Abstract
Kidney failure (KF) is a public health problem in all regions of the world. We aim to provide comprehensive information regarding the disease burden of KF and capacity for providing optimal care in the International Society of Nephrology North and East Asia region based on data from the International Society of Nephrology Global Kidney Health Atlas project. Seven of eight jurisdictions participated, and wide variation was found in terms of KF burden and care capacity. Prevalence of long-term dialysis ranged from 88.4 per million population in mainland China to 3251 per million population in Taiwan. Hemodialysis was the predominant modality of dialysis in all jurisdictions, except for Hong Kong, where peritoneal dialysis (PD) was much more prevalent than hemodialysis. All jurisdictions provided public funding for kidney replacement therapy (dialysis and transplantation). Although the frequency and duration of hemodialysis followed a standard pattern in all investigated jurisdictions, the density of nephrologists and kidney replacement therapy centers varied according to income level. Conservative care, whether medically advised or chosen by patients, was available in most jurisdictions. All jurisdictions had official registries for KF and recognized KF as a health priority. These comprehensive data provide information about the burden of KF and capacity to provide optimal care in North and East Asia, which varied greatly across jurisdictions in the region.
Keywords: end-stage kidney disease, epidemiology, Global Kidney Health Atlas, kidney failure, kidney replacement therapy, North and East Asia
The area identified as the North and East Asia region by the International Society of Nephrology (ISN) comprises 8 jurisdictions (i.e., countries and semiautonomous regions—China, Hong Kong [China], Macao [China], Taiwan [China], Japan, Mongolia, North Korea, South Korea) with a population of more than 1.6 billion. Economic development varies substantially in the region, including both well-developed and developing jurisdictions. The world’s most populous country, China, is also located in the region. After 4 decades of rapid economic development, China is now an upper-middle income country, but it still faces challenges associated with social and economic inequality across rural and urban areas and different geographic regions. The aging population in most jurisdictions in North and East Asia is an important factor driving the increasing incidence of kidney failure (KF).1, 2, 3, 4, 5 In developed jurisdictions, diabetes and hypertension are the leading causes of chronic kidney disease (CKD) and KF alike.1, 2, 3, 4, 5 However, in low- and middle-income countries, evidence has shown that the predominant cause of CKD and KF is transitioning from glomerulonephritis to metabolic disorders, mirroring the trend in high-income countries.6,7
Patients with KF typically need expensive kidney replacement therapy (KRT; i.e., dialysis and/or kidney transplantation) to sustain life. The availability, affordability, accessibility, and quality of KRT and conservative care vary across jurisdictions in North and East Asia. An extensive body of evidence has accumulated, thanks to the routine data collection efforts of national CKD/KF registries. However, effective health information systems are not always available, especially in developing countries. Comprehensive information regarding the disease burden of KF and capacity to provide the optimal KF care is still lacking in the region. The aim of the ISN-Global Kidney Health Atlas (ISN-GKHA) project is to provide a high-level overview of the burden of KF, the current state of KF care, and a comparative analysis of the capacity to deliver KF care.8,9 Here, we present findings for the ISN’s North and East Asia region based on data collected for the second iteration of the ISN-GKHA. The methodology for this research is described in detail elsewhere.10
Results
The results of this study are presented in the tables and figures and are broadly summarized into 2 categories: desk research (Tables 111, 12, 13, 14, 29,11, 12, 13, 14, 15, and 316, 17, 18, 19, 20, 21; Figure 1; Supplementary Table S1; and Supplementary Appendix) and survey administration (Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figures S1–S3).
Table 1.
| Country | World Bank income level | Area (thousand km2) | Total population (2018, millions) | GDP (PPP), $ billiona | Total health expenditures, % of GDPa |
Government expenditure % of total expenditure on healtha | Out-of-pocket expenditure % of private expenditure on healtha |
|---|---|---|---|---|---|---|---|
| North and East Asia median [IQR] | — | 11,796.4 | 1622.1 | 822 [56–3739] | 6.2 [4.5–9.2] | — | — |
| China | Upper-middle | 9597.0 | 1384.7 | 23,210.0 | 5.0 | 59.8 | 32.4 |
| Hong Kong (China) | High | 1.1 | 7.2 | 455.9 | 2.4 | — | — |
| Japan | High | 377.9 | 126.2 | 5443.0 | 10.9 | — | 13.1 |
| South Korea | High | 99.7 | 51.4 | 2035.0 | 7.4 | 56.4 | 36.8 |
| Macao (China) | High | 0.0 | 0.6 | 71.8 | — | — | — |
| Mongolia | Lower-middle | 1564.1 | 3.1 | 39.7 | 3.9 | 52.2 | 39.3 |
| Taiwan (China) | High | 36.0 | 23.6 | 1189.0 | — | — | — |
—, Data not reported/unavailable; GDP, gross domestic product; IQR, interquartile range; PPP, purchasing power parity.
