Abstract
We developed and pilot-tested an eight-session community-based cognitive behavior therapy group intervention to improve coping with intersectional stigma, address medical mistrust, and improve antiretroviral treatment adherence. Seventy-six HIV-positive Latinx sexual minority men (SMM; 38 intervention, 38 wait-list control) completed surveys at baseline, and four- and seven-months post-baseline. Adherence was electronically monitored. Intention-to-treat, repeated-measures regressions showed improved adherence in the intervention vs. control group from baseline to follow-up [electronically monitored: b (95% CI) = 9.24 (−0.55, 19.03), p = 0.06; self-reported: b (95% CI) = 4.50 (0.70, 8.30), p = .02]. Intervention participants showed marginally decreased negative religious coping beliefs in response to stigma [b (95% CI) = −0.18 (−0.37, 0.01), p = .06], and significantly lower medical mistrust [b (95% CI) = −0.47 (−0.84, −0.09), p = .02]. Our intervention holds promise for improving HIV outcomes by empowering Latinx SMM to leverage innate resilience resources when faced with stigma. (TRN: NCT03432819, 01/31/2018)
Keywords: coping, HIV, Latinx, sexual minority men, stigma/discrimination
Resumen
Hemos desarrollado un estudio piloto para poner a prueba un programa de ocho-sesiones de terapia cognitivo-conductual basado en un grupo de comunidad para abordar el estigma interseccional, la desconfianza médica y mejorar la adherencia al tratamiento antirretroviral. Setenta y seis hombres Latinos de minorías sexuales VIH positivos (38 en el grupo de intervención, 38 en el grupo de control de lista de espera) completaron encuestas al inicio, y cuatro y siete meses después de la línea de base. La adherencia fue medida electrónicamente. Los resultados del análisis mostraron una mejor adherencia en el grupo de intervención en comparación al grupo de control desde el inicio hasta el seguimiento [monitoreado electrónicamente: b (95% IC) = 9.24 (−0.55, 19.03), p = .06; y autoreporte: b (95% IC) = 4.50 (0.70, 8.30), p = .02]. Los participantes del grupo de intervención mostraron una disminución marginal en las creencias negativas de afrontamiento religioso al estigma [b (95% IC) = −0.18 (−0.37, 0.01), p = .06], y significativamente menor desconfianza médica [b (95% IC) = −0.47 (−0.84, −0.09), p = .02]. Nuestra intervención es prometedora para mejorar los resultados del VIH al empoderar a hombres Latinos de minorías sexuales para tomar ventaja de los recursos de resiliencia innatos cuando se enfrentan al estigma.
INTRODUCTION
HIV-related inequities disproportionately affect Latinx individuals, especially those who are immigrants and sexual minority men (SMM) [1–3]. In comparison to Non-Hispanic Whites, Latinx individuals tend to have greater delays in HIV diagnosis [4, 5], as well as less HIV medical care utilization and antiretroviral therapy (ART) use [6, 7], and are less likely to be virally suppressed [8].
Stigma due to HIV and related intersectionalities (e.g., minority race/ethnicity and sexual identity) is thought to be a barrier to effective HIV prevention and treatment [9–15], beyond effects of healthcare access and socioeconomic status [16]. Biopsychosocial models posit that stigma can contribute to inequities by increasing detrimental physiological stress responses [17–20], resulting in “weathering,” a cumulative negative impact on health (and immune function) that leads to premature mortality [21, 22]. Stigma-related stressors have a unique and potentially stronger association with poor health than non-stigma-related stressors [23, 24].
Ineffective coping with the stress of discrimination may lead to inequities through behavioral pathways, such as healthcare avoidance and ART non-adherence among people with HIV. Specifically, individuals who anticipate discrimination in healthcare settings may not engage with healthcare due to heightened medical mistrust, which can be conceptualized as an adaptive, functional coping response [25]. Mistrust can help individuals to maintain a sense of meaning, control, and empowerment in the face of an external threat, such as a discrimination experience [26–29], by attributing HIV inequities to structural discrimination and an unjust social system [30, 31]. Although avoidant coping may minimize one’s exposure to discrimination, one consequence may be that Latinx individuals are less engaged with healthcare due to anticipated discrimination—including potential mistreatment and deportation among immigrants [3].
Cognitive behavior therapy (CBT) interventions can improve adherence to HIV treatment, diabetes self-care, and medication [32–36]. Moreover, CBT interventions are effective in improving coping with stress and, in turn, boosting mental health among people with HIV [37, 38]. However, research has not tested the application of CBT specifically to address coping with discrimination, a particularly harmful stressor among people with multiple intersecting stigmatized identities, or whether enhanced coping skills can lead to improved health behaviors. Two pilot studies suggested that CBT can improve coping with discrimination among HIV-positive Black and Latinx SMM [28, 39], but effects on health behaviors such as ART adherence were not tested.
We conducted a pilot randomized controlled trial of a group-based CBT intervention to enhance coping with intersectional stigma and discrimination, and improve ART adherence among HIV-positive Latinx SMM. The intervention addressed adherence through psychoeducation and examples about the importance of adherence, and used CBT strategies to identify and examine the consequences of ineffective coping with discrimination for health and health behaviors, including adherence. The intervention also addressed the consequences of perceived discrimination for medical mistrust, such as the link between perceptions of mistreatment by healthcare providers and resultant distrust of healthcare providers’ and public health recommendations—including for medication-taking and the effectiveness of treatment. We hypothesized that intervention participants would show improved effective coping, reduced medical mistrust, and increased ART adherence compared to control participants.
METHODS
Study Design and Procedures
The study design was a pilot individually randomized group-treatment trial, in which intervention participants were clustered into groups [40]. Following principles of community-based participatory research (CBPR) [41, 42], the study was co-designed and conducted in the context of an established community-academic partnership that included leadership and key stakeholders of a community partner organization that offers culturally congruent HIV social services to a primarily Latinx client base in Los Angeles County, CA. The community-academic team met one-to-two times per year with the organization’s Community Advisory Coalition, composed of clients who guided the team in designing project materials, making suggestions for recruitment, and interpreting study results. All study activities were conducted on-site at the community partner organization, by staff employed by the organization and trained by the academic partners, which helped to build community capacity for research. A prior publication contains a full description of the CBPR intervention development and research process [28].
Participants completed study data collection visits at baseline, and two-, four-, five-, and seven-months post-baseline. At baseline, participants completed a survey and received a Medication Event Monitoring System (MEMS) bottle cap (AARDEX, Inc.) to monitor their adherence electronically throughout the study. Participants were randomized to the intervention or wait-list control group during the second study visit, when baseline adherence data were downloaded (to serve as the pre-intervention measure of adherence). Blocked one-to-one randomization was used to ensure balance across arms. At four-months and seven-months post-baseline, participants completed follow-up surveys. At all post-baseline study visits, research assistants downloaded participants’ electronic adherence data and updated participants’ contact information, if needed.
Approximately two months were needed to recruit and interview all intervention and control group members for the baseline assessment prior to each administration of the intervention, which lasted for about two months. Thus, the four-month follow-up occurred immediately after the last intervention session. Three intervention-control cohorts were recruited, and three sets of intervention sessions were conducted. Wait-list control group participants were offered the intervention sessions after all data collection was completed for the pilot trial.
Participants received $40 in gift cards for the baseline, four-, and seven-month assessments; $20 for the second post-baseline visit, in which staff downloaded electronic adherence data and randomized participants; and $10 each for the two- and five-month check-in visits, in which staff downloaded electronic adherence data. Participants who completed all three survey visits received a $20 bonus. For each intervention session attended, intervention participants were given a $10 gift card to cover transportation costs; participants who attended at least six of the seven sessions were given a $20 bonus. Refreshments were provided at each intervention session. All procedures were approved by the institutional review boards of the RAND Corporation and Los Angeles County Department of Public Health.
