Abstract
Unmet needs can impede optimal care engagement, impacting the health and well-being of people living with HIV (PLWH); yet, whether unmet needs differ by care engagement status is not well understood. Using surveys and qualitative interviews, we examined and compared unmet needs for PLWH (n = 172) at different levels of care engagement. Unmet needs varied only slightly by care status. Survey findings revealed that provision of housing, emergency financial assistance, employment assistance, and food security were the greatest unmet need; for those in care, housing was the greatest unmet need, whereas for those sporadically in care or out of care, employment assistance was the greatest unmet needs. Qualitative interviews likewise illustrated that a lack of financial resources including insurance, housing, employment, and transportation presented barriers to care engagement across all care groups. Our findings indicate that unmet needs among PLWH are complex and multi-faceted across care engagement status.
Keywords: HIV, Engagement in care, Unmet needs, Continuum of care
Introduction
For persons living with HIV (PLWH), the ability to link to and remain engaged in care plays a crucial factor in improving health outcomes and in preventing HIV transmission to others [1–8]. Even with advances in HIV treatment, a significant portion of PLWH do not consistently receive antiretroviral therapy or achieve viral suppression, often due to poor engagement and retention in care [9]. Recent surveillance data from the United States (US) Centers for Disease Control and Prevention (CDC), for example, indicates that retention in HIV care among PLWH nationally has improved, from 53.6% in 2011 to 57.6% in 2016 [10]; yet, these estimates remain critically below the updated National HIV/AIDS Strategy 2020 goal of at least 90% retention in HIV care among PLWH [11].
Numerous studies have identified barriers and facilitators to optimal care engagement among PLWH, including needs that PLWH have which may hinder retention in care such as mental health and substance use disorders, inadequate health care coverage, unstable housing and homelessness, stigma, discrimination, fear, geographical difficulties accessing care, and a lack of social and structural support [12–21]. Structural and individual-level interventions such as providing comprehensive and easy-to-access services and reducing negative health beliefs about HIV have been shown to enhance engagement and retention in care among PLWH [22, 23]. Such multipronged strategies targeting various stages of the HIV care continuum are key priorities of the US Ending the HIV Epidemic (EHE) initiative, which aims to reduce new HIV infections by 90% in the next ten years [24].
The first phase of the EHE plan focuses on increasing resources to select US regions, including Washington DC (DC), with high concentrations of new HIV infections [24]. DC has long been considered a geographic hotspot for HIV; at its peak in 2007, the rate of new diagnoses was 269 per 100,000 persons, making it one of the US cities with the highest HIV rates [25–27]. Between 2007 and 2018, the HIV diagnosis rate fell to 46.5 diagnoses per 100,000 persons after health officials, local organizations, and academic partners employed a coordinated, multipronged strategy to reduce HIV incidence and improve outcomes for PLWH, including increased engagement in care efforts for newly diagnosed individuals and those out of care [28–30]. For instance, since 2008, the District of Columbia Department of Health (DC DOH) has conducted multiple data to care efforts (locally known as Recapture Blitzes), a set of activities designed to identify and re-engage clients in care after they are lost to follow-up for more than six months [31].
Despite these remarkable achievements in reducing the overall HIV rate in DC, the proportion of PLWH who are retained in care continues to be stalled below the 90% targets, at 80% [28]. Assessing the unmet needs of PLWH is essential to increased awareness of the complex dynamics of the HIV care continuum, particularly in identifying and resolving gaps in engagement and retention in care [32, 33]. Understanding whether unmet needs differ by care engagement status can better inform engagement in care strategies and strengthen HIV programs in high burdened areas such as DC. Few studies have compared unmet needs among PLWH with different levels of care engagement. As part of a larger study to assess facilitators and barriers to care engagement among PLWH in DC [34], through this analysis, we sought to assess whether unmet needs differed among people at various stages of care engagement. We also examined facilitators and barriers to care, HIV status disclosure and social support, and patient-provider relationships among PLWH with different levels of engagement in care.
Methods
Engagement in Care Definitions
Participants’ care statuses were determined based on the US Health Resources and Services Administration HIV/AIDS Bureau definitions of retention in care as these are the standard measures used both federally and by local and state health departments [35]. Based on dates of clinical visits, participants who reported at least two visits at least 90 days apart in a 12 month period were considered to be ‘in care’. Participants reporting a care pattern that did not meet the definition of in care were considered to be in ‘sporadic care’. For example, participants who reported two visits less than 90 days apart or reported only one HIV-related medical visit in the past 12 months would have been in sporadic care. Participants who reported not having any HIV-related medical visits in at least six months were considered to be ‘out of care’.
Participant Recruitment
Persons in care or sporadic care were identified through clinic-based convenience sampling. In conjunction with the 2013 DC DOH Recapture Blitz, lists of individuals not receiving an HIV care visit in the previous six to 12 months were used to identify persons who were out of care [31]. Methods utilized for the Recapture Blitz and identification of participants for this study have been previously described [31, 34]. In brief, recruitment occurred in three HIV clinics, through a local emergency department (ED), and by way of outreach with a community-based organization (CBO) to identify study participants at different stages of care between June 2013 and July 2016. To be enrolled in the study, participants had to be 18 years of age or older, self-reported living with HIV, and not attending their first HIV visit if recruited at a clinic. Participants were screened for eligibility and consented to participate in a one-time cross-sectional survey. A subsample of participants also participated in in-depth, qualitative interviews to gather additional information regarding participant perspectives on engagement in care. For the qualitative interviews, all out of care participants were asked to participate in an in-depth interview and every other participant who was in care or sporadic care was asked to participate.
Data Sources
Data for this analysis were collected from self-administered structured surveys and in-depth interviews. The surveys included questions about demographics, general health and HIV care-seeking behaviors, HIV treatment history, facilitators to care for in care and sporadic care participants, and barriers to care engagement among all participants including patient-provider relationships, attitudes regarding clinic visits, and unmet and met needs. A need was defined as ‘unmet’ if the participant reported a service or support was needed or desired but not received, whereas a need was considered to be met if it had been fulfilled per participant self-report. Qualitative interviews focused on linkage to care, availability of support systems, stigma, engagement with care providers, and barriers to care. All interviews were audio-recorded and transcribed, and separate informed consent was obtained for these interviews. Participants received $25 for participation in the survey, an additional $25 for the qualitative interview, and Metro fare cards to compensate them for travel. Study procedures were reviewed and approved by both the George Washington University and DC DOH Institutional Review Boards.
Analytic Methods
Descriptive statistics were used to summarize participants’ demographics, reported social supports, provider relationships, unmet needs, and barriers and facilitators to care. Bivariate tests were used to examine differences among the three categories of engagement in care. These tests included chi-square tests for categorical outcomes, Fisher’s exact tests for categorical outcomes with small sizes, and Kruskal Wallis tests for non-normally distributed continuous variables. All analyses were conducted using SAS version 9.3.
Qualitative data from semi-structured interviews were analyzed using open and axial coding to identify emergent patterns, categories, and themes in the data. Three experienced qualitative researchers on the project team coded interview transcripts using ATLAS.ti 7. Initial codes were developed based on the study conceptual framework, and subsequent codes were selected as they emerged from the interviews. The analysis process employed the constant comparative method, following an iterative process of coding, analysis, and recoding based on inductive reasoning, that identified and characterized emergent and relevant domains elucidated during the interview and identified through the overall objectives of the project [36, 37]. A conceptually clustered matrix was further developed to illustrate the relationships between the perspectives among the three care groups [38].