Estimates are in $US 2017.
Table 2.
Burden of kidney failure, capacity for dialysis and kidney transplantation, and nephrology workforce in North and East Asia9,11, 12, 13, 14, 15
| Country | Treated KF (pmp) |
Prevalence of long-term dialysis (pmp) |
Long-term dialysis centers (pmp) |
Kidney transplantation (pmp) |
Nephrology workforce (pmp) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | Prevalence | HD | PD | Total (HD + PD) | HD | PD | Incidence | Prevalence | Centers | Nephrologists | Nephrology trainees | |
| North and East Asia Median [IQR] | 311.0 [296.0–493.0] | 2599.0 [1816.0–3392.0] | 1661.4 [646.2–2127.6] | 107.5 [42.0–179.5] | 1789.7 [723.7–2271.6] | 14.2 [1.8–34.8] | 1.9 [1.6–4.0] | 6.7 [6.5–13.1] | 141.0 [67.0–352.0] | 0.6 [0.4–1.3] | 19.5 [9.7–54.6] | 3.2 [1.9–5.9] |
| China | — | — | 76.3 | 12.1 | 88.4 | 0.5 | 0.4 | 6.5 | — | 0.4 | 5.8 | 1.1 |
| Hong Kong (China) | 171 | 1315 | 165.8 | 531.0 | 818.0 | 1.8 | 1.9 | — | 519 | 0.6 | 18.0 | 2.1 |
| Japan | 296 | 2599 | 2148.4 | 71.9 | 2532.0 | 34.8 | 4.0 | 13.1 | 67 | 1.1 | 79.3 | 5.9 |
| South Korea | 311 | 1816 | 1216.0 | 143.0 | 1464.0 | 14.2 | 1.9 | — | 352 | 1.2 | 19.5 | 1.9 |
| Macao (China) | — | — | — | — | — | 5.0 | 1.7 | — | — | 1.7 | 25.6 | 9.1 |
| Mongolia | — | — | — | — | — | 16.1 | 1.6 | 6.7 | — | 0.3 | 9.7 | 3.2 |
| Taiwan (China) | 493 | 3392 | 2106.8 | 216.0 | 3251.0 | 35.4 | 5.4 | — | 141 | 0.4 | 54.6 | 3.9 |
—, Data not reported/unavailable; HD, hemodialysis; IQR, interquartile range; KF, kidney failure; PD, peritoneal dialysis; pmp, per million population.
Table 3.
Annual cost of kidney replacement therapya and out-of-pocket cost (% paid by patient from total cost)b in North and East Asia16, 17, 18, 19, 20, 21
| Country | HD/% | PD/% | Kidney transplantation, % |
HD/PD ratio | |
|---|---|---|---|---|---|
| First year | Later years | ||||
| North and East Asia median [IQR] | 28,846 [21,215–43,954] | 15,265 [11,661–36,717] | 43,374 [25,356–50,613] | — | 1.9 |
| China | 22,617/1–25 | 8122/1–25 | 25,356/1–25 | — | 2.8 |
| Hong Kong (China) | 35,074/1–25 | 15,199/1–25 | —/1–25 | — | 2.3 |
| Japan | 52,834/1–25 | 58,103/1–25 | 43,374/1–25 | 22,886 | 0.9 |
| South Korea | 19,812/1–25 | 15,330/1–25 | 50,613/1–25 | 35,765 | 1.3 |
| Macao (China) | —/1–25 | —/1–25 | —/1–25 | — | — |
| Mongolia | —/1–25 | —/1–25 | —/1–25 | 5392 | — |
| Taiwan (China) | —/1–25 | —/1–25 | —/1–25 | — | — |
—, Data not reported/unavailable; HD, hemodialysis; IQR, interquartile range; PD, peritoneal dialysis.
Detailed reference list on annual cost of KRT is available in the Supplementary Appendix.
Cost is in $US 2016.
Figure 1.
Countries in North and East Asia participating in the International Society of Nephrology Global Kidney Health Atlas survey. NIS, Newly Independent States.
