Abstract
Lateral ankle sprains are very common injuries that sometimes lead to chronic lateral ankle instability. The modified Broström operation is the gold standard procedure for treatment of chronic lateral ankle instability. Currently, this operation is performed arthroscopically. Broström repair depends on the quality of the remnant ligament. In cases with an insufficient remnant ligament, Gould augmentation or reconstruction using the gracilis tendon is generally performed. Recently, tape augmentation (internal brace) also has been used to support an insufficient ligament. This article introduces arthroscopic tape augmentation with arthroscopic modified Broström operation. This technique consists of creation of a talar anchor hole and fibular anchor hole, reattachment of the remnant ligament to the fibula with tape, and tape fixation to the talus. This technique uses only one knotless anchor screwed to the fibula for both the modified Broström operation and fixation of the tape. This technique is relatively simple and produces similar results as an open procedure.
Technique Video
This video demonstrates each step of the arthroscopic internal brace augmentation with arthroscopic modified Broström operation. The procedure is performed with the patient in the supine position. The patient's leg is placed on the leg holder, and the hip and knee joints are flexed to about 45°. For creation of the talar anchor hole, the viewing portal and working portal are the anteromedial and accessory anterolateral portals, respectively. For the other procedures, the viewing and working portals are the anterolateral and accessory anterolateral portals, respectively. Surgical steps consist of creation of the talar anchor hole (1:19-1:41), creation of the fibular anchor hole (1:41-1:54), suture lasso using an 18-G needle and 2-0 PROLENE (1:54-2:09), suture relay from the 2-0 PROLENE to a tape (2:09-2:17), grasping of the ATFL and CFL complex by the tape (2:17-2:35), suture lasso insertion for the artificial ligament (2:36-2:45), insertion of the anchor into the fibula with an artificial ligament and tape (2:46-3:15), suture relay from the 2-0 PROLENE to the artificial ligament (3:20-3:28), and insertion of the knotless anchor into the talus (3:35-3:55). (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)
Lateral ankle sprains (LAS) are very common traumas, especially in the field of sports. Usually, conservative treatment is chosen for most patients with acute LAS. However, 10% to 30% of patients with acute LAS develop chronic lateral ankle instability (CLAI).1 Currently, the modified Broström procedure is the gold standard procedure for CLAI.2 However, poor quality of the remnant ligament and general joint laxity are contraindications to this surgery, because the procedure depends on ligament quality. Moreover, it requires postoperative immobilization for several weeks, which is an additional problem with this procedure. To resolve these problems, tape augmentation, called internal brace (IB), was developed, and the modified Broström repair with IB has been shown to produce reliable results.2
Currently, the modified Broström procedure is performed arthroscopically.3,4 A previous report showed that the arthroscopic procedure is superior to the open procedure in terms of early recovery.1 If the modified Broström repair with IB is also performed arthroscopically, this procedure would likely improve the utility of the procedure in terms of early recovery. The purpose of this study was to introduce the new arthroscopic IB augmentation with arthroscopic modified Broström procedure for CLAI in cases with a poor remnant ligament, which has not been previously reported.
Surgical Technique
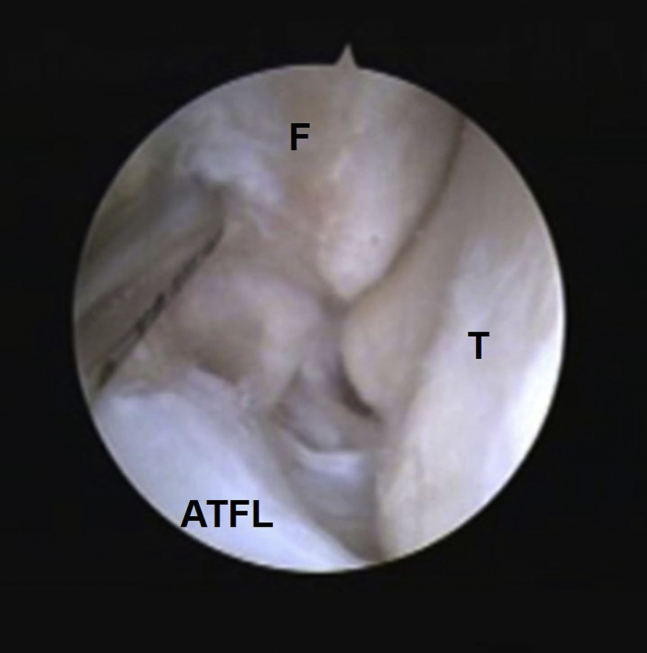
The surgery is performed under sciatic and saphenous nerve block, lumbar spinal anesthesia, or general anesthesia. The patient is placed in the supine position with ankle traction (Non-Invasive Ankle Distractor; Smith & Nephew, Andover, MA). Irrigation is provided by a flow pump system (Continuous Wave II Arthroscopy Pump; Arthrex, Naples, FL), in which the pressure is adjusted between 30 and 50 mm Hg. A 2.7-mm 30°arthroscope is used for this technique. Standard anteromedial, anterolateral, and accessory anterolateral portals are used for this procedure (Table 1). After conventional ankle arthroscopy, the ankle traction is removed and ligament tensions are loosened to allow easy manipulation of the ligaments. Synovectomy is performed to secure viewing and identify remnants of the lateral ligament complex (Fig 1).
