Abstract
Kidney failure is the permanent impairment of kidney function associated with increased morbidity, hospitalization, and requirement for kidney replacement therapy. A total of 11 countries in the Middle East region (84.6%) responded to the survey. The prevalence of chronic kidney disease in the region ranged from 5.2% to 10.6%, whereas prevalence of treated kidney failure ranged from 152 to 826 per million population. Overall, the incidence of kidney transplantation was highest in Iran (30.9 per million population) and lowest in Oman and the United Arab Emirates (2.2 and 3.0 per million population, respectively). Long-term hemodialysis services were available in all countries, long-term peritoneal dialysis services were available in 9 (69.2%) countries, and transplantation services were available in most countries of the region. Public funding covered the costs of nondialysis chronic kidney disease care in two-thirds of countries, and kidney replacement therapy in nearly all countries. More than half of the countries had dialysis registries; however, national noncommunicable disease strategies were lacking in most countries. The Middle East is a region with high burden of kidney disease and needs cost-effective measures through effective health care funding to be available to improve kidney care in the region. Furthermore, well-designed and sustainable health information systems are needed in the region to address current gaps in kidney care in the region.
Keywords: chronic kidney disease, dialysis, funding, kidney failure, kidney registries, workforce
Kidney failure (KF) has become a major public health issue around the world and is associated with excess costs from kidney replacement therapy (KRT; dialysis and kidney transplantation), hospitalization, morbidity, and mortality.1 Although several countries in the Middle East have an abundance of mineral resources, there are still several challenges in the region in the capacity to provide adequate kidney care for its people. Some of the challenges include ongoing conflicts and wars,2 refugee crises and differences in language,3 religious practices/beliefs,4 and culture.5 One study suggested the presence of additional, less obvious challenges, including variable availability of infrastructure, constraints on health expenditure related to gross national income, lack of data on kidney disease, and low-level awareness within the medical community and the public about the advances of therapeutic and preventive measures to reduce KF.6 Regional bodies, such as the Middle East Society for Organ Transplantation, have been formed as a platform for filling the gaps and improving education, training, research, and collaboration within the region.7 Despite these, there still remains a significant gap of information on funding, availability, accessibility, health information systems, and national strategies for kidney care in the region. We leveraged on available data from the second iteration of the International Society of Nephrology (ISN) Global Kidney Health Atlas to report on various states of KF care in the Middle East region. The methods for this research are described in detail elsewhere.8
