Abstract
Serum neurofilament light chains (sNfL) are biomarkers of disease activity in multiple sclerosis (MS), but their value to predict response to treatment, and their association with patient immunological profile, need to be further explored. We studied 80 relapsing–remitting MS patients initiating dimethyl fumarate (DMF) treatment. sNfL levels were explored at baseline and at 3, 6 and 12 months by single molecule array. Blood lymphocyte subsets were measured at baseline and at 6 months by flow cytometry. Patients were followed a year and classified as NEDA (no evidence of disease activity) or ODA (ongoing disease activity). NEDA patients had lower sNfL levels at baseline (p = 0.0001), and after three (p = 0.004) and six (p = 0.03) months of DMF treatment. Consequently, low baseline sNfL values (≤ 12 pg/ml) increased the probability of NEDA (OR 5.8; CI 1.82–15.6; p = 0.002, after correcting by disease activity in the previous year), and associated with significant reductions of central memory CD4+ T lymphocytes, interferon-gamma+ CD8+ T lymphocytes, Natural Killer T cells, and memory B cells upon DMF treatment, being the highest differences in memory B cells (p < 0.0001). This shows that low baseline sNfL values identify MS patients with higher probability of optimal response to DMF and of a reduction in effector immune cells.
Subject terms: Immunology, Autoimmunity, Immunological disorders, Lymphocytes, Neuroimmunology, Translational immunology, Neuroscience, Diseases of the nervous system, Molecular neuroscience, Neuroimmunology, Neurology, Multiple sclerosis
Introduction
Dimethyl fumarate (DMF; Biogen, Cambridge, MA), is an approved treatment for relapsing remitting multiple sclerosis (RRMS). DMF demonstrated efficacy in ameliorating disease course in RRMS patients in two large 2-year double-blind, multinational, phase III trials, DEFINE1 and CONFIRM2 and their dose-blind extension, ENDORSE3,4. Optimal responders to this drug show a shift from an inflammatory to a tolerogenic blood cell profile5. Serum neurofilament light chains (sNfL) are biomarkers of inflammation and axonal damage in MS, and several studies support their role as biomarkers of treatment response6–11. Results from a prospective open label phase IV trial TREMEND showed that DMF was effective in reducing NfL concentration in CSF, plasma and serum of treatment-naïve RRMS patients and that NfL levels in the CSF at 12 months of DMF treatment associated with disease activity12. In another study performed in naïve and previously treated RRMS patients, the ability of DMF in decreasing sNfL levels was similar to that of Teriflunomide but relatively lower than high efficacy drugs as Fingolimod, Natalizumab or Alemtuzumab, and was highly dependent on baseline sNfL levels13.
The aim of this work was to study sNfL changes during DMF treatment and to explore if they could be early predictors of treatment response in MS.
Results
DMF treatment decreased sNfL values in RRMS patients
We included 80 RRMS patients (76% females) who initiated consecutively treatment with DMF in this prospective longitudinal study. Baseline clinical and demographic characteristics are shown in Table 1. Patient age was 41.5 (33.6–47.3) years (median, IQR), disease duration was 9.5 (4.4–16.3) years and EDSS was 1.5 (1.5–2.5). Fifty five patients (68.7%) received previous disease modifying treatments.
Table 1.
Baseline clinical and demographic data of patients included in the study.
| Variable | (n = 80) |
|---|---|
| Age (years). Median (IQR) | 41.5 (33.6–47.3) |
| Disease duration (years). Median (IQR) | 9.5 (4.4–16.3) |
| Sex (Male/female) | 19/61 |
| EDSS score. Median (IQR) | 1.5 (1.5–2.5) |
| MSSS score. Median (IQR) | 2.2 (1.3–4.2) |
| N. of total previous relapses. Median (IQR) | 4 (2–6) |
| N. of patients with relapses in the previous year (Yes/no) | 50/30 |
| N. of relapses in the previous year. Median (IQR) | 1 (0–1) |
| Time from the last relapse (months). Median (IQR) | 6.0 (3.0–9.2) |
| N. of patients with relapses in the previous 3 months (Yes/no) | 16/64 |
| N. of T2 lesions. Median (IQR) | 19 (12–27) |
| N. of patients with Gd+ enhanced lesions (Yes/no) | 24/56 |
| N. of Gd+ enhanced lesions. Median (IQR) | 0 (0–1) |
| Previous treatments (Naïve/Previously treated) | 25/55 |
| Previous treatments (FL/SL) | 45/10 |
| Washout period (months). Median (IQR) | 2 (2–4) |
EDSS Expanded Disability Status Scale, Gd gadolinium, FL first line drugs, IQR interquartile range, MSSS Multiple Sclerosis Severity Score, N. number, SL second line drugs.
