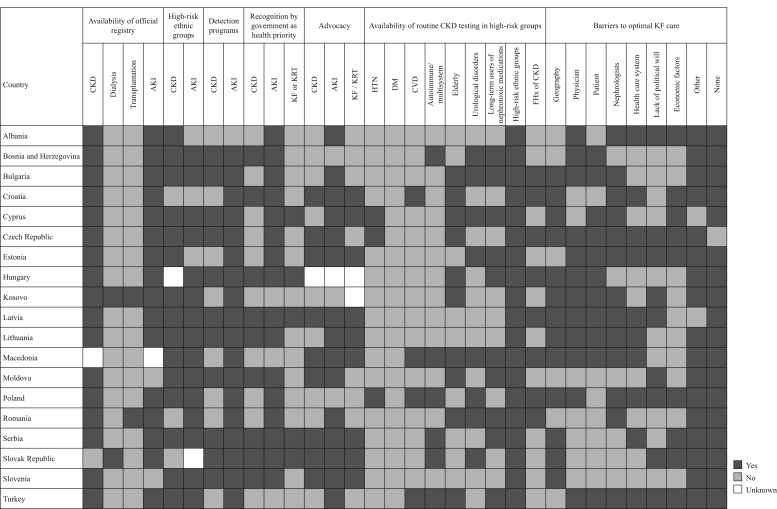
Figure 5.
Country-level scorecard for kidney care in Eastern and Central European countries. AKI, acute kidney injury; CKD, chronic kidney disease; CVD, cardiovascular disease; DM, diabetes mellitus; FHx, family history; HTN, hypertension; KF, kidney failure; KRT, kidney replacement therapy.
Setting
The ISN Eastern and Central Europe region includes 20 countries: Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Cyprus, the Czech Republic, Estonia, Hungary, Latvia, Lithuania, Kosovo, Macedonia, Moldova, Montenegro, Poland, Romania, Serbia, Slovenia, Slovakia, and Turkey. The region covers approximately 2,170,000 square kilometers, equivalent to 0.42% of the world’s surface area (Figure 1) and has a growing population of more than 614 million. Turkey has both the largest surface area and the highest share of the regional population (approximately 40%), followed by Poland and Romania, respectively (Table 1).11 According to World Bank data, the region is mostly developed, with 10 high-income countries, 9 upper-middle income countries, and only 1 lower-middle income country (Table 1).11, 12, 13
Older people comprise an increasing share of the population in the region, although individual countries are at different stages of this demographic transition. For several years now, the average birth rate has consistently been lower than the death rate, leading to a natural decline in the total population. Net migration, which has caused a decline of more than 5% of the regional population, has impacted Bulgaria, Estonia, and Latvia in particular.21 On the other hand, the number of refugees in the region has also increased during the last 4 years, mainly in Turkey.22
Although Eastern and Central Europe has rich ethnic, cultural, and religious diversity, the Human Development Index—a composite indicator of a country’s life expectancy, education index, and gross national income per capita—reflects low variation in quality of life in the region, with scores for all countries ranging between 0.9 and 0.7 (out of a perfect score of 1).23 Despite this relatively homogeneous quality of life, the political turmoil and social unrest that has plagued this region throughout much of its history has contributed to the socioeconomic polarization and inequality, both within and between countries. This is reflected in the ratio of total health expenditures to gross domestic product, which varies considerably across the region, ranging from 5% or less in Romania and Turkey, to more than 8% in Moldova, Serbia, Slovenia, and Bulgaria.13 Since the 1990s, all countries in the region have implemented reforms focused on improving health insurance programs and promoting the more efficient use of health resources. Despite these improvements, however, many organizational and funding problems continue to compromise the quality of nephrological care.
