Abstract
Despite positive economic forecasts, stable democracies, and reduced regional conflicts since the turn of the century, Africa continues to be afflicted by poverty, poor infrastructure, and a massive burden of communicable diseases such as HIV, malaria, tuberculosis, and diarrheal illnesses. With the rising prevalence of chronic kidney disease and kidney failure worldwide, these factors continue to hinder the ability to provide kidney care for millions of people on the continent. The International Society of Nephrology Global Kidney Health Atlas project was established to assess the global burden of kidney disease and measure global capacity for kidney replacement therapy (dialysis and kidney transplantation). The aim of this second iteration of the International Society of Nephrology Global Kidney Health Atlas was to evaluate the availability, accessibility, affordability, and quality of kidney care worldwide. We identified several gaps regarding kidney care in Africa, chief of which are (i) severe workforce limitations, especially in terms of the number of nephrologists; (ii) low government funding for kidney care; (iii) limited availability, accessibility, reporting, and quality of provided kidney replacement therapy; and (iv) weak national strategies and advocacy for kidney disease. We also identified that within Africa, the availability and accessibility to kidney replacement therapy vary significantly, with North African countries faring far better than sub-Sahara African countries. The evidence suggests an urgent need to increase the workforce and government funding for kidney care, collect adequate information on the burden of kidney disease from African countries, and develop and implement strategies to enhance disease prevention and control across the continent.
Keywords: chronic kidney disease, dialysis, funding, kidney failure, kidney registries, workforce
As in many parts of the world, the demographic, socioeconomic, and political landscape of most of Africa has changed significantly since the turn of the century. Despite positive economic forecasts, stable democracies, and a significant reduction in regional conflicts, the continent continues to be plagued by poverty, excessive corruption, a lack of infrastructure, and a huge burden of communicable diseases such as human immunodeficiency virus disease , malaria, tuberculosis, diarrheal illnesses, and recurring epidemics like Ebola virus disease.1 Given these significant challenges, addressing issues associated with noncommunicable diseases (NCDs) like chronic kidney disease (CKD) and kidney failure (KF) is a low priority for governments in Africa.2 The lack of a continent-wide kidney disease registry to guide physicians and policymakers makes it even more difficult to fully grasp the scope of the disease and economic impacts in Africa. Moreover, published studies are often limited by small sample size and poor study design. Thus, the gap between those with KF and those receiving kidney replacement therapy (KRT; dialysis and kidney transplantation) is projected to continue to widen in Africa.3 The first iteration of the International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA) provided a broad overview of the state of kidney care across the continent.4 In the second iteration, we collected more detailed information on the burden of kidney disease from more countries in Africa, as well as data on the capacity for, accessibility to, and quality of KF care. The methodology for this research is described in detail elsewhere.5
Results
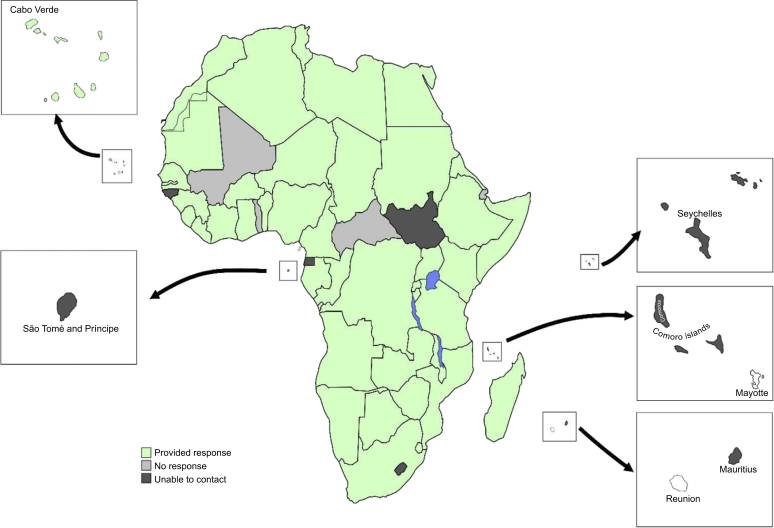
The results of this study are presented in the tables and figures and broadly summarized into 2 categories: desk research (Tables 16, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 and 23,8,9,13,17,18, Figure 1, Supplementary Table S1, and Supplementary Appendix) and survey administration (Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figures S1–S10).
Table 1.
Demographics, health expenditures, and kidney replacement therapy costs in African countries that responded to the ISN-GKHA survey6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16
| Country | World Bank income level | Area (km2) | Total population (2018) | GDP (PPP), $ billionsa |
Total health expenditures (% of GDP)a | Annual cost KRTb (US$) and out-of-pocket cost/% paid by patient from total costc |
||
|---|---|---|---|---|---|---|---|---|
| HD | PD | KT (first year) | ||||||
| Global median | — | — | — | — | 6.5 | 22,617 | 20,524 | 25,356 |
| Africa median | — | 29,974,508 | 1,255,518,570 | 118.5 | 6.1 | 15,800 | 17,542 | 16,312 |
| Algeria | Upper-middle | 2,381,741 | 41,657,488 | 630.0 | 6.6 | 9,152/0 | —/0 | —/0 |
