Abstract
Displaced greater tuberosity fractures of the humerus require anatomic reduction with stable fixation to optimize rotator cuff function and prevent subacromial impingement. A wide variety of surgical approaches and fixation constructs have been reported, largely with favorable results. Arthroscopic management of these fractures allows excellent visualization with strong suture anchor fixation while minimizing soft tissue disruption, blood loss, and radiation exposure. The purpose of this article is to describe an arthroscopic technique for reduction and suture-anchor fixation of displaced greater tuberosity fractures.
Technique Video
Narrated video of arthroscopic greater tuberosity fracture fixation in 2 patients. The first case demonstrates the classic posteromedial displacement of this fracture pattern from the pull of the infraspinatus tendon. An anterolateral suture anchor placed well away from the fracture bed is used to correct this displacement. The second case demonstrates superomedial displacement of the fracture fragment. Provisional reduction is performed with a spinal needle, which helps guide the position of the anchor. Anchor placement at the margin of the fracture site is demonstrated, with care to gain appropriate purchase of the anchor with precise starting position and trajectory. Retrograde suture passage in a horizontal mattress pattern is shown. Tensioning and later tying the sutures facilitates anatomic reduction, which can be confirmed from subacromial and glenohumeral views. Note the restoration of rotator cuff position just medial to the fracture site in each view.
Isolated greater tuberosity fractures of the humerus account for approximately 20% of proximal humerus fractures.1,2 In contrast to comminuted fragility fractures, these fractures often occur in younger patients and may be associated with glenohumeral dislocation. Due to the rotator cuff attachments on the fragment, displacement tends to occur superiorly and posteriorly.3,4 The vast majority (85%-95%) of these fractures are minimally displaced and can be managed conservatively with good results.5,6 Surgical fixation is recommended for displacement greater than 5 mm in the general population or 3 mm in high-demand patients, such as athletes or overhead laborers.5,6 In surgical cases, accurate reduction of the fracture is important to optimize rotator cuff function and prevent subacromial impingement.3,4,7
Open reduction and internal fixation (ORIF) allows direct visualization of the fracture and surrounding anatomy via a deltoid-split or deltopectoral approach. Fixation can be achieved with cancellous screws and washers, plate and screw constructs, all-suture constructs, or suture anchors.3 Benefits of an open approach include excellent visualization, technical ease, and high rates of bony union.8 Disadvantages of this approach include increased soft-tissue dissection, a larger surgical scar, increased infection risk and loss of motion. Yoon et al.9 recently reported a high rate of postoperative stiffness after mini-open screw fixation, with 31% of patients requiring reoperation for arthroscopic release and manipulation.
Arthroscopic fixation avoids deltoid disruption and open dissection while still allowing excellent visualization and manipulation of the fracture. Likewise, an arthroscopic approach affords the opportunity to visualize the entire joint, identify any additional pathology, and treat such conditions arthroscopically as indicated. Several arthroscopic techniques and implants have been described including single-row, double-row, and suture bridge constructs.7,10, 11, 12 Arthroscopic repair can be more technically demanding and time-consuming, although similarities to rotator cuff repair may decrease the learning curve. Additional benefits of arthroscopic fixation include intra-articular access for diagnosing and treating other shoulder pathology, reduced radiation exposure, decreased blood loss, and a smaller surgical scar. Thin or comminuted fractures that will not accept screw fixation can be addressed with arthroscopic suture fixation, preserving the potential for bone-to-bone healing and reducing the risk of hardware failure. We describe a technique for arthroscopic fixation of greater tuberosity fractures using a suture anchor-based construct, along with several technical tips to maximize success with this procedure.
Surgical Technique (With Video Illustration)
Preoperative orthogonal radiographs are essential to determine the fracture pattern and confirm a reduced glenohumeral joint. Computed tomography may be used when there is concern of fracture comminution, significant posterior displacement, or nondisplaced fracture extension into the remaining proximal humerus.5 The surgery can be performed in the beach chair or lateral decubitus position. The authors prefer the beach chair position to allow manipulation of the arm during fracture reduction. This position also allows easier conversion to an open approach if needed. The technique for arthroscopic fixation of a greater tuberosity fracture is demonstrated in Video 1. Key concepts for success with the procedure are highlighted in Table 1.
Table 1.