Median (IQR) baseline sNfL concentration was 10.1 (6.3–15.6) pg/ml. We observed a clear decline in sNfL values during the first year of DMF treatment (Fig. 1). It became evident at 3 months (median decrease from baseline: 4.0 pg/ml; CI 2.4–5.6; p < 0.0001), being less pronounced from 3 to 12 months of treatment, when median sNfL decrease from baseline was 6.7 pg/ml (CI 5.5–8.3; p < 0.0001).
Figure 1.
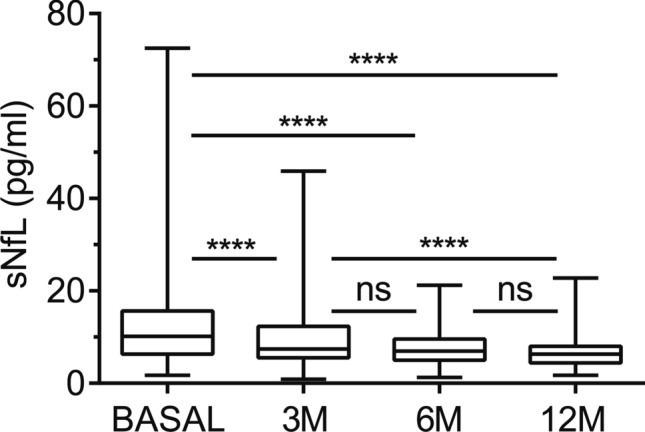
Serum neurofilament light chain (sNfL) levels in relapsing–remitting multiple sclerosis (RRMS) patients. sNfL concentration (median, IQR) obtained in 80 RRMS patients at baseline (Basal) and 3, 6, and 12 months (M) after dimethyl fumarate initiation. ****p < 0.0001; ns not significant.
To investigate the influence of disease activity at baseline in sNfL decrease, we classified patients according to baseline disease activity as “Active Disease” (AD, n = 30) or “No Active Disease” (NAD, n = 50). AD patients were defined as those showing Gd+ enhancing lesions in the basal MRI or having relapses in the previous three months to treatment initiation. AD patients had a modest increase in sNfL levels at baseline compared to NAD ones (p = 0.04), and this difference was lost after three months of DMF treatment. In addition, both groups of patients experienced a clear decrease in sNfL values during the first year of treatment, independently of previous disease activity (p < 0.0001 in both cases).
Association of sNfL values with response to DMF
We first explored baseline clinical and demographic differences between patients achieving NEDA (n = 50, 62.5%) or ODA (n = 30, 37.5%) status at 12 months of DMF treatment. As shown in Table 2, NEDA patients had lower numbers of Gd+ enhancing lesions (p = 0.006). Likewise, we observed a moderate decrease in the proportion of patients showing Gd+ enhancing lesions at baseline in the same group (p = 0.02). No differences were found in other clinical, demographic or radiological variables.
Table 2.
Baseline clinical and demographic data of NEDA and ODA patients.
