Abstract
Information about disease burden and the available infrastructure and workforce to care for patients with kidney disease was collected for the second edition of the International Society of Nephrology Global Kidney Health Atlas. This paper presents findings for the 8 countries in the South Asia region. The World Bank categorizes Afghanistan and Nepal as low-income; Bangladesh, Bhutan, India, and Pakistan as lower-middle-income; and Sri Lanka and the Maldives as upper-middle-income countries. The prevalence of chronic kidney disease (CKD) in South Asia ranged from 5.01% to 13.24%. Long-term hemodialysis and long-term peritoneal dialysis are available in all countries, but Afghanistan lacks peritoneal dialysis services. Kidney transplantation was available in all countries except Bhutan and Maldives. Hemodialysis was the dominant modality of long-term dialysis, peritoneal dialysis was more expensive than hemodialysis, and kidney transplantation overwhelmingly depended on living donors. Bhutan provided public funding for kidney replacement therapy (dialysis and transplantation); Sri Lanka, India, Pakistan, and Bangladesh had variable funding mechanisms; and Afghanistan relied solely on out-of-pocket expenditure. There were shortages of health care personnel across the entire region. Reporting was variable: Afghanistan and Sri Lanka have dialysis registries but publish no reports, whereas Bangladesh has a transplant registry. South Asia has a large, but poorly documented burden of CKD. Diabetes and hypertension are the major causes of CKD throughout the region with a higher prevalence of infectious causes in Afghanistan and a high burden of CKD of an unknown cause in Sri Lanka and parts of India. The extent and quality of care delivery is suboptimal and variable. Sustainable strategies need to be developed to address the growing burden of CKD in the region.
Keywords: chronic kidney disease, dialysis, kidney failure, kidney registries, kidney transplantation
In recent years, causes of death and disability in the South Asia region have shifted from infectious diseases and reproductive conditions to noncommunicable diseases (NCDs) and injuries. Data from the World Health Organization Global Health Observatory show that across different countries in the region, 33.2% to 79.9% of mortality was attributed to NCDs in 2016.1 Whereas cardiovascular disease, stroke, cancer, and diabetes have received attention, the growing contribution of chronic kidney disease (CKD) to morbidity and mortality in the region is less widely acknowledged in the response by the national health ministries in the region. According to the Global Burden of Disease Study 2017, the number of CKD deaths increased 42% worldwide between 1990 and 2017. In South Asia, 9,459,473 disability-adjusted life years—26% of all disability-adjusted life years worldwide—were attributable to CKD in 2017.2 The region is also witnessing a rapid rise in diabetes and hypertension, 2 major CKD risk factors.3,4 Emerging risk factors exacerbated by climate change are likely to further compound the already large CKD burden in the region.5
Addressing the growing disease burden in the South Asia region is complicated by weak and unorganized health systems, inadequate preparedness and response capabilities, deficient quality of care, and poor data systems. Primary health systems focus mainly on managing infections and providing maternal and newborn care. In recent years, some countries have announced policies to address NCDs, but have failed to include CKD. A major reason for this is lack of data. Unlike other parts of the world, there are no national registries for kidney diseases in the region.6
This report presents findings from the second edition of the International Society of Nephrology Global Kidney Health Atlas (ISN-GKHA), a multinational project conducted to assess capacity and availability of kidney care across different regions via cross-sectional surveys. We describe the disease burden, as well as the available infrastructure and workforce to care for patients with kidney disease in South Asia. The methodology for this research is described in detail elsewhere.7
Results
Results of this study are presented in tables and figures and broadly summarized into 2 categories: desk research (Tables 18, 9, 10, 11, 12, 13 and 214, 15, 16, 17, 18, 19, 20, 21, Figure 1, and Supplementary Table S1) and survey administration (Figure 2, Figure 3, Figure 4 and Supplementary Figure S1).
Table 1.
Demographics, economic and health indicators, and annual cost of kidney replacement therapy in South Asia8, 9, 10, 11, 12, 13
| Country | Population (millions) | Life expectancy (yr) | Growth rate (annual %) | Total GDP (PPP), $ billiona | Per capita GDPa | Health care expenditures, % GDPa | Annual cost KRTb (US$) and out-of-pocket cost/% paid by patient from total costc |
HD/PD cost ratio | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HD | PD | KT (first year) | KT (later years) | ||||||||
| South Asia, median [IQR] | 5202 [4873−9849] | 8764 [7913−12,230] | 6262 [3285−9238] | — | 0.6 | ||||||
| Afghanistan | 34.9 | 64 | −1.4 | 69.5 | 520.9 | 10.2 | —/0 | — | —/0 | — | — |
| Bangladesh | 159.4 | 72 | 6.7 | 690.3 | 1698.3 | 2.4 | 5202/>75 | 7219/100 | 3285/>75 | — | 0.7 |
| Bhutan | 0.7 | 71 | 1.8 | 7.2 | 3243.2 | 3.5 | —/0 | —/0 | — | — | — |
| India | 1296.8 | 69 | 5.7 | 9474.0 | 2010.0 | 3.9 | 9849/51–75 | 15,538/>75 | 9238/51−75 | 10,367 | 0.6 |
| Maldives | 0.3 | 78 | 2.9 | 6.9 | 10,330.6 | 10.6 | 10,400 | — | — | — | — |
| Nepal | 29.7 | 70 | 4.9 | 79.2 | 1033.9 | 6.1 | 2727/51−75 | —/>75 | —/51−75 | — | — |
| Pakistan | 207.8 | 67 | 3.7 | 1061.0 | 1482.4 | 2.7 | 4873/51−75 | 8606/— | —/51−75 | — | 0.6 |
| Sri Lanka | 22.5 | 77 | 2.1 | 275.8 | 4102.5 | 3.0 | 7000/26−50 | 8361/1−25 | 7596/1−25 | 5313 | 0.8 |
—, Data not reported/unavailable; GDP, gross domestic product; HD, hemodialysis; IQR, interquartile range; KT, kidney transplantation; PD, peritoneal dialysis; PPP, purchasing power parity.
