Abstract
Objectives:
To examine whether increased socioeconomic disadvantage, indexed using a measure of community distress, is associated with variation in caregiver-reported early childhood sleep patterns and problems in a large US sample using a mobile health application (app).
Design:
Cross-sectional.
Setting:
Data were collected using the free, publicly available Johnson’s Bedtime© baby sleep app.
Participants:
A total of 14,980 caregivers (85.1% mothers) of children ages 6 to 35.9 months (M = 13.88 months; 52.6% boys) participated in this study.
Measures:
Caregivers reported on child sleep using the Brief Infant Sleep Questionnaire-Revised. Socioeconomic disadvantage was indexed by zip code using the Distressed Communities Index (DCI), which combines seven US census indicators of socioeconomic disadvantage. DCI scores range from prosperous (lowest quintile) to distressed (highest quintile).
Results:
Socioeconomic disadvantage was significantly associated with later bedtimes, longer sleep onset latency, and shorter nighttime and 24-hour (total) sleep duration, with children living in distressed communities showing the poorest sleep. However, caregivers living in distressed communities reported a significantly lower prevalence of overall child sleep problems (43% vs 58% in prosperous communities), and more confidence in managing child sleep (42% vs 34% in prosperous communities).
Conclusions:
Children living in the most distressed communities have the poorest reported sleep patterns and bedtime behaviors, however their caregivers are less likely to report problematic child sleep. These findings highlight the need for community-level sleep health promotion interventions, as well as further investigation of caregiver perceptions about child sleep and sleep health promotion among families living in socioeconomically disadvantaged contexts.
Keywords: Socioeconomic disadvantage, infants, sleep, toddlers
Introduction
Early childhood is both a critical period for promoting healthy child development1 and a period of significant sleep problems,2 including frequent night awakenings, prolonged sleep onset latency, and insufficient sleep. Sleep problems impact 20–30% of young children and are associated with subsequent neurocognitive,3 socio-emotional,4 and physical health outcomes,5 underscoring the importance of understanding factors linked to the development of sleep problems in infancy and toddlerhood. A number of studies have found that family factors, such as parent behaviors and/or presence at bedtime,6 parent-child interactions,7 and parent cognitions,8,9 are associated with early childhood sleep patterns and problems.
Research has also demonstrated that in addition to notable racial/ethnic disparities,10 there are significant socioeconomic disparities in sleep patterns and problems in childhood, with children of lower socioeconomic status (SES) backgrounds having poorer sleep behaviors and outcomes.11–15 Previous research has examined various proximal, family-level indicators of SES, such as caregiver educational attainment, household income, and occupation, or more distal indicators of SES at the neighborhood level. At the family level, controlling for racial/ethnic background, preschoolers of mothers with lower educational attainment are less likely to exhibit positive sleep health behaviors, such as having a consistent bedtime routine.12 Both lower maternal education and lower family income have also been linked to shorter sleep duration longitudinally, from 6 months to 7 years of age.14 In addition, decreased caregiver social capital, or fewer connections with individuals who hold prestigious occupations, has been associated with caregiver-report of a prolonged child sleep onset latency and frequent night awakenings.16
Although there are fewer studies conducted with young children,17 a variety of neighborhood-level factors have been examined in relation to pediatric sleep. Such neighborhood factors include the ambient environment (e.g., light, noise),18 the built environment (e.g., population density),19 the social context (e.g., perceptions of safety or social cohesion),20,21 and the neighborhood poverty rate.11,22 Several studies of early childhood sleep have used United States (US) census-derived or other administrative data to construct indexes of neighborhood SES. In a study of Black three-month-old infants, greater neighborhood deprivation scores (percentage of households below the poverty level, households receiving nutritional assistance, residents without a high school diploma, and female-headed households with children under age 18 years) was associated with greater actigraphy-derived infant night awakenings, controlling for family-level maternal education and poverty.23 In a study of kindergarteners, greater neighborhood disadvantage, based on US census variables (percentage of residents without a high school diploma, unemployment rate, etc.), was linked to later bedtimes and accounted for a proportion of the significant racial/ethnic sleep disparities found in the sample.24 In a Canadian sample, an index of administratively-based neighborhood deprivation variables (percentage of lower-income and lower-education residents, unemployed adults, single-parent households, etc.) was indirectly associated with shorter stretches of caregiver-reported infant sleep, through a link with increased neighborhood disorder and diminished caregiver-rated neighborhood safety.25
Research to date linking lower family- and neighborhood-level SES to poor child sleep has primarily focused on caregiver-reported or actigraphy-derived child sleep patterns, such as total sleep duration or insufficient sleep, sleep onset latency, and night awakenings. Interestingly, there is little available research on whether SES is associated with a caregiver-perceived child sleep problem (i.e., whether the parent considers the child’s sleep to be a problem), with mixed findings. One study of young children found that mothers with lower levels of educational attainment were less likely to report child difficulty falling asleep.26 By contrast, another study found that increased exposure to socio-demographic risk factors, including lower maternal education and family income, was associated with greater caregiver-reported insomnia symptoms in preschoolers, although the overall rate of caregiver-identified sleep problems was lower (15%) than other studies.15 In line with these latter findings, large-scale research indicates that, beginning in preschool, diagnosed sleep disorders are more common among children from lower-SES neighborhoods compared to those from higher-SES neighborhoods.27 Qualitative research suggests that caregivers of lower SES backgrounds may have less available information about recommended early childhood sleep health guidelines (e.g., duration), which could contribute to differences by SES in caregiver-perceived child sleep problems.28,29
Additional information about variation by SES in caregiver-reported early childhood sleep patterns (e.g., sleep duration, sleep onset latency, night awakenings) as well as behaviorally-based, caregiver-perceived sleep problems, is necessary to better understand how caregiver perceptions about child sleep may differ according to culture and context.30 This information is particularly important given that caregiver report is critical for identifying and treating behavioral sleep problems in childhood,31 and caregiver-reported child sleep problems that begin in infancy can persist through middle childhood and adversely impact child development.32 Information about variation by SES in caregiver perceptions of early childhood sleep problems can also inform targeted efforts concentrated on families of the highest socioeconomic need, an approach recommended to address prevalent sleep health disparities and the downstream consequences of poor sleep for broader disparities in health and wellbeing.33
The current study
The objective of this study was to examine variation in caregiver-reported infant and toddler sleep patterns and sleep problems by SES in a large US sample, using data drawn from a free and publicly available mobile health application (app), the Johnson’s® Bedtime® app. We hypothesized that, in line with previous research,19,20,23–25 increased socioeconomic disadvantage, indexed by a Distressed Communities Index (DCI) score rank, would be associated with poorer caregiver-reported child sleep patterns (e.g., later bedtimes, increased sleep onset latency, decreased sleep consolidation, shorter nighttime and total [24-hours] sleep duration) and less consistent bedtime routines. We also hypothesized that increased socioeconomic disadvantage would be linked to fewer caregiver-perceived child sleep problems.26
Methods
Participants
Caregivers (85.1% mothers) of 14,980 infants and toddlers ages 6 to 35.9 months (M = 13.88; SD = 7.49) participated in this study. Only US-based app users were included given that the SES variable is based on US census data drawn from zip codes. Participant sociodemographic information is presented in Table 1.
Table 1.
Socio-demographic and descriptive information.
| Variable | Mean (SD) | % (n) |
|---|---|---|
| Child age (months; range = 6.0–35.9) | 13.88 (7.49) | |
| Child male sex | 52.6 (7880) | |
| Caregiver age (years; range = 18–75) | 29.07 (6.92) | |
| Caregiver: mother | 85.1 (12744) | |
| Father | 4.5 (669) | |
| Grandparent | 1.9 (283) | |
| Babysitter/nanny/au pair | 0.7 (107) | |
| Other guardian | 7.8 (1177) | |
| DCI Quintile: distressed | 15.7 (2351) | |
| At-risk | 18.5 (2772) | |
| Mid-tier | 19.1 (2855) | |
| Comfortable | 21.3 (3184) | |
| Prosperous | 25.5 (3818) | |
| Sleeps in caregivers’ room or bed | 60.2 (9023) | |
| Bedtime | 20:45 (70 minutes) | |
| Sleep onset latency (minutes) | 39.49 (31.07) | |
| Night awakening frequency | 2.14 (1.38) | |
| Night awakening duration (minutes) | 45.71 (49.62) | |
| Longest stretch asleep (hours) | 6.38 (3.05) | |
| Nighttime sleep duration (hours) | 9.17 (1.87) | |
| Nap duration (minutes) | 147.67 (65.12) | |
| Total (24-hour) sleep duration (hours) | 11.54 (2.04) | |
| Bedtime routine ≥5 nights/week | 56.5 (8474) | |
| Child sleep problem | 51.7 (7739) | |
| Child bedtime resistance | 42.4 (6345) | |
| Caregiver is confident managing child sleep | 37.5 (5624) | |
| Child sleep negatively affects caregiver sleep | 65.1 (9747) |
Note. DCI = distressed communities index.