| Variable | NEDA (n = 50) | ODA (n = 30) | p |
|---|---|---|---|
| Age (years) | 42.2 (36.3–47.8) | 38.2 (28.3–46.5) | ns |
| Disease duration (years). Median (IQR) | 9.9 (5.9–16.7) | 7.7 (2.2–13.3) | ns |
| Sex (male/female) | 13/37 | 6/24 | ns |
| EDSS score. Median (IQR) | 1.5 (1.5–2.5) | 1.5 (1.5–3.0) | ns |
| MSSS score. Median (IQR) | 2.1 (1.2–4.5) | 2.4 (1.8–3.3) | ns |
| N. of previous relapses. Median (IQR) | 4 (2–5) | 4 (2–7) | ns |
| Patients with relapses in the previous year (Yes/No) | 28/22 | 22/8 | ns |
| N. of relapses in the previous year. Median (IQR) | 1 (0–1) | 1 (0–1) | ns |
| Time from the last relapse (months). Median (IQR) | 6.0 (3.0–9.7) | 4.5 (3.0–9.5) | ns |
| Patients with relapses in the previous 3 months (Yes/No) | 8/42 | 8/22 | ns |
| N. of T2 lesions. Median (IQR) | 18 (11–26) | 19 (11–37) | ns |
| Patients with Gd + enhancing lesions (Yes/No) | 10/40 | 14/16 | 0.02 |
| N. of Gd+ enhancing lesions. Median (IQR) | 0 (0–0) | 0 (0––2) | 0.006 |
| Treatment naïve/ Previously treated | 17/33 | 8/22 | ns |
| Previous treatments (FL/SL) | 25/8 | 20/2 | ns |
| Wash-out period (months). Median (IQR) | 2 (2–4) | 3.0 (1.7–5.5) | ns |
EDSS Expanded Disability Status Scale, Gd Gadolinium, FL first line drugs, IQR interquartile range, NEDA no evidence of disease activity, MSSS Multiple Sclerosis Severity Score, N. number, NS NOT significant, ODA ongoing disease activity, SL second line drugs.
We further explored differences in baseline, 3, 6 and 12-months sNfL values between patients achieving NEDA or ODA status at 1 year of treatment. NEDA and ODA patients experienced a gradual decrease in sNfL values during the first year of DMF treatment (p < 0.0001 in both cases). However, sNfL stabilization occurred at three months of DMF treatment in NEDA patients, while it took 12 months in ODA ones (Fig. 2a). In addition, NEDA patients had lower sNfL levels at baseline (Median [IQR]: 8.8 [5.8–12.4] vs 14.5 [8.7–23.7] pg/ml; p = 0.0001), and at three (6.5 [4.9–10.9] vs 10.2 [7.1–13.1] pg/ml; p = 0.004) and six months (6.5 [4.4–8.9] vs 8.3 [5.8–11.8] pg/ml; p = 0.03) of DMF treatment than ODA ones, although differences were lost after 12 months (5.3 [4.4–7.7] vs 6.8 [5.3–8.5] pg/ml; p = 0.150) (Fig. 2b).
Figure 2.
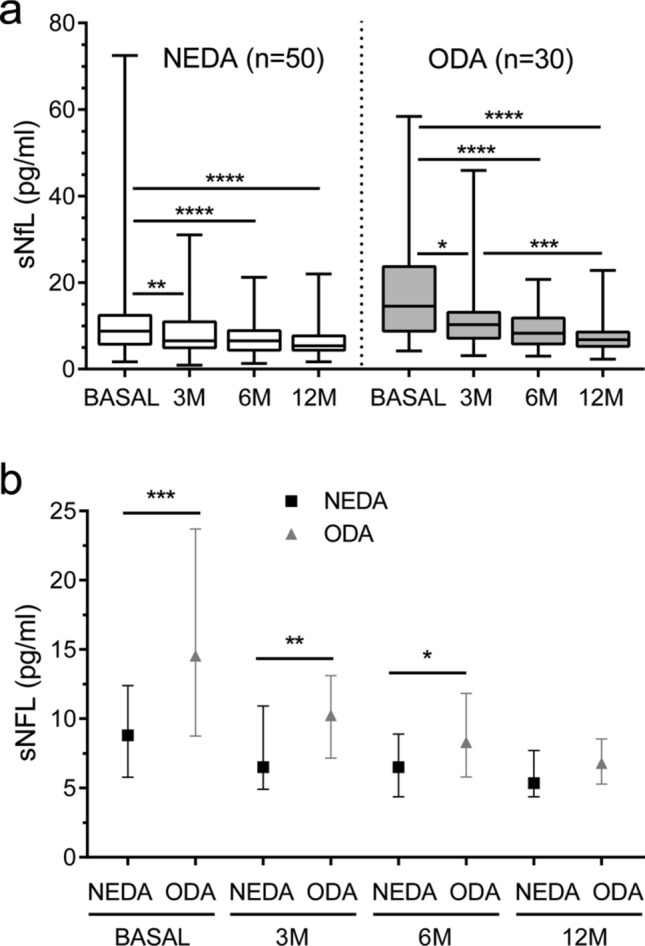
Serum neurofilament light chain (sNfL) values in NEDA and ODA patients. (a) sNfL levels (median, IQR) of NEDA (white rectangle; n = 50) and ODA (grey rectangle; n = 30) relapsing–remitting multiple sclerosis patients at baseline (basal) and at 3, 6, and 12 months (M) of dimethyl fumarate treatment initiation. (b) Differences in sNfL values (median, IQR) between NEDA (black square) and ODA (grey triangle) patients at each time point. Only p values below 0.05 are shown. *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. NEDA no evidence of disease activity, ODA ongoing disease activity.
