Abstract
Purpose:
To identify the facilitators and barriers to implementing glaucoma screening programs in two community clinics.
Methods:
A concurrent mixed-methods process analysis using community-engaged research. Key stakeholders—including patients, providers, and staff members—from two community clinics were interviewed using a semi-structured interview guide. Interviews had two parts: 1) asking patients about community-based facilitators and barriers to implementing glaucoma screening and care and 2) eliciting feedback about a personalized coaching program. The transcripts were coded using Grounded Theory. Number of participants and number of representative citations were counted per theme. The qualitative analysis was coded using Dedoose 8.3.17 (Los Angeles, CA).
Results:
Thematic saturation was reached after coding 12 interviews. 30 participants were interviewed, 13 from Hamilton Clinic, (Flint, Michigan), (8 patients, 5 providers and staff members) and 17 from Hope Clinic, (Ypsilanti, Michigan), (6 patients, 11 providers and staff members). The most commonly cited themes were: Priorities (98 citations, 30 participants), Knowledge (73, 26) Transportation (63, 26), Cost (60, 23), and Convenience/Access (63, 22). Broadly applicable barriers to glaucoma care, such as Cost, Transportation, and Trust were identified alongside community-specific barriers such as Language and Convenience/Access. Participants rated their likelihood to follow up with an ophthalmologist after participating in the personalized coaching program at a mean of 8.83 (on a scale of 1 to 10 with 10 being the most confident).
Conclusions:
Community-engaged research enables researchers to identify community-specific barriers and facilitators, allowing more effective program implementation.
Keywords: community engaged research, glaucoma screening, telemedicine
Précis:
Community-engaged research enables researchers to identify community-specific barriers and facilitators to program implementation. Broadly applicable barriers to glaucoma care, such as Cost, Transportation, and Trust, and community-specific barriers, such as Language and Convenience/Access, were identified.
Introduction:
Glaucoma is the leading cause of irreversible blindness globally and is expected to affect approximately 111.8 million people worldwide by 2040.1 In the United States, of the estimated 3.1 million people affected by glaucoma, 2.4 million individuals are thought to have undiagnosed and untreated glaucoma.2 Blacks and Hispanics also have a much greater odds of having their glaucoma go undiagnosed, illustrating a significant racial disparity.2 Consequently African-Americans often present later in their disease course and are twice as likely to have bilateral blindness from glaucoma compared to Caucasians.3 People with lower socio-economic status are at increased risk of developing glaucoma, even after accounting for race, education, and comorbid conditions.4 Despite these findings, the US Preventive Services Task Force, based on the low prevalence of open-angle glaucoma in 2013 (2.1%), concluded that there is insufficient evidence to balance the benefits and risks of population screening adults for open-angle glaucoma.5, 6 Case finding among high-risk populations with greater prevalence of glaucoma – African Americans over 50 years, Hispanics over 65 years, and anyone with a family history of glaucoma – is likely to have a more favorable cost-benefit ratio than population screening, but this benefit is greatly underutilized.7
Currently, glaucoma screening takes place in eye care provider clinics, which tend to be farther from uninsured and underinsured people’s homes and their usual primary care provider. Telemedicine enables specialty glaucoma services to be available at local primary care community clinics by using a local health care worker to obtain basic information and clinical measures and send it to a glaucoma care provider located elsewhere.8 This can make glaucoma screening more accessible and may offer an improved cost-benefit ratio for screening high risk populations. The Technology-based Eye Care Services (TECS) developed in the Department of Veterans Affairs (VA) uses the principles of telemedicine to bring eye care to rural primary care clinics. In this Center for Disease Control Vision Health Initiative program, we use the VA TECS program framework to bring eye care to primary care clinics that serve the under and un-insured: a free clinic and a federally qualified health center. In addition, in our Screening and Intervention for Glaucoma and eye Health through Telemedicine (SIGHT) Program, we have created an eHealth personalized coaching tool which generates personalized educational content about a patient’s test results to enable a health coach – not a physician – to offer tailored education to motivate patients to return for follow-up care if they screen positive for eye disease during their telemedicine eye health screening visit.9, 10
Community-engaged research (CER) provides an opportunity to bridge the gap between research and the targeted population it is intended for. By learning from key stakeholders and patients how to best implement programs to meet the community’s needs, programs based on CER will have greater participation rates and decreased loss to follow-up.11 This method has been used in prior piloted eye screening programs, and was successful in identifying high rates of individuals with undiagnosed glaucoma in two separate high-risk populations.12, 13
The objective of this study is to use CER to assess key stakeholder opinions about best practices, including barriers and facilitators to implementation, to devise a glaucoma screening program and eHealth coaching program to improve adherence to follow-up recommendations after screening in two community clinics.
Methods:
Study sites:
The Screening and Intervention for Glaucoma and eye Health through Telemedicine (SIGHT) Program project will be carried out through a partnership between the University of Michigan Kellogg Eye Center, the Hope Clinic, in Ypsilanti, MI, and the Hamilton Clinic in Flint, MI.
Approximately 5,000 patients access the Hope Clinic per year and 25,000 people access the Hamilton Clinic per year. The Hope Clinic is a free clinic that serves uninsured and underinsured patients. It has a general reception area, medical clinic, dental clinic, food pantry, chapel, laundromat, area for baby supplies, and meeting rooms. Details of the demographics of the Hope Clinic patient population are discussed in detail in a prior study,14 Ypsilanti, MI where Hope Clinic is located has a per capita income was $24,562 in 2018 with over 32% of the population living in poverty.15
Hamilton Clinic in Flint, MI, is the main branch of the Hamilton Community Health Network, a federally qualified health center that serves the population of the greater Flint area through the main clinic and six satellite clinics throughout Genesee and Lapeer counties. It includes a general reception area, a medical clinic, a dental clinic, an eye clinic, a social work department, an obstetrics clinic, a residency training program and meeting rooms. Three-quarters of people served by the Hamilton clinic live at or below the federal poverty level and 96.9% live at or below 200% of the federal poverty level. In terms of insurance, 16.2% are uninsured, 59% have Medicaid, 8.3% have Medicare, and 4.2% are dually eligible for Medicaid and Medicare.16
Both clinics were in Michigan, which through its Medicaid expansion program, Healthy Michigan, provides government-funded health insurance for those people who live at or below 133% of the federal poverty level ($16,000 for a single person or $33,000 for a family of four).17 People who live above the poverty level and who are younger than 65 are expected to have private health insurance. People over the age of 65 who have met citizenship requirements can obtain government-based health insurance coverage through Medicare, which covers roughly 80% of medical expenses, and many people opt to have secondary private insurance coverage for this gap. The Hope Clinic serves a population of people who are under-insured or uninsured, and the Hamilton Clinic serves a population of people who are mainly insured through Medicaid.