Estimates are in US$ 2017.
Detailed reference list for the annual cost of KRT is available in the Supplementary Appendix.
Cost is in US$ 2016.
Table 2.
Capacity for kidney replacement therapy modalities and nephrology workforce statistics in South Asia14, 15, 16, 17, 18, 19, 20, 21
| Country | Long-term HD centers (pmp) | Long-term PD centers (pmp) | KT availability | Transplant centers (pmp) | Nephrologists (pmp) | Nephrology trainees (pmp) |
|---|---|---|---|---|---|---|
| South Asia, median [IQR] | 1.4 [0.6−1.7] | 0.2 [0.0−0.2] | ✓ | 0.1 [0.1−0.2] | 1.2 [0.6−1.4] | 0.23 [0.2−0.6] |
| Afghanistan | 0.3 | — | ✓ | 0.1 | 0.1 | — |
| Bangladesh | 0.6 | 0.0 | ✓ | 0.0 | 0.9 | 0.3 |
| Bhutan | 3.9 | 1.3 | — | — | 1.3 | 0.0 |
| India | 1.4 | 0.2 | ✓ | 0.2 | 1.4 | 0.2 |
| Nepal | 1.7 | 0.2 | ✓ | 0.1 | 1.7 | 0.3 |
| Pakistan | 0.6 | 0.0 | ✓ | 0.1 | 0.6 | 1.1 |
| Sri Lanka | 1.7 | 0.1 | ✓ | 0.5 | 1.2 | 0.89 |
| Maldives | 10.0 | — | — | — | 10.0 | — |
—, Data not reported/unavailable; ✓, yes; HD, hemodialysis; IQR, interquartile range; KT, kidney transplantation; PD, peritoneal dialysis; pmp, per million population.
Figure 1.
Map of countries in South Asia participating in the International Society of Nephrology Global Kidney Health Atlas survey.
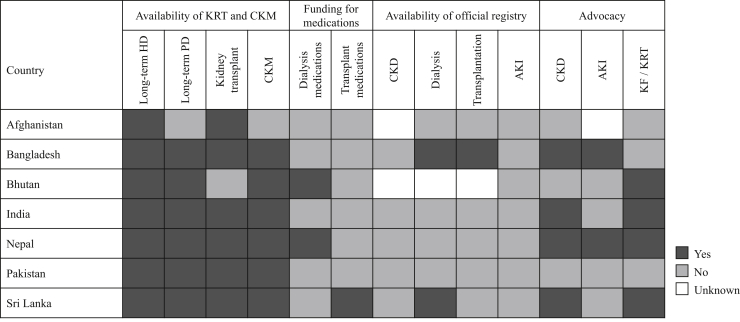
Figure 2.
Country-level scorecard on the availability of kidney care services, registries, funding, and workforce in South Asia. AKI, acute kidney injury; CKD, chronic kidney disease; CKM, conservative kidney management; HD, hemodialysis; KF, kidney failure; KRT, kidney replacement therapy.
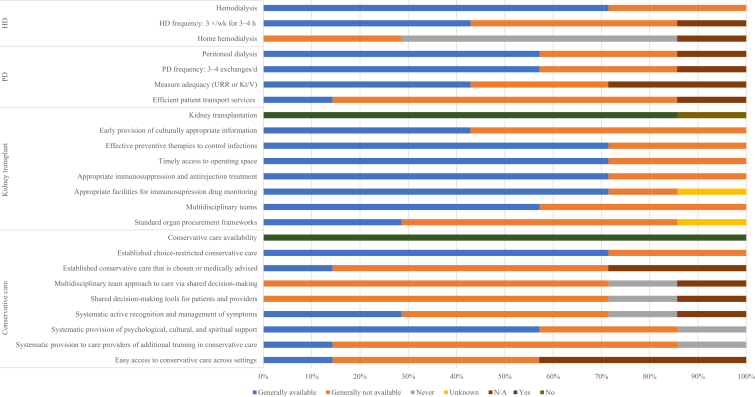
Figure 3.
Availability of services within dialysis care and conservative kidney management in the South Asia region. Values represent the absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not provided; PD, peritoneal dialysis; URR, urea reduction ratio.