Results
Participant Demographics
Of the 172 participants recruited, based on their self-reported care patterns, 114 (66.3%) were in care, 34 (19.8%) were in sporadic care, and 24 (14.0%) were out of care. All in care and sporadic care participants were recruited from HIV clinics; 21% and 13% of out of care participants were recruited from a local CBO and ED, respectively. Overall, survey participants were mainly non-Hispanic Black (72.8%), men (63.0%), DC residents (88.4%), and had a mean age of 50.9 years old (SD:8.9 years; range 25–70 years). Survey participants were living with their HIV diagnosis for a median of 17 years (12.6 IQR). Most survey participants had health insurance (91.3%) and were unemployed (62.8%). Commonly reported co-morbidities included mental health diagnoses (46.5%), hepatitis C (28.5%), cardiovascular disease (27.9%) and diabetes (14%); slightly more than half of the participants reported multiple comorbidities (53.5%) (data not shown). As shown in Table 1, survey participant demographics did not differ significantly by care status except based on race/ethnicity and history of incarceration. A higher proportion of out of care participants reported having been in jail, detention, or prison in the last year (29.2% vs. 2.6% in care vs. 5.8% in sporadic care, p < 0.0001) and a lower proportion of sporadic care participants were non-Hispanic Black (36.4% vs. 75.5% in care vs. 83.3% out of care, p = 0.0359).
Table 1.
Distribution of demographics and social supports among survey participants by level of HIV care engagement, Washington, DC, N = 172
| Characteristics | Total n = 172 |
In care n = 114 |
Sporadic care N = 34 |
Out of care N = 24 |
Test statistic | p-value |
|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |||
| Age (yrs), mean (SD) | 50.9 (8.9) | 51.9 (8.5) | 46.3 (12.8) | 51.1 (6.6) | 2.3114 | 0.3148a |
| Race/ethnicity (n = 92) | N/A | 0.0359a | ||||
| Black non-Hispanic | 67 (72.8) | 43 (75.5) | 4 (36.4) | 20 (83.3) | ||
| White non-Hispanic | 14 (15.2) | 7 (12.3) | 3 (27.3) | 4 (16.7) | ||
| Hispanic | 5 (5.4) | 3 (5.3) | 2 (18.2) | 0 (0) | ||
| Other (including multi-racial) | 6 (6.5) | 4 (7.0) | 2 (18.2) | 0 (0) | ||
| DC resident | 152 (88.4) | 101 (88.6) | 31 (91.2) | 20 (83.3) | N/A | 0.6751a |
| Gender (n = 92) | N/A | 0.4161a | ||||
| Female | 34 (37.0) | 22 (38.6) | 2 (18.2) | 10 (41.7) | ||
| Male | 58 (63.0) | 35 (61.4) | 9 (81.8) | 14 (58.3) | ||
| Insured in past 12 months | 157 (91.3) | 105 (92.1) | 32 (94.1) | 20 (83.3) | 2.7204 | 0.2566 |
| Homeless/unstably housedb | 44 (25.6) | 27 (23.7) | 8 (23.5) | 9 (37.5) | 2.0816 | 0.3532 |
| Ever been in jail, detention, or prison in last year | 12 (7.0) | 3 (2.6) | 2 (5.8) | 7 (29.2) | N/A | < 0.0001a |
| Education | 8.164 | 0.2263 | ||||
| Less than high school | 31 (18.0) | 17 (15.0) | 9 (26.5) | 5 (20.8) | ||
| High school/GED | 55 (32.0) | 35 (30.7) | 11 (32.4) | 9 (37.5) | ||
| Some college | 54 (31.4) | 42 (36.8) | 5 (14.7) | 7 (29.2) | ||
| College/post baccalaureate | 32 (18.6) | 20 (17.5) | 9 (26.5) | 3 (12.5) | ||
| Employment status | N/A | 0.5398a | ||||
| Unemployed | 108 (62.8) | 75 (66.8) | 17 (50.0) | 16 (66.7) | ||
| Part-time or less | 29 (16.9) | 17 (14.9) | 8 (23.5) | 4 (16.7) | ||
| Full-time | 35 (20.4) | 22 (19.3) | 9 (26.5) | 4 (16.7) | ||
| Relationship status | N/A | 0.6086a | ||||
| Legally married | 15 (8.7) | 10 (8.8) | 3 (8.8) | 2 (8.3) | ||
| Committed relationship | 35 (20.4) | 24 (21.1) | 5 (14.7) | 6 (25.0) | ||
| Open relationship | 1 (0.6) | 1 (0.9) | 0 (0) | 0 (0) | ||
| Single | 90 (52.3) | 62 (54.4) | 20 (58.8) | 8 (33.3) | ||
| Widowed/divorced/separated | 30 (17.4) | 17 (14.9) | 6 (17.7) | 7 (29.2) | ||
| Years diagnosed with HIV (median, IQR) | 17.0 (12.6) | 16.8 (12.8) | 14.6 (12.6) | 17.1 (15.8) | 3.6778 | 0.159a |
| Comorbidities | ||||||
| Mental health | 80 (46.5) | 55 (48.3) | 16 (47.1) | 9 (37.5) | 0.9253 | 0.6296 |
| Hepatitis C | 49 (28.5) | 33 (29.0) | 9 (26.5) | 7 (29.2) | 0.0852 | 0.9583 |
| Cardiovascular disease | 48 (27.9) | 35 (30.7) | 6 (17.7) | 7 (29.2) | 2.2404 | 0.3262 |
| Diabetes | 24 (14.0) | 18 (15.8) | 3 (8.8) | 3 (12.5) | N/A | 0.6785a |
| Primary caregiver of: | ||||||
| Child(ren) under 18 | 29 (16.9) | 15 (13.2) | 9 (26.5) | 5 (20.8) | 3.6252 | 0.1632 |
| Elderly person(s) | 13 (7.6) | 8 (7.0) | 4 (11.8) | 1 (4.2) | N/A | 0.5682a |
| Person(s) living with HIV/AIDS | 12 (7.0) | 9 (7.9) | 1 (2.9) | 2 (8.3) | N/A | 0.6620a |
| Person(s) living with a disability or illness that is not HIV or AIDS | 19 (11.1) | 13 (11.4) | 4 (11.8) | 2 (8.3) | N/A | 1.00a |
| Have received help getting into HIV care | 82 (47.7) | 50 (43.9) | 20 (58.8) | 12 (50.0) | 2.4112 | 0.2995 |
| Have told someone that you are living with HIV | 165 (95.9) | 109 (95.6) | 32 (94.1) | 24 (100.0) | N/A | 0.6154a |
| Number of people told about HIV status other than healthcare workers | N/A | 0.5101a | ||||
| None | 1 (0.6) | 1 (0.9) | 0 (0) | 0 (0) | ||
| 1 person | 10 (5.8) | 8 (7.0) | 1 (2.9) | 1 (4.2) | ||
| 2–5 people | 43 (25.0) | 26 (22.8) | 11 (32.4) | 6 (25.0) | ||
| 6–10 people | 24 (14.0) | 14 (12.3) | 7 (20.6) | 3 (12.5) | ||
| More than 10 people | 86 (50.0) | 60 (52.6) | 13 (38.2) | 13 (54.2) | ||
| Have disclosed to: | ||||||
| Family member(s) | 142 (82.6) | 92 (80.7) | 29 (85.3) | 21 (87.5) | N/A | 0.7215a |
| Friend(s) | 136 (79.1) | 86 (75.4) | 29 (85.3) | 21 (87.5) | N/A | 0.3303a |
| Other people | 76 (44.2) | 49 (43.0) | 14 (41.2) | 13 (54.2) | 1.1612 | 0.5596 |
| Social support: always or most of the time have: | ||||||
| Someone to give you good advice during a crisis | 127 (73.8) | 84 (73.7) | 27 (79.4) | 16 (66.7) | 1.1871 | 0.5524 |
| Someone to confide in or talk to about yourself or your problems | 124 (72.1) | 85 (74.6) | 24 (70.6) | 15 (62.5) | 1.4813 | 0.4768 |
| Someone who understands your problems | 119 (69.2) | 80 (70.2) | 23 (67.7) | 16 (66.7) | 0.1616 | 0.9224 |
Indicates Kruskal Wallis or Fisher’s exact test used. N/A indicates not applicable as a test statistic is not generated
Defined as yes to living on street, single room occupancy hotel, shelter, car or staying with friends without paying rent in prior 12 months Significant p-values are bolded
Qualitative interviews were conducted with a subset of 62 participants across the care groups (40 in care, 10 sporadic care, and 12 out of care). A majority of interview participants identified as men (57%) and non-Hispanic Black (77%), the median age was 52 years, and the median length of time since diagnosis among all participants was 16 years. Sporadic care participants were younger [median age 42 vs. 52 years (in care) vs. 53 years (out of care)], fewer were Black [50% vs. 75% (in care) vs. 83% (out of care)] and had a more recent HIV diagnosis [median 11 vs. 15 years (in care) vs. 19 years (out of care)].