Intervention Description
Descriptions of the intervention development and content process is available in a prior publication [28]. Community stakeholders named the intervention Siempre Seguiré, translated as “I will always continue,” based on a popular Spanish-language song by the artist Thalia (“A Quien Le Importa”-in English, “Who Cares”) that is seen as a message of empowerment in Latinx gay communities, conveying that the strength of being true to oneself will help one to persevere through challenging times.
The eight-session Spanish-language intervention had seven sessions of content plus a “graduation” ceremony. The intervention included psychoeducation about discrimination, HIV disparities, and HIV treatment adherence, including defining discrimination to enable participants to be more aware in recognizing identity-based mistreatment. The facilitators acknowledged historical and current structural discrimination as reasons for disparities, and discussed how discrimination can lead to medical mistrust, as well as mental health issues, substance use, and poverty, which disproportionally affect communities of color.
The facilitators used CBT and dialectical behavior therapy (DBT) techniques to address coping with discrimination based on intersectional identities [43–47]. Specifically, participants were taught how to do a functional, chain analysis of a discrimination event, in terms of understanding the precursors to the event, including vulnerability factors (e.g., not getting enough sleep) and resilience factors (e.g., social support), as well as their proximal and distal thoughts, behaviors, and emotions in response to the event, and the immediate and longer-term consequences of their responses [48]. Participants learned how to identify problematic ‘links’ in the chain, i.e., factors (e.g., immediate emotional responses) that increased the risk of ineffective coping with discrimination that might lead to non-adherence or lack of care engagement [43, 48]. Participants practiced skills in session (e.g., with example vignettes) and in take-home activities in between sessions (e.g., tracking cognitions, emotions, and behaviors in response to discrimination) [49, 50].
For instance, to illustrate the CBT model, participants discussed a hypothetical scenario in which a man visits a clinic to get HIV treatment and the receptionist loudly asks if he is there to obtain HIV medications. The man is embarrassed and leaves the clinic, and he does not reschedule his appointment. Participants discussed how the critical link was feeling embarrassed, and the man coped with the embarrassment by disengaging from care; participants discussed more effective ways to cope, such as reporting the receptionist to the clinic manager and finding a new place to get care. Participants were then encouraged to discuss healthcare-related examples from their own lives.
Two separate sessions were devoted to specific forms of ineffective coping, internalized stigma and medical mistrust. Internalized stigma was discussed as a barrier to effective coping that could lead to non-adherence, such as when a person feels ashamed of being HIV-positive and, in turn, less willing to take ART—because the ART is perceived to be a daily reminder of being HIV-positive. The CBT model was used to illustrate to participants how to identify and respond to such internalized negative thoughts. Medical mistrust was discussed as an understandable consequence of discrimination. The CBT model was used to illustrate how medical mistrust can be an ineffective coping response, because it may lead to avoidance of healthcare and non-adherence. Men brainstormed ways to counteract medical mistrust.
The intervention was based in an intersectionality perspective, i.e., that the sum of the parts of an identity are greater than the identities’ individual components, and participants’ intersectional identities are a consequence of interlocking systems of power and oppression, which devalue racial/ethnic and sexual minority identities and lead to social inequality [51–53]. Thus, intervention participants were encouraged to process and discuss how stigma and discrimination affected the whole of their identity, rather than the separate components, related to race/ethnicity, gender, sexual identity, and HIV serostatus—along with whatever other identities were central to them. They completed an “Identity Pie” activity in Session 1, in which they drew a pie chart to show how multiple interlocking identities comprised their holistic, overall sense of self. Facilitators referred to the Identity Pie in later sessions, as men discussed discrimination experiences based on their overall identity, and also brainstormed ways to obtain social support for their whole self and all of their identities simultaneously, rather than for portions of their identity that they compartmentalized into different social groups (e.g., support for being a Latinx SMM, rather than support for being Latinx only, regardless of their sexual orientation).
Facilitators guided intervention participants in recognizing how discrimination experiences were affected by the context of their whole identity—for example, an experience with discrimination due to being Latinx might be qualitatively different if they were heterosexual or a woman. Discussions were guided by the experiences of men in the group; for example, rather than imposing ‘correct’ ways to cope with discrimination in a didactic manner, facilitators encouraged men to share and model different effective strategies. A major tenet of the intervention was acknowledgement that the men have considerable innate resilience resources to cope with discrimination that they can teach each other, and that they can generalize from some discrimination situations to others. Rather than teaching a prescribed list of skills, the facilitators used their clinical skills to identify the skills needed based on the behavioral analyses that the participants shared. Thus, the intervention honored and recognized the richness and complexity of men’s intersectional identities, to lead to insights about the consequences of discrimination for men’s health and well-being.
Intervention Facilitators and Fidelity
Intervention sessions were led by a trained peer facilitator with expertise in group therapy with Latinx SMM, and a trained peer co-facilitator; both were matched in identities with participants (Latinx SMM; both also were immigrants, as were the majority of participants). After each session, the facilitator and co-facilitator independently rated their fidelity to the protocol using standardized forms tailored to session content. Specifically, they rated the extent to which each content area was covered in each session (1, not at all covered; 2, somewhat covered; 3, completely covered). A Co-Investigator trained in clinical social work listened to each session recording and also provided fidelity ratings, as well as weekly supervision to the intervention facilitators on general therapy skills, group management, use of CBT, and any culturally relevant issues. The senior author provided the social worker with clinical supervision focused on balancing the clinical needs of the participants with the constraints of the protocol, as well as general clinical supervision topics.
Participants
Participants were recruited via flyers (within and outside of the organization, e.g., at local HIV-focused events, as well as posted online, e.g., on Facebook), through presentations to relevant client and provider groups within the organization, and by word-of-mouth from participants and the organization’s staff. Eligibility criteria included: (1) self-identify as Hispanic or Latino; (2) at least 18 years-old; (3) HIV-positive (verified with medication bottles at the first study visit); (4) biologically male; (5) ever had sex with another man; and (6) not currently taking ART or taking ART and reported missing at least 1 dose in the past month, or reported fewer than two HIV care visits in the past 12 months. Transgender individuals were excluded, because the intervention did not address discrimination based on gender identity, which would require differently tailored content.
As shown in the CONSORT diagram (Figure I), we screened 92 individuals for eligibility, of whom nine were deemed ineligible and one eligible participant declined; 82 completed the baseline assessment and 76 were randomized (38 intervention, 38 control). Reasons for not being randomized after completing the baseline assessment included: self-withdrawn due to being homeless and unable to commit to study visits (n = 1); and unable to re-contact despite multiple attempts (n = 5). Eleven participants (seven intervention, four control) were not retained in between randomization and follow-up 1 (four had substance abuse issues, one lived too far from the study area, two were too busy to commit, and four had unknown reasons because they were never reached despite multiple attempts). One control group participant was not retained in between the two follow-ups due to a conflicting work schedule. Thus, 65 participants were retained at four-month follow-up (86% of those randomized) and 64 at seven-month follow-up (84% of those randomized).
Figure I.