Study Population and Interview Process
A purposive sample of eyecare providers, staff members, and patients from the Hope Clinic and the Hamilton Community Health Network Clinic were interviewed. Roles of Hamilton clinic staff members interviewed included one ophthalmologist, one facility manager, one community outreach coordinator, one optician, and one health educator. Roles of Hope clinic staff members interviewed included one director of operations, one receptionist, one referral nurse, two clinic managers, two office managers, one patient support service nurse, one communications manager and one nurse practitioner.
Written informed consent was obtained from all participants. Semi-structured interviews lasted between 30–45 minutes and consisted of two parts. One interviewer completed all of the interviews. During the first part of the interview, the interviewer explored community-specific barriers to eye care and follow-up. Participants were asked how a telemedicine glaucoma screening program could be best implemented into the clinic in order to meet the community’s needs. In the second part of the interview, the interviewer demonstrated the eHealth coaching program with the participant role-playing as a potential patient. The program is written at an 8th grade reading level and the coach reads the written content aloud to participants while showing them audio-visual content on a tablet, using the tablet as a teacher would use a storybook. The interviewer elicited participant’s feedback on the program, including what educational components were most salient in motivating participants to return for glaucoma follow-up care. Patients who participated were provided with a $20 cash card at the end of their interview. Interviews were audio-recorded and transcribed verbatim.
As the data gathered contained no identifiers, the study was determined to be exempt by the University of Michigan Institutional Review Board. This study adhered to all tenets of the Declaration of Helsinki.
Community-Advisory Board
Using the Socio-Ecological Model of Health, a Community Advisory Board composed of clinic patients and various executive members was formed to help guide the proposed glaucoma care program.18 The executive members included key stakeholders from University of Michigan, Hamilton, and Hope clinic. From the University of Michigan, these members were the primary and co-investigators of the study, including a telemedicine specialist, an epidemiologist, a therapist, and three glaucoma specialists. From Hamilton clinic, these members included the Chief Executive Officer, Chief Operating Officer, and head ophthalmologist. From Hope clinic, these members included the medical director, medical clinics manager, and operations manager. The semi-structured interview guide (see Text, Supplemental Digital Content 1) was created after discussion and approval by the executive members of the community advisory board prior to recruiting participants.
Qualitative Analysis
Analysis followed a concurrent mixed-methods approach.19 Qualitative analysis of transcribed interviews was guided by Grounded Theory (GT), an inductive process of generating theories, beginning with qualitative data.20–22 Coders followed a stepwise approach typical of GT: 1) familiarization, 2) open coding, 3) axial coding, 4) focused coding, and 5) theory building.
Once the interviews were finished, two coders (DB, JC) read the transcripts during the familiarization stage in order to become familiar with the interview structure and general topics. Coders determined that thematic saturation, the point at which additional interviews provided no new themes, was reached after analyzing twelve of the thirty finished interviews.23 They then used open coding to identify recurring concepts from the twelve semi-structured interviews. These recurring concepts were defined and a codebook was created. Two coders (DB, JC) then worked separately to code a portion of the transcripts using the codebook, coming together to resolve inconsistences. A third party (PANC) was included when inconsistences could not be resolved between the coders. Once >80% agreement was achieved on >95% of the codes, the two coders re-analyzed and coded the remaining transcripts.24 The instances of these codes were identified, and their relationships were considered during the axial coding process. All coded excerpts were characterized as either facilitators or barriers, if applicable; however, some excerpts were related to a specific theme but were neither a facilitator nor a barrier, and so they were coded without this classification. The total number of times a given barrier or facilitator was expressed and the number of patients who commented on them was tabulated. The qualitative analysis was coded using Dedoose 8.3.17 (Los Angeles, CA).
Results:
Of the 30 individuals interviewed, 13 were from Hamilton Clinic (8 patients, 5 eyecare providers and staff members) and 17 from Hope Clinic (6 patients, 11 eye care providers and staff members). The kappa value for inter-rater reliability between the two coders was 0.93. Frequencies of themes as facilitators (Figure 1) and barriers (Figure 2) were recorded as well as their representative quotes as shown in Supplemental Digital Content 3 (See Table, Supplemental Digital Content 2, which includes frequencies and additional quotes). Five main themes arose in the content analysis of the transcripts: Priorities (number of citations: 98; number of participants: 30), Knowledge (73; 26), Transportation (63;26), Convenience/Access (63; 22), and Cost (60;23).
Figure 1.