Brief summary of the current state of kidney care in the region
The latest report from the European Renal Association – European Dialysis and Transplant Association Registry and data from national registries in Eastern and Central Europe (e.g., the Polish Renal Replacement Therapy Registry) reveal gradual growth in the incidence and prevalence of treated KF.1,4,5 Hemodialysis (HD) is the primary KRT modality; the data reveal a slow, but insufficient increase in the rate of transplantation, and no growth in the use of peritoneal dialysis (PD).1,4,5 Some inter-regional variations have been observed in workforce capacity, training, and resources dedicated to KF care, as well as the extent of funding coverage available for KRT.4 Here, we report findings for Eastern and Central Europe based on data from the second iteration of the ISN-GKHA, which followed previously published methods.24
Respondents representing 19 of the 20 (95%) countries in the ISN’s Eastern and Central Europe region completed most of the online questionnaire (no response was obtained from Montenegro) (Figure 1). There were 36 respondents from the region, representing a response rate of 80%. Most of the respondents were nephrologists (n = 32; 89%), with responses also from non-nephrologist physicians (n = 1; 3%), administrators (n = 2; 6%), and others (e.g., nurses, community health workers – n = 1; 3%). The total population of participating countries is approximately 614 million, representing 99.7% of the total population in Eastern and Central Europe. Among countries in the region, 9 are classified as high income, 10 are classified as upper-middle income, and 1 is classified as lower-middle income by the World Bank.13 This income level distribution is representative of countries within this ISN region.
Burden of CKD and KF
The average prevalence of CKD in Eastern and Central Europe is 13.15% (95% confidence interval: 8.95, 20.67), ranging from 8.95% in Cyprus to 20.67% in Latvia. The highest proportions of deaths and disability-adjusted life years attributed to CKD are found in Cyprus, Turkey, Serbia, and Montenegro (Supplementary Table S1). The prevalence of CKD risk factors differs across countries in the region: the prevalence of obesity ranges from 32.2% in Turkey to 19.4% in Bosnia and Herzegovina; the prevalence of hypertension ranges from 32.4% in Croatia to 19.8% in Cyprus; and the prevalence of smoking ranges from 31.4% in Macedonia to 15.6% in Albania (Supplementary Table S1).
Data on the prevalence of KF in Eastern and Central Europe are available for all participating countries except Montenegro; partial data are available for Moldova and Kosovo. The median prevalence of treated KF in Eastern and Central Europe is 764 per million population (pmp) (interquartile range [IQR]: 319–1248), slightly higher than the global median of 759 pmp, with a higher prevalence observed in high- and upper-middle-income countries (n = 3 [15.8%]; prevalence greater than 1100 pmp) (Table 2).16, 17, 18, 19, 20 The median number of new cases of treated KF in the region (150 pmp; IQR: 66–236) is higher than the global median (144 pmp), with Cyprus, the Czech Republic, and Hungary experiencing much of this growing burden (236, 232, and 222 pmp, respectively). In a majority of countries (n = 12 [63.2%]; 6 high income, 6 upper-middle income), over 90% of dialysis patients receive HD (Table 2).16, 17, 18, 19, 20 PD is most prevalent in Turkey (81.6 pmp), Romania (70.2 pmp), Hungary (68.3 pmp), and Serbia (61.8 pmp), and least prevalent in Moldova (0.5 pmp), Cyprus (2.5 pmp), and Macedonia (13.8 pmp). Patients living with a functioning graft represent less than one-third of total patients with treated KF, with the highest prevalence in Estonia (396 pmp), Hungary (344 pmp), Slovenia (328 pmp), Poland (305 pmp), and Slovakia (302 pmp) (Table 2).16 The median incidence of deceased donor kidney transplantation is 17.7 pmp, with the highest incidence in the Czech Republic (39.43 pmp), Croatia (36.67 pmp), and Hungary (26.49 pmp), and the lowest incidence in Albania (0 pmp) and Bosnia and Herzegovina (2.63 pmp) (Table 2).16 The median incidence of living donor kidney transplantation is 5.10 pmp, with highest incidence in Turkey (33.15 pmp), Latvia (6.84 pmp), and the Czech Republic (4.81 pmp). Only 5 countries reported data concerning the incidence of pre-emptive transplantations, ranging from 0.7 pmp in Romania to 3.7 pmp in Serbia.16