We next studied if baseline and 3-months sNfL values could predict response to DMF treatment. Using ROC curves, we established a cut-off value of 12.0 pg/ml for baseline sNfL levels (AUC: 0.75; CI 0.63–0.86; p = 0.0002). As shown in Fig. 3a, patients showing baseline sNfL below 12 pg/ml had increased probability to achieve NEDA status at 12 months (OR 6.6; CI 2.4–18.1; p = 0.0002). After performing a multivariate analysis and adjusting results by presence of baseline Gd+ enhancing lesions, number of Gd+ enhancing lesions and of NEDA status in the previous year, we found that sNfL ≤ 12 pg/ml at baseline maintained its ability in predicting NEDA at 12 months (OR 5.8; CI 1.8–15.6; p = 0.002).
Figure 3.

Serum neurofilament light chain (sNfL) values identify optimal responders to dimethyl fumarate (DMF) treatment. Number (N.) of relapsing–remitting multiple sclerosis patients achieving NEDA (white rectangle) or ODA (grey rectangle) status after 12 months of DMF treatment, depending on their baseline (basal) sNfL (a) or their 3-months (M) sNfL levels (b). CI 95% confidence interval, NEDA no evidence of disease activity, ODA ongoing disease activity, OR odds ratio.
ROC curves also let us to establish a cut-off value of sNfL values of 7 pg/ml at three months of DMF treatment (AUC: 0.69; CI 0.57–0.81; p = 0.004). Figure 3b shows that patients with sNfL below 7 pg/ml at three months showed higher probability of being NEDA at 12 months (OR 4.9; 1.8–13.6; p = 0.002). Adjusting by presence and number of baseline Gd+ enhancing lesions and by NEDA status in the previous year, the OR obtained was 4.8 (CI 1.6–14.2; p = 0.005).
Association between sNfL values and changes in blood leukocyte subsets
Since sNFL values below 12 pg/ml at baseline associated with NEDA status after a year of treatment, we aimed to further investigate if this cut-off value could also identify changes in any leukocyte subset. Thus, we explored changes in blood leukocyte populations after six months of DMF treatment in 62 RRMS patients with available peripheral blood mononuclear cells (PBMCs) samples, showing low (≤ 12 pg/ml, n = 36) or high (> 12 pg/ml, n = 26) baseline sNfL values. Both groups of patients showed significant decreases in effector memory CD4+ and CD8+ T lymphocytes, total and terminally differentiated CD8+ T lymphocytes, TNF-alpha+ CD8+ T lymphocytes and CD4+ T cells producing IFN-gamma. Results are shown in Supplementary Fig. S1. Remarkably, only patients with sNfL ≤ 12 pg/ml at baseline showed a decrease in the percentages of blood central memory CD4+ T lymphocytes (p = 0.02), memory B cells (p < 0.0001), Natural Killer T cells (p = 0.02) and CD8+ T lymphocytes producing IFN-gamma (p < 0.0001) after six months of DMF treatment (Fig. 4). No differences were observed after six months of DMF treatment in the remaining populations studied (Supplementary Fig. S1 and S2).