Results
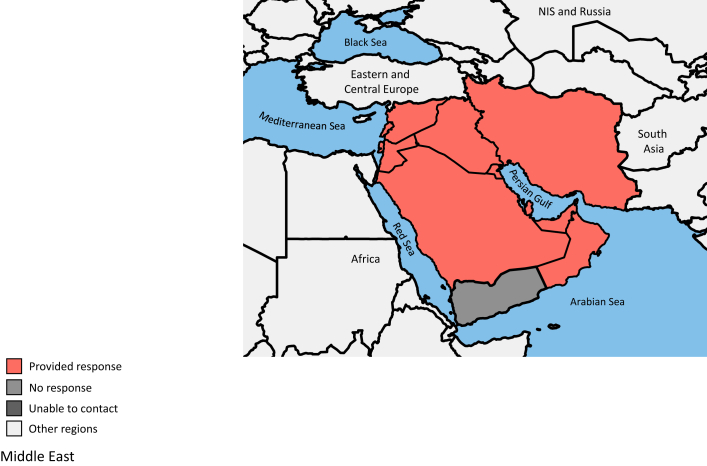
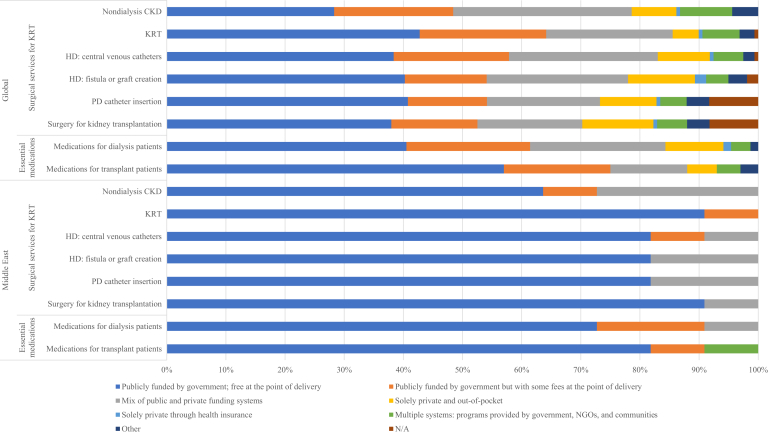
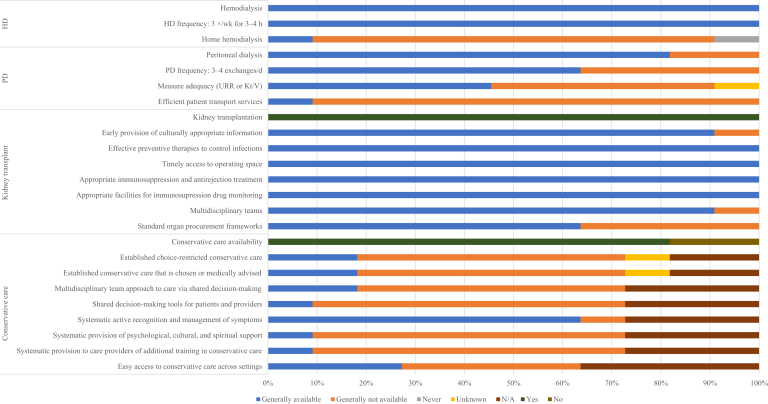
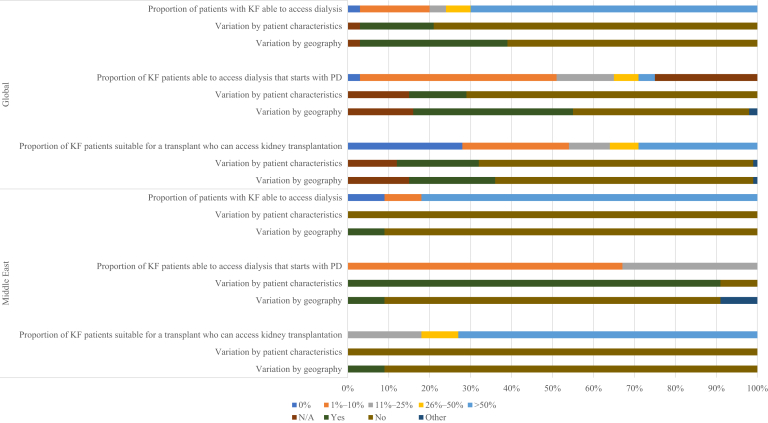
Results of this study are presented in tables and figures and broadly summarized into 2 categories: desk research (Tables 19, 10, 11, 12, 13, 14, 15, 16, 17 and 210,18, 19, 20, 21, Figure 1, and Supplementary Table S1) and survey administration (Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figures S1–S5).
Table 1.
Health finance, service delivery, and workforce prevalence in ISN Middle East countries9, 10, 11, 12, 13, 14, 15, 16, 17
| Country | World Bank income level | Area, km2 | Total population (2018) | GDP (PPP), US$ billiona | Total health expenditures, % of GDPa | Annual cost KRTb (US$) and out-of-pocket cost/% paid by patient from total costc |
||
|---|---|---|---|---|---|---|---|---|
| HD | PD | KT (first year) | ||||||
| Glo6bal median [IQR]d | — | — | — | — | 6.5 [4.9–8.8] | 22,617 [14,882–49,690] | 20,524 [14,305–33,905] | 25,356 [15,913–43,901] |
| Middle East median [IQR]d | 5,478,576 | 245,543,388 | 190 [74–649] | 5.2 [3.7–6.5] | 19,489 [15,860–41,535] | 16,551 [11,441–31,260] | 18,361 [17,465–26,839] | |
| Bahrain | High | 760 | 1,442,659 | 71.2 | 4.9 | 41,535 | — | 18,361 |
| Iran, Islamic Rep. | Upper-middle | 1,648,195 | 83,024,745 | 1640.0 | 7.6 | 13,619/1–25 | 13,026/1–25 | 11,129/1–25 |
| Iraq | Upper-middle | 438,317 | 40,194,216 | 649.3 | 5.5 | —/51–75 | —/26–50 | —/51–75 |
| Jordan | Upper-middle | 89,342 | 10,458,413 | 89.0 | 6.9 | 15,860/1–25 | 9855/0 | 26,839/100 |
| Kuwait | High | 17,818 | 2,916,467 | 289.7 | 4.0 | —/0 | —/0 | —/0 |
| Lebanon | Upper-middle | 10,400 | 6,100,075 | 88.3 | 7.4 | 19,489/1–25 | 20,075/1–25 | —/1–25 |
| Oman | High | 309,500 | 3,494,116 | 190.1 | 3.8 | —/1–25 | —/0 | —/0 |
| Qatar | High | 11,586 | 2,363,569 | 339.5 | 3.1 | —/1–25 | —/1–25 | —/1–25 |
| Saudi Arabia | High | 2,149,690 | 33,091,113 | 1775.0 | 5.8 | 50,739/— | 42,444/— | 113,935/100 |
| Syrian Arab Rep. | Low | 185,180 | 19,454,263 | 50.3 | 3.3 | —/1–25 | —/26–50 | —/100 |
| United Arab Emirates | High | 83,600 | 9,701,315 | 696.0 | 3.5 | 41,535/1–25 | —/0 | 18,361/100 |
| West Bank and Gaza | Lower-middle | 6220 | 4,635,207 | 21.2 | — | 17,259/0 | —/— | 17,465/0 |
| Yemen | Low | 527,968 | 28,667,230 | 73.6 | 6.0 | — | — | — |
—, Data not reported/unavailable; GDP, gross domestic product; HD, hemodialysis; IQR, interquartile range; ISN, International Society of Nephrology; KRT, kidney replacement therapy; KT, kidney transplantation; PD, peritoneal dialysis; PPP, purchasing power parity; Rep., Republic.
Estimates are in US$ 2017.
Detailed reference list on annual cost of KRT is available in the Supplementary Appendix.
Cost is in US$ 2016.