Health finance and service delivery
Relative to the rest of the world, countries in Eastern and Central Europe generally provide more public funding to cover expenses related to treatment for kidney disease. Medical expenses for nondialysis CKD are covered by public funding with no fees at the point of delivery in 58% of countries in Eastern and Central Europe (vs. 28% of countries worldwide), by public funding with some fees at the point of delivery in 5 countries, and by a combination of public and private funding in 3 countries (Figure 2). Costs of KRT in this region are also covered by public funding with no fees at the point of delivery in 79% of countries (vs. 43% of countries worldwide) (Figure 2). Public funding for KRT is almost universal in Eastern and Central Europe, except in Albania, which has a combination of public and private funding, and Bulgaria where KRT is publicly founded by government with some fees at the point of delivery. Among the 19 participating countries, 16 (80%) reported data about the annual cost of dialysis. In the region, median annual costs (in USD) per person for maintenance HD ($19,510; IQR: $12,673–$49,720) and maintenance PD ($19,800; IQR:$11,078–$47,893) are close to global averages ($22,617 and $20,524, respectively), except in Slovenia ($49,720) and Estonia ($36,300) where costs are significantly higher (Table 1).14,15 The ratio of HD to PD costs also differs by country, ranging from 1.71 in Serbia to 0.43 in Bosnia and Herzegovina.
Four countries reported data on the costs of kidney transplantation. Costs in the first year range from $16,385 in Serbia to $109,180 in Slovenia.15 Annual costs of kidney transplantation in later years also differ, likely due to different reimbursement policies (Table 1).15 There were significant variations in proportion of out-of-pocket costs for KRT in the region. For instance, although the proportion for all KRT types were 100% in Albania (middle-income country), it was 0% for kidney transplantation and 1%–25% for HD or PD in Bosnia and Herzegovina—also a middle-income country. The proportion of out-of-pocket cost tended to be lower as country’s income group increased (Table 1).15
Health workforce for nephrology care
Mirroring the global trend, nephrologists are primarily responsible for KF care in Eastern and Central Europe (n = 19, 95%), with varying support from multidisciplinary teams and primary care physicians (Table 2).15 The median number of nephrologists is 25.3 pmp (IQR: 8 in Turkey to 53.9 in Albania), and the median number of nephrology trainees is 4.12 pmp (IQR: 0.7 in Serbia to 14.27 in Slovenia) in the region; these numbers are significantly higher than median numbers worldwide (9.95 and 1.4 pmp, respectively) (Table 2).15 These numbers seem to be tied with income level: Lithuania, Slovenia, Croatia, and Albania have over 39 nephrologists pmp, whereas Turkey, Moldova, Macedonia, and Estonia have less than 15 nephrologists pmp. Four countries (Bulgaria, Moldova, Romania, and Turkey) reported that primary care physicians play a significant role in providing care for patients with CKD and KF; only Estonia reported the involvement of multidisciplinary teams in care provision. As shown in Supplementary Figure S1, the most commonly reported workforce shortages are for nephrologists (68%, n = 13), surgeons who perform vascular access procedures (68%, n = 13), transplant surgeons (53%, n = 10), and dialysis nurses (53%, n = 10); relatively few countries reported a shortage of interventional radiologists for HD access (n= 6; 32%). Three countries—Romania, Macedonia, and Estonia—reported significant shortages of almost all of the 14 types of care providers listed in Supplementary Figure S1. Interestingly, there are no shortages of dieticians and radiologists/nephrologists, who can perform ultrasound examination, in the region.