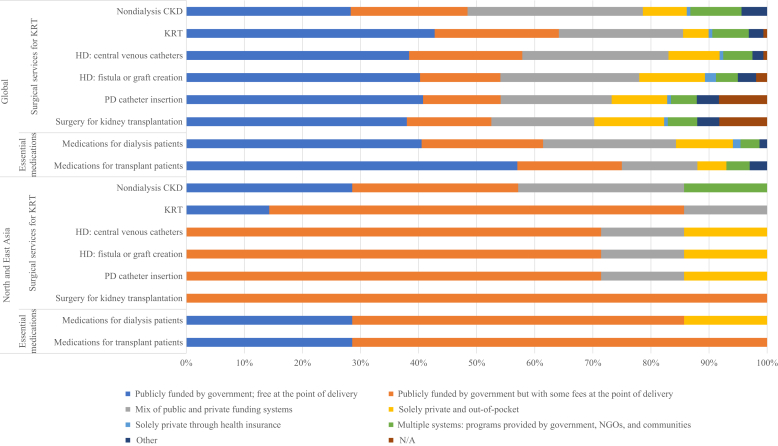
Figure 2.
Funding for kidney replacement therapy, nondialysis chronic kidney disease (CKD), and medications for dialysis and transplantation patients. Values represent absolute number of countries in each category, expressed as a percentage of total number of countries. HD, hemodialysis; KRT, kidney replacement therapy; N/A, not provided; NGOs, nongovernmental organizations; PD, peritoneal dialysis.
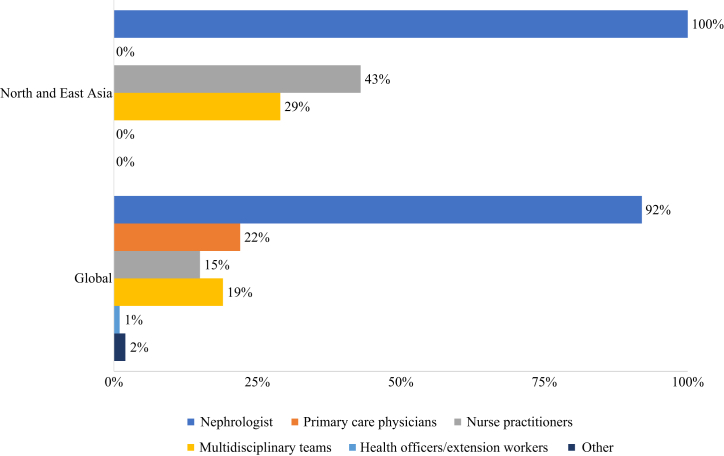
Figure 3.
Providers primarily responsible for kidney failure care.
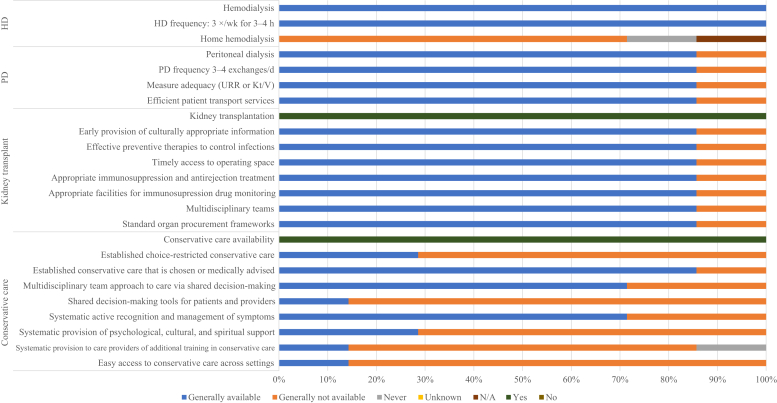
Figure 4.
Availability of choice in kidney replacement therapy or conservative care for patients with kidney failure. Values represent absolute number of countries in each category, expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
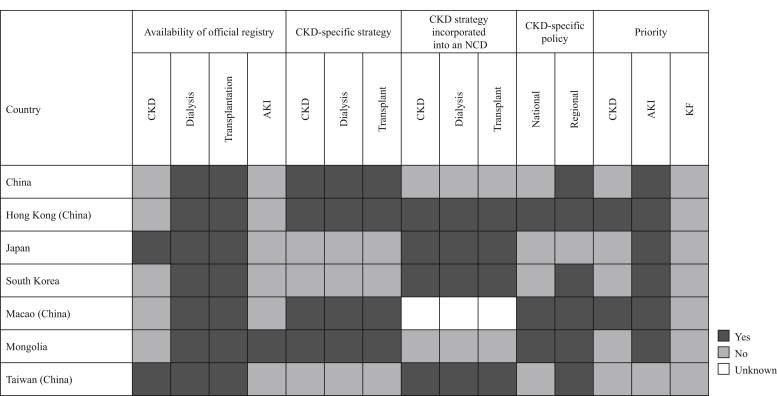
Figure 5.
