Abstract
Little is known about how social networks among women who inject drugs (WWID) can be leveraged to increase awareness about pre-exposure prophylaxis (PrEP). We tested the hypothesis that interpersonal characteristics influence willingness of WWID to communicate PrEP information with peers. Forty WWID ≥ 18 years completed social network surveys. Participants named on average 9.3 (SD = 3.3) network members, resulting in 375 unique relationships. WWID were willing to share PrEP information with 83% of network members. Participants had higher odds of willingness to share information within relationships when the network member was female, homeless and perceived to be at risk for HIV. Among relationships with family members and transactional sex clients, stronger emotional closeness was associated with higher odds of willingness to share information. Peer interventions where WWID share PrEP information with peers may be an efficient approach to increase PrEP awareness among this vulnerable population.
Keywords: Interpersonal communication, HIV prevention, Women who inject drugs, Peer support
Introduction
In North America, an estimated 2.5 million people have injected drugs (PWID) in the previous year, 30% (766,000) of whom are women [1]. While new HIV diagnoses among PWID in the United States (US) dropped dramatically from 40% in the 1990s to 6% in 2017 [2], injection drug use fuelled by the opioid crisis has been associated with HIV outbreaks across the country [3–6]. Women who inject drugs (WWID) are particularly at risk for HIV given difficulties negotiating the use of harm reduction supplies, such as condoms and sterile syringes, with male partners [7, 8]. This suggests an urgent need to scale programs that arm at-risk WWID with woman-controlled HIV prevention tools, such as daily oral pre-exposure prophylaxis (PrEP) [9].
Despite its immense promise, WWID remain largely unaware of PrEP [10–12] and therefore have little opportunity to benefit from this medication. While efforts to increase WWID’s awareness about PrEP are clearly needed [13–15], traditional strategies, such as education sessions during medical appointments, are suboptimal for reaching WWID given their limited engagement with traditional health-care systems [16–18]. Innovative approaches are therefore needed to deliver PrEP information to WWID. One such approach may be to leverage social networks, such as by having WWID deliver information about PrEP to peers in their social networks. This has been an effective approach to increase awareness and utilization of other HIV prevention methods (i.e. use of condoms) [19–24], which suggests a similar approach could be used to promote PrEP among WWID.
Research suggests that individuals from vulnerable populations (e.g., men who have sex with men) are willing and interested in sharing PrEP information with people they know [25, 26]. However, little is known about with which network members (e.g. friends, romantic partners etc.) these individuals would be willing to share PrEP information. Knowing this is important because outcomes from peer-delivered HIV interventions focusing on other harm reduction approaches among PWID show differential information spread among network members by relationship type [21, 22, 27]. For example, information tends to be delivered to friends and people who use drugs, but rarely to sex partners [21, 28]. This suggests that that not all relationships are conducive to the sharing of intervention information, and that peer-led information diffusion interventions would benefit from a deeper understanding of the characteristics of relationships that facilitate or challenge the interpersonal communication of HIV-related information.
To understand how and why information may be communicated within relationships, research often focuses on three elements known to influence interpersonal communication: social relations, similarities, and interactions [29]. (1) Social Relations reflects the type of social connection two people share, such as the social role (e.g. kin, friend, etc.) and emotional closeness [30]. For example, Roberts and Dunbar (2011) show that among social networks of 251 women, relationships characterized by higher emotional closeness communicate more frequently. This association was moderated by social role, whereby the effect of emotional closeness on communication frequency was greater for kin than for friends [31]. (2) Homophily refers to the extent to which people share attributes, such as being of the same sex. The more similar people are, the more likely they are to communicate [32]. (3) Interactions refer to the series of interchanges that occur within relationships, such as what individuals do together (e.g. have sex) and relationship length. For example, relationship length has been positively associated with communication about sexual health topics, such as HIV status disclosure [33].
This study uses a social network approach to identify the degree to which characteristics of relationships influence WWID’s willingness to share PrEP information with social network members. We hypothesized that social relations, similarities and interactions within relationships influence willingness to share PrEP information. Additionally, given that emotional closeness influences communication differently given the specific social role [31], we hypothesize that there will be an interaction between emotional closeness and social role such that when there is higher emotional closeness within relationships, women will have increased willingness to share information.
Methods
Sample
Participants were recruited from a PrEP demonstration project assessing barriers and facilitators to PrEP engagement when clinical care was provided to 95 WWID within a community-based syringe services program (SSP) in Philadelphia. Participants were HIV-negative English-speaking cisgender females, 18 years or older, who were eligible for PrEP based on CDC clinical guidelines [34] and were offered a PrEP prescription. To be eligible for the present study, women had to be enrolled in the PrEP demonstration project and answer affirmatively to the following baseline question: Would you be willing to talk to someone you know about PrEP, such as telling someone what PrEP is? This could include a friend, a sex partner, family member etc. Recruitment for the present study occurred sequentially, based on examination of the baseline question.