Disclosure and Social Support
Most participants reported having disclosed their HIV status (95.9%) (Table 1), with the majority (64.0%) disclosing to six or more people, not including health care workers. Disclosure occurred to family members (82.6%), friends (79.1%), and others (44.2%). The majority of the participants reported having social support always or most of the time, such as someone to receive advice from during a crisis (73.8%) and someone to confide in (72.1%). This did not differ significantly between participants’ care statuses.
Engagement in Care and Patient-Provider Relationships
Most participants reported good provider relationships regardless of their care status: 98.3% felt listened to; 98.3% felt respected; and 99.4% and 94.8% respectively felt their provider gave clear explanations and spent sufficient time with them (Table 2). A significantly higher proportion of in care participants felt their provider was informed and up-to-date than those in sporadic care (82.7% vs. 72.2%, X2 = 4.447; p = 0.0350). Despite positive patient-provider relationships, only 56.9% of in care and sporadic care participants reported having spoken with their primary HIV provider about a personal or family problem, alcohol use, or a mental or emotional illness they were experiencing in the last 12 months.
Table 2.
Patient-provider relationship and engagement in care
| Strongly or somewhat agree with the following statementsa | Total N (%) |
In care N (%) |
Sporadic care N (%) |
Out of care N (%) |
Test statistic | p-value |
|---|---|---|---|---|---|---|
| During my most recent visit at this clinic, my main HIV medical provider listened carefully to me | 169 (98.3) | 113 (99.1) | 34 (100.0) | 22 (91.7) | N/A | 0.0748c |
| During my most recent visit at this clinic, my main HIV medical provider explained things in a way that I could understand | 171 (99.4) | 114 (100.0) | 34 (100.0) | 23 (95.8) | N/A | 0.1395c |
| During my most recent visit at this clinic, my main HIV medical provider showed respect for what I had to say | 169 (98.3) | 113 (99.1) | 34 (100.0) | 22 (91.7) | N/A | 0.0748c |
| During my most recent visit at this clinic, my main HIV medical provider spent enough time with me | 163 (94.8) | 107 (93.9) | 34 (100.0) | 22 (91.7) | N/A | 0.2869c |
| In the last 12”months, main HIV health care provider usually or always seemed informed and up-to-date about the care you got from specialists (n = 99)b | 80 (80.8) | 67 (82.7) | 13 (72.2) | N/Ad | 4.447 | 0.0350 |
| In the last 12 months, I talked with main HIV health care provider about a personal problem, family problem, alcohol use, or a mental or emotional illness they were experiencing (n = 130)b | 74 (56.9) | 57 (58.2) | 17 (53.1) | N/Ad | N/A | 0.6173c |
Questions were asked on a Likert Scale with possible responses of strongly agree, somewhat agree, strongly disagree, don’t know, refuse to answer
Includes only those who responded to the question
Indicates Fisher’s exact test used; otherwise Chi-Square test used. N/A indicates not applicable as a test statistic is not generated
Not asked of out of care participants as by definition they were not seen by a provider in the last 6 to 12 months
Significant p-values are bolded
Reported Unmet Needs
Overall, a mean of 1.7 unmet needs were reported among all participants (1.6 in care vs. 1.9 sporadic care vs. 2.3 out of care). Counseling was the most commonly reported need (50.9%) among all participants (Table 3). Reported needs differed slightly by care status. Counseling was the most commonly reported need for both in care and sporadic care participants; emergency financial assistance was the most commonly reported need for out of care participants. Significantly more out of care participants reported needing emergency financial assistance than in care and sporadic care participants [54.2% vs. 30.7% (in care) vs. 23.5% (sporadic care), X2 = 6.5447; p = 0.0379].
Table 3.
Self-reported needs and unmet needs stratified by care status
| Service | Total | In care | Sporadic care | Out of care | Needs test statistic | Needs p-value | Unmet needs test statistic | Unmet needs p-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Needed | Unmet | Needed | Unmet | Needed | Unmet | Needed | Unmet | |||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||||
| Mean number of unmet needs (SD) | 3.2 (1.6) | 1.7 (1.1) | 3.2 (1.6) | 1.6 (0.95) | 2.8 (1.5) | 1.9 (1.1) | 3.6 (1.9) | 2.3 (1.3) | 1.3726 | 0.5034b | 4.363 | 0.1129b |
| Housing | 51 (29.7) | 30 (58.8) | 37 (32.5) | 22 (59.5) | 7 (20.6) | 3 (42.9) | 7 (29.2) | 5 (71.4) | 1.7715 | 0.4124 | N/A | 0.6342a |
| Counseling | 87 (50.9) | 14 (16.1) | 62 (54.4) | 8 (12.9) | 14 (41.2) | 3 (21.4) | 11 (45.8) | 3 (27.8) | 2.0797 | 0.3535 | N/A | 0.3908a |
| Substance abuse | 29 (16.9) | 3 (10.3) | 16 (14.0) | 2 (12.5) | 6 (17.7) | 0 (0) | 7 (29.2) | 1 (14.3) | 3.2571 | 0.1962 | N/A | 1.0000a |
| Emergency financial assistance | 56 (32.6) | 20 (35.7) | 35 (30.7) | 10 (28.6) | 8 (23.5) | 3 (37.5) | 13 (54.2) | 7 (53.9) | 6.5447 | 0.0379 | N/A | 0.0342a |
| Employment assistance | 49 (28.5) | 21 (42.9) | 34(29.8) | 11 (32.4) | 8 (23.5) | 4 (50.0) | 7 (29.2) | 6 (85.7) | 6 (85.7) | 0.7727 | N/A | 0.1266a |
| Food, groceries, meals | 77 (45.0) | 6 (7.8) | 57 (50.0) | 4 (7.0) | 8 (24.2) | 1 (12.5) | 12 (50.0) | 1 (8.3) | 7.1381 | 0.0282 | N/A | 0.7868a |
| Benefits | 49 (28.5) | 12 (24.5) | 31 (27.2) | 7 (22.6) | 11 (32.4) | 3 (27.3) | 7 (29.2) | 2 (28.6) | 0.03486 | 0.8401 | N/A | 0.7736a |
A service was defined as being needed if a participant indicated needing access to service in the prior year. A service was defined as unmet if participant indicated not having received a service in the past year
Indicates Fisher’s exact test used. N/A indicated not applicable as a test statistic is not generated
Indicates Kruskal–Wallis test used
Significant p-values are bolded
Housing was the most commonly reported unmet need overall, with 58.8% of participants reporting they were unable to obtain housing services. Among those reporting an unmet need for housing, 66.7% (20/30) also reported experiencing unstable housing (data not shown). The second most frequent unmet need was employment assistance (42.9%). Across the different care statuses, housing was the greatest reported unmet need for in care (59.5%) participants, whereas employment assistance was the greatest reported unmet need for sporadic care (50.0%) and out of care (85.7%) participants. Significantly more out of care participants reported not receiving emergency financial assistance [53.9% versus 28.6% (in care) vs. 37.5% (sporadic care), p = 0.0342].
