Abstract
The role of pharmacists in the treatment of HIV has expanded beyond medication dispensing to include a host of cost-effective, evidence-based strategies across the HIV continuum of care. However, wide-scale adoption of pharmacy-based HIV prevention and treatment interventions has been slow. We conducted a systematic review to evaluate the evidence on the role of pharmacists across the HIV continuum of care. Thirty-two studies were identified, most of which provided evidence of feasibility of HIV testing and efficacy of non-prescription syringe sale services in pharmacies. However, only two studies implemented an experimental design to rigorously test pharmacy-based strategies. Notably, no pharmacy-based strategies have specifically targeted the highest HIV risk populations such as black and Latinx men who have sex with men, women, or trans populations. Efficacy trials and effectiveness studies should rigorously test existing pharmacy-based strategies to build greater support for wide-scale adoption and implementation. Moreover, in order to integrate pharmacies into the strategy to end the HIV epidemic, studies are needed to ensure that pharmacy-based HIV prevention and treatment services can reach the highest risk populations.
Background
Ending the HIV epidemic initiative is a landmark goal of the United States Department of Health and Human Services requiring collaborative efforts across multiple government organizations to prevent new HIV infections1–3. In order to effectively reduce HIV over the next ten years, a multi-pronged approach that tackles behavioral and biomedical prevention approaches for populations who are HIV negative, as well as behavioral and biomedical treatment approaches for populations living with HIV is critical. In order to make sweeping progress along the continuums of HIV prevention and care, a drastic shift in our efforts is needed to expand access to HIV prevention and treatment resources.
Recent publications4,5 and non-systematic reviews6,7 have noted the central role that pharmacists can play in ending the HIV epidemic. Indeed, pharmacy-based interventions have been implemented across the HIV prevention and care continuums for a number of compelling reasons. There is a natural draw to engaging pharmacies given their physical accessibility in terms of location and store hours8. Pharmacies are often perceived as neutral, non-stigmatizing environments9–14; and pharmacies have the ability to reach a range of populations15–18. Despite these strengths, HIV prevention and care in pharmacies has not been fully integrated into pharmacy services on a national level as have other primary prevention (i.e., vaccinations) and treatment services19.
There is a growing menu of cost-effective, evidenced-based strategies that could be integrated into pharmacy services to include HIV prevention and treatment adherence. While expanding HIV prevention and treatment services in pharmacies nationally could further push the needle and make a larger impact on the HIV continuum of care, it is unclear if there is compelling scientific evidence to justify wide-spread adoption of these services into all pharmacies necessitating additional pharmacy staff training and integration of accompanied systems. Herein, the purpose of this systematic literature review is to synthesize the recent literature on the role of pharmacists across the HIV continuum of care to understand whether sufficient evidence exists to make an argument for scaling up this work and making a large impact on ending the HIV epidemic. Additionally, we identify research gaps and make recommendations for future research priorities to integrate pharmacies into the HIV prevention and care continuums.
Methods
Article selection
We conducted a search in the Web of Science and Pubmed to identify studies published between January 2004 and August 2019 that described studies and interventions in a non-hospital-based pharmacy setting designed to reduce HIV transmission, either through prevention or treatment. This review followed the PRISMA guidelines for systematic reviews, which include pre-defining the rationale and objectives for the study, inclusion criteria, databases used for searches, study selection, and data collection20. We limited the search to published articles and peer-reviewed articles in the United States. Unpublished articles and those published in the grey literature were not included. The final search terms which were developed in collaboration with a resource librarian included were a combination of the following terms: “pharmacy,” “structural intervention,” “HIV,” “HIV treatment,” “HIV prevention,” “pharmacists,” and “United States”.
Eligibility criteria
Studies were included in the review if they were: 1) conducted in the United States, 2) were in a (non-hospital based) pharmacy setting, 3) were related to the HIV continuum of care (from prevention to treatment) and 4) published in the last 16 years. Exclusion criteria included studies that were 1) systematic or non-systematic reviews or 2) theoretical models.
Data collection and Analysis
All articles were cross-referenced to remove duplicates. Titles and abstracts of the articles were screened for inclusion in the final analytic sample. Keyword identification was performed so that articles with abstracts that included the words pharmacies and/or HIV were included in the sample for full article review. In cases where the abstract seemed to fit the inclusion criteria but it was unclear whether it included HIV prevention or treatment resources specifically, we reviewed the abstract of the article in its entirety to determine whether the study would be included in the final analytic sample. Full text review of the articles was performed and double coded by two independent raters (NC and SM). Data extraction from the articles included study design, population, and the primary study outcomes. We performed an applied thematic analysis to determine the main themes assessed in the final analytic sample.