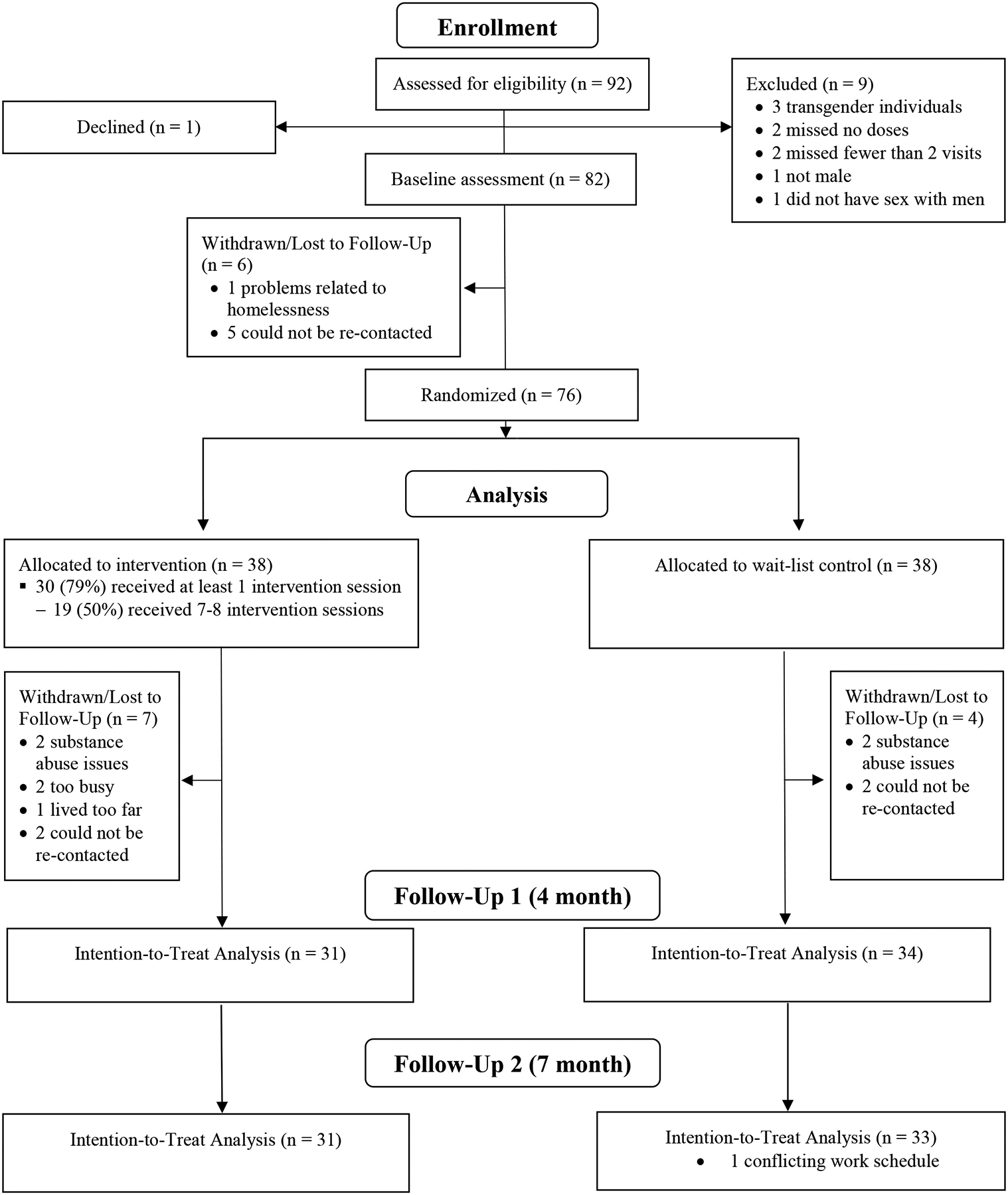
CONSORT Diagram of Participant Flow in the Siempre Seguiré Intervention Test
Of the 38 participants randomized to the intervention, two-thirds received over half of the sessions (at least four of the seven, not counting the graduation session), 61% received at least six sessions, and half received at least seven sessions. Eight participants who were randomized to the intervention attended no sessions. Among the 30 who attended at least one session, the mean number of sessions attended was 6.17 (SD = 2.32).
Reasons for missed sessions were generally unrelated to the intervention: ten participants reported a scheduling conflict; nine were sick or caring for a sick relative; six were traveling outside of the study area; two had transportation difficulties; one had relationship issues that prevented participation; and three did not provide a reason. Only two withdrew from the intervention due to reasons directly related to the intervention. One described feeling uncomfortable with the intervention content (about discrimination) and the other was concerned about confidentiality among group members.
Assessment
Socio-demographic and health characteristics.
Table I shows participants’ socio-demographic and medical characteristics. The survey assessed age (used as a continuous variable); total annual household income (dichotomized as less than or greater than or equal to $5,000); education level (dichotomized as less than a high school diploma vs. a high school diploma/equivalent or greater); employment status (dichotomized as working full-time or part-time vs. not working/unemployed); residency status (dichotomized as undocumented vs. not); length of time in U.S. (dichotomized as less than 20 years vs. 20 or more years); housing stability in past year [dichotomized as any unstable housing (i.e., not having a permanent place to live of one’s own; living in supportive or transitional housing, in a shelter, or in single room occupancy housing; being in a residential treatment program; or being homeless) vs. living in one’s own home/apartment], relationship status (married or in a committed relationship); and sexual orientation (gay, bisexual, heterosexual, or “other”). English acculturation (α = .91) and Spanish acculturation (α = .76) were assessed with the Bidimensional Acculturation Scale for Hispanics [54]. Participants were also asked the month and year of their HIV diagnosis (converted into years) and whether they had a detectable or undetectable HIV viral load.
Table I.
Baseline Descriptive Statistics Overall and by Intervention Group (n = 38 intervention, 38 wait-list control)
| Overall (n = 76) M (SD) or % | Intervention M (SD) or % | Control M (SD) or % | Intervention vs. Control p-value (baseline) | |
|---|---|---|---|---|
| Age | 52.9 (12.9) | 52.4 (12.9) | 53.5 (13.1) | .72 |
| Residency Status | .13a | |||
| U.S. citizen | 32.0 | 32.4 | 31.6 | |
| Permanent legal resident | 20.0 | 35.1 | 5.3 | |
| Temporary visa | 17.3 | 10.8 | 23.7 | |
| Undocumented | 30.7 | 21.6 | 39.5 | |
| Length of time in U.S. 20+ years | 64.5 | 71.1 | 57.9 | .34 |
| Education (<high school diploma) | 46.1 | 44.7 | 47.4 | 1.00 |
| Employment status: Working full-time or part-time | 21.1 | 21.1 | 21.1 | 1.00 |
| Any unstable housing, past year | 73.7 | 71.1 | 76.3 | .80 |
| Income < $5,000 annually | 27.0 | 19.4 | 34.2 | .19 |
| Married/committed relationship | 18.4 | 18.4 | 18.4 | 1.00 |
| Sexual orientation | 1.00 | |||
| Gay | 85.5 | 86.8 | 84.2 | |
| Bisexual | 11.8 | 10.5 | 13.2 | |
| Heterosexual | 1.3 | 2.6 | 0.0 | |
| Other | 1.3 | 0.0 | 2.6 | |
| Acculturation (Spanish) | 5.01 (0.47) | 5.02 (0.45) | 5.00 (0.48) | .84 |
| Acculturation (English) | 3.48 (0.84) | 3.57 (0.83) | 3.39 (0.86) | .35 |
| Length of time diagnosed with HIV (years) | 16.6 (9.5) | 15.5 (9.8) | 17.7 (9.2) | .32 |
| Undetectable viral load (self-report) | 86.7 | 89.5 | 83.8 | .52 |
Test of permanent legal resident vs. other categories
Primary outcome: ART adherence.
We assessed adherence electronically with MEMS, and via self-report. A MEMS cap with an electronic chip that recorded the date and time of each bottle opening was used to monitor daily ART adherence over the seven-month study period. Participants were provided with the cap about two months prior to their cohort’s intervention start-date [M (SD) = 56.8 (14.2) days prior], for a valid pre-intervention, baseline adherence measure that allowed for time to decrease reactance to the assessment. Research assistants assisted participants with dispensing the medication with the most complex dosing schedule, or the base medication of the regimen if all medications had the same schedule, into a bottle [55].