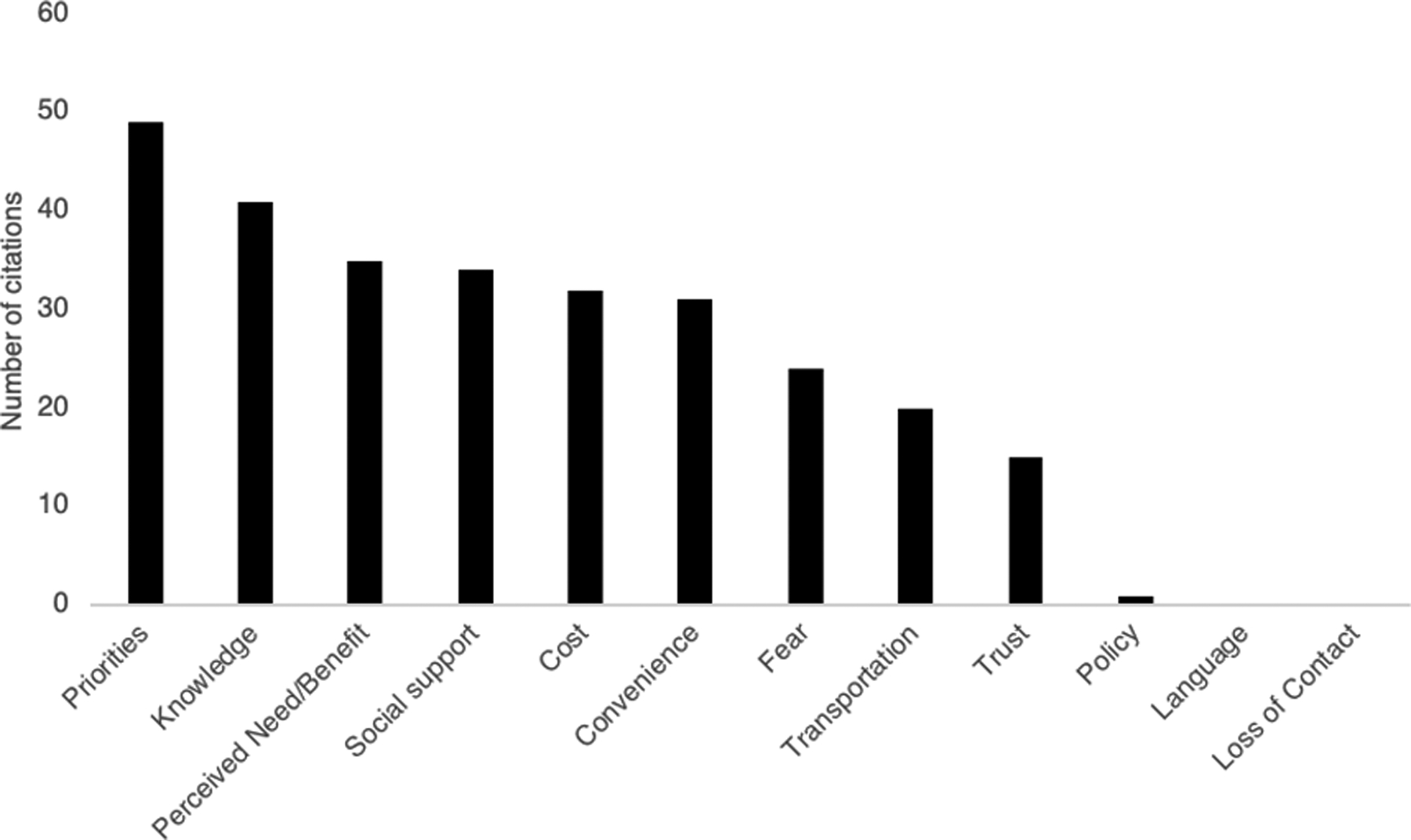
Bar graph showing the number of representative citations per theme when mentioned as a facilitator
Figure 2.
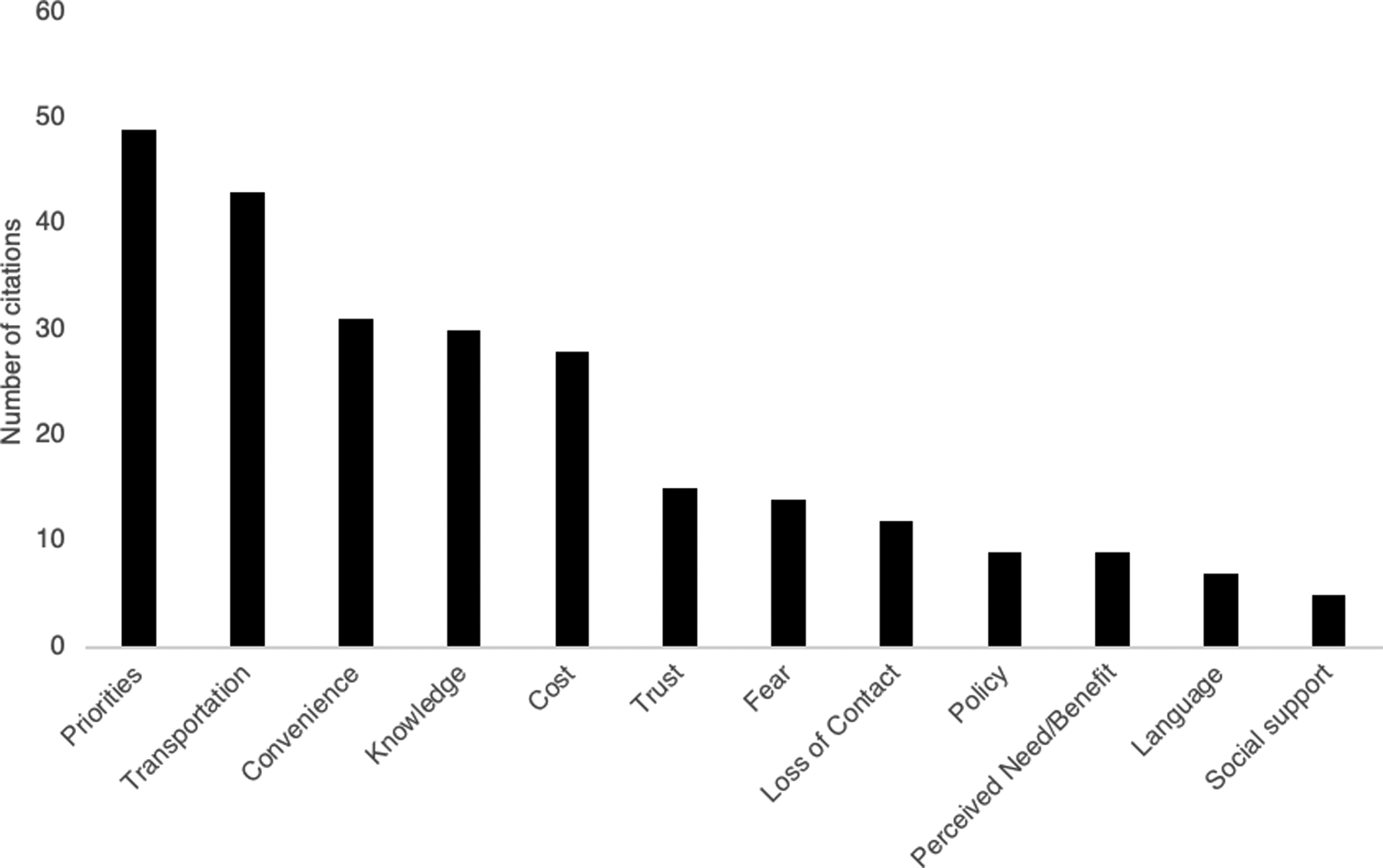
Bar graph showing the number of representative citations per theme when mentioned as a barrier
Priorities:
Priorities was mentioned by all 30 participants for a total of 98 times: 49 times as a barrier (50%) and 49 times as a facilitator (50%). Each person prioritized their vision and health differently. Twenty-three participants mentioned how vision was low on their priority list due to many other competing concerns such as, “bad diabetes, hypertension, kidney problems, dealing with a family member who’s incarcerated and unruly kids, three to four kids.” Other competing priorities that were frequently mentioned included personal issues, childcare, jobs, and other health conditions. Just about as many participants (n=22) mentioned vision as a priority, discussing their vision or overall health as something they value, saying, “I’ve already been [to health screenings], you know, I keep a track of my health because of my age” and “my sight is very, very important to me, I value my sight.”