Results
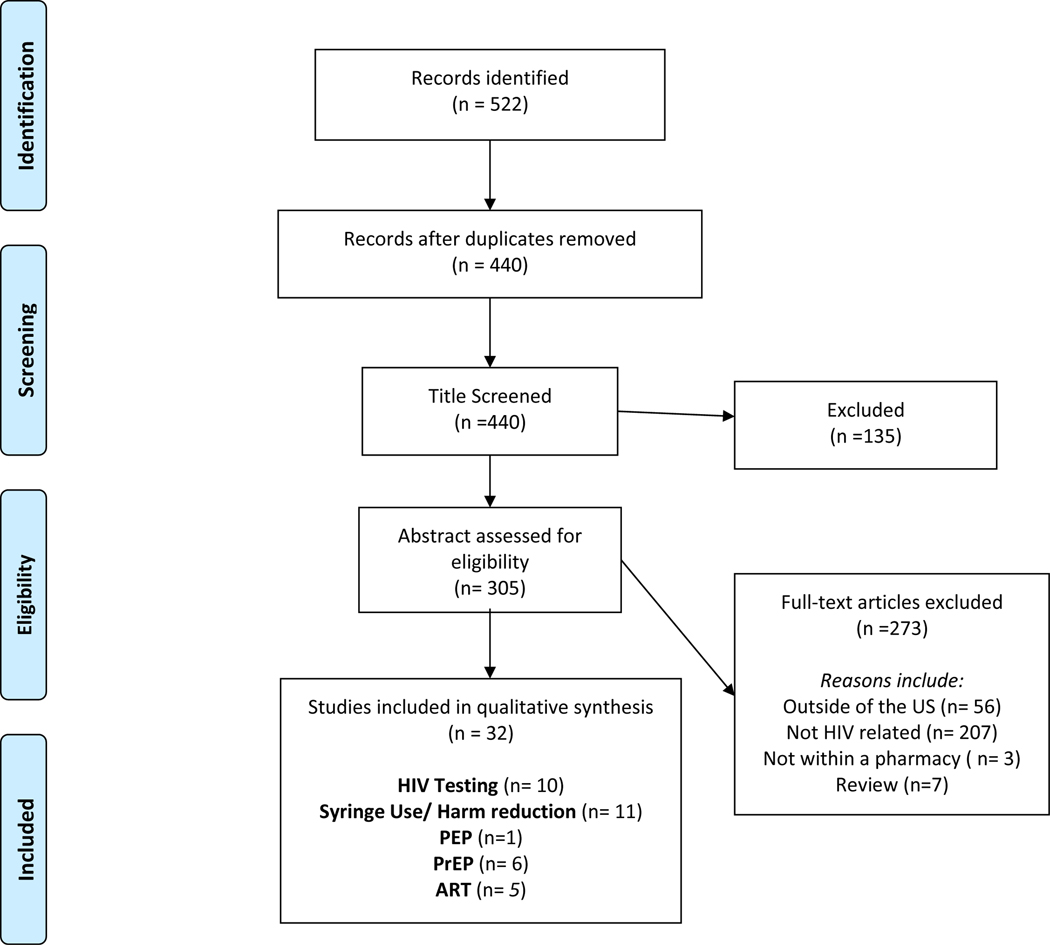
Our search yielded a total of 522 articles. After duplicates were removed, we performed a title and abstract review to ensure the articles were relevant to the aims of the study. We identified 32 studies for inclusion in the final sample for complete review (Figure 1).
Figure 1.
PRISMA Flow Diagram of Systematic Review Search Process
As shown in Table 1, of the 32 eligible studies, 19 were cross-sectional, 4 were qualitative, 2 were spatial, 1 was a retrospective cohort, 3 were prospective cohorts, 1 was a non-randomized intervention and 2 were randomized control trials (RCTs). Study participants’ included individuals from the general population, HIV positive patients, MSM, people who inject drugs (PWID), pharmacists and pharmacy technicians. We organized the manuscripts thematically around five key areas of the HIV continuum of care: HIV testing12–14,21–26, safe syringe access and harm reduction15,18,27–35, post exposure prophylaxis (PEP)36, pre-exposure prophylaxis (PrEP)37–42, and antiretrovirals (ART)43–46. Herein, we synthesize the findings within each of these areas.
Table 1.