Essential medications and health product access for KF care
All countries in the region have the capacity to provide long-term HD (Figure 3). The median number of HD centers is 9 pmp (n = 19, IQR: 2.9–22.2), with the highest densities in Lithuania and Slovakia (22.2 and 13.4 pmp, respectively) and the lowest densities in Moldova and Albania (2.91 and 3.93 pmp, respectively) (Table 2).15 Home HD is generally not available in the region due to a lack of reimbursement rather than technical ability (Figure 3). There are no data concerning the proportion of patients with temporary versus permanent HD vascular access; however, patients tend to start dialysis with permanent access. PD is generally available in 95% of countries (n = 18) (Figure 3). The median number of PD centers in the region is 1.92 pmp (n = 18, IQR: 0.33–5.85), which is close to the global average; Albania, Macedonia, Lithuania, and Turkey have the lowest PD capacity, and PD is not available in Moldova (Table 2).15,16 All countries are able to offer adequate long-term HD frequency (3 times per week; 3–4 hours per treatment) and patient transport services. Eighteen countries (95%) are able to offer adequate PD frequency (3–4 manual exchanges per day or equivalent cycles on automated PD) (Figure 3). These countries also have full capacity to measure PD adequacy and have efficient patient material transport services available. In all surveyed countries, all patients with KF are able to access dialysis, but only a small minority begin with PD (2.5–14.4 pmp). Among the 6 countries with available data, Estonia and Serbia have the highest PD incidence rates (14.4 and 13.9 pmp, respectively) (Table 2).15,16
Kidney transplantation is available across most of the region (n = 18, 94.7%), with a regional median of 0.62 transplant centers pmp (IQR: 0.16–0.94), which is slightly above the global median of 0.42 pmp (IQR: 0.20–0.72) (Table 2).16 Croatia, Turkey, Albania, Cyprus, and Estonia have the highest capacity for transplantation (0.94, 0.82, 0.82, 0.81, and 0.80 transplant centers pmp, respectively), whereas Romania has the lowest capacity (0.16 pmp). In all countries with transplant capacity, both deceased and living donors are used, except in Albania and Macedonia, where only living donors are used. A majority of countries with kidney transplantation available have national transplant waitlists (n = 16, 84.2%); Romania and Bosnia and Herzegovina have regional waitlists only, and data from Kosovo are not available.
Conservative care is available in almost all countries (n = 15, 78%) in Eastern and Central Europe; only 4 countries—Turkey, Latvia, Lithuania, and Macedonia—are unable to provide conservative care when it is medically advised or chosen by the patient (Figure 3). However, this is probably because patients who receive conservative care are transferred to primary care medicine. Among the countries that offer this service, most take a multidisciplinary approach to care via shared decision-making; no country has decision-making tools that are readily available for patients and providers.
KRT quality indicators
All countries are able to provide information about the adequacy of HD, PD, and transplantation. The least-reported indicator of dialysis adequacy is patient-reported outcome measures (Figure 4).
Health information systems, statistics, and national health policies
Almost all countries in Eastern and Central Europe (n = 17, 89.5%) have official dialysis and transplantation registries; Moldova and Slovenia are the only 2 countries with acute kidney injury registries (Figure 5). Kosovo has no registries at all, and Romania only has a dialysis registry; Slovakia has a CKD registry, but no dialysis registry. In general, participation in registries is mandatory. Most registries have national coverage and collect general information on the etiology of kidney disease, dialysis modality, or transplant source; patient outcome measures, as well as data about comorbidities, viral status, and mortality, are more consistently collected in dialysis registries.
Routine testing for kidney disease is available to all patients with diabetes and hypertension in the region, as well as to long-term users of nephrotoxic medications, and patients with a family history of kidney disease. Several countries in the region have CKD detection programs; for example, in 2011, the NATPOL study25,26 actively screened a cohort of over 24,000 patients for CKD in Poland. No country has an acute kidney injury detection program.
A majority of countries have national strategies to improve care for patients with CKD. The existence of advocacy groups in each domain is well established (Figure 5). Only 5 countries (Serbia, Slovenia, Cyprus, Hungary, and Latvia) have no KF/KRT advocacy groups. In contrast, CKD and acute kidney injury advocacy groups are present in just 42% and 10.5% of countries, respectively.