Country scorecard for kidney care in the International Society of Nephrology North and East Asia region for registries, strategies, policies, and health priority designations. AKI, acute kidney injury; CKD, chronic kidney disease; KF, kidney failure; NCD, noncommunicable disease.
Setting
North and East Asia covers an area of 11.8 million square kilometers and comprises more than one-fifth of the world’s population (1.62 billion).22 The region includes mainland China, Hong Kong, Macao, Taiwan, South Korea, North Korea, Japan, and Mongolia. Although ethnicity is highly homogeneous across the jurisdictions, the levels of economic development differ considerably. Among the jurisdictions, Hong Kong, Japan, Macao, South Korea, and Taiwan belong to the high-income group, as defined by the 2018 World Bank ranking. Mainland China is classified as an upper-middle income country, Mongolia is classified as a lower-middle income country, and North Korea is classified as a low-income country.23 Consistent with income level, Hong Kong, Japan, and South Korea have high scores on the Human Development Index, a composite measure of life expectancy, education, and gross national income per capita (0.939, 0.915 and 0.906 in 2018, respectively), indicating a high quality of life in those jurisdictions. Mainland China and Mongolia have moderately high scores (0.758 and 0.735 in 2018, respectively).24
Characteristics of participating countries
Twenty-one respondents representing 7 of the 8 jurisdictions in North and East Asia and 98.4% of the region’s total population (1596.7 million) completed the online questionnaire; stakeholders in North Korea did not participate (Figure 1). The respondents included 20 nephrologists (95%) and 1 non-nephrologist physician (5%), with an overall response rate of 77.8%. Measured as a proportion of gross domestic product (GDP), total health expenditures were highest in Japan (10.9%) and lowest in Mongolia (3.9%) (Table 1).11, 12, 13, 14
Burden of CKD and KF in North and East Asia
The prevalence of CKD in North and East Asia ranged from 8.68% in Mongolia to 17.62% in Japan. The proportions of death and disability adjusted life years attributable to CKD were highest in Taiwan (3.75% and 2.53%, respectively) and lowest in Mongolia (1.55% and 1.25%, respectively). Regarding the risk factors associated with CKD, there was a disproportionately higher prevalence of obesity (19.6%) and high blood pressure (29.0%) in Mongolia than in other jurisdictions in North and East Asia. The prevalence of smoking was consistent across the jurisdictions, with the exception of Taiwan, where the prevalence was significantly lower (11.5%) (Supplementary Table S1).
Taiwan bore the highest burden of treated KF, with a prevalence of 3392 per million population (pmp), followed by Japan and South Korea (2599 pmp and 1816 pmp, respectively). Long-term dialysis accounted for the majority of treated KF (>95% in Taiwan and Japan, 80.6% in South Korea, and 62.2% in Hong Kong). The prevalence of long-term dialysis was remarkably lower in mainland China (88.4 pmp) than in other jurisdictions (range, 818 to 3251 pmp). HD was the predominant type of dialysis in all jurisdictions except for Hong Kong, where the prevalence of PD was much higher than that of HD (531 vs. 165.8 pmp). Regarding kidney transplantation, the highest prevalence was in Hong Kong (497 pmp), and the lowest prevalence was in Japan (67 pmp) (Table 2).11, 12, 13, 14 No relevant data were available for the prevalence of kidney transplantation in mainland China.
Health finance and service delivery
In all jurisdictions except for Hong Kong, KRT was funded by the government, either with or without fees at the point-of-care delivery. In Hong Kong, KRT costs were covered by a combination of public and private funding systems. Public funding covered medication costs for dialysis patients in all jurisdictions except for Mongolia, where costs were covered by private systems or paid out of pocket. Regarding nondialysis CKD, Japan, South Korea, Mongolia, and Taiwan provided public funding for therapy with no fees (in Mongolia and Taiwan) or some fees (in Japan and South Korea) at the point of delivery. By contrast, a combination of public and private funding systems covered therapy costs in mainland China and Hong Kong, and multiple systems were used in Macao (Figure 2).