| Angola | Lower-middle | 1,246,700 | 30,355,880 | 193.6 | 2.9 | —/0 | —/0 | — |
| Benin | Low | 112,622 | 11,340,504 | 25.4 | 3.9 | —/0 | —/0 | —/0 |
| Botswana | Upper-middle | 581,730 | 2,249,104 | 39.0 | 5.5 | —/100 | —/100 | — |
| Burkina Faso | Low | 274,200 | 19,742,715 | 35.9 | 6.8 | —/>75 | — | — |
| Burundi | Low | 27,830 | 11,844,520 | 8.0 | 6.2 | 12,480/1–25 | — | — |
| Cabo Verde | Lower-middle | 4033 | 568,373 | 3.8 | 5.2 | —/0 | — | — |
| Cameroon | Lower-middle | 475,440 | 25,640,965 | 89.5 | 4.7 | 1560/1–25 | — | — |
| Cen. African Rep. | Low | 622,984 | 5,745,062 | 3.4 | 4.3 | — | — | — |
| Chad | Low | 1,284,000 | 15,833,116 | 28.6 | 4.5 | —/100 | — | — |
| Comoros | Lower-middle | 2235 | 821,164 | 1.3 | 7.6 | — | — | — |
| Congo, Dem. Rep. | Low | 2,344,858 | 85,281,024 | 68.6 | 3.9 | 43,902/>75 | 34,165/100 | — |
| Congo, Rep. | Lower-middle | 342,000 | 5,062,021 | 29.4 | 4.6 | —/1–25 | —/26–50 | — |
| Cote d'Ivoire | Lower-middle | 322,463 | 26,260,582 | 97.2 | 4.4 | — | — | — |
| Djibouti | Lower-middle | 23,200 | 884,017 | 3.6 | 3.5 | — | — | — |
| Egypt | Lower-middle | 1,001,450 | 99,413,317 | 1204.0 | 4.6 | 3217/0 | 6979/0 | 7482/0 |
| Equatorial Guinea | Upper-middle | 28,051 | 797,457 | 31.5 | 3.4 | — | — | — |
| Eritrea | Low | 117,600 | 5,970,646 | 9.4 | 3.0 | — | — | — |
| Ethiopia | Low | 1,104,300 | 108,386,391 | 200.6 | 4.0 | —/100 | — | —/1–25 |
| Gabon | Upper-middle | 267,667 | 2,119,036 | 36.7 | 2.7 | —/1–25 | — | — |
| Gambia | Low | 11,300 | 2,092,731 | 5.6 | 6.7 | —/0 | — | — |
| Ghana | Lower-middle | 238,533 | 28,102,471 | 134.0 | 5.9 | —/>75 | — | —/100 |
| Guinea | Low | 245,857 | 11,855,411 | 28.0 | 4.5 | — | — | — |
| Guinea-Bissau | Low | 36,125 | 1,833,247 | 3.2 | 6.9 | — | — | — |
| Kenya | Lower-middle | 580,367 | 48,397,527 | 163.7 | 5.2 | 17,736/1–25 | 13,302/26–50 | —/51–75 |
| Lesotho | Lower-middle | 30,355 | 1,962,461 | 6.7 | 8.4 | — | — | — |
| Liberia | Low | 111,369 | 4,809,768 | 6.1 | 15.2 | — | — | — |
| Libya | Upper-middle | 1,759,540 | 6,754,507 | 62.0 | 5.0 | —/>75 | —/>75 | —/51–75 |
| Madagascar | Low | 587,041 | 25,683,610 | 39.9 | 5.2 | —/>75 | —/>75 | — |
| Malawi | Low | 118,484 | 19,842,560 | 22.4 | 9.3 | —/0 | — | — |
| Mali | Low | 1,240,192 | 18,429,893 | 41.2 | 5.8 | — | — | — |
| Mauritania | Lower-middle | 1,030,700 | 3,840,429 | 17.3 | 4.6 | —/1–25 | — | — |
| Mauritius | Upper-middle | 2040 | 1,364,283 | 28.3 | 5.5 | — | — | — |
| Morocco | Lower-middle | 446,550 | 34,314,130 | 298.6 | 5.5 | 5282 | 6812 | 7357 |
| Mozambique | Low | 799,380 | 27,233,789 | 37.1 | 5.4 | —/26–50 | — | — |
| Namibia | Upper-middle | 824,292 | 2,533,224 | 26.6 | 8.9 | 27,159/1–25 | 27,159 | —/1–25 |
| Niger | Low | 1,267,000 | 19,866,231 | 21.9 | 7.2 | — | — | — |
| Nigeria | Lower-middle | 923,768 | 203,452,505 | 1121.0 | 3.6 | 23,606/100 | 35,582 | 21,460/100 |
| Rwanda | Low | 26,338 | 12,187,400 | 24.7 | 7.9 | — | — | — |
| Sao Tome & Principe | Lower-middle | 964 | 204,454 | 0.7 | 9.8 | — | — | — |
| Senegal | Lower-middle | 196,722 | 15,020,945 | 54.8 | 4.0 | 20,311/1–25 | 19,404/1–25 | 20,510 |
| Seychelles | High | 455 | 94,633 | 2.8 | 3.4 | — | — | — |
| Sierra Leone | Low | 71,740 | 6,312,212 | 11.6 | 18.3 | —/100 | — | — |
| Somalia | Low | 637,657 | 11,259,029 | 20.4 | — | — | — | — |
| South Africa | Upper-middle | 1,219,090 | 55,380,210 | 767.2 | 8.2 | 10,736/0 | 13,302/0 | 23,827/0 |
| South Sudan | Low | 644,329 | 10,204,581 | 20.0 | 2.5 | — | — | — |
| Sudan | Lower-middle | 1,861,484 | 43,120,843 | 177.4 | 6.3 | 11,639/1–25 | 13,202/1–25 | 15,680/1–25 |
| Swaziland | Lower-middle | 17,364 | 1,087,200 | 11.6 | 7.7 | —/0 | — | — |
| Tanzania | Low | 947,300 | 55,451,343 | 162.5 | 6.1 | 28,446/1–25 | — | —/1–25 |
| Togo | Low | 56,785 | 8,176,449 | 13.0 | 6.6 | — | — | — |
| Tunisia | Upper-middle | 163,610 | 11,516,189 | 137.7 | 6.7 | 5980/1–25 | 5520/1–25 | 17,870/1–25 |
| Uganda | Low | 241,038 | 40,853,749 | 89.2 | 7.3 | —/26–50 | — | — |
| Zambia | Lower-middle | 752,618 | 16,445,079 | 68.9 | 5.4 | —/1–25 | —/1–25 | — |
| Zimbabwe | Lower-middle | 390,757 | 14,030,368 | 34.3 | 10.3 | -—/>75 | —/>75 | — |
—, Data not reported/unavailable; Cen., Central; Dem. Rep., Democratic Republic; GDP, gross domestic product; GKHA, Global Kidney Health Atlas; HD, hemodialysis; ISN, International Society of Nephrology; KRT, kidney replacement therapy; KT, kidney transplantations; PD, peritoneal dialysis; PPP, purchasing power parity; Rep, Republic.
Estimates are in US$ 2017.
Detailed reference list on annual cost of KRT is available in the Supplementary Appendix.
Costs are in $US 2016.
Table 2.