Figure 4.
Blood cell subsets changes after 6 months of dimethyl fumarate (DMF) treatment depend on basal serum neurofilament light chain (sNfL) values. Percentages of blood Central Memory (CM) CD4+ T lymphocytes, memory B (Bmem) cells, Natural Killer T (NKT) cells, and CD4+ and CD8+ T lymphocytes producing Interferon-gamma (IFN-g) at baseline (0 M) and after six months (6 M) of dimethyl fumarate treatment in 62 relapsing–remitting multiple sclerosis patients showing baseline sNfL values ≤ 12 (n = 36, a) or > 12 (n = 26, b) pg/ml. Percentages are referred to total peripheral blood mononuclear cells (PBMCs). Medians and Interquartile Ranges are shown. ns: not significant. p values are corrected by Bonferroni test. *p < 0.05; **p < 0.01; ****p < 0.0001.
Discussion
DMF has been shown to be an effective drug in the treatment of RRMS patients with intermediate disease activity14. However, some patients show a suboptimal response and need to escalate to a second-line therapy. Thus, it is highly important the early identification of optimal responders to DMF treatment, to avoid potential relapses or disability progression in suboptimal responders. Using ultra sensible SIMOA technique, we quantified sNfL values of 80 RRMS patients initiating DMF and at 3, 6 and 12 months of treatment, and studied their association with treatment response. Baseline sNfL results obtained in our cohort were similar to those reported in other series12,13. We explored differences between NEDA and ODA patients and found that the first group had lower sNfL values at baseline. These values allowed us to identify patients with high probability of being optimal responders 1 year after DMF treatment initiation. This is highly relevant, as achieving NEDA status after the first year of treatment associates with a high probability of remaining free of progression for longer periods15. sNfL values strongly associated with the presence of Gd+ enhancing lesions and are ultimately related to acute inflammation in MS6,16–18. Likewise, a higher proportion of ODA patients showed Gd+ enhancing lesions in baseline MRI in our cohort. However, differences were clearer when studying sNfL values at this time point. In consequence, they might be more accurate and accessible biomarkers compared to radiological variables for predicting treatment response in patients with moderate disease course, who have only limited radiological activity. To further explore the influence of previous disease activity in our results, we analyzed our data by logistic regression, correcting by the number of baseline Gd+ enhancing lesions and by NEDA status in the previous year of treatment initiation. We found that, although disease activity had an influence on baseline sNfL values, the ability of baseline sNfL values for identifying optimal responders to DMF treatment remained significant. Baseline sNfL levels also predicted the outcome of Fingolimod treatment11, which reinforces their value as a tool for personalized treatment in MS.
As described in various cohorts of MS patients treated with different disease modifying drugs12,13, we found that sNfL levels decreased during DMF treatment. The reduction did not depend on age, sex, previous treatments or disease duration and occurred in both NEDA and ODA patients, thus showing that sNFL decrease does not necessarily associate with an optimal response to the drug. However, reaching sNfL levels below 7 pg/ml after three months of DMF treatment allowed us to identify NEDA patients. These results suggest that early normalization of sNfL values are related with an optimal response. Thus, it is important to establish accurate reference values showing good inter-laboratory reproducibility. In this line, the use of the SIMOA platform gave excellent correlation across different laboratories19. The development of new highly sensitive platforms will represent a challenge to maintain sNFL standardization in the next future20.
We found that all patients experienced changes in their immunological profile at some degree after six months of DMF treatment. However, baseline sNfL values lower than 12 pg/ml implied deeper changes including significant decreases in some effector and memory populations previously associated with NEDA status5,21–23. This strongly suggests that these baseline sNfL values identify MS patients capable of modifying their abnormal immune response during DMF treatment and thus, with high probability of achieving an optimal response to the drug.
Although this data should be confirmed in multi-center studies, our results show that sNfL levels in MS patients are excellent biomarkers to early identify optimal responders to DMF.
Patients and methods
Patients
Eighty RRMS patients who initiated DMF treatment at the MS Unit of Ramon y Cajal University Hospital (Madrid, Spain) were consecutively included in the study.