Median and interquartile range are calculated for the selected countries in the ISN Global Kidney Health Atlas survey only.
Table 2.
Kidney replacement therapy and nephrology workforce statistics for the ISN Middle East countries10,18, 19, 20, 21
| Country | Treated KF, pmp |
Prevalence of long-term dialysis, pmp |
Long-term dialysis centers, pmp |
Kidney transplantation, pmp |
Nephrology workforce, pmp |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | Prevalence | HD | PD | Total (HD + PD) | HD | PD | Incidence | Prevalence | Centers | Nephrologists | Nephrology trainees | |
| Global median [IQR] | 142 [106–193] | 787 [522–1047] | 310.0 [99.0–597.0] | 25.0 [2.0–56.0] | 359.0 [112.0–636.0] | 4.5 [1.0–10.0] | 1.3 [0.4–2.5] | 14.0 [5.0–36.0] | 269.0 [66.0–468.0] | 0.4 [0.2–0.7] | 10.0 [1.2–22.7] | 1.4 [0.4–3.7] |
| Middle East median [IQR] | 132 [120.0–145.0] | 636 [295.4–728.5] | 256.7 [184.1–409.5] | 17.5 [10.9–17.5] | 255.6 [178.3–422.7] | 3.8 [2.1–5.7] | 0.77 [0.4–1.5] | 12.9 [11.7–25.2] | 277 [106–311] | 0.4 [0.3–0.4] | 8.1 [5.0–15.9] | 1.8 [0.7–2.9] |
| Bahrain | 208 | 340 | — | — | 250.2 | — | — | — | 52.7 | — | — | — |
| Iran, Islamic Rep. | 81 | 654 | 211.4 | 17.6 | 229.0 | 6.9 | 0.8 | 31.0 | 311.0 | 0.4 | 5.0 | 0.4 |
| Iraq | — | 251 | — | — | 145.0 | 1.2 | 0.2 | — | 106.0 | 0.2 | 2.5 | 1.0 |
| Jordan | — | — | 428.9 | 17.4 | 446.3 | 5.2 | 0.3 | 25.2 | — | 1.0 | 8.1 | 1.8 |
| Kuwait | 141 | 787 | 263.3 | 41.3 | 304.6 | 2.1 | 2.1 | 21.7 | 363.0 | 0.3 | 10.3 | 24.0 |
| Lebanon | — | — | 668.5 | 25.5 | 694.0 | 11.9 | 1.5 | 12.9 | — | 0.7 | 28.3 | 2.1 |
| Oman | 120 | 670 | 250.0 | 10.9 | 260.9 | 5.7 | 2.2 | 2.2 | 279.0 | 0.4 | 20.0 | 2.9 |
| Qatar | 123 | 618 | 296.4 | 104.5 | 400.9 | 2.5 | 1.3 | 11.7 | 277.0 | 0.4 | 15.9 | 2.1 |
| Saudi Arabia | 145 | 826 | 409.5 | 35.0 | 444.5 | 5.3 | 0.6 | 28.0 | 269.0 | 0.4 | 8.5 | 15.9 |
| Syrian Arab Rep. | — | — | 149.1 | 6.0 | 155.1 | 3.6 | — | 12.7 | — | 0.3 | 5.1 | 1.0 |
| United Arab Emirates | — | 152 | 184.1 | 17.3 | 201.4 | 2.1 | 0.4 | 3.0 | — | 0.4 | 6.7 | 0.7 |
| West Bank and Gaza | — | — | — | — | — | 3.78 | — | — | — | 0.4 | 3.0 | 0.0 |
| Yemen | — | — | 99.1 | 9.3 | 108.4 | — | — | — | — | — | — | — |
—, Data not reported/unavailable; HD, hemodialysis; IQR, interquartile range; ISN, International Society of Nephrology; KF, kidney failure; PD, peritoneal dialysis; pmp, per million population; Rep., Republic.
Figure 1.
Map of Middle East countries participating in the International Society of Nephrology Global Kidney Health Atlas survey. NIS, Newly Independent States.
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT) care. Values represent absolute number of countries in each category, expressed as a percentage of total number of countries. HD, hemodialysis; NGOs, nongovernmental organizations; N/A, not provided; PD, peritoneal dialysis.
Figure 3.
Availability of choice in kidney replacement therapy or conservative kidney management for patients with kidney failure. Values represent absolute number of countries in each category, expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
Figure 4.
Accessibility of kidney replacement therapy for patients with kidney failure (KF). Values represent absolute number of countries in each category, expressed as a percentage of total number of countries. N/A, not provided; PD, peritoneal dialysis.