Procedure
Cross-sectional data were collected from the Johnson’s® Bedtime® baby sleep app, a free and publicly available app offering sleep education and management for young children. Real-world data collected via the baby sleep app have been published previously in research on infant and toddler sleep.34,35 The app includes an optional assessment of sleep using the Brief Infant Sleep Questionnaire—Revised (BISQ-R)35 to track childhood sleep as well as optional, tailored behavioral sleep recommendations via the Customized Sleep Profile (CSP), which has demonstrated effectiveness for improving child sleep problems.34,36 Although app users may download the app for assistance with early childhood sleep problems, many users report no child sleep problems.34
All data for this study were collected from naturally acquired participants’ first completion of the BISQ-R, prior to provision of CSP recommendations. Data were collected between August 2013 and September 2018. Participants provided informed consent for the use of their app data for research purposes. Caregivers were free to decline study participation and continue free use of the app. This study was approved by a university Institutional Review Board.
Measures
Brief Infant Sleep Questionnaire – Revised (BISQ-R).
The BISQ-R is a caregiver-report measure of infant and toddler sleep. The measure is based on the well-validated and widely used BISQ, which has shown good correspondence with actigraphy-derived sleep in early childhood37 and has been validated for use with young children between 6 and 36 months of age.38 The BISQ-R includes items related to the child sleep environment (e.g., sleep space, location, and arrangement) and patterns (e.g., bedtime [lights out time], sleep onset latency [minutes from bedtime until the child falls asleep], night awakening frequency and duration, wake time). Likert scales assess caregiver-perceived child sleep problems (e.g., bedtime resistance, overall sleep problem severity), bedtime routine frequency, whether the caregiver feels confident managing their child’s sleep, and whether their child’s sleep negatively affects the caregiver’s sleep. These outcomes were dichotomized according to previous research,30,32,34,39 with 1 reflecting: a bedtime routine 5 or more nights/week, moderate to severe bedtime resistance, a small to serious child sleep problem, somewhat to very confident managing the child’s sleep, and the child’s sleep impacting the caregiver’s sleep somewhat to very much.
Sociodemographic information.
Information collected included caregiver relationship to the child (e.g., mother, father, relative), child age, child sex, and family zip code.
Socioeconomic disadvantage.
Zip codes were linked to the Disadvantaged Communities Index (DCI) score for each child. Created by the Economic Innovation Group (www.eig.org/dci), the DCI score reflects seven community-level variables drawn from the US Census Bureau’s American Community Survey 5-Year Estimates and Business Patterns Datasets.40 The seven variables are: (1) percent of the population without a high school diploma or equivalent, (2) percent housing vacancy rate, (3) percent of the population ages 25–64 who are without work, (4) percent of the population living under the poverty line, (5) median income ratio as a percentage of the state’s median income, (6) percent change in the number of jobs from the previous Census period, and (7) percent change in the number of business establishments from the previous Census period. Zip codes are ranked on each of the 7 indicators, which are then averaged, normalized (0 – 100), and grouped into five quintiles from prosperous (lowest quintile; 1st quintile), comfortable (2nd), mid-tier (3rd), at-risk (4th), and distressed (5th quintile, or most distressed community).
The DCI contains many of same US census variables used in previous research examining pediatric sleep and SES (i.e., rate of poverty, residents without a high school diploma, and unemployment).11,20,23,24 In the creation of DCI scores, zip codes are ranked on each factor across the US, making this index particularly useful for examining SES in a sample comprised of different regions. Research on DCI score characteristics shows that individuals of Asian and non-Latinx white backgrounds are more likely to reside in prosperous communities, whereas those of Hispanic/Latinx, Black and American Indian/Alaska Native backgrounds are more likely to reside in at-risk and distressed communities.40 In addition, there is regional variation in the distribution of DCI scores, with prosperous communities being more prevalent in the West and distressed communities being more prevalent in the South.40 Previous studies have examined DCI quintiles in relation to adult health outcomes41 and as part of a cumulative risk index in a study of pediatric sleep.15
Statistical analyses
We used analysis of covariance (ANCOVA) models with post-hoc Bonferroni-adjusted contrasts to examine variation in continuous caregiver-reported child sleep outcomes by DCI quintile rank. Partial eta squared was used to estimate effect sizes in these analyses. For dichotomous sleep outcomes, we used logistic regression with comparisons by DCI quintile. In all analyses, the distressed quintile served as the reference group for quintile comparisons, and we covaried for child age, child sex, and whether children shared a bed or a room with a caregiver, as bed- and room-sharing is associated with caregiver-perceived child sleep patterns and problems,42 and differed across quintiles (see below). We also covaried for participants’ US region, given regional differences in the clustering of distressed quintile ranks,40 noted above. Due to the large sample size and number of analyses, a p-value of <.01 was considered statistically significant. Effect sizes are expressed in partial eta squared values for ANCOVA models and in odds ratios, converted to proportions to facilitate interpretation, for logistic regression models. To reflect clinical significance, we also express differences in sleep hours and minutes for relevant outcomes (e.g., sleep onset latency, nighttime sleep).
Results
Sleep outcomes and DCI distribution
Table 1 provides descriptive information for the sleep variables. Figure 1 shows the geographical distribution of DCI quintiles across the United States in the current sample. Overall, participants were relatively evenly distributed across the five DCI quintiles. A total of 25.5% lived in a prosperous community, 21.3% lived in a comfortable community, 19.1% in a mid-tier community, 18.5% in an at-risk community, and 15.7% in a distressed community. Although the sample was more advantaged (prosperous, comfortable, or mid-tier) overall, these data align with DCI quintile distribution across the US, with the majority of households residing in an advantaged quintile.40 A total of 37.2% of the sample (n = 5,578) resided in the Southern region of the US, 24.0% (n = 3,588) in the West, 22.1% (n = 3,310) in the Midwest, and 16.7% (n = 2,504) in the South.
Figure 1.
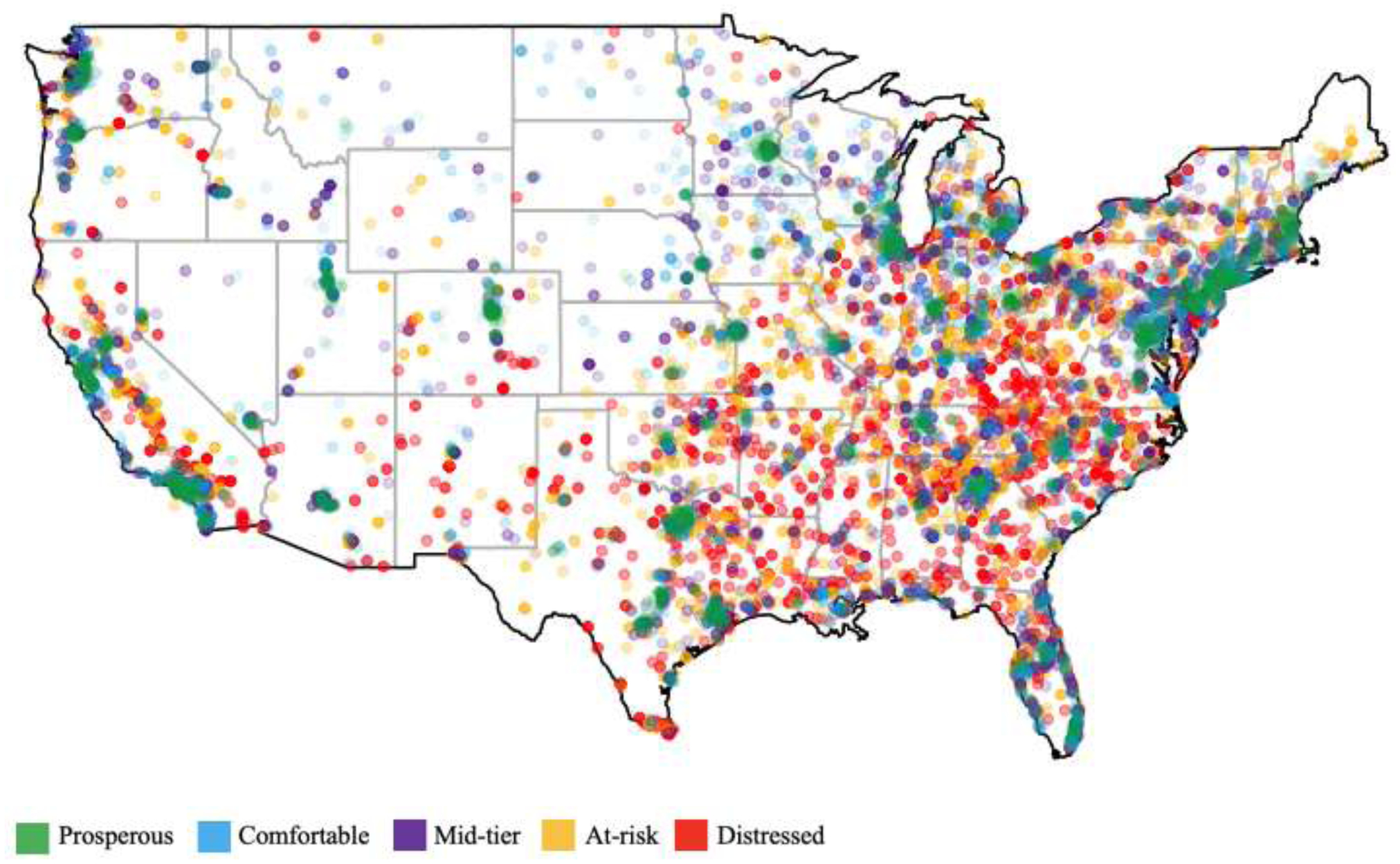
Distribution and density of DCI quintiles in the current sample.