Annual costs of HD and PD were highest in Japan (52,834 and 58,103 $US per person, respectively) and lowest in mainland China (22,617 and 8122 $US per person, respectively); no corresponding data were available in Macao, Mongolia, and Taiwan. HD costs more than PD in mainland China, Hong Kong, and South Korea, whereas the reverse was true in Japan. Only 3 jurisdictions reported data on the costs of kidney transplantation, with South Korea reporting the highest costs, both in the first year (50,613 $US) and in later years (35,765 $US) (Table 3).16, 17, 18, 19, 20, 21
Health workforce for nephrology care
Nephrologists were primarily responsible for KF care in North and East Asia (100% in all 7 jurisdictions), with support from nurse practitioners/specialized nurses in mainland China, Hong Kong, and Japan, and from multidisciplinary teams in Japan and Taiwan. These findings mirrored the overall pattern worldwide (Figure 3). High-income jurisdictions reported more nephrologists and nephrology trainees (e.g., 79.26 pmp in Japan and 54.6 pmp in Taiwan) than did middle income jurisdictions (e.g., 5.78 pmp in mainland China and 9.67 pmp in Mongolia) (Table 2).9 A shortage of KF care providers was more commonly reported in high-income jurisdictions than in middle-income jurisdictions. For example, a shortage of nephrologists was reported in Japan, South Korea, Macao, and Taiwan, but not in mainland China, Hong Kong, and Mongolia (Supplementary Figure S1).
Essential medications and health product access for KF care
HD was generally available in all jurisdictions in North and East Asia, and all jurisdictions followed the standard pattern of frequency and duration (i.e., treatment 3 times per week for 3 or 4 hours). However, home HD was generally not available in most jurisdictions (mainland China, Hong Kong, Japan, South Korea, and Taiwan) and was never available in Macao (Figure 4). Taiwan and Japan had the highest densities of HD centers (35.36 and 34.84 pmp, respectively), and mainland China and Hong Kong had the lowest densities (0.54 and 1.80 pmp, respectively) (Table 2).11,14 Most patients (51%–75%) began dialysis with a functioning vascular access (arteriovenous fistula or graft) in mainland China, Japan, and Mongolia, whereas a lower proportion (11$–50%) did so in Hong Kong, South Korea, Macao, and Taiwan.
PD was also generally available in all jurisdictions. All jurisdictions except Macao reported adequate dialysis frequency (3–4 manual exchanges per day or equivalent cycles on automated PD), measurement of adequacy via measurement of urea reduction ratio (URR) or Kt/V, and the availability of efficient patient transport services (Figure 4). Similar to the statistics for HD centers, Taiwan and Japan had the highest densities of PD centers (5.44 and 3.96 pmp, respectively) and mainland China had the lowest (0.36 pmp) (Table 2).12
Kidney transplantation was generally available across all jurisdictions (Figure 4). The density of centers for kidney transplantation was >1 pmp in Japan, South Korea, and Macao (1.14, 1.23, and 1.65 pmp, respectively), in contrast to mainland China and Mongolia, where densities were only 0.36 pmp and 0.32 pmp, respectively (Table 2).11,15 All jurisdictions had transplantation waitlists and used kidneys from a combination of live and deceased donors except for Macao, where only kidneys from live donors were used (Supplementary Figure S2). All jurisdictions except for Macao reported general availability of standard organ procurement frameworks, multidisciplinary teams to support patients, appropriate facilities for immunosuppression drug monitoring, appropriate immunosuppression and antirejection treatment, timely access to operating space, effective preventive therapies to control infections, and early provision of culturally appropriate information (Figure 4).
Conservative care, whether medically advised or chosen by the patient, was generally available in all jurisdictions except Macao, where it was generally not available. Choice-restricted conservative care was generally available in mainland China and Hong Kong. Few jurisdictions reported the general availability of shared decision-making tools for patients and providers (Hong Kong), systematic provision of psychological, cultural, and spiritual support (Hong Kong and Japan), systematic provision of additional training to care providers (Hong Kong), and easy access to conservative care across settings (Hong Kong). By contrast, most jurisdictions (mainland China, Hong Kong, Japan, South Korea, and Taiwan) reported general availability of a multidisciplinary team approach to care via shared decision making and systematic active recognition and management of symptoms (Figure 4).
Health information systems, strategies, policies, health priorities, and barriers
All jurisdictions in North and East Asia had official registries for dialysis and transplantation, whereas only Japan and Taiwan had official CKD registries, and only Mongolia had an official AKI registry. Most jurisdictions had strategies for CKD that covered care for non–dialysis-dependent CKD, long-term dialysis, and kidney transplantation. Japan, South Korea, and Taiwan had specific CKD strategies, whereas CKD strategies in mainland China and Mongolia were incorporated into general noncommunicable disease strategies. Mainland China, Japan, South Korea, and Taiwan had CKD-specific policies at the national level, and Japan also had CKD-specific policies at the regional level. All jurisdictions recognized KF as a health priority, most jurisdictions (except Hong Kong and Macao) recognized CKD as a health priority, and only Taiwan recognized AKI as a health priority (Figure 5). The most commonly cited barriers to optimal KF care were geographic characteristics and physicians (both 57.1%), followed by individual patients, nephrologists, the health care system, and economic factors (all 42.9%) (Supplementary Figure S3).