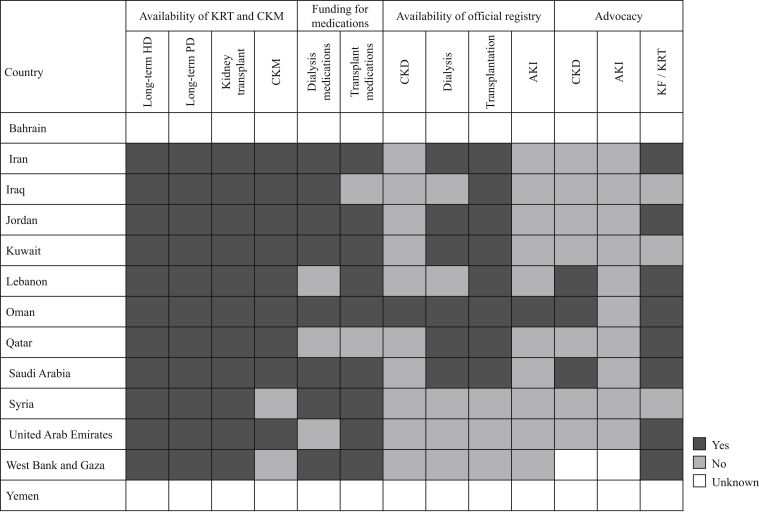
Figure 5.
Country-level scorecard for kidney care in the International Society of Nephrology Middle East countries. AKI, acute kidney injury; CKD, chronic kidney disease; CKM, conservative kidney management; HD, hemodialysis; KF, kidney failure; KRT, kidney replacement therapy; PD, peritoneal dialysis.
Setting
The Middle East is a geographic region covering almost 7.208 million km2 that extends from the eastern shores of the Mediterranean Sea to the Indian Ocean (Figure 1). The region comprises 18 countries with a total population of >410 million people, with the most populous countries being Egypt, Iran, Turkey, Iraq, and Saudi Arabia. Of the 18 countries in the Middle East, 13 belong to the Arab community.22
However, the ISN Middle East region23 is a subset of these countries, comprising Bahrain, Iran, Iraq, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, Syria, United Arab Emirates, West Bank and Gaza, and Yemen, with a total population of 243.7 million. Among these, Saudi Arabia has the largest land mass, whereas the Islamic Republic of Iran (the only Persian-speaking country in the region) has the largest population (Table 1).9
In 2017, gross national income per capita in the Middle East and North Africa was US$13,763, ranging from US$61,150 in Qatar to <US$2000 in Yemen (US$1460) and Syria (US$1820).24 The outlook for economic growth in the Middle East and North Africa dropped to 0.6% in 2019.25 Voluntary cuts to oil production, growing global economic headwinds, and the marked contraction of Iran’s economy due to rising geopolitical tensions are collectively responsible for this downward revision from the 1.5% growth rate projected in April 2019. Despite the downward trend of the past year, economic growth in the region is projected to rise to 2.6% in 2020 and to 2.9% in 2021.25 However, given the recent crisis in the world economy due to the coronavirus disease 2019 pandemic, these expectations are likely to change. One of the important limiting factors to chronic kidney disease (CKD) care delivery and research projects in the Middle East is the low gross national income in many countries in the region.10
Current state of kidney care in the Middle East
The burden of CKD and KF remains high in the Middle East and may be growing faster than other world regions.26 The overall prevalence of KF reported in the Middle East in 2008 was 430 per million population (pmp), and the pooled prevalence calculated in a recent study in the Middle East region was 360 pmp.26,27 Diabetes, glomerulonephritis, and hypertensive nephrosclerosis were leading causes of CKD in the region; however, many cases were frequently labeled as “unknown causes” because of late referral and late patient presentation.10 Data from the region show that hemodialysis (HD) was the most frequently used KRT modality, whereas peritoneal dialysis (PD) was the least frequently used.10,28
Characteristics of contributing countries
Responses were received from 11 (84.6%) countries in the ISN region (of 13 countries in the region), representing 243.7 million people (87% of the regional population). The response rate for the region was 80.6%, with most responses from nephrologists (n = 26 [90%]) and one response (3%) each for a nonnephrologist physician, a nonphysician health professional, and a policy maker. The World Bank classified approximately half of the participating countries as high income (n = 6 [54.5%]) and one-third as upper-middle income (n = 4 [36.4%]). The total health expenditure, as a percentage of gross domestic product in the region, ranged from 3.1% in Qatar to 7.6% in Iran (Table 1).11,12
Burden of CKD and KF in the Middle East
The prevalence of CKD in the Middle East ranged from 5.24% in Yemen (low income) to 10.57% in Iran (upper-middle income). The proportion of deaths and disability-adjusted life-years attributed to CKD were highest in Saudi Arabia (high income) and Jordan (upper-middle income) (Supplementary Table S1).
Data on the prevalence of treated KF were available for only 8 of the 13 countries in the region (Table 2).18, 19, 20 All 3 modes of KRT (long-term HD, PD, and kidney transplantation) were available from most countries; Saudi Arabia (826 pmp) and the United Arab Emirates (152 pmp) reported the highest and lowest prevalence of treated KF in the region, respectively. Lebanon reported the highest prevalence of HD (668.5 pmp), whereas Qatar reported the highest prevalence of long-term PD (104.5 pmp), although the prevalence of long-term HD was still more than twice as high in Qatar (296.4 pmp), indicating a preference of HD over PD.
The incidence of kidney transplantation was highest in Iran (30.96 pmp) and lowest in Oman and the United Arab Emirates (2.22 and 3.04 pmp, repectively) (Table 2).18, 19, 20 Iran reported the highest incidence of deceased donor transplantation (17.49 pmp), comprising 56.5% of transplants, whereas Jordan had the highest incidence of living donor transplantation (25.19 pmp), comprising 100% of transplants. Of the 11 countries that provided transplant data, in 4 countries, kidneys from deceased donors were not used (Jordan, Oman, Syria, and the United Arab Emirates). Dialysis and transplantation services were funded by public and private insurance systems in most countries in the Middle East. Data registries for CKD and acute kidney injury were scarce in most countries.