Sleep arrangement by DCI quintiles
Overall, 60.2% of children shared a bed or a room with a caregiver, although this varied significantly by DCI quintile, χ2(4) = 340.82, p <.001. Across DCI quintile, bed- or room-sharing with a caregiver occurred in 51.2% of those living in a prosperous community, 56.3% of those in a comfortable community, 60.4% of those in a mid-tier community, 66.8% of those living in an at-risk community, and 72.2% of those living in a distressed community.
Caregiver-reported child sleep patterns by DCI quintiles
ANCOVA models showing variation in sleep patterns by DCI quintile are summarized in Table 2. Average bedtimes were progressively later as community disadvantage increased, such that children living in distressed communities evidenced the latest bedtimes (20:55) versus 20:33 in prosperous communities, p<.001 (Table 2 and Figure 2a). Post-hoc contrasts showed that bedtimes for children living in distressed communities were significantly later than in all other communities, by 6 minutes compared to those in at-risk communities (p = .007), by 8 minutes compared to mid-tier communities (p<.001), by 10 minutes compared to comfortable communities (p<.001), and by 22 minutes compared to prosperous communities (p<.001).
Table 2.
ANCOVA models for sleep pattern outcomes by DCI quintile rank
| Adjusted Mean (95% CI) | F (df) | p | ES | |||||
|---|---|---|---|---|---|---|---|---|
| DCI quintile | Prosperous | Comfortable | Mid-tier | At-risk | Distressed | |||
| Bedtime | 20:33 (20:31, 20:35) | 20:45 (20:43, 20:47) | 20:47 (20:45, 20:50) | 20:49 (20:46, 20:52) | 20:55 (20:53, 20:58) | 44.62 (4) | <.001 | .012 |
| Sleep onset latency (minutes) | 36.28 (35.30, 37.26) | 38.74 (37.66, 39.81) | 40.93a (39.79, 42.07) | 40.78a (39.61, 41.94) | 42.66 (41.38, 43.94) | 18.90 (4) | <.001 | .005 |
| NA frequency | 2.20 (2.16, 2.24) | 2.16 (2.12, 2.21) | 2.17 (2.12, 2.22) | 2.08a (2.03, 2.13) | 2.04 (1.99, 2.09) | 7.03 (4) | <.001 | .002 |
| NA duration | 43.40a (41.75, 45.05) | 43.19a (41.39, 45.00) | 47.88a (45.96, 49.80) | 48.86a (46.91, 50.81) | 46.63 (44.48, 48.78) | 7.57 (4) | <.001 | .002 |
| LSA (hours) | 6.30a (6.21, 6.39) | 6.30a (6.20, 6.40) | 6.36a (6.25, 6.46) | 6.50a (6.38, 6.61) | 6.53 (6.41, 6.65) | 3.65 (4) | .006 | .001 |
| Nighttime sleep duration (hours) | 9.44 (9.38, 9.50) | 9.21 (9.14, 9.27) | 9.10 (9.03, 9.17) | 9.06a (8.99, 9.14) | 8.91 (8.83, 8.98) | 32.84 (4) | <.001 | .009 |
| Total (24-hour) sleep duration (hours) | 11.78 (11.72, 11.85) | 11.61 (11.54, 11.68) | 11.49 (11.41, 11.56) | 11.42a (11.35, 11.50) | 11.29 (11.20, 11.37) | 23.98 (4) | <.001 | .007 |
Note.
= Not statistically different from distressed quintile. NA = night awakening; LSA = longest stretch asleep. DCI = distressed communities index. Analyses covaried for child age, sex, whether the child slept in the caregiver’s room and/or bed, and US region.
Figures 2a–2d.
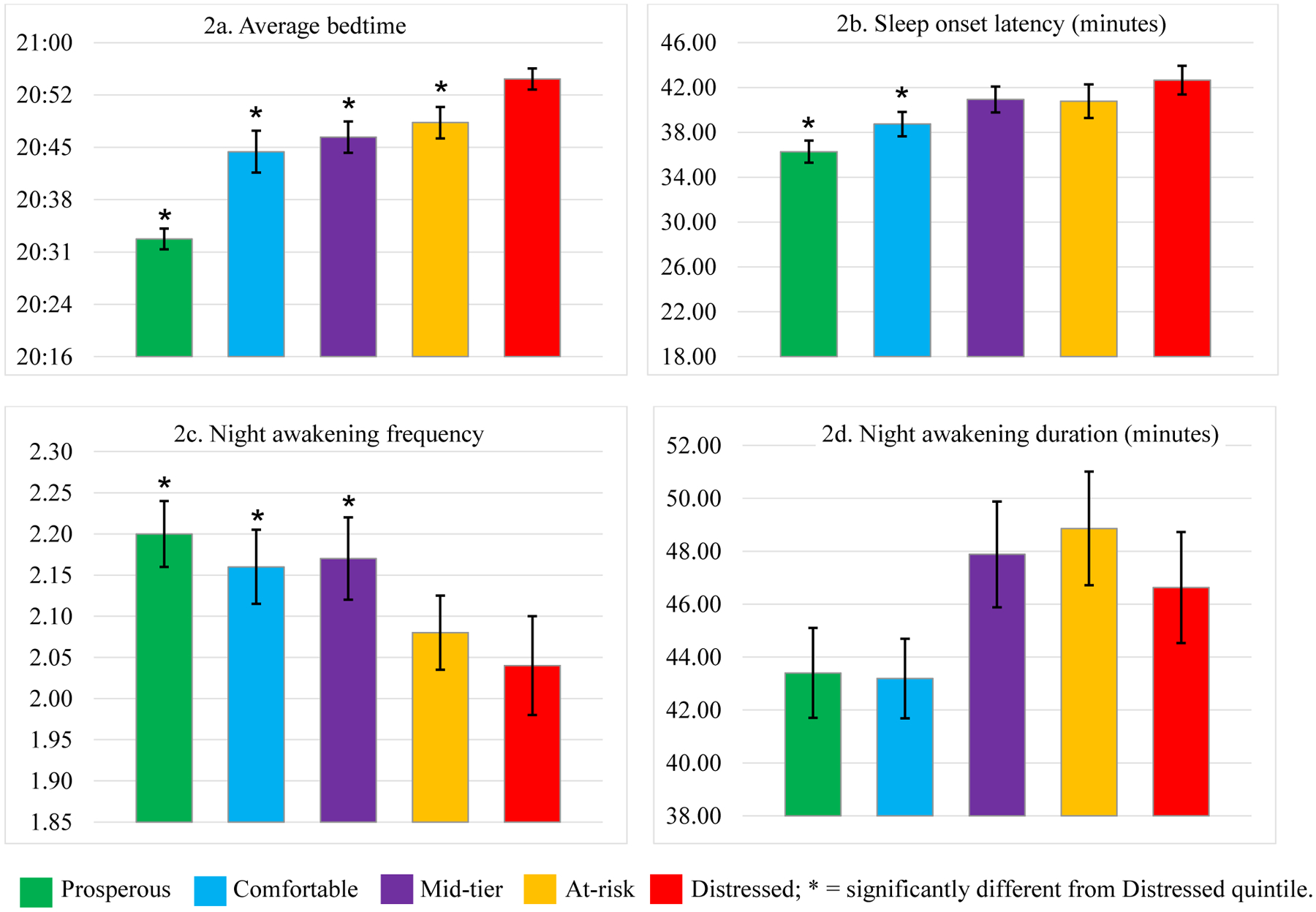
Sleep patterns by DCI quintile.