Pearls and Pitfalls of Surgical Technique for Arthroscopic Greater Tuberosity Fixation
| Carefully evaluate for coexisting labral or rotator cuff injury |
| Improve visualization and fracture mobilization with thorough subacromial bursectomy and hematoma debridement |
| Use an 18-gauge spinal needle to determine reduction vector and provisionally reduce |
| Place anchors perpendicular to direction of displacement so suture vector anatomically reduces the fracture |
| Place anchors in intact bone away from the fracture bed to avoid pullout |
| Use a retrograde suture passer for precise, well-visualized suture passage around the fracture fragment |
The operative extremity is prepped in standard fashion and bony anatomic landmarks are referenced when establishing arthroscopic portals. A standard posterior portal is created and a 30-degree arthroscope is introduced into the glenohumeral joint. An anterosuperior portal is created in outside-in fashion through the rotator interval. A diagnostic arthroscopy is performed and any intra-articular pathology is addressed. The subacromial space is entered and a lateral portal is established after spinal needle localization. An arthroscopic shaver is used to perform a subacromial bursectomy to improve visualization and ease of instrument passage. An arthroscopic acromioplasty also may be carried out at the discretion of the surgeon. The camera is switched to the lateral portal, providing excellent visualization of the fracture fragment and rotator cuff. Close attention is paid to the size, comminution, and direction of displacement for the greater tuberosity fragment. To maximize healing potential, the fracture bed can be gently debrided using an arthroscopic shaver. In cases with early healing or retraction, careful mobilization of the fragment may be required before reduction. At this point, accessory portals can be created at the surgeon’s discretion to aid in visualization or instrument passage.
An 18-gauge spinal needle or arthroscopic probe can be used to percutaneously reduce the fracture, confirming appropriate mobility of the fragment and demonstrating the vector of required reduction force when planning anchor placement (Video 1). In addition to superior displacement, the fragment may be pulled posteriorly by the infraspinatus and/or teres minor tendons (Fig 1). For fractures with significant medialization or multidirectional displacement, a grasper may be used for reduction. Similarly, a traction suture, passed through the adjacent rotator cuff tissue attached to the displaced greater tuberosity fragment, can aid in reducing the fracture fragment.
Fig 1.

Arthroscopic subacromial view of a right shoulder from a lateral portal in the beach chair position demonstrating posteromedial displacement of the greater tuberosity fracture fragment (∗) due to pull of the infraspinatus tendon, with its corresponding fracture bed.
Precise suture anchor placement is essential in achieving and maintaining appropriate reduction (HEALICOIL REGENESORB 5.5 mm; Smith & Nephew, Andover, MA). The size and pattern of the fracture dictates the number of anchors and their position in the humeral head. The exact construct should be tailored to each patient’s fracture. A single- or double-row anchor construct can be used to secure the fracture fragment. The anchors should be placed in a position so that the vector created by the passed sutures corrects displacement in multiple planes to facilitate an effective and stable reduction. For example, a posteromedially displaced fracture should be fixed with an anterolaterally positioned anchor. The ideal anchors are placed at the margin of the fracture site into intact cortical bone (Fig 2). Spinal needles are used to percutaneously localize the position and trajectory of the anchors prior to insertion. Anchor placement may be challenging due to loss of the greater tuberosity bone at the perimeter of the fracture site and anchor pullout can occur if placed within or in immediate proximity to the fracture bed. When possible, at least several millimeters of intact bone should remain between the anchor and fracture site. Trajectory of the anchor should be away from the fracture site to maximize fixation in uninjured bone (Video 1). We recommend a trial of suture tensioning prior to passage to confirm a well-fixed anchor.
Fig 2.

Arthroscopic view of a left shoulder from a posterior portal in the beach chair position demonstrating anchor placement at the margin of the fracture site in intact bone, with the fracture fragment seen behind (∗). Note the position and trajectory of anchor placement avoiding the fracture bed (red lines) to prevent anchor pullout.
Once the anchors are secure, the sutures are sequentially passed through both the fracture fragment and the adjacent rotator cuff tissue, thus incorporating the rotator cuff tendon in the repair (Fig 3). The suture pattern should broadly distribute compressive forces over the fracture. We prefer a 60° retrograde suture passing device for ease of visualization and accurate passage (IDEAL Suture Grasper, DePuy Mitek, Raynham, MA). This technique is particularly useful in capturing thin or comminuted fracture fragments, in which repair strategies mimic those of a large rotator cuff tear. The camera typically remains in the lateral portal during suture passage and fracture reduction. Sutures can be passed via the anterior or posterior portal depending on the fracture location and degree of displacement.