Description of literature on pharmacy-based HIV prevention interventions (n=27)
| First Author, year | Study Design | Study Population | Main Findings |
|---|---|---|---|
| HIV testing | |||
| Amesty, 2012 | Cross-sectional | Pharmacists and technicians; majority Latino cis female | High support for in-pharmacy HIV testing among pharmacy staff and pharmacists. |
| Collins, 2018 | Cross-sectional | General population; majority Black cis male | Chain pharmacy HIV testing program tested 3630 people, 46% of whom had never been tested. |
| Crawford, 2011 | Cross-sectional | Pharmacists and technicians; mostly Latino female | Pharmacy staff that supported in-pharmacy vaccination were more likely to support in-pharmacy HIV testing. |
| Crawford, 2016 | Cross-sectional | PWID; majority Latino and Black cis male | Pairing HIV testing with other screening tests such as blood pressure, diabetes, etc. resulted in more HIV tests taken. |
| Darin, 2015 | Cross-sectional | General population; majority White and Black cis female | Interest in pharmacy-based HIV screening was reported by almost 36% of the sample and was higher for younger, black and Other racial groups. Lower perceived risk of HIV, cost and time were reported as barriers to HIV screening. |
| Darin, 2015 | Cross-sectional | General population; majority White and Black cis female | Pharmacy based HIV testing was acceptable and feasible. Pharmacy based HIV testing captured 42% of never testers who also engaged in high risk behaviors. |
| Lecher, 2015 | Cross-sectional | Pharmacists; race and gender not reported | Providing POC HIV rapid testing services required a modest amount of staff time and costs that are comparable to other services offered in these settings. HIV testing in pharmacies and retail clinics can provide an additional alternative venue for increasing the availability and accessibility of HIV testing services in the United States. |
| Ryder, 2013 | Qualitative | Pharmacists; cis male and female, race not reported | Participants accepted the idea of pharmacy-based HIV testing, describing it as accessible, convenient, and non-stigmatizing. Acceptability was closely linked to positive patient relationships and pharmacist comfort with consultation. |
| Weidle, 2014 | Cross-sectional | Pharmacies; race and gender not reported | Project established HIV testing in several community pharmacies and retail clinics to be a feasible model for offering rapid, point-of-care HIV testing. It also demonstrated the willingness and ability of staff at community pharmacies and retail clinics to provide confidential HIV testing to patients. |
| Safe syringe access and harm reduction | |||
| Crawford, 2014 | RCT | Pharmacists and technicians; majority Latino and Other race females | Pharmacy staff trained to deliver harm reduction services to PWID have significant decreases in negative beliefs about PWID over time. |
| Davidson, 2015 | Spatial | General population; race and gender not reported | There is no statistically significant change in the relationship between overdoses locations and pharmacies after de-regulating syringe sales in pharmacies. |
| Lewis, 2015 | RCT | PWID; majority Latino and Black cis male | Provision of medical and social service referrals to PWID who purchase syringes in pharmacies can improve safe syringe practices. |
| Lutnick, 2012 | Qualitative | PWID; majority White female | PWID had strong reservations about expanding pharmacy syringe access due to privacy, ability to obtain services elsewhere and pharmacy staff attitudes. |
| Meyerson, 2018 | Cross-sectional | Pharmacists; majority White cis male and cis female | Pharmacists supportive beliefs about syringe sales predict willingness to sell syringes without a prescription. High opioid overdose mortality is inversely related to willingness to sell syringes. |
| Pollini, 2015 | Cross-sectional | Test buyers; majority cis female, race not reported | Despite recently passed legislation syringe access in pharmacies in California was poor. Only 1/5 of attempts to purchase syringes in pharmacies were successful. |
| Pollini, 2017 | Cross-sectional | Pharmacists and technicians; majority female, race not reported | Almost 1/3 of pharmacy staff would sell syringes to someone they suspected injected drugs. Knowledge about legal syringe sales and required syringe sale practices was low and negative beliefs about PWID were high. |
| Rudolph, 2010 | Cross-sectional | PWID; majority Latino and Black | PWID who patron pharmacies that are trained to provide social and medical referrals to PWID have more positive experiences |
| Siddiqui, 2015 | Cross-sectional | PWID; White and non-White male | PWID in a city with legal non-prescription syringe sales in pharmacies were more likely to obtain syringes in a pharmacy compared to PWID in a city without legal non-prescription syringe sales in a pharmacy. |
| Stopka, 2012 | Spatial | PWID; majority White and Black male | Black Americans had significantly lower access to purchasing a syringe from a pharmacy. Methamphetamine users had higher access to syringes in pharmacies. Geographical access to syringes in pharmacies was poor in two neighborhoods with high proportions of PWID. |
| Zaller, 2010 | Cross-sectional | Pharmacists; majority White Latino cis male | Online survey of 146 pharmacy staff revealed that staff though pharmacies were important for PWID and 59% were wiling to provide health information and referrals. There was concern about a private space and safety when providing HIV prevention services to PWID. |
| Post exposure prophylaxis | |||
| Fuller, 2013 | Qualitative | Pharmacists and clinicians; majority White male | Pharmacists and clinicians support the use of an interactive web application to assist with post exposure prophylaxis access and patient management. |
| PrEP | |||
| Broekhuis, 2018 | Cross-sectional | Pharmacists; majority White cis female | Pharmacists familiarity with PrEP and CDC guidelines for PrEP use was low. But over half were willing to provide PrEP through a collaborative physician relationship. Willingness to provide PrEP was related to previous experience with HIV. |
| Havens, 2019 | Prospective | MSM; majority White | High (100%) satisfaction for pharmacy PrEP. None of the participants seroconverted. Pharmacists felt comfortable and had almost no disruptions to workflow. |
| Hoth, 2019 | Cross-sectional | MSM; majority White cis male | Pharmacy-based PrEP telemedicine feasibility study showed high PrEP uptake (91%), retention (61%) and completion of laboratory tests (96%). |
| Shaeer, 2014 | Cross-sectional | Pharmacists; White cis male and cis female | Most (75%) pharmacists recently completed continuing education related to HIV, but only 22% had dispensed PrEP. Knowledge about PrEP, CDC PrEP guidelines and having the ability to counsel patients about PrEP was low. |