Washout periods of at least one or two months were established for patients previously treated with first or second line drugs respectively.
Patient follow-up
Patients were monitored at least every three months, with extra visits in case of relapses. Demographical, clinical and radiological variables recorded at baseline were listed in Table 1. In the follow-up visit after 12 months, patients were classified as follows: optimal responders, if they showed no evidence of disease activity (NEDA) in terms of absence of relapses, progression in the EDSS score or MRI activity, or suboptimal responders, if they showed evidence of ongoing disease activity (ODA). ODA status was defined by the presence of at least a relapse, or confirmed disability progression (CDP) measured with the EDSS score24, or new T2 or Gd+ enhancing lesions at 1 year MRI.
Essential requirements of MRI used in this work
A MRI of the brain was essentially performed as described previously5 with the only difference being that slices of 3 mm thickness without gap between slices were acquired in the current study.
Samples
Serum samples at baseline (immediately before), 3, 6 and 12 months after DMF treatment initiation were obtained from every patient and stored at -80ºC until used. Heparinized blood samples at baseline and at 6 months were also collected. PBMCs were obtained and cryopreserved as previously described5.
sNfL detection
NfL values were quantified in 25 µl duplicate serum samples obtained from every patient by single molecule array (SIMOA) technique in a SR-X instrument (Quanterix, MA, USA), following manufacturer instructions. Baseline, 3, 6 and 12 months samples were assayed simultaneously to avoid inter-assay variability.
Flow cytometry
Monoclonal antibodies used in this study are listed in Table 3. Extracellular protein labelling, PBMC stimulation and staining for intracellular cytokine detection was performed as described previously5. After antigen staining, scattered light properties and fluorescent emission by PBMCs were evaluated in a FACSCanto II flow cytometer (BD Biosciences). For establishing cut-off values of PBMC autoflorescence, isotype controls were employed. PBMCs subsets were identified by using FACSDiva Software V.8.0 (BD Biosciences) as previously reported5. At least 5 × 104 events were analyzed. We used non-stimulated PBMCs as a control of basal intracellular cytokine production.
Table 3.
Monoclonal antibodies (MoAb) used in the study.
| MoAb | Manufacturer |
|---|---|
| CD8-FITC | Becton Dickinson |
| CD27-FITC | Becton Dickinson |
| IFN-gamma-FITC | Becton Dickinson |
| CD24-PE | Becton Dickinson |
| CD197(CCR7)-PE | Becton Dickinson |
| GM-CSF-PE | Becton Dickinson |
| IL-10-PE | Biolegend |
| CD3-PerCP | Becton Dickinson |
| CD38-PE-Cy5.5 | Becton Dickinson |
| TNF-alpha-PerCP-Cy5.5 | Becton Dickinson |
| CD19-PE-Cy7 | Becton Dickinson |
| CD25-PE-Cy7 | Becton Dickinson |
| CD45RO-APC | Becton Dickinson |
| CD56-APC | Becton Dickinson |
| IL-17-APC | R&D Systems |
| CD4-APC-H7 | Becton Dickinson |
| CD8-APC-H7 | Becton Dickinson |
| CD3-BV421 | Becton Dickinson |
| CD127-BV421 | Becton Dickinson |
| CD45-V500 | Becton Dickinson |
GM-CSF granulocyte/macrophage-colony stimulating factor, IFN interferon, IL interleukin, TNF tumor necrosis factor.
Statistical analysis
We used GraphPad Prism 8.0 software (GraphPad Prism Inc, La Jolla, CA) and Stata 16 software (StataCorp LLC, Lakeway, TX) to perform statistical analyses. Absolute and relative frequencies were used to describe categorical variables, and mean and standard deviation or median and 25th–75th percentile (IQR) to illustrate continuous ones. Two-tailed Mann–Whitney U tests and two-tailed Wilcoxon matched-pair tests were employed to compare two independent groups of patients and to assess differences between baseline and 6 months samples respectively. Two-tailed Fisher's exact tests were used to analyze categorical variables, while Friedman ANOVA tests for paired data were utilized to compare sNfL results along treatment. Generalized Linear Model (GLM) tests were employed for testing interaction with age, sex, previous disease-modifying treatments or disease duration. Multivariate analyses were used for exploring influence of the presence of Gd+ enhancing lesions at baseline MRI study and of the NEDA status in the previous year in the ability of sNfL values for predicting NEDA at 12 months. sNfL cut-off values were established by using ROC curves; basal and 3-month sNfL values rendering the best specificity and sensibility were chosen. 95% confidence intervals were provided. p values were adjusted by using Bonferroni test. p values below 0.05 were assumed to be significant.