| Country | World Bank income level | Treated KF (pmp) | Prevalence of long-term dialysis (pmp) |
Long-term dialysis centers (pmp) |
Kidney transplantation (pmp) |
Nephrology workforce (pmp) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HD | PD | Total (HD+PD) | HD | PD | Incidence | Centers | Nephrologists | Nephrology trainees | |||
| Global median | — | 787.0 | 310.0 | 25.0 | 359.0 | 4.5 | 1.3 | 14.0 | 0.4 | 10.0 | 1.4 |
| Africa median | — | 541.0 | 13.8 | 2.1 | 16.9 | 0.5 | 0.1 | 4.6 | 0.2 | 0.6 | 0.4 |
| Algeria | Upper-middle | — | 240.3 | 11.1 | 251.4 | 7.7 | 0.2 | 4.3 | 0.2 | 12.0 | 1.9 |
| Angola | Lower-middle | — | 23.6 | 0.0 | 23.6 | 0.3 | 0.0 | — | — | 1.0 | 0.4 |
| Benin | Low | — | 30.2 | 0.0 | 30.2 | 0.4 | — | — | — | 0.9 | 0.5 |
| Botswana | Upper-middle | — | — | 18.3 | 18.3 | 2.2 | 0.9 | — | — | 0.7 | 0.9 |
| Burkina Faso | Low | — | — | — | — | 0.2 | — | — | — | 0.7 | 0.9 |
| Burundi | Low | — | — | — | — | 0.2 | — | — | — | 0.2 | — |
| Cabo Verde | Lower-middle | — | — | — | — | 1.8 | — | — | — | 3.5 | 3.5 |
| Cameroon | Lower-middle | — | 12.2 | 0.0 | 12.2 | 0.4 | — | — | — | 0.6 | 0.3 |
| Cen. African Rep. | Low | — | — | — | — | — | — | — | —— | — | — |
| Chad | Low | — | — | — | — | 0.1 | — | — | — | 0.2 | — |
| Comoros | Lower-middle | — | — | — | — | — | — | — | — | — | — |
| Congo, Dem. Rep. | Low | — | 0.3 | 0.3 | 0.6 | 0.2 | 0.0 | — | — | 0.3 | 0.0 |
| Congo, Rep. | Lower-middle | — | 0.4 | 0.3 | 0.7 | 1.0 | — | — | — | 1.6 | 0.0 |
| Cote d'Ivoire | Lower-middle | — | 23.3 | 0.0 | 23.3 | 0.3 | 0.0 | — | 0.04 | 1.0 | 0.2 |
| Djibouti | Lower-middle | — | — | — | — | — | — | — | — | — | — |
| Egypt | Lower-middle | 624.0 | 517.7 | 0.1 | 517.8 | 3.0 | 0.1 | 15.5 | 0.2 | 23.1 | 3.0 |
| Equatorial Guinea | Upper-middle | — | — | — | — | — | — | — | — | — | — |
| Eritrea | Low | — | — | — | — | 0.3 | — | — | — | — | — |
| Ethiopia | Low | — | 5.8 | 0.0 | 5.8 | 0.2 | — | — | 0.0 | 0.1 | 0.1 |
| Gabon | Upper-middle | — | 103.0 | 0.0 | 103.0 | 2.8 | — | — | — | 4.7 | — |
| Gambia | Low | — | — | — | — | 0.5 | — | — | — | 0.5 | 0.5 |
| Ghana | Lower-middle | — | 4.4 | 0.0 | 4.4 | 0.5 | — | — | 0.0 | 0.3 | 0.1 |
| Guinea | Low | — | — | — | — | 0.2 | — | — | — | 0.5 | 0.7 |
| Guinea-Bissau | Low | — | — | — | — | — | — | — | — | — | — |
| Kenya | Lower-middle | — | 9.2 | 1.1 | 10.3 | 0.8 | — | 0.6 | 0.1 | 0.6 | 0.1 |
| Lesotho | Lower-middle | — | — | — | — | — | — | — | — | — | — |
| Liberia | Low | — | — | — | — | — | — | — | — | 0.2 | 0.0 |
| Libya | Upper-middle | — | 351.8 | 12.6 | 360.1 | 9.5 | 0.7 | — | 0.2 | — | — |
| Madagascar | Low | — | 5.1 | 0.0 | 5.1 | 0.2 | — | — | — | 0.2 | 0.2 |
| Malawi | Low | — | — | — | — | — | 0.1 | — | — | 0.0 | 0.0 |
| Mali | Low | — | 3.9 | 0.0 | 3.9 | — | — | — | — | — | — |
| Mauritania | Lower-middle | — | 80.5 | 0.0 | 80.5 | 4.2 | — | — | — | 1.6 | 1.6 |
| Mauritius | Upper-middle | — | — | — | — | — | — | — | — | — | — |
| Morocco | Lower-middle | 541.0 | 185.0 | 0.6 | 185.6 | 9.6 | 0.1 | 1.5 | 0.2 | 12.5 | 2.2 |
| Mozambique | Low | — | 0.9 | 0.0 | 0.9 | 0.1 | 0.0 | — | — | 0.1 | 0.1 |
| Namibia | Upper-middle | — | 16.8 | 9.6 | 26.4 | 2.0 | — | — | 0.4 | 0.8 | 1.0 |
| Niger | Low | — | — | — | — | 0.2 | — | — | — | 0.4 | 0.0 |
| Nigeria | Lower-middle | — | 7.4 | 0.0 | 7.4 | 0.7 | — | 0.3 | 0.1 | 0.9 | 0.5 |
| Rwanda | Low | 4.4 | — | — | 2.8 | — | — | — | — | — | — |
| Sao Tome & Principe | Lower-middle | — | — | — | — | — | — | — | — | — | — |
| Senegal | Lower-middle | — | 9.7 | 1.6 | 11.3 | — | — | — | — | 2.0 | 4.3 |
| Seychelles | High | — | — | — | — | — | — | — | — | — | — |
| Sierra Leone | Low | — | — | — | — | 1.0 | 0.1 | — | — | 0.2 | 0.0 |
| Somalia | Low | — | — | — | — | 0.3 | — | — | — | 0.3 | 0.9 |
| South Africa | Upper-middle | 181.0 | 134.3 | 23.3 | 157.6 | 0.5 | — | 4.6 | — | 2.7 | 0.4 |
| South Sudan | Low | — | — | — | — | — | — | — | — | — | — |
| Sudan | Lower-middle | — | 67.9 | 2.5 | 70.4 | 4.7 | 0.3 | 5.3 | 0.2 | 1.3 | 0.4 |
| Swaziland | Lower-middle | — | 15.4 | 0.0 | 15.4 | 1.7 | 0.1 | — | 0.0 | 0.9 | 0.9 |
| Tanzania | Low | — | 0.5 | 0.0 | 0.5 | 2.8 | 0.9 | — | 0.0 | 0.2 | 0.1 |
| Togo | Low | — | 8.3 | 0.0 | 8.3 | — | — | — | — | — | — |
| Tunisia | Upper-middle | 1018.0 | 722.8 | 36.8 | 759.6 | 0.3 | — | 11.1 | 0.0 | 15.6 | 5.5 |
| Uganda | Low | — | 1.2 | 0.7 | 1.8 | 14.8 | 0.7 | — | — | 0.2 | — |
| Zambia | Lower-middle | — | 1.7 | 0.0 | 1.7 | 0.2 | — | — | — | 0.3 | 0.1 |
| Zimbabwe | Lower-middle | — | 2.8 | 0.0 | 2.8 | 0.4 | 0.3 | — | — | 0.4 | 0.0 |
—, Data not reported/unavailable; Cen., Central; Dem. Rep., Democratic Republic; HD, hemodialysis; KF, kidney failure; PD, peritoneal dialysis; pmp, per million population; Rep, Republic.
Figure 1.
African countries participating in the International Society of Nephrology Global Kidney Health Atlas survey.