| Smith, 2016 | Cross-sectional | Pharmacists; majority White cis male | Pharmacists can financially support PrEP services for patients through medication management therapy or a collaborative practice agreement. |
| Tung, 2018 | Prospective | MSM; majority cis male, race not reported | Same-day pharmacy-based PrEP has high uptake, follow-up and is cost-effective to prevent HIV infections. |
| Antiretrovirals | |||
| Cocohoba, 2012 | Retrospective cohort study | Patients with HIV and 30 days of ART prescription claims; majority cis male, race not reported | Patients who attended HIV focused pharmacies were significantly more likely to refill their ART. |
| Cocohoba, 2012 | Cross-sectional | HIV positive and negative women; majority Black | Only 30% of women received counseling from a pharmacist. No differences in counseling prevalence was present by HIV status. Pharmacy counseling did not significantly impact ART adherence or CD4 counts among HIV positive women. |
| Dilworth, 2018 | Non-randomized intervention | HIV positive patients with ART adherence problems; majority Latino and White | Intensive pharmacist counseling at 1–2 weeks, 6 weeks, 3- and 6- months cost-effectively increased adherence, viral load and decreased approximately 0.13 secondary HIV infections. |
| Kibicho, 2011 | Qualitative | Pharmacists; majority White cis male and cis female | Pharmacists implemented a combination of patient-specific interventions to reduce ART adherence barriers including medication education, follow-up calls and patient referrals. But, internal and external pharmacy challenges were present. |
| Murphy, 2012 | Prospective | HIV positive patients; male, race not reported | HIV specialized community pharmacies show higher patient adherence persistence on ART. |
HIV Testing
Nine studies in our sample directly examined the provision of HIV testing in pharmacies. These studies highlighted that pharmacy-based HIV testing is feasible and reaches those at the highest risk of HIV transmission (e.g., never testers, racial minorities and those who report high HIV stigma). Specifically, in a cross-sectional analysis, Darin et al showed that interest in HIV testing in community pharmacies was highest among non-Hispanic Blacks and Hispanics13. Similarly, Crawford et al and Amesty et al showed that customers who injected drugs and had high HIV testing stigma12, as well as racial minority customers and customers who reported more sex partners11 were more willing to receive HIV testing in the pharmacy. Notably, willingness and acceptability of pharmacy-based HIV testing has not been tested specifically among MSM, particularly MSM of color. However, the ability to reach the populations with the highest need are complemented by strong willingness of pharmacy staff to perform HIV testing. In a qualitative study, Ryder et al noted that pharmacists believed pharmacy-based HIV testing was accessible, convenient and non-stigmatizing24. Moreover, Weidle et al showed that pharmacy-based HIV testing was feasible within a 30-minute period that included pre-test counselling, test processing time and post-test counselling in 21 pharmacies in both rural and urban areas25. In terms of cost, pharmacy-based HIV testing was also low. The time to distribute and costs of test kits, control kits, shipping, test supplies, training, reporting, program administration, and advertising, was about ~47.21 per patient tested14. However, pharmacy staff training should be considered since pharmacists who were more likely to report a high comfort level with HIV consultation were more willing to participate in HIV testing in pharmacies. Notably, less than half of the studies (n=4) briefly described that pharmacy clients who tested positive for HIV were referred to confirmatory HIV treatment services with a medical provider or health department. Only one study described a model where pharmacy clients were personally connected to confirmatory testing. Therefore, systematic assessment of these referrals is needed to ensure that individuals who have a positive HIV screen are linked to HIV care and this does not result in another break in the HIV care continuum.
Safe syringe access and harm reduction
A number of studies examined the role of pharmacies in disease prevention for people who inject drugs (PWID). Four studies examined pharmacists’ attitudes towards selling non-prescription syringes for PWID and while many pharmacists believed pharmacies are an important resource for PWID, only 59% were willing to provide health information and referrals34. In another study, only about 33% would sell syringes to individuals they suspected injected drugs despite legislation allowing non-prescription syringe sales35. Moreover, test buys by secret shoppers (e.g., individuals posing as a PWID to determine whether they could successfully purchase a syringe from a pharmacy) revealed that only about 20% of syringe purchase attempts were successful in California30, which is one of many states where pharmacies can legally sell syringes without a prescription. Misconceptions about syringe access being related to increased substance use and disease transmission have long been barriers to increasing syringe access despite a consistent lack of evidence between pharmacy syringe sales and mortality27. However, for some pharmacists, these ideas prevail. For example, in Indiana where over half of pharmacists interviewed sold syringes without a prescription to PWID, pharmacies located in communities with high opioid overdose were less willing to sell syringes to PWID29. Ethical and moral values influence some pharmacists’ decisions to deter PWID from attempting to purchase syringes from their pharmacy27. But, these behaviors may have broader effects on PWID willingness and comfort with utilizing any pharmacies as syringe sources. These findings indicate the need for additional training on substance use, addiction and the benefit of syringe access in reducing opioid related morbidity and overdose. Our review only yielded one experimental study, which sought to train pharmacy staff to increase knowledge about PWID17,18. The PHARM-Link study showed that negative beliefs about the PWID significantly declined over time among pharmacies randomly assigned to a treatment group which included trainings to engage and provide social and medical service referrals to PWID who purchased non-prescription syringes17,18. Promisingly, this structural intervention also led to positive outcomes for PWID who patronized pharmacies that received harm reduction training15. Specifically, PWID showed increases in safe syringe practices including reduced syringe sharing and improper syringe disposal15.