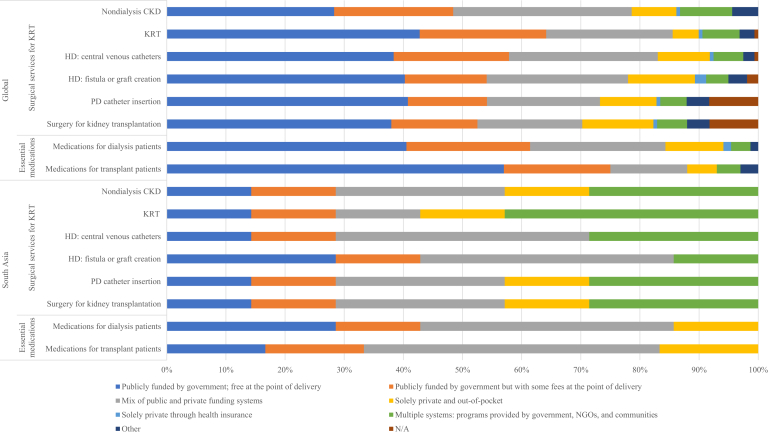
Figure 4.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT) care globally and in the International Society of Nephrology South Asia region. Depicted as percentage of contribution of each structure. HD, hemodialysis; N/A, not provided; NGOs, nongovernmental organizations; PD, peritoneal dialysis.
Setting
The ISN South Asia region (Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka) is home to almost one-quarter of the world’s population, distributed across just 3% of the global land area (Figure 1). The total population of the region represented here is approximately 1.75 billion. Table 18, 9, 10, 11 presents data regarding important socioeconomic and health indicators in these countries. The World Bank categorizes Afghanistan and Nepal as low-income; Bangladesh, Bhutan, India, and Pakistan as lower-middle-income; and Sri Lanka and the Maldives as upper-middle-income countries.10 This region ranks second in global poverty, with large income inequalities reflected by Gini index values ranging from 35 to 40.22 Except Bhutan and Afghanistan, all countries are amongst the 20 most densely populated regions in the world. The region is highly diverse in terms of culture, language, and dietary habits. Economies in all South Asian countries are primarily agrarian, with 53% to 80% of the populations living in rural areas.
Sixteen respondents completed the online questionnaire. Of these, 11 (69%) were nephrologists, 3 (19%) were non-nephrologist physicians, and 2 (13%) were administrators/policy makers, with an overall response rate of 94.1%.
A review of the current state of kidney care in the region
Several small studies have described the burden of CKD and its underlying etiology in some South Asian countries.14, 15, 16, 17, 18, 19,23 Representative national data documenting existing kidney disease management programs, workforce availability, and support for kidney care were not available from any country.
Burden of CKD and kidney failure in South Asia
The prevalence of CKD in South Asia ranged from 5.01% (95% confidence interval: 4.63−5.46) in Afghanistan to 13.24% (95% confidence interval: 12.26−14.31) in Sri Lanka. Data regarding disease prevalence, prevalence of risk factors, morbidity, and mortality in each country are presented in Supplementary Table S1. India and Pakistan had the highest proportion of death and disability-adjusted life years due to CKD.14 ISN-GKHA desk research data were available for 3 CKD risk factors: obesity, high blood pressure, and smoking. Data on the prevalence of total treated kidney failure (KF) were available only for Bangladesh (117 per million population [pmp]). Findings from a population-based study had shown the age-adjusted incidence of KF in India to be 226 pmp.14
Data on the burden of long-term dialysis were available for less than half of the countries in the survey. Hemodialysis (HD) was the dominant modality of long-term dialysis. Bangladesh reported the highest prevalence of long-term dialysis at 113 pmp, followed by India (49.2 pmp), Pakistan (53.3 pmp), and Nepal (11.6 pmp).14,17,18 A recent review, published after the ISN-GKHA survey, estimated the number of patients receiving dialysis in Afghanistan (5000), Bangladesh (18,000), Bhutan (140), India (174,478), Nepal (2500), Pakistan (8381), and Sri Lanka (5482).14 Kidney transplantation (KT) in South Asia overwhelmingly depended on living donors. As per recent data from the Global Observatory on Donation and Transplantation, the annual number of kidney transplants was 5.48 pmp in India and 5.09 pmp in Pakistan.20 The aforementioned review also reported the number of transplants performed within the last year in Bangladesh (130), Bhutan (0), India (6857), Nepal (312), Pakistan (476), and Sri Lanka (267).14 Data on the availability of kidney care services in the countries of South Asia region are presented in Figure 2.
Health finance and service delivery
Long-term HD was available in all countries in the South Asia region. Peritoneal dialysis (PD) and conservative care were available in all countries in the region except Afghanistan; Bhutan and Maldives did not have any KT services. Data on the capacity for kidney replacement therapy (KRT; dialysis and/or transplantation) in the South Asia region are presented in Table 2.14, 15, 16, 17, 18, 19, 20 A comparison of the availability of services within dialysis care and conservative kidney management globally and in South Asia is shown in Figure 3.