Ethics declarations
This study was authorized by Clinical Research Ethics Committee of Ramón y Cajal University Hospital (approval number: 162-19). All experiments were conducted according to the Ramón y Cajal Health Research Institute (IRYCIS) guidelines on good scientific practice and to the Declaration of Helsinki. Every patient signed an informed consent and accepted the publication of the anonymized results before entering the study.
Supplementary Information
Supplementary Information 1.[Replace ESM 2 with the attached "Supplementary_information_reviewed_ESM"].
Acknowledgements
Authors acknowledge MA Fernández de Pablos, AI Pérez Macías and S Ortega for their excellent technical support. The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: this work was supported by Biogen [Grant No. 2019-0365]; Fondo para la Investigación Sanitaria from the Instituto de Salud Carlos III, the Ministerio de Ciencia e Innovación (Spain) and Fondo Europeo de Desarrollo Regional (FEDER) [Grant Nos. PI15/00513, PI18/00572 and RD16/0015/0001].
Author contributions
S.S.M., E.M., L.C.F. and J.M.V. visited M.S. patients and collected samples and clinical data. D.L. performed MRI studies. P.E.W.-D., M.E., J.I.F.V. and S.M. stored blood samples and performed the experiments. E.R.M. and E.R. supervised flow cytometry studies. N.V. wrote the manuscript draft, stored blood samples and performed statistical analyses. A.M. performed and supervised statistical analyses. L.M.V. designed and supervised the study and corrected the manuscript. All authors read and approved the final version of the manuscript.
Data availability
Anonymized data supporting the findings of this study will be shared by reasonable request from any qualified investigator during 3 years after the publication of the study.
Competing interests
LMV, LCF, JMV, EM and SSM, received payment for lecturing, or travel expenses or research grants from Merck-Serono, Biogen, Sanofi-Genzyme, Roche Farma, Bristol-Myers Squibb and Novartis. The remaining authors declare that they have no conflict of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-88624-7.
References
- 1.Gold R, et al. Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N. Engl. J. Med. 2012;367:1098–1107. doi: 10.1056/NEJMoa1114287. [DOI] [PubMed] [Google Scholar]
- 2.Fox RJ, et al. Placebo-controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N. Engl. J. Med. 2012;367:1087–1097. doi: 10.1056/NEJMoa1206328. [DOI] [PubMed] [Google Scholar]
- 3.Gold R, et al. Long-term effects of delayed-release tecfidera in multiple sclerosis: Interim analysis of ENDORSE, a randomized extension study. Mult. Scler. 2017;23:253–265. doi: 10.1177/1352458516649037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gold R, et al. Sustained effect of delayed-release tecfidera in newly diagnosed patients with relapsing–remitting multiple sclerosis: 6-Year interim results from an extension of the DEFINE and CONFIRM studies. Neurol. Ther. 2016;5:45–57. doi: 10.1007/s40120-016-0042-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Medina S, et al. Optimal response to dimethyl fumarate associates in MS with a shift from an inflammatory to a tolerogenic blood cell profile. Mult. Scler. 2018;24:1317–1327. doi: 10.1177/1352458517717088. [DOI] [PubMed] [Google Scholar]
- 6.Disanto G, et al. Swiss Multiple Sclerosis Cohort Study Group Serum Neurofilament light: A biomarker of neuronal damage in multiple sclerosis. Ann. Neurol. 2017;81:857–870. doi: 10.1002/ana.24954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Håkansson I, et al. Neurofilament levels, disease activity and brain volume during follow-up in multiple sclerosis. J. Neuroinflamm. 2018;15:209. doi: 10.1186/s12974-018-1249-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuhle J, et al. Serum neurofilament is associated with progression of brain atrophy and disability in early MS. Neurology. 2017;88:826–831. doi: 10.1212/WNL.0000000000003653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Novakova L, et al. Monitoring disease activity in multiple sclerosis using serum neurofilament light protein. Neurology. 2017;89:2230–2237. doi: 10.1212/WNL.0000000000004683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yaldizli Ö. Value of serum neurofilament light chain levels as a biomarker of suboptimal treatment response in MS clinical practice. ECTRIMS Online Library. 232015 (2018).