Discussion
The burden of KF was high in high-income jurisdictions in North and East Asia but comparatively lower in middle-income jurisdictions. All jurisdictions provided public funding for KRT and were able to follow standard patterns of dialysis. However, the capacity for KRT varied across the jurisdictions in terms of the densities of dialysis/transplantation centers and the nephrology workforce. Conservative care, whether medically advised or chosen by patients, was widely available, and the choice-restricted form also existed in some jurisdictions. KF has been recognized as a health priority by all jurisdictions in the region, and specific strategies and policies regarding KF and/or CKD care have been widely implemented.
The burden of KF was high among the developed jurisdictions in North and East Asia, particularly in Taiwan and Japan, which had the highest incidence and prevalence of KF worldwide.11 Population aging and the high prevalence of obesity, hypertension, and diabetes are believed to be main contributors to the high burden of KF.1,25 By contrast, data from the ISN-GKHA survey showed that mainland China had a much lower burden of KF. However, several recent studies have provided further information about the epidemiology of KF in this populous country. In 2015, based on data from the national insurance database, the China Kidney Disease Network (CK-NET) reported a prevalence of HD and PD of 402.18 pmp and 39.95 pmp, respectively, and an incidence of dialysis of 122.19 pmp, all of which were relatively higher than the figures reported in the current study. However, selection bias resulting from the representativeness of the insurance database should be considered.26 In addition, the incidence and prevalence of KF may be even higher in big cities in mainland China. For example, Chen and colleagues reported that the incidence and prevalence of HD in Shanghai in 2014 were 128.1 pmp and 898.2 pmp, respectively, based on data from the local HD registry. However, sufficient facility and workforce capacity in the city and significant support from the health insurance system may partly explain the high disease burden by fulfilling the need for KRT.27 Whereas most cases of KF in developed jurisdictions in North and East Asia are associated with diabetes, the cause of KF is transitioning from glomerulonephritis to diabetic kidney disease in mainland China. On the basis of the national hospitalization database, the CK-NET group reported that the percentage of CKD cases related to diabetes exceeded that of CKD related to glomerulonephritis in 2011, and the gap between the 2 causes has gradually increased since then.6 Among patients receiving HD, the local HD registry in Beijing also reported that diabetes had replaced glomerulonephritis as the leading cause of incident cases since 2011.28 According to data from national KF registries, this trend has been observed in Korea since 1994, in Japan since 1997, and in Taiwan since 2001.3,4,29 Cumulatively, the evidence suggests that the disease burden of KF is likely to continue to increase in the future. Likewise, a recent systematic review projected an increasing burden of KF in the next decade, with the greatest contribution from Asia.30
Public financial support is essential to guarantee access to KRT for patients with KF, especially those living in low- and middle-income countries who likely cannot afford to cover the high costs of KRT out of pocket. Fortunately, all jurisdictions in North and East Asia provided public funding to cover the costs of KRT. Interestingly, this may be another factor driving the increase in the reported incidence and prevalence of KF in the region. For example, in 1995, Taiwan implemented a national health insurance plan, which covered all KRT costs; data for that year showed a sharp increase in both the incidence and the prevalence of KF.4 In the current ISN-GKHA survey, most of the jurisdictions reported an out-of-pocket fee at the point-of-care delivery, and in Mongolia, medications associated with KRT were covered entirely by private funding. These funding structures may create obstacles to universal access to KRT for patients. According to the report by CK-NET, the national Urban Basic Medical Insurance system, which is the predominant health insurance program in urban areas in mainland China, covered 76.61% of dialysis costs in 2015.26 For rural residents, the proportion of reimbursement for KRT varies from 60% to 90% according to geographic region.31 In 2016, the Chinese government announced that it would merge the health insurance systems in urban and rural regions over the next few years, with the aim of increasing the rate of reimbursement for rural residents.32 These efforts may help improve the affordability of therapy.
Guaranteeing access to KRT requires having enough dialysis facilities and qualified workers to meet the needs of the population. Generally, developed jurisdictions in North and East Asia reported higher densities of both dialysis centers and members of the nephrology workforce than did developing jurisdictions in the region. Mainland China has the lowest densities, with only 0.54 pmp for HD centers, 0.36 pmp for PD centers, and 1.09 pmp for the nephrology workforce.9 Given the projected increase in the number of KF patients, the country may need to expand its capacity to provide KRT. Between 2011 and 2015, the number of HD centers in mainland China increased from 3511 to 4089.31 Since the 2016 announcement of a policy eliminating mandatory affiliation with public hospitals, more than 150 independent HD centers have been established.31 To address gaps in the nephrology workforce, China has been considering strategies that involve both shifting care responsibilities to primary health care workers and training more nephrologists.7 The ISN also plays a vital role by supporting training programs for nephrologists at the international level through short- and long-term fellowships, education ambassadors, and other activities.33 For example, a tight relationship between the Peking University First Hospital (China) and the Second General Hospital in Ulaanbaatar (Mongolia) has been established to strengthen clinical capacity in Mongolia through fellowships and the Sister Renal Centers program.