Six of the 8 countries surveyed provided data on the annual cost (in US$ 2016) of KRT (Table 1).12,13 The annual cost of HD was highest in Sri Lanka ($26,242), nearly 3 times more than the annual cost of HD in the country. In India, the annual cost of PD ($15,538) was higher than the annual cost of HD ($9,849). India and Bangladesh provided data on the cost of KT in the first year; these figures compare favorably with the annual cost of HD in these countries, and Bangladesh reported lower absolute values than India. The average cost of KT in South Asia varies from a minimum of $700 in government-funded hospitals to $15,000 in private hospitals. The yearly maintenance cost for post-transplant drugs in the region amounts to $15,118 in the first year and $10,367 in later years.12,13
Expenditures for nondialysis CKD care were covered entirely by public funds in Bhutan, whereas in Sri Lanka, expenditures were publicly funded with some fees at the point of care delivery (Figure 4). Multiple funding systems were in place in India and Bangladesh. Pakistan and Nepal also had a mix of public and private funding systems. In Afghanistan, treatment was provided solely in private hospitals, with patients paying for all costs. Funding for KRT in India, Pakistan, and Bangladesh was based on a mix of public and private funding mechanisms and out-of-pocket expenditure. Bhutan and Nepal had a public funding mechanism for dialysis, whereas Sri Lanka provided public funding for transplant medication. India recently launched a National Dialysis Program that provides public funding for dialysis for those whose incomes fall below a certain level (Figure 4).
Health workforce for nephrology care
A range of providers (e.g., nephrologists, primary care physicians, and multidisciplinary teams) were involved in the provision of CKD care. In Afghanistan and Bhutan, the majority of CKD care was provided by primary care physicians and multidisciplinary teams, respectively. Nephrologists were primary CKD care providers in other countries in the region. Overall, nephrologists constituted 70% of CKD care providers. Afghanistan had the fewest nephrologists relative to the population (0.14 pmp), whereas Maldives had the highest (10 pmp) in the region. Except Afghanistan, Bhutan, and Maldives, all countries had nephrology training programs. Data on the density of nephrologists and nephrology trainees in the region are presented in Table 2.21 A comparison to the first edition of the ISN-GKHA (2017) reveals that the population-adjusted number of nephrologists has risen in all countries in the region except Pakistan.24
Supplementary Figure S1 presents data based on respondents’ subjective assessment of the number of kidney care professionals relative to needs in the region. It revealed shortages of all types of KF care providers, including nephrologists, transplant surgeons, HD access surgeons, PD access surgeons, radiologists, laboratory technicians, dieticians, vascular access coordinators, counselors/psychologists, transplant coordinators, dialysis nurses, and dialysis technicians across all countries in South Asia except Bhutan. Bhutan reported no shortage of PD access surgeons, laboratory technicians and dieticians, radiologists for ultrasound, dialysis nurses, or dialysis technicians, but did report shortages of all other types of KF care providers.
Essential medications and health product access for KF care
Long-term HD services were available but inadequate in all countries. The average number of HD treatment centers in the region was 1.21 pmp (Table 2).14, 15, 16, 17, 18, 19, 20 Services for PD care were generally available in India, Pakistan, Nepal, and Bangladesh. The average number of PD treatment centers in the region was 0.18 pmp. KT was available in all countries except Bhutan and the Maldives. The average number of KT centers in the region was 0.16 pmp. Home HD was generally unavailable in the region, except in India and Sri Lanka, which had a few patients using this modality. Conservative care, either chosen or medically advised, was generally available in Sri Lanka; less so in Afghanistan, Bhutan, India, and Nepal; and completely unavailable in Bangladesh and Pakistan (Figure 3).
None of the countries in the South Asia region had a national transplant waitlist. Regional or hospital-based transplant waitlists were available only in India. Both living and deceased donor transplant services were available in India, Pakistan, and Sri Lanka, whereas Afghanistan, Bangladesh, and Nepal relied solely on living donor programs.
Standard of care immunosuppressants for KT are generally available in India, Pakistan, and Bangladesh. The availability of cheaper generic drugs in India reduces the cost of immunosuppression. Funding mechanisms for medications for KT maintenance differ somewhat from those for dialysis, as shown in Figure 4. Costs of KT medications were covered by public funding in Sri Lanka and Nepal, with patients paying some fees in Nepal. Bangladesh, India, and Pakistan had mixed public and private funding systems that cover only 25% to 50% of the population needing KRT, with the rest relying on out-of-pocket expenditure. As for dialysis medication, KT medication was covered solely by private out-of-pocket expenditure in Afghanistan.
Health information systems, statistics, and national health policy
National strategies for NCDs were in place in less than one-third of countries in the South Asia region and were being developed in others. Sri Lanka had an official registry for dialysis and KT, but the data were incomplete, and reports were not published. Some form of data recording system for dialysis was available in Afghanistan, and a transplant registry was available in Bangladesh.
Discussion
This analysis of data from the second edition of the ISN-GKHA highlights inadequacies in the existing domains of kidney care from detection and management of early stages of CKD to providing contextually appropriate care for those with advanced KF. Particularly striking is the urgent need to restructure health systems to support the changing disease burden, low spending, severe shortages of health care workers for kidney care, and the absence of robust data collection systems to inform health policies and monitor progress.