Data Collection
Baseline data about participant characteristics was obtained from the PrEP demonstration project baseline survey. To collect the social network data, one interviewer administered a Qualtrics survey via an iPad, conducted in a private space at the SSP. All participants received a $20 gift card incentive for completing the interview which was approximately one hour. Research was approved by the institutional review boards at Drexel University and Prevention Point Philadelphia. Because we describe the study sample in terms of participants as well as their social network members (hereafter referred to as “alters”) we use the letter “n” to designate sample size related to participants, and “m” to designate sample size related to alters.
Measures
Participant-Level Data
Participant-level data include socio-demographic characteristics such age (measured in years), race (categorized as non-Hispanic White, non-Hispanic Black or Other), home-lessness (yes/no), engagement in transactional sex in the last 6 months (yes/no) and whether participants accepted a PrEP prescription in the demonstration project (yes/no). Self-perceived HIV risk was measured on a 5-point Likert scale ranging from extremely unlikely to extremely likely to acquire HIV. Due to small cell sizes, HIV risk was dichotomized to extremely/very likely or extremely/very unlikely/neutral for analysis.
Network Instrument
Social networks were delineated using a set of name generating questions to elicit up to 20 network members with whom participants have interacted in the past 6 months, which included: 5 people with whom participants discussed important matters; 5 people with whom participants have had sex; 5 people with whom participants injected drugs; and 5 women who inject drugs. Socio-demographic characteristics of alters, as reported by participants, included age (in years), gender (answer choices male, female, trans male or trans female), and race/ethnicity (answer choices non-Hispanic White, non-Hispanic Black and non-Hispanic other).
Social relations were assessed by eliciting: the main relationship type with each alter (e.g. acquaintance, family member, main romantic partner, etc.), emotional closeness (scale from 0–10, where 0 is no closeness and 10 is high closeness), trust (scale 0–10, where 0 is no trust and 10 is high trust), and frequency of verbal and physical arguments (answer choices never, rarely, often, or always) [35], and whether or not the participant thinks the alter currently is homeless, injects drugs, engages in transactional sex, and takes PrEP. We also assessed perceptions of alters’ HIV status (answer choices HIV positive, negative or unsure), HIV risk (answer choices none, low, medium and high, later dichotomized to medium/high and none/low) and interest in taking PrEP (Likert scale 1–7 where 1 indicated no interest and 7 highly interested).
Homophily was measured with a set of variables indicating whether or not each participant/alter dyad were of the same race, gender, and if they both engaged in transactional sex or injection drug use. A variable was generated to assess age differences between the participant and alter by subtracting participant age from alter age. Geographic distance was assessed by asking, “How far do you live from [alter x]” (answer choices within my same neighborhood or outside my neighborhood).
Social interactions were assessed by asking participants if they have had sex or shared injection drug equipment with each alter, both within the last 6 months. Frequency of interaction was measured with, “How often do you talk with or see each of the people you have listed?” (answer choices multiple times a week or monthly/less frequently). Length of relationship was also assessed (in years).
The primary outcome of interest is willingness to share PrEP information within each dyad. To assess this, participants were presented with the following prompt:
Let’s pretend that we developed a program where we trained and paid women to spread information about PrEP to people who they know. For example, tell them what PrEP is, what it does, and where they could go to access it. We are interested in knowing who you would be willing to give information about PrEP to. It is OK to be willing to give information to some but not all people.
Participants were then asked of each alter, “Would you be willing to give information about PrEP to [alter x]?” (answer choices no/yes).
Analysis
Analyses were performed using STATA version 14 [36]. Descriptive statistics were constructed to examine participant, alter and relationship-level summary measures. Logistic generalized estimating equations (GEE) models were used to examine the bivariate relationship between each predictor variable and the primary outcome of willingness to share PrEP information within each relationship, with the participant-alter dyad being the unit of analysis. GEE was used to account for the correlated nature between participants and alters that is inherent in social network data. Next, a multivariable logistic GEE model was fit using purposive model selection [38]: first, variables from bivariate analyses significant at the a priori significance level of p = 0.20 were included simultaneously in a single model [38]. Because alter gender and gender homophily conceptually measured the same construct, only gender homophily was included in the multivariable model. Next, variables significant at ≤ p = 0.10 were retained for the final model. Finally, an interaction between emotional closeness and relationship type was examined using a product term to evaluate our a priori hypothesis that higher emotional closeness would increase willingness to share PrEP information across relationship types.