PD is a less resource-demanding dialysis modality than is HD; yet, it can be equally effective.34 However, PD is much less prevalent than HD in all jurisdictions in North and East Asia, except for Hong Kong, where the PD First policy has driven a high prevalence of the modality since 1985.5 In Hong Kong, the survival rate of patients who receive PD continues to improve, and it has been equivalent to that of HD patients since 2005.5 The experience in Hong Kong may have implications for mainland China. Given its simplicity, low cost, and low dependency on facilities, PD may be a way to address the increasing number of patients with KF, especially in rural areas that lack sufficient resources to establish HD centers. However, as suggested by an in-depth review of the state of nephrology in China, staff training, patient education, standard protocols, and strict quality control measures should all be implemented to ensure the effectiveness of PD. It is encouraging to see that 31 training centers for PD have been established in mainland China with the mission to expand satellite PD centers and promote high-quality service for surrounding areas.7
Conclusion
In conclusion, the burden of KF is high in North and East Asia and is projected to increase, owing to risk factors such as the aging of the population and the high prevalence of metabolic diseases. Although KRT and conservative care for KF are generally available and affordable, ongoing efforts to improve KF care capacity are required, especially in middle-income countries. Increasing financial support, establishing effective health information systems, developing and implementing proper policies and strategies, and engaging in advocacy are essential to improvement.
Disclosure
VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. RPF reports grants from Baxter Healthcare and Fresenius Medical Care, personal fees from Astra Zeneca and AKEBIA,outside the submitted work. DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care, travel sponsorship from Amgen, personal fees from Astra Zeneca, AWAK, and Ono, and grants from National Health and Medical Research Council of Australia, outside the submitted work. All the other authors declared no competing interests.
Acknowledgments
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
The authors thank Kara Stephenson Gehman in for International Society of Nephrology Global Kidney Health Atlas Project (ISN-GKHA) for carefully editing the English text of a draft of this manuscript; Jo-Ann Donner, Coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements; Sandrine Damster, Senior Research Project Manager at the ISN; and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support. They also thank the ISN headquarters staff, including the Executive Director, Charu Malik, and the Advocacy team. They also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey.
Footnotes
Table S1. Burden and risk factors of chronic kidney disease in North and East Asia.
Figure S1. Shortage of kidney failure care providers.
Figure S2. Capacity for kidney transplantation based on transplant donor type (A) and the existence of transplantation waitlists (B).
Figure S3. Barriers to optimal kidney failure care in the North and East Asia region.
Supplementary Appendix. Reference list for annual cost of kidney replacement therapy (for Table 3).
Supplementary Material
References
- 1.Wang J., Zhang L., Tang S.C. Disease burden and challenges of chronic kidney disease in North and East Asia. Kidney Int. 2018;94:22–25. doi: 10.1016/j.kint.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 2.Masakane I., Nakai S., Ogata S. Annual dialysis data report 2014, JSDT Renal Data Registry (JRDR) Ren Replace Ther. 2017;3:18. [Google Scholar]
- 3.Jin D.C., Yun S.R., Lee S.W. Lessons from 30 years' data of Korean end-stage renal disease registry, 1985-2015. Kidney Res Clin Pract. 2015;34:132–139. doi: 10.1016/j.krcp.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang W.C., Hwang S.J. Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transplant. 2008;23:3977–3982. doi: 10.1093/ndt/gfn406. [DOI] [PubMed] [Google Scholar]
- 5.Ho Y.W., Chau K.-F., Choy B.Y. Hong Kong renal registry report 2012. Hong Kong J Nephrol. 2013;1:28–43. [Google Scholar]
- 6.Zhang L., Long J., Jiang W. Trends in chronic kidney disease in China. N Engl J Med. 2016;375:905–906. doi: 10.1056/NEJMc1602469. [DOI] [PubMed] [Google Scholar]
- 7.Liu Z.-H. Nephrology in China. Nat Rev Nephrol. 2013;9:523–528. doi: 10.1038/nrneph.2013.146. [DOI] [PubMed] [Google Scholar]