Facilitators and Barriers to Care
Reported facilitators to care did not differ significantly between in care and sporadic care participants, as shown in Fig. 1. The most commonly reported facilitators of engagement in care among in care and sporadic care participants were flexible appointments (86.5%), appointment reminders (77.7%), HIV provider working in the same clinic as participants’ other health care providers (55.4%), and transportation (51.4%).
Fig. 1.
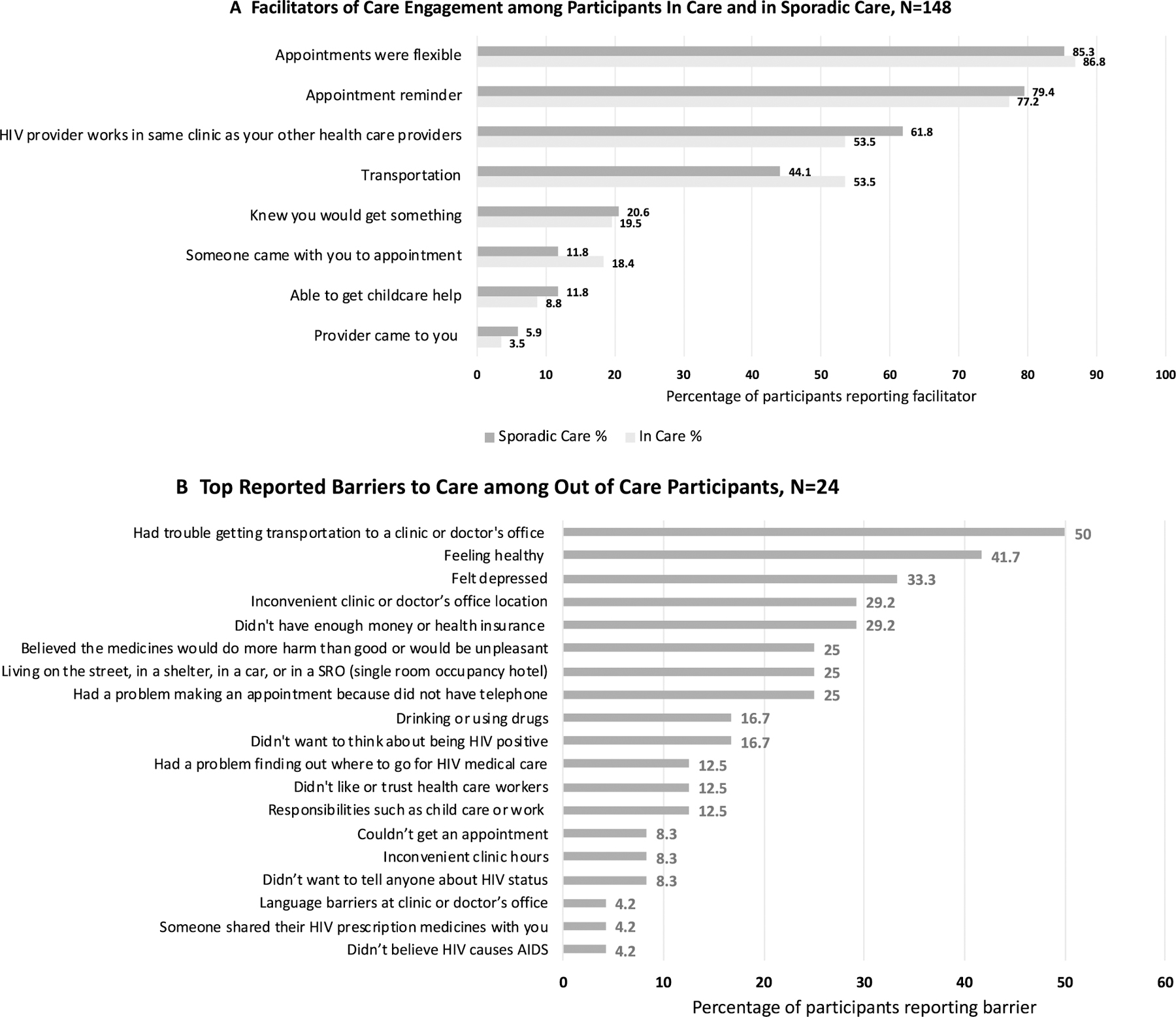
Reported Barriers and Facilitators of Engagement in Care, by Engagement Status. A. illustrates the most commonly reported facilitators of engagement in care reported among persons living with HIV stratified by participants who were regularly engaged in care and those who were in sporadic care (N= 148). B. illustrates the most commonly reported barriers to care reported among persons living with HIV who had been out of care for at least 6 months (N = 24).
Among out of care participants, the most commonly reported barriers to care were transportation (50.0%), feeling healthy (41.7%), and feeling depressed (33.3%) (Fig. 1). Additionally, out of care participants also reported lack of money or insurance (29.2%), inconvenient clinic or doctor’s office location (29.2%), unstable housing (25.0%), and belief that medicines would do more harm than good or would be unpleasant (25.0%) as other barriers to care.
In-Depth Interviews
Qualitative interviews were conducted to gain in-depth information regarding the care continuum and to complement and expand the survey data. Regardless of care status, participants highlighted the pervasive role of HIV stigma in their lives, and how it impacts their decisions about disclosure due to fear of rejection and discrimination (Table 4). However, they also recognized how disclosing to others and having social support resulted in positive effects on their health, including the ability to be engaged in care which substantiates survey findings on high rates of disclosure and social support among all care groups. Participants, regardless of care status, also discussed having numerous barriers and challenges in engaging in care including substance use, lack of money and time, and denial of HIV status. Others also stated that feeling “well” or “healthy” kept them from making and keeping appointments or adhering to treatment. Most participants overall expressed positive relationships with their providers. Similar to the survey responses, many stated that they were motivated to engage in care with providers who were patient, treated them with respect, and expressed genuine concern for their health and overall well-being.
Table 4.