Results
Participant, Alter and Relational Characteristics
Table 1 shows that participants (n = 40) were predominately White (54%, n = 20) with a mean age of 40.1 (SD ± 9.3), and 60.0% were currently homeless (n = 24). Half (47.5%, n = 19) perceived themselves to be at high risk for HIV, and almost all accepted a PrEP prescription through the demonstration project. The forty WWID named a mean of 9.3 network members (SD ± 3.3) for a total of 375 dyads. Table 2 shows that alters (m = 375) were mostly female (63%, m = 237) and White (54%, m = 203). The most frequently reported alter relationships were friends (36%, m = 133) and acquaintances (23%, m = 87), and participants usually interacted with alters daily or multiple times per week (72%, m = 271). About one-third of alters (34%, m = 126) were homeless, and half (51%, m = 186) of alters were perceived to be at risk for HIV.
Table 1.
Participant Characteristics (n = 40)
| Mean Age ± SD | 40.1 ± 9.3 |
|---|---|
| Race (n = 37)* | |
| White | 20 (54.1%) |
| Black | 11 (29.7%) |
| Other | 6 (16.2%) |
| Hispanic ethnicity | 6 (15.0%) |
| Currently homeless | 24 (60.0%) |
| Transactional sex | 25 (92.5%) |
| Perceives herself as extremely/very likely to acquire HIV | 19 (47.5%) |
| Accepted PrEP Rx | 39 (97.5%) |
| Mean network size ± SD | 9.3 ± 3.3 |
Does not add to 40 due to missing data
Table 2.
Predictors of willingness to Share PrEP information within Dyads (Tie Level, m = 375)
| Total sample | Willing to share PrEP information within Dyad | ||||
|---|---|---|---|---|---|
| No 63 (16.8%) | Yes 312 (83.2%) | Unadjusted Odds Ratios (95%CI) | Adjusted Odds Ratios (95% CI) | ||
| Alter socio-demographics | |||||
| Mean Age ± SD | 40.0 ± 12.8 | 43.8 ± 14.7 | 39.2 ± 12.2 | 0.9** (0.9–0.9) | – |
| Female | 237 (63.2) | 19 (30.2) | 218 (69.9) | 5.8** (2.5–13.6) | – |
| Race | |||||
| White | 203 (54.3) | 23 (36.5) | 180 (57.9) | REF | – |
| Black | 116 (31.0) | 31 (49.2) | 85 (27.3) | 0.36** (0.2–0.8) | – |
| Other | 55 (14.7) | 9 (14.3) | 46 (14.8) | 0.65 (0.3–1.6) | – |
| Hispanic ethnicity | 49 (13.1) | 9 (14.2) | 40 (12.9) | 0.84 (0.4–1.9) | – |
| Social relations | |||||
| Relationship | |||||
| Acquaintance | 87 (23.2) | 13 (20.6) | 74 (23.7) | REF | REF |
| Friend | 133 (35.5) | 13 (20.6) | 120 (38.5) | 1.03 (0.9–1.1) | 0.6 (0.1–5.4) |
| Family member | 64 (17.1) | 9 (14.3) | 55 (17.6) | 1.02 (0.9–1.2) | 0.1** (0.0–0.3) |
| Main romantic partner | 29 (7.7) | 5 (7.9) | 24 (7.7) | 1.0 (0.8–1.1) | 1.0 (0.0–33.8) |
| Casual sex partner | 14 (3.7) | 6 (9.5) | 8 (2.6) | 0.2** (0.0–1.3) | 0.7 (0.02–19.3) |
| Transactional sex client | 23 (6.1) | 11 (17.5) | 12 (3.9) | 0.1** (0.0–0.6) | 0.1 (0.0–1.8) |
| Drug buddy | 25 (6.7) | 6 (9.5) | 19 (6.1) | 0.8* (0.7–0.9) | 0.6 (0.0–8.4) |
| Mean trust ± SD | 5.6 ± 3.5 | 4.5 ± 3.12 | 5.8 ± 3.6 | 1.1** (1.0–1.3) | 0.56 (0.1–5.4) |
| Mean emotional closeness ± SD | 5.8 ± 3.31 | 4.4 ± 2.9 | 6.1 ± 3.3 | 1.2** (1.0–1.4) | – |
| Never/rarely verbally fight | 271 (72.3) | 44 (69.8) | 227 (72.8) | 1.0 (1.0–1.1) | – |
| Never/rarely physically fight | 351 (93.8) | 60 (95.2) | 291 (93.6) | 1.0 (0.9–1.2) | – |