Post-exposure Prophylaxis (PEP)
Our review only yielded one study on PEP, which qualitatively showed that clinicians and pharmacists support the use of a web-application to track and monitor PWID that are prescribed PEP in New York City36. To our knowledge, no studies have been published to highlight the integration of PEP into pharmacy practice. New York is the only state to our knowledge with a pharmacy-based PEP program that has been implemented4, but utilization of this program is unknown. California also recently passed legislation to allow limited non-prescription sales of PEP and PrEP in pharmacies beginning in 202047. However, data are limited to inform the integration of these services into pharmacy practice. Data are also needed to show effectiveness of PEP reach for PWID and other at-risk populations.
Pre-Exposure Prophylaxis (PrEP)
Although early studies revealed poor pharmacist knowledge about PrEP, recently published studies are beginning to show great promise for PrEP screening and same-day dispensing in pharmacies. For example, in 2014 Shaeer et al showed that despite most Florida pharmacists’ receipt of recent continuing education training on HIV, only 22% had ever dispensed PrEP40. Moreover, most pharmacists were unaware of the CDC’s eligibility guidelines (63%), were uncomfortable prescribing PrEP (47%), and believed it was too expensive (92%) and led to increases in sexually transmitted infections (65%). Just four years later, two studies have shown the strong possibility of cost-effectively providing PrEP in a pharmacy setting through collaborative practice agreements38,42. These studies have integrated PrEP into the pharmacy by creating a pharmacist led model where pharmacy staff administer PrEP screenings and dispense PrEP. Another study highlighted the possibility of a pharmacy-based PrEP telemedicine model39. Across all of these studies, PrEP uptake over time was high at baseline (>90%), but declined by about half over a six-month period. None of the participants were acutely HIV-infected when beginning PrEP and none sero-converted across any of the studies over a one-year period. Moreover, pharmacists were able to easily integrate PrEP into their existing workflow. Most of the participants reached in these studies identified as white MSM and these studies were located in relatively low HIV transmission areas. So, it is unclear if pharmacist collaborative practice agreements (CPAs) with physicians can be easily established in high transmission areas to reach populations at the highest risk of HIV such as black MSM. A study by Smith et al noted that most pharmacists reported being able to support PrEP services for their patients through reimbursable medication therapy management services (66%), while only 43% currently provide services under a CPA41. So, alternative reimbursement strategies should be examined for cost-effectiveness.
Antiretrovirals therapy (ARTs)
Only a few studies have utilized pharmacies to promote ART adherence among people living with HIV. Data show that patients living with HIV who obtain ART from HIV specialized pharmacies are more likely to obtain their refills39. Moreover, when pharmacists provide more HIV counseling to patients living with HIV, adherence increases, and viral load as well as the number of secondary infections in the community decreases43,44. However, these findings were not consistent for women48. Since pharmacy staff routinely obtain additional continuing education, increasing HIV specialized training opportunities may help integrate these services into pharmacies and have wide impact for populations living with and without HIV.
Discussion
This systematic review showed that substantial research has been performed across the HIV continuum of care and has reached several HIV risk populations including PWID and white MSM, but more research is still needed to rigorously test the interventions especially across other risk populations. Importantly, a range of studies have shown that pharmacies can cost-effectively provide HIV testing, and have the potential to reach several high HIV risk populations that have not been recently been tested, but this warrants additional investigation. HIV testing is not only well-received among pharmacy customers, but pharmacists and technicians feel this is in their purview and are willing to provide this primary prevention service. Pharmacies can currently provide clinical laboratory improvement amendment (CLIA)-waived HIV tests within their existing practice or establish CPAs with physicians to integrate services. A major barrier to massive integration of HIV testing will rest on pharmacy staff HIV counseling capabilities, and their ability to effectively link customers who test positive for HIV. From a pharmacy perspective, this support could result in additional customer visits and revenue if the patient is successfully initiated into HIV treatment (for patients with HIV) or PrEP (for patients without HIV). There is also a gap in understanding whether a referral system could integrate into existing pharmacy workflow and whether patients are effectively linked with physicians – two areas that should be further explored.
The literature reviewed here show that pharmacies have made the most progress with respect to HIV prevention services for PWID. With legislative support, pharmacies have disseminated clean syringes to reduce syringe sharing practices among PWID and the only RCT conducted in a pharmacy setting showed that pharmacy referrals to social and medical services can significantly reduce HIV risk behaviors. This finding is critically important for understanding the potential reach of pharmacy counseling, suggesting that if pharmacies are structurally equipped with basic HIV prevention resources (e.g., syringes, HIV tests, condoms), and pharmacy staff are trained with cultural competence on the appropriate community organizations to send patients, reductions in risk behavior can occur. However, the literature also reveal important gaps in education among pharmacy staff that are needed to reduce stigma among PWID and other risk populations.