Table 1.
Surgical Steps, Pearls, and Pitfalls
| Surgical Steps | Pearls | Pitfalls |
|---|---|---|
| Arthroscopic portal | The accessory anterolateral portal is placed to allow easy access to both fibular and talar bone hole positions. | Poor positioning of the portal makes it difficult to create a hole in the bone. |
| Creation of the talar anchor hole | The talus cartilage and ATFL remnant are good guides to the drill hole position. The drill position is located medial to the talus footprint of the ATFL and it has no cartilage area. We recommend performing the procedure under fluoroscopic guidance. |
Poor visualization might lead to damage to the ATFL or cartilage. |
| Creation of the fibular anchor hole | Peeling off the ATFL and shaving the footprint is important for reconstruction of the ligament heeling and good visualization during creation of the drill hole. The center of the fibular anchor hole is positioned about 5 mm proximal to the fibular obscure tubercle. |
Insufficient preparation would prevent biological healing. If a drill is inserted into the fibula perpendicularly, the anchor might blow out the posterior cortex of the fibula. |
| Suture lasso using an 18-gauge needle and 2-0 PROLENE | The 18G needle with a 2-0 nylon loop is inserted into the center of the ATFL and CFL complex. | Care should be taken to avoid penetrating the peroneal tendons or damaging the sural nerve. |
| Insertion of the knotless anchor into the fibula with ligament and tape | The racking hitch knot enhances fixation of the ligament. The ligament is reattached with the ankle in the dorsiflexion and valgus position. |
Once the anchor is introduced, tension in the suture cannot be controlled. |
| Insertion of the knotless anchor into the talus | A guidewire or K-wire is inserted into the talar drill hole under arthroscopy, to confirm the hole position and to avoid incorrect insertion. The knotless anchor is inserted into the talus under direct view. | If the positions of the holes are not carefully checked, incorrect insertion could occur. |
ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.
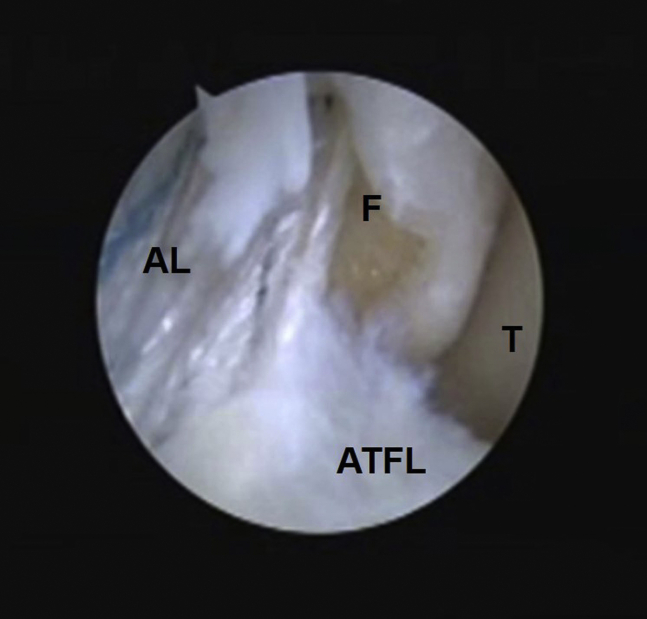
Fig 1.