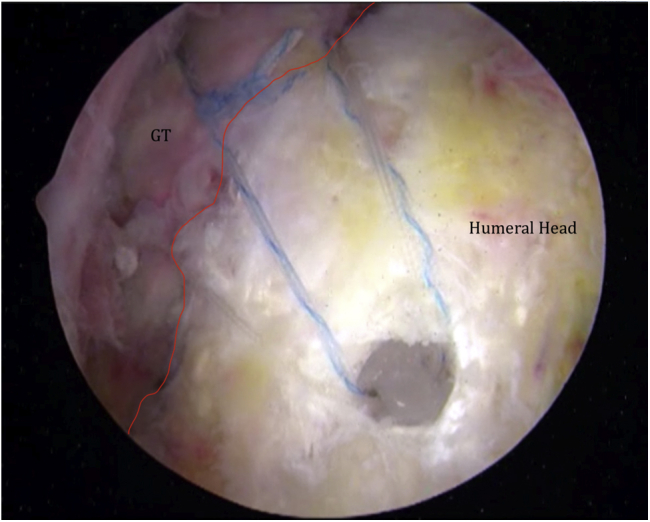
Fig 3.

Arthroscopic view of a left shoulder from a posterior portal in the beach chair position demonstrating precise suture retrieval around the greater tuberosity fracture (GT) in a horizontal mattress configuration (blue arrows) using a retrograde suture passer. The biceps tendon (BT) can be visualized and is avoided during suture passage.
After suture passage, tension on the limbs can be used to reduce the fracture (Fig 4). If fracture reduction is inadequate at this point, the position of the anchors and trajectory of suture passage should be altered as needed. Once appropriate reduction is achieved, the sutures are sequentially tied and cut. In double-row constructs, the medial row is typically secured first. At the conclusion of the procedure, subacromial (Fig 5) and intra-articular (Fig 6) views should demonstrate near anatomic reduction of the fracture fragment and restoration of rotator cuff tendon position. Gentle range of motion should confirm excellent stability of the fragment moving as a single unit without gapping (Fig 7). Fluoroscopic imaging can be used to confirm fracture alignment.
Fig 4.

Arthroscopic view of a left shoulder from a posterior portal in the beach chair position demonstrating fracture (∗) reduction facilitated by gentle tension on the horizontal mattress sutures prior to final knot tying.
Fig 5.

Arthroscopic subacromial view of a left shoulder from a posterior portal in the beach chair position demonstrating anatomic reduction of the greater tuberosity fracture (GT) with a suture anchor construct. The position of the rotator cuff tendon (RC) is restored anatomically.
Fig 6.

Arthroscopic glenohumeral joint view of a left shoulder from a posterior portal in the beach chair position demonstrating reduction of the fracture fragment (∗) and rotator cuff tendon (RC). (BT, biceps tendon.)
Fig 7.
Arthroscopic subacromial view of a right shoulder from a lateral portal in the beach chair position demonstrating anatomic reduction (red line) of the fracture fragment (GT) with a suture anchor construct. Gentle motion of the shoulder under arthroscopic visualization shows no fracture displacement.
In these patients, postoperative recovery is similar to that of arthroscopic repair of a large rotator cuff repair. In the immediate postoperative period, the patient remains in an abduction sling with a focus on pendulum exercises, while maintaining elbow and hand motion. Formal physical therapy for passive and active-assisted motion begins at 4 weeks, while strengthening exercises are initiated at 8 weeks. Radiographs are regularly checked in the postoperative period to monitor fracture reduction and document healing.
Discussion
Arthroscopic management of greater tuberosity fractures allows for anatomic reduction and biomechanically stable fixation while avoiding the morbidity associated with traditional open procedures. There are key advantages inherent to both the arthroscopic approach and the suture-anchor fixation construct (Table 2). These features make this technique a viable alternative to traditional open treatment.
Table 2.