Health finance and service delivery for kidney care in the Middle East
Funding for KRT was “publicly funded by government” in 91% (n = 10) of countries (vs. 43% [n = 69] globally), with the remaining 9% (n = 1) funded “publicly by government with some fees at the point of delivery” (Figure 2). However, nondialysis CKD was “publicly funded by government” in 64%, whereas “a mixture of public and private funding” covered 27% of nondialysis CKD care in the region. Surgical services, such as central venous catheter insertion, HD fistula and graft creation, and insertion of PD catheters, were also largely covered by public funds by government in 82% of countries for all services. The annual cost of HD was lowest in Iran (US$13,619), with 1% to 25% out-of-pocket (OOP) payment, and was highest in Saudi Arabia (US$50,739), with data on OOP not available. Iran also had the lowest cost of first year treatment for transplant patients (US$11,361; OOP, 1%–25%), whereas Saudi Arabia had the highest (US$113,935; OOP, 100%) (Table 1).11, 12, 13, 14, 15, 16, 17
Health workforce for kidney care in the Middle East
Data on workforce showed similarities in number of nephrologists and nephrology trainees in the Middle East region and globally (Table 2).21 The median number of nephrologists in the region was 8.08 pmp (vs. 9.95 pmp globally). The median number of nephrologists was lowest in Iraq (2.49 pmp) and highest in Lebanon (28.28 pmp), and 4 countries in the region (Kuwait, Lebanon, Oman, and Qatar) had more nephrologists than the global median. The median number of nephrology trainees was also similar to the global median (1.82 versus 1.42 pmp, respectively), and there were no nephrology trainees in West Bank and Gaza (Table 2).18, 19, 20 There were shortages reported in other categories of KF care providers in most countries, with the shortages more severe for interventional radiologists for HD and PD access; there were no shortages reported in Lebanon (Supplementary Figure S1).
Capacity for KRT service provision in the Middle East
Although all countries in the region had capacity for long-term HD provision, there was more capacity for HD care than for PD in the region (Figure 3 and Table 2).18, 19, 20 Lebanon had the highest number of HD centers (11.9 pmp); the lowest was in Iraq (1.24 pmp), which also had the lowest number of PD centers (0.20 pmp) (Table 2).18, 19, 20 Home HD was reported to be “generally available” in 9% of countries. All countries (100%) had capacity to provide adequate HD (i.e., 3 times/week for 3-4 hours per session). Capacity to provide adequate PD (i.e., 3–4 exchanges per day) was reported to be “generally available” in 64% of countries (Figure 3). The capacity to treat complications of KF was readily available for most factors assessed in nearly all countries (Supplementary Figure S2). When factors influencing access to KRT were considered, neither geography nor patient characteristics played significant roles in determining access (Figure 4). Although the incidence and prevalence of kidney transplantation were highest in Iran (incidence, 30.96 pmp; prevalence, 311 pmp), data on the number of kidney transplant centers showed that Jordan had the highest (1.00 pmp).10 There were no data on kidney transplant prevalence from Jordan, Lebanon, Syria, United Arab Emirates, West Bank and Gaza, and Yemen (Table 2).18, 19, 20 Standard organ procurement frameworks were reported as “generally available” in 64% of countries, whereas effective preventive therapies to control infections in transplant patients, immunosuppression, and facilities for monitoring immunosuppression drugs were available in 100% (Figure 3).
Conservative kidney management was reported to be available in 82% of countries (Figure 5); however, established choice-restricted conservative care and conservative care that was chosen or medically advised were available in only 18% of countries, whereas easy access to conservative care across settings was available in 27% of countries. Other aspects of conservative care management, including systematic provision by care providers of additional training in conservative care and systematic provision of psychological, cultural, and spiritual support to patients, were only available in 9% of countries (Figure 3).
Health information systems, statistics, and national health policies in the Middle East
Health information services for kidney care, including registries and advocacy groups for kidney care, were mostly unavailable in many countries in the Middle East region (Figure 5). A CKD registry was only available in Oman, which also had the only acute kidney injury registry in the region. No registries were available in Syria, United Arab Emirates, and West Bank and Gaza. Eight countries had a kidney transplant registry. All the registries mainly had a national coverage (100%), and most were predominantly mandatory (acute kidney injury, 100%; dialysis, 83%; transplant, 88%) (Supplementary Figure S3). There was variable quality of reporting in the registries, with most reporting information on patient hospitalization. There were no countries with acute kidney injury advocacy groups in the region, 3 countries (Lebanon, Oman, and Saudi Arabia) had CKD advocacy groups, and 8 countries had a KF/KRT advocacy group (Figure 5).
A national noncommunicable disease (NCD) strategy was available in 27%, under development in 9%, and unavailable in 55% of countries in the region. A national strategy for improving the care of CKD patients was available in 18% of countries but was unavailable in 73% (Supplementary Figure S4). All nondialysis CKD patients (100%) were covered in the national CKD-specific strategy, whereas 50% of long-term dialysis and kidney transplant patients were covered in this strategy (Supplementary Figure S5).