This review revealed notable gaps in the methodologies implemented, and areas of research along the HIV continuum of care. First, as mentioned previously, only one study (which produced two published manuscripts to date) included in our review has used an experimental design to test pharmacy-based HIV prevention strategies. Preliminary findings of cross-sectional pharmacy-based PrEP and ART interventions that utilize pharmacist counseling to improve adherence are promising. These strategies need to be tested rigorously using experimental or cross-over designs to determine the true effect of these strategies. Future studies could also test the effectiveness of pharmacist-led counseling using mobile applications. Moreover, implementation science frameworks are needed to evaluate the integration and scalability of these services into existing pharmacy workflows.
Of particular significance, no pharmacy-based HIV prevention or treatment studies in our review have specifically targeted populations at the highest risk of sexual HIV transmission. Only three studies have assessed MSM at all and these studies do not inform how BMSM will accept pharmacy-based HIV prevention and care services. BMSM have the fastest growing rate of HIV when compared to any other racial or risk behavior group and account for over 60% of incident HIV infections among MSM. Little is also known about Latinx MSM, women and trans populations who are disproportionately affect by HIV49, have greater barriers to HIV prevention50 and care51. As the HIV epidemic has shifted substantially from intravenous transmission to sexual transmission in the US52, pharmacy-based studies need to examine whether pharmacies are a comfortable source of HIV prevention and care services for populations other than PWID such as Black and Latinx MSM, women and trans populations. Feasibility studies should assess whether pharmacies can reach these populations using strategies such as direct targeting of patients who obtain prescriptions for STIs. For women specifically, existing interventions can reach high-risk women who obtain emergency contraception in pharmacies.
Utilizing standard systematic review protocols and drawing on the expertise of a resource librarian, this review examined the range of pharmacy-based studies across the HIV continuum of care. We explored two online databases for published manuscripts, which may have omitted relevant articles from other databases as well as unpublished articles. We are also limited by publication bias of findings that only show significant effects, in either a positive or negative direction, which may influence the final analytic sample of articles we reviewed. While statistical significance is generally considered the benchmark for publication, we cannot exclude the possibility that papers published with positive significance or in favor of the intervention are not over represented in the literature. We did not use a standard rating scale on the rigor of each article since many of these scales give lower credence to qualitative methodologies, which we feel is a strong contribution to the literature. We do, however, note that in order to expand HIV prevention and treatment resources, experimental designs that test the best approaches are needed. Studies utilizing these methodological designs may be limited since it requires strong partnership with the private sector and it would also be important to assess financial outcomes. Some studies in our review systematically assessed cost-effectiveness of HIV prevention and treatment services in pharmacies. Future studies and resources that are dedicated to improving the role of pharmacists in HIV prevention and treatment should consider cost-effectiveness as an important component of the studies’ viability.
This systematic review highlights data showing that pharmacists can fill a critical gap, particularly with respect to HIV testing, and harm reduction services for PWID. In order to effectively end the HIV epidemic the translation of pharmacy services to populations most affected with the poorest access to resources is critical. There is an urgent need to further explore rigorous strategies that integrate PrEP into pharmacy practice, improve ART adherence, and reach populations at high risk for HIV transmission.
Acknowledgements
The authors would like to acknowledge the National Institutes on Mental Health for its support (R34 MH119007–01).
References
- 1.Buchbinder SP, Liu AY. CROI 2019: advances in HIV prevention and plans to end the epidemic. Top Antivir Med. 2019;27(1):8–25. [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Department of Health & Human Services. Ending the HIV Epidemic: A plan for America. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Published 2019. Accessed August 1, 2019, 2019.