| Homeless | 126 (34.0) | 9 (14.8) | 117 (37.7) | 3.3** (1.5–7.6) | 2.8* (1.0–7.5) |
| Injects drugs | 231 (61.6) | 28 (44.4) | 203 (65.1) | 2.3** (1.1–4.7) | – |
| Receives drugs/money/goods in exchange for sex | 157 (41.8) | 10 (15.9) | 147 (47.1) | 4.5** (1.6–12.5) | – |
| Perceived HIV status of alter | |||||
| HIV negative | 223 (59.5) | 47 (74.6) | 176 (56.4) | REF | – |
| HIV positive | 9 (2.4) | 1 (1.6) | 8 (2.5) | 1.1 (0.8–1.4) | – |
| Unknown HIV status | 143 (38.1) | 15 (23.8) | 128 (41.0) | 1.1* (1.0–1.2) | – |
| Perceived to be at high/medium risk for HIV | 186 (50.8) | 21 (33.9) | 165 (54.3) | 1.1* (1.1–1.2) | 4.2* (1.6–11.1) |
| Currently taking PrEP | 19 (5.1) | 0 (0.0) | 19 (6.1) | 1.2+ (0.9–1.4) | – |
| Mean alters’ interest in taking PrEP ± SD | 3.3 ± 2.5 | 2.4 ± 1.9 | 3.5 ± 2.6 | 1.0 (1.0–1.0) | – |
| Homophily | |||||
| Gender homophily | 237 (63.2) | 19 (30.2) | 218 (69.9) | 5.8** (2.5–13.6) | 3.7* (1.2–11.6) |
| Race/ethnicity homophily | 234 (64.7) | 40 (64.5) | 194 (64.7) | 1.0 (0.9–1.1) | – |
| Injection drug use Homophily | 231 (61.6) | 28 (44.4) | 203 (65.1) | 2.3* (1.1–4.7) | – |
| Transactional sex homophily | 95 (25.8) | 5 (7.9) | 90 (29.5) | 1.2* (1.1–1.2) | – |
| Mean age difference ± SD | 0.25 ± 1.9 | −2.0 ± 1.9 | 0.7 ± 0.78 | 1.0 (1.0–1.0) | – |
| Do not live in same neighborhood | 209 (55.7) | 25 (39.7) | 184 (59.0) | 0.5+ (0.2–1.0) | – |
| Interactions within Dyads | |||||
| Shares drug injection equipment | 18 (7.8) | 3 (10.7) | 15 (7.4) | 0.95 (0.8–1.1) | – |
| Sexual relationship | 85 (22.7) | 27 (42.9) | 58 (18.6) | 0.3** (0.1–0.5) | – |
| Frequency of interaction | – | ||||
| Daily/multiple times per week | 271 (72.3) | 36 (57.1) | 235 (75.3) | REF | – |
| Monthly | 76 (20.3) | 18 (28.6) | 58 (18.6) | 0.5+ (0.3–1.1) | – |
| Yearly or less | 28 (7.5) | 9 (14.3) | 19 (6.1) | 0.3+ (0.1–1.0) | – |
| Mean relationship length in years ± SD | 11.4 ± 0.73 | 14.6 ± 18.2 | 10.8 ± 13.2 | 0.5+ (0.3–1.1) | 0.9+ (0.9–0.9) |
| Interaction terms | |||||
| Closeness x Friend | – | – | – | – | 1.3 (0.9–1.9) |
| Closeness x Family | – | – | – | – | 1.9* (1.1–3.4) |
| Closeness x Main Partner | – | – | – | – | 1.2 (0.8–1.9) |
| Closeness x Casual Partner | – | – | – | – | 1.0 (0.6–1.7) |
| Closeness x Transactional sex client | – | – | – | – | 1.7* (1.1–2.8) |
| Closeness x Drug Buddy | – | – | – | – | 1.1 (0.6–1.9) |
| Closeness x Friend | – | – | – | – | 1.3 (0.9–1.9) |
p < 0.10
p < 0.05
p < 0.01
Predicting Willingness to Diffuse PrEP Information within Dyads
WWID were willing to share PrEP information with 83% (m = 312) of alters (Table 2). WWID had increased odds of willingness to share PrEP information with alters who were homeless (UOR 3.3, 95% CI 1.5–7.6), injection drug users (UOR 2.3, 95% CI 1.1–4.7), engaged in transactional sex (UOR 4.5, 95% CI 1.6–12.5), and those perceived to be at high risk for HIV (UOR 1.1, 95% CI 1.1–1.2). Related to interpersonal attributes, participants had increased odds of willingness to share PrEP information with alters of the same gender (UOR 5.8, 95% CI 2.5–13.6) and lower odds of willingness to share PrEP information as the relationship length increased (UOR 0.5, 95% CI 0.3–1.1).