Discussion
The present study reveals major features of KF management in the ISN Middle East region. By documenting the current status of kidney care and revealing variation across the region, our data can be used to improve kidney care in the region and can lay the foundation for a universal surveillance network for CKD care in the region. This study showed that there were significant variations in funding structures, availability, accessibility, and quality of KF care across countries in the Middle East region. Our study also demonstrated a lack of adequate health information about various aspects of kidney disease and lack of national strategies for NCDs and strategies for improving the care of CKD patients across the region.
Middle East countries that are members of the Gulf Cooperation Council (i.e., Bahrain, Kuwait, Qatar, Oman, Saudi Arabia, and the United Arab Emirates) have higher national incomes and, therefore, larger budgets for health services, including KRT. Almost two-thirds (63%) of countries in the Middle East region provide public funding for nondialysis CKD care, with either no or some OOP fees at the point of care delivery. In the other one-quarter (27%) of countries, public and private systems collectively provide funding for nondialysis CKD. Moreover, no country in the Middle East relies solely on private and OOP funding for KRT programs, which may explain both the high accessibility of HD and transplantation services in the region and the comparable prevalence values of treated KF in the Middle East and globally (Table 2).10 Studies have shown that the incidence and prevalence of treated KF, both indexes of KRT service delivery, ranged from 0 to 175 pmp (mean, <100 pmp) and from 0 to 753 pmp (mean, <250 pmp), respectively, in the Middle East region.26,29, 30, 31, 32 In addition to wide governmental support for KRT, it is equally important that KRT services should be reasonably priced in the region to enable countries with low health care budgets to access KRT. The cost of KRT in the region, although comparable to global values, was excessively high in some countries (Table 1).10,17
Workforce shortages, especially of nephrologists, constitute a major constraint to the delivery of kidney care in many parts of the world. Health care workforce provide leadership and guide governments on policy making on issues of public health concerns, as the ongoing coronavirus disease 2019 pandemic has demonstrated across the world. Thus, an adequate health care workforce remains the pillar of any country’s health care system, without which universal health care and sustainable development goals cannot be attained.33,34 Although this study showed that the median number of nephrologists in the region was slightly below global median, there were still some countries in the region with few nephrologists and trainees. As nephrologists were primarily responsible for care of KF patients in the region, efforts should be made to increase training and attract more trained nephrologists to the region. Also, as some low-income countries in the region rely on primary care physicians to provide kidney care, efforts should also go into training and improving kidney care education for primary care physicians in the region. Given the shortages of other specialties, especially access surgeons for KF care in the region, time and resources need to be also allocated to training these specialists while simultaneously delegating less specialized tasks to primary care providers. Notably, no countries in the region reported a shortage of kidney pathologists, specialists who ensure proper diagnosis and management of primary kidney diseases.
Long-term HD services were available in all countries, and HD was the most prevalent type of KRT in the Middle East. Our findings showed that long-term PD, although available in 82% of countries in the region, is not widely utilized, perhaps because of a lack of trained staff, financial support, and PD-specific health programs. It is noteworthy that the proportion of KF patients using PD increased from 0.5% to 4.1% between 2001 and 2010 in Iran, but has not increased further, largely because of these reasons.35 Although PD was less common, the advent of automated PD could make it a more attractive choice for patients.10,27
The availability of kidney transplantation services varied across the region. Gross national income, municipal education, governmental conflicts, and funding structures were some principal factors influencing kidney transplantation programs.36 Kidney transplantation services were available in most countries in the Middle East, and organs typically came from living donors who were related to patients; nonrelatives who donated organs typically receive monetary compensation.6 Because of a high rate of trauma, deceased organ donation is highly feasible in the region; however, this source of organs for transplantation was underutilized in many countries because of an ongoing religious debate over the nature of brain death and inadequate public awareness about the importance of organ donation and transplantation. Religious and social/cultural acceptance, legal approval for organ donation and transplantation following brain death, and government support are criteria that must be fully met to establish organ transplantation from deceased donors in the Middle East region.6
Half of the countries in the Middle East region, including Iran, Jordan, Oman, Kuwait, Qatar, and Saudi Arabia, had dialysis registries, and 73% had transplant registries. Only one country (Oman) had a CKD registry. Patients undergoing dialysis or transplantation in the region are typically documented in health systems records and are therefore easier to track than patients with CKD who do not need dialysis or other care that requires tracking for resource allocation purposes. Despite this, there is evidence that health information systems for KF and transplantation are incomplete and lacking detail in most countries in the region.7 Countries with low Human Development Index scores tend to have high disease burden, shortages of expert human resources, and underdeveloped health systems. Countries with Human Development Index scores at the middle and high end of the spectrum, on the other hand, have some health-related registry data, assess essential needs, and try to develop and improve the quality of care and reduce risk factors of disease, depending on their ability to access funds.7 However, we believe it is critically important to also establish databases of CKD patients in the region to enable better understanding of key patient characteristics, disease patterns, and resource needs to improve care of patients with kidney disease in the region. Studies from registry data from the region have shown comparable results of HD and transplant patients with data from other parts of the world.37, 38, 39, 40
This study also showed that only 27% of countries in the region had a national NCD strategy, with 9% of countries reporting an NCD strategy under development. These strategies are important in all countries, and especially in developing countries to enable early detection and prevention of NCDs, such as diabetes and hypertension, which are major causes of kidney disease in the region. Effective prevention requires coordinated national strategies for tackling NCDs and CKD risk factors, especially as the burdens of some NCDs have been projected to rise significantly in the Middle East over the next decade.41,42 Approaches to improve and increase early disease detection and preventive measures for CKD and KF would benefit both patients and the health care systems in the region by reducing treatment-related costs of kidney disease. Such strategies should be universal, should be similar to funding structures for KRT, and should include provision of funding to improve awareness and ensure early and adequate treatment of CKD risk factors.