Advantages and Disadvantages for the Arthroscopic Management of Displaced Greater Tuberosity Fractures
| Minimally invasive with decreased blood loss and soft-tissue disruption |
| Improved evaluation and treatment of other injured shoulder structures |
| Reduced radiation exposure for patient and surgeon |
| Increased biomechanical strength with suture anchor constructs |
| Disadvantages |
| Technically challenging with early learning curve |
| Longer operative time than open procedures |
| Risks inherent to arthroscopic surgery (fluid extravasation, cartilage injury, neurovascular injury) |
The minimally invasive nature of arthroscopy results in less soft tissue disruption, decreased blood loss, and a cosmetically-favorable surgical scar. This may result in reduced patient discomfort, less stiffness, and earlier return to function. Liao et al.13 demonstrated improved postoperative range of motion, greater American Shoulder and Elbow Surgeons scores, and lower reoperation rates with arthroscopic fixation over traditional ORIF for these fractures in a nonrandomized retrospective case series of 32 patients. In addition, the arthroscopic camera can be used to visualize the entire glenohumeral joint and subacromial space, with treatment of any coexisting shoulder pathology at the index surgery. Labral injury can occur with tuberosity fractures that occur secondary to a glenohumeral instability event. Injury to the rotator cuff tendons can also occur and may be frequently missed in patients treated nonoperatively or with ORIF. Kim and Ha14 reported the presence of symptomatic partial articular-sided rotator cuff tears requiring surgery in 23 patients after conservative treatment of minimally displaced greater tuberosity fractures. Addressing all shoulder pathology at the time of initial arthroscopic surgery is cost effective, enhances recovery times, and improves overall patient satisfaction.
Advantages to fixation with a suture anchor construct include excellent strength, low profile implants, and the ability to broadly distribute compressive loads. Lin et al.8 demonstrated superior biomechanical strength in greater tuberosity fixation with suture anchors over screws in a cadaveric study, both in cyclical load force to displacement and catastrophic failure. In their study, all failures with screw fixation occurred with screw pullout.8 Seppel et al.15 reported favorable biomechanical results with single-row and double-row repair in a cadaver study, reinforcing either as a viable option for this injury pattern. Suture anchors also avoid the risk of intra-articular penetration inherent to screw-based constructs. The suture anchor-based repair also allows incorporation of rotator cuff tendons, potentially reducing strain at the fracture site and addressing partial rotator cuff injuries. This is particularly useful in comminuted or thin “eggshell” fractures, where purchase within the bone is suboptimal.
The main disadvantage with this procedure is potentially increased operative time, largely attributable to its technical demands, and the learning curve for surgeons not experienced with this technique.13 In their comparative study, Liao et al.13 demonstrated at 55% increase in operative time with the arthroscopic technique. This may be minimized in surgeons well versed in arthroscopic rotator cuff repair, as the technical skills and instrumentation are similar in both procedures. Another potential downside of this technique is increased cost due to longer operative times and more expensive implants. This may be offset by lower rates of postoperative stiffness and fewer reoperations, although no detailed cost analysis between open and arthroscopic surgery has been reported in the literature for this injury.
The authors believe that this arthroscopic technique is useful in treating displaced greater tuberosity fractures, with several advantages over traditional ORIF. Our technique incorporates equipment and principles commonly used in rotator cuff repair. We believe most isolated, displaced fractures can be treated in this manner with careful planning and surgical precision (Fig 8).
Fig 8.
Radiographic images of a right shoulder in the anteroposterior plane, demonstrating a greater tuberosity fracture (arrows). Preoperative displacement of the fracture (left image) is corrected to the anatomic position after arthroscopic fixation (right image). (GT, greater tuberosity fracture.)
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.F. reports consulting income from Smith & Nephew and research and educational support from Arthrex, Mitek, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Narrated video of arthroscopic greater tuberosity fracture fixation in 2 patients. The first case demonstrates the classic posteromedial displacement of this fracture pattern from the pull of the infraspinatus tendon. An anterolateral suture anchor placed well away from the fracture bed is used to correct this displacement. The second case demonstrates superomedial displacement of the fracture fragment. Provisional reduction is performed with a spinal needle, which helps guide the position of the anchor. Anchor placement at the margin of the fracture site is demonstrated, with care to gain appropriate purchase of the anchor with precise starting position and trajectory. Retrograde suture passage in a horizontal mattress pattern is shown. Tensioning and later tying the sutures facilitates anatomic reduction, which can be confirmed from subacromial and glenohumeral views. Note the restoration of rotator cuff position just medial to the fracture site in each view.