In terms of disease burden, representative national data were not available for any countries in the region. Current estimates are based on scattered surveys and the Global Burden of Disease report, which is based on modeled data. Accurate recording of the cause of death, the most robust indicator of the effect of a disease on populations, is quite immature in all countries. Data from the Million Death Study in India25 show high mortality rates due to KF amongst diabetics in their 40s. Although not captured in this survey, there is a need to identify region-specific unique CKD risk factors such as environmental factors (e.g., air pollution,26 outdoor heat stress,5 and agrochemicals), impact of low birth weight due to maternal malnutrition and the resultant low nephron endowment,27 and prevalent infections like leptospirosis.
Although many South Asian countries conduct health surveys, such as the National Family Health Survey and District Level Household Survey in India, and Demographic and Health Surveys in Pakistan, Bangladesh, Sri Lanka, and Nepal,13,21,24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 none of these surveys collect information on kidney disease. The current study also did not allow subnational disaggregation of data. A 2012 report of the Indian CKD registry showed regional variations in the patterns of disease.16 Similarly, the MDS showed differences in the death rate due to CKD in different parts of India.25 An interesting observation is the geographically clustered description of CKD of uncertain etiology described in Sri Lanka and certain areas in the southern and eastern states of India.16 A recent population-based study from an endemic region reported a prevalence of 21%.35 Despite work by several groups, no progress has been made toward the identification of its etiology.
KRT modalities are generally available in South Asian countries. However, availability is not synonymous with equitable access. India, Pakistan, and Bangladesh are amongst the 10 most populous countries and have major within-country regional variations. It has been shown that the epidemiologic transition, whereby major communicable diseases and conditions of poverty are progressively replaced by NCDs over time, occurs at different times in different parts of a country, a phenomenon that contributes further to variations within the South Asia region.36
The report shows wide variation in the prevalence of patients receiving long-term dialysis in different countries. There are no good explanations for this variability. In fact, the 2 countries with more liberal funding policies for dialysis have relatively low rates of uptake, indicating that simply removing the financial barrier at the point of care does not improve access to this life-saving treatment. A study from India suggests that the year-on-year uptake of dialysis increases when the financial barrier is removed, but outcomes do not necessarily get better, as approximately 60% of patients stopped treatment within 1 year of starting dialysis.37 This implies that beyond financial constraints, other socioeconomic issues such as travel costs, medication costs, and time away from work may play a vital role in the utilization of KF care services. Recently, the Indian government announced an ambitious national program to provide dialysis either free or at highly subsidized prices to all citizens. Still, these programs do not cover the cost of medications, which are covered through a mix of private and public funds. This is in stark contrast to global norms, as in most countries, public funding covers such medications.
These findings also highlight the inadequacy and variability in funding for kidney care and a shortage of kidney care providers. The 3 countries with the highest gross domestic product in the region have the lowest investment in terms of the proportion of gross domestic product expenditure for health care.10 Despite compelling data and unique challenges like CKD of uncertain etiology, none of the countries in the region have a national strategy to address the growing CKD burden. This is reflected in the multitude of ways by which patients with CKD in the region fund their care, and the high prevalence of catastrophic health care expenditure as well as distress financing for those requiring KRT.38,39
In their analysis of the Global Burden of Disease data, Xie et al.40 showed that 7 of the 8 South Asian countries were in the bottom 50% of all 196 countries in terms of the gap between the observed disease burden and potentially achievable burden with optimal care, given their level of development, with 2 being in the bottom 10.
In general, all types of KRT cost much less in this region than in other parts of the world. However, there is substantial variation in the relative utilization and costs of individual modalities. PD is more expensive than HD in India,41 Pakistan, Bangladesh, and Sri Lanka. These variations can be explained by how costs are calculated by respondents. In public funding systems, HD costs are heavily subsidized, whereas all costs for PD are passed on to patients. The government levies duties on imported PD components, which further increases the price. As most of the reported costs in the survey reflect costs to patients rather than the total costs of therapy, PD is reported as being more expensive. In a study from India, researchers estimated the overall cost of HD to the system and found it to be 2 to 3 times greater than that previously reported.41
KRT programs in all countries of the region are dominated by HD. Globally, PD is considered to be less expensive for health systems to administer; hence, it would be expected that emerging economies of South Asia would embrace this modality, as has been done by countries such as Thailand and Mexico. However, in South Asia, patients on HD outnumber those on PD by 9 to 1. The likely reasons are a lack of insurance coverage, disinclination of nephrologists to prescribe PD due to a lack of expertise and incentives to favor HD, a lack of awareness and preference for in-hospital services over domiciliary care, inconsistent supply of PD solutions and other consumables, and a lack of housing conditions conducive to home therapy.42 Home HD is practically nonexistent in the region. In recent months, the government of India has brought PD under the ambit of the National Dialysis Program, with the hope that it might improve access to KRT among patients living in remote areas, but this requires the workforce to be trained in PD practice and for barriers to reimbursement for PD to be overcome.