Knowledge:
Knowledge was mentioned by 26 participants (87%) for a total of 73 times: 30 times as a barrier (41%), 41 times as a facilitator (56%), and 2 times neither as a facilitator nor a barrier (3%). Knowledge was mentioned in two contexts: knowledge of eye disease (mentioned 49 times, 67%) and knowledge of resources (mentioned 24 times, 33%).
Participants expressed how personal knowledge (or lack thereof) of different eye diseases affected their motivation to seek out care. Twelve participants shared how lack of knowledge prevented them and others from seeking out care, such as in the case of one staff member who shared, “because [glaucoma is] painless, people who have it don’t realize it.” Twenty-two participants mentioned how personal experience and symptoms of other eye diseases (i.e. cataracts, low visual acuity) motivated them to seek out glaucoma care. One patient shared how a family member’s recent cataract symptoms motivated him to “take a little bit more interest in [his] eyesight,” and thus seek out glaucoma screening. Others expressed an interest in glaucoma follow-up after learning more about glaucoma during the eHealth program, for example sharing, “But now I listened [I know] that it’s very, very important to check your vision […and] to know if you’ll have glaucoma.”
Seven participants expressed barriers related to knowledge of resources. A participant commented on not getting care as they “didn’t even realize that [there was an] eye center here.” A staff participant remarked, “They don’t really take advantage of what’s here, you know, because if the information doesn’t come directly to them, they don’t seek it out.” Eight participants cited knowledge of resources as a facilitator. A staff participant said, “Public knows about [Hope Clinic] and the word has gotten out. So, this [SIGHT] program can certainly help with that also.”
Transportation:
Transportation was mentioned by 26 participants (87%) for a total of 63 times: 43 times as a barrier (68%) and 20 times as a facilitator (32%). Twenty-four participants discussed lack of access to cars or reliable public transportation as barriers, sharing that, “A lot of people don’t have cars, so lot of our people rely on public transportation,” and, “Public transportation […] are out of my control.” Ten participants cited availability of many transportation options to get to the clinics as facilitators to care, specifically mentioning, “Friends, family. Some people [can] use Uber,” or the fact that, “[Hope clinic is] directly on public transportation line with the bus stop being right out front.”
Cost:
Cost was mentioned by 23 participants (76%) for a total of 60 times: 28 times as a barrier (47%) and 32 times as facilitator (53%). Fifteen participants cited high out of pocket cost without insurance, high co-pay, and medication expense as important barriers to care, as reflected in the quotes, “I haven’t met a doctor for two years. Because I didn’t have any vision insurance,” and, “Am I going to have to pay for that medication? Some of them can be very expensive…” Nineteen participants mentioned how the SIGHT program being completely free will help patients seek out care. For example, “You know, if you need that help and is offered to you free, any person would go and get that help.”
Convenience/Access:
Convenience or access was mentioned by 22 participants (73%) 63 total times; 31 times as a barrier (50%), 31 times as a facilitator (50%), and 1 time neither as a facilitator nor a barrier (2%). Sixteen participants mentioned how long wait times, difficulty scheduling, and inaccessible clinic locations served as barriers to care. One patient described the situation as, “You’re 10 minutes behind or the bus 10 minutes behind. Bam, I have got to wait a whole another two, three months, you know, to get help.” Seventeen participants mentioned close proximity of clinics and availability of specific popular time slots (usually 4pm) as facilitators. This sentiment is reflected in the quotes, “but having something that simple on site, immediate, understandable, I think that’s a huge benefit,” and, “if [the time slot] is convenient for me, then yeah, I will take it.”
Remaining themes:
The remaining themes that were mentioned were Fear (number of citations: 49; number of participants: 25), Perceived Need/Benefit (45; 22), Social Support (41; 22), Trust (30; 18), Loss of Contact (12; 7), Policy (10; 7), and Language (7; 5). Fear was mentioned as a facilitator 24 times (49%) and as a barrier 14 times (29%). There were also 11 instances (22%) where Fear was discussed neither as a facilitator nor barrier; usually in reaction to audio-visual demonstrations of what un-treated glaucoma may look like. Thirteen participants shared fear of losing their vision motivated them to seek eyecare, “You’re running scared now and you’re frightened […] So, you’re going to ask what can I do? Is this reversible? How can you help me?” Seven interviewees remarked how fear of finding out what may be wrong with them prevented them from seeking care, as illustrated in the quote, “The fear, you know. A lot of times you’re just afraid of what might be found.”
Both Perceived Need/Benefit and Social Support were identified more frequently as facilitators (35 times, 34 times, respectively) than as barriers (9 times, 5 times, respectively). For social support, 20 participants primarily talked about availability of help from family members, friends, and community resources as facilitators. As for Perceived Need/Benefit, 20 participants quoted the benefits of participating in the research project (free glasses) as well as presence of symptoms (blurry vision) as strong facilitators of seeking out care.