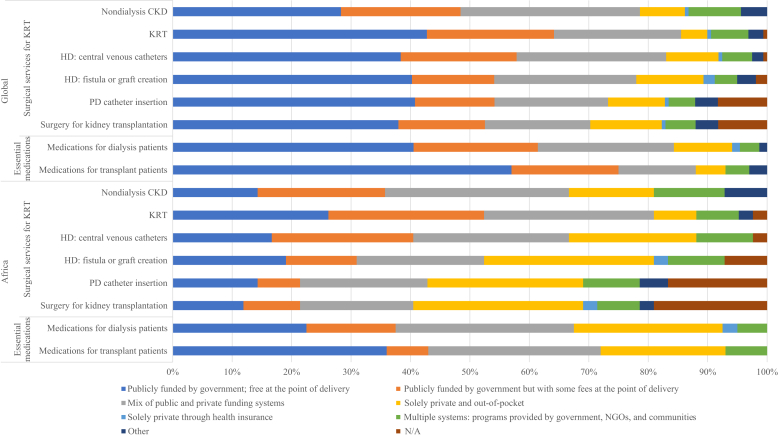
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT) care. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; N/A, not provided; NGOs, nongovernmental organizations; PD, peritoneal dialysis.
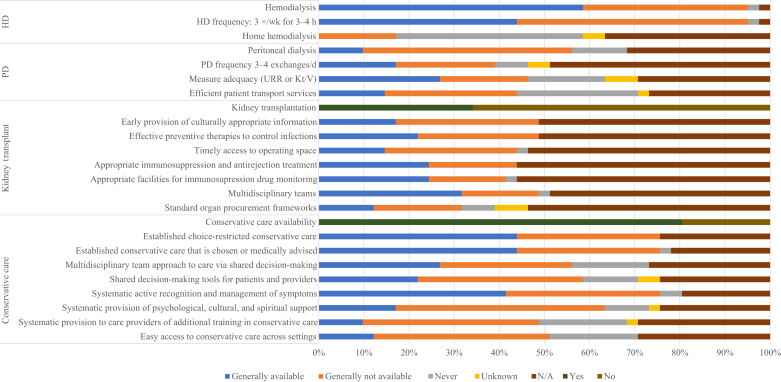
Figure 3.
Availability of choice in kidney replacement therapy or conservative care for patients with kidney failure. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
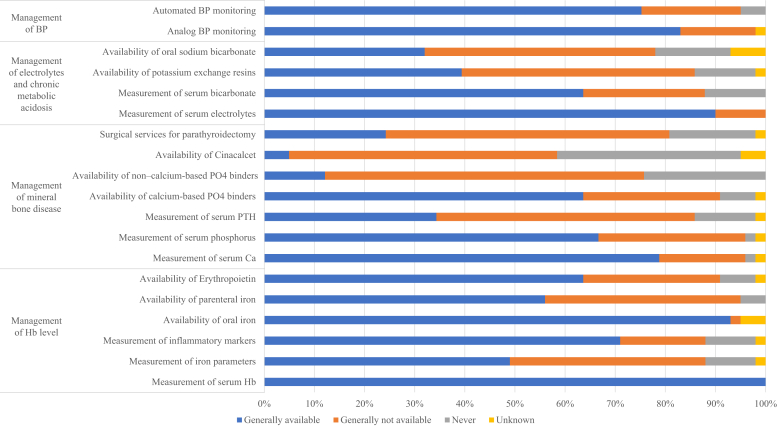
Figure 4.
Available services to diagnose and treat complications of kidney failure. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. BP, blood pressure; CA, calcium; Hb: hemoglobin; PO4, phosphate; PTH, parathyroid hormone.
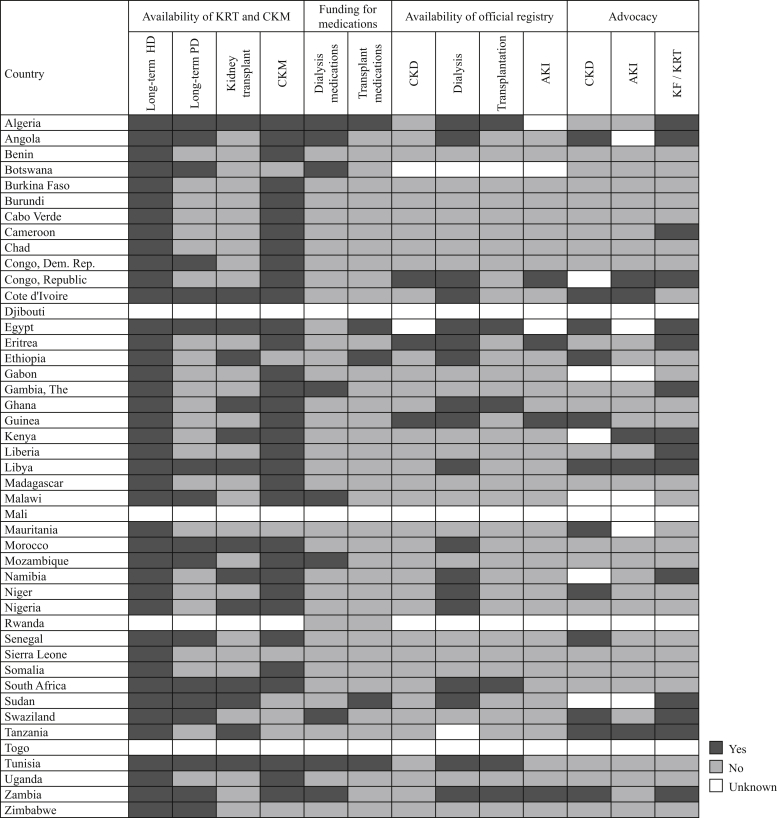
Figure 5.
Country-level scorecard for kidney care in Africa. AKI, acute kidney injury; CKD, chronic kidney disease; CKM, conservative kidney management; Dem. Rep., Democratic Republic; HD, hemodialysis; KF, kidney failure; KRT, kidney replacement therapy; PD, peritoneal dialysis.
Study setting
Africa is the second largest and second-most populous continent in the world after Asia. With a land mass of about 30.3 million km2 including adjacent islands, Africa covers 6% of the earth’s total surface area and 20% of the earth’s total land area. In 2019, Africa’s population was 1.3 billion people, representing 17% of the world’s population.19 It is composed of 54 countries divided into 5 geographic and economic regions: northern Africa, central Africa, eastern Africa, southern Africa, and western Africa. There are also 8 territories and 2 independent states with limited recognition on the continent. Algeria has the largest total land area in Africa (2.4 million km2), whereas Nigeria has the largest population (206 million).20 Africa encompasses a rich diversity of ethnicities, cultures, religions, and languages, with English, French and numerous indigenous languages being the most prevalent means of communication.