- 3.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV Epidemic: A Plan for the United States. JAMA. 2019;321(9):844–845. [DOI] [PubMed] [Google Scholar]
- 4.Myers JE, Farhat D, Guzman A, Arya V. Pharmacists in HIV Prevention: An Untapped Potential. Am J Public Health. 2019;109(6):859–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCray E. Pharmacists Can Play Key Role in Ending the HIV Epidemic. In: U.S. Department of Health & Human Services, ed. HIV.gov 2019. [Google Scholar]
- 6.Farmer EK, Koren DE, Cha A, Grossman K, Cates DW. The Pharmacist’s Expanding Role in HIV Pre-Exposure Prophylaxis. AIDS Patient Care STDS. 2019;33(5):207–213. [DOI] [PubMed] [Google Scholar]
- 7.Hill LA, Ballard C, Cachay ER. The Role of the Clinical Pharmacist in the Management of People Living with HIV in the Modern Antiretroviral Era. AIDS Rev. 2019;21(4):195–210. [DOI] [PubMed] [Google Scholar]
- 8.Gebhart F. Provider status: Keep the pressure on lawmakers and push for payment. Drug Topics. http://drugtopics.modernmedicine.com/drug-topics/news/provider-status?page=0,4. Published 2016. Accessed. [Google Scholar]
- 9.Rosenbluth SA, Madhavan SS, Borker RD, Maine LL. Pharmacy immunization partnerships: a rural model. J Am Pharm Assoc (Wash). 2001;41(1):100–107. [DOI] [PubMed] [Google Scholar]
- 10.Joyce A, Berbatis CG, Sunderland VB, Dhaliwal SS. Analysis of primary prevention services for cardiovascular disease in Australia’s community pharmacies. Aust N Z J Public Health. 2007;31(6):516–519. [DOI] [PubMed] [Google Scholar]
- 11.Amesty S, Crawford ND, Nandi V, et al. Evaluation of Pharmacy-Based HIV Testing in a High-Risk New York City Community. AIDS Patient Care STDS. 2015;29(8):437–444. [DOI] [PubMed] [Google Scholar]
- 12.Crawford ND, Dean T, Rivera AV, et al. Pharmacy Intervention to Improve HIV Testing Uptake Using a Comprehensive Health Screening Approach. Public Health Rep. 2016;131 Suppl 1:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Darin KM, Klepser ME, Klepser DE, et al. Pharmacist-provided rapid HIV testing in two community pharmacies. J Am Pharm Assoc (2003). 2015;55(1):81–88. [DOI] [PubMed] [Google Scholar]
- 14.Lecher SL, Shrestha RK, Botts LW, et al. Cost analysis of a novel HIV testing strategy in community pharmacies and retail clinics. J Am Pharm Assoc (2003). 2015;55(5):488–492. [DOI] [PubMed] [Google Scholar]
- 15.Lewis CF, Rivera AV, Crawford ND, DeCuir J, Amesty S. Pharmacy-randomized intervention delivering HIV prevention services during the syringe sale to people who inject drugs in New York City. Drug Alcohol Depend. 2015;153:72–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fuller CM, Galea S, Caceres W, Blaney S, Sisco S, Vlahov D. Multilevel community-based intervention to increase access to sterile syringes among injection drug users through pharmacy sales in New York City. Am J Public Health. 2007;97(1):117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crawford ND, Amesty S, Rivera AV, Harripersaud K, Turner A, Fuller CM. Randomized, community-based pharmacy intervention to expand services beyond sale of sterile syringes to injection drug users in pharmacies in New York City. Am J Public Health. 2013;103(9):1579–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crawford ND, Amesty S, Rivera AV, Harripersaud K, Turner A, Fuller CM. Community Impact of Pharmacy-Randomized Intervention to Improve Access to Syringes and Services for Injection Drug Users. Health Educ Behav. 2014;41(4):397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poudel A, Lau ETL, Deldot M, Campbell C, Waite NM, Nissen LM. Pharmacist role in vaccination: Evidence and challenges. Vaccine. 2019;37(40):5939–5945. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- 21.Amesty S, Blaney S, Crawford ND, Rivera AV, Fuller C. Pharmacy staff characteristics associated with support for pharmacy-based HIV testing. J Am Pharm Assoc (2003). 2012;52(4):472–479, 471–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins B, Bronson H, Elamin F, Yerkes L, Martin E. The “No Wrong Door” Approach to HIV Testing: Results From a Statewide Retail Pharmacy-Based HIV Testing Program in Virginia, 2014–2016. Public Health Rep. 2018;133(2_suppl):34S–42S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darin KM, Scarsi KK, Klepser DG, et al. Consumer interest in community pharmacy HIV screening services. J Am Pharm Assoc (2003). 2015;55(1):67–72. [DOI] [PubMed] [Google Scholar]
- 24.Ryder PT, Meyerson BE, Coy KC, von Hippel CD. Pharmacists’ perspectives on HIV testing in community pharmacies. J Am Pharm Assoc (2003). 2013;53(6):595–600. [DOI] [PubMed] [Google Scholar]
- 25.Weidle PJ, Lecher S, Botts LW, et al. HIV testing in community pharmacies and retail clinics: a model to expand access to screening for HIV infection. J Am Pharm Assoc (2003). 2014;54(5):486–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crawford ND, Blaney S, Amesty S, et al. Individual- and neighborhood-level characteristics associated with support of in-pharmacy vaccination among ESAP-registered pharmacies: pharmacists’ role in reducing racial/ethnic disparities in influenza vaccinations in New York City. J Urban Health. 2011;88(1):176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davidson PJ, Martinez A, Lutnick A, Kral AH, Bluthenthal RN. Drug-related deaths and the sales of needles through pharmacies. Drug Alcohol Depend. 2015;147:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lutnick A, Case P, Kral AH. Injection drug users’ perspectives on placing HIV prevention and other clinical services in pharmacy settings. J Urban Health. 