Arthroscopic view of the lateral gutter in the right ankle. Viewing from the anterolateral portal, the ATFL fiber is detached from the fibula footprint. (ATFL, anterior talofibular ligament; F, fibula; T, talus.)
First, a talus anchor hole is made at a medial position relative to the talus footprint of the anterior talofibular ligament (ATFL) (Fig 2). A guidewire is inserted at the center of the anchor hole via the accessory anterolateral portal while viewing from the anteromedial portal. A 3.4-mm cannulated drill is inserted through the guidewire and the SwiveLock tap (4.75-mm SwiveLock; Arthrex), which has a laser line to show adequate depth, is inserted.
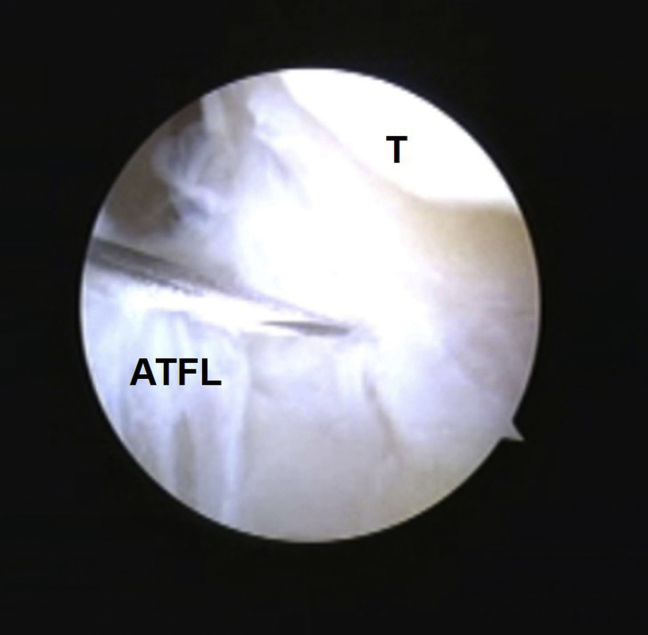
Fig 2.
Arthroscopic view of the talar ligament footprint in the right ankle. Viewing from the anteromedial portal, the tip of the needle indicates the talar footprint of the ATFL. We make the accessory anterolateral portal after checking accessibility of the talar footprint from this position. A guide wire is inserted at the center of the anchor hole via the accessory anterolateral portal, and a cannulated drill is inserted through the guide wire for the knotless anchor. (ATFL, anterior talofibular ligament; T, talus.)
Next, a fibula anchor hole is made. The position of this hole is determined referring to the fibular obscure tubercle described in the report of Matsui et al.5 The center of the fibular anchor hole is positioned about 5 mm proximal to the fibular obscure tubercle. A guidewire is inserted into this point of the fibula from the accessory anterolateral portal under viewing from the anterolateral portal. A 2.7-mm cannulated drill is inserted through the guidewire, and the SwiveLock tap (3.5-mm SwiveLock; Arthrex) is inserted following the laser line (Fig 3).
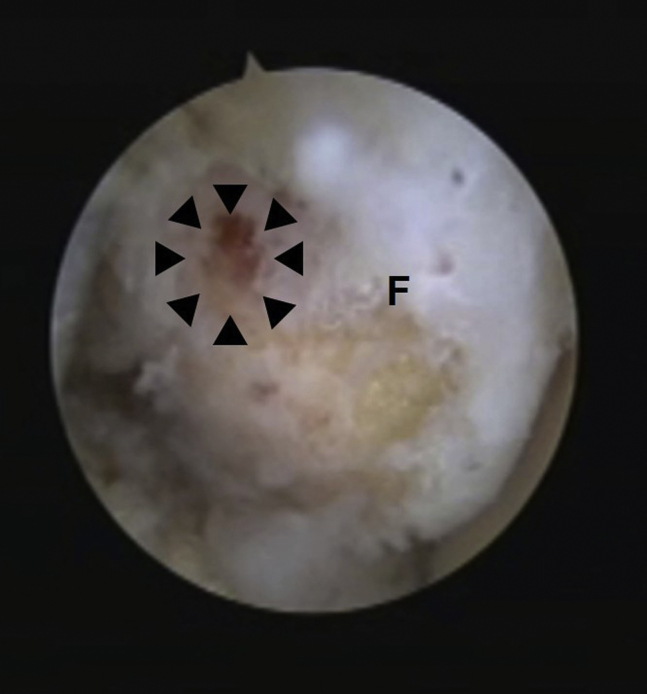
Fig 3.