In the multivariable model (Table 2), participants had significantly higher odds of willingness to share PrEP information with alters who were of the same gender (adjusted odds ratio [AOR] 3.7; 95% CI 1.2–11.6), homeless (AOR 2.8; 95% CI 1.0–7.5), and those perceived to be at risk for HIV (AOR 4.2; 95% CI 1.6–11.1). As the relationship length with the alter increased, participants had decreased odds of being willing to share PrEP information (AOR 0.9; 95% CI 0.9–0.9). Given the previous literature [31], we tested the hypothesis that increasing levels of emotional closeness may heighten willingness within different relationship types via an interaction term. The interaction term was positive and significant for closeness among family members (AOR 1.9; 95% CI 1.1–3.4) and closeness among transactional sex clients (AOR 1.7; 95% CI 1.1–2.8; see Fig. 1 for an interaction plot of results). Among family members and transactional sex clients, decreasing emotional closeness was associated with lower odds of willingness to share PrEP information, and stronger emotional closeness was associated with higher odds of willingness to share PrEP information.
Fig. 1.
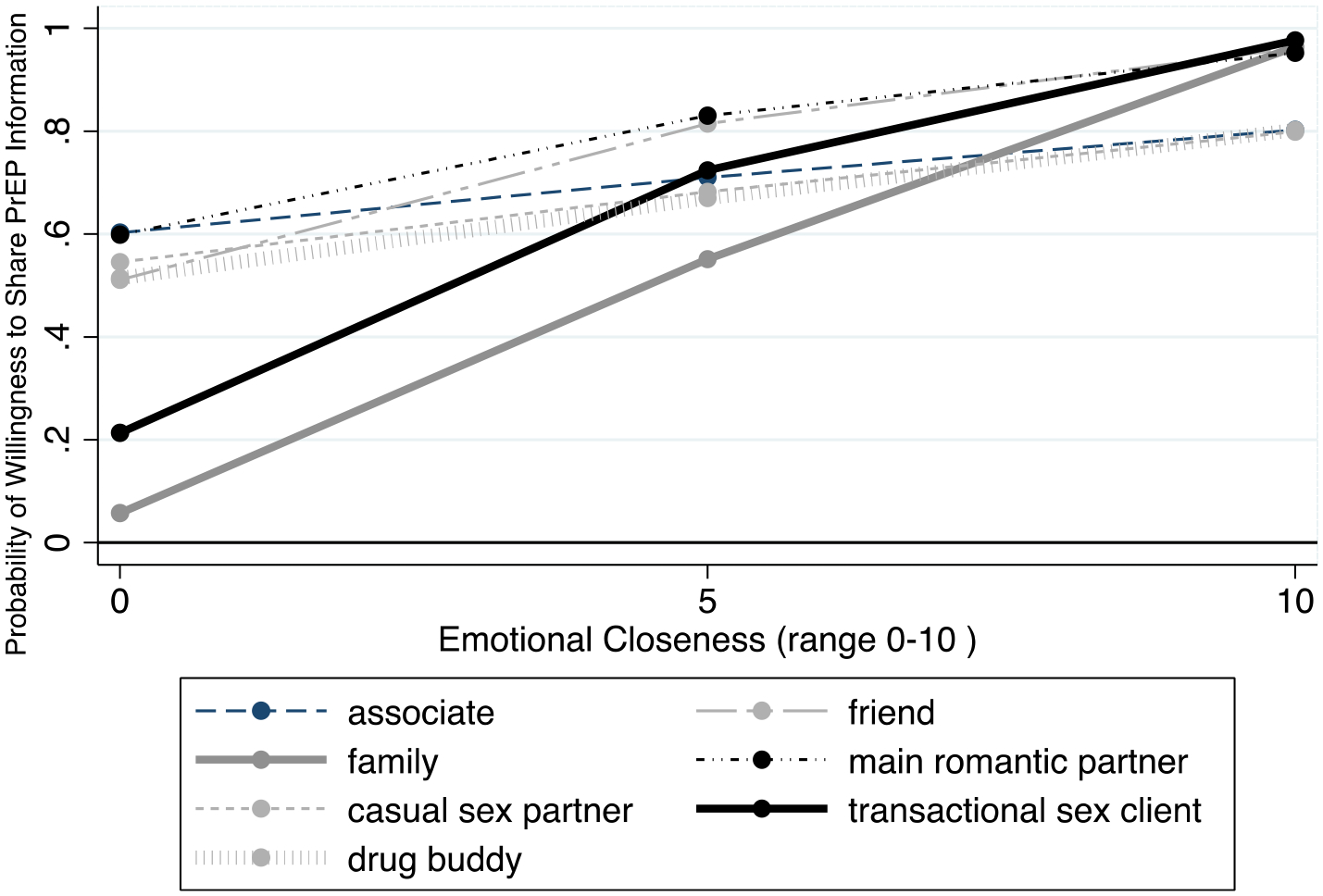
Interaction of emotional closeness and relationship type
Discussion
This study found that interpersonal characteristics such as similarities, social relations, and interactions were important predictors of willingness to share PrEP information within dyads. Additionally, emotional closeness increased odds of willingness to share PrEP information among transactional sex clients and family members, but not other relationship types. Taken together, findings support our primary hypothesis and partially support our secondary hypotheses. This analysis provides insight into the types of relationships with whom WWID may share PrEP information in the context of a peer intervention. Findings should be used to guide the design and evaluation of a peer intervention to educate WWID about PrEP, which has been sorely lacking to date.