Key qualitative interview domains and sample quotes
| Domain | In Care (N = 40) | Sporadic Care (N = 10) | Out of Care (N = 12) |
|---|---|---|---|
| Social support and stigma | I just wouldn’t trust people with such sensitive information because I don’t know how they would use it, manipulate it, share it. I just don’t know where the information would go. And there is still a stigma with the HIV status and I’m just not prepared to be exposed that way. It’s not their business; I don’t want to tell nobody. You confide in people, it normally comes back in your face, with me. So I’m very skeptical about who I tell about my illness, because for one I don’t want to blurt it out at me because we had a misunderstanding about something, you know. So I am very selective. It was hard disclosing because of fear of rejection. But I wanted to be loved for me totally, and not just partially. |
If there is someone in your life that you can trust and you share that with and they can relate because they’re in the same situation, it does make it easier for you to maintain and then when you’re having difficult times and you think about it more—someone that is in the same situation as you has a better understanding. They’re less likely to judge you. I know that sometimes people feel like they have really good friends, but until you’re really facing a life-threatening situation or something happens, I don’t know if you really know how good your friends are. It’s really not easy to talk about with me. At best I don’t hold a conversation. I mean it’s been months and years; it’s not talked about. |
Just knowing the fact that [my family is] there in my corner and they are concerned about my health. Just the fact that they know, and they are supportive of me keeps me healthy. I am afraid of the stigma. What are they going to think of me? They are not going to want to have anything to do with me, you know. Our kids go to school together, you know, I don’t even want to think of what would happen if people found out. I need more information. I need somebody more to talk to, somebody more to explain it. I need people like me that understand what I’m going through. So people that are already positive. Some people HIV positive understand more what I’m going through than some people that don’t. |
| Engagement with care providers | My [primary care provider] was just so like in and out. He was just like he didn’t care like I’m just here to get a check. He didn’t answer my questions when I came so I never went back to him. I didn’t like that. It was just like he was there for a paycheck and not to assist me, and what I needed, so I never went back to him. I have had a wonderful doctor. Wonderful nurses, wonderful staff. People that are very compassionate, and understanding, and educated about the disease. They’ve embraced me. Not only my HIV, but they want to know about my other illnesses, they want to know about my home life, they want to know about my children, they want to know about my mental stability, they want to know about my housing. They want to know about me as a whole individual, and not just HIV. |
My doctor is very helpful and caring. He shows me that he cares about me. He talks to me, he makes me want to come back, you know, ‘cause it’s like I have to help myself for him to help me. Their personality… how they treat people. I mean, they treat you like family. From my caseworker—and everything is right here and it’s convenient. But more, among it all, their personality. They have genuine concern. And they’re patient. And they help you. I mean, they do all they can, from the doctor to the nurses upstairs, even the one taking my blood, my case manager, the drug counselor, mental health. |
Staff is wonderful. I love the staff. I love how they treat you, how they talk to you, how they get you express your own opinions, how they take your opinions and use them. I think my doctor is the bomb.com, because he does not force nothing on nobody he gives them the information that is needed to have them to make a conscious decision. So patience is needed sometimes, cause sometimes doctors don’t have patience. |
| Linkage to care | I felt healthy. I mean I feel really healthy even though the doctors freak out every time they see my numbers, but I feel like there’s nothing wrong… I just feel like I am healthy all the time, I am not sick, so that’s why I don’t make appointments and that’s why I don’t take my medicine. If I have heroin problem, well addiction, if for some reason I didn’t get heroin, then I have to go to heroin withdrawal. So any type of appointment was not important at that particular time. The drug was more important. |
I didn’t want to believe I had HIV. It was painful for me every time I talked about it or acknowledged it. At first I thought I was going to die… At that time, I didn’t want to come see the doctor. And it was a lack of money, I had to pay to come to the doctor so I wanted to get high more than I wanted to do my health. But now, I don’t want to get high. You know, take care of myself and live longer. I am going back to school I want to do something for myself. I want to live. The sooner you get involved, the sooner you start to allow people to come in and do what they do, the better chance you have. Because if not, you can get swallowed up whole. |
Just got sick and tired of being sick and tired. By the time I got into care, it wasn’t about my HIV; it was about my addiction. My addiction had spiraled so far from my morals, my principles, my family. My addiction carried me, would you say, to a place that nobody wanna go. I just turned around one day and was like “oh my God I can’t believe it’s been a year since I have been to the doctor.” Wow, time just went by that fast, so just the inconvenience of life and scheduling, and commuting. |
| Unmet needs | I have a lot of bills piled up for doctors, just coming to the visits or you know just being positive for twenty something years or whatever. All these bills are piling up. But that’s the big…how am I going to pay for this? You know, ‘cause every month, it costs me $300 every month to go get my medicine and I can’t afford that. Sometimes I’m lacking transportation because of finances. I can’t get to my appointments because of finances. I am on SSI, which is a very limited amount of money once per month. So I would say finances. Housing is biggest thing that I need right now. I live in a pretty terrible neighborhood, that’s just drug-infested. You know, which is not good for me, mentally, emotionally, physically, or my sons. But housing plays a part of my HIV also. |
Got to be insurance, I need a better insurance, I need a good insurance, ‘cause these insurance, once you tell them the disease that you have, it’s like the costs go up higher… And as a retiree I am not getting enough money. What worries me is a lapse in coverage like if I make too much to not qualify for Medicare or Medicaid, sometimes I don’t work so I get both. That bothers me. Or if I make too much to not qualify for Medicaid but then I could never afford private insurance, except now for Obamacare, on my own. And when I do look at Obamacare it’s like $400 a person, that’s a lot of money for someone who doesn’t make a lot. So that can be a hindrance too. Financial. That’s definitely an issue with me, even though I know that, I could always go back to school and you know change my financial status, gain employment. |
So transportation is one of the biggest issues for me seeing the doctor. First it was insurance but now I got insurance, sometimes I don’t have the money to get there. So transportation is the biggest thing. If I have the money, I’ll catch the bus. But if I don’t have the money, I won’t go, because I can’t get there. The only thing for me is insurance. Insurance and transportation were the two main reasons. Two barriers. Sometimes it’s like ok, like the medicine sometimes if I don’t have the money to get it. So it sits in the pharmacy, because I don’t have a dollar to go pay for it. The location of the clinic is not so bad. And the hours not so bad. It’s just how far it is to get to it. |
As reflected in the survey data, poverty and a lack of money was a prominent unmet need among interview participants across all care groups. Specifically, many participants noted that they did not have enough money for medical care, such as co-pays for treatment and doctor’s visits even with insurance. Being uninsured or under-insured, unstably housed, unemployed, and not having access to reliable transportation, in conjunction with a lack of financial resources, impeded PLWH’s ability to engage in care.
Conclusions
Engagement and retention in care is an essential component of the HIV care continuum. Identifying unmet needs as well as facilitators and barriers to care can help engage PLWH in care and result in improved health outcomes and prevent further HIV transmission. In this study, we identified and compared unmet needs as well as identified facilitators and barriers to care for PLWH at different levels of care engagement. Our sample, although relatively small, is consistent with the wider population of PLWH in DC, wherein a majority are non-Hispanic Black, older men who have health insurance [28]. There was a slight demographic difference among the out of care participants compared to those in care and in sporadic care, with a higher proportion of out of care participants having been in and out of the criminal justice system in the prior year. This is important to note as it may have affected their ability to engage and remain in care. Other studies, for instance, have highlighted how numerous acute barriers such as poverty, homelessness, unemployment, and addiction limit PLWH’s ability to engage in HIV care after incarceration [39–42] and this may be an area for further qualitative exploration.
All survey participants reported high rates of HIV status disclosure, social support and provider engagement with no differences by care status. Qualitative interviews further support the survey findings with the majority of participants feeling as though their providers cared for and listened to them. These findings align with previous studies that have reported poor provider relationships as a barrier to engagement and retention in care [43–46] and suggest that positive patient-provider relationships alone are not sufficient to keep out of care and sporadic care participants in DC retained in care. Given the positive experiences reported, providers could help reinforce the need for regular HIV care visits and treatment adherence, as well as address patients’ questions and concerns.
In the qualitative interviews, participants noted that despite having social support, they continued to struggle with HIV stigma, fear of rejection, and experiences of discrimination, all of which hindered decisions about disclosure. Participants also expressed a desire to have more social support from PLWH because they understood their experience. Stigma is clearly present in participants’ social networks and communities and may prevent them from asking for and receiving support related to engagement in care from family and friends. While social support is generally considered to be a facilitator of engagement in care, our findings underscore the need to better understand the different sources and types of support that are most effective for successful engagement and retention in HIV care [47, 48].