Trust was mentioned as a facilitator 15 times (50%), and as a barrier 15 times (50%). Thirteen participants mentioned how prior good experiences with their community clinic encouraged them to take part in the research project, saying, “Hope [Clinic] has a history of giving quality service, and maintaining standards, and it’s not about the money.” The program’s association with the University of Michigan was also quoted as a facilitator, for instance, “[y]ou’re connected with a very identifiable hospital.” Seven participants questioned the intention of the program and whether participation is truly free. This is reflected in comments such as, “Take a day off work […] and then to find out why you don’t qualify, it’s not really going to be free for you,” and “[p]eople are suspicious [about] what is it really for and what does it mean, and will it really help, do I really need [it]?”
Policy, Loss of Contact and Language were all mentioned almost exclusively as barriers to screening. Barriers posed by policy mainly referred to complicated insurance and hospital rules. Loss of Contact was brought up by staff members with regard to how high no-show rates and patients’ frequent contact information changes made coordination of care difficult. Language was mentioned as an important barrier by Hope Clinic staff members as approximately 50% of their patients do not speak English. As we were unable to interview patients who did not speak English, we could not include the perspective of non-English speaking patients on their perception of how language functions as a barrier to obtaining medical care.
Description of experience with the coaching program:
Before taking part in the eHealth glaucoma coaching intervention, interviewees’ knowledge of glaucoma ranged from “I don’t know much” to “I just know that it can affect your vision” to “…some kind of pressure built up in your eye.” Staff members or individuals who knew somebody with glaucoma tended to have a better understanding of the disease. After going through the eHealth coaching program, all individuals shared that they had a better and a more confident understanding of the pathophysiology and prognosis of glaucoma. The most representative quote after the coaching program was, “glaucoma is a buildup of pressure in your eye and that affects your optic nerve and can damage your optic nerve to the point where you can go blind.”
When asked about their experience with the coaching program, all participants gave at least one positive comment. The comments specifically praised three aspects of the program: 1) The approachability of the interviewer; 2) The simple language, and 3) The salient visual aids. Our participants shared that the simple language and good visual aids were key to helping them understand the diagnosis of glaucoma. One of our participants who self-identified English as her second language specifically mentioned the program’s easy to understand language as its key strength. The most powerful visual aids that participants commented on were depictions of what blind spots look like, sharing their opinions including, “I think the visual aids are really eye-opening and laid out what glaucoma really is about,” and “the actual seeing what you’re missing is the thing that really got me.”
At the end of the eHealth glaucoma coaching intervention every patient was able to identify in their own words that they should follow-up and attend their appointment with an ophthalmologist if they ever were to be diagnosed as suspicious for glaucoma as they would have during the role-play. Each patient was then asked to say, on a scale of 1 to 10, what the likelihood was that they would make it to this follow-up appointment with 1 being not at all confident and 10 being the most confident. The average value given was an 8.83 (8.55 for Hamilton participants, 9.04 for Hope participants).
Program Suggestions:
Participants made suggestions ranging from cosmetic concerns to changing educational content to adding entirely new elements to the coaching program. Cosmetic concerns were infrequently mentioned and usually secondary to personal preferences regarding the visual aids or the color of the font used. There were two main suggestions made with regard to the program content. First, many participants expressed confusion about a diagram explaining what a visual field was. Second, many participants expressed an interest in learning more about the genetic nature of glaucoma and hoped the program would tell them more about how likely their family members may have glaucoma.
Participants gave suggestions on how to reach out to the community to advertise the eye screening program. These suggestions recommended putting flyers and posters up at clinics, bus stops, and different community centers around the city. The community centers mentioned included churches, libraries, barber shops, and foodbanks. Other recommendations suggested using social media, television, and radio advertisements to reach a large number of people.
Discussion:
The goal of this study was to use the lens of CER to understand key stakeholder opinions on how to best implement a glaucoma screening program within two local community clinics. Through interviews of patients, providers, and staff members we were able to identify common barriers and facilitators to participating in a glaucoma screening program. The most frequently mentioned facilitators to glaucoma screening were Priorities, Knowledge, Perceived Need/Benefit, Social Support, and Cost (Figure 1). Similarly, the top five barriers were Priorities, Transportation, Convenience/Access, Knowledge, and Cost (Figure 2). Priorities was both the most commonly encountered facilitator and barrier for our participants. There were no differences in the themes discussed between patients and staff, although there were some thematic differences between the participants in the two different clinics.
Many of the barriers – such as Cost, Transportation, Knowledge and Trust - identified in this study are broadly applicable barriers frequently encountered in many aspects of delivering health care to people who live in poverty or come from minority backgrounds. Cost is one of the largest barriers to correcting refractive error with eyeglasses, in part due to lack of universal vision coverage in the United States.25, 26 In a landmark randomized controlled trial conducted by the RAND corporation, health care utilization between those randomized to plans with no cost-sharing (“free care”) and those randomized to plans with high out-of-pocket payment for each medical service was analyzed. Participants with out-of-pocket payments were significantly less likely to seek out appropriate vision examinations than those on the free care plan, especially if they had limited financial resources.27 In contrast, providing patients with free28 or low-cost generic glaucoma medications may significantly improve follow-up and medication adherence rates.29
The issue of transportation has been frequently documented as a salient barrier to obtaining eye care. Nearly one-quarter (24%) of counties in the United States do not have either an optometrist or an ophthalmologist, resulting in individuals having to travel long distances to obtain eye care.26, 30 Transportation as a barrier has specifically been cited among patients of the Hope Clinic who no-showed to their free eye appointment.31 In a systematic review of multiple chronic illnesses, it has been shown that providing patients with bus passes, taxi vouchers, or free shuttle services improve linkage to follow-up care.32 Trust has been cited as a barrier to seeking out care in both ophthalmologic and non-ophthalmologic settings,25, 33, 34 and has been shown to impact both willingness to seek care and medication adherence.35, 36 This is specifically important in minority populations, who have been shown to report lower trust in physicians and the health care system,37 likely due to longstanding violations of trust throughout history.38 However, in this study Trust acted as a facilitator almost as frequently as it acted as a barrier, usually in the context of prior good experiences at the community clinic. It has been shown that prior good experiences within the health-care system can increase trust.39 This further supports the implementation of glaucoma screening for high risk populations within community clinics that already have an existing positive relationship with their patients.