2012;89(2):354–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meyerson BE, Davis A, Agley JD, et al. Predicting pharmacy syringe sales to people who inject drugs: Policy, practice and perceptions. Int J Drug Policy. 2018;56:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pollini RA, Rudolph AE, Case P. Nonprescription syringe sales: a missed opportunity for HIV prevention in California. J Am Pharm Assoc (2003). 2015;55(1):31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rudolph AE, Standish K, Amesty S, et al. A community-based approach to linking injection drug users with needed services through pharmacies: an evaluation of a pilot intervention in New York City. AIDS Educ Prev. 2010;22(3):238–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siddiqui SS, Armenta RF, Evans JL, et al. Effect of legal status of pharmacy syringe sales on syringe purchases by persons who inject drugs in San Francisco and San Diego, CA. Int J Drug Policy. 2015;26(11):1150–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stopka TJ, Lutnick A, Wenger LD, Deriemer K, Geraghty EM, Kral AH. Demographic, risk, and spatial factors associated with over-the-counter syringe purchase among injection drug users. Am J Epidemiol. 2012;176(1):14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zaller N, Jeronimo A, Bratberg J, Case P, Rich JD. Pharmacist and pharmacy staff experiences with non-prescription (NP) sale of syringes and attitudes toward providing HIV prevention services for injection drug users (IDUs) in Providence, RI. J Urban Health. 2010;87(6):942–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pollini RA. Self-reported participation in voluntary nonprescription syringe sales in California’s Central Valley. J Am Pharm Assoc (2003). 2017;57(6):677–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fuller CM, Turner AK, Hernandez D, et al. Attitudes toward Web application supporting pharmacist-clinician comanagement of postexposure prophylaxis patients. J Am Pharm Assoc (2003). 2013;53(6):632–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broekhuis JM, Scarsi KK, Sayles HR, et al. Midwest pharmacists’ familiarity, experience, and willingness to provide pre-exposure prophylaxis (PrEP) for HIV. PLoS One. 2018;13(11):e0207372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Havens JP, Scarsi KK, Sayles H, Klepser DG, Swindells S, Bares SH. Acceptability and feasibility of a pharmacist-led HIV pre-exposure prophylaxis (PrEP) program in the Midwestern United States. Open Forum Infect Dis. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoth AB, Shafer C, Dillon DB, Mayer R, Walton G, Ohl ME. Iowa TelePrEP: A Public-Health-Partnered Telehealth Model for HIV Pre-Exposure Prophylaxis (PrEP) Delivery in a Rural State. Sex Transm Dis. 2019. [DOI] [PubMed] [Google Scholar]
- 40.Shaeer KM, Sherman EM, Shafiq S, Hardigan P. Exploratory survey of Florida pharmacists’ experience, knowledge, and perception of HIV pre-exposure prophylaxis. J Am Pharm Assoc (2003). 2014;54(6):610–617. [DOI] [PubMed] [Google Scholar]
- 41.Smith DK, Mendoza MC, Stryker JE, Rose CE. PrEP Awareness and Attitudes in a National Survey of Primary Care Clinicians in the United States, 2009–2015. PLoS One. 2016;11(6):e0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tung EL, Thomas A, Eichner A, Shalit P. Implementation of a community pharmacy-based pre-exposure prophylaxis service: a novel model for pre-exposure prophylaxis care. Sex Health. 2018;15(6):556–561. [DOI] [PubMed] [Google Scholar]
- 43.Cocohoba JM, Murphy P, Pietrandoni G, Guglielmo BJ. Improved antiretroviral refill adherence in HIV-focused community pharmacies. J Am Pharm Assoc (2003). 2012;52(5):e67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dilworth TJ, Klein PW, Mercier RC, Borrego ME, Jakeman B, Pinkerton SD. Clinical and Economic Effects of a Pharmacist-Administered Antiretroviral Therapy Adherence Clinic for Patients Living with HIV. J Manag Care Spec Pharm. 2018;24(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kibicho J, Owczarzak J. Pharmacists’ strategies for promoting medication adherence among patients with HIV. J Am Pharm Assoc (2003). 2011;51(6):746–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murphy P, Cocohoba J, Tang A, Pietrandoni G, Hou J, Guglielmo BJ. Impact of HIV-specialized pharmacies on adherence and persistence with antiretroviral therapy. AIDS Patient Care STDS. 2012;26(9):526–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zraick K GS. California makes HIV prevention drugs available without a prescription. The New York Times 2019. [Google Scholar]
- 48.Cocohoba JM, Althoff KN, Cohen M, et al. Pharmacist counseling in a cohort of women with HIV and women at risk for HIV. Patient Prefer Adherence. 2012;6:457–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bradley ELP, Williams AM, Green S, et al. Disparities in Incidence of Human Immunodeficiency Virus Infection Among Black and White Women - United States, 2010–2016. MMWR Morb Mortal Wkly Rep. 2019;68(18):416–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elopre L, Kudroff K, Westfall AO, Overton ET, Mugavero MJ. Brief Report: The Right People, Right Places, and Right Practices: Disparities in PrEP Access Among African American Men, Women, and MSM in the Deep South. J Acquir Immune Defic Syndr. 2017;74(1):56–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Geter A, Sutton MY, Armon C, et al. Trends of racial and ethnic disparities in virologic suppression among women in the HIV Outpatient Study, USA, 2010–2015. PLoS One. 2018;13(1):e0189973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beyrer C, Abdool Karim Q. The changing epidemiology of HIV in 2013. Curr Opin HIV AIDS. 2013;8(4):306–310. [DOI] [PubMed] [Google Scholar]