Average sleep onset latency (SOL) was generally longer with increased community disadvantage (p<.001, Table 2 and Figure 2b), and children in distressed communities had a significantly longer average SOL (42.66 minutes) compared to children in comfortable (38.74 minutes, p<.001), by about 4 minutes, and compared to those in prosperous communities (36.28 minutes, p<.001), by about 6.5 minutes. However, the average SOL for children in mid-tier communities (40.93 minutes) and those in at-risk communities (40.78 minutes) did not significantly differ from those in distressed communities.
Variables reflecting nighttime sleep consolidation, including night awakening frequency (Figure 2c) and duration (Figure 2d), as well as longest stretch asleep (Figure 2e), varied by DCI quintile, but the pattern of results was mixed across outcomes (Table 2). There was a linear association between night awakening frequency and DCI quintile (p<.001), with post-hoc contrasts showing that children in distressed communities had significantly fewer awakenings (2.04) than those in prosperous (2.20, p<.001), comfortable, and mid-tier communities, but not those in at-risk communities (2.08). Although overall night awakening duration varied significantly by DCI quintile (p<.001), children in distressed communities did not show the longest night awakening duration (46.63 minutes) and did not significantly differ from any other DCI quintile in post-hoc comparisons. Longest stretch of child sleep similarly showed overall variability by DCI quintile (p =.006), as well as a linear pattern of decreasing stretches of sleep with each increase in DCI quintile (6.53 hours in distressed communities versus 6.30 hours in prosperous communities, an overall difference of about 14 minutes). However, post-hoc contrasts indicated no significant differences between the distressed quintile and any of the other quintiles.
Figures 2e–2g.
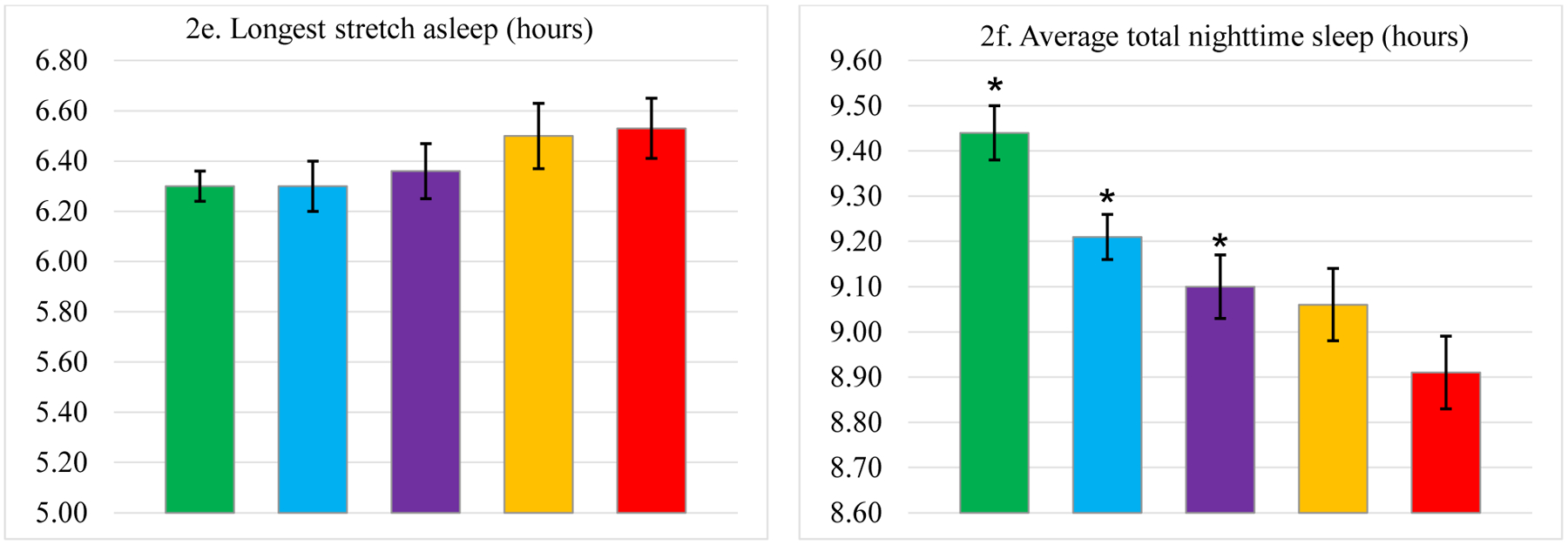
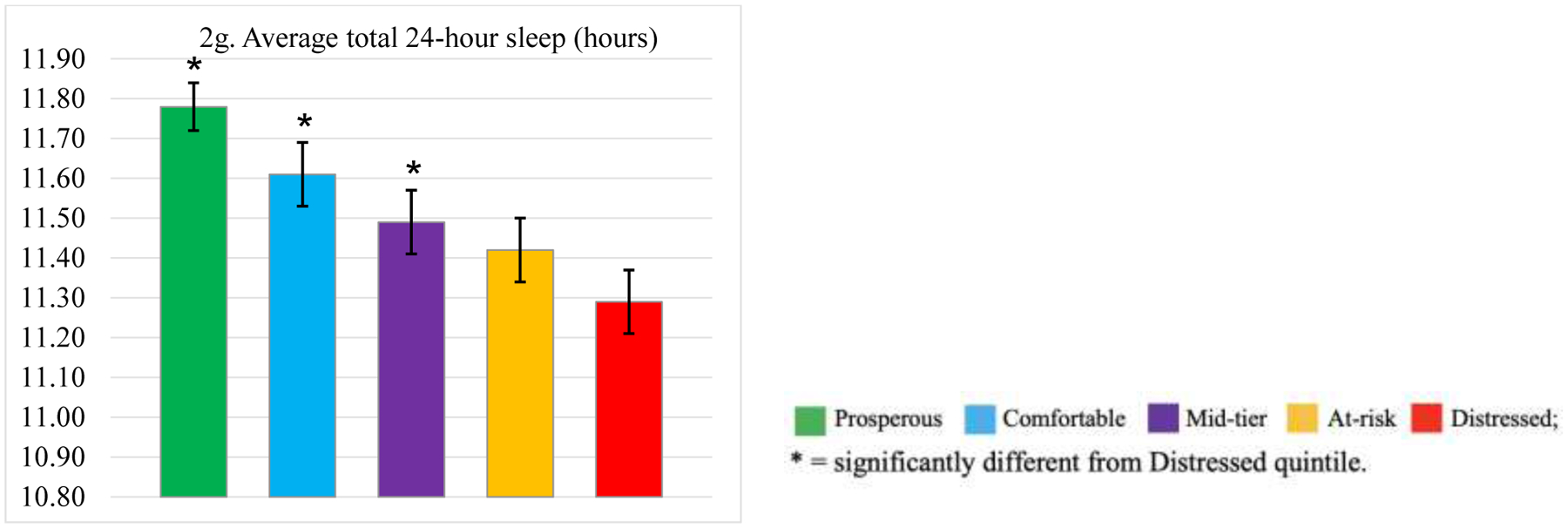
Sleep patterns by DCI quintile.
Increased levels of community disadvantage were associated with both reduced total nighttime sleep (Figure 2f) and total (24-hour) sleep duration (Figure 2g) in a linear fashion (p<.001, Table 2). Post-hoc contrasts showed that children in distressed communities had significantly shorter nighttime sleep (8.91 hours) compared to those in all other quintiles except those in the at-risk quintile (9.06 hours; difference of 9 minutes). Those in distressed communities had shorter nighttime sleep by about 32 minutes compared to those in prosperous communities (9.44 hours; p<.001), 18 minutes compared to those in comfortable communities (9.21 hours; p<.001), and 11 minutes compared to those in mid-tier communities (9.10 hours; p=.004). Post-hoc contrasts for total (24-hour) sleep duration followed a similar pattern, with children in distressed communities showing significantly shorter total sleep (11.29 hours) compared to those in all other DCI quintiles except for the at-risk quintile (11.42 hours; difference of about 8 minutes). Total sleep duration for children in distressed communities was shorter by about 29 minutes compared to those in prosperous communities (11.78 hours; p<.001), 19 minutes compared to those in comfortable communities (11.61 hours; p<.001), and 12 minutes compared to those in mid-tier communities (11.49; p =.007).