Although it has abundant natural resources, Africa is the world’s poorest and least developed continent, excluding Antarctica; its total nominal gross domestic product is lower than that of many individual countries, including the United States, China, Japan, Germany, the United Kingdom, India, and France. According to the World Bank, more than half of the extreme poor live in sub-Saharan Africa, with 413 million people living on less than US$1.90 a day in 2015.21
Although sub-Saharan Africa’s score on the Human Development Index—a statistical composite index of life expectancy, education, and per capita income indicators—increased from 0.402 in 1990 to 0.541 in 2018, it remained the lowest among all developing regions of the world. Scores in sub-Saharan Africa ranged from 0.377 in Niger to 0.801 in the Seychelles.22 Six of the 10 countries with the highest Gini index scores are in Africa (Lesotho, South Africa, Botswana, Namibia, Zambia, and Comoros),23 highlighting massive gaps in wealth distribution. In addition, the proportion of government spending on health is low in Africa. In 2017, the World Health Organization reported a 70-fold difference in health care spending between high-income and lower-income countries, with the lowest spending in the countries of West, Central, and East Africa. In the same year, more than half of donor funding for health went to 14 countries, and one-fifth went to only 4 countries, 3 of which are in Africa (Kenya, Nigeria, and Uganda).24
Current state of kidney care in Africa
Several reviews have been published on the state of nephrology in Africa.25, 26, 27, 28, 29 There are, however, no continent-wide or regional studies from Africa with data on CKD, KF, or KRT. A major reason for this has been the lack of a continent-wide registry on kidney disease. Recognizing the importance of a continent-wide kidney registry, the African Association of Nephrology (AFRAN) and the African Paediatric Nephrology Association embarked on the establishment of a continental kidney registry in 2015.30 It is thought that this initiative could make a substantial impact on the practice of nephrology and the provision of services for adults and children with KF in many African countries. Currently, the only source of comprehensive information on kidney disease in Africa is the ISN-GKHA from 2017.4
Characteristics of participating countries
Among the ISN regions, Africa had the highest number of survey respondents (n = 63); these represented 42 countries with a population of 1.2 billion (95.04% of the African population) (Figure 1). The World Bank classifies 7 (16.7%) of these countries as upper-middle, 16 (38.1%) as lower-middle, and 19 as low (45.2%) income.6 The sole high-income country in Africa, the Seychelles, did not respond to the survey. Health care expenditure as a percentage of gross domestic product ranged from 2.7% in Gabon to 18.3% in Sierra Leone (Table 1).7 Respondents included nephrologists (n = 48, 76%), nonnephrology physicians (n = 8, 13%), nonphysician health care professionals (n = 3, 5%), hospital administrators or policymakers (n = 2, 3%), and others (n = 2, 3%), with a regional response rate of 70%.
Burden of CKD, KF, and risk factors in Africa
The prevalence of CKD in Africa was 6.28%, which was lower than the global prevalence of 9.46%. Mauritius, an upper-middle income country, had the highest prevalence of CKD in Africa (17.63%), whereas Uganda, a low-income country, had the lowest prevalence (4.87%). The percentage of deaths attributable to CKD ranged from 0.57% in Zambia to 10.36% in Mauritius, and the percentage of disability-adjusted life years ranged from 0.58% in Nigeria to 6.85% in Mauritius. Among CKD risk factors, obesity was most prevalent in Libya (31.8%), high blood pressure was most prevalent in Niger (33.4%), and smoking was most prevalent in Tunisia (19.9%) (Supplementary Table S1). Although available data on the prevalence of treated KF were scant, significant disparities were observed in the reported prevalence across countries, ranging from as low as 4.4 per million population (pmp) in Rwanda to 1018 pmp in Tunisia (Table 2).3,8,9,17
Health finance and service delivery for kidney care in Africa
The 2 major modalities of funding for kidney care and service delivery in Africa were (i) a mix of public and private funding and (ii) solely private and out-of-pocket (OOP) payments. For example, a combination of public and private systems funded nondialysis CKD and KRT in 31% and 29% of countries, respectively, whereas services such as hemodialysis (HD) fistula creation, peritoneal dialysis (PD) catheter insertion, and surgery for kidney transplantation were mainly paid for solely OOP in 29%, 26%, and 29% of countries, respectively (Figure 2). In most countries around the world, these services were covered by public funding and were free at the point-of-care delivery. The annual costs of HD and PD were generally more than US$10,000 higher in sub-Saharan Africa than in North Africa. KRT was not affordable in most countries, in as much as only 22% and 12% of countries required no copayment at the point-of-care delivery for HD and PD, respectively (Supplementary Figure S1). The annual cost for HD was lowest in Cameroon (US$1560; OOP cost of 1% to 25%) and highest in the Democratic Republic of Congo (US$43,902; OOP cost of >75%). The annual cost for PD was highest in Nigeria (US$35,582) (Table 1).6, 7, 8,10, 11, 12, 13, 14, 15, 16
Health workforce for kidney care in Africa
Data on the available workforce for kidney care revealed stark differences between Africa and the rest of the world. In Africa, the number of nephrologists was 0.62 pmp, compared with 9.95 pmp globally, and the number of nephrology trainees was 0.36 pmp, compared with 1.42 pmp globally. Among the 42 responding countries in Africa, 27 (income: 2 upper-middle, 8 lower-middle, 17 low) reported <1 nephrologist pmp; collectively, these countries had a population of 850 million people (67.3% of Africa’s total population). All countries in North Africa (except Libya) had >10 nephrologists pmp. Overall, there were significant shortages of other health care workers needed for kidney care, including transplantation surgeons, dialysis access surgeons, dialysis technicians, interventional radiologists, transplantation coordinators, and dialysis nurses (Supplementary Figure S2).
Capacity for KRT service provision in Africa
Among responding countries in Africa, 100% reported that long-term HD services were available, whereas only 41% reported that long-term PD services were available. The highest prevalence of long-term dialysis (both HD and PD) was found in North Africa, in Tunisia (759.6 pmp), Egypt (610.0 pmp), Libya (360.1 pmp), Algeria (251.4 pmp), and Morocco (185.6 pmp). Tanzania had the lowest prevalence of long-term dialysis (0.5 pmp) (Table 2).3,8,9,17 Only 51% of countries reported HD to be generally available as a modality of choice (vs. 10% for PD); home HD was not available in Africa (Figure 3). Only 44% of countries reported the capacity to adhere to standard HD prescriptions (3 treatments per week, 3 to 4 hours per session) and just 17% reported the capacity to perform 3 to 4 PD exchanges daily. Efficient transport services for PD patients were generally available in only 15% of countries in the region. PD was not the predominant form of dialysis in any country and was not readily available in many countries. In Africa, the median number of HD centers was 0.53 pmp (vs. 4.46 pmp globally), and the median number of PD centers was 0.09 pmp (vs. 1.27 pmp globally) (Figure 3).
The capacity to diagnose complications of KF in Africa was comparable to, albeit lower than, global capacity. Analog and automated BP monitoring as well as the capacity to measure hemoglobin and serum electrolytes were generally available in >75% of countries. However, basic treatments for complications of KF were not readily available; oral sodium bicarbonate, potassium exchange resins, parenteral iron, and non–calcium-based phosphate binders were available in just 32%, 39%, 56%, and 12% of countries, respectively (Figure 4). Access to KRT was very limited in Africa. More than 50% of patients had access to HD in just 34% of countries, and 26% to 50% of patients were able to initiate KRT with PD in just 2% of countries (Supplementary Figure S3). When factors influencing access to dialysis were considered, geography played a big role in 54% of countries. Patient characteristics played a limited role in determining access to HD and PD (Supplementary Figure S4).