In each subsequent assessment visit, research assistants downloaded adherence data and participants completed a brief survey to assess instances in which the cap was not used as intended in the past two weeks (how often the bottle was opened without removing a dose, a dose was taken from a source other than the bottle, such as a pillbox, and whether multiple doses were removed at a time and pocketed for later ingestion). Data for the past two weeks at each time-point were adjusted using these responses, for a more valid assessment [56, 57].
The main outcome derived from MEMS data was continuous adherence, i.e., percentage of total scheduled doses taken. This measure was derived for each 1-month time-period that participants were in the study. Self-reported adherence was assessed by asking participants to estimate on a visual analogue scale the percentage of prescribed ART doses that they took last month, a measure validated against more objective indicators such as viral load and pill count [58, 59].
Secondary outcome: coping with discrimination.
The Brief COPE and R-COPE, which assess coping strategies when faced with stress [60, 61], were adapted to assess coping with discrimination, following prior research [39]. The instructions were revised to ask participants to indicate the extent to which they had responded in each way “when faced with discrimination,” with response categories 1 = I haven’t been doing this at all, 2 = I’ve been doing this a little bit, 3 = I’ve been doing this a medium amount, and 4 = I’ve been doing this a lot. We added three functional coping items to the Brief COPE, based on prior qualitative research on coping in communities of color (“I tell myself that other people are ignorant”; “I avoid certain situations or people so that I am not discriminated against in the future”; and “I change the way that I dress or talk so that I am not discriminated against in the future”) [28, 62].
The focus of the intervention was to increase functional, effective coping, and to decrease dysfunctional, ineffective coping, without prescribing the type of coping that participants should use. Thus, following prior research and guidance by the scale developers that the subscales depend on researchers’ needs [39, 60, 63, 64], we created two subscales from the Brief COPE: functional/effective coping (α = .82; 19 items, including 16 Brief COPE items on active coping, acceptance, social support, positive reframing, planning, humor, and religion, and the three items noted above) and dysfunctional/ineffective coping (α = .71; 12 items; denial, substance use, behavioral disengagement, venting, self-blame, and self-distraction). Two R-COPE subscales were created: positive religious coping (α = .90; assesses secure relationships with a divine force/spiritual connectedness) and negative religious coping (α = .70; assesses underlying spiritual tensions/internal struggles).
Secondary outcomes: medical mistrust and internalized stigma.
General medical mistrust was measured with the Mistrust of Healthcare Scale (α = .79) [65]. HIV-specific medical mistrust was measured with the HIV Conspiracy Beliefs Scale (α = .89) [66]. Response options were 1, Strongly Disagree to 5, Strongly Agree. Internalized HIV stigma was assessed with the Internalized AIDS-Related Stigma Scale (α = .82) [15]. Internalized sexual minority stigma was assessed with the Internalized-Homophobia Scale-Revised (α = .82) [67]. Response options were 1, Strongly Disagree to 5, Strongly Agree.
Post-Intervention Interviews
To assess intervention acceptability, the extent to which people receiving an intervention consider it to be well-matched to their genuine needs [68], intervention participants were asked to complete semi-structured qualitative interviews immediately after the 8-week intervention ended. Interviews were conducted by two trained bilingual Latina research assistants. The interview contained questions on attitudes about the program overall and specific attitudes regarding program content, structure, and facilitators. Interviews were transcribed in Spanish and translated from Spanish to English, after which the team conducted a qualitative content analysis, allowing for themes to emerge through a bottom-up, iterative coding process [69, 70]. Specifically, two study investigators and one research assistant independently read all responses to develop an initial list categorizing positive and negative feedback overall and for each aspect of the intervention, from which they developed a codebook. Two coders (a Latina study investigator with a PhD and a Latina research assistant with a BA) double-coded three transcripts, representing 63 coded passages (of 28 interviews conducted, or 11%) and established inter-rater reliability (κ = .73) [71, 72], after which the research assistant coded all of the transcripts using the qualitative data management software Dedoose (Version 7.0.23).
Statistical Analysis
We calculated descriptive statistics for all variables and tested differences between the intervention and control groups at baseline to examine comparability between groups on socio-demographic and health-related characteristics, using Fisher’s exact tests for categorical characteristics and t-tests for continuous characteristics (Table I). To test for intervention efficacy, a repeated-measures regression was conducted on each outcome using an intention-to-treat approach in which the response for survey outcomes may have come from either follow-up survey (and each participant could contribute up to two follow-up responses), and for electronically-monitored adherence may have been measured at five, six, or seven months (and each participant could contribute up to three measurements). The predictors were an indicator for study arm, the baseline value of the outcome (to account for variability in the outcome, which improves the standard error for the estimation of the intervention effect), the follow-up time-point, and covariates. Standard errors were adjusted for clustering at the individual-level following ultimate clustering methods, which recommend that clustering is only necessary for the primary sampling unit, the individual [73]. For all regressions, the covariates consisted of baseline socio-demographic and health-related variables that were associated with the outcome at p < .05. Among participants who completed any follow-up survey, covariates were never missing except for income (n = 2) and residency status (n = 1); overall means were imputed for those cases. Effect sizes were estimated by dividing adjusted regression coefficients by the pooled standard deviation of the outcome at baseline.
We accounted for missingness in the outcomes (i.e., missing follow-up assessments) using nonresponse weights, following recommended procedures for missing data in clinical trials [74]. Specifically, complete cases for each follow up survey were weighted by the inverse of an estimate of the probability of completing the follow up survey. For each follow up, the probability of a complete survey was estimated with logistic regression using baseline data that was not missing for any participant. The model for nonresponse included socio-demographic characteristics (age, education, employment status, Spanish acculturation, and stable housing), baseline measures of the outcomes, and the intervention arm indicator. Among participants with electronically-monitored (MEMS) ART adherence for the first month post-baseline, a similar set of logistic regressions was conducted modeling the probability of collecting adherence at five, six, and seven months. These logistic regression models included the same set of baseline predictors as for the follow-up survey models, with the exception of employment status and functional coping, which were highly correlated with other predictors. After estimating the probability of observation, all weights were standardized to have a mean of one.
RESULTS
Participants
Of the 76 participants randomized, the majority were of Mexican ethnicity (n = 57, 75.0%); five were of Guatemalan ethnicity, five El Salvadorian, three Venezuelan, two Honduran, two Argentinian, one Ecuadorean, and one Nicaraguan. About one-third were U.S. citizens and one-fifth were permanent legal residents (Table I); the remainder were of undocumented legal status (30.7%) or on a temporary visa (17.3%). Nearly half did not have a high school diploma or equivalent, only about one-fifth were employed, and over a quarter had an annual income of less than $5,000. Nearly three-quarters had a recent unstable housing situation. About one-fifth were married or in a committed relationship, and nearly all identified as gay or bisexual. On average, the sample was more highly acculturated in Spanish than in English. Participants had been diagnosed with HIV an average of 17 years, and most (87%) were virally suppressed. None of these characteristics were associated with statistically significant differences between intervention and control participants at baseline, indicating no obvious violations of randomization.
Intervention Facilitator Fidelity
Ratings indicated high fidelity to intervention session content across sessions and observers (i.e., the facilitator, co-facilitator, and supervisor): 93.7% of observer ratings were 3, “completely covered” [M (SD) = 2.93 (0.28)]. Observers agreed on ratings 88.4% of the time.
Primary Outcome: Adherence
Electronically Monitored Adherence.
Figure II shows electronically monitored continuous adherence over time in the intervention and control groups, suggesting an upward trend in adherence post-intervention, after 4–5 months. A repeated-measures regression indicated a marginally significant effect post-intervention for adherence, b (95% CI) = 9.24 (−0.55, 19.03), p = 0.06. This effect indicated that, during the three months after the end of the intervention period, intervention participants on average had an adjusted adherence more than 9% higher than control participants—a medium effect size.
Figure II.