Overall, DCI score rank accounted for a small amount of the variance in these models, with partial eta squared effect sizes ranging from 0.1% (longest stretch of child sleep) to 1.2% (bedtime) of the variance (Table 2).
Caregiver behaviors and perceived sleep problems by DCI quintiles
Logistic regression models showing variation in caregiver-perceived child sleep behaviors and problems by DCI quintile are summarized in Table 3. Consistent bedtime routine implementation (Figure 3a) declined with each increased community disadvantage in a linear fashion, with children in distressed communities having the lowest prevalence of consistent bedtime routine implementation (49.1% versus 63.0% in a prosperous community; p<.001). In comparison to those in the distressed quintile, children in all other quintiles had significantly higher odds of having a consistent bedtime routine, by 53% (p<.001) for those in a prosperous community, 29% (p<.001) for those in a comfortable community, 17% (p =.006) for those in a mid-tier community, and 17% (p=.007) for those in an at-risk community (Table 3).
Table 3.
Logistic regression models for caregiver-perceived child sleep problems by DCI quintile rank
| % (n) | |||||||
|---|---|---|---|---|---|---|---|
| Adjusted Odds Ratio (95% CI) | χ2 (df) | p | |||||
| DCI quintile | Prosperous | Comfortable | Mid-tier | At-risk | Distressed | ||
| Bedtime routine ≥5 nights/week |
63.0% (2404) 1.53 (1.37, 1.71) |
58.2% (1852) 1.29 (1.16, 1.44) |
54.9% (1568) 1.17 (1.04, 1.30) |
53.9% (1495) 1.17 (1.05, 1.31) |
49.1% (1155) | 530.11 (10) | <.001 |
| Child bedtime resistance |
40.0% (1527) 0.94 (0.84, 1.04)a |
40.8% (1299) 0.94 (0.84, 1.05)a |
43.7% (1248) 1.02 (0.91, 1.14)a |
43.5% (1206) 0.98 (0.87, 1.09)a |
45.3% (1065) | 424.57 (10) | <.001 |
| Child sleep problem |
57.9% (2209) 1.86 (1.67, 2.06) |
54.4% (1731) 1.60 (1.43, 1.78) |
52.0% (1486) 1.46 (1.31, 1.64) |
47.3% (1311) 1.20 (1.07, 1.34) |
42.6% (1002) | 295.27 (10) | <.001 |
| Confident managing child sleep |
34.4% (1314) 0.69 (0.62, 0.77) |
35.9% (1142) 0.75 (0.67, 0.84) |
37.1% (1060) 0.80 (0.71, 0.89) |
40.7% (1128) 0.96 (0.85, 1.07)a |
41.7% (980) | 301.08 (10) | <.001 |
| Child sleep affects caregiver sleep |
68.3% (2606) 1.46 (1.30, 1.62) |
67.1% (2136) 1.36 (1.21, 1.52) |
65.9% (1882) 1.30 (1.16, 1.45) |
61.5% (1705) 1.05 (0.94, 1.18)a |
60.3% (1418) | 294.59 (10) | <001 |
Note.
= Not statistically different from distressed quintile. DCI = distressed communities index. Analyses covaried for child age, sex, whether the child slept in the caregiver’s room and/or bed, and US region.
Figures 3a–3e.
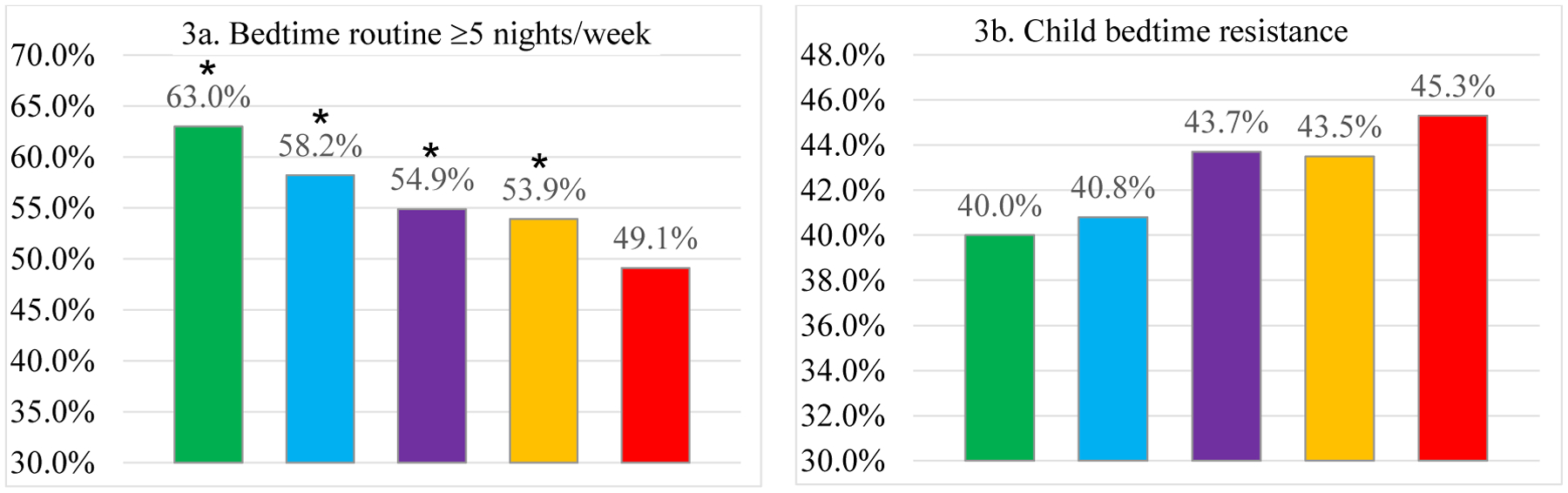
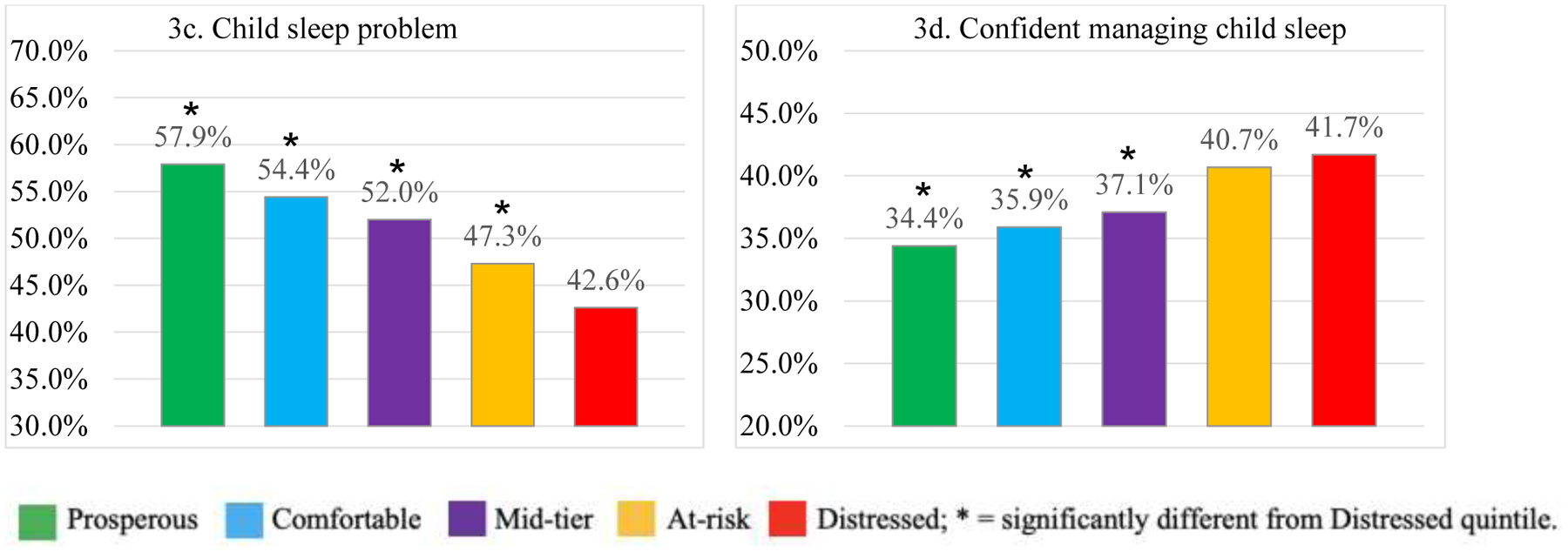
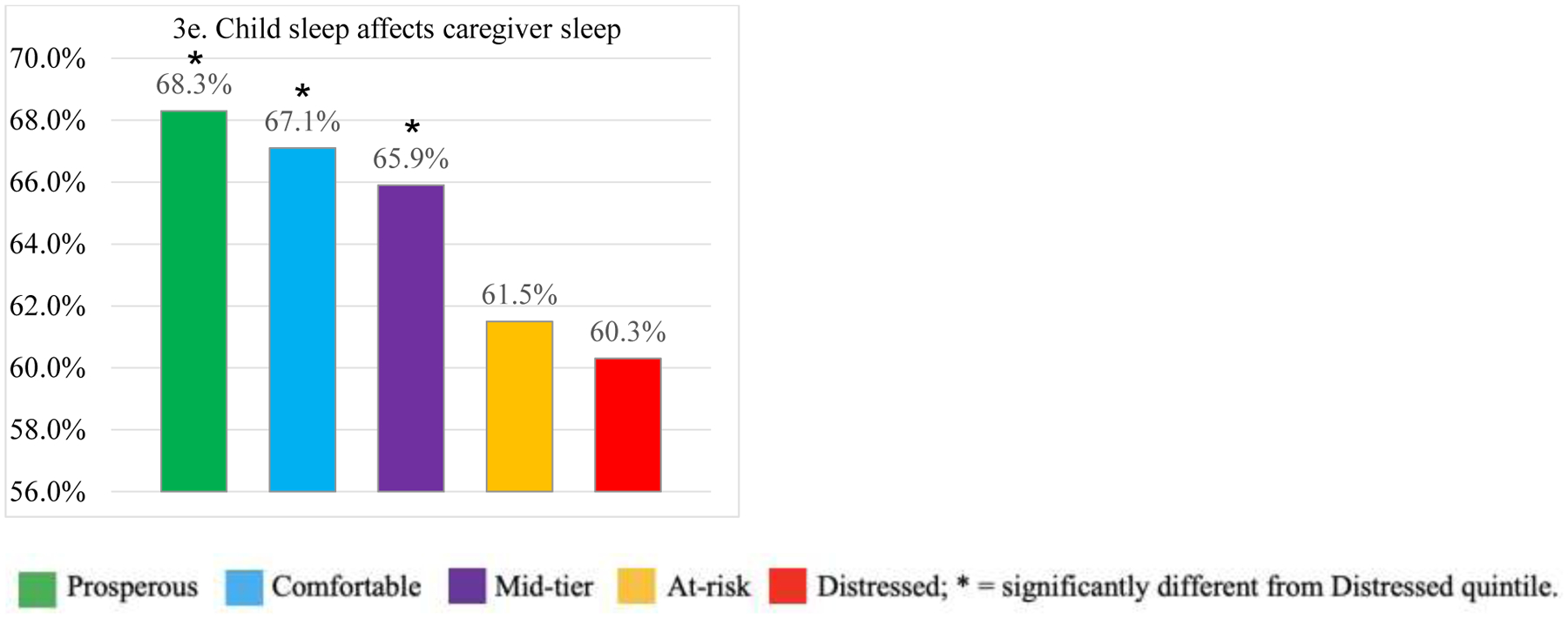
Sleep problems by DCI quintile.
The prevalence of a caregiver-perceived child sleep problems (Figure 3c) significantly decreased with greater community disadvantage, such that caregivers in the most distressed quintile reported the lowest prevalence of child sleep problems (42.6% versus 57.9% in prosperous communities, p<.001; Table 3). Compared to those in distressed communities, the odds of a child sleep problem were 86% higher for those in prosperous communities, 60% higher for those in comfortable communities, 46% higher for those in mid-tier communities, and 20% higher for those in at-risk communities (p values <.001, Table 3). In contrast, although the prevalence of child bedtime resistance significantly varied by DCI quintile (p<.001; Table 3, Figure 3b), with an increasing proportion of caregivers endorsing child bedtime resistance with each increase in community disadvantage level (45.3% in distressed communities versus 40.0% in prosperous communities), there were no significant differences in odds of child bedtime resistance for those in distressed communities compared to all other communities.
The proportion of caregivers endorsing confidence in managing child sleep increased as community disadvantage increased, in a linear fashion (34.4% in prosperous communities versus 41.7% in distressed communities, p<.001; Table 3, Figure 3d). Compared to those in distressed communities, the odds of a caregiver reporting confidence in managing child sleep was significantly lower by 31% for the prosperous quintile, 25% for the comfortable quintile, and 20% for the mid-tier quintile (p<.001), but not the at-risk quintile (4% lower odds, p>.01). The proportion of caregivers reporting that their child’s sleep negatively affects their own sleep linearly decreased as community disadvantage increased, from 68.3% in prosperous communities to 60.3% in distressed communities (p<.001; Table 3, Figure 3d). Compared to those in distressed communities, the odds of a caregiver reporting the negative impact of child sleep increased significantly by 46% for those in prosperous communities, 36% for those in comfortable communities, and 30% for those in mid-tier communities (p values <.001).
Discussion
In this study leveraging real-world data collected via a publicly available app, we found that residing in a lower-SES community, indexed via the Distressed Communities Index (DCI), is associated with poorer caregiver-reported child sleep patterns, including later bedtimes, longer sleep onset latencies, and shorter nighttime and total (24-hour) sleep duration. Although aspects of sleep consolidation (night awakening frequency and duration, longest stretch of child sleep) varied by the DCI quintile, the pattern of results was inconsistent, with longer stretches of sleep and less frequent awakenings in more distressed communities, but a generally increased duration of night awakenings. Caregivers in the distressed DCI quintile were also less likely to report consistent child bedtime routine implementation. Interestingly, caregivers in the most distressed communities reported fewer perceived sleep problems, as well increased caregiver confidence in managing their child’s sleep and a decreased likelihood that their child’s sleep negatively impacted their own sleep. Importantly, these collective findings are independent of caregiver-child bed- or room-sharing, which was more prevalent in distressed communities in this sample.