Data on kidney transplantation in Africa were scant; among countries with available data, the reported incidence was highly variable, ranging from 0.3 pmp in Nigeria to 15.5 pmp in Egypt (Table 2).3,8,9,17 The median number of kidney transplantation centers in Africa was 0.15 pmp (vs. 0.42 globally), and the availability of transplantation-related services was generally low. For instance, availability of standard organ procurement frameworks, access to operating space, and availability of immunosuppression and antirejection treatments were generally available in just 12%, 15%, and 24% of countries, respectively (Figure 3). There was no access to transplantation in 68% of countries, and 15% reported geography-based variations in access (Supplementary Figures S3 and S4). There was limited monitoring and reporting of KRT quality indicators in Africa. Indices such as hemoglobin and blood pressure were well monitored and reported in HD and PD patients. Other indices, such as small solute clearance, technique survival, and patient-reported outcome measures, were not as well monitored or reported (Supplementary Figures S5–S7).
Although conservative care was available in 80% of reporting countries in Africa, only 44% offered choice-restricted conservative care or a form that was chosen or medically advised. Conservative care was easily accessible in just 12% of countries, and 10% of countries provided additional training in conservative care to care providers (Figure 3). Shared decision-making tools and a multidisciplinary approach to care were generally available in 22% and 27% of countries, respectively.
Health information systems, statistics, and national health policies in Africa
Various health information services for kidney care, including registries and advocacy groups for kidney care, were mostly unavailable in many countries in Africa (Figure 5). Few countries in Africa had official registries for CKD (7%), dialysis (44%), transplantation (15%), and/or acute kidney injury (10%). For dialysis registries, participation was mandatory in 65% of countries and coverage was national in 72% of countries; registries typically collected data about the causes of KF (78%) and modality of dialysis (83%), with modest reporting on patient-based outcome measures such as hospitalization (33%), quality of life (17%), and mortality (67%) (Supplementary Figure S8).
Supplementary Figures S9A–S9D summarize national health policies for NCDs and for advocacy efforts related to CKD and KF in Africa. Among reporting countries in Africa, 34% had a developed national NCD strategy (vs. 47% of countries globally), and only 10% had a specific national strategy to improve care for CKD patients; 24% of countries reported that CKD strategies were incorporated into NCD strategies. National NCD strategies covered nondialysis CKD patients, dialysis patients, and transplantation patients in 60%, 40%, and 10% of countries, respectively. There were very few advocacy groups for CKD (29%) and KRT (29%) in Africa, and only 51% of countries recognized CKD as a health priority.
Barriers to optimal KF care in Africa
The proportion of countries reporting barriers to optimal KF care was higher in Africa than in the rest of the world (Supplementary Figure S10). Several countries reported a lack of nephrologists (83%), challenges with the health care system (83%), and economic factors (95%) as significant barriers to optimal care.
Discussion
CKD is a public health problem.31 Nowhere is this truer than in low-income and middle-income countries, particularly in Africa, where resources to tackle the severe burden of CKD are severely lacking.25 Moreover, owing to challenges associated with health transition, Africa is experiencing a significant double burden of communicable and noncommunicable diseases to which many health care systems are not prepared to respond.32,33 Thus, although the prevalence of CKD is projected to increase in Africa, the gap between those needing and those receiving KRT is widest in Africa than in other regions,3 and mortality among patients with KF in Africa remains alarmingly excessive.34
The results of our study highlight significant gaps in the capacity to provide kidney care in Africa. The gaps are apparent when measured against global data; however, significant variations exist among African countries in the capacity to provide KRT and the ability to access it. The main findings of our study are (i) severe workforce shortages, particularly with regard to the number of nephrologists; (ii) low government funding for kidney care; (iii) limited availability, accessibility, reporting, and quality of provided KRT; and (iv) weak national strategies and advocacy for kidney disease.
Workforce shortages, especially of nephrologists, constitute a major constraint to the delivery of kidney care in Africa. Compared with the rest of the world, where the average number of nephrologists is 9.95 pmp, the number in Africa is 0.62 pmp, with significant variations between North Africa and sub-Saharan Africa (Table 2).18 A sufficient health workforce has been described as the cornerstone of a country’s health care system, without which universal health coverage and sustainable development goals cannot be attained.35, 36, 37 Health workers often provide leadership and advise governmental decision makers responsible for developing policies and establishing health care priorities. The shortage of nephrologists in many African countries may explain why various aspects of kidney care remain weak across the continent. Among several factors contributing to the low number of nephrology workers worldwide, several are relevant to Africa, including the increasing burden of CKD, lack of exposure to nephrology among students and residents, inflexible work schedules, and inadequate training resulting from a lack of trainers and the necessary infrastructure for training.28,38
The ISN Fellowship Program was specifically established to mitigate shortages in the nephrology workforce, especially in developing countries.39 Data show that Africa benefitted immensely from the ISN Fellowship Program and other ISN programs geared toward augmenting the workforce or equipping members of the existing workforce to improve kidney disease care in Africa.40 “Brain-drain” of African nephrologists to greener pastures in North America, Europe, or Australia because of difficult working environments, economic hardships, or personal security challenges also contributes to the low number of nephrologists in Africa.41,42 Workforce shortages in Africa also extend beyond nephrologists to other workers, including dialysis nurses, access surgeons, dialysis technicians, and interventional radiologists (Supplementary Figure S2).
When developing strategies to tackle the rising burden of CKD in Africa, governments must improve funding for training health care workers in nephrology. Given the time and funding needed to train nephrology specialists, immediate strategies may include task shifting and task sharing to improve the primary care treatment of patients with kidney disease.43 AFRAN also needs to work with the ISN Fellowship Program to identify key areas of need across the continent, standardize nephrology training in the region, and engage in advocacy by sensitizing various governments to the need to support workforce development through increased funding.
Inadequate funding of various aspects of kidney care together with the lack of political will are also important barriers to the effective delivery of kidney care in Africa. Over half of the world’s extreme poor live in Africa,21 where annual dialysis costs exceed US$10,000, a high proportion of which is covered by OOP payments. It thus should come as no surprise that KRT is accessible to relatively few people. For example, in a study performed in the Democratic Republic of Congo, the monthly mean cost of dialysis was US$1270; yet, among participants with KF who needed dialysis, monthly income was US$205 for 52.8% of patients, US$525 for 34% of patients, and US$750 for 13.2% of patients.14 In the Democratic Republic of Congo, which has a population of >85 million, the prevalence of HD and PD is 0.6 pmp, and the current estimated annual cost for HD is US$43,902 per year (Tables 1 and 2).9,13 Other studies have attributed the inability to continue treatment (for ≤90 days) and the excessive mortality associated with KF in Africa to the significant financial burden of KF treatment.34 Our findings likewise showed that economic factors constituted one of the largest barriers to optimal KF care in Africa (Supplementary Figure S10).