References
- 1.Lind T., Kroner K., Jensen J. The epidemiology of fractures of the proximal humerus. Arch Orthop Trauma Surg. 1989;108:285–287. doi: 10.1007/BF00932316. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown C.M., Garg A., McQueen M.M. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 3.DeBottis D., Anavian J., Green A. Surgical management of isolated greater tuberosity fractures of the proximal humerus. Orthop Clin N Am. 2014;45:207–218. doi: 10.1016/j.ocl.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Yin B., Moen T.C., Thompson S.A., LU Bigliani, Ahmad C.S., Levine W.N. Operative treatment of isolated greater tuberosity fractures: retrospective review of clinical and functional outcomes. Orthopedics. 2012;35:e807–e814. doi: 10.3928/01477447-20120525-17. [DOI] [PubMed] [Google Scholar]
- 5.Rouleau D.M., Mutch J., Laflamme G.Y. Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg. 2016;24:46–56. doi: 10.5435/JAAOS-D-14-00289. [DOI] [PubMed] [Google Scholar]
- 6.Platzer P., Kutscha-Lissberg F., Lehr S., Vecsei V., Gaebler C. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury. 2005;36:1185–1189. doi: 10.1016/j.injury.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 7.Godin J.A., Katthagen J.C., Fritz E.M., Pogorzelski J., Millett P.J. Arthroscopic treatment of greater tuberosity avulsion fractures. Arthrosc Tech. 2017;6:e777–e783. doi: 10.1016/j.eats.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin C.L., Hong C.K., Jou I.M., Lin C.J., Su F.C., Su W.R. Suture anchor versus screw fixation for greater tuberosity fractures of the humerus—a biomechanical study. J Orthop Res. 2012;30:423–428. doi: 10.1002/jor.21530. [DOI] [PubMed] [Google Scholar]
- 9.Yoon T.H., Choi C.H., Choi Y.R., Oh J.T., Chun Y.M. Clinical outcomes of minimally invasive open reduction and internal fixation by screw and washer for displaced greater tuberosity fracture of the humerus. J Shoulder Elbow Surg. 2018;27:e173–e177. doi: 10.1016/j.jse.2017.11.029. [DOI] [PubMed] [Google Scholar]
- 10.Kim D.R., Noh Y.M., Lee S.Y. Arthroscopic reduction and suture bridge fixation of a large displaced greater tuberosity fracture of the humerus. Arthrosc Tech. 2019;8:e975–985. doi: 10.1016/j.eats.2019.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ji J.H., Kim W.Y., Ra K.H. Arthroscopic double-row suture anchor fixation of minimally displaced greater tuberosity fractures. Arthroscopy. 2007;23:1133.e1–1133.e4. doi: 10.1016/j.arthro.2006.11.029. [DOI] [PubMed] [Google Scholar]
- 12.Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Arthroscopic fixation for displaced greater tuberosity fracture using the suture-bridge technique. Arthroscopy. 2008;24:120.e1–120.e3. doi: 10.1016/j.arthro.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Liao W., Zhang H., Li Z., Li J. Is arthroscopic technique superior to open reduction internal fixation in the treatment of isolated displaced greater tuberosity fractures? Clin Orthop Relat Res. 2016;474:1269–1279. doi: 10.1007/s11999-015-4663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim S.H., Ha K.I. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy. 2000;16:695–700. doi: 10.1053/jars.2000.9237. [DOI] [PubMed] [Google Scholar]
- 15.Seppel G., Saier T., Martetschlager F. Single versus double row suture anchor fixation for greater tuberosity fractures- a biomechanical study. BMC Musculoskelet Disord. 2017;18:506. doi: 10.1186/s12891-017-1868-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Narrated video of arthroscopic greater tuberosity fracture fixation in 2 patients. The first case demonstrates the classic posteromedial displacement of this fracture pattern from the pull of the infraspinatus tendon. An anterolateral suture anchor placed well away from the fracture bed is used to correct this displacement. The second case demonstrates superomedial displacement of the fracture fragment. Provisional reduction is performed with a spinal needle, which helps guide the position of the anchor. Anchor placement at the margin of the fracture site is demonstrated, with care to gain appropriate purchase of the anchor with precise starting position and trajectory. Retrograde suture passage in a horizontal mattress pattern is shown. Tensioning and later tying the sutures facilitates anatomic reduction, which can be confirmed from subacromial and glenohumeral views. Note the restoration of rotator cuff position just medial to the fracture site in each view.
Narrated video of arthroscopic greater tuberosity fracture fixation in 2 patients. The first case demonstrates the classic posteromedial displacement of this fracture pattern from the pull of the infraspinatus tendon. An anterolateral suture anchor placed well away from the fracture bed is used to correct this displacement. The second case demonstrates superomedial displacement of the fracture fragment. Provisional reduction is performed with a spinal needle, which helps guide the position of the anchor. Anchor placement at the margin of the fracture site is demonstrated, with care to gain appropriate purchase of the anchor with precise starting position and trajectory. Retrograde suture passage in a horizontal mattress pattern is shown. Tensioning and later tying the sutures facilitates anatomic reduction, which can be confirmed from subacromial and glenohumeral views. Note the restoration of rotator cuff position just medial to the fracture site in each view.