Behavioral health issues were identified through both survey and qualitative interviews. All three care groups identified at least two unmet needs with counseling reported as the greatest need overall in the survey, and depression was also identified as a barrier to care by out of care participants. Qualitative interviews further revealed that stigma along with substance use impeded participants’ ability to engage in care. Issues with mental health, including depression, are commonly observed among PLWH and have been noted by multiple studies as a barrier to care [49–52]. Depression also may indicate the presence of other mental health issues such as trauma, substance use disorder, negative perceptions of HIV diagnosis and treatment, and the presence of competing priorities [14, 18, 33, 43, 53–55]. Delivery of mental health counseling and support services is recommended by multiple HIV-focused programs and organizations [56] as studies have shown that access to these services can lead to improved treatment adherence and engagement in care [57–61]. Therefore, the provision of counseling services and related mental health and harm reduction support systems should be a cornerstone of effective HIV care engagement.
Unmet needs, which varied only slightly by care status, were identified as the provision of housing, emergency financial assistance, employment assistance, and food security in the survey data. For in care participants, housing was the greatest unmet need, whereas for sporadic and out of care participants, employment assistance was the greatest unmet need. Housing services may remain an unmet need for in care participants because many housing program services are directed toward those who are homeless, and may not reach those who are marginally housed or perceived to be stably housed. Further, while more in care participants reported needing housing, out of care participants still had the largest gap in having that need met. Emergency financial assistance was also a significant unmet need for out of care participants. Qualitative interviews further supported these survey findings, indicating that a lack of financial resources was an overwhelming unmet need across the care groups, along with a lack of adequate insurance coverage, housing, employment opportunities, and transportation. The identification of these unmet needs highlights the complex issues PLWH face in their daily lives and reinforces the pervasive social and structural inequities faced by racial/ethnic PLWH [13, 62–66]. Competing life priorities have been shown to be a common reason for lack of engagement and retention in care [33, 46, 62, 67]. Several programs in DC are designed to address these needs, such as Housing Opportunities for People with AIDS, DC Ticket to Work, and Project Empowerment Program, but participants may have been unaware of or unable to access them. Highly structured coordination approaches between different organizations involving a substantial investment of resources and ongoing interagency activities need to be developed to link PLWH to available programs, along with more innovative approaches to integrating sustainable housing, financial assistance, and job programs within HIV care. Interventions that address these structural barriers and deliver services to facilitate care may relieve the burden of competing priorities, allowing individuals to focus on their HIV care.
The most common facilitators for in care and sporadic care participants were flexible appointments, appointment reminders, and transportation availability. Additionally, a common identified barrier to care among out of care participants was transportation in both the survey and qualitative interviews. Transportation has been identified by numerous studies as an integral part of retention in care for PLWH [68–70], yet it is surprising to find as the main barrier to care for this sample of out of care participants in DC, a city that has a relatively small geographic area and a well-developed and highly accessible public transportation system [71]. However, the cost of public transportation, perceptions around safety, inconvenient clinic locations, and long public transport times may play a role in the identification of transportation as a barrier to care. Recent research in other large cities like Philadelphia and Atlanta, for instance, found that complex associations exist between transportation, community-level care linkage and viral suppression, and community poverty levels [68, 72]. Mobile service delivery may be one way to address this barrier, allowing for more continuous care for PLWH by bringing care to them [73, 74]. Providers should also be trained to assess transportation vulnerability at the time of diagnosis and during follow-up appointments.
There were several limitations to the study. Out of care participants were difficult to recruit since they have little to no contact with the HIV providers from where we were recruiting. While multiple recruiting strategies were used, the out of care participants who were enrolled in the study tended to be similar to in care and sporadic care participants in terms of socio-demographics. It is possible that the out of care participants in our study were more willing to re-engage in care than out of care individuals more broadly, a factor in our ability to recruit them. Therefore, there may have been some selection bias and those who participated may not be representative of all out of care PLWH in DC, particularly those who are hardest to reach and re-engage in care. Similarly, since participants for the in care and sporadic care groups were recruited from clinics, there is the potential for selection bias among those approached to be in the study and those who participated. Moreover, the smaller numbers of PLWH recruited from the out of care and sporadic care categories is also a limitation which may have hindered our ability to reach meaningful conclusions given our limited statistical power. Completion of the survey in a clinic may have also led to bias in the participants’ responses, influencing their reports of provider relationships in particular. There was also the potential for social desirability bias since the data collected were based on participant self-report, especially for categorizing care status as they may have overestimated their engagement in care. Additionally, while we asked about all unmet needs, future studies of PLWH at different stages of the care continuum should consider assessing a hierarchical ranking of needs to determine those that are most salient for PLWH based on their care status. Finally, while we assessed facilitators to care among in care and sporadic participants, follow up surveys and in-depth interviews should ask PLWH who are out of care about facilitators of care to identify potential interventions that may improve their care engagement.
This study enabled a comparison of unmet needs and facilitators and barriers to care between people at different stages of HIV care engagement and demonstrated a general consistency of unmet needs of individuals across varied levels of care engagement. Our findings illustrate the multifaceted, complex nature of unmet needs among PLWH and the individual and structural challenges they face throughout the HIV care continuum. They also underscore the critical importance of developing multi-level (i.e., individual and social-structural) interventions to address social, psychological, and economic needs and promote engagement and retention in care among PLWH.
Acknowledgements
The authors would like to thank the staff at DC Department of Health HIV/AIDS Hepatitis, STD, TB Administration for their assistance with the Recapture Blitz; staff at the participating clinics and organizations for their assistance with recruitment; and the study participants without whom these data would not be possible. The authors would also like to acknowledge the DC Center for AIDS Research (P30AI117970) and the ECHPP-2 study team.
Funding
This study was funded through a supplemental to the DC Center for AIDS Research (P30AI117970).
Footnotes
Code Availability Not applicable.
Compliance with Ethical Standards
Conflict of interest The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval All procedures and study materials were reviewed and approved by the George Washington and DC Department of Health Institutional Review Boards. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate Informed consent was obtained from all individual participants included in the study.
Data Availability
Not applicable.