Health care spending by governments in Africa is low. According to the Abuja Declaration, governments are expected to allocate 15% of their total national budgets to health care; however, progress toward this target has been slow, and health spending continues to be viewed as “consumption” rather than “investment.”44 There is no doubt that the double burden of disease, especially the higher burden of communicable diseases, plays a role in determining what should be spent on NCDs. However, adequate health care service provision should be a key objective of every governmental intervention in the region. African institutions such as the African Union, the Southern African Development Community, the West African Health Organization, and others could potentially play stronger roles in advocating and developing policies that ensure adequate allocation of health care budgets to the provision of kidney care in the region.
Although all countries in the region reported the availability of dialysis services, access varies on the basis of geography and the quality of HD or PD provided (Figure 3 and Supplementary Figure S4). Several reports from Africa show a skewed distribution of KRT services in favor of a few large cities.28,45 With the low utilization of PD and few services available to transport patients to PD centers (Figure 3), millions of people in rural areas are left with no access to treatment or must travel several hundred kilometers to receive it.46 There is a need to ramp up available services to diagnose and treat KF complications to improve conservative care services in the region. For example, Chad, the Gambia, Malawi, and Zambia reported that potassium exchange resins are never available, and 19 other countries reported that they are generally not available. Even when KRT is unavailable or inaccessible, the diagnosis and treatment of common complications such as metabolic acidosis, hyperkalemia, and fluid retention should be mandatory in all countries. Even though it is important to follow standard guidelines for KRT delivery, there is a need to assess the impacts of different treatment patterns in the region, given the excessive OOP costs for dialysis. Previous findings showed no difference in outcomes between standard dialysis treatment (i.e., 3 times weekly) and twice-weekly dialysis treatment.47 These results suggest that treatment patterns with lower frequency may be able to be leveraged in Africa without sacrificing health outcomes.
Owing to the substantial challenges encountered in the provision of kidney care in Africa, prevention of CKD should play a dominant role. Effective prevention requires coordinated national strategies for tackling NCDs and CKD risk factors. The burdens of NCDs, such as hypertension and diabetes mellitus, are increasing or are projected to rise sharply in Africa over the next decade.48,49 However, only 34% of African countries have an existing NCD strategy in place, and just 10% have a dedicated strategy to improve care for CKD patients (Supplementary Figure S9). National nephrology associations and the regional body for nephrology (AFRAN) should collaborate with NCD specialists to develop or adapt existing strategies for NCDs that include measures to prevent and treat risk factors and CKD in the population. They should also leverage their important roles in the health care community to advocate for governments to increase funding and implement programs that enhance kidney care across the continent.
Finally, it is important to establish an Africa-wide registry of kidney diseases because the current value of good data cannot be overemphasized. Such information will be valuable for understanding disease burden (incidence and prevalence), economic impacts of CKD and KF, mortality, and quality of life, just to name a few, and it could highlight discrepancies in the provision of services within and between countries and therefore encourage governments to allocate more resources for kidney care. The South African Renal Registry50,51 has published data consistently for nearly a decade and could be leveraged as a model for an Africa-wide registry. AFRAN should encourage participation in this registry, commit funds to support it, and make it operational by the end of this decade.30
In summary, this study has uncovered numerous gaps regarding kidney disease care in Africa. Although it is important to address all areas of need, there is an urgent need to focus on issues such as attending to workforce shortages, increasing government funding, reporting more information on kidney disease, and implementing strategies for disease prevention and control in Africa.
Disclosure
DSK reports grants from the International Society of Nephrology during the conduct of the study. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care, travel sponsorship from Amgen, personal fees from Astra Zeneca, AWAK, and Ono, and grants from National Health and Medical Research Council of Australia, outside the submitted work. All the other authors declared no competing interests.
Acknowledgments
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
The authors thank Kara Stephenson Gehman in International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA) for carefully editing the English text of a draft of this manuscript; Jo-Ann Donner, Coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements; Sandrine Damster, Senior Research Project Manager at the ISN, and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support; the ISN headquarters staff including the Executive Director, Charu Malik, and the Advocacy team. The authors also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey. They especially thank Dr. Anthony Were (recently deceased), President of AFRAN and an esteemed nephrology leader in Africa, for his support and help with the ISN-GKHA survey.
Footnotes
Table S1. Burden of chronic kidney disease and its risk factors in countries of Africa.
Figure S1. Affordability of kidney replacement therapy (proportion of out-of-pocket payments made by patients) in Africa.
Figure S2. Shortages in kidney re providers identified by responding countries in Africa.
Figure S3. Accessibility of kidney replacement therapy in Africa.
Figure S4. Geographic and patient-based factors influencing accessibility to kidney replacement therapy in Africa.
Figure S5. Hemodialysis quality indicators monitored and reported in Africa.
Figure S6. Peritoneal dialysis quality indicators monitored and reported in Africa.
Figure S7. Kidney transplantation quality indicators monitored and reported in Africa.
Figure S8. Characteristics of acute kidney injury, chronic kidney disease, dialysis, and transplantation registries in Africa.
Figure S9. Strategies and advocacy efforts: (A) national NCD strategy, (B) national strategy to improve care for CKD patients, (C) population covered by national CKD-specific and general NCD strategy, (D) national advocacy for CKD/KF.
Figure S10. Barriers to optimal kidney failure care in Africa.
Supplementary Appendix Reference list for annual cost of kidney replacement therapy (for Table 1).
Supplementary Material
References
- 1.United Nations Global issues (Africa) https://www.un.org/en/sections/issues-depth/africa/index.html Available at: Published 2020. Accessed June 22, 2020.
- 2.Okpechi I.G. ESKD in sub-Saharan Africa: will governments now listen? Lancet Glob Health. 2017;5:e373–e374. doi: 10.1016/S2214-109X(17)30070-0. [DOI] [PubMed] [Google Scholar]
- 3.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 4.Bello A.K., Levin A., Tonelli M. Assessment of global kidney health care status. JAMA. 2017;317:1864–1881. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11:e4–e10 [Google Scholar]
- 6.World Bank GDP ranking. June 2019. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at: Published 2019. Accessed June 15, 2020.
- 7.Central Intelligence Agency The world factbook. https://www.cia.gov/the-world-factbook/ Available at: Published 2019. Accessed March 11, 2021.
- 8.Abu-Aisha H., Elamin S. Peritoneal dialysis in Africa. Perit Dial Int. 2010;30:23–28. doi: 10.3747/pdi.2008.00226. [DOI] [PubMed] [Google Scholar]
- 9.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahmoud K.M., Sheashaa H.A., Gheith O.A. Continuous ambulatory peritoneal dialysis in Egypt: progression despite handicaps. Perit Dial Int. 2010;30:269–273. doi: 10.3747/pdi.2009.00001. [DOI] [PubMed] [Google Scholar]
- 11.Matri A., Elhassan E., Abu-Aisha H. Renal replacement therapy resources in Africa. Arab J Nephrol Transplant. 2008;1:9–14. [Google Scholar]
- 12.Soliman A.R., Fathy A., Roshd D. The growing burden of end-stage renal disease in Egypt. Ren Fail. 2012;34:425–428. doi: 10.3109/0886022X.2011.649671. [DOI] [PubMed] [Google Scholar]
- 13.Sumaili E.K., Krzesinski J.M., Zinga C.V. Prevalence of chronic kidney disease in Kinshasa: results of a pilot study from the Democratic Republic of Congo. Nephrol Dial Transplant. 2009;24:117–122. doi: 10.1093/ndt/gfn469. [DOI] [PubMed] [Google Scholar]
- 14.Tshamba H.M., Van Caillie D., Nawej F.N. Risk of death and the economic accessibility at the dialysis therapy for the renal insufficient patients in Lubumbashi city, Democratic Republic of Congo. Pan Afr Med J. 2014;19:61. doi: 10.11604/pamj.2014.19.61.3742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Tol A., Lameire N., Morton R.L. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization The global health observatory. https://www.who.int/gho/en/ Available at: Published 2019. Accessed June 22, 2020.