Although effect sizes in this study were small overall, differences between the most prosperous and the most distressed quintiles were still clinically meaningful for many outcomes. For instance, there was a 29-minute difference in sleep duration between the distressed and prosperous DCI quintiles and 10% fewer children with a caregiver-perceived sleep problem. Experimental sleep restriction research shows that a 27-minute extension in sleep duration is associated with significant improvements in daytime child behavioral functioning,43 and that toddlers who are nap-restricted struggle with emotion-regulation and problem-solving.44,45 It is also imperative to acknowledge that sleep deficits accumulate over time, meaning that a sleep curtailment of 30 minutes per night translates to a loss of 3.5 hours of sleep per week. These findings are especially meaningful from a population health perspective in light of the large and growing body of research highlighting the importance of a healthy sleep duration and other aspects of sleep health for buffering against later deleterious health disparities.33
Study findings are in line with results of previous research on early childhood sleep patterns and neighborhood SES,22,24,25 and with the possibility that increased neighborhood disadvantage could be representative of aspects of the ambient, built, and social neighborhood context that contribute to poor sleep outcomes.17 However, although this study did not include family-level socio-demographic variables, the DCI score may also reflect family-level differences in SES and related work schedules, childcare resources, and living conditions46 that in turn impact child sleep patterns and caregiver perceptions about sleep. For example, later child bedtimes and curtailed nighttime and total (24-hour) sleep duration among children living in more disadvantaged communities could be due to caregivers having inflexible, later, or shift work schedules as well as limited childcare availability. Qualitative studies have provided support for this hypothesis, with caregivers of young children from disadvantaged homes raising these issues as barriers to positive sleep routines28 and to addressing early childhood behavioral sleep problems.29 Living in a single female-headed household and household overcrowding are also more common in disadvantaged communities, and these factors have been associated with poorer sleep health behaviors (i.e., bedtime routine consistency, insufficient sleep) in early childhood.15
It could also be that DCI score is a proxy for family-level factors such as caregiver education, health literacy, and sleep knowledge, which are linked to variation in child sleep duration47 and healthy sleep behaviors.12,48 If caregivers living in distressed communities are less aware of healthy sleep recommendations, such as optimal child sleep duration,48 and the impact of poor sleep on child outcomes, then caregivers may be less likely to perceive certain sleep patterns as being problematic. Indeed, due to decreased awareness of the importance of healthy sleep at a population level, and especially among those experiencing health disparities, a workshop report from the National Institutes of Health highlighted the need for culturally-tailored sleep health interventions.33 If DCI quintiles are reflective of contextual stress, such as housing instability, community violence exposure, single caregiver households, limited economic resources, and household overcrowding, it could also be that caregivers in these communities are more focused on managing these issues than child bedtime resistance or night awakenings. For example, in a qualitative study of lower-SES, Black mothers of 3–6-month-olds, 0% endorsed an infant sleep problem, focusing instead on a number of other family, work, and school-related stressors as being barriers to high-quality maternal sleep and wellbeing.49
Unlike another study that found decreased actigraphy-defined overnight sleep consolidation with increased community disadvantage in a sample of 3-month-olds,23 sleep consolidation increased with increased community disadvantage, with longer stretches of child sleep and fewer night awakenings in more distressed communities, although these patterns were not linear. Our discrepant findings could be due to differences in both our measurement approach and the age of children in this study. It could be that caregiver reports of sleep consolidation only reflect awakenings in which the child signals and wakes the parent, and underestimate night awakenings in comparison to actigraphy- and video-derived sleep consolidation. Alternatively, it could be that caregivers in more prosperous communities are more likely to report awakenings. In addition, our study is limited to DCI score as an index of community disadvantage, whereas the previous study examined both community and family-level SES. As children in the present study were older, between 6 and 35.9 months of age, than those in the previous study, caregivers also could have grown more accustomed to environmental disruptions to overnight sleep. Future studies should compare caregiver-reported awakenings and those observed via actigraphy or video to better understand these findings.