The Middle East is a region with high burden of kidney disease. This matter of concern must be urgently addressed. CKD can be prevented in a cost-effective manner when proper guidelines are followed at the level of primary care. It is critically important to ensure the appropriate allocation of funds and health care staff and the affordability of kidney care and KRT. In addition, well-designed and sustainable registry systems must be established to help to collect updated data, develop existing facilities, and address current gaps in kidney care in the region.
Disclosure
AKA-A reports personal fees from Baxter Healthcare, outside the submitted work. DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care, travel sponsorship from Amgen, personal fees from Astra Zeneca, AWAK, and Ono, and grants from National Health and Medical Research Council of Australia, outside the submitted work. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. All the other authors declared no competing interests.
Acknowledgements
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
We thank Kara Stephenson Gehman in International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA) for carefully editing the English text of a draft of this article. We thank Jo-Ann Donner, coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements; and Sandrine Damster, senior research project manager at the ISN, and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support. We also thank the ISN headquarters staff, including the Executive Director, Charu Malik, and the Advocacy team. We also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey.
Footnotes
Table S1. Burden of chronic kidney disease and its risk factors in countries of the ISN Middle East region that participated in the ISN-GKHA survey.
Figure S1. Shortages of kidney failure care providers in the ISN Middle East region.
Figure S2. Availability of services to treat complications of kidney failure.
Figure S3. Registry characteristics for countries that reported having ≥1 registry in the ISN-GKHA survey.
Figure S4. National strategies available in countries.
Figure S5. Population covered under national noncommunicable disease and chronic kidney disease strategies.
Supplementary Appendix. Reference list for annual cost of kidney replacement therapy (for Table 1).
Supplementary Material
References
- 1.Jha V., Garcia-Garcia G., Iseki K. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 2.Isreb M.A., Kaysi S., Rifai A.O. The effect of war on Syrian refugees with end-stage renal disease. Kidney Int Rep. 2017;2:960–963. doi: 10.1016/j.ekir.2017.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hadziabdic E., Hjelm K. Arabic-speaking migrants' experiences of the use of interpreters in healthcare: a qualitative explorative study. Int J Equity Health. 2014;13:49. doi: 10.1186/1475-9276-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khazneh E., Qaddumi J., Hamdan Z. The effects of Ramadan fasting on clinical and biochemical markers among hemodialysis patients: a prospective cohort study. PLoS One. 2019;14 doi: 10.1371/journal.pone.0218745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sekkarie M.A., Abdel-Rahman E.M. Cultural challenges in the care of refugees with end-stage renal disease: what Western nephrologists should know. Nephron. 2017;137:85–90. doi: 10.1159/000477362. [DOI] [PubMed] [Google Scholar]
- 6.Shaheen F.A., Souqiyyeh M.Z. Kidney health in the Middle East. Clin Nephrol. 2010;74(suppl 1):S85–S88. doi: 10.5414/cnp74s085. [DOI] [PubMed] [Google Scholar]
- 7.Rouchi A.H., Mahdavi-Mazdeh M. Kidney transplantation in the Middle East. Clin Nephrol. 2016;86:101–105. doi: 10.5414/CNP86S109. [DOI] [PubMed] [Google Scholar]
- 8.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11 e4–e10. [Google Scholar]
- 9.Central Intelligence Agency The world factbook. https://www.cia.gov/the-world-factbook/ Available at: Published 2019. Accessed March 11, 2021.