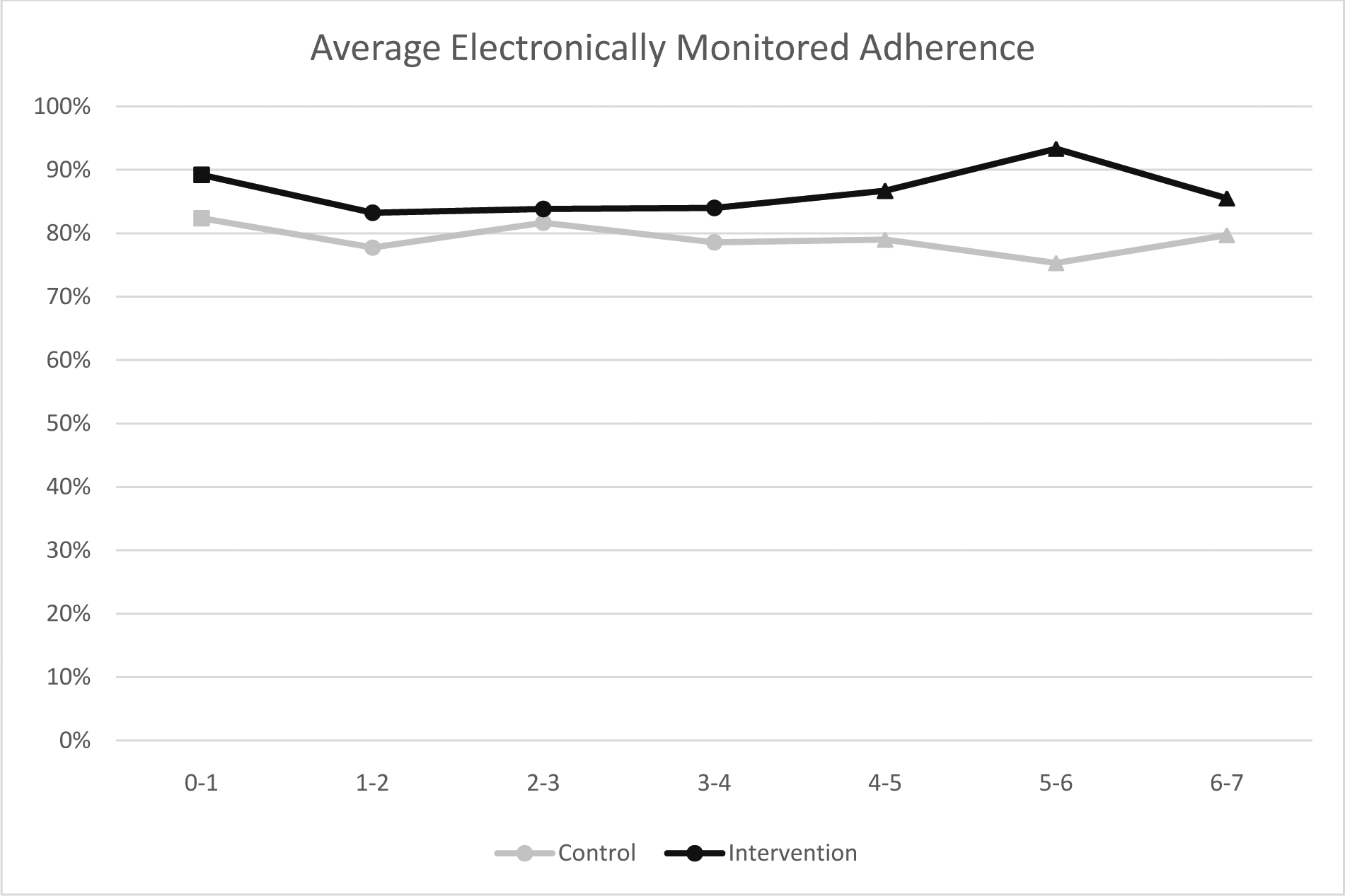
Electronically Monitored Adherence Over Time (in Months) by Study Arm
Note. Squares on the lines designate the preintervention period, circles the intervention period, and triangles the post-intervention period. Repeated-measures regression for intervention vs. control difference in the post-intervention period: b (95% CI) = 9.24 (−0.55, 19.03), p = 0.06 (Cohen’s effect size d = .44).
Regression results and average adherence are weighted to account for presence of data at each month, among those with data at 0–1 month.
Self-reported Adherence.
Repeated-measures regressions indicated that the intervention significantly improved self-reported adherence, b (95% CI) = 4.50 (0.70, 8.30) p = 0.02 (Table II). Although the average percentage of doses taken appeared to increase in both the intervention and control groups, the increase among intervention participants was greater relative to controls (a small effect size of 0.26).
Table II.
Descriptive Statistics and Intention-to-Treat Repeated-Measures Regressions for Study Outcomes (Survey Data)
| Intervention [M (SD) or %] | Control [M (SD) or %] | Repeated-Measures Regressions | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Four-month follow-up | Seven-month follow-up | Baseline | Four-month follow-up | Seven-month follow-up | b (95% CI) or OR (95% CI) and p | Effect Size (Cohen’s d) | |
| Adherence (Self-Report) | ||||||||
| % of doses taken, past month | 94.61 (6.62) | 97.48 (5.42) | 99.17 (1.51) | 91.08 (8.97) | 94.57 (6.56) | 92.91 (16.78) | 4.50 (0.70, 8.30), p = .02 | .26 |
| Coping | ||||||||
| Functional | 2.74 (0.45) | 2.75 (0.43) | 2.82 (0.44) | 2.78 (0.48) | 2.68 (0.36) | 2.74 (0.45) | 0.08 (−0.10, 0.26), p =.39 | .16 |
| Dysfunctional | 2.09 (0.36) | 2.05 (0.33) | 2.06 (0.38) | 2.14 (0.44) | 2.09 (0.41) | 2.09 (0.54) | −0.02 (−0.18, 0.14), p = .81 | .04 |
| Positive religious | 1.86 (0.66) | 1.84 (0.85) | 1.72 (0.84) | 2.14 (0.62) | 2.08 (0.65) | 1.99 (0.72) | −0.09 (−0.37, 0.20), p = .54 | .12 |
| Negative religious | 0.44 (0.48) | 0.17 (0.24) | 0.22 (0.40) | 0.25 (0.35) | 0.34 (0.52) | 0.30 (0.48) | −0.18 (−0.37, 0.01), p = .06 | .43 |
| Medical Mistrust | ||||||||
| General | 2.53 (1.10) | 2.34 (0.94) | 2.28 (1.20) | 2.90 (0.96) | 2.78 (0.96) | 2.88 (1.08) | −0.33 (−0.78, 0.13), p = .16 | .30 |
| HIV conspiracy beliefs | 2.33 (1.06) | 1.81 (0.86) | 1.90 (1.03) | 2.30 (0.94) | 2.26 (0.90) | 2.40 (0.90) | −0.47 (−0.84, – 0.09), p = .02 | .44 |
| Internalized Stigma | ||||||||
| Sexual orientation | 1.70 (0.96) | 1.53 (0.79) | 1.68 (1.06) | 1.84 (0.84) | 1.59 (0.69) | 1.59 (0.85) | 0.08 (−0.32, 0.47), p = .71 | .07 |
| HIV | 2.76 (1.20) | 2.38 (0.93) | 2.14 (0.90) | 2.54 (0.88) | 2.38 (0.98) | 2.65 (1.17) | −0.34 (−0.73, 0.06), p = .10 | .30 |
Notes. Statistics restricted to participants who were randomized and completed either follow-up survey. All means and regression results were weighted to account for nonresponse to either follow-up survey. Effect sizes are defined as the regression coefficient divided by the pooled standard deviation of the outcome at baseline. Covariates were baseline socio-demographic and health characteristics that were associated with the outcome at p < .05: self-reported adherence (Hispanic acculturation); negative religious coping (education, Hispanic acculturation, trauma history); and internalized sexual minority stigma (English acculturation). No covariates were used for functional or dysfunctional coping, positive religious coping, medical mistrust, or internalized HIV stigma.