This increased reported sleep consolidation by families in disadvantaged communities aligns with their report of fewer sleep problems, given that past studies have noted that caregiver-perceived sleep problems are more likely to be reported in association with night wakings.30 In addition, compared to the more advantaged communities, more caregivers in distressed communities reported confidence in managing child sleep, and fewer reported that child sleep negatively affects their own sleep. It may be that caregivers in more advantaged communities are more aware of healthy sleep guidelines and/or have unrealistic expectations about early childhood sleep consolidation,50 resulting in potential over-reporting of child sleep problems and less confidence in managing child sleep. It is also plausible that sleep disturbances are less concerning or impactful overall for caregivers who are room- or bed-sharing with their young child due to limited economic resources (fewer individual rooms or sleep spaces) because they have not yet attempted to have their child in a separate room or sleep space. However, our analyses covaried for room- and bed-sharing, underscoring the importance of examining factors beyond sleep arrangement that could be linked to variation in caregiver perceived child sleep problems.
Taken in the context of previous research linking family- or neighborhood-level SES with sleep problems, typically defined as problematic child sleep patterns (e.g., night awakenings, insufficient sleep),11,13,16 these findings highlight the importance of exploring both childhood sleep patterns and caregiver-perceived child sleep problems. Large-scale research demonstrates cross-cultural variation in caregiver perceived child sleep problems,30 but there is a paucity of research that compares caregiver definitions of and expectations about early childhood sleep patterns and problems within different levels of family and neighborhood SES and across caregivers of different racial, ethnic, and cultural backgrounds. Without accompanying information about family level income, racial/ethnic background, and cultural beliefs about sleep, we are unable to discern whether the observed differences in sleep outcomes by DCI quintiles could be attributable to these important factors. It should be noted, however, that as a result of current and historical discriminatory policies and practices (e.g., “redlining”), those of racial/ethnic minority backgrounds disproportionately experience socioeconomic disadvantage and live in lower-SES contexts, perpetuating health disparities.33,51 The inclusion of family and neighborhood SES has also attenuated associations between race/ethnicity and sleep outcomes in studies of children11,17,24 as well as in adults.51
Despite our limited information about family-level factors, with the need for future research that examines variation by both DCI and family-level income/SES indicators, study findings have implications for early childhood sleep health promotion and behavioral sleep interventions. These interventions rarely include families living in lower SES contexts or those of racial/ethnic minority backgrounds.52 An assessment of both caregiver-perceived child sleep problems as well as child sleep patterns, and whether such patterns are problematic for the family, will be critical in future sleep health promotion research that seeks to ameliorate early sleep health disparities. More importantly, there is a need for sleep health promotion efforts that are tailored to better address barriers to healthy sleep that families may face at multiple levels, especially at the broader community and socio-political context.29,33 Such multilevel approaches could address family-level sleep-related beliefs and behaviors while also making improvements at the community level to increase green space and tree canopy to reduce light and noise18 and partnering with policymakers to enact housing and healthcare access improvements that benefit sleep health.17,33
The findings from this study must be considered in light of its limitations, including the previously mentioned lack of family-level SES and other information. Our findings should be replicated with additional and more nuanced family and contextual information. Variables such as family income, race/ethnicity, cultural beliefs, family composition, education and health literacy, parenting behaviors, caregiver mood, and factors may interact with or independently contribute to child sleep outcomes. Future research using longitudinal data should also examine potential mechanisms linking SES and early childhood sleep outcomes, particularly as modifiable mechanisms could be a target of preventive interventions to promote population-level pediatric sleep health. Another limitation of this research is that a family’s residence in a particular DCI quintile may not be consistent with that family’s financial situation, as not all families of lower SES live in disadvantaged communities, and vice versa. It is notable, however, that the full spectrum of community contexts in the US, from prosperous to distressed, were represented in this study, as a suspected limitation noted in previous large-scale Internet-based studies is that the sample is likely reflective of more advantaged backgrounds. The DCI distribution of this study is also similar to that of the larger US population.40 Although we covaried for regional differences in the distribution of DCI quintiles throughout the US, this does not substitute for other family-level and other socio-cultural factors.
Furthermore, study findings are limited to app-using caregivers who self-select to use a mobile health platform for information about and support around child sleep. Finally, the use of data from a smartphone app could be considered a limitation, however smartphone ownership continues to increase across SES and racial/ethnic backgrounds, with 81% of Americans owning a smartphone.53 Smartphone apps are well-positioned to facilitate “crowd science,” which expands research participation to a large population of potential contributors.54 There are also a plethora of available apps for parenting and child health,55 with evidence of high engagement in and support of such apps among caregivers.56,57
Conclusions
Findings from this real-world study suggest that increased socioeconomic disadvantage is associated with poor early child sleep outcomes that are critical for optimal development, including later bedtimes, increased sleep onset latency, and decreased nighttime and total (24-hour) sleep duration. However, overall, caregivers from disadvantaged communities also endorsed fewer child sleep problems and more confidence in managing child sleep than families in more advantaged communities. These findings support the need for community-level sleep health promotion interventions, especially in the most disadvantaged neighborhoods. Furthermore, these results have important implications for pediatric providers in the assessment and promotion of sleep health, as there clearly is a need to focus on sleep outcomes, sleep-related behaviors, as well as caregiver-perceived sleep problems within the clinical setting. Furthermore, behavioral sleep intervention research will continue to focus primarily on families of non-Latinx white and higher SES backgrounds52 if inclusion criteria are solely based on broad caregiver perceptions of child sleep problems. To inform the development of culturally- and contextually-tailored sleep health promotion efforts that can effectively address sleep health disparities at multiple levels,33 research is needed to better understand variation in caregiver perceptions about and confidence related to child sleep patterns and problems by community context and across families of different socioeconomic, as well as racial, ethnic, and cultural, backgrounds.
Acknowledgments
We thank the Economic Innovation Group for the use of the Distressed Communities Index data. The findings expressed in this publication are solely those of the authors and not necessarily those of the Economic Innovation Group. The Economic Innovation Group does not guarantee the accuracy or reliability of, or necessarily agree with, the information provided herein.
Funding
This work was supported by Johnson & Johnson Consumer Inc., Skillman, NJ, USA. Dr. Williamson was supported by the Sleep Research Society Foundation and the Eunice Kennedy Shriver National Institute on Child Health and Human Development (K23HD94905).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement
Drs. Mindell and Leichman have served as consultants for Johnson & Johnson Consumer Inc. Drs. Gould and Walters are former employees of Johnson & Johnson Consumer Inc.