References
- 1.Crawford TN. Poor retention in care one-year after viral suppression: a significant predictor of viral rebound. AIDS Care 2014;26(11):1393–9. 10.1080/09540121.2014.920076. [DOI] [PubMed] [Google Scholar]
- 2.Horberg MA, Hurley LB, Silverberg MJ, Klein DB, Quesenberry CP, Mugavero MJ. Missed office visits and risk of mortality among hiv-infected subjects in a large healthcare system in the United States. AIDS Patient Care STDS 2013;27(8):442–9. 10.1089/apc.2013.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sabin CA, Howarth A, Jose S, et al. Association between engagement in-care and mortality in HIV-positive persons. AIDS 2017;31(5):653–60. 10.1097/QAD.0000000000001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital signs: HIV transmission along the continuum of care - United States, 2016. MMWR Morb Mortal Wkly Rep 2019;68(11):267–72. 10.15585/mmwr.mm6811e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zinski A, Westfall AO, Gardner LI, et al. The contribution of missed clinic visits to disparities in HIV viral load outcomes. Am J Public Health 2015;105(10):2068–75. 10.2105/AJPH.2015.302695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011;52(6):793–800. 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yehia BR, French B, Fleishman JA, et al. Retention in care is more strongly associated with viral suppression in HIV-infected patients with lower versus higher CD4 counts. J Acquir Immune Defic Syndr 2014;65:333–9. 10.1097/QAI.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med 2015;175(4):588–96. 10.1001/jamainternmed.2014.8180. [DOI] [PubMed] [Google Scholar]
- 9.Marks G, Gardner LI, Craw J, Crepaz N. Entry and retention in medical care among HIV-diagnosed persons: a meta-analysis. AIDS 2010;24(17):2665–78. 10.1097/QAD.0b013e32833f4b1b. [DOI] [PubMed] [Google Scholar]
- 10.Centers for disease control and prevention 2016 Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas, 2016. Atlanta, 2019. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-24-3.pdf. Accessed 17 Mar 2020. [Google Scholar]
- 11.White house office of national AIDS policy 2015 National HIV/AIDS strategy for the United States: updated to 2020. Washington, DC [Google Scholar]
- 12.Kempf MC, McLeod J, Boehme AK, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: implications for targeted interventions. AIDS Patient Care STDS 2010;24(8):515–20. 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 13.Aidala AA, Lee G, Abramson DM, Messeri P, Siegler A. Housing need, housing assistance, and connection to HIV medical care. AIDS Behav 2007. 10.1007/s10461-007-9276-x. [DOI] [PubMed] [Google Scholar]
- 14.Dombrowski JC, Simoni JM, Katz DA, Golden MR. Barriers to HIV care and treatment among participants in a public health HIV care relinkage program. AIDS Patient Care STDS 2015;29(5):279–87. 10.1089/apc.2014.0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coyle RP, Schneck CD, Morrow M, et al. Engagement in mental health care is associated with higher cumulative drug exposure and adherence to antiretroviral therapy. AIDS Behav 2019;23(12):3493–502. 10.1007/s10461-019-02441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chartier M, Maier M. Engagement along the HIV care continuum and the potential role of mental health and substance use disorders. Fed Pract 2015;32(Suppl 2):10S. [PMC free article] [PubMed] [Google Scholar]
- 17.Calsyn RJ, Klinkenberg WD, Morse GA, Miller J, Cruthis R. Recruitment, engagement, and retention of people living with HIV and co-occurring mental health and substance use disorders. AIDS Care 2004. 10.1080/09540120412331315286. [DOI] [PubMed] [Google Scholar]
- 18.Yehia BR, Stewart L, Momplaisir F, et al. Barriers and facilitators to patient retention in HIV care. BMC Infect Dis 2015;15(1):246. 10.1186/s12879-015-0990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care. AIDS 2012;26(16):2059–67. 10.1097/QAD.0b013e3283578b9b. [DOI] [PubMed] [Google Scholar]
- 20.Nelson JA, Kinder A, Johnson AS, et al. Differences in selected HIV care continuum outcomes among people residing in rural, urban, and metropolitan areas-28 US jurisdictions. J Rural Health 2018;34(1):63–70. 10.1111/jrh.12208. [DOI] [PubMed] [Google Scholar]
- 21.Sangaramoorthy T, Jamison AM, Dyer TV. HIV stigma, retention in care, and adherence among older black women living with HIV. J Assoc Nurses AIDS Care 2017. 10.1016/j.jana.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Higa DH, Marks G, Crepaz N, Liau A, Lyles CM. Interventions to improve retention in hiv primary care: a systematic review of U.S. studies. Curr HIV/AIDS Rep 2012;9(4):313–25. 10.1007/s11904-012-0136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis 2013;57(8):1164–71. 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 24.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA 2019;321(9):844–5. 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 25.Greenberg AE, Hader SL, Masur H, Young AT, Skillicorn J, Dieffenbach CW. Fighting HIV/AIDS in washington, D.C. Health Aff 2009;28(6):1677–87. 10.1377/hlthaff.28.6.1677. [DOI] [PubMed] [Google Scholar]
- 26.Walensky RP, Paltiel AD, Losina E, et al. Test and treat DC: forecasting the impact of a comprehensive HIV strategy in Washington DC. Clin Infect Dis 2010;51(4):392–400. 10.1086/655130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for disease control and prevention 2019. Diagnoses of HIV infection in the United States and dependent areas, 2018 HIV surveillance report. HIV Surveill Rep 30:1–129. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-vol-30.pdf. Accessed 16 Mar 2020. [Google Scholar]
- 28.District of Columbia Department of Health HIV/AIDS, Hepatitis, STD and Tuberculosis Administration (HAHSTA) 2020 Annual epidemiology and surveillance report data through December 2020, Washington DC. [Google Scholar]
- 29.Castel AD, Greenberg AE, Befus M, et al. Temporal association between expanded HIV testing and improvements in population-based HIV/AIDS clinical outcomes, district of Columbia. AIDS Care 2014;26(6):785–9. 10.1080/09540121.2013.855296. [DOI] [PubMed] [Google Scholar]
- 30.Castel AD, Magnus M, Peterson J, et al. Implementing a novel citywide rapid HIV testing campaign in Washington, D.C.: findings and lessons learned. Public Health Rep 2012;127(4):422–31. 10.1177/003335491212700410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saafir-Callaway B, Castel AD, Lago L, et al. Longitudinal outcomes of HIV- infected persons re-engaged in care using a community-based re-engagement approach. AIDS Care 2019. 10.1080/09540121.2019.1619662. [DOI] [PubMed] [Google Scholar]
- 32.Jain KM, Maulsby C, Kinsky S, Charles V, Holtgrave DR, PC Implementation Team. 2015–2020 national HIV/AIDS strategy goals for HIV linkage and retention in care: recommendations from program implementers. Am J Public Health 2016;106(3):399–401. 10.2105/AJPH.2015.302995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tobias C, Cunningham WE, Cunningham CO, Pounds MB. Making the connection: the importance of engagement and retention in HIV medical care. AIDS Patient Care STDS 2007;21(s1):S3–8. 10.1089/apc.2007.9992. [DOI] [PubMed] [Google Scholar]
- 34.Castel AD, Tang W, Peterson J, et al. Sorting through the lost and found: are patient perceptions of engagement in care consistent with standard continuum of care measures? J Acquir Immune Defic Syndr 2015;6:S44–55. 10.1097/QAI.0000000000000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Health research services administration (HRSA) [8 Jan 2020];HIV care continuum. 2020 https://hab.hrsa.gov/about-ryan-white-hivaids-program/hiv-care-continuum. Accessed.