Secondary Outcomes: Coping, Medical Mistrust, and Internalized Stigma
As shown in Table II, the intervention led to marginally improved coping, in the form of lower negative religious coping, b (95% CI) = −0.18 (−0.37, 0.01), p = .06—a medium effect size of .43 (and a reduction of .18 toward less frequent negative religious coping on the 4-point Likert scale). The intervention also led to significantly reduced HIV-specific medical mistrust (i.e., lower levels of HIV conspiracy beliefs), b (95% CI) = −0.47 (−0.84, −0.09), p = .02—a medium effect size of .44 (and a decrease of about half a point toward greater trust on the 5-point Likert scale). There were no other significant intervention effects for secondary outcomes, most of which showed small effect sizes—with the exception of general medical mistrust and internalized HIV stigma, both of which showed small-to-medium effect sizes.
Intervention Acceptability
In the semi-structured interviews, participants showed high intervention acceptability (Table III). Participants were extremely enthusiastic about the intervention overall and its specific elements, including the context, structure, and facilitators. Specific comments focused on the intervention helping participants to be aware of discrimination experiences when they occurred and giving them options for responding in ways that were effective and consistent with their values and goals. Some participants noted that the sessions were organized in a way that both built content knowledge over time and strong, trusting relationships among members and facilitators. Participants valued how caring and skilled the facilitators were, and said that they learned information from their peers that they could apply to their current situations or that they could imagine being useful in the future. After the group ended, some participants said they continued to journal their daily discrimination experiences in ways that mimicked the take-home assignments.
Table III.
Semi-structured Interview Quotes on Perceived Intervention Acceptability
| Theme | Quote |
|---|---|
| Positive Attitudes about Intervention (Overall, and Related to Content and Structure) | “Because they make you see things, and suddenly, you get to notice, and you realize all the times you have been discriminated before and one may think they have never been discriminated but truth is you have. And then sometimes you think you have not been discriminated against, but deep down is being discriminated against.” (50-year old gay Latinx man; undocumented) “I still practice it today even after the sessions. I’ll write down what it was that happened, what was I doing, and how I responded, and who was I with. For instance, not too long ago, I was attacked by a homeless man. He spat on me and insulted me. [Before I participated,] I would have fallen into his provocations, but I did not. I did not get physical with him because, if I did, I would end up in prison. I was looking out for my best interests, so I just walked away… But I walked away being free.” (60 year-old gay Latinx man; U.S. citizen) “All the topics/talks were centered around discrimination. But for me, in each session, I learned something new every day, week after week. Each week, there was something new that was taught, and it was important for me … It was a beautiful experience, you get to know more, and then you realize that you are not the only one… and you learn from other people’s discrimination experiences. But you may go through similar situations in the future, then you know how to deal with the situations.” (48 year-old gay Latinx man; permanent resident) |
| Positive Attitudes about Facilitators | “[They] are great facilitators. They are very comprehensive, very good at explaining. I have a really good impression of both of them.” (70 year-old gay Latinx man; U.S. citizen) “In my opinion, I think they are great people. I think they are very capable and qualified to speak on the topics that were discussed. They have experience, and so they can help you more… The best thing they knew how to do is to direct the group, how to establish trust with everyone, and then how to interact with all of us in the group.” (33 year-old gay Latinx man; expired visa) “They led the group very well—a group of 8 people, 8 different perspectives. Even though we shared [some identities], we, all of us, had different thoughts … Yes, they were able to manage all that and they treated us well. They answered the questions well. They knew to make the workshops, the seminar, very pleasant.” (52 year-old gay Latinx man; U.S. citizen) |
| Suggestions for Improvement |
Longer Sessions: “[I suggest] for the time of the sessions to be longer. Because there is much more to talk about but time does not allow it, because there is not sufficient time.” (55 year-old gay Latinx man; temporary visa) More Sessions: “For me, everything went very well! I would like there to be more sessions, and more groups. For me, that would be best, because it is such a beautiful communication. [I would want] to know more about our medications, to know so much more about HIV.” (52 year-old gay Latinx man; permanent resident) Additional Content: “[I would have liked the groups to focus] more on immigration. There are some of my fellow participants who do not have proper documents—they are immigrants—and immigration services would help.” (53 year-old gay Latinx man; suspended deportation) |
| Concerns |
Diversity of Latinx Experiences: “I went only once and decided that I didn’t feel comfortable with the conversation they had… because one [other participant who] was White, they were ‘more worthy,’ and talked about, as a child, attending a private Catholic school in Mexico. He said that he got in trouble and that the nun said, ‘You should be thankful that you are White because if you were Brown I would have given you a worse punishment! ‘ And, as I consider myself Brown, I said, for me, where do I stand in this? … but I felt bad that day, and I didn’t feel like coming back. And then you [and other staff] called me to see if I wanted to come back. I felt the urge but not the courage to come back, as I imagined that the discussion could be the same as the last week’s.” (55 year-old bisexual Latinx man; permanent resident) Material Too Intense: “It brought me bad memories, or it made me re-live past moments in my life. Childhood memories, that I thought I had forgotten about—and referencing now to my current life—made me feel really uncomfortable. I had to talk to my therapist, because it was too much for me to take, what had happened to me [in childhood].” (58 year-old bisexual Latinx man; permanent resident) Other group members’ Disrespectful or Inconsistent Participation, or Failure to Maintain Confidentiality: “I was not willing to attend the presentations anymore because I felt uncomfortable. Of the people who surrounded me, at that moment, some of the people—two or three of them—they usually talked about [the group content] outside the room where these meetings were held. So, it makes me uncomfortable to say anything that should be private and that should be kept in confidence.” (78 year-old gay Latinx man; U.S. citizen) “The only bad thing I found to be [frustrating] was the poor participation from fellow members. That took away a bit of my attention and peace because I expected everyone to show up every week… I know that, on your behalf, an excellent job was done and that this is out of the control for the study team. And, from them, they did not give it the time—maybe it was because of work, or for whatever reason they did not sacrifice—like some of us did. And I found that bad… because this minimizes their credibility.” (53 year-old heterosexual Latinx man; permanent resident) “I did not feel as if I could trust [the other group members]. Because I noticed that when [one participant] talked, there was someone making fun of him, or saying comments and whispering, and so, for that reason I did not feel as if I could trust [the group].” (33 year-old gay Latinx man; expired visa) |
Participants made suggestions about changes that they believed would improve the program. Many suggested increasing the dose of the intervention, either by making each session longer, by adding more sessions, or both. Some participants made suggestions for content and format, including content that was covered but that they wanted more information about—such as HIV or immigration—and some areas that the intervention did not specifically cover, such as economic problems/poverty.
Seven participants expressed concerns. Two participants noted that the group discussion sometimes did not feel sensitive to the diversity of ethnicities and cultures represented among the Latinx participants. For example, one participant who described his race as “Brown” felt that he could not relate to other participants, due to an anecdote shared by a group member who identified as “White.” One participant stated that initial material on discrimination was too intense—triggering what sounded like re-experiencing of past traumatic experiences (not discrimination-related). Four participants expressed frustration about behaviors of group members, including witnessing what they saw as a lack of respectful communication, perceiving a failure to maintain confidentiality outside of the sessions, or observing some members’ inconsistent attendance.