Fear as a theme arose almost twice as frequently as a facilitator than as a barrier. As a facilitator, it was mentioned usually in the context of the simulation that was shown during the coaching program that demonstrates how vision is lost over time – without people necessarily noticing - when glaucoma is not treated. A driving scene is shown, and as time progresses, different parts of the image go missing until ten years have passed, at which point the entire scene becomes blurry. Immediately after this simulation, the counselor tells the patient that this vision loss is preventable with use of and adherence to eye drops and continued follow-up care with an eye care provider. It has been shown that fear-based messaging is more effective when it is accompanied by an efficacy message that assures participants that they are capable of performing actions to avoid the fear-based negative consequences.40, 41 This invokes self-referential thinking, a concept from the Elaboration Likelihood Model of Persuasion.42 This model indicates that when individuals are truly cognitively engaged, they will apply what they have learned to their own situation. Self-referential thinking has been shown to lead to more sustained behavior changes,43 which may explain why fear was cited as a facilitator more frequently than a barrier in this analysis.
The themes of Priorities and Knowledge were the most frequently mentioned facilitators in our study. These themes are also broadly applicable to other screening programs and have been studied extensively within the context of Self-Determination Theory (SDT). SDT states that in order for individuals to implement behavior change, they require intrinsic motivation to do so and motivation is influenced by three factors: 1) Autonomy, in which someone believes they are in charge of their destiny, 2) Competence, in which they have the information in order to deal effectively with their environment, and 3) Relatedness, in which they acquire close relationships to their health care providers. The theme of “Priorities” is analogous to Motivation within SDT, and “Knowledge” is analogous to Competence. It is important to note that Priorities was a more important facilitator in our study than knowledge. SDT posits that while knowledge and feeling competent to carry out a behavior can plant the seeds of change, they cannot successfully modify behavior without intrinsic motivation. This is consistent with prior work studying glaucoma medication adherence, in which educational materials alone, even if personalized, did not improve adherence,44–46 but programs that targeted both knowledge and motivation were successful.47 In order to increase motivation to participate in follow-up eye care, our eHealth coaching program uses a Motivational Interviewing (MI)-based coaching technique,48 which allows the technician to create a relationship with the patient, explore resistance to change, and build autonomous motivation.49 MI is consistent with the framework of SDT, engaging patients by discussing priorities and obstacles to facilitate intrinsic motivation—personally compelling reasons—to change health behavior.50 After going through the coaching program, participants rated their likelihood of going to their recommended follow-up appointment as 8.83 on a scale of 1 to 10 (8.55 for Hamilton participants, 9.04 for Hope participants).
Community based screenings often suffer from poor follow-up rates. For instance, the follow-up rate for a definitive eye exam in a community-based glaucoma screening program in Baltimore, Maryland was only 41%.13 However, Hark et al has demonstrated that through reminder phone calls, individual counselling, reminders, and education, the follow-up rate can improve as much as up to 70%.12 Similarly, Johnson et al51 and Zyl et al52 have shown that providing glaucoma patients with educational workshops and definite follow up appointment respectively were effective in improving rates of follow-up care. We have found that the follow-up rate for comprehensive ophthalmic examinations among Hope Clinic patients is high in this context at around 76.6%.31 We attribute the high follow-up rates as well as the high intention to attend to the positive and trusting relationship these clinics have built with their clients. We also hypothesize that the personalized education and coaching we’ve provided may have contributed to our participant’s high desire to attend follow up appointments. The SIGHT Program has an embedded randomized controlled trial that will assess whether personalized education and coaching improves adherence to follow-up recommendations, so that data will be available in the future.
While some of the barriers and facilitators that we identified in our analysis may apply widely to other researchers or public health experts who are developing eye health screening programs for deployment in high-risk communities, there were some barriers and facilitators that were unique to our two communities. For example, language was exclusively an important barrier for patients at Hope Clinic. This is likely due to the fact that about 50% of patients at Hope Clinic do not speak English as a first language, compared to the 0.13% at Hamilton.16 Similarly, cost was also was mentioned more frequently among Hope clinic participants than Hamilton clinic participants. This is likely due to the difference in insurance coverage of patients between the two clinics: 82.3% of Hamilton patients are insured46 while only 24% of Hope patients are.14 CER allows researchers to more thoughtfully tailor the program to the particular community they are trying to engage. This will contribute to the adoption, implementation, and maintenance of this program in the community clinics.53 The differences between these two community clinics that are only 63 miles apart suggest that each community clinic has their own unique set of challenges and strengths that should be properly assessed to successfully identify the needs of each community. The hope is that using a community-engaged approach will translate into longer term adoption and maintenance of the successful aspects of the eye health screening program within each clinic.
Results from these interviews were used to influence changes to promotional materials, the eHealth glaucoma coaching program, and the overall screening program. The issue of cost came up frequently as both a facilitator and barrier, as well as within the context of trust. Patients were unsure if they could believe a glaucoma screening program would actually be free. In response to this, promotional materials were changed to have a greater emphasis on the program being completely free to participants. Changes to the eHealth glaucoma coaching program included removing descriptions of visual field testing, which were frequently commented on as “confusing” and “intimidating.” Also during the coaching session, many participants asked questions that had not been directly addressed. In response, we have added educational components to the coaching program including whether glaucoma is reversible or curable, the demographics of those most commonly diagnosed, and whether there is a genetic component. Structural changes to the glaucoma screening program were also made in response to comments. Many participants cited the proximity of screening being at their community clinic as a very important facilitator in terms of both Convenience/Access and Transportation. This reflects the findings of our prior study, in which patients had a difficult time going to ophthalmology clinics that were far from their homes.31 In addition, many patients expressed that their complicated schedules necessitate very specific appointment times, including during lunch breaks and at the end of the day. We have addressed this by ensuring that the ophthalmic technician will be at the clinic during business hours every day that the medical clinic is open.