Arthroscopic view of the fibular ligament footprint in the right ankle. Viewing from the anterolateral portal, the area surrounded by arrowheads shows the center of the fibular anchor hole, which is positioned about 5 mm proximal to the fibular obscure tubercle. A guidewire is inserted from the accessory anterolateral portal and this anchor direction is confirmed by fluoroscopy. (F, fibula.)
An 18-G hollow needle with a 2-0 nylon loop is inserted into the center of the ATFL and the calcaneofibular ligament (CFL) complex via the skin (Fig 4). The loop of the nylon is picked up through the accessory anterolateral portal with a grasper or mosquito forceps. Then, the tape (SutureTape; Arthrex) is passed through the nylon loop and the end of the nylon opposite the loop is pulled out through the skin (the tape is put through the ATFL). The tape is picked up subcutaneously through the accessory anterolateral portal. We use the racking hitch knot6 to firmly capture the ligament. By this procedure, the SutureTape tightly grasps the ligament and capsule. Then, an 18-G needle with a 2-0 nylon loop is inserted just in front of the fibular knotless anchor hole from the lateral side, and the nylon loop is picked up subcutaneously from the accessory anterolateral portal (Fig 5). Next, a knotless anchor (3.5-mm SwiveLock; Arthrex) with the artificial ligament (FiberTape; Arthrex) is prepared. The tape that was used to capture the ligament is inserted into the eyelet of the knotless anchor. Then, the knotless anchor is inserted into the fibula hole with the ankle in the dorsiflexion and valgus position. By this procedure, both the ATFL and CFL remnants are fixed on the fibula (Fig 6). The artificial ligament is passed through the nylon loop and pulled out. Then, the artificial ligament is picked up subcutaneously from the accessory anterolateral portal. With these processes, the artificial ligament runs outside of the capsule. The ligament is passed into the eyelet of a 4.75-mm knotless anchor (4.75-mm SwiveLock; Arthrex), and the eyelet of the anchor is brought to the top edge of the drill hole of the talus. The ligament is pulled to the desired tension. Finally, the anchor is inserted into the talus (Fig 7). After the final anchor has been correctly inserted, the remnant ligament tails are cut with a tape cutter (Video 1).
Fig 4.
Suture relay passing through the anterior talofibular ligament in the right ankle. Viewing from the anterolateral portal, an 18-G hollow needle with a 2-0 nylon loop (as a suture lasso) is inserted into the center of the anterior talofibular ligament and the CFL complex via the skin. (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; F, fibula; T, talus.)
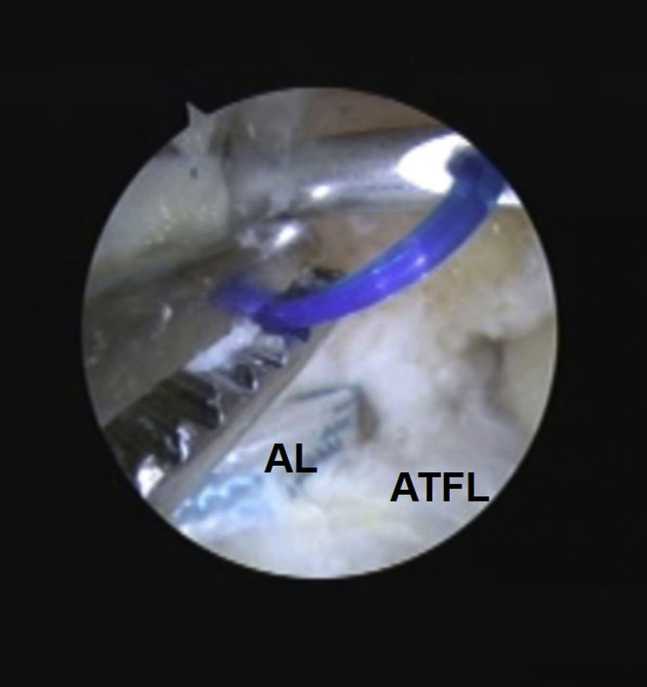
Fig 5.