- 17.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2018. 2018 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. [Google Scholar]
- 18.Bello A.K., Levin A., Lunney M. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 19.United Nations Global issues: population. https://www.un.org/en/sections/issues-depth/population/index.html Available at: Published 2019. Accessed June 22, 2020.
- 20.United Nations Population Fund World population dashboard. https://www.unfpa.org/data/world-population-dashboard Available at: Published 2020. Accessed March 15, 2020.
- 21.World Bank Understanding poverty. https://www.worldbank.org/en/topic/poverty/overview Available at: Published 2019. Accessed June 22, 2020.
- 22.UNDP-United Nations Development Programme Human development data (1990-2018) http://hdr.undp.org/en/data Available at: Published 2018. Accessed March 15, 2020.
- 23.Central Intelligence Agency Distribution of family income - GINI Index. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2172rank.html Available at: Published 2019. Accessed March 15, 2020.
- 24.World Health Organization Global spending on health: a world in transition. Geneva. https://www.who.int/health_financing/documents/health-expenditure-report-2019/en/ Available at: Published 2019. Accessed March 8, 2020.
- 25.Swanepoel C.R., Wearne N., Okpechi I.G. Nephrology in Africa—not yet uhuru. Nat Rev Nephrol. 2013;9:610–622. doi: 10.1038/nrneph.2013.168. [DOI] [PubMed] [Google Scholar]
- 26.Naicker S. Burden of end-stage renal disease in sub-Saharan Africa. Clin Nephrol. 2010;74(suppl 1):S13–S16. doi: 10.5414/cnp74s013. [DOI] [PubMed] [Google Scholar]
- 27.Barsoum R.S., Khalil S.S., Arogundade F.A. Fifty years of dialysis in Africa: challenges and progress. Am J Kidney Dis. 2015;65:502–512. doi: 10.1053/j.ajkd.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Wearne N., Okpechi I.G., Swanepoel C.R. Nephrology in South Africa: not yet ubuntu. Kidney Dis (Basel) 2019;5:189–196. doi: 10.1159/000497324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okpechi I.G., Swanepoel C.R., Venter F. Access to medications and conducting clinical trials in LMICs. Nat Rev Nephrol. 2015;11:189–194. doi: 10.1038/nrneph.2015.6. [DOI] [PubMed] [Google Scholar]
- 30.Davids M.R., Eastwood J.B., Selwood N.H. A renal registry for Africa: first steps. Clin Kidney J. 2016;9:162–167. doi: 10.1093/ckj/sfv122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jha V., Garcia-Garcia G., Iseki K. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 32.Maher D., Smeeth L., Sekajugo J. Health transition in Africa: practical policy proposals for primary care. Bull World Health Organ. 2010;88(12):943–948. doi: 10.2471/BLT.10.077891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kushitor M.K., Boatemaa S. The double burden of disease and the challenge of health access: evidence from access, bottlenecks, cost and equity facility survey in Ghana. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ashuntantang G., Osafo C., Olowu W.A. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5:e408–e417. doi: 10.1016/S2214-109X(17)30057-8. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization Health workforce requirements for universal health coverage and the sustainable development goals. http://www.who.int/hrh/resources/health-observer17/en/ Available at: Published 2016. Accessed March 15, 2020.
- 36.Reich M.R., Harris J., Ikegami N. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387:811–816. doi: 10.1016/S0140-6736(15)60002-2. [DOI] [PubMed] [Google Scholar]
- 37.Osman M.A., Alrukhaimi M., Ashuntantang G.E. Global nephrology workforce: gaps and opportunities toward a sustainable kidney care system. Kidney Int Suppl. 2018;8:52–63. doi: 10.1016/j.kisu.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharif M.U., Elsayed M.E., Stack A.G. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J. 2016;9(1):11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harris D.C., Dupuis S., Couser W.G., Feehally J. Training nephrologists from developing countries: does it have a positive impact? Kidney Int Suppl (2011) 2012;2:275–278. doi: 10.1038/kisup.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feehally J. The International Society of Nephrology (ISN). Roles & challenges in Africa and other resource-limited communities. Clin Nephrol. 2016;86(suppl 1):3–7. doi: 10.5414/CNP86S101. [DOI] [PubMed] [Google Scholar]
- 41.Eastwood J.B., Conroy R.E., Naicker S. Loss of health professionals from sub-Saharan Africa: the pivotal role of the UK. Lancet. 2005;365:1893–1900. doi: 10.1016/S0140-6736(05)66623-8. [DOI] [PubMed] [Google Scholar]
- 42.Katz I.J., Gerntholtz T., Naicker S. Africa and nephrology: the forgotten continent. Nephron Clin Pract. 2011;117:c320–c327. doi: 10.1159/000321524. [DOI] [PubMed] [Google Scholar]
- 43.Okel J., Okpechi I.G., Qarni B. Nephrology training curriculum and implications for optimal kidney care in the developing world. Clin Nephrol. 2016;86:110–113. doi: 10.5414/CNP86S123. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organization The Abuja declaration: ten years on. https://www.who.int/healthsystems/publications/abuja_declaration/en/ Available at: Published 2011. Accessed March 14, 2020.
- 45.Tannor E.K., Awuku Y.A., Boima V. The geographical distribution of dialysis services in Ghana. Ren Replac Ther. 2018;4:3. [Google Scholar]
- 46.Tamayo Isla R.A., Ameh O.I., Mapiye D. Baseline predictors of mortality among predominantly rural-dwelling end-stage renal disease patients on chronic dialysis therapies in Limpopo, South Africa. PLoS One. 2016;11 doi: 10.1371/journal.pone.0156642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yan Y., Wang M., Zee J. Twice-weekly hemodialysis and clinical outcomes in the China dialysis outcomes and practice patterns study. Kidney Int Rep. 2018;3:889–896. doi: 10.1016/j.ekir.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cho N.H., Shaw J.E., Karuranga S. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 50.Davids M.R., Jardine T., Marais N. South African renal registry annual report 2017. Afr J Nephrol. 2019;22:12. [Google Scholar]
- 51.Davids M.R., Jardine T., Wong E. SAT-023 Survival of South African patients on renal replacement therapy. Kidney Int Rep. 2019;4:S12. doi: 10.1093/ckj/sfaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.