One significant limitation to the study was that we were not able to interview non-English speaking participants, and so we were not able to gain their perspective on the best ways to implement eye disease screening in their community. Furthermore, we used a purposive sampling method to recruit patients who we thought were generally representative of the clientele in each clinic and did not collect their demographic data, precluding a mixed-methods analysis of these demographic factors. The strengths of this qualitative analysis include the inclusion of patients, providers, and staff from the two community clinics as key stakeholders. Using a CER lens allowed us to refine an eye disease screening program to best meet the needs of these two communities. The benefit of these methods is best described by one of the patients interviewed: “Well, I have to say that because you’ve taken the time to talk to me, I feel like I’m more part of the program and I’m not just, you know, outside or doing what I’m told to do and not understanding what your real job is.”.
Supplementary Material
Acknowledgements:
The authors acknowledge Phalatha McHaney-Conner for interviewing participants, and the input from Chamisa MacKenzie, MSW, MPH who helped create the eHealth coaching session.
Financial support: Centers for Disease Control and Prevention (U01 DP006442-01). The funding organizations had no role in the design or conduct of this research.
Footnotes
Supplemental Digital Content
Supplemental Digital Content 1. pdf
Supplemental Digital Content 2. Pdf
Supplemental Digital Content 3.
References:
- 1.Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040: A Systematic Review and Meta-Analysis. Ophthalmology. 2014/11/01/ 2014;121(11):2081–2090. [DOI] [PubMed] [Google Scholar]
- 2.Shaikh Y, Yu F, Coleman AL. Burden of Undetected and Untreated Glaucoma in the United States. American Journal of Ophthalmology. 2014/12/01/ 2014;158(6):1121–1129.e1. [DOI] [PubMed] [Google Scholar]
- 3.Tielsch JM, Sommer A, Katz J, Quigley H, Ezrine S. Socioeconomic status and visual impairment among urban Americans. Baltimore Eye Survey Research Group. Arch Ophthalmol. May 1991;109(5):637–41. [DOI] [PubMed] [Google Scholar]
- 4.Newman-Casey PA, Talwar N, Nan B, Musch DC, Stein JD. The relationship between components of metabolic syndrome and open-angle glaucoma. Ophthalmology. July 2011;118(7):1318–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moyer VA, Force aUSPST. Screening for Glaucoma: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine. 2013;159(7):484–489. [DOI] [PubMed] [Google Scholar]
- 6.Gupta P, Zhao D, Guallar E, Ko F, Boland MV, Friedman DS. Prevalence of Glaucoma in the United States: The 2005–2008 National Health and Nutrition Examination Survey. Investigative ophthalmology & visual science. 2016;57(6):2905–2913–2905–2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim S, Stewart JF, Emond MJ, Reynolds AC, Leen MM, Mills RP. The effect of a brief education program on glaucoma patients. Journal of glaucoma. 1997;6(3):146–151. [PubMed] [Google Scholar]
- 8.Hark LA, Myers JS, Pasquale LR, et al. Philadelphia Telemedicine Glaucoma Detection and Follow-up Study: Intraocular Pressure Measurements Found in a Population at High Risk for Glaucoma. J Glaucoma. April 2019;28(4):294–301. [DOI] [PubMed] [Google Scholar]
- 9.Killeen OJ, MacKenzie C, Heisler M, Resnicow K, Lee PP, Newman-Casey PA. User-centered Design of the eyeGuide: A Tailored Glaucoma Behavior Change Program. J Glaucoma. October 2016;25(10):815–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Newman-Casey PA, Niziol LM, Mackenzie CK, et al. Personalized behavior change program for glaucoma patients with poor adherence: a pilot interventional cohort study with a pre-post design. Pilot Feasibility Stud. 2018;4:128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. Evid Rep Technol Assess (Summ). August 2004;(99):1–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Hark L, Waisbourd M, Myers JS, et al. Improving Access to Eye Care among Persons at High-Risk of Glaucoma in Philadelphia--Design and Methodology: The Philadelphia Glaucoma Detection and Treatment Project. Ophthalmic Epidemiol. 2016;23(2):122–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quigley HA, Park CK, Tracey PA, Pollack IP. Community screening for eye disease by laypersons: the Hoffberger program. Am J Ophthalmol. March 2002;133(3):386–92. [DOI] [PubMed] [Google Scholar]
- 14.Guo W, Woodward MA, Heisler M, et al. Risk Factors for Visual Impairment in an Uninsured Population and the Impact of the Affordable Care Act. Clinics in surgery. 2016;1:1236. [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau QuickFacts: Ypsilanti city, Michigan. Accessed March 22, 2020. //www.census.gov/quickfacts/ypsilanticitymichigan
- 16.2018 Hamilton Community Health Network, Inc. Health Center Program Awardee Data - Hamilton Community Health Network, Inc. Flint, Michigan. Accessed February 29, 2020. https://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=053300&state=MI&year=2018#
- 17.MDHHS. Michigan Medicaid State Plan. Accessed September 14, 2020. http://www.mdch.state.mi.us/dch-medicaid/manuals/MichiganStatePlan/MichiganStatePlan.pdf
- 18.CDC. The Social-Ecological Model: A Framework for Prevention |Violence Prevention|Injury Center|CDC. Updated 2020-01-28T04:53:20Z. Accessed February 18, 2020. https://www.cdc.gov/violenceprevention/publichealthissue/social-ecologicalmodel.html
- 19.Gallo J, Lee S. Mixed Methods in Behavioral Intervention Research. Behavioral Intervention Research: Designing, Evaluating, and Implementing. Springer Publishing Company; 2015. [Google Scholar]
- 20.Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45(3):201–5. [DOI] [PubMed] [Google Scholar]
- 21.The SAGE Handbook of Current Developments in Grounded Theory. 2019. Accessed 2020/02/16. https://methods.sagepub.com/book/the-sage-handbook-of-grounded-theory-2e
- 22.Foley G, Timonen V. Using Grounded Theory Method to Capture and Analyze Health Care Experiences. Health Serv Res. August 2015;50(4):1195–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.D W, D G Mixed Methods Research. Oxford University Press; 2015. [Google Scholar]