- 36.Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- 37.Glaser BG, Strauss AL 2009. The discovery of grounded theory: strategies for qualitative research Transaction Publishers; http://books.google.com/books?hl=en&lr=&id=rtiNK68Xt08C&pgis=1. Accessed 20 Apr 2015 [Google Scholar]
- 38.Miles MB, Huberman AM, Saldana J. Qualitative data analysis: a methods sourcebook 3rd ed. Newbury Park, CA: Sage Publications; 2014. [Google Scholar]
- 39.Zelenev A, Marcus R, Kopelev A, et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS Behav 2013. 10.1007/s10461-013-0472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zaller ND, Holmes L, Dyl AC, et al. Linkage to treatment and supportive services among HIV-positive ex-offenders in project bridge. J Health Care Poor Underserved 2008;19(2):522–31. 10.1353/hpu.0.0030. [DOI] [PubMed] [Google Scholar]
- 41.Williams CT, Kim S, Meyer J, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav 2013. 10.1007/s10461-012-0391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haley DF, Golin CE, Farel CE, et al. Multilevel challenges to engagement in HIV care after prison release: a theory-informed qualitative study comparing prisoners’ perspectives before and after community reentry. BMC Public Health 2014;14(1):1253. 10.1186/1471-2458-14-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Remien RH, Bauman LJ, Mantell JE, et al. Barriers and facilitators to engagement of vulnerable populations in HIV primary care in New York city. J Acquir Immune Defic Syndr 2015;69:S16–24. 10.1097/QAI.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Magnus M, Herwehe J, Murtaza-Rossini M, et al. Linking and retaining HIV patients in care: the importance of provider attitudes and behaviors. AIDS Patient Care STDS 2013;27(5):297–303. 10.1089/apc.2012.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mallinson RK, Rajabiun S, Coleman S. The provider role in client engagement in HIV care. AIDS Patient Care STDS 2007. 10.1089/apc.2007.9984. [DOI] [PubMed] [Google Scholar]
- 46.Rajabiun S, Mallinson RK, McCoy K, et al. “Getting me back on track”: the role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical care. AIDS Patient Care STDS 2007. 10.1089/apc.2007.9990. [DOI] [PubMed] [Google Scholar]
- 47.McDoom MM, Bokhour B, Sullivan M, Drainoni M-L. How older black women perceive the effects of stigma and social support on engagement in HIV care. AIDS Patient Care STDS 2015;29(2):95–101. 10.1089/apc.2014.0184. [DOI] [PubMed] [Google Scholar]
- 48.George S, Garth B, Wohl AR, Galvan FH, Garland W, Myers HF. Sources and types of social support that influence engagement in HIV care among Latinos and African Americans. J Health Care Poor Underserved 2009;20(4):1012–35. 10.1353/hpu.0.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Farber EW, Shahane AA, Brown JL, Campos PE. Perceived stigma reductions following participation in mental health services integrated within community-based HIV primary care. AIDS Care 2014;26(6):750–3. 10.1080/09540121.2013.845285. [DOI] [PubMed] [Google Scholar]
- 50.Irvine MK, Chamberlin SA, Robbins RS, Kulkarni SG, Robertson MKM, Nash D. Come as you are: improving care engagement and viral load suppression among HIV care coordination clients with lower mental health functioning, unstable housing, and hard drug use. AIDS Behav 2017;21(6):1572–9. 10.1007/s10461-016-1460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Basta T, Shacham E, Reece M. Psychological distress and engagement in HIV-related services among individuals seeking mental health care. AIDS Care 2008;20(8):969–76. 10.1080/09540120701767240. [DOI] [PubMed] [Google Scholar]
- 52.Levy ME, Monroe AK, Horberg MA, et al. Pharmacologic treatment of psychiatric disorders and time with unsuppressed HIV viral load in a clinical HIV cohort. JAIDS J Acquir Immune Defic Syndr 2019;82(3):329–41. 10.1097/QAI.0000000000002138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mugavero M, Ostermann J, Whetten K, et al. Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care STDS 2006;20(6):418–28. 10.1089/apc.2006.20.418. [DOI] [PubMed] [Google Scholar]
- 54.Willie TC, Overstreet NM, Sullivan TP, Sikkema KJ, Hansen NB. Barriers to HIV medication adherence: examining distinct anxiety and depression symptoms among women living with HIV who experienced childhood sexual abuse. Behav Med 2016;42(2):120–7. 10.1080/08964289.2015.1045823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Messer LC, Quinlivan EB, Parnell H, et al. Barriers and facilitators to testing, treatment entry, and engagement in care by HIV-positive women of color. AIDS Patient Care STDS 2013;27(7):398–407. 10.1089/apc.2012.0435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.U.S. Department of Health and Human Services, health resources and services administration Bureau of Primary Health Care 2017. Integrating HIV care, treatment and prevention services into primary care—a toolkit for health centers Rockville, MD. [Google Scholar]
- 57.Meyerson B, Chu BC, Mills MV. State agency policy and program coordination in response to the co-occurrence of HIV, chemical dependency, and mental illness. Public Health Rep 2003;118(5):408–14. 10.1093/phr/118.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Soto TA, Bell J, Pillen MB. Literature on integrated HIV care: a review. AIDS Care 2004. 10.1080/09540120412331315295. [DOI] [PubMed] [Google Scholar]
- 59.Chuah FLH, Haldane VE, Cervero-Liceras F, et al. Interventions and approaches to integrating HIV and mental health services: a systematic review. Health Policy Plan 2017. 10.1093/heapol/czw169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.El-Bassel N, Gilbert L, Witte S, Wu E, Hunt T, Remien RH. Couple-based HIV prevention in the United States: advantages, gaps, and future directions. J Acquir Immune Defic Syndr 2010;55(Suppl 2):S98–101. 10.1097/QAI.0b013e3181fbf407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Remien RH, Stirratt MJ, Nguyen N, Robbins RN, Pala AN, Mellins CA. Mental health and HIV/AIDS. AIDS 2019;33(9):1411–20. 10.1097/QAD.0000000000002227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Maulsby C, Enobun B, Batey DS, et al. A mixed-methods exploration of the needs of people living with HIV (PLWH) enrolled in access to care, a national HIV linkage, retention and re-engagement in medical care program. AIDS Behav 2018;22(3):819–28. 10.1007/s10461-017-1809-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nijhawan AE, Liang Y, Vysyaraju K, et al. Missed initial medical visits: predictors, timing, and implications for retention in HIV care. AIDS Patient Care STDS 2017;31(5):213–21. 10.1089/apc.2017.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Park E, Stockman JK, Thrift B, Nicole A, Smith LR. Structural barriers to women’s sustained engagement in HIV care in southern California. AIDS Behav 2020;24(10):2966–74. 10.1007/s10461-020-02847-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dasgupta S, Oster AM, Li J, Hall HI. Disparities in consistent retention in HIV care–11 states and the district of columbia 2011–2013. MMWR Morb Mortal Wkly Rep 2016;65(4):77–82. 10.15585/mmwr.mm6504a2. [DOI] [PubMed] [Google Scholar]
- 66.Conyers LM, Richardson LA, Datti PA, Koch LC, Misrok M. A critical review of health, social, and prevention outcomes associated with employment for people living with HIV. AIDS Educ Prev 2017;29(5):475–90. 10.1521/aeap.2017.29.5.475. [DOI] [PubMed] [Google Scholar]
- 67.Kalichman SC, Hernandez D, Kegler C, Cherry C, Kalichman MO, Grebler T. Dimensions of poverty and health outcomes among people living with HIV infection: limited resources and competing needs. J Community Health 2015;40(4):702–8. 10.1007/s10900-014-9988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goswami ND, Schmitz MM, Sanchez T, et al. Understanding local spatial variation along the care continuum: the potential impact of transportation vulnerability on HIV linkage to care and viral suppression in high-poverty areas, Atlanta, Georgia. J Acquir Immune Defic Syndr 2016;72(1):65–72. 10.1097/QAI.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health 2013;38(5):976–93. 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sagrestano LM, Clay J, Finerman R, Gooch J, Rapino M. Transportation vulnerability as a barrier to service utilization for HIV-positive individuals. AIDS Care 2014;26(3):314–9. 10.1080/09540121.2013.819403. [DOI] [PubMed] [Google Scholar]
- 71.Tomer A, Kneebone E, Puentes R, Berube A 2011. Missed opportunity: transit and jobs in metropolitan America Washington, DC: https://www.brookings.edu/research/missed-opportunity-transit-and-jobs-in-metropolitan-america/. Accessed 8 Jan 2020. [Google Scholar]
- 72.Eberhart MG, Yehia BR, Hillier A, et al. Individual and community factors associated with geographic clusters of poor HIV care retention and poor viral suppression. J Acquir Immune Defic Syndr 2015;69:S37–43. 10.1097/QAI.0000000000000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dillingham R, Ingersoll K, Flickinger TE, et al. Positive links: a mobile health intervention for retention in HIV care and clinical outcomes with 12-month follow-up. AIDS Patient Care STDS 2018;32(6):241–50. 10.1089/apc.2017.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Rana AI, van den Berg JJ, Lamy E, Beckwith CG. Using a mobile health intervention to support HIV treatment adherence and retention among patients at risk for disengaging with care. AIDS Patient Care STDS 2016;30(4):178–84. 10.1089/apc.2016.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