- 10.Shaheen F.A.M., Al-Attar B., Ahmad M.K. Burden of disease: prevalence and incidence of endstage renal disease in Middle Eastern countries. Clin Nephrol. 2020;93:120–123. doi: 10.5414/CNP92S121. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Global health observatory. https://www.who.int/gho/en/ Available at:
- 12.World Bank GDP ranking. Published June 2019. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at:
- 13.Abu-Aisha H., Elamin S. Peritoneal dialysis in Africa. Perit Dial Int. 2010;30:23–28. doi: 10.3747/pdi.2008.00226. [DOI] [PubMed] [Google Scholar]
- 14.Mahmoud K.M., Sheashaa H.A., Gheith O.A. Continuous ambulatory peritoneal dialysis in Egypt: progression despite handicaps. Perit Dial Int. 2010;30:269–273. doi: 10.3747/pdi.2009.00001. [DOI] [PubMed] [Google Scholar]
- 15.Matri A., Elhassan E., Abu-Aisha H. Renal replacement therapy resources in Africa. Arab J Nephrol Transpl. 2008;1:9–14. [Google Scholar]
- 16.Soliman A.R., Fathy A., Roshd D. The growing burden of end-stage renal disease in Egypt. Ren Fail. 2012;34:425–428. doi: 10.3109/0886022X.2011.649671. [DOI] [PubMed] [Google Scholar]
- 17.van der Tol A., Lameire N., Morton R.L. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jain A.K., Blake P., Cordy P., Garg A.X. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2018. 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. [Google Scholar]
- 20.Alalawi F., Ahmed M., AlNour H. Epidemiology of end-stage renal disease in Dubai: single-center data. Saudi J Kidney Dis Transpl. 2017;28:1119–1125. doi: 10.4103/1319-2442.215126. [DOI] [PubMed] [Google Scholar]
- 21.Bello A.K., Levin A., Lunney M. Status of care for end stage kidney disease in countries and regions worldwide: international cross sectional survey. BMJ. 2019;367:l5873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 22.Encyclopedia Britannica, Inc. Middle East. https://www.britannica.com/place/Middle-East Available at:
- 23.International Society of Nephrology Regional boards Middle East. https://www.theisn.org/about-isn/governance/regional-boards/the-middle-east/#102 Available at:
- 24.IndexMundi. GNI per capita - Middle East. https://www.indexmundi.com/facts/indicators/NY.GNP.PCAP.CD/map/middle-east Available at:
- 25.World Bank Middle East and North Africa. https://www.worldbank.org/en/region/mena/overview Available at:
- 26.Mousavi S.S., Soleimani A., Mousavi M.B. Epidemiology of end-stage renal disease in Iran: a review article. Saudi J Kidney Dis Transpl. 2014;25:697–702. doi: 10.4103/1319-2442.132242. [DOI] [PubMed] [Google Scholar]
- 27.Malekmakan L., Tadayon T., Roozbeh J. End-stage renal disease in the Middle East: a systematic review and meta-analysis. Iran J Kidney Dis. 2018;12:195–203. [PubMed] [Google Scholar]
- 28.Najafi I. Peritoneal dialysis in Iran and the Middle East. Perit Dial Int. 2009;29(suppl 2):S217–S221. [PubMed] [Google Scholar]
- 29.Süleymanlar G., Serdengeçti K., Altiparmak M.R. Trends in renal replacement therapy in Turkey, 1996-2008. Am J Kidney Dis. 2011;57:456–465. doi: 10.1053/j.ajkd.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Shaheen F.A., Al-Khader A.A. Preventive strategies of renal failure in the Arab world. Kidney Int Suppl. 2005;(98):S37–S40. doi: 10.1111/j.1523-1755.2005.09807.x. [DOI] [PubMed] [Google Scholar]
- 31.El-Reshaid W., El-Reshaid K., Kapoor M. Chronic renal disease in Kuwaiti nationals: a prospective study during the past 4 years. Ren Fail. 2005;27:227–233. [PubMed] [Google Scholar]
- 32.Barsoum R.S. Burden of end-stage kidney disease: North Africa. Clin Nephrol. 2016;86:14–17. doi: 10.5414/CNP86S102. [DOI] [PubMed] [Google Scholar]
- 33.Reich M.R., Harris J., Ikegami N. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387:811–816. doi: 10.1016/S0140-6736(15)60002-2. [DOI] [PubMed] [Google Scholar]
- 34.Osman M.A., Alrukhaimi M., Ashuntantang G.E. Global nephrology workforce: gaps and opportunities toward a sustainable kidney care system. Kidney Int Suppl. 2018;8:52–63. doi: 10.1016/j.kisu.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Najafi I., Alatab S., Atabak S. Seventeen years' experience of peritoneal dialysis in Iran: first official report of the Iranian peritoneal dialysis registry. Perit Dial Int. 2014;34:636–642. doi: 10.3747/pdi.2012.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shaheen F.A.M. End-stage renal disease in the Middle East. In: García-García G., Agodoa L.Y., Norris K.C., editors. Chronic Kidney Disease in Disadvantaged Populations. Elsevier; London, UK: 2017. pp. 107–111. [Google Scholar]
- 37.Ghods A.J., Ossareh S., Savaj S. Results of renal transplantation of the Hashemi Nejad Kidney Hospital--Tehran. Clin Transpl. 2000:203–210. [PubMed] [Google Scholar]
- 38.Ajami S., Askarianzadeh M., Saghaeiannejad-Isfahani S. Comparative study on the National Renal Disease Registry in America, England and Iran. J Educ Health Promot. 2014;3:56. doi: 10.4103/2277-9531.134755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hassanien A.A., Al-Shaikh F., Vamos E.P. Epidemiology of end-stage renal disease in the countries of the Gulf Cooperation Council: a systematic review. JRSM Short Rep. 2012;3:38. doi: 10.1258/shorts.2012.011150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ossareh S., Farrokhi F., Zebarjadi M. Survival of patients on hemodialysis and predictors of mortality: a single-centre analysis of time-dependent factors. Iran J Kidney Dis. 2016;10:369–380. [PubMed] [Google Scholar]
- 41.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho N.H., Shaw J.E., Karuranga S. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.