DISCUSSION
The present study demonstrated high acceptability and preliminary effectiveness of Siempre Seguiré, a group-based CBT intervention that addresses coping with intersectional stigma and discrimination that was developed using CBPR methods. Our study provides evidence that a CBT intervention focused on coping with discrimination can lead to improved ART adherence, at least in the short-term. Prior tests of CBT interventions have similarly led to improvements in adherence and other health-related behaviors [32, 36]. However, prior interventions have used CBT explicitly to build adherence skills and set up a detailed plan for improving adherence through, for example, cue control strategies (e.g., alarm reminders) or restructuring beliefs about adherence. Our intervention suggests that a CBT group with a broad focus on skills-building to respond effectively to stigma and discrimination can improve adherence as well, with medium effect sizes that are comparable to what has been found in prior research [36].
Intervention feasibility was moderate, in that the majority (over 60%) of participants attended nearly all sessions, and two-thirds attended over half of sessions. Nearly all reasons for lack of attendance were directly related to challenges in the men’s lives and not to the intervention itself. For example, several individuals moved outside of the study area, including out of the country. Our results reflect the difficulties in retaining members of especially vulnerable populations in multi-session intervention programs, and suggest the possibility that alternate intervention modalities (e.g., more frequent sessions over a shorter timeframe, or online sessions) may be helpful for some men. In the present study, if a participant were to miss a session, the facilitators met with him prior to the start of the next session to review the previous sessions’ material and, thus, they were still exposed to key content. However, these participants did not gain the full benefits of social support and of learning through the group process and skills modeling, practice, and feedback.
Results for secondary outcomes were mixed. For example, there is some evidence that the intervention may have led to decreased belief in HIV conspiracies, a form of medical mistrust—although general levels of medical mistrust were unchanged. These disparate results may result from the intervention’s strong HIV focus. The intervention addressed beliefs and misconceptions about HIV medications specifically, rather than overall beliefs about healthcare and the medical system. Further, the intervention did not improve changes in the frequency of coping strategies use, except for use of negative religious coping—which, interestingly, was not a coping strategy discussed more or less than the others. Perhaps there were changes in the quality or consequences of coping responses—but the measures we included did not capture that facet of coping.
We acknowledge some limitations. We recruited participants using convenience sampling at one community-based organization in one U.S. county, and the majority of participants were from Mexico. Thus, generalizability is limited, and results may vary among different locations or immigrant groups. There were some elements that we did not measure, such as birth country (and whether those who were U.S. citizens were U.S.-born), or the quality of coping responses. Moreover, the sample size was small and the statistical analyses were underpowered, potentially leading to some of the mixed results we observed—and we could not test mediational effects, such as whether the intervention’s effects on improved coping and reduced medical mistrust led, in turn, to better adherence. Thus, our promising results need to be confirmed in a fully powered randomized controlled trial in which hypotheses about mediation and any moderating effects of participant characteristics can be fully tested.
CONCLUSIONS
In conclusion, the present study showed promising effects of Siempre Seguiré, an intervention that aims to change vulnerable individuals’ coping responses to intersectional stigma and discrimination and in turn, improve their health and health behaviors. Future research should work to develop and test anti-racism interventions and policies in tandem with such individual-level interventions, to change the structures in society from which discrimination originates.
ACKNOWLEDGMENTS
This study was supported by the National Institutes of Mental Health (R34 MH113413, R01MH121256, P30MH058107).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
ClinicalTrials.gov ID (TRN): NCT03432819, 01/31/2018
Ethics approvals: All procedures performed were in accordance with the ethical standards of the institutional review boards of the RAND Corporation and Los Angeles County Department of Public Health, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate: Freely-given, informed consent to participate in the study was obtained from all participants.
REFERENCES
- 1.CDC. HIV Surveillance Report, 2017. 2018; Vol. 29. [Google Scholar]
- 2.McCree DH, Williams AM, Chesson HW, et al. Changes in disparities in estimated HIV incidence rates among Black, Hispanic/Latino, and white men who have sex with men (MSM) in the United States, 2010–2015. J Acquir Immune Defic Syndr. 2019;81(1):57–62. [DOI] [PubMed] [Google Scholar]
- 3.Levison JH, Levinson JK, Alegría M. A critical review and commentary on the challenges in engaging HIV-infected Latinos in the continuum of HIV care. AIDS Behav. 2018;22(8):2500–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2012;14(1):65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dailey AF, Hoots BE, Hall HI, et al. Vital signs: Human Immunodeficiency Virus testing and diagnosis delays—United States. MMWR. 2017;66(47):1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lillie-Blanton M, Stone VE, Snow Jones A, et al. Association of race, substance abuse, and health insurance coverage with use of highly active antiretroviral therapy among HIV-infected women, 2005. Am J Public Health. 2010;100(8):1493–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gant Z, Dailey A, Hu X, Johnson AS. HIV care outcomes among Hispanics or Latinos with diagnosed HIV infection - United States, 2015. MMWR. 2017;66(40):1065–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crepaz N, Dong X, Wang X, Hernandez AL, Hall HI. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV Care - United States, 2014. MMWR. 2018;67(4):113–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bogart LM, Chetty S, Giddy J, et al. Barriers to care among people living with HIV in South Africa: contrasts between patient and healthcare provider perspectives. AIDS Care. 2013;25(7):843–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogart LM, Cowgill BO, Kennedy D, et al. HIV-related stigma among people with HIV and their families: a qualitative analysis. AIDS Behav. 2008;12(2):244–54. [DOI] [PubMed] [Google Scholar]
- 11.Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychol. 2003;22(5):533–40. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser Family Foundation. 2011 Survey of Americans on HIV/AIDS Washington, D.C.: Kaiser Family Foundation; 2012. Available from: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8186-t.pdf. [Google Scholar]
- 13.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Ann Behav Med. 2010;40(2):184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving towards resilience. Am Psychol. 2013;68(4):225–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. [DOI] [PubMed] [Google Scholar]
- 16.Williams DR. The health of men: structured inequalities and opportunities. Am J Public Health. 2008;98(Supplement_1):S150–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003;25(1):55–65. [DOI] [PubMed] [Google Scholar]
- 18.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54:805–16. [DOI] [PubMed] [Google Scholar]
- 19.Landrine H, Klonoff EA. The schedule of racist events: a measure of racial discrimination and a study of its negative physical and mental health consequences. J Black Psychol. 1996;22(2):144–68. [Google Scholar]
- 20.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among Blacks and whites in the United States. Am J Public Health. 2006;96(5):826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fields EL, Bogart LM, Galvan FH, Wagner GJ, Klein DJ, Schuster MA. Association of discrimination-related trauma with sexual risk among HIV-positive African American men who have sex with men. Am J Public Health. 2013;103(5):875–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frost DM, Lehavot K, Meyer IH. Minority stress and physical health among sexual minority individuals. J Behav Med. 2015;38(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bogart LM, Takada S, Cunningham WE. Medical Mistrust, Discrimination, and the Domestic HIV Epidemic. In: Ojikutu B, Stone V, editors. HIV in US Communities of Color: Springer. p. 207–31. [Google Scholar]