- 24.Miles MB, Huberman AM. Qualitative data analysis : an expanded sourcebook. 1994. [Google Scholar]
- 25.Elam AR, Lee PP. Barriers to and Suggestions on Improving Utilization of Eye Care in High-Risk Individuals: Focus Group Results. International scholarly research notices. 2014;2014:527831–527831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Academies of Sciences E, Medicine. Making Eye Health a Population Health Imperative: Vision for Tomorrow. The National Academies Press; 2016:586. [PubMed] [Google Scholar]
- 27.Lohr KN, Brook RH, Kamberg CJ, et al. Use of medical care in the Rand Health Insurance Experiment. Diagnosis- and service-specific analyses in a randomized controlled trial. Med Care. September 1986;24(9 Suppl):S1–87. [PubMed] [Google Scholar]
- 28.Yang K, Jin L, Li L, et al. Interventions to Promote Follow-up After Trabeculectomy Surgery in Rural Southern China: A Randomized Clinical Trial. JAMA Ophthalmology. 2016;134(10):1135–1141. [DOI] [PubMed] [Google Scholar]
- 29.Stein JD, Shekhawat N, Talwar N, Balkrishnan R. Impact of the introduction of generic latanoprost on glaucoma medication adherence. Ophthalmology. 2015;122(4):738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson DM. The geographic distribution of eye care providers in the United States: Implications for a national strategy to improve vision health. Prev Med. April 2015;73:30–6. [DOI] [PubMed] [Google Scholar]
- 31.Woodward MA, Jeganathan VSE, Guo W, Cederna J, Newman-Casey PA. Barriers to Attending Eye Appointments among Underserved Adults. J Ophthalmic Vis Res. Oct-Dec 2017;12(4):449–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Starbird LE, DiMaina C, Sun CA, Han HR. A Systematic Review of Interventions to Minimize Transportation Barriers Among People with Chronic Diseases. J Community Health. April 2019;44(2):400–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blackstock OJ, Addison DN, Brennan JS, Alao OA. Trust in primary care providers and antiretroviral adherence in an urban HIV clinic. J Health Care Poor Underserved. February 2012;23(1):88–98. [DOI] [PubMed] [Google Scholar]
- 34.Newman-Casey PA, Robin AL, Blachley T, et al. The Most Common Barriers to Glaucoma Medication Adherence: A Cross-Sectional Survey. Ophthalmology. July 2015;122(7):1308–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–39, v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Safran DG, Taira DA, Rogers WH, Kosinski M, Ware JE, Tarlov AR. Linking primary care performance to outcomes of care. J Fam Pract. September 1998;47(3):213–20. [PubMed] [Google Scholar]
- 37.Hausmann LRM, Kwoh CK, Hannon MJ, Ibrahim SA. Perceived Racial Discrimination in Health Care and Race Differences in Physician Trust. Race and Social Problems. 2013/06/01 2013;5(2):113–120. [Google Scholar]
- 38.Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. Summer 2007;14(2):56–60. [PubMed] [Google Scholar]
- 39.Halbert CH, Armstrong K, Gandy OH, Jr., Shaker L. Racial differences in trust in health care providers. Arch Intern Med. April 24 2006;166(8):896–901. doi: 10.1001/archinte.166.8.896 [DOI] [PubMed] [Google Scholar]
- 40.Tannenbaum MB, Hepler J, Zimmerman RS, et al. Appealing to fear: A meta-analysis of fear appeal effectiveness and theories. Psychol Bull. November 2015;141(6):1178–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. October 2000;27(5):591–615. [DOI] [PubMed] [Google Scholar]
- 42.Petty RE, Cacioppo JT. The Elaboration Likelihood Model of Persuasion. Elsevier Science & Technology; 1986:123–205. [Google Scholar]
- 43.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. June 2008;23(3):454–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beckers HJ, Webers CA, Busch MJ, Brink HM, Colen TP, Schouten JS. Adherence improvement in Dutch glaucoma patients: a randomized controlled trial. Acta Ophthalmol. November 2013;91(7):610–8. [DOI] [PubMed] [Google Scholar]
- 45.Lim MC, Watnik MR, Imson KR, Porter SM, Granier AM. Adherence to glaucoma medication: the effect of interventions and association with personality type. J Glaucoma. August 2013;22(6):439–46. [DOI] [PubMed] [Google Scholar]
- 46.Lunnela J, Kääriäinen M, Kyngäs H. Web-based intervention for improving adherence of people with glaucoma. Journal of Nursing and Healthcare of Chronic Illness. 2011/06/01 2011;3(2):119–129. [Google Scholar]
- 47.Dreer LE, Owsley C, Campbell L, Gao L, Wood A, Girkin CA. Feasibility, Patient Acceptability, and Preliminary Efficacy of a Culturally Informed, Health Promotion Program to Improve Glaucoma Medication Adherence Among African Americans: “Glaucoma Management Optimism for African Americans Living with Glaucoma” (GOAL). Curr Eye Res. 2016;41(1):50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Markland D, Ryan R, Tobin V, Rollnick S. Motivational interviewing and self–determination theory. Journal of social and clinical psychology. 2005;24(6):811–831. [Google Scholar]
- 49.Ng JY, Ntoumanis N, Thogersen-Ntoumani C, et al. Self-Determination Theory Applied to Health Contexts: A Meta-Analysis. Perspect Psychol Sci. July 2012;7(4):325–40. [DOI] [PubMed] [Google Scholar]
- 50.Miller WR, Rollnick S. Meeting in the middle: motivational interviewing and self-determination theory. Int J Behav Nutr Phys Act. March 2 2012;9:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson DM, Stratford S, Shyu AP, et al. The impact of educational workshops on individuals at risk for glaucoma in the Philadelphia Glaucoma Detection and Treatment Project. Patient Education and Counseling. 2016/04/01/ 2016;99(4):659–664. [DOI] [PubMed] [Google Scholar]
- 52.van Zyl T, Su Z, Zhou E, et al. Providing Prescheduled Appointments as a Strategy for Improving Follow-Up Compliance After Community-Based Glaucoma Screening: Results from an Urban Underserved Population. Journal of Community Health. February 2015 2015-02-11 2015;40(1):27–33. [DOI] [PubMed] [Google Scholar]
- 53.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. August 7 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