- 8.Bello A.K., Levin A., Tonelli M. Assessment of global kidney health care status. JAMA. 2017;317:1864–1919. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bello A.K., Levin A., Lunney M. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 10.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11 e4–e10. [Google Scholar]
- 11.Leung C.B., Cheung W.L., Li P.K. Renal registry in Hong Kong-the first 20 years. Kidney Int Suppl (2011) 2015;5:33–38. doi: 10.1038/kisup.2015.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2018. 2018 USRDS annual data report: epidemiology of kidney disease in the United States. [Google Scholar]
- 14.Tang S.C.W., Yu X., Chen H.C. Dialysis care and dialysis funding in Asia. Am J Kidney Dis. 2020;75:772–781. doi: 10.1053/j.ajkd.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 15.GODT Global observatory on donation and transplantation database. http://www.transplant-observatory.org/data-charts-and-tables/ Available at:
- 16.Fukuhara S., Yamazaki C., Hayashino Y. The organization and financing of end-stage renal disease treatment in Japan. Int J Health Care Finance Econ. 2007;7:217–231. doi: 10.1007/s10754-007-9017-8. [DOI] [PubMed] [Google Scholar]
- 17.Hu R.H., Lee P.H., Tsai M.K., Lee C.Y. Medical cost difference between renal transplantation and hemodialysis. Transplant Proc. 1998;30:3617–3620. doi: 10.1016/s0041-1345(98)01161-0. [DOI] [PubMed] [Google Scholar]
- 18.Shimizu U., Saito S., Lings Y. Cost-effectiveness achieved through changing the composition of renal replacement therapy in Japan. J Med Econ. 2012;15:444–453. doi: 10.3111/13696998.2011.653512. [DOI] [PubMed] [Google Scholar]
- 19.Tumurbaatar B., Nyamsuren D., Byambadorj B. Kidney transplantation in Mongolia using effective and economical immunosuppression: a three-year experience. Ann Transplant. 2012;17:132–139. doi: 10.12659/aot.882647. [DOI] [PubMed] [Google Scholar]
- 20.van der Tol A., Lameire N., Morton R.L. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu A.W., Chau K.F., Ho Y.W., Li P.K. Development of the "peritoneal dialysis first" model in Hong Kong. Perit Dial Int. 2007;27(suppl 2):S53–S55. [PubMed] [Google Scholar]
- 22.Central Intelligence Agency The world factbook. https://www.cia.gov/the-world-factbook/ Available at: Published 2019. Accessed March 11, 2021.
- 23.World Bank GDP ranking. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at: Published 2019. Accessed July 17, 2020.
- 24.United Nations Development Programme National Human Development Report 2018. http://hdr.undp.org/sites/default/files/reports/2843/978-92-1-126436-4_web.pdf Available at: Published 2018. Accessed July 17, 2020.
- 25.Saran R., Robinson B., Abbott K.C. US Renal Data System 2019 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2020;75(1 suppl 1):A6–A7. doi: 10.1053/j.ajkd.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 26.Zhang L., Zhao M.H., Zuo L. China Kidney Disease Network (CK-NET) 2015 annual data report. Kidney Int Suppl. 2019;9:e1–e81. doi: 10.1016/j.kisu.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Z., Zhang W., Chen X., Hsu C.Y. Trends in end-stage kidney disease in Shanghai, China. Kidney Int. 2019;95:232. doi: 10.1016/j.kint.2018.08.044. [DOI] [PubMed] [Google Scholar]
- 28.Gan L., Zuo L. Current ESRD burden and its future trend in Beijing, China. Clin Nephrol. 2015;83(7 suppl 1):17–20. doi: 10.5414/cnp83s017. [DOI] [PubMed] [Google Scholar]
- 29.Hanafusa N., Nakai S., Iseki K., Tsubakihara Y. Japanese society for dialysis therapy renal data registry-a window through which we can view the details of Japanese dialysis population. Kidney Int Suppl (2011) 2015;5:15–22. doi: 10.1038/kisup.2015.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 31.Yang C., Wang H., Zhao X. CKD in China: evolving spectrum and public health implications. Am J Kidney Dis. 2020;76:258–264. doi: 10.1053/j.ajkd.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 32.Zhang L., Zuo L. Current burden of end-stage kidney disease and its future trend in China. Clin Nephrol. 2016;86:27–28. doi: 10.5414/CNP86S104. [DOI] [PubMed] [Google Scholar]
- 33.International Society of Nephrology (ISN) Programs. https://www.theisn.org/about-isn/supporting-groups/programs-supporting-groups/ Available at: Published 2020. Accessed July 17, 2020.
- 34.Niang A., Iyengar A., Luyckx V.A. Hemodialysis versus peritoneal dialysis in resource-limited settings. Curr Opin Nephrol Hypertens. 2018;27:463–471. doi: 10.1097/MNH.0000000000000455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.