Suture relay for the artificial ligament in the right ankle. Viewing from the anterolateral portal, an 18-G hollow needle with a 2-0 nylon loop (as a suture lasso) is inserted just in front of the fibular knotless anchor hole via the lateral side of the skin, and the nylon loop is picked up from the accessory anterolateral portal. (AL, artificial ligament; ATFL, anterior talofibular ligament.)
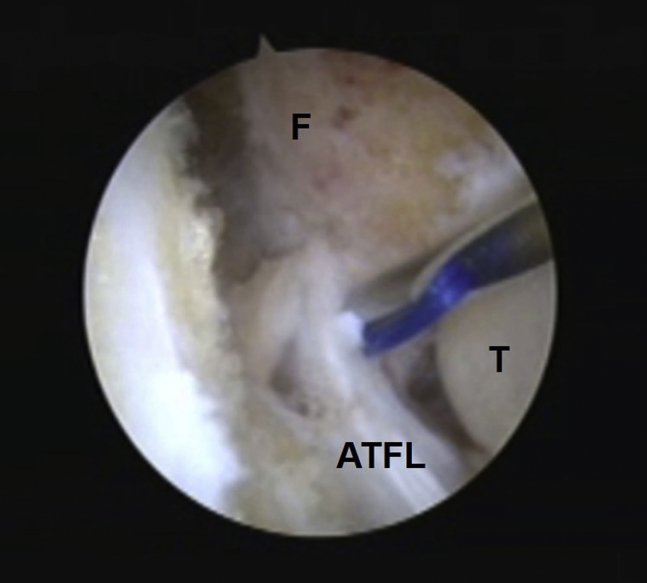
Fig 6.
Fibular anchor insertion in the right ankle. A knotless anchor with an artificial ligament and a suture tape that captures the anterior talofibular and calcaneofibular ligaments is inserted into the fibular anchor hole. At this time, the ankle is held in the dorsiflexion and valgus position. (AL, artificial ligament; ATFL, anterior talofibular ligament; F, fibula; T, talus.)
Fig 7.
Macroscopic view of talar anchor insertion of the right ankle. The anchor with the artificial ligament is inserted into the talus. At this time, the ankle is held in the dorsiflexion and valgus position.
For postoperative care, the patient is put in a plaster shell for 1 week, but movement of the toes is permitted 1 day after surgery. One week after surgery, the patient is permitted to walk with an ankle brace, and ankle range of motion, proprioception, and strengthening training are initiated. If there is no swelling or pain, jogging is permitted 4 weeks after surgery. Return to full sports activity is permitted approximately 8 weeks after the surgery.
Discussion
Less-invasive surgeries are preferable to conventional open surgeries. Arthroscopic surgeries, such as anterior cruciate ligament reconstruction and rotator cuff repair, are some of the most common less-invasive surgeries. Recently, the arthroscopic Broström procedure for CLAI is also becoming increasingly common in the foot and ankle area.3,4 Our procedure of arthroscopic Broström procedure with tape augmentation might be useful from the point of view of limited invasiveness (Table 2).
Table 2.
Advantages and Risks and/or Limitations of This Technique
| Advantages | Risks and/or Limitations |
|---|---|
| We can more clearly assess the condition of intra-articular lesions. | Arthroscopic surgery experience is needed. |
| Arthroscopic procedures are less invasive than open procedures. | This technique only allows ATFL augmentation |
| Our procedure is simpler than previous procedures because only one anchor is used to fix both the remnant ligament and the artificial ligament on the fibula. | The long-term results are unclear. |
| In young children who still have epiphyseal lines, the fibula side knotless anchor can destroy their epiphyseal line. |
ATFL, anterior talofibular ligament.
The Broström procedure is a reasonable technique from an anatomical aspect. However, the procedure depends on the quality of the remnant ligament. In general, the repaired ligament is strengthened using the extensor retinaculum (Gould technique). However, the course of the extensor retinaculum is different from those of the ATFL and CFL. Thus, it might limit the postoperative range of motion. The course of our tape augmentation is almost similar to that of the superior bundle of the ATFL. Hence, it is less likely to limit range of motion of the ankle.