References
- 1.Black MM, Walker SP, Fernald LC, et al. Early childhood development coming of age: science through the life course. Lancet. 2017;389(10064):77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129(2):e276–e284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kocevska D, Rijlaarsdam J, Ghassabian A, et al. Early childhood sleep patterns and cognitive development at age 6 years: the Generation R Study. J Pediatr Psychol. 2017;42(3):260–268. [DOI] [PubMed] [Google Scholar]
- 4.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr. 2015;169(6):575–582. [DOI] [PubMed] [Google Scholar]
- 5.Alamian A, Wang L, Hall AM, Pitts M, Ikekwere J. Infant sleep problems and childhood overweight: Effects of three definitions of sleep problems. Prev Med Rep. 2016;4:463–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mindell J, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: A cross-cultural comparison. Sleep Med. 2010;11:393–399. [DOI] [PubMed] [Google Scholar]
- 7.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. [DOI] [PubMed] [Google Scholar]
- 8.Teti DM, Crosby B. Maternal depressive symptoms, dysfunctional cognitions, and infant night waking: The role of maternal nighttime behavior. Child Dev. 2012;83(3):939–953. [DOI] [PubMed] [Google Scholar]
- 9.Tikotzky L, Shaashua L. Infant sleep and early parental sleep-related cognitions predict sleep in pre-school children. Sleep Med. 2012;13(2):185–192. [DOI] [PubMed] [Google Scholar]
- 10.Smith JP, Hardy ST, Hale LE, Gazmararian JA. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health. 2019;5(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychol. 2013;32(8):849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr. 2009;30(5):394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol. 2014;33(3):301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peña M-M, Rifas-Shiman SL, Gillman MW, Redline S, Taveras EM. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williamson AA, Mindell JA. Cumulative socio-demographic risk factors and sleep outcomes in early childhood. Sleep 2020;43(3):zsz233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagy E, Moore S, Gruber R, Paquet C, Arora N, Dubé L. Parental social captial and children’s sleep disturbances. Sleep Health. 2016;2:330–334. [DOI] [PubMed] [Google Scholar]
- 17.Johnson DA, Billings ME, Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. 2018;5(2):61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rudolph KE, Shev A, Paksarian D, et al. Environmental noise and sleep and mental health outcomes in a nationally representative sample of urban US adolescents. Environ Epidemiol. 2019;3(4):e056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bottino CJ, Rifas-Shiman SL, Kleinman KP, et al. The association of urbanicity with infant sleep duration. Health Place. 2012;18(5):1000–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Troxel WM, Shih RA, Ewing B, Tucker JS, Nugroho A, D’Amico EJ. Examination of neighborhood disadvantage and sleep in a multi-ethnic cohort of adolescents. Health Place. 2017;45:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bagley EJ, Kelly RJ, Buckhalt JA, El-Sheikh M. What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment. Sleep Med. 2015;16(4):496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheehan C, Powers D, Margerison-Zilko C, McDevitt T, Cubbin C. Historical neighborhood poverty trajectries and child sleep. Sleep Health. 2018;4:127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grimes M, Camerota M, Propper CB. Neighborhood deprivation predicts infant sleep quality. Sleep Health. 2019;5(2):148–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Graham C, Reither EN, Ciciurkaite G, Dev DA, Fargo J. Does context matter? A multilevel analysis of neighborhood disadvantage and children’s sleep health. Sleep Health. 2020. [Online ahead of print]. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon AL, Tomfohr-Madsen L, Tough S. Neighborhood socio-economic factors and associations with infant sleep health. Behav Sleep Med. 2020:1–13.[Online ahead of print]. [DOI] [PubMed] [Google Scholar]
- 26.Milan S, Snow S, Belay S. The context of preschool children’s sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21(1):20. [DOI] [PubMed] [Google Scholar]
- 27.Meltzer LJ, Johnson C, Crosette J, Ramos M, Mindell JA. Prevalence of diagnosed sleep disorders in pediatric primary care practices. Pediatrics. 2010;125(6):e1410–e1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Caldwell B, Ordway M, Sadler L, Redeker N. Parent perspectives on sleep and sleep habits among young children living with economic adversity. J Pediatr Health Care. 2020;34(1):10–22. [DOI] [PubMed] [Google Scholar]
- 29.Williamson A, Milaniak I, Watson B, et al. Early childhood sleep intervention in urban primary care: Caregiver and clinician perspectives. J Pediatr Psychol. 2020;54(8):933–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sadeh A, Mindell JA, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12(5):478–482. [DOI] [PubMed] [Google Scholar]
- 31.American Academy of Sleep Medicine. International classification of sleep disorders—third edition (ICSD-3). AASM Resource Library. 2014. [Google Scholar]
- 32.Williamson AA, Mindell JA, Hiscock H, Quach J. Longitudinal sleep problem trajectories are associated with multiple impairments in child well- being. J Child Psychol Psychiatr. 2020. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jackson CL, Walker JR, Brown MK, Das R, Jones NL. A workshop report on the causes and consequences of sleep health disparities. Sleep. 2020;43(8):zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leichman ES, Gould R, Williamson A, Walters R, Mindell J. Effectiveness of an mHealth intervention for infant sleep disturbances. Behav Ther. 2020;51(4):548–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mindell JA, Gould R, Tikotzky L, Leichman ES, Walters R. Norm-referenced scoring system for the Brief Infant Sleep Questionnaire—Revised (BISQ-R). Sleep Med. 2019;63:106–114. [DOI] [PubMed] [Google Scholar]
- 36.Mindell JA, Du Mond CE, Sadeh A, Telofski LS, Kulkarni N, Gunn E. Long-term efficacy of an internet-based intervention for infant and toddler sleep disturbances: one year follow-up. J Clin Sleep Med. 2011;7(5):507–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kushnir J, Sadeh A. Correspondence between reported and actigraphic sleep measures in preschool children: the role of a clinical context. J Clin Sleep Med. 2013;9(11):1147–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. [DOI] [PubMed] [Google Scholar]
- 39.Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics. 2011;128:692–701. [DOI] [PubMed] [Google Scholar]
- 40.Economic Innovation Group. From great recession to great reshuffling: Charting a decade of change across American communities. Findings from the 2018 Distressed Communities Index. https://eig.org/wp-content/uploads/2018/10/2018-DCI.pdf. Accessed September 2, 2020. [Google Scholar]
- 41.Weeks WB, Ouayogodé MH, Weinstein JN. Association between a measure of community economic distress and medicare patients’ health care utilization, quality, outcomes, and costs. J Gen Intern Med. 2018; 33(9):1433–1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mindell JA, Leichman ES, Walters RM. Sleep location and parent-perceived sleep outcomes in older infants. Sleep Med. 2017;39:1–7. [DOI] [PubMed] [Google Scholar]
- 43.Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact of sleep extension and restriction on children’s emotional lability and impulsivity. Pediatrics. 2012;130(5):e1155–e1161. [DOI] [PubMed] [Google Scholar]
- 44.Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute sleep restriction effects on emotion responses in 30- to 36- month- old children. J Sleep Res. 2012;21(3):235–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller AL, Seifer R, Crossin R, Lebourgeois MK. Toddler’s self- regulation strategies in a challenge context are nap- dependent. J Sleep Res. 2015;24(3):279–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Evans GW, Kim P. Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status–health gradient. Ann NY Acad Sci. 2010;1186(1):174–189. [DOI] [PubMed] [Google Scholar]
- 47.McDowall PS, Galland BC, Campbell AJ, Elder DE. Parent knowledge of children’s sleep: A systematic review. Sleep Med Rev. 2017;31:39–47. [DOI] [PubMed] [Google Scholar]
- 48.Bathory E, Tomopoulos S, Rothman R, et al. Infant Sleep and Parent Health Literacy. Acad Pediatr. 2016;16(6):550–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zambrano DN, Mindell JA, Reyes NR, Hart CN, Herring SJ. “It’s not all about my baby’s sleep”: A qualitative study of factors influencing low-income African American mothers’ sleep quality. Behav Sleep Med. 2016;14(5):489–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pennestri M-H, Laganière C, Bouvette-Turcot A-A, et al. Uninterrupted infant sleep, development, and maternal mood. Pediatrics. 2018;142(6). [DOI] [PubMed] [Google Scholar]
- 51.Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity-a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schwichtenberg A, Abel E, Keys E, Honaker SM. Diversity in pediatric behavioral sleep intervention studies. Sleep Med Rev. 2019;47:103–111. [DOI] [PubMed] [Google Scholar]
- 53.Pew Reserach Center. Mobile fact sheet. Pew Research Center: Internet, Science & Tech 2019, June; https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed September 2, 2020. [Google Scholar]
- 54.Franzoni C, Sauermann H. Crowd science: The organization of scientific research in open collaborative projects. Res Pol. 2014;43(1):1–20. [Google Scholar]
- 55.Davis DW, Logsdon MC, Vogt K, et al. Parent education is changing: a review of smartphone apps. MC-Am J Matern-Chil. 2017;42(5):248–256. [DOI] [PubMed] [Google Scholar]
- 56.Cushing CC, Fedele DA, Brannon EE, Kichline T. Parents’ perspectives on the theoretical domains framework elements needed in a pediatric health behavior app: A crowdsourced social validity study. JMIR mhealth uhealth. 2018;6(12):e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McCloskey ML, Thompson DA, Chamberlin B, Clark L, Johnson SL, Bellows LL. Mobile device use among rural, low-income families and the feasibility of an app to encourage preschoolers’ physical activity: qualitative study. JMIR Pediatr Parent. 2018;1(2):e10858. [DOI] [PMC free article] [PubMed] [Google Scholar]