- 11.Kuhle J, et al. Blood neurofilament light chain as a biomarker of MS disease activity and treatment response. Neurology. 2019 doi: 10.1212/WNL.0000000000007032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sejbaek T, et al. Dimethyl fumarate decreases neurofilament light chain in CSF and blood of treatment naïve relapsing MS patients. J. Neurol. Neurosurg. Psychiatry. 2019;90:1324–1330. doi: 10.1136/jnnp-2019-321321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delcoigne B, et al. Blood neurofilament light levels segregate treatment effects in multiple sclerosis. Neurology. 2020;94:e1201–e1212. doi: 10.1212/WNL.0000000000009097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ingwersen J, Aktas O, Hartung H-P. Advances in and algorithms for the treatment of relapsing–remitting multiple sclerosis. Neurotherapeutics. 2016;13:47–57. doi: 10.1007/s13311-015-0412-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rotstein DL, et al. Evaluation of no evidence of disease activity in a 7-year longitudinal multiple sclerosis cohort. JAMA Neurol. 2015;72:152–158. doi: 10.1001/jamaneurol.2014.3537. [DOI] [PubMed] [Google Scholar]
- 16.Jakimovski D, et al. Serum neurofilament light chain levels associations with gray matter pathology: a 5-year longitudinal study. Ann. Clin. Transl. Neurol. 2019;6:1757–1770. doi: 10.1002/acn3.50872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siller N, et al. Serum neurofilament light chain is a biomarker of acute and chronic neuronal damage in early multiple sclerosis. Mult. Scler. 2019;25:678–686. doi: 10.1177/1352458518765666. [DOI] [PubMed] [Google Scholar]
- 18.Akgün K, et al. Profiling individual clinical responses by high-frequency serum neurofilament assessment in MS. Neurol. Neuroimmunol. Neuroinflamm. 2019 doi: 10.1212/NXI.0000000000000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gray E, et al. A multi-center study of neurofilament assay reliability and inter-laboratory variability. Amyotroph. Lateral Scler. Frontotemporal Degener. 2020;21:452–458. doi: 10.1080/21678421.2020.1779300. [DOI] [PubMed] [Google Scholar]
- 20.Kapoor R, et al. Serum neurofilament light as a biomarker in progressive multiple sclerosis. Neurology. 2020;95:436–444. doi: 10.1212/WNL.0000000000010346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li R, et al. Dimethyl fumarate treatment mediates an anti-inflammatory shift in B cell subsets of patients with multiple sclerosis. J. Immunol. 2017;198:691–698. doi: 10.4049/jimmunol.1601649. [DOI] [PubMed] [Google Scholar]
- 22.Fleischer V, et al. Treatment response to dimethyl fumarate is characterized by disproportionate CD8+ T cell reduction in MS. Mult. Scler. 2018;24:632–641. doi: 10.1177/1352458517703799. [DOI] [PubMed] [Google Scholar]
- 23.Carlström KE, et al. Therapeutic efficacy of dimethyl fumarate in relapsing–remitting multiple sclerosis associates with ROS pathway in monocytes. Nat. Commun. 2019;10(1):3081. doi: 10.1038/s41467-019-11139-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tur C, et al. Assessing treatment outcomes in multiple sclerosis trials and in the clinical setting. Nat. Rev. Neurol. 2018;14:75–93. doi: 10.1038/nrneurol.2017.171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Information 1.[Replace ESM 2 with the attached "Supplementary_information_reviewed_ESM"].
Data Availability Statement
Anonymized data supporting the findings of this study will be shared by reasonable request from any qualified investigator during 3 years after the publication of the study.