Biomechanical studies7,8 have reported mechanical superiority of augmented ATFL reconstruction using a suture tape. Viens et al.7 reported that the mean ultimate load of the Broström repair with tape augmentation (250.8 ± 122.7 N) was not significantly different from that of the intact ATFL (154.0 ± 63.7 N). Schuh et al.8 reported that there was a 95% greater torque in cases of failure of the suture-tape augmentation construct compared with the Broström repair and a 54% greater torque with failure in the construct compared with the suture anchor repair alone. With regard to stress radiographs of clinical results, Cho et al.9 reported that talar tilt angle and anterior talar translation significantly improved from the preoperative average of 16.2 and 12.1 mm to 3.6 and 4.2 mm, respectively, on an average of 35.8 months after surgery.
Yoo et al.10 and Ulku et al.11 also reported their arthroscopic modified Broström repair with IB for CLAI. However, the technique of Ulku et al. only uses tape as the artificial ligament, and they do not simultaneously perform remnant ligament repair (Broström procedure). They reported good intermediate-term results, and their technique had similar clinical outcomes as the arthroscopic Broström procedure. However, their long-term outcomes were worrisome, because of degeneration of the tape over time, since the tape is not regenerated. In contrast, Yoo et al. used 2 anchors for fixation of the remnant ligament as an arthroscopic modified Broström procedure and a 3.5-mm knotless anchor for tape augmentation. Their technique is expected to facilitate ligament regeneration. However, their technique requires the insertion of 3 anchors onto the fibula. Hence, their technique is more complicated than our technique because we use only one knotless anchor for the fibula fixation.
The main limitation of our technique is that it only results in ATFL augmentation, since the IB does not support the CFL. However, the simultaneously performed arthroscopic Broström technique repairs both the ATFL and CFL complex. Hence, CFL repair is performed in conjunction with that of the ATFL. At the least, our technique is better than tape augmentation alone without Broström repair from the point of CFL repair.
In conclusion, an arthroscopic Broström repair with IB was described. This procedure needs to be further investigated to determine whether it is less invasive than the conventional open procedure. Further, the long-term results of our procedure need to be assessed because the utility of tape augmentation in the long term, even with the conventional technique, have not been evaluated. This procedure requires some training, but it seems to be a viable alternative to conventional open procedures and is a simple technique as compared with previous techniques.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates each step of the arthroscopic internal brace augmentation with arthroscopic modified Broström operation. The procedure is performed with the patient in the supine position. The patient's leg is placed on the leg holder, and the hip and knee joints are flexed to about 45°. For creation of the talar anchor hole, the viewing portal and working portal are the anteromedial and accessory anterolateral portals, respectively. For the other procedures, the viewing and working portals are the anterolateral and accessory anterolateral portals, respectively. Surgical steps consist of creation of the talar anchor hole (1:19-1:41), creation of the fibular anchor hole (1:41-1:54), suture lasso using an 18-G needle and 2-0 PROLENE (1:54-2:09), suture relay from the 2-0 PROLENE to a tape (2:09-2:17), grasping of the ATFL and CFL complex by the tape (2:17-2:35), suture lasso insertion for the artificial ligament (2:36-2:45), insertion of the anchor into the fibula with an artificial ligament and tape (2:46-3:15), suture relay from the 2-0 PROLENE to the artificial ligament (3:20-3:28), and insertion of the knotless anchor into the talus (3:35-3:55). (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)
References
- 1.Matsui K., Takao M., Miyamoto W., Matsushita T. Early recovery after arthroscopic repair compared to open repair of the anterior talofibular ligament for lateral instability of the ankle. Arch Orthop Trauma Surg. 2016;136:93–100. doi: 10.1007/s00402-015-2342-3. [DOI] [PubMed] [Google Scholar]