Discussion
Our study reveals important aspects of KF care in the ISN region of Eastern and Central Europe. The prevalence of patients with treated KF varies slightly throughout the region, but generally exceeds the global median.15,16 This is attributable primarily to the aging of the population in the region. According to the WOBASZ Senior Survey, the prevalence of CKD among people in Poland aged 75 years and older is 26.9%; the frequency of CKD increases with age, from 24.2% (75–79 years) to 37.2% (90+ years).27 The majority (70.1%) of people with CKD are in stage G3A.27 In 2018, patients over the age of 65 comprised more than 60% of incident HD patients, and patients over the age of 75 accounted for over 30% of long-term dialysis (PD and HD).5
Given these trends, the life quality of elderly patients, particularly those requiring frequent KRT treatments, has become a central focus. Several initiatives have been undertaken in Eastern and Central Europe (e.g., the QC-QL survey in Poland) to measure how quality of care impacts quality of life.28 Evidence from this study shows that only the highest quality of care increases quality of life. The most visible barriers to achieving this goal are inadequate health care funding (measured as the ratio of health expenditures to gross domestic product) in most countries in the region and poor organization of health systems.29,30 These barriers partly explain regional shortages of KF care providers, especially nephrologists, surgeons who perform HD access procedures, and, to a lesser extent, surgeons who implant PD catheters, all of whom play essential roles in ensuring the quality of KRT. A growing problem in health care more generally is a shortage of nurses, which was also reported by 10 countries in the region. In some respects, the situation could be improved by introducing a coordinated model of nephrological care, similar to the model that will be implemented soon in Poland (NEPHRO-Unit).31 The main idea is to merge various elements of specialized kidney care. It is expected that for the population with CKD stage 3B, the NEPHRO-Unit will accelerate patient access to fistula creation, qualification for transplantation, and access to physiotherapists, dieticians, psychologists, and various other medical specialists experienced in meeting these patients’ specific needs. This new model is expected to create efficiencies at the health system level that will stabilize the prevalence of dialysis, improve predialysis care, increase pre-emptive kidney transplantation, and cut waiting time for kidney transplantation for those already on dialysis. It should also result in increased utilization of PD and home HD practices.31
The disproportionate use of HD rather than PD in the region is striking. Although PD is generally available in 18 of 19 surveyed countries, the median prevalence of PD centers is still lower than the median number in Western Europe.16 A minority of dialysis patients begin treatment with PD, suggesting that this dialysis modality is a highly underutilized resource in the Eastern and Central Europe, especially in lower income countries (e.g., Moldova, Albania, Macedonia) and geographically large countries (e.g., Romania, Turkey).
The disproportionate expansion of HD compared with PD in this region has been described several times in the past, with common barriers being a shortage of trained staff and a lack of financial support and health policies, as well as a lack of support from patients’ families, which is particularly important for elderly or disabled patients.4 Moreover, the limited uptake of PD may be explained in some instances by private sector investments in HD centers; in general, HD is perceived as being easier to implement and likely more profitable procedure than PD.4 Nevertheless, several countries have successfully overcome barriers and implemented PD programs, including Croatia and Serbia.
Financial factors are known to have a significant impact on the use of KRT in all parts of the world; likewise, treating patients with KF has significant economic impacts. Health care coverage data for the region show that the mean cost for HD is 110 euros per week (range: 54–250), or 16,500 euros (8100–37,500) per year; in contrast, the mean cost for PD is 17 euros (range: 9–27) per day, or 24,820 euros (range: 13,140–39,420) per year.4 A partial explanation for these differences may be the variation in price of the fluids and labor costs for dialysis personnel across the region.4
The incidence of deceased donor kidney transplantations remains unsatisfactory, given the number of patients on national waiting lists. Also, the incidence of living donor kidney transplantation in Eastern and Central Europe is much lower than in Western Europe,16 with the exception of Turkey, which can be explained by cultural conditioning.