Despite large demand, KT rates in the region are relatively low, ranging from 0.18 to 14.08 pmp annually.20 Furthermore, transplantation activity largely depends on organs from living donors. Deceased donor programs are patchy, and there are few national or regional transplant waitlists. It is worth pointing out that even as a large proportion of the local population remains disenfranchised, India is considered an important destination for patients from overseas for “cheap” transplant surgery. Until recently, different countries in the region had been considered hubs for transplant tourism at different times.43,44 However, with the enactment of legislation banning such transplants, this practice has decreased substantially.
The available workforce is quite inadequate to address the needs of the large number of patients in the region, as evidenced by the low number of nephrologists (0.14−1.68 pmp), relative to developed countries (23.2 pmp).21 There are also shortages of other personnel involved in kidney care (dialysis nurses, dialysis technicians, KT surgeons, HD and PD access surgeons, intervention radiologists, laboratory technicians, dieticians, radiologists, vascular access coordinators, counselors/psychologists, and transplant coordinators). Reflecting this shortage, health care providers who do not have specialized nephrology training (e.g., general physicians, endocrinologists, and practitioners of traditional systems of medicine) often address the medical needs of patients with CKD. Nephrology training programs do exist in most of the countries in the region, but given the low number of trainees, it will take a long time before the population density of nephrologists in South Asia comes anywhere close to that in the Western world. Furthermore, what is not evident from this country level analysis is the uneven distribution of the trained health care workforce, with particularly large deficiencies in rural areas. This indicates the need to adopt flexible approaches to managing patients with CKD at different stages of disease. As with other NCDs, during early stages of CKD, care can be provided by more ubiquitous nonphysician health care workers such as nurses and other frontline health workers with the help of standardized algorithms and checklists to perform risk stratification, provide standardized recommendations, make appropriate referrals, and perform follow-up to ensure treatment adherence. Such an approach frees up nephrologists to optimally use their skills, for example, to develop treatment plans, prepare patients for KRT, and manage special situations and complications. The ISN-GKHA data show, however, that these “physician extender” providers have not been used to provide kidney care in the region thus far, indicating a missed opportunity.
Finally, because of a lack of registries, the incidence and prevalence of KF and outcomes for dialysis patients cannot be accurately estimated. Overall, transplant waitlists are not available in 62.5% (n = 5) of countries in the South Asia region compared with a global unavailability of 19%. National waitlists are not available in any countries in the region, whereas regional waitlists are available in only 37.5% (n = 3) of countries in the region. Even though Sri Lanka reports having a dialysis and kidney transplant registry and Bangladesh records its transplant data, neither country publishes data in any form. Similarly, the National Organ and Tissue Transplant Organization (https://notto.gov.in/), which is mandated to collect data on all transplants in India, has failed to produce a single report over the 10 years of its existence. The lack of registries hampers the abilities of policy makers in these countries to engage in long-term planning and make decisions about resource allocation.
In the absence of national registries in all countries of the region, the ISN-GKHA project provides vital information on disease burden, availability, and organization of health care services for the management of KF in the region. These data are of paramount importance in planning strategies for tackling the growing burden of kidney disease and provide a basis for the national and international bodies to suggest measures that can help in formulating policies dedicated to improving access to health care for patients with KF. National and regional leaders should use these data for advocacy and draw the attention of policy makers to address the prevalent deficiencies in care. A regular system of data collection through robust and functional registries to inform resource planning should be instituted. The SharE-RR project of the International Society of Nephrology is developing essential datasets and a toolkit for setting up registry that can be adapted by countries in the region.45 National nephrology societies should advocate for making registries an essential part of dialysis services with possible linkages to reimbursement in their respective countries. All registries should regularly publish reports. Registry operations should be appropriately resourced, the staff trained, and quality checks should be incorporated.46
In conclusion, South Asia, which is home to approximately 25% of the world’s population, has a large, but poorly documented burden of CKD. The extent and quality of care delivery are suboptimal and variable, thereby imposing economic hardships on the population and resulting in poor outcomes. The failure of South Asian countries to adequately address the burden of CKD is likely to have a major adverse impact on global metrics of kidney care. This is a call to action, not only for national governments, but also for professional societies, multilateral agencies, and donors to support the development of sustainable strategies to address the growing burden of CKD in the region.
Disclosure
DWJ reports grants and personal fees from Baxter Healthcare and Fresenius Medical Care; travel sponsorship from Amgen; personal fees from Astra Zeneca, AWAK, and Ono; and grants from National Health and Medical Research Council of Australia, outside the submitted work. VJ reports grants from GlaxoSmithKline and Baxter Healthcare, provides scientific leadership to George Clinical, and consultancy fees for Biocon, Zudis Cadilla, and NephroPlus, all paid to his institution, outside the submitted work. All the other authors declared no competing interests.
Acknowledgments
This article is published as part of a supplement supported by the International Society of Nephrology (ISN; grant RES0033080 to the University of Alberta).