- 26.Newheiser A-K, Farias M, Tausch N. The functional nature of conspiracy beliefs: examining the underpinnings of belief in the Da Vinci Code conspiracy. Pers Individ Differ. 2011;51(8):1007–11. [Google Scholar]
- 27.van Prooijen JW, Acker M. The influence of control on belief in conspiracy theories: conceptual and applied extensions. Appl Cogn Psychol. 2015;29(5):753–61. [Google Scholar]
- 28.Bogart LM, Galvan FH, Leija J, MacCarthy S, Klein DJ, Pantalone DW. A pilot intervention addressing coping with discrimination among HIV-positive Latino sexual minority men. Ann LGBTQ Public Pop Health. 2020;1(1):6–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wyatt GE. Enhancing cultural and contextual intervention strategies to reduce HIV/AIDS among African Americans. Am J Public Health. 2009;99(11):1941–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myers JR, Ball K, Jeffers SL, Lawson WB. Medical mistrust, HIV-related conspiracy beliefs, and the need for cognitive closure among urban-residing African American women: an exploratory study. J Health Dispar Res Pract. 2018;11(4):138–48. [Google Scholar]
- 31.Crocker J, Luhtanen R, Broadnax S, Blaine BE. Belief in US government conspiracies against Blacks among Black and white college students: powerlessness or system blame? Pers Soc Psychol Bull. 1999;25(8):941–53. [Google Scholar]
- 32.Safren SA, O’Cleirigh C, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80(3):404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Safren SA, Gonzalez JS, Wexler DJ, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in patients with uncontrolled type 2 diabetes. Diabetes Care. 2014;37(3):625–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL. Interventions to improve medication adherence among older adults: meta-analysis of adherence outcomes among randomized controlled trials. Gerontol. 2009;49(4):447–62. [DOI] [PubMed] [Google Scholar]
- 36.Pantalone DW, Nelson KM, Batchelder AW, Chiu C, Gunn HA, Horvath KJ. A systematic review and meta-analysis of combination behavioral interventions co-targeting psychosocial syndemics and HIV-related health behaviors for sexual minority men. J Sex Res. 2020;20:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cruess S, Antoni MH, Hayes A, et al. Changes in mood and depressive symptoms and related change processes during cognitive-behavioral stress management in HIV-infected men. Cognit Ther Res. 2002;26(3):373–92. [Google Scholar]
- 38.Folkman S, Chesney M, McKusick L, Ironson G, Johnson DS, Coates TJ. Translating coping theory into an intervention. In: Eckenrode J, editor. The Social Context of Coping. The Plenum Series on Stress and Coping New York, NY: Plenum Press; 1991. p. 239–60. [Google Scholar]
- 39.Bogart LM, Dale SK, Daffin GK, et al. Pilot intervention for discrimination-related coping among HIV-positive Black sexual minority men. Cult Divers Ethnic Minor Psychol. 2018;24(4):541–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hedges LV, Citkowicz M. Estimating effect size when there is clustering in one treatment group. Behav Res Methods. 2015;47(4):1295–308. [DOI] [PubMed] [Google Scholar]
- 41.Israel B, Eng E, Schulz A, Parker E. Methods of Community Based Participatory Research. 2nd ed. San Francisco, CA: Jossey-Bass; 2013. [Google Scholar]
- 42.Wallerstein N, Duran B, Oetzel JG, Minkler M. Community-based Participatory Research for Health: Advancing Social and Health. 3rd ed. San Francisco, CA: Jossey-Bass; 2018. [Google Scholar]
- 43.Linehan MM. Skills training manual for treating borderline personality disorder. New York; NY: Guilford Press; 1993. [Google Scholar]
- 44.Dimidjian S, Linehan MM. Mindfulness Practice. In: O’Donohue WT, Fisher JE, editors. General principles and empirically supported techniques of cognitive behavior therapy. Hoboken, NJ,: John Wiley & Sons Inc.; 2009. p. 425–34. [Google Scholar]
- 45.Ellis A Cognitive restructuring of the disputing of irrational beliefs. In: O’ Donohue WT, Fisher JE, editors. Cognitive behavior therapy: Applying empirically supported techniques in your practice. 2nd ed. Hoboken, N J: Wiley & Sons, Inc.; 2008. p. 79–83. [Google Scholar]
- 46.Newman CF. Identifying and modifying maladaptive schemas. In: O’ Donohue WT, Fisher JE, editors. Cognitive Behavior Therapy: Applying empirically supported techniques in your practice. Hoboken, NJ: Wiley & Sons, Inc.; 2008. p. 89. [Google Scholar]
- 47.Ferguson KE, Sgambati RE. Relaxation. In O’Donohue WT & Fisher JE (Eds.), editor. Hoboken, NJ, US: John Wiley & Sons Inc.,2008. 434–44 p. [Google Scholar]
- 48.Rizvi SL, Ritschel LA. Mastering the art of chain analysis in dialectical behavior therapy. Cogn Behav Pract. 2014;21(3):335–49. [Google Scholar]
- 49.Heidt JM, Marx BP. Self-monitoring as a treatment vehicle. In: O’ Donohue WT, Fisher JE, Hayes SC, editors. Cognitive Behavior Therapy: Applying empirically supported techniques in your practice. Hoboken, NJ: Wiley & Sons, Inc.; 2004. p. 361–7. [Google Scholar]
- 50.O’Donohue WT, Fisher JE, Hayes SC. Cognitive Behavior Therapy: Applying Empirically Supported Techniques in Your Practice. Hoboken, NJ: Wiley & Sons, Inc.; 2004. [Google Scholar]
- 51.Bowleg L “Once you’ve blended the cake, you can’t take the parts back to the main ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. J Sex Roles. 2013;68(11–12):754–67. [Google Scholar]
- 52.Cole ER. Intersectionality and research in psychology. J Am Psychol. 2009;64(3):170. [DOI] [PubMed] [Google Scholar]
- 53.Moradi B, Grzanka PR. Using intersectionality responsibly: Toward critical epistemology, structural analysis, and social justice activism. J Couns Psychol. 2017;64(5):500–513. [DOI] [PubMed] [Google Scholar]
- 54.Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: The Bidimensional Acculturation Scale for Hispanics (BAS). Hisp J Behav Sci. 1996;18(3):297–316. [Google Scholar]
- 55.Arnsten JH, Demas PA, Farzadegan H, et al. Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: comparison of self-report and electronic monitoring. Clin Infect Dis. 2001;33(8):1417–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bangsberg DR, Hecht FM, Charlebois ED, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14(4):357–66. [DOI] [PubMed] [Google Scholar]
- 57.Bogart LM, Mutchler MG, McDavitt B, et al. A randomized controlled trial of Rise, a community-based culturally congruent adherence intervention for Black Americans living with HIV. Ann Behav Med. 2017;51(6):868–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cunningham WE, Nance RM, Golin CE, et al. Self-reported antiretroviral therapy adherence and viral load in criminal justice-involved populations. BMC Infec Dis. 2019;19(1):913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carver CS. You want to measure coping but your protocol too long: consider the brief cope. Int J Behav Med. 1997;4(1):92–100. [DOI] [PubMed] [Google Scholar]
- 61.Pargament K, Feuille M, Burdzy D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions. 2011;2(1):51–76. [Google Scholar]
- 62.MacCarthy S, Bogart LM, Galvan FH, Patel KN, Pantalone DW. Experiences with between- and within-group discrimination among Latino MSM living with HIV in Los Angeles, California. Ann LGBTQ Public Population Health. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Krägeloh CU. A systematic review of studies using the Brief COPE: Religious coping in factor analyses. Religions. 2011;2(3):216–46. [Google Scholar]
- 64.Rood BA, McConnell EA, Pantalone DW. Distinct coping combinations are associated with depression and support service utilization in men who have sex with men living with HIV. J Psychol Sex Orientat Gend Divers. 2015;2(1):96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(1_suppl):146–61. [DOI] [PubMed] [Google Scholar]
- 66.Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005;38(2):213–8. [DOI] [PubMed] [Google Scholar]
- 67.Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. J Couns Psychol. 2009;56(1):32–43. [Google Scholar]
- 68.Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ryan GW, Bernard HR. Data Management and Analysis Methods. In: Denzin N, Lincoln Y, editors. Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 2000. p. 769–802. [Google Scholar]
- 70.Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003;15(1):85–110. [Google Scholar]
- 71.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37–46. [Google Scholar]
- 72.Bakeman R, Gottman JM. Observing interaction: an introduction to sequential analysis. New York, NY: Cambridge University Press; 1997. [Google Scholar]
- 73.Kalton G. Ultimate cluster sampling. J Royal Stats Society. 1979;142(2):210–22. [Google Scholar]
- 74.Little RJ, D’Agostino R, Cohen ML, et al. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367(14):1355–60. [DOI] [PMC free article] [PubMed] [Google Scholar]