- 2.Xu D.L., Gan K.F., Li H.J. Modified Brostrom repair with and without augmentation using suture tape for chronic lateral ankle instability. Orthop Surg. 2019;11:671–678. doi: 10.1111/os.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takao M., Matsui K., Stone J.W. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sports Traumatol Arthrosc. 2016;24:1003–1006. doi: 10.1007/s00167-015-3638-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vega J., Golano P., Pellegrino A., Rabat E., Pena F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34:1701–1709. doi: 10.1177/1071100713502322. [DOI] [PubMed] [Google Scholar]
- 5.Matsui K., Oliva X.M., Takao M. Bony landmarks available for minimally invasive lateral ankle stabilization surgery: A cadaveric anatomical study. Knee Surg Sports Traumatol Arthrosc. 2017;25:1916–1924. doi: 10.1007/s00167-016-4218-7. [DOI] [PubMed] [Google Scholar]
- 6.Kelly J.D., 2nd, Vaishnav S., Saunders B.M., Schrumpf M.A. Optimization of the racking hitch knot: how many half hitches and which suture material provide the greatest security? Clin Orthop Relat Res. 2014;472:1930–1935. doi: 10.1007/s11999-014-3478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Viens N.A., Wijdicks C.A., Campbell K.J., Laprade R.F., Clanton T.O. Anterior talofibular ligament ruptures, part 1: Biomechanical comparison of augmented Brostrom repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405–411. doi: 10.1177/0363546513510141. [DOI] [PubMed] [Google Scholar]
- 8.Schuh R., Benca E., Willegger M. Comparison of Brostrom technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:1101–1107. doi: 10.1007/s00167-015-3631-7. [DOI] [PubMed] [Google Scholar]
- 9.Cho B.K., Park K.J., Park J.K., SooHoo N.F. Outcomes of the modified Brostrom Procedure augmented with suture-tape for ankle instability in patients with generalized ligamentous laxity. Foot Ankle Int. 2017;38:405–411. doi: 10.1177/1071100716683348. [DOI] [PubMed] [Google Scholar]
- 10.Yoo J.S., Yang E.A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ulku T.K., Kocaoglu B., Tok O., Irgit K., Nalbantoglu U. Arthroscopic suture-tape internal bracing is safe as arthroscopic modified Brostrom repair in the treatment of chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:227–232. doi: 10.1007/s00167-019-05552-w. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates each step of the arthroscopic internal brace augmentation with arthroscopic modified Broström operation. The procedure is performed with the patient in the supine position. The patient's leg is placed on the leg holder, and the hip and knee joints are flexed to about 45°. For creation of the talar anchor hole, the viewing portal and working portal are the anteromedial and accessory anterolateral portals, respectively. For the other procedures, the viewing and working portals are the anterolateral and accessory anterolateral portals, respectively. Surgical steps consist of creation of the talar anchor hole (1:19-1:41), creation of the fibular anchor hole (1:41-1:54), suture lasso using an 18-G needle and 2-0 PROLENE (1:54-2:09), suture relay from the 2-0 PROLENE to a tape (2:09-2:17), grasping of the ATFL and CFL complex by the tape (2:17-2:35), suture lasso insertion for the artificial ligament (2:36-2:45), insertion of the anchor into the fibula with an artificial ligament and tape (2:46-3:15), suture relay from the 2-0 PROLENE to the artificial ligament (3:20-3:28), and insertion of the knotless anchor into the talus (3:35-3:55). (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)
This video demonstrates each step of the arthroscopic internal brace augmentation with arthroscopic modified Broström operation. The procedure is performed with the patient in the supine position. The patient's leg is placed on the leg holder, and the hip and knee joints are flexed to about 45°. For creation of the talar anchor hole, the viewing portal and working portal are the anteromedial and accessory anterolateral portals, respectively. For the other procedures, the viewing and working portals are the anterolateral and accessory anterolateral portals, respectively. Surgical steps consist of creation of the talar anchor hole (1:19-1:41), creation of the fibular anchor hole (1:41-1:54), suture lasso using an 18-G needle and 2-0 PROLENE (1:54-2:09), suture relay from the 2-0 PROLENE to a tape (2:09-2:17), grasping of the ATFL and CFL complex by the tape (2:17-2:35), suture lasso insertion for the artificial ligament (2:36-2:45), insertion of the anchor into the fibula with an artificial ligament and tape (2:46-3:15), suture relay from the 2-0 PROLENE to the artificial ligament (3:20-3:28), and insertion of the knotless anchor into the talus (3:35-3:55). (ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament.)