The ISN provided administrative support for the design and implementation of the study and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
We thank Kara Stephenson Gehman in ISN-GKHA for carefully editing the English text of a draft of this manuscript; Jo-Ann Donner, coordinator at the ISN, for her prominent role and leadership in the manuscript management, editorial reviews, and submission process to Kidney International Supplements; and Sandrine Damster, senior research project manager at the ISN, and Alberta Kidney Disease Network staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for helping to organize and conduct the survey and for providing project management support. We also thank the ISN headquarters staff including the Executive Director Charu Malik and the Advocacy team. We also appreciate the support from the ISN’s Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN-GKHA survey.
Footnotes
Table S1. Burden of chronic kidney disease and its risk factors in South Asia.
Figure S1. Shortages of kidney failure care providers in South Asia, as per the subjective ISN-GKHA survey.
Supplementary Appendix. Reference list for annual cost of kidney replacement therapy (for Table 1).
Supplementary Material
References
- 1.World Health Organization NCD mortality and morbidity. 2016. https://www.who.int/gho/ncd/mortality_morbidity/en/ Available at:
- 2.Bibkov B., Purcell C.A., Levey A.S. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. doi: 10.1016/S0140-6736(20)30045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jayawardena R., Ranasinghe P., Byrne N.M. Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health. 2012;12:380. doi: 10.1186/1471-2458-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta R., Gaur K., CV S.R. Emerging trends in hypertension epidemiology in India. J Hum Hypertens. 2019;33:575–587. doi: 10.1038/s41371-018-0117-3. [DOI] [PubMed] [Google Scholar]
- 5.Glaser J., Lemery J., Rajagopalan B. Climate change and the emergent epidemic of CKD from heat stress in rural communities: the case for heat stress nephropathy. Clin J Am Soc Nephrol. 2016;11:1472–1483. doi: 10.2215/CJN.13841215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu F.X., Rutherford P., Smoyer-Tomic K. A global overview of renal registries: a systematic review. BMC Nephrol. 2015;16:31. doi: 10.1186/s12882-015-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bello A.K., Okpechi I.G., Jha V. Understanding distribution and variability in care organization and services for the management of kidney care across world regions. Kidney Int Suppl. 2021;11 e4–e10. [Google Scholar]
- 8.Central Intelligence Agency. The world factbook. Available at: https://www.cia.gov/the-world-factbook/. Published 2019. Accessed March 11, 2021.
- 9.World Health Organization The Global Health Observatory. Published 2019. https://www.who.int/gho/en/ Available at:
- 10.World Bank GDP ranking. 2019. https://datacatalog.worldbank.org/dataset/gdp-ranking Available at:
- 11.Institute for Health Metrics and Evaulation Global Burden of Disease (GBD). Global Burden of Disease study. 2016. http://www.healthdata.org/gbd Available at:
- 12.Khanna U. The economics of dialysis in India. Indian J Nephrol. 2009;19:1–4. doi: 10.4103/0971-4065.50671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abraham G., John G.T., Sunil S. Evolution of renal transplantation in India over the last four decades. NDT Plus. 2009;3:203–207. [Google Scholar]
- 14.Jha V., Ur-Rashid H., Agarwal S.K. The state of nephrology in South Asia. Kidney Int. 2019;95:31–37. doi: 10.1016/j.kint.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Singh A.K., Farag Y.M., Mittal B.V. Epidemiology and risk factors of chronic kidney disease in India—results from the SEEK (Screening and Early Evaluation of Kidney Disease) study. BMC Nephrol. 2013;14:114. doi: 10.1186/1471-2369-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rajapurkar M.M., John G.T., Kirpalani A.L. What do we know about chronic kidney disease in India: first report of the Indian CKD registry. BMC Nephrol. 2012;13:10. doi: 10.1186/1471-2369-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imtiaz S., Salman B., Qureshi R. A review of the epidemiology of chronic kidney disease in Pakistan: a global and regional perspective. Saudi J Kidney Dis Transpl. 2018;29:1441–1451. doi: 10.4103/1319-2442.248307. [DOI] [PubMed] [Google Scholar]
- 18.Hasan M., Sutradhar I., Gupta R.D., Sarker M. Prevalence of chronic kidney disease in South Asia: a systematic review. BMC Nephrol. 2018;19:291. doi: 10.1186/s12882-018-1072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abraham G., Varughese S., Thandavan T. Chronic kidney disease hotspots in developing countries in South Asia. Clinl Kidney J. 2016;9:135–141. doi: 10.1093/ckj/sfv109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global Observatory on Donation and Translantation (GODT) Summary. 2020. http://www.transplant-observatory.org/summarys/ Available at:
- 21.Bello A., Levin A., Lunney M. Current status of end-stage kidney disease care in world countries and regions-an international survey. BMJ. 2019;367:15873. doi: 10.1136/bmj.l5873. [DOI] [PubMed] [Google Scholar]
- 22.World Bank World Bank Open Data. 2020. http://data.worldbank.org/indicator Available at:
- 23.Ranasinghe A.V., Kumara G., Karunarathna R.H. The incidence, prevalence and trends of chronic kidney disease and chronic kidney disease of uncertain aetiology (CKDu) in the North Central Province of Sri Lanka: an analysis of 30,566 patients. BMC Nephrol. 2019;20:338. doi: 10.1186/s12882-019-1501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bello A.K., Levin A., Tonelli M. International Society of Nephrology; Global Kidney Health Atlas: a report by the International Society of Nephrology on the current state of organization and structures for kidney care across the globe. Brusels, Belgium: 2017. Global Kidney Health Atlas: a report by the International Society of Nephrology on the current state of organization and structures for kidney care across the globe. [Google Scholar]
- 25.Dare A.J., Fu S.H., Patra J. Renal failure deaths and their risk factors in India 2001-13: nationally representative estimates from the Million Death Study. Lancet Global Health. 2017;5:e89–e95. doi: 10.1016/S2214-109X(16)30308-4. [DOI] [PubMed] [Google Scholar]
- 26.Bowe B., Xie Y., Li T. Particulate matter air pollution and the risk of incident CKD and progression to ESRD. J Am Soc Nephrol. 2018;29:218–230. doi: 10.1681/ASN.2017030253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luyckx V.A., Brenner B.M. Birth weight, malnutrition and kidney-associated outcomes: a global concern. Nat Rev Nephrol. 2015;11:135–149. doi: 10.1038/nrneph.2014.251. [DOI] [PubMed] [Google Scholar]
- 28.Abariga S.A., Khachan H., Al Kibria G.M. Prevalence and determinants of hypertension in India based on the 2017 ACC/AHA guideline: evidence from the India National Family Health Survey. Am J Hypertens. 2020;33:252–260. doi: 10.1093/ajh/hpz181. [DOI] [PubMed] [Google Scholar]
- 29.Vennu V., Abdulrahman T.A., Bindawas S.M. The prevalence of overweight, obesity, hypertension, and diabetes in India: analysis of the 2015-2016 National Family Health Survey. Int J Environ Res Public Health. 2019;16:3987. doi: 10.3390/ijerph16203987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The DHS Program Demographic and Health Hurveys. https://www.dhsprogram.com/What-We-Do/Survey-Types/DHS.cfm Available at:
- 31.National Institute of Population Research and Training (NIPORT) Mitra and Associates, and Macro International 2009. Bangladesh Demographic and Health Survey 2007. https://www.dhsprogram.com/pubs/pdf/FR207/FR207[April-10-2009].pdf Available at:
- 32.Department of Census and Statistics (DCS) and Ministry of Healthcare and Nutrition (MOH) Sri Lanka Demographic and Health Survey 2006–07 Colombo. 2009. https://microdata.worldbank.org/index.php/catalog/1425/study-description Available at:
- 33.Ministry of Health and Population (MOHP) New ERA and Macro International Inc . . 2006. 2007. Nepal Demographic and Health Surveyhttps://dhsprogram.com/pubs/pdf/FR191/FR191.pdf Available at: [Google Scholar]
- 34.Family Health Division, Department of Health Services, Ministry of Health Nepal Family Health Survey. 1996. https://dhsprogram.com/pubs/pdf/FR78/FR78.pdf Available at:
- 35.Gummidi B., John O., Ghosh A. A systematic study of the prevalence and risk factors of chronic kidney disease in Uddanam. Kidney Int Rep. 2020;5:2246–2255. doi: 10.1016/j.ekir.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.India State-level Disease Burden Initiative Collaborators Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390:2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaikh M., Woodward M., John O. Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440–445. doi: 10.1016/j.kint.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 38.Bradshaw C., Gracious N., Narayanan R. Paying for hemodialysis in Kerala, India: a description of household financial hardship in the context of medical subsidy. Kidney Int Rep. 2019;4:390–398. doi: 10.1016/j.ekir.2018.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramachandran R., Jha V. Kidney transplantation is associated with catastrophic out of pocket expenditure in India. PLoS One. 2013;8 doi: 10.1371/journal.pone.0067812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xie Y., Bowe B., Mokdad A.H. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94:567–581. doi: 10.1016/j.kint.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 41.Kaur G., Prinja S., Ramachandran R. Cost of hemodialysis in a public sector tertiary hospital of India. Clin Kidney J. 2018;11:726–733. doi: 10.1093/ckj/sfx152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jha V. Providing dialysis in India: many pieces in the puzzle. Natl Med J India. 2019;32:321–324. doi: 10.4103/0970-258X.279969. [DOI] [PubMed] [Google Scholar]
- 43.Jha V. Paid transplants in India: the grim reality. Nephrol Dial Transplant. 2004;19:541–543. doi: 10.1093/ndt/gfg576. [DOI] [PubMed] [Google Scholar]
- 44.Rizvi S.A., Naqvi S.A., Zafar M.N. Commercial transplants in local Pakistanis from vended kidneys: a socio-economic and outcome study. Transpl Int. 2009;22:615–621. doi: 10.1111/j.1432-2277.2009.00836.x. [DOI] [PubMed] [Google Scholar]
- 45.Hole B.D., Evans K.M., Pyart R. International collaborative efforts to establish kidney health surveillance systems. Kidney Int. 2020;98:812–816. doi: 10.1016/j.kint.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bassi A., John O., Gallagher M. Methodological challenges to collecting clinical and economic outcome data: lessons from the pilot dialysis outcomes India study. Nephrology. 2019;24(4):445–449. doi: 10.1111/nep.13257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.