Another important finding in this region is the large heterogeneity in workforce capacity (both nephrologists and trainees) between upper-middle-income countries and high-income countries.3,4 Although no global recommendation exists for the optimal density of nephrologists, the fact that they are generally responsible for most aspects of KF care (a condition required by national health care payers in many countries in the region) highlights the importance of having an adequate number of training centers and sufficient workforce capacity and distribution to coordinate care.
Almost all countries in the region have official national registries, but only for HD and PD patients. Only 1 country has a CKD registry; most countries do not have CKD registries due to extremely high costs and extensive organizational problems. Most countries reported aggregate data, yet only data collected at the individual level can provide a precise picture of the health of patients with KF. KRT advocacy groups provide valuable support for patients who are starting KRT, especially after kidney transplantation. Targeted CKD detection programs, despite some successful initiatives such as NATPOL in Poland,25 are still too small and restricted by available funds.
In conclusion, the region of Eastern and Central Europe has a high burden of kidney disease and variable capacity to deal with it. Insufficient funding and workforce shortages coupled with the increasing prevalence of comorbidities among aging patients and underutilization of cost-effective dialysis therapies such as PD and kidney transplantation often contribute to suboptimal quality of life and health outcomes for patients with KF. Some of these barriers to optimal care could be overcome by improving the organization of nephrological care in particular countries.
Disclosure
DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care; travel sponsorship from Amgen; personal fees from Astra Zeneca, AWAK, and Ono; and grants from National Health and Medical Research Council of Australia, outside the submitted work. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. All the other authors declared no competing interests.
Acknowledgments
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
We thank Kara Stephenson Gehman in International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA) for carefully editing the English text of a draft of this manuscript. We thank Jo-Ann Donner, Coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements, Sandrine Damster, Senior Research Project Manager at the ISN, and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support. We also thank the ISN headquarters staff including the Executive Director, Charu Malik, and the Advocacy team. We also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey.
Footnotes
Table S1. Burden of chronic kidney disease and its risk factors in Eastern and Central European countries participating in the ISN-GKHA survey.
Figure S1. Shortages in kidney failure providers identified by responding countries in Eastern and Central Europe.
Supplementary Appendix. Reference list for annual cost of kidney replacement therapy (for Table 1).
Supplementary Material
References
- 1.Kramer A., Pippias M., Noordzij M. The European Renal Association—European Dialysis and Transplant Association (ERA-EDTA) Registry Annual Report 2016: a summary. Clin Kidney J. 2019;12:702–720. doi: 10.1093/ckj/sfz011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luyckx V.A., Tonelli M., Stanifer J.W. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ. 2018;96:414–422. doi: 10.2471/BLT.17.206441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bello A., Levin A., Lunney M. Global Kidney Health Atlas: a report by the International Society of Nephrology on the Global Burden of End-stage Kidney Disease and Capacity for Kidney Replacement Therapy and Conservative Care across World Countries and Regions. Brussels, Belgium: International Society of Nephrology. 2019 [Google Scholar]
- 4.Spasovski G., Rroji M., Vazelov E. Nephrology in the Eastern and Central European region: challenges and opportunities. Kidney Int. 2019;96:287–290. doi: 10.1016/j.kint.2019.02.040. [DOI] [PubMed] [Google Scholar]
- 5.Dębska-Ślizień A.R.B., Rutkowski P. Actual condition of renal replacement therapy in Poland in year 2018. Nefrol Dial Pol. 2019;23:113–122. [Google Scholar]
- 6.Pavlović N.M. Balkan endemic nephropathy-current status and future perspectives. Clin Kidney J. 2013;6:257–265. doi: 10.1093/ckj/sft049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.European Commission Country Health Profiles; 2019. https://ec.europa.eu/health/state/country_profiles_en Available at:
- 8.European Environment Agency Premature deaths attributable to air pollution; 2016. https://www.eea.europa.eu/media/newsreleases/many-europeans-still-exposed-to-air-pollution-2015/premature-deaths-attributable-to-air-pollution Available at:
- 9.Afsar B., Elsurer Afsar R., Kanbay A. Air pollution and kidney disease: review of current evidence. Clin Kidney J. 2019;12:19–32. doi: 10.1093/ckj/sfy111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11 e4–e10. [Google Scholar]
- 11.Central Intelligence Agency The world factbook. https://www.cia.gov/the-world-factbook/ Available at: Published 2019. Accessed March 11, 2021.