In this study, we measured a variety of interpersonal factors to identify their associations with willingness to share PrEP information. We found that half of alters elicited were perceived to be at risk for HIV, and perceiving a network member to be at risk for HIV was associated with increased odds of willingness to share PrEP information. Thus, a peer intervention where WWID share PrEP information with peers may be an effective strategy to increase awareness of PrEP among network members perceived to be at risk for HIV. More information about how WWID appraise risk of network members is needed to ensure people at objective risk for HIV are receiving the intervention information. This is important because studies show that risk perceptions are complex, and shaped by variables such as race [39], gender [40], and the context of relationships with sexual partners [41, 42], and not necessarily by objective assessments of engaging in risk behaviours. Given that HIV perceptions are salient for sharing PrEP information, future research should examine how WWID decide which network members may be at risk for HIV.
This study also found a significant interaction between being a transactional sex client or family member, and emotional closeness, on willingness to share PrEP information. However, the interaction was not significant for other relationship types. One possible explanation for why emotional closeness matters in these two relationships in particular is that ‘transactional sex client’ and ‘family’ may encompass the widest range of emotional closeness while the other types have less variability of emotional closeness. For example, Robertson et al. (2014) report that among women who engage in transactional sex in Tijuana, Mexico, transactional sex clients embody multiple, fluid types of relationships, ranging from a one-time nonregular client to long-term financial providers, and that as commercial relationships develop, social and emotional connections also increase [43]. In the present analysis, it is possible that sex clients with whom participants are not emotionally close are nonregular clients and discussing PrEP within the context of these relationships could be harmful [44, 45]. Sex clients with whom participants are emotionally close may be long-term financial providers with whom they feel safe to discuss PrEP. This same pattern of safety within relationships may also be relevant to family members. This finding is important because if only the main effect of relationship type was examined, the relational dynamics underlying PrEP information sharing would be missed, and it would likely be deduced that alters who are transactional sex clients and family members would most likely not receive PrEP information in a peer intervention.
Multiple dimensions of homophily were positively associated with willingness to share PrEP information within dyads. At the bivariate level, homophily of gender, injection drug use, and transactional sex were positively associated with willingness to share PrEP information. These finding are consistent with other studies that demonstrate the importance of homophily within relationships for sharing and receiving information [46]. Rogers (1995) explains that interpersonal similarity breeds both more communication and more effective communication [46]. Additionally receiving health information from a similar peer may result in a more positive attitude toward the information [46]. When adjusting for other factors, gender homophily is the only statistically significant homophily variable. The implications for peer-delivered PrEP interventions is that encouraging women to share information with other women may be effective at increasing PrEP awareness in this population.
The results of this study should be interpreted within the context of study limitations. The sample was not randomly selected and may not be generalizable to the broader population of WWID. In particular, it is possible that our study included more social and extroverted WWID who were willing to talk about PrEP because participants were selected if they were willing to speak with a network member about PrEP. It also needs to be highlighted that the interview guide asked participants to describe their willingness to share PrEP information in the context of an intervention where they would be trained and paid to share PrEP information. Thus, the willingness scenario is premised on participants getting paid and trained to share information. Lastly, we measured participants’ “willingness” to share PrEP information with network members, which we acknowledge does not necessarily translate into future behaviour. However, we are primarily interested in knowing hypothetically with whom WWID are amenable to sharing PrEP information in the context of an intervention, and never expected participants to actually share information. Despite limitations, results suggest that HIV prevention efforts that tap into existing social networks among WWID to share PrEP information could be a viable way to increase PrEP awareness among vulnerable peers.
Conclusions
WWID interact with social network members who engage in a variety of behaviours that elevate their HIV risk, and WWID are willing to share PrEP information with the majority of people in their social network. Important dyadic characteristics such as gender homophily, relationship type and emotional closeness, are positively associated with willingness to share PrEP information. An important next step is to pilot and evaluate the effectiveness of a peer intervention where WWID share PrEP information with peers.
Funding
This work was supported by NIDA under Grant Award R21DA043417-02 and NIH / NICHD Grant Award R25HD079352 to Duke University.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. The Lancet Global Health. 2017;5(12):e1192–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV surveillance report; vol. 27. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. Published Nov. 2016. Accessed 5 Jan 2017. [Google Scholar]
- 3.HIV and the Opioid Epideic: 5 Key Points [press release]. Henry J Kaiser Family Foundation, March 27, 2018 2018. [Google Scholar]
- 4.CDC joins Department of Public Health in investigating HIV cluster among people who inject drugs [press release]. mass.gov, 04/05/2018 2018.
- 5.DeMio T CDC called in to investigate HIV surges in the Cincinnati region. The Enquirer. 2018. [Google Scholar]
- 6.Archibald A HIV outbreak among homeless people worries health officials. Real Change. 2018. [Google Scholar]
- 7.Worth D Sexual decision-making and AIDS: why condom promotion among vulnerable women is likely to fail. Stud Fam Plann. 1989;20(6):297–307. [PubMed] [Google Scholar]
- 8.El-Bassel N, Shaw SA, Dasgupta A, Strathdee SA. People Who Inject Drugs in Intimate Relationships: It Takes Two to Combat HIV. Current Hiv/Aids Reports. 2014;11(1):45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choopanya K, Martin M, Suntharasamai P. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet. 2013;381. [DOI] [PubMed] [Google Scholar]
- 10.Stein M, Thurmond P, Bailey G. Willingness to use HIV pre-exposure prophylaxis among opiate users. AIDS Behav. 2014;18(9):1694–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shrestha R, Karki P, Altice FL. Correlates of willingness to initiate pre-exposure prophylaxis and anticipation of practicing safer drug-and sex-related behaviors among high-risk drug users on methadone treatment. Drug Alcohol Depend. 2017;173:107–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuo I, Olsen H, Patrick R, Phillips G 2nd, Magnus M, Opoku J, et al. Willingness to use HIV pre-exposure prophylaxis among community-recruited, older people who inject drugs in Washington. DC Drug Alcohol Depend. 2016;164:8–13. [DOI] [PubMed] [Google Scholar]
- 13.Kuo I, Gregory Phillips I, Magnus M, Opoku J, Rawls A, Peterson J, et al. Willingness to use pre-exposure prophylaxis among community-recruited injection drug users. Race/Ethnicity. 2014;50(228):82–7. [Google Scholar]
- 14.Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduction Journal. 2017;14(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherman SG, Schneider KE, Park JN, Allen ST, Hunt D, Chaulk CP, et al. PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore. Maryland Drug and alcohol dependence. 2019;195:148–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edelman EJ, Moore BA, Calabrese SK, Berkenblit G, Cunningham C, Patel V, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams LM, Balderson BH. HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: a short report. AIDS care. 2016;28(9):1154–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neale J, Tompkins C, Sheard L. Barriers to accessing generic health and social care services: a qualitative study of injecting drug users. Health Soc Care Community. 2008;16(2):147–54. [DOI] [PubMed] [Google Scholar]
- 19.Theall KP, Sterk CE, Elifson KW, Kidder D. Factors associated with positive HIV serostatus among women who use drugs: continued evidence for expanding factors of influence. Public Health Rep. 2003;118(5):415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into Action study: a peer-based, personal risk network focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction (Abingdon, England). 2011;106(2):366–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Latkin CA. Outreach in natural settings: the use of peer leaders for HIV prevention among injecting drug users’ networks. Public Health Rep. 1998;113(Suppl 1):151. [PMC free article] [PubMed] [Google Scholar]
- 22.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22(4):332–9. [DOI] [PubMed] [Google Scholar]