- 12.World Health Organization The Global Health Observatory; 2019. https://www.who.int/gho/en/ Available at:
- 13.World Bank GDP ranking; June 2019. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at:
- 14.van der Tol A., Lameire N., Morton R.L. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bello A.K., Levin A., Lunney M. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 16.ERA-EDTA Registry ERA-EDTA Registry Annual Report 2017. https://www.era-edta.org/en/registry/ Available at:
- 17.GODT Global Observatory on Donation and Transplantation database. http://www.transplant-observatory.org/data-charts-and-tables/ Available at:
- 18.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polish Transplant Coordinating Centre Information Bulletin of the Organizational and Coordination Center for Transplantation "Poltransplant"; 2019. http://www.poltransplant.org.pl/biuletyny.html Available at:
- 20.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2018. 2018 USRDS Annual Data Report: epidemiology of kidney disease in the United States. [Google Scholar]
- 21.King R., Lulle A. Research on migration: facing realities and maximising opportunities: a policy review. http://ec.europa.eu/research/bitlys/migration/migration-realities-opportunities.html Available at:
- 22.Gursu M., Arici M., Ates K. Hemodialysis experience of a large group of Syrian refugees in Turkey: all patients deserve effective treatment. Kidney Blood Press Res. 2019;44:43–51. doi: 10.1159/000498832. [DOI] [PubMed] [Google Scholar]
- 23.United Nations Development Programme (UNDP) Human Development Data (1990-2018); 2018. http://hdr.undp.org/en/data Available at:
- 24.Bello A.K., Johnson D.W., Feehally J. Global Kidney Health Atlas (GKHA): design and methods. Kidney Int Suppl. 2017;7:145–153. doi: 10.1016/j.kisu.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suligowska K., Gajewska M., Stokwiszewski J. Insufficient knowledge of adults in Poland on criteria of arterial hypertension and its complications—results of the NATPOL 2011 Survey. Arterial Hypertension. 2014;18:9–18. [Google Scholar]
- 26.Zdrojewski Ł., Zdrojewski T., Rutkowski M. Prevalence of chronic kidney disease in a representative sample of the Polish population: results of the NATPOL 2011 survey. Nephrol Dial Transpl. 2016;31:433–439. doi: 10.1093/ndt/gfv369. [DOI] [PubMed] [Google Scholar]
- 27.Zdrojewski Ł., Król E., Rutkowski B. Chronic kidney disease in Polish elderly population aged 75+: results of the WOBASZ Senior Survey. Int Urol Nephrol. 2017;49:669–676. doi: 10.1007/s11255-016-1477-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rutkowski B., Nowaczyk R., Rutkowski P., Mierzicki P. Results of QC vs QL study (quality of care vs quality of life) 2006-2009. The way of providing hemodialysis and a concomitant therapy. Przegl Lek. 2011;68:1170–1178. [PubMed] [Google Scholar]
- 29.White S.L., Chadban S.J., Jan S. How can we achieve global equity in provision of renal replacement therapy? Bull World Health Organ. 2008;86:229–237. doi: 10.2471/BLT.07.041715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang Y.T., Hwang J.S., Hung S.Y. Cost-effectiveness of hemodialysis and peritoneal dialysis: a national cohort study with 14 years follow-up and matched for comorbidities and propensity score. Sci Rep. 2016;6:30266. doi: 10.1038/srep30266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gellerta R., editor. Coordinated care over patients with chronic kidney disease. NEFRON Nephrology Section of the Polish Medicine Chamber of Commerce (Sekcja Nefrologiczna Izby Gospodarczej Medycyna Polska) 2018. Warsaw. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.