- 23.Garfein RS, Golub ET, Greenberg AE, Hagan H, Hanson DL, Hudson SM, et al. A peer-education intervention to reduce injection risk behaviors for HIV and hepatitis C virus infection in young injection drug users. Aids. 2007;21(14):1923–32. [DOI] [PubMed] [Google Scholar]
- 24.Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, et al. The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. Soc Sci Med. 2009;68(4):740–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mutchler MG, McDavitt B, Ghani MA, Nogg K, Winder TJA, Soto JK. Getting PrEPared for HIV prevention navigation: young black gay men Talk About HIV prevention in the biomedical era. AIDS patient care and STDs. 2015;29(9):490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly JA, Amirkhanian YA, Walsh JL, Brown KD, Quinn KG, Petroll AE, et al. Social network intervention to increase pre-exposure prophylaxis (PrEP) awareness, interest, and use among African American men who have sex with men. AIDS care. 2020;32(sup2):40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dickson-Gomez J, Weeks M, Martinez M, Convey M. Times and places: process evaluation of a peer-Led HIV prevention intervention. Subst Use Misuse. 2006;41(5):669–90. [DOI] [PubMed] [Google Scholar]
- 28.Weeks MR, Li J, Dickson-Gomez J, Convey M, Martinez M, Radda K, et al. Outcomes of a peer HIV prevention program with injection drug and crack users: The risk avoidance partnership. Subst Use Misuse. 2009;44(2):253–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borgatti SP, Mehra A, Brass DJ, Labianca G. Network analysis in the social sciences. Science. 2009;323(5916):892–5. [DOI] [PubMed] [Google Scholar]
- 30.Borgatti SP, Cross R. A relational view of information seeking and learning in social networks. Manage Sci. 2003;49(4):432–45. [Google Scholar]
- 31.Roberts SG, Dunbar RI. Communication in social networks: Effects of kinship, network size, and emotional closeness. Personal Relationships. 2011;18(3):439–52. [Google Scholar]
- 32.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: Homophily in social networks. Ann Rev Sociol. 2001;27(1):415–44. [Google Scholar]
- 33.Hampanda KM, Rael CT. HIV status disclosure among postpartum women in Zambia with varied intimate partner violence experiences. AIDS Behav. 2018;22(5):1652–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Pre-exposure Prophylaxis for the Prevention of HIV Infection in the United States, 2014 Clinical Practice Guideline Atlanta: Centers for Disease Control and Prevention; 2014. [Available from: http://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf. [Google Scholar]
- 35.Ennett ST, Bailey SL, Federman EB. Social network characteristics associated with risky behaviors among runaway and homeless youth. Journal of health and social behavior. 1999:63–78. [PubMed] [Google Scholar]
- 36.StataCorp. Stata Statistical Software: Release 14. 14 ed. College Station, TX: StataCorp; 2014. [Google Scholar]
- 37.Rabe-Hesketh S, Skrondal A. Multilevel and longitudinal modeling using Stata: STATA press; 2008. [Google Scholar]
- 38.Zhang Z Model building strategy for logistic regression: purposeful selection. Annals of translational medicine. 2016;4(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klein H, Elifson KW, Sterk CE. “At risk” women who think that they have no chance of getting HIV: self-assessed perceived risks. Women Health. 2003;38(2):47–63. [DOI] [PubMed] [Google Scholar]
- 40.Theall KP, Elifson KW, Sterk CE, Klein H. Perceived susceptibility to HIV among women: Differences according to age. Research on Aging. 2003;25(4):405–32. [Google Scholar]
- 41.Mehrotra P, Noar SM, Zimmerman RS, Palmgreen P. Demographic and personality factors as predictors of HIV/STD partner-specific risk perceptions: implications for interventions. AIDS Educ Prev. 2009;21(1):39–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koku E, Felsher M. The Effect of Social Networks and Social Constructions on HIV Risk Perceptions. AIDS Behav. 2020;24(1):206–21. [DOI] [PubMed] [Google Scholar]
- 43.Robertson AM, Syvertsen JL, Amaro H, Martinez G, Rangel MG, Patterson TL, et al. Can’t buy my love: a typology of female sex workers’ commercial relationships in the Mexico-US Border Region. Journal of Sex Research. 2014;51(6):711–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ghimire L, Smith WCS, van Teijlingen ER, Dahal R, Luitel NP. Reasons for non-use of condoms and self-efficacy among female sex workers: a qualitative study in Nepal. BMC women’s health. 2011;11(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Okal J, Chersich MF, Tsui S, Sutherland E, Temmerman M, Luchters S. Sexual and physical violence against female sex workers in Kenya: a qualitative enquiry. AIDS Care. 2011;23(5):612–8. [DOI] [PubMed] [Google Scholar]
- 46.Rogers Everett M Diffusion of innovations. New York. 1995;12. [